Abstract
Background:
People who inject drugs are vastly over-represented, often accounting for 50% of prison inmates, so, the transmission of human immunodeficiency virus (HIV), hepatitis C virus (HCV) and tuberculosis (TB) is a serious problem in many prison systems. The prevalence of HCV infection is so disproportionately high in the correctional population that one in four detainees worldwide is living with HCV and the story is similar for HIV.
Objective:
The objective of the study is to find the prevalence of HIV, HCV and dual HIV-HCV infection in the prison inmates.
Materials and Methods:
A sample of 1569 jail inmates was assessed, after obtaining formal approval from the ethical committee for assessment of the medical record of subjects, to know sero-positivity for HIV and HCV. The data generated is then analysed.
Results:
The results show a very high point prevalence of HIV (10.0%) and HCV (31.6%) in the jail inmates, which is 40 and 30 times higher, respectively, as compared to the national average. A staggering 8.5% of the inmates were found to be positive for both viruses. The sero-prevalence for mono-infection for HCV (23.1%) is found to be significantly higher compared to HIV (1.5%). The infection rate of HCV was found to be three times higher compared to HIV.
Conclusions:
Substantially high prevalence of HIV, HCV and dual HIV-HCV infection exists in the prison inmates. Data suggests high virulence for HCV compared to HIV, as both viruses have common routes of transmission. There is an urgent need to keep a constant check on the intravenous drug usage (IDU) in the prisons that is linked to the common transmission of both these blood-borne viruses.
Keywords: HCV, HIV, HIV-HCV co-infection, prevalence, prisoners
Introduction
It is estimated that more than 10.2 million people, including sentenced and pre-trial detainees, are held in detention centres worldwide.[1] There are 16 million people who inject drugs worldwide and there are an estimated 165,000 injecting drug users (IDUs) in India.[2] People who inject drugs are vastly over-represented, often accounting for 50% of prison inmates,[3] so, the transmission of human immunodeficiency virus (HIV), hepatitis C virus (HCV) and tuberculosis (TB) is a serious problem in many prison systems.[4] Global HIV prevalence is up to 50 times higher among the prison population than in the general public.[5] Due to the enhanced transmissibility of HCV by percutaneous injection, compared with that of HIV, the prevalence of HCV infection can exceed 85% among HIV-infected injection drug users.[6,7] The prevalence of HCV infection is so disproportionately high in the correctional population that one in four detainees worldwide is living with HCV.[8]
As one-third of these inmates return to their communities every year,[9] so prison health is somewhere very intimately connected to public health.[10] Inmates also often may bounce between community and correctional settings without knowing that they are carriers of HCV infection and may engage in virus-spreading behaviour.[11] So very early, it became clear that correctional facilities would offer an important place to diagnose, treat and prevent hepatitis C viral infection, so that released individuals do not spread the virus to those in the community.[12,13,14]
Among patients with chronic HCV infection, approximately one-third progress to cirrhosis, at a median time of less than 20 years.[15,16] The rate of progression increases with older age, alcoholism, male sex and HIV infection.[17,18] A meta-analysis found that HCV-HIV coinfected patients had a three-fold greater risk of progression to cirrhosis or decompensated liver disease than HCV mono-infected patients.[19] It has been similarly demonstrated that coinfected patients diagnosed with hepatocellular carcinoma tend to have a more advanced and aggressive liver disease at younger ages, associated with significantly higher mortality rates.[20] Although antiretroviral therapy (ART) appears to slow the rate of HCV disease progression in HCV-HIV coinfected patients, by preserving or restoring immune function and by reducing HIV-related immune activation and inflammation,[21,22,23] but several studies have demonstrated that the progression rate still continues to exceed that observed in patients without HIV infection.[24,25] The major contributor to mortality among HIV-HCV coinfected subjects during the highly active antiretroviral therapy (HAART) era is still a liver disease,[26,27,28] as the drug-induced liver injury following the initiation of ART is more common in HCV-HIV coinfected patients than in those with HIV mono-infection.[29] So first eradicating HCV infection with ART, may decrease the likelihood of antiretroviral (ARV)-associated liver injury.[30]
Aims and Objectives
To find the prevalence of HIV, HCV and dual HIV-HCV infection rate in prison inmates.
Materials and Methods
-
Study setting:
This study is carried out in the Modern Central Jail at Faridkot, Punjab. It has usually about 1500–1700 inmates, which includes both convicts and under-trials. There are around 80 females. There are significant numbers of inmates who have been convicted for drug-related crimes. On an average, 60–70 people come and go daily to the prison. All the new admissions in the jail are routinely tested for sero-positivity for HIV after getting their due consent.
The study was only carried out after taking an ethical approval from the Institution Review Board of the GGS Medical College and Hospital, Faridkot and the permission from jail authorities.
-
Sample selection:
This study included 1609 subjects who had been tested for HIV and their further HIV-positive status was confirmed through sequential testing as per the protocol provided by the National AIDS Control Organisation (NACO). The subjects were also tested for sero-positivity for HCV through an HCV Tri-dot test (Punjab, India) that detects all serotypes of HCV. This retrospective cross-sectional study was carried out in the year 2017 and it includes data generated in the year 2016. The inclusion criteria included all inmates who participated in the mandatory HIV and HCV testing carried out after obtaining informed consent from the inmates in the prison. The exclusion criteria included those subjects who could not be tested for HIV and HCV in the prison.
Out of 1609 subjects, 40 subjects could not be tested for HCV. So effectively, the study sample consisted of a total of 1569 subjects, who were tested for both infections and it included 1483 males and 86 females in total. A proper protocol of maintaining confidentiality and pre- and post-test counselling of inmates was adopted.
Data analysis
Results are expressed as percentages for qualitative variables.
Results
Out of 1569 subjects, 157 subjects were confirmed to be HIV positive after sequential testing and 496 confirmed sero-positive for HCV. The point prevalence for HIV came out to be 10.0%, which is 40 times the current national average. The average HIV prevalence in India is 0.26% and that of this region (state of Punjab) is 0.19%.[31]
The prevalence rate for HCV came out to be 31.6%, which is also astonishingly 31 times the current national average. The average prevalence of HCV in India currently is 1%[32] [Table 1].
Table 1.
Data from HIV and HCV testing of study sample (n=1569)
| Parameter | Number | Prevalence | ||
|---|---|---|---|---|
| 1 | Inmates who were tested for HIV and HCV | 1569 | ----- | ---- |
| 2 | Inmates who tested/confirmed positive for HIV | 157 | 157/1569×100 | 10.0% |
| 3 | Inmates who tested/confirmed positive for HCV | 496 | 496/1569×100 | 31.6% |
| 4 | Inmates who had mono-infection with HIV | 24 | 24/1569×100 | 1.5% |
| 5 | Inmates who had mono-infection with HCV | 363 | 363/1569×100 | 23.1% |
| 6 | Inmates who had dual diagnosis of HIV-HCV positive status | 133 | 133/1569×100 | 8.5% |
| 7 | HCV prevalence in HIV positive subgroup | 133 | 133/157×100 | 84.7% |
| 8 | HIV prevalence in HCV positive subgroup | 133 | 133/496×100 | 26.8% |
The point prevalence for HIV and HCV for female inmates came out to be 0% and 0.25%, respectively. The point prevalence for the dual infection of HIV and HCV came out to be 8.5% as 133 subjects tested positive for both HCV and HIV. More inmates were found to be mono-positive for HCV compared to HIV. Mono-positivity for HCV came out to be 23.1%, whereas for HIV it was a meagre 1.5% only. Data shows that among all HIV-positive subgroups, the prevalence of HCV is 84.7% and among all HCV-positive subgroups, the prevalence of HIV is 26.8%, which is one-third that of HCV. For more details, refer to Charts 1 and 2.
Chart 1.
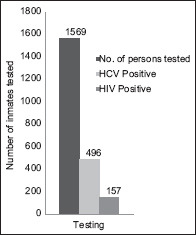
Data shows that the prevalence of HCV is nearly three times that of HIV in the sample population
Chart 2.
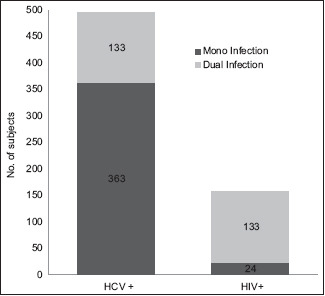
Data shows that the prevalence of HCV among HIV positive inmates is 84.7% and that of HIV among HCV positive subgroup is 26.8%
Discussion
The present study finds a very high prevalence of HIV and HCV in jail inmates, compared to the national average and it is a point of big concern. High rates of co-infection for dual HIV and HCV are also a point of concern for both further prognosis and transmission. Both these viruses are linked with IDU and the world over, prisons are places known for high usage of IDUs. As HCV and HIV share common routes for transmission, a disproportionately high mono-positivity for HCV indicates a high virulence rate of HCV compared to HIV. In the wake of the above data, it is a matter of great concern for the health authorities of the state, as there are many examples where prisons acted as a source of a local epidemic for blood-borne diseases like HIV and HCV. Keeping in view of this fact, NACO has stressed on expediting surveillance sites for blood-borne viral infections in prisons.[33] This study finds that HCV prevalence in HIV inmates is 3.2 times higher than that of HIV prevalence in HCV inmates. As both these diseases have the same mode of transmission, it can be safely concluded that the infection rate of HCV is three times more compared to HIV.
The findings of this study are in comparison to other studies that quote the high prevalence of HIV and HCV in prisons.[4] In a similar study carried out in Brazil, the presence of anti-HCV antibodies was found to be five times higher in prisons than the estimated prevalence (0.53%) for the Brazilian population.[34] The study confirms that prisons also pose a serious threat to the propagation of HIV and HCV for the public outside, due to the high prevalence and dynamic population in prison. These facts are in agreement with other research findings that have similar results.[10,11]
The major limitation of this study was that it was limited to one correctional centre only and the data only represented a particular part of the region. To get more exact prevalence, the study should be replicated in more correctional centres.
Conclusions
Substantially high prevalence of HIV, HCV and dual HIV-HCV infection exists in the prison inmates. Data suggests high virulence for HCV compared to HIV, despite the fact both viruses have common routes of transmission. There is an urgent need to keep a constant check on the IDU in the prisons which is linked to the common transmission of both these blood-borne viruses.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors would like to thank Mr. Sunny Sharma (inmate) and Dr. Rahul Khurana (inmate) for organising peer group activities among HIV-positive inmates and providing valuable support in data collection and data feeding on the computer for carrying out the analysis of this study.
References
- 1.Prison Reform International. Global Prison Trends. London: PRI; 2015. [Google Scholar]
- 2.Mathers DM, Degenhardt L, Phillips B, Wiessing L, Hickman M, Strathdee S, et al. Global epidemiology of injecting drug use and HIV among people who inject drugs:A systematic review. Lancet. 2008;372:1733–45. doi: 10.1016/S0140-6736(08)61311-2. [DOI] [PubMed] [Google Scholar]
- 3.Dolan K, Khoei EM, Brentari C, Stevens A. Oxford: The Beckley Foundation; 2007. Report 12-Prisons and Drugs:A Global Review of Incarceration, Drug Use and Drug Services. [Google Scholar]
- 4.11th General Report, European Committee for the Prevention of Torture and Inhuman or Degrading Treatment of Punishment. 2001 [Google Scholar]
- 5.Mariner J, Schleifer R. The right to health in prisons. In: Zuniga JM, Marks SP, Gostin LO, editors. Advancing the Human Right to Health. Oxford: Oxford University Press; 2013. [Google Scholar]
- 6.Sherman KE, Rouster SD, Chung RT, Rajicic N. Hepatitis C virus prevalence among patients infected with human immunodeficiency virus:A cross-sectional analysis of the US adult AIDS Clinical Trials Group. Clin Infect Dis. 2002;34:831–7. doi: 10.1086/339042. [DOI] [PubMed] [Google Scholar]
- 7.Sulkowski MS, Thomas DL. Hepatitis C in the HIV-infected person. Ann Intern Med. 2003;138:197–207. doi: 10.7326/0003-4819-138-3-200302040-00012. [DOI] [PubMed] [Google Scholar]
- 8.Lamey S, Kopinski H, Beckwith CG, Zaller ND, Jarlais DD, Hagan H, et al. Incidence and prevalence of hepatitis C in prisons and other closed settings:Results of a systematic review and meta-analysis. Hepatology. 2013;58:1215–24. doi: 10.1002/hep.26387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization 'Prisons and Health –WHO Guide'. Geneva: WHO; 2014. p. xi. [Google Scholar]
- 10.Declaration on Prison Health as Part of Public Health (Moscow Declaration), adopted in Moscow on 24 October 2003 [Google Scholar]
- 11.Fox RK, Currie SL, Evans J, Wright RL, Tobler L, Phelps B, et al. Hepatitis C virus infection among prisoners in the California state correctional system. Clin Infect Dis. 2005;41:177–86. doi: 10.1086/430913. [DOI] [PubMed] [Google Scholar]
- 12.Allen SA, Spaulding AC, Osei AM, Taylor LE, Cabral AM, Rich JD. Brief communication. treatment of chronic hepatitis C in a state correctional facility. Ann Intern Med. 2003;138:187–90. doi: 10.7326/0003-4819-138-3-200302040-00010. [DOI] [PubMed] [Google Scholar]
- 13.Hammett TM. Adopting more systematic approaches to hepatitis C treatment in correctional facilities. Ann Intern Med. 2003;138:235–6. doi: 10.7326/0003-4819-138-3-200302040-00021. [DOI] [PubMed] [Google Scholar]
- 14.Spaulding AC, Kim AY, Harzka AJ, Sullivan JC, Linas BP, Brewer A, et al. Impact of new therapeutics for hepatitis C virus infection in incarcerated populations. Top Antivir Med. 2013;21:27–35. [PMC free article] [PubMed] [Google Scholar]
- 15.Alter MJ, Margolis HS, Krawczynski K, Judson FN, Mares A, Alexander WJ, et al. The natural history of community-acquired hepatitis C in the United States. The sentinel counties chronic non-A, non-B hepatitis study team. N Engl J Med. 1992;327:1899–905. doi: 10.1056/NEJM199212313272702. [DOI] [PubMed] [Google Scholar]
- 16.Thomas DL, Astemborski J, Rai RM. The natural history of hepatitis C virus infection:Host, viral, and environmental factors. JAMA. 2000;284:450–6. doi: 10.1001/jama.284.4.450. [DOI] [PubMed] [Google Scholar]
- 17.Poynard T, Bedossa P, Opolon P. Natural history of liver fibrosis progression in patients with chronic hepatitis C. The OBSVIRC, METAVIR, CLINIVIR, and DOSVIRC groups. Lancet. 1997;349:825–32. doi: 10.1016/s0140-6736(96)07642-8. [DOI] [PubMed] [Google Scholar]
- 18.Wiley TE, McCarthy M, Breidi L, Layden TJ. Impact of alcohol on the histological and clinical progression of hepatitis C infection. Hepatology. 1998;28:805–9. doi: 10.1002/hep.510280330. [DOI] [PubMed] [Google Scholar]
- 19.Graham CS, Baden LR, Yu E, Mrus JM, Carnie J, Heeren T, et al. Influence of human immunodeficiency virus infection on the course of hepatitis C virus infection:A meta-analysis. Clin Infect Dis. 2001;33:562–9. doi: 10.1086/321909. [DOI] [PubMed] [Google Scholar]
- 20.Bourcier V, Winnock M, Ait Ahmed M, Sogni P, Pambrun E, Poizot-Martin I, et al. Primary liver cancer is more aggressive in HIV-HCV coinfection than in HCV infection. A prospective study (ANRS CO13 Hepavih and CO12 Cirvir) Clin Res Hepatol Gastroenterol. 2012;36:214–21. doi: 10.1016/j.clinre.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 21.Macias J, Berenguer J, Japon MA, Girón JA, Rivero A, López-Cortés LF, et al. Fast fibrosis progression between repeated liver biopsies in patients coinfected with human immunodeficiency virus/hepatitis C virus. Hepatology. 2009;50:1056–63. doi: 10.1002/hep.23136. [DOI] [PubMed] [Google Scholar]
- 22.Verma S, Goldin RD, Main J. Hepatic steatosis in patients with HIV-Hepatitis C Virus coinfection:Is it associated with antiretroviral therapy and more advanced hepatic fibrosis? BMC Res Notes. 2008;1:46. doi: 10.1186/1756-0500-1-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ragni MV, Nalesnik MA, Schillo R, Dang Q. Highly active antiretroviral therapy improves ESLD-free survival in HIV-HCV co-infection. Haemophilia. 2009;15:552–8. doi: 10.1111/j.1365-2516.2008.01935.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weber R, Sabin CA, Friis-Moller N, Reiss P, El-Sadr WM, Kirk O, et al. Liver-related deaths in persons infected with the human immunodeficiency virus:The D:A:D study. Arch Intern Med. 2006;166:1632–41. doi: 10.1001/archinte.166.15.1632. [DOI] [PubMed] [Google Scholar]
- 25.Kitahata MM, Gange SJ, Abraham AG, Merriman B, Saag MS, Justice AC, et al. Effect of early versus deferred antiretroviral therapy for HIV on survival. N Engl J Med. 2009;360:1815–26. doi: 10.1056/NEJMoa0807252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pineda JA, Garcia-Garcia JA, Aguilar-Guisado M, Ríos-Villegas MJ, Ruiz-Morales J, Rivero A, et al. Clinical progression of hepatitis C virus–related chronic liver disease in human immunodeficiency virus-infected patients undergoing highly active antiretroviral therapy. Hepatology. 2007;46:622–30. doi: 10.1002/hep.21757. [DOI] [PubMed] [Google Scholar]
- 27.Thein HH, Yi Q, Dore GJ, Krahn MD. Natural history of hepatitis C virus infection in HIV infected individuals and the impact of HIV in the era of highly active antiretroviral therapy:A meta-analysis. AIDS. 2008;22:1979–91. doi: 10.1097/QAD.0b013e32830e6d51. [DOI] [PubMed] [Google Scholar]
- 28.Rosenthal E, Poiree M, Pradier C, Perronne C, Salmon-Ceron D, Geffray L, et al. Mortality due to hepatitis C related liver disease in HIV-infected patients in France (Mortavic 2001 study) AIDS. 2003;17:1803–9. doi: 10.1097/00002030-200308150-00009. [DOI] [PubMed] [Google Scholar]
- 29.Aranzabal L, Casado JL, Moya J, Quereda C, Diz S, Moreno A, et al. Influence of liver fibrosis on highly active antiretroviral therapy-associated hepatotoxicity in patients with HIV and hepatitis C virus coinfection. Clin Infect Dis. 2005;40:588–93. doi: 10.1086/427216. [DOI] [PubMed] [Google Scholar]
- 30.Labarga P, Soriano V, Vispo ME, Pinilla J, Martin-Carbonero L, Castellares C, et al. Hepatotoxicity of antiretroviral drugs is reduced after successful treatment of chronic hepatitis C in HIV-infected patients. J Infect Dis. 2007;196:670–6. doi: 10.1086/520092. [DOI] [PubMed] [Google Scholar]
- 31.India HIV Estimations, Technical Report, NACO, Ministry of Health &Family Welfare, Govt. of India. 2015 [Google Scholar]
- 32.NCDC (National Centre for Disease Control). Ministry of Health &Family Welfare, Government of India. Vol 3. Newsletter; 2014 [Google Scholar]
- 33.Report of the national consultation on HIV intervention in prisons and other correctional institutions. National AIDS Control Organization, Ministry of Health &Family Welfare, Govt. of India, New Delhi. 2017 [Google Scholar]
- 34.Ferreto LED, Guedes S, Pauli FB, Rovani SS, Follador FAC, Vieira AP, et al. Seroprevalence and associated factors of HIV and Hepatitis C in Brazilian high-security prisons:A state-wide epidemiological study. PLoS One. 2021;16:e0255173. doi: 10.1371/journal.pone.0255173. [DOI] [PMC free article] [PubMed] [Google Scholar]


