Abstract
Aim:
The aim of this article is to estimate prevalence of menopausal symptoms among women in the menopausal age group and study the urban-rural differences.
Methods and Design:
Analytical cross-sectional study conducted in rural and urban field practice areas of a tertiary care center affiliated to Medical College, where 290 women (145 each from urban and rural areas) were interviewed to measure prevalence of menopausal symptoms. Forty-one symptoms were divided into ‘Psycho-somatic’ (17 symptoms), ‘genito-urinary (9 symptoms)’ and musculo-skeletal (5 symptoms) domains. The prevalence of each of these symptoms is reported as proportion and the differences in the median scores in the two groups were tested using Mann-Whitney U test.
Results:
From among 145 women each, in urban and rural settings, most common psychosomatic symptoms were physical exhaustion-fatigue (73.1%), difficulty climbing stairs (59.3%), sleep problems (45.2%), body ache (43.4%), and hot flushes (41.4%). Among the urban participants, most common was physical exhaustion (42.1%), difficulty climbing stairs (62.1%), anger (46.9%), sleep problems (45.5%), and irritability (42.1%), while among the rural participants they were physical exhaustion (66.2%), difficulty climbing stairs (56.6%), insomnia (54.5%), and body ache (46.2%). Most common genito-urinary symptoms overall and in rural areas were urinary urgency (35.9% and 38.6%), increased frequency of urine (31.7% and 37.2%) and incontinence (30% and 35.2% respectively). Among the urban women, common symptoms were urinary urgency (33.1%) followed by itching of private parts (30.3%) and increased frequency of urination (26.2%). Among musculo-skeletal symptoms, joint pain (74.1%, 74.5%, 73.8%) was the most common symptom followed by joint and muscular discomfort (71.7%, 73.8%, 69.7%) among the overall, urban and rural participants. There was a significant difference in the median psychosomatic score as per the symptoms experienced by the urban and rural participants (U = 36, Z statistic = 2.31, and P = 0.02). However, there was no significant difference in the scores for genito-urinary and musculo-skeletal symptoms; thereby, median scores under both these domains were almost similar in both urban and rural groups
Conclusion:
There was significant difference in the median psychosomatic score as per the symptoms experienced by the urban and rural participants however; there was no significant difference in genito-urinary and musculo-skeletal symptom scores.
Keywords: Climacteric, menopause, rural, urban, women’s health
Introduction
Menopause, as defined by the World Health Organization,[1] is a public health problem with a varied range of symptoms and signs among different age groups of women that affect the way routine activities are carried out, as well as the quality of life.[2,3,4] The loss of fertility is often deeply felt by women and is associated with a gamut of emotional and social effects and feelings, alongside the other associated menopausal symptoms due to depletion of estrogen.[5,6]
Though much literature is available on women’s health and reproductive issues, there is very less content on issues, guidelines, and healthcare services related to menopause,[7,8,9,10,11,12,13] both in urban and rural settings. Studies and reviews to see associations between menopausal symptoms and age, education and occupation have been done.[14,15] It is important to study menopausal symptoms in rural and urban settings in order to identify the symptoms to focus on and direct necessary healthcare measures with optimal resource utilization.
In this study, a local tool was used for rating of the menopausal symptoms among women in Vadodara, using factor analysis method,[16,17,18] to measure the prevalence of three set of symptoms: psycho-somatic, genito-urinary, and musculo-skeletal.
The findings of this study aim to increase the body of knowledge regarding the urban-rural differences in menopausal symptoms and increase the information we have for facilitating better treatment options. The information gained from this study can be put to good use at the level of general practitioners and family physicians; who are often the first point of contact for any such symptoms related to menopause. The knowledge regarding differences in symptoms in the rural and urban areas can help tackle the local menopausal health issues in a better way.
Material and Methods
This is an analytical cross-sectional study for which the pilot was conducted at rural and urban field practice area of health centers of a Medical College in Central Gujarat. Permission to conduct the study was obtained from the Scientific Review Committee and Institutional Ethics Committee for Human Research (IECHR).
The study included women in the menopausal age group between 45 and 55 years, as defined by the Indian Menopause Society.[3] Exclusion criteria included women below the age of 45 years or above the age of 55 years and those women in the age group of 45-55 years who did not give consent.
Two hundred and ninety women (145 each) were interviewed from rural and urban areas, using a validated tool based on the International MRS and a local instrument for signs and symptoms during menopause. A list of all women between 45 and 55 years was collected from the family registers available at Anganwadi centers. The women participants for the study were informed about the study and data collection with the help of Anganwadi workers, Anganwadi Helpers, and Community Volunteers, a week before the date of data collection.
The participants were assured of confidentiality and written informed consent was taken prior to the interview. A structured interview guide was used to elicit menopausal symptoms commonly experienced by these women and factors associated with them. In all, 41 symptoms were divided into ‘Psycho-somatic’ (17 symptoms), ‘genito-urinary’ (9 symptoms), and ‘musculo-skeletal’ (5 symptoms) domains.
All the symptoms were assessed in the vernacular language using Likert scale for severity of symptoms. If the answer was ‘symptom absent’, that is, ‘None’ the score given was ‘zero’. If the symptoms were present, that is, ‘Yes’, the women were further asked to grade the symptoms experienced by them, that is, mild, moderate, severe, very severe, based on which a score of ‘1’, ‘2’, ‘3’, ‘4’ was given, respectively. Therefore, a maximum score for psychosomatic symptoms was 108, for genito-urinary 36 and for musculo-skeletal 20.
The prevalence of each of these symptoms as well as their median scores was calculated and difference in the scores among the rural and urban women was assessed using Mann-Whitney U test. P value of less than 0.05 is considered statistically significant.
Results
The study included 145 participants each from urban and rural areas of the city. The median (IQR) age of urban women was 48 (46-53) years while that of rural women was 50 (47-54) years. Among them, 83.45% and 74.48% of the urban and rural participants were married. Among the urban women participants, 54.5% were literate, while among the rural women 45.5% were literate (Chi-square = 4.43, P = 0.03). Almost one-thirds of women in the urban area were from Classes IV and V socioeconomic status, while 84.83% from among the rural women were from Class V socioeconomic status, as per Modified Prasad’s classification.
Age at menarche was 14 (13-15) years in both the groups. Regular cycles were more common in urban area (116/145) compared to rural women (88/145) among women. Pre-menstrual syndrome was twice more common in rural women compared to urban, while dysmenorrhea was experienced by one-third of them. Menopause was attained in 93/145 and 117/145 women in the urban and rural group (Chi-square = 9.94, P = 0.002). Median BMI was higher in the urban as compared to rural women participants [24.84 (21.3-27.9) and 21.1 (18.1-24.9)], respectively.
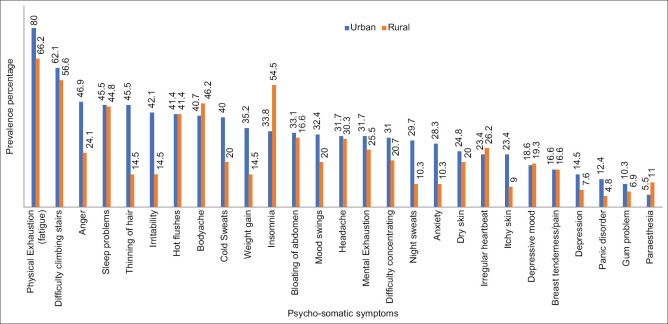
Figure 1 shows the psychosomatic symptoms experienced by the participants overall and in urban and rural groups. The most common psychosomatic symptom experienced by the participants was physical exhaustion-fatigue (73.1%), followed by difficulty climbing stairs (59.3%), sleep problems (45.2%), body ache (43.4%), and hot flushes (41.4%). Among the urban participants, most common was physical exhaustion (42.1%), difficulty climbing stairs (62.1%), anger (46.9%), sleep problems (45.5%), and irritability (42.1%), while among the rural participants they were physical exhaustion (66.2%), difficulty climbing stairs (56.6%), insomnia (54.5%), and body ache (46.2%) [Table 1].
Figure 1.
Prevalence of psychosomatic symptoms among women in the peri-enopausal age group in urban and rural area
Table 1.
Prevalence of psychosomatic symptoms among women in the peri-menopausal age group in urban and rural Vadodara
| Symptoms present | Total n=290 | Urban n=145 | Rural n=145 | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| n (%) | Median | n (%) | Median | n (%) | Median | |
| Hot flushes | 120 (41.4) | 0 (0-1) | 60 (41.4) | 0 (0-1) | 60 (41.4) | 0 (0-1) |
| Cold Sweats | 87 (30.0) | 0 (0-1) | 58 (40.0) | 0 (0-1) | 29 (20.0) | 0 (0-0) |
| Night sweats | 58 (20.0) | 0 (0-0) | 43 (29.7) | 0 (0-1) | 15 (10.3) | 0 (0-0) |
| Sleep problems | 131 (45.2) | 0 (0-1) | 66 (45.5) | 0 (0-1) | 65 (44.8) | 0 (0-1) |
| Insomnia | 128 (44.1) | 0 (0-1) | 49 (33.8) | 0 (0-1) | 79 (54.5) | 1 (0-1) |
| Depressive mood | 55 (19.0) | 0 (0-0) | 27 (18.6) | 0 (0-0) | 28 (19.3) | 0 (0-0) |
| Mood swings | 76 (26.2) | 0 (0-1) | 47 (32.4) | 0 (0-1) | 29 (20.0) | 0 (0-0) |
| Anger | 103 (35.5) | 0 (0-1) | 68 (46.9) | 0 (0-1) | 35 (24.1) | 0 (0-0) |
| Irritability | 82 (28.3) | 0 (0-1) | 61 (42.1) | 0 (0-1) | 21 (14.5) | 0 (0-0) |
| Anxiety | 56 (19.3) | 0 (0-0) | 41 (28.3) | 0 (0-1) | 15 (10.3) | 0 (0-0) |
| Panic disorder | 25 (08.6) | 0 (0-0) | 18 (12.4) | 0 (0-0) | 07 (04.8) | 0 (0-0) |
| Breast tenderness/pain | 48 (16.6) | 0 (0-0) | 24 (16.6) | 0 (0-0) | 24 (16.6) | 0 (0-0) |
| Difficulty concentrating | 75 (25.9) | 0 (0-1) | 45 (31.0) | 0 (0-1) | 30 (20.7) | 0 (0-0) |
| Physical exhaustion (fatigue) | 212 (73.1) | 1 (0-2) | 116 (80.0) | 1 (1-2) | 96 (66.2) | 1 (0-2) |
| Mental exhaustion | 83 (28.6) | 0 (0-1) | 46 (31.7) | 0 (0-1) | 37 (25.5) | 0 (0-1) |
| Difficulty climbing stairs | 172 (59.3) | 1 (0-1.25) | 90 (62.1) | 1 (0-2) | 82 (56.6) | 1 (0-1) |
| Dry skin | 65 (22.4) | 0 (0-0) | 36 (24.8) | 0 (0-.5) | 29 (20.0) | 0 (0-0) |
| Thinning of hair | 87 (30.0) | 0 (0-1) | 66 (45.5) | 0 (0-1) | 21 (14.5) | 0 (0-0) |
| Weight gain | 72 (24.8) | 0 (0-.25) | 51 (35.2) | 0 (0-1) | 21 (14.5) | 0 (0-0) |
| Headache | 90 (31.0) | 0 (0-1) | 46 (31.7) | 0 (0-1) | 44 (30.3) | 0 (0-1) |
| Body ache | 126 (43.4) | 0 (0-1) | 59 (40.7) | 0 (0-1) | 67 (46.2) | 0 (0-1) |
| Depression | 32 (11.0) | 0 (0-0) | 21 (14.5) | 0 (0-0) | 11 (07.6) | 0 (0-0) |
| Bloating of abdomen | 93 (32.1) | 0 (0-1) | 48 (33.1) | 0 (0-1) | 45 (31.0) | 0 (0-1) |
| Irregular heartbeat | 72 (24.8) | 0 (0-.25) | 34 (23.4) | 0 (0-0) | 38 (26.2) | 0 (0-1) |
| Gum problem | 25 (08.6) | 0 (0-0) | 15 (10.3) | 0 (0-0) | 10 (06.9) | 0 (0-0) |
| Itchy skin | 47 (16.2) | 0 (0-0) | 34 (23.4) | 0 (0-0) | 13 (09.0) | 0 (0-0) |
| Paresthesia | 24 (08.3) | 0 (0-0) | 08 (05.5) | 0 (0-0) | 16 (11.0) | 0 (0-0) |
Least common symptoms experienced by the study participants were gum problems, panic disorder, and paresthesia. It was also noted that 14.5% women in urban and 7.6% women in rural settings met the criteria of being depressed. Most common genito-urinary symptoms overall and in the rural areas are urinary urgency (35.9% and 38.6%), increased frequency of urine (31.7% and 37.2%), and incontinence (30%and 35.2%). In the urban women, common symptoms were urinary urgency (33.1%) followed by itching of vaginal or private parts (30.3%) and increased frequency of urination (26.2%) [Table 2; Figure 2].
Table 2.
Prevalence of genito-urinary symptoms among women in the peri-menopausal age group in urban and rural Vadodara
| Symptoms present | Total n=290 | Urban n=145 | Rural n=145 | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| n (%) | Median | n (%) | Median | n (%) | Median | |
| Urinary urgency | 104 (35.9) | 0 (0-1) | 48 (33.1) | 0 (0-1) | 56 (38.6) | 0 (0-1) |
| Sexual dissatisfaction* | 31 (13.5) | 0 (0-0) | 18 (14.9) | 0 (0-0) | 13 (12.0) | 0 (0-0) |
| Dyspareunia * | 20 (08.7) | 0 (0-0) | 12 (09.9) | 0 (0-0) | 08 (07.4) | 0 (0-0) |
| (Vaginal/private parts) Irritation | 46 (15.9) | 0 (0-0) | 32 (22.1) | 0 (0-0) | 14 (09.7) | 0 (0-0) |
| Vaginal/private parts Itching | 83 (28.6) | 0 (0-1) | 44 (30.3) | 0 (0-1) | 39 (26.9) | 0 (0-1) |
| Pruritis vulvae | 68 (23.4) | 0 (0-0) | 29 (20.0) | 0 (0-0) | 39 (26.9) | 0 (0-1) |
| Dysuria | 23 (07.9) | 0 (0-0) | 07 (04.8) | 0 (0-0) | 16 (11.0) | 0 (0-0) |
| Increased frequency of urine | 92 (31.7) | 0 (0-1) | 38 (26.2) | 0 (0-1) | 54 (37.2) | 0 (0-1) |
| Incontinence | 87 (30.0) | 0 (0-1) | 36 (24.8) | 0 (0-.5) | 51 (35.2) | 0 (0-1) |
*n=229, n=121, n=108 for total, urban and rural participants (currently married)
Figure 2.

Prevalence of genito-urinary symptoms among women in the peri-menopausal age group in urban and rural area
Among the musculo-skeletal symptoms, joint pain (74.1%, 74.5%, 73.8%) was the most common symptom followed by joint and muscular discomfort (71.7%, 73.8%, 69.7%) overall, and among urban and rural participants. This was followed by difficulty in ‘get up and go process’ in all and rural women (55.5% and 58.6%, respectively) and difficulty in getting up from the chair (58.6%) in urban women participants. Muscle pain was a generalized symptom, which was least experienced by them [Table 3; Figure 3].
Table 3.
Prevalence of musculo-skeletal symptoms among women in the peri-menopausal age group in urban and rural Vadodara
| Symptoms present | Total n=290 | Urban n=145 | Rural n=145 | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| n (%) | Median | n (%) | Median | n (%) | Median | |
| Joint and muscular discomfort | 208 (71.7) | 1 (0-1) | 107 (73.8) | 1 (0-1) | 101 (69.7) | 1 (0-1) |
| Difficulty getting up from chair | 159 (54.8) | 1 (0-1) | 85 (58.6) | 1 (0-1) | 74 (51.0) | 1 (0-1) |
| Difficulty in ‘get up and go’ process | 161 (55.5) | 1 (0-1) | 76 (52.4) | 1 (0-1) | 85 (58.6) | 1 (0-1) |
| Muscle pain | 153 (52.8) | 1 (0-1) | 86 (59.3) | 1 (0-1) | 67 (46.2) | 0 (0-1) |
| Joint pain | 215 (74.1) | 1 (0-2) | 108 (74.5) | 1 (0-2) | 107 (73.8) | 1 (0-2) |
Figure 3.

Prevalence of musculo-skeletal symptoms among women in the peri-menopausal age group in urban and rural area
The Median Psychosomatic, genito-urinary, and musculo-skeletal score for all the women included in the study as well as the urban and rural women are shown in Table 4 and a box-and-whisker diagram for visual comparison in Figure 4.
Table 4.
Median Psychosomatic, genito-urinary, and musculo-skeletal scores of women in the peri-menopausal age group in urban and rural Vadodara
| Symptoms’ Score | Total n=290 | Urban n=145 | Rural n=145 | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Median IQR | Min-max | Median IQR | Min-max | Median IQR | Min-max | |
| Psychosomatic | 9 (5-14) | 0-31 | 10 (6-15) | 0-31 | 8 (5-12) | 1-27 |
| U*=36.00, P=0.02 | ||||||
| Z#=2.311 | ||||||
| Genito-urinary | 2 (0-4) | 0-15 | 2 (0-4) | 0-15 | 2 (0-4) | 0-13 |
| U=684.50, P=1.00 | ||||||
| Z=0.00 | ||||||
| Musculo-skeletal | 4 (2-6) | 0-14 | 4 (2-6) | 0-14 | 4 (2-6) | 0-12 |
| U=420.50, P=1.00 | ||||||
| Z=0.00 | ||||||
| Total | 15.5 (10-21.25) | 17 (11-23) | 1-45 | 14 (10-19.25) | 3-46 | |
| U=8868.50, P=0.02 | ||||||
| Z=2.304 | ||||||
*Mann-Whitney U# Z statistic, corrected for ties
Figure 4.

Median Psychosomatic, genito-urinary, and musculo-skeletal scores for the peri-menopausal women in urban and rural area
There was a significant difference in the median psychosomatic score as per the symptoms experienced by the urban and rural participants (U = 36, Z statistic = 2.31, and P = 0.02). However, there was no significant difference in the scores for genito-urinary and musculo-skeletal symptoms; thereby, median scores under both these domains were almost similar in both urban and rural groups.
Median (IQR) number of symptoms experienced by the women was 12 (8-17). The minimum and maximum number of symptoms experienced was 0 and 31, respectively. For the urban women the median (IQR) was 14 (9-18) while it was 12 (8-15.5) for the rural women [Figure 4]. There was no significant correlation in the mean number of symptoms experienced and the total score of symptoms [Spearman’s correlation coefficient  Rho = (-0.08), P = 0.3] and between duration of menopause and the score of symptoms
Rho = (-0.08), P = 0.3] and between duration of menopause and the score of symptoms  Rho = (-0.004), P = 0.95].
Rho = (-0.004), P = 0.95].
There was a significant difference in the total scores of symptoms experienced by the urban and rural women participants in the study (Z = 2.30, P-0.02).
Discussion
Menopause affects the lives of millions of women globally and will be an issue of increasing concern as the population ages over the next few decades.[3,19,20] Age of menopause is said to be genetically determined and is unaffected by race, socio-economic status, age at menarche, or number of prior ovulations. However, there is a vast spectrum of menopausal symptoms experienced by women, which vary with urban and rural population that could be related to a higher literacy rate and socio-economic class of urban women as compared to rural. This has also been postulated by Khademi and Cooke in their study which states that environmental factors, the socioeconomic status and the quality of health services can affect women in the menopausal age group.[21,22]
The purpose of conducting this study was two-fold: (1) To understand the spectrum of symptoms experienced by women of menopausal age in developing countries, by classifying them in three main categories: Psychosomatic, genito-urinary, and musculo-skeletal, and (2) To compare these symptoms between the rural and urban women in Vadodara district of Central Gujarat.
Multiple studies have shown that urban women experience more symptoms than rural women.[23,24,25] However, this study shows that even though there was a significantly higher median psychosomatic score and combined total score as per the symptoms experienced by the urban and rural participants; there was no significant difference in the scores given for genito-urinary and musculo-skeletal symptoms.
Many symptoms highlight issues related to the somatic domain, both in rural and urban areas, although the prevalence is greater in urban areas. With changing lifestyles, diet and exercise or the lack of it, these issues may be related to menopausal changes, as well as the multi-tasking activities of the modern woman.[19,23,26] The most common psychosomatic symptom experienced in the study group was physical exhaustion-fatigue, followed by difficulty climbing stairs, sleep problems, body ache, and hot flushes. Among the urban women participants most common was physical exhaustion, difficulty climbing stairs, anger, sleep problems and irritability, while among the rural participants they were physical exhaustion, difficulty climbing stairs, insomnia, and body ache. Some studies show an increased rate of hot flushes in rural women,[27,28] while some advocate more prevalence in urban women.[28,29] However, our study saw that despite being one of the five most common symptoms, hot flushes have equal prevalence in rural and urban women. We found physical exhaustion as highly prevalent and a more concerning symptom, which is in line with a similar study which was carried out on 500 women between 40 and 60 years of age.[29] Hence is it prudent to address physical exhaustion and fatigue adequately and not dismiss it due to its vague nature.
Depression, though agreed by some (14.5% in urban and 7.6% in rural), is a matter of concern, as this summates the overall experience of their quality of life.[12,30,31,32] Studies have also shown anxiety to be more common in urban than rural women.[19,23] However, on the other hand, it is also important to note that some studies have found an increased rate of depression amongst rural women.[25,28,33] This variability shows that depression may or may not be related directly to menopause, however, in the wake of the current World Health Day 2017 theme on Depression: Let’s Talk,[34] this gives an impetus to the public health community to talk about it in the peri-menopausal group and provide counseling accordingly.
It was difficult to estimate the prevalence and assess genito-urinary symptoms and complaints related to intercourse history viz. sexual dissatisfaction and dyspareunia and needed more probing. With regard to decreased sexual desire, some studies showed a higher prevalence in urban women,[12,23,28] while some argued that women in rural areas more commonly suffer from dyspareunia, vaginal dryness, and loss of sexual interest.[28] This variation could be explained by the difficulty in elicitation of information due to cultural barriers. Contrary to expectation, rural women were relatively more open about their sexual problems than the urban women. However, these issues were not considered as ‘abnormal’ as women consider ‘Menopause as end of sexuality.’ Even uro-genital complaints were found to be more prevalent among urban women.[12,23]
While joint pain was the most common symptom, which was equally present in both urban and rural women, muscle pain was a generalized symptom, which was least experienced by them. This is in contrast to the results in the study obtained by Bernis and Reher[33,35] done in Spain and another study conducted in Australia[29] which found an equally high prevalence of both joint and muscle pain in menopausal women. This could be explained by the higher prevalence of labor class women in India, which might attribute to a lower degree of muscle pain as compared to joint pain due to early introduction of strenuous activities which cause muscle training. This significant variation among countries further reinforces the need for more studies for better understanding of symptom prevalence.
Finally, on analyzing the intensity of symptoms, it was found that overall severity of symptoms was similar in urban and rural women except dry skin, thinning of hair and muscle pain, which was more in urban women, maybe due to more awareness, while irregular heartbeat and bloating of abdomen was more in rural women, which could be attributed to a delayed health seeking behavior.
While our study takes a step forward in highlighting the differences in menopausal symptoms between rural and urban women, there are certain limitations which were hard to overcome. Due to the social difference in the literacy rate and socioeconomic status between rural and urban population, a significantly higher rate of literacy was found in the women belonging to urban households as compared to women coming from rural areas. More women in rural Vadodara were also found to fall into category five of modified Prasad’s classification based on socioeconomic status, as compared to urban women, which could be attributed to lands and farms owned by families in rural areas, wherein they cultivate their own food or work as laborers in other farms and get the produce in return instead of money.
It was found that from the study population, which included women facing some peri-menopausal/menopausal symptoms, more women from the rural group had already attained menopause. Having employed a purposive sampling technique, any difference in the area of stay and attainment of menopause does not hold much significance, however, it shows that relatively earlier menopause could be a possibility in rural areas.
Thus, this is an analytical study that categorizes menopausal symptoms into three components, of these, significant differences among rural-urban women were found only in the median psychosomatic score. Some issues were more prevalent in urban women accounting to their lifestyle and modern ways of living. it highlights to conduct more such studies for a greater geographical region, thus giving a way ahead to tackle these menopausal health issues in a better way. It also gives areas to focus on the mainstay symptoms, differently targeting rural and urban menopausal women.
Conclusion
Women in menopausal age group tend to suffer from a multitude of symptoms, some of which are universally prevalent across the globe. However, there is a significant difference in the distribution of these symptoms between rural and urban women, which also tends to vary geographically. Further studies to identify the root cause of these variations and identify confounding symptoms would help to target appropriate modalities of symptom management to overcome this challenge and provide a healthy method of dealing with menopausal symptoms for women across the world.
Declaration of patient consent
The authors certify that they have obtained all appropriate participant consent forms. In the form, the participant has given her consent for other clinical information to be reported in the journal. The participants understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We acknowledge Dr V S Mazumdar, Professor and Head, Department of PSM, Medical College Baroda and Dr A T Leuva, Dean, Medical College Baroda, for their constant support during the conduct of this study.
References
- 1.Jha UP, Vaidya R. Elsevier; 2008. Menopause. [Google Scholar]
- 2.Meeta M, Digumarti L, Agarwal N, Vaze N, Shah R, Malik S. Clinical practice guidelines on menopause:*An executive summary and recommendations:Indian Menopause Society 2019–2020. J Midlife Health. 2020;11:55–95. doi: 10.4103/jmh.JMH_137_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meeta, Digumarti L, Agarwal N, Vaze N, Shah R, Malik S. Clinical practice guidelines on menopause:An executive summary and recommendations. J Midlife Health. 2013;4:77–106. doi: 10.4103/0976-7800.115290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pal A, Hande D, Khatri S. Assessment of menopausal symptoms in perimenopause and postmenopause women above 40 years in rural area. Int J Healthc Biomed Res. 2013;1:166–74. [Google Scholar]
- 5.Banaczek Z, Saracen A. Life satisfaction and self-esteem among women in the menopausal time. Wiad Lek. 2016;69:174–9. [PubMed] [Google Scholar]
- 6.Hilditch JR, Lewis J, Peter A, van Maris B, Ross A, Franssen E, et al. A menopause-specific quality of life questionnaire :Development and psychometric properties. Maturitas. 1996;24:161–75. doi: 10.1016/s0378-5122(96)82006-8. [DOI] [PubMed] [Google Scholar]
- 7.The Health Status Of Women Health Essay. Availablefrom: http://www.uniassignment.com/essay-samples/health/the-health-status-of-women-health-essay.php .
- 8.Raj A. Gender equity and universal health coverage in India. Lancet. 2011;377:618–9. doi: 10.1016/S0140-6736(10)62112-5. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. Moving forward on the SDGs [Google Scholar]
- 10.The menopause |Women's Health Concern. Available from: https://www.womens-health-concern.org/help-and-advice/factsheets/menopause/
- 11.Quick J, Jay J, Langer A. Improving women's health through universal health coverage. PLoS Med. 2014;11:e1001580. doi: 10.1371/journal.pmed.1001580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Joseph N, Nagaraj K, Vittal S, Nelliyanil M, Roa PPJ. Assessment of menopausal symptoms among women attending various outreach clinics in South Canara District of India. J Midlife Health. 2014;5:84–90. doi: 10.4103/0976-7800.133996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Poomalar GK, Arounassalame B. The quality of life during and after menopause among rural women. J Clin Diagnostic Res. 2013;7:135–9. doi: 10.7860/JCDR/2012/4910.2688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ohn Mar S, Mona R. Rural-urban difference in natural menopausal age and the correlating factors. Int J Women's Health Reprod Sci. 2020;8:112–8. [Google Scholar]
- 15.Meeta, Harinarayan CV, Marwah R, Sahay R, Kalra S, Babhulkar S. Clinical practice guidelines on postmenopausal osteoporosis:An executive summary and recommendations. J Midlife Health. 2013;4:107–26. doi: 10.4103/0976-7800.115293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jahangiry L, Parviz R, Mirghafourvand M, Khazaee-Pool M, Ponnet K. The psychometric properties of the Persian menopause rating scale. BMC Womens Health. 2020;20:172. doi: 10.1186/s12905-020-01027-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.UCLA. A Practical Introduction to Factor Analysis [Internet] [Last accessed on 2022 May 16];Statistical Consulting Group. 2016 7:1–6. Available from: yhttps://stats.oarc.ucla.edu/spss/seminars/introduction-to-factor-analysis/ [Google Scholar]
- 18.Yong AG, Pearce S. A Beginner's Guide to Factor Analysis:Focusing on Exploratory Factor Analysis. Tutor Quant Methods Psychol. 2013;9:79–94. [Google Scholar]
- 19.Sharma S, Mahajan N. Menopausal symptoms and its effect on quality of life in urban versus rural women:A cross-sectional study. J Midlife Heal. 2015;6:16–20. doi: 10.4103/0976-7800.153606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ki-moon HEBan. UN Commission on Life-saving Commodities for Women and Children:Commissioners'Report 2012. [Last accessed on 2014 Sep 19]. Available from: https://www.unfpa.org/sites/default/files/pub-pdf/Final%20UN%20Commission%20Report_14sept2012.pdf .
- 21.Khademi S, Cooke MS. Comparing the attitudes of urban and rural Iranian women toward menopause. Maturitas. 2003;46:113–21. doi: 10.1016/s0378-5122(03)00182-8. [DOI] [PubMed] [Google Scholar]
- 22.Hakimi S, Haggi HB, Shojai SK, Farahbakhsh M, Farhan F. Comparing the pattern of menopausal symptoms, concern and attitudes in urban and rural postmenopausal Iranian women. J Menopausal Med. 2018;24:50–5. doi: 10.6118/jmm.2018.24.1.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sagdeo MM, Arora D. Menopausal symptoms :A comparative study in rural and urban women. JK Science. 2011;13:23–6. [Google Scholar]
- 24.K S, Ugargol A. A comparative study on postmenopausal symptoms in rural and urban women. Int J Community Med Public Heal. 2015;2:604–9. [Google Scholar]
- 25.Wilson NW, Couper ID, De Vries E, Reid S, Fish T, Marais BJ. A critical review of interventions to redress the inequitable distribution of healthcare professionals to rural and remote areas. Rural Remote Health. 2009;9:1060. [PubMed] [Google Scholar]
- 26.Dasgupta D, Ray S. Menopausal problems among rural and urban women from Eastern India. J Soc Behav Heal Sci. 2009;3:20–33. [Google Scholar]
- 27.Martínez JA, Palacios S, Chavida F, Pérez M. Urban-rural differences in Spanish menopausal women. Rural Remote Health. 2013;13:1865. [PubMed] [Google Scholar]
- 28.Malacara JM, Canto de Cetina T, Bassol S, González N, Cacique L, Vera-Ramírez ML, et al. Symptoms at pre- and postmenopause in rural and urban women from three States of Mexico. Maturitas. 2002;43:11–9. doi: 10.1016/s0378-5122(02)00077-4. [DOI] [PubMed] [Google Scholar]
- 29.Mishra GD, Brown WJ, Dobson AJ. Physical and mental health:Changes during menopause transition. Qual Life Res. 2003;12:405–12. doi: 10.1023/a:1023421128141. [DOI] [PubMed] [Google Scholar]
- 30.Jorge MP, Santaella DF, Pontes IMO, Shiramizu VKM, Nascimento EB, Cabral A, et al. Hatha Yoga practice decreases menopause symptoms and improves quality of life:A randomized controlled trial. Complement Ther Med. 2016;26:128–35. doi: 10.1016/j.ctim.2016.03.014. [DOI] [PubMed] [Google Scholar]
- 31.Kothiyal P, Sharma M. Post menopausal quality of life and associated factors- A Review. J Sci Innov Res. 2013;2:814–23. [Google Scholar]
- 32.Zang H, He L, Chen Y, Ge J, Yao Y. The association of depression status with menopause symptoms among rural midlife women in China. Afr Health Sci. 2016;16:97–104. doi: 10.4314/ahs.v16i1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bernis C, Reher DS. Environmental contexts of menopause in Spain:Comparative results from recent research. Menopause. 2007;14:777–87. doi: 10.1097/gme.0b013e31803020ff. [DOI] [PubMed] [Google Scholar]
- 34.World health day:Depression-let's talk. Indian J Soc Psychiatry. 2017;33:5. [Google Scholar]
- 35.Heinemann LA, Potthoff P, Schneider HP. International versions of the Menopause Rating Scale (MRS) Health Qual Life Outcomes. 2003;1:28. doi: 10.1186/1477-7525-1-28. [DOI] [PMC free article] [PubMed] [Google Scholar]