Abstract
Background:
Cervical cancer is a primary preventable cancer. The current study aims to assess relevant knowledge and attitude of cervical cancer screening among female high school teachers in Hail city, Saudi Arabia.
Materials and Methods:
This cross-sectional study was conducted among female high school teachers in the Hail Province of Saudi Arabia. It is worth mentioning that Pap smear screening every 3–5 years with appropriate follow-up can reduce cervical cancer incidence by up to 80%, and abnormal results may suggest the presence of precancerous changes, allowing examination and possible preventive treatment.
Results:
Data from 387 participants were included in the final analysis. The study participants were female high school teachers. Mean age of the participants was 41.4 ± 5.3 years. Only 42% participants appeared to have good level of knowledge about cervical cancer. Fifty-eight percentage of females had not heard of it before. Only 22 (5.7%) participants had undergone Pap smear testing. A total of 182 (47.0%) participants believed that Pap smear test is a useful test and would undergo the test. Around 139 females (35.9%) will be allowing their daughters to get the human papilloma virus (HPV) vaccine.
Conclusions:
Interventions to increase cervical cancer knowledge are needed in Hail city in Saudi Arabia. In addition, further research is needed to understand and assess the effectiveness of different strategies to improve attitudes regarding cervical cancer, in order to increase the uptake of screening services.
Keywords: Cervical Cancer, HPV vaccine, knowledge and attitudes, Pap smear, Saudi Arabia
Introduction
Cancer of the cervix uteri is the fourth most common cancer among females all over the world, with an estimated 527,624 new cases and 265,672 deaths in 2012.[1] Cervical cancer is defined as a malignant disease of the cervix, usually occurring in the fifth or sixth decade of life at a mean age of 54 years.[2] The disease has a premalignant stage which generally occurs in younger women under the age of 40. Deaths resulting from cervical cancer are tragic, as this type of cancer develops slowly and has a detectable precursor condition known as carcinoma, which is treatable and can be prevented through screening.[3]
Cervix cancer is a preventable disease, and an essential aspect of its prevention is the detection of the premalignant form by cervical screening; in addition, it is one type of cancer that can be cured if detected early enough.[4] In Saudi Arabia, cervical cancer presents in 4.1/100,000 females. It is estimated that about 7% of all newly diagnosed cancers are cervical cancer in females, and that cervical cancer is the eighth reason of cancer mortality in Saudi females.[5]
Heena et al.[6] performed a cross-sectional study to estimate the knowledge, attitudes, and practices toward cervical cancer and screening among female health-care professionals. Most of the participants were nurses (66.1%). The mean age of the participant population was 34.7 years, and 60.5% of the individuals were married. Only 4.0% appeared to have good level of knowledge about cervical cancer, and 14.7% individuals had moderate-level knowledge. In addition, 86.8% individuals believed that the Pap smear test is a useful test for the detection of cervical cancer, and 26.2% individuals had undergone Pap smear testing.
Tapera et al.[7] performed a cross-sectional study among the University of Botswana female students to elicit information about their knowledge and attitudes on cervical cancer screening. In this study, all the 335 individuals who completed the questionnaire reported that they were aware of cervical cancer. The most common awareness methods were brochures, posters, and other printed material. Regarding the cervical cancer risk, 94% reported that cervical cancer is attributed to smoking and 89.9% attributed it to early sexual debut. Most of the individuals (about 98.2%) were aware of cervical cancer screening. Pap smear was the most known screening test, as reported by 47.8% of the individuals, compared to human papilloma virus (HPV) testing, which was reported by 31.6% of the individuals.
Asgarlou et al.[8] performed a study to assess the relevant knowledge and attitude of female students and hospital staff in Iran. The study found that the response rates were 71% and 63.5% for students and staff, respectively. Also, 29.1% admitted that they had no information about cervical cancer, while only 10.3% had a high knowledge level of cervical cancer, 52.9% had an intermediate knowledge level, and 34.9% had a low knowledge level. While 93% of individuals considered cervical cancer as a severe health problem, the only statistically significant relationships with knowledge were for education.
This study, therefore, aims to assess the knowledge and attitudes of females toward cervical cancer screening. For the cervical cancer screening methods to be utilized in full, females need to be aware of the availability of such methods and to have knowledge of the disease. This will maximize the uptake of the screening and, therefore, reduce the morbidities and mortalities resulting from cervical cancer.
In Saudi Arabia, there is not enough data collected yet about the knowledge and attitude of cervical cancer screening among female high school teachers. So, this study aims to assess relevant knowledge and attitude of cervical cancer screening among female high school teachers in Hail city, Saudi Arabia.
Materials and Methods
Study design
This cross-sectional study was conducted in 2021. The study started on June 1, 2021 and ended on October 1, 2021. Data were collected using a predesigned, tested, and self-administered questionnaire. The questionnaire included specific sections to test the participants’ knowledge and attitude related to cervical cancer and its screening. The questionnaire was developed from previously published studies after an in-depth literature review[5,9,10,11,12,13,14] and then validated through experts.
Sample size
The study population consisted of female high school teachers in Hail city. The study enrolled 387 women female high school teachers in Hail city. The study included married women and excluded single women. The mean age of the included females was 41.4 years with the standard deviation (SD) being 5.3.
Quantitative analysis
Data analysis for the survey was conducted using univariate and multivariate methods. Univariate analyses were conducted to obtain proportions with respect to demographic data of female high school teachers in Hail city. Since Likert scales were used in some variables such as cigarette smoking, history of hospitalization, knowledge of the virus that causes cervical cancer, vaccine that prevents cervical cancer, and cervical cancer screening tests, the responses were compressed to generate the binary variables “Yes” and “No.” The multivariate analysis variables used in some variables as attitudes related to Pap and HPV vaccine. The participants were asked to choose one of the three options, “Yes,” “No,” or “not sure.”
The confounding variables that were adjusted for in the multivariate analysis were sources of cervical cancer information such as social media, advertisements, television (TV), radio, magazines, and others. The identification of these confounders was based on similar studies in the literature.
Ethical consideration
All participants who agreed to participate in the study were assured of confidentiality. The respondents were given a brief description of the study and its objectives.
Statistical analysis
Data were simultaneously entered into proforma and updated. The data were entered into Microsoft Excel (MS Office 2010), and the Master Chart was prepared. The data were analyzed using Statistical Package for the Social Sciences (SPSS) software version 22.0. Statistical analysis of data among groups was carried out, and nominal data were presented as number and percentages. Continuous data (such as age, etc.) were expressed as mean and standard deviation, and Chi-square test was applied as appropriate for comparison of data. P value of 0.05 was considered as statistically significant.
Results
The study sample consisted of 386 women aged between 25 and 58 years, with the mean age being 41.4 years (SD 5.3). Of these, 3.9% (15/386) were aged 20–30 years and approximately 39.4% (152/386) were aged 31–40 years. In addition, 54% (209/386) were aged 40–50 years and 10 women were aged 51–60 years [Figure 1].
Figure 1.
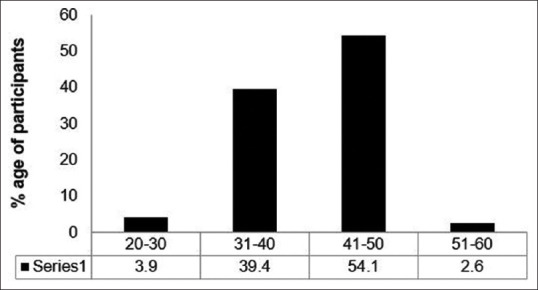
Age of precipitants involved in the study (N = 386)
Knowledge assessment of cervical cancer
Regarding the level of knowledge about the virus that causes cervical cancer, 17% (66/386) responded that they had knowledge about the virus. In addition, 83% (321/386) of females reported that they had not heard about cervical cancer.
Those who were aware of cervical cancer reported that their primary sources of information were social media (30%, n = 117), advertisements (2%, n = 9), TV (6%, n = 21), magazines (1%, n = 4), and others (3%, n = 10) [Figure 2].
Figure 2.
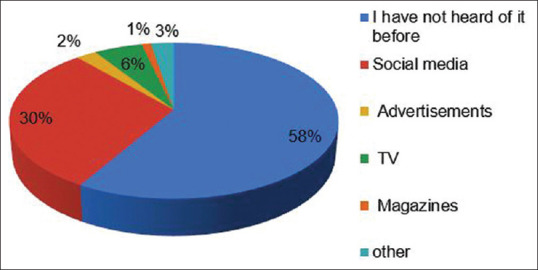
Sources of knowledge about cervical cancer
In the study, 64 females (16.6%) reported having knowledge about the vaccine that prevents cervical cancer. In addition, 163 females (42.3%) had knowledge about the screening tests of cervical cancer [Table 1].
Table 1.
Knowledge of cervical cancer risk factors among female high school teachers in Hail city (n=386)
| Questions to assess knowledge of cervical cancer | Yes | No | P | ||
|---|---|---|---|---|---|
|
|
|
||||
| n | % | n | % | ||
| Are you a smoker? | 1 | 0.3 | 385 | 99.7 | 0.0 |
| Have you suffered from any medical illness that required hospitalization? | 106 | 27.5 | 280 | 72.5 | 0.0 |
| Do you know the virus that causes cervical cancer? | 66 | 17.0 | 321 | 83.0 | 0.0 |
| Do you know the vaccine that prevents cervical cancer? | 64 | 16.5 | 323 | 83.5 | 0.0 |
| Do you know cervical cancer screening tests? | 163 | 42.3 | 223 | 57.7 | 0.0 |
| Have you ever had a Pap smear? | 22 | 5.7 | 365 | 94.3 | 0.0 |
Attitude assessment of cervical cancer and cervical screening
Attitudes toward cervical cancer were assessed separately using four questions [Table 2]. In the study, 17/386 females (4.4%) reported having asked their doctors to do Pap smear. Around 94% of the females (366/386) refused to undergo Pap smear. The lack of awareness was the largest reason for 182/386 females (47%) not doing Pap smear [Figure 3].
Table 2.
Attitude assessment of Pap smear and HPV vaccine among female high school teachers in Hail city (n=386)
| Questions to assess attitudes related to Pap and HPV vaccine | Yes | Not sure | No | P* | |||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| n | % | n | % | n | % | ||
| Have you asked your doctor to do this for you? | 17 | 4.4 | 3 | 0.8 | 366 | 94.8 | 0.0 |
| Did your doctor give it to you? | 17 | 4.4 | 2 | 0.5 | 367 | 95.1 | 0.0 |
| If you were given a pamphlet about the Pap smear and HPV vaccine, would you make the test? | 180 | 46.6 | 144 | 37.3 | 62 | 16.1 | 0.0 |
| Will you allow your daughter to get the HPV vaccine when she is at school? | 147 | 38.0 | 128 | 33.2 | 111 | 28.8 | 0.080 |
HPV=human papilloma virus
Figure 3.
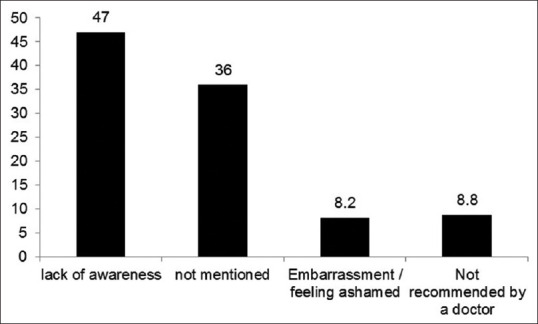
The reasons for rejecting to undergo the Pap test
After the information about the important role of Pap smear and HPV vaccine was given, an increase in the number of females who responded that they would do Pap smear and get the vaccine was found, that is, to 180 females (46.6%). It was found that 147 females (38%) will allow their daughters to get the HPV vaccine [Table 2].
Discussion
Increase in understanding of cervical cancer helped recognize its preventable nature.[15] It was established that HPV vaccination and screening can decrease the burden of the disease to a great extent.[16,17]
Spreading information on Pap smear test is important, as it is used in cervical cancer detection. Many women believed that cervical cancer is a terminal illness with no hope of cure, even when detected in early stages. This attitude toward cancer and death needs to be changed. Women need to be educated about these misconceptions.
The results reported a deficiency in knowledge about cervical cancer as well as low Pap smear uptake, which was surprisingly common among the educated women. For example, in the United Arab Emirates, a study of knowledge, attitude, and practice among female school teachers in Sharjah has documented that, although the teachers had good knowledge about the Pap smear test, they were not commonly doing it.[18] In Jordan, the knowledge of the Pap smear test and cervical cancer was inadequate in less-educated and older patients.[19] In Kuwait, a study that was conducted in 2008 reported that about 52% of women had knowledge about cervical cancer screening.[11] In addition, the study provided an insight into the beliefs and attitudes of Saudi women with respect to why they do not go for screening. The results of the present study matched with the results from other studies.[20,21,22,23] A poor level of knowledge was found. Only 17% (66/386) of female high school teachers in Hail city had awareness about cervical cancer. In addition, 83% (321/386) of females reported that they had not heard about cervical cancer.
One of the significant findings in this study was that majority of the women got their knowledge about cervical cancer screening from social media (30%, n = 117) (relatives and friends) rather than advertisements (2%, n = 9), TV (6%, n = 21), magazines (1%, n = 4), and others (3%, n = 10). This result agreed with the findings of a study from Qatar.[24] In our study, 64 females (16.6%) reported having knowledge about the vaccine that prevents cervical cancer. In addition, 163 females (42.3%) reported having knowledge about the screening tests of cervical cancer. Women’s attitudes and beliefs affected their screening behaviors. The personal interest to do Pap smear lacked in many women. This can be attributed to the absence of an organized cervical cancer screening program, which can include mass media awareness and encouraging women to take up Pap smear test. The women clinic in most of the primary health centers in Saudi supported the Pap smear test.
In the study, only 17/386 females (4.4%) reported asking their doctors to do Pap smear. Around 94% of females (366/386) rejected undergoing Pap smear. The lack of awareness was the largest reason for 182/386 females (47%) not doing Pap smear. After the information about the important role of Pap smear and HPV vaccine was given, an increase in the number of females who responded that they would do Pap smear and get the vaccine was found, that is, to 180 females (46.6%). The study showed that 147 females (38%) would allow their daughters to get the HPV vaccine. This information encourages primary health-care providers to target women clinics as the ideal setting for any national cervical cancer screening program.
Conclusion
This study reported that the overall knowledge of female high school teachers in Hail city who participated in the study toward cervical cancer and its prevention was inadequate. Majority (>80%) of the women lacked knowledge that HPV is a causative agent of cervical cancer. This is extremely worrying as the most important way to prevent cervical cancer is by blocking HPV infection. The lack of awareness about cervical cancer and lack of knowledge are the likely barriers in accessing cervical cancer screening services and related care. The media was the perfect source of information regarding cervical cancer. However, any public health problem cannot be solved by isolation. Thus, nongovernmental and governmental organizations and other concerned bodies have to work in collaboration to increase the level of women’s general awareness about cervical cancer and prevent it.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide:Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–86. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 2.Wong LP, Wong YL, Low WY, Khoo EM, Shuib R. Knowledge and awareness of cervical cancer and screening among Malaysian women who have never had a Pap smear:A qualitative study. Singapore Med J. 2009;50:49–53. [PubMed] [Google Scholar]
- 3.Abotchie PN, Shokar NK. Cervical cancer screening among college students in Ghana:Knowledge and health beliefs. Int J Gynecol Cancer. 2009;19:412–6. doi: 10.1111/IGC.0b013e3181a1d6de. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mongsawaeng C, Kokorn N, Kujapun J, Norkaew J, Kootanavanichpong N, Chavenkun W, et al. Knowledge, attitude, and practice regarding cervical cancer among rural community women in Northeast Thailand. Asian Pac J Cancer Prev. 2016;17:85–8. doi: 10.7314/apjcp.2016.17.1.85. [DOI] [PubMed] [Google Scholar]
- 5.Blanco M, Chen L, Melamed A, Tergas AI, Khoury-Collado F, Hou JY, et al. Cost of care for the initial management of cervical cancer in women with commercial insurance. Am J Obstetr Gynecol. 2021;224:286.e1–11. doi: 10.1016/j.ajog.2020.08.039. [DOI] [PubMed] [Google Scholar]
- 6.Heena H, Durrani S, AlFayyad I, Riaz M, Tabasim R, Parvez G, et al. Knowledge, attitudes, and practices towards cervical cancer and screening amongst female healthcare professionals:A cross-sectional study. J Oncol. 2019;2019:5423130. doi: 10.1155/2019/5423130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tapera R, Manyala E, Erick P, Maswabi TM, Tumoyagae T, Mbongwe B, et al. Knowledge and attitudes towards cervical cancer screening amongst University of Botswana female students. Asian Pac J Cancer Prev. 2017;18:2445–50. doi: 10.22034/APJCP.2017.18.9.2445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Asgarlou Z, Tehrani S, Asghari E, Arzanlou M, Naghavi-Behzad M, Piri R, et al. Cervical cancer prevention knowledge and attitudes among female university students and hospital staff in Iran. Asian Pac J Cancer Prev. 2016;17:4921–7. doi: 10.22034/APJCP.2016.17.11.4921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ackerson K, Gretebeck K. Factors influencing cancer screening practices of underserved women. J Am Acad Nurse Pract. 2007;19:591–601. doi: 10.1111/j.1745-7599.2007.00268.x. [DOI] [PubMed] [Google Scholar]
- 10.So VH, Channon AA, Ali MM, Merdad L, Al Sabahi S, Al Suwaidi H, et al. Uptake of breast and cervical cancer screening in four Gulf Cooperation Council countries. Eur J Cancer Prev. 2019;28:451–6. doi: 10.1097/CEJ.0000000000000466. [DOI] [PubMed] [Google Scholar]
- 11.Al Sairafi M, Mohamed FA. Knowledge, attitudes, and practice related to cervical cancer screening among Kuwaiti women. Med Princ Pract. 2009;18:35–42. doi: 10.1159/000163044. [DOI] [PubMed] [Google Scholar]
- 12.Mbamara SU, Ikpeze OC, Okonkwo JE, Onyiaorah IV, Ukah CO. Knowledge, attitude and practice of cervical cancer screening among women attending gynecology clinics in a tertiary level medical care center in southeastern Nigeria. J Reprod Med. 2011;56:491–6. [PubMed] [Google Scholar]
- 13.Mukama T, Ndejjo R, Musabyimana A, Halage AA, Musoke D. Women's knowledge and attitudes towards cervical cancer prevention:A cross sectional study in Eastern Uganda. BMC Womens Health. 2017;17:9. doi: 10.1186/s12905-017-0365-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Narayana G, Suchitra MJ, Sunanda G, Ramaiah JD, Kumar BP, Veerabhadrappa KV. Knowledge, attitude, and practice toward cervical cancer among women attending Obstetrics and Gynecology Department:A cross-sectional, hospital-based survey in South India. Indian J Cancer. 2017;54:481–7. doi: 10.4103/ijc.IJC_251_17. [DOI] [PubMed] [Google Scholar]
- 15.Braaten KP, Laufer MR. Human Papillomavirus (HPV), HPV-related disease, and the HPV vaccine. Rev Obstet Gynecol. 2008;1:2–10. [PMC free article] [PubMed] [Google Scholar]
- 16.Adegoke O, Kulasingam S, Virnig B. Cervical cancer trends in the United States:A 35-year population-based analysis. J Womens Health (Larchmt) 2012;21:1031–7. doi: 10.1089/jwh.2011.3385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bray F, Loos AH, McCarron P, Weiderpass E, Arbyn M, Møller H, et al. Trends in cervical squamous cell carcinoma incidence in 13 European countries:Changing risk and the effects of screening. Cancer Epidemiol Biomarkers Prev. 2005;14:677–86. doi: 10.1158/1055-9965.EPI-04-0569. [DOI] [PubMed] [Google Scholar]
- 18.Emirates UA. The knowledge, attitude and practice of pap smear among local school teachers in the sharjah district. Middle East J Fam Med. 2004;4:10–8. [Google Scholar]
- 19.Amarin ZO, Badria LF, Obeidat BR. Attitudes and beliefs about cervical smear testing in ever-married Jordanian women. East Mediterr Health J. 2008;14:389–97. [PubMed] [Google Scholar]
- 20.Jirojwong S, Thassri J, Skolnik M. Perception of illness and the use of health care givers among cervical cancer patients at Songkla Nagarind Hospital. A study in southern Thailand. Cancer Nurs. 1994;17:395–402. [PubMed] [Google Scholar]
- 21.Maaita M, Barakat M. Jordanian women's attitudes towards cervical screening and cervical cancer. J Obstet Gynaecol. 2002;22:421–2. doi: 10.1080/01443610220141416. [DOI] [PubMed] [Google Scholar]
- 22.Holroyd E, Twinn S, Adab P. Socio-cultural influences on Chinese women's attendance for cervical screening. J Adv Nurs. 2004;46:42–52. doi: 10.1111/j.1365-2648.2003.02964.x. [DOI] [PubMed] [Google Scholar]
- 23.Islam N, Kwon SC, Senie R, Kathuria N. Breast and cervical cancer screening among South Asian women in New York City. J Immigr Minor Health. 2006;8:211–21. doi: 10.1007/s10903-006-9325-y. [DOI] [PubMed] [Google Scholar]
- 24.Al-Meer FM, Aseel MT, Al-Khalaf J, Al-Kuwari MG, Ismail MF. Knowledge, attitude and practices regarding cervical cancer and screening among women visiting primary health care in Qatar. East Mediterr Health J. 2011;17:855–61. doi: 10.26719/2011.17.11.856. [DOI] [PubMed] [Google Scholar]


