Introduction
Concealed His extrasystoles are a well-known masquerader of atrioventricular (AV) block. It is therefore necessary to consider pseudo-AV block in patients who develop unexpected AV block without a clear etiology. In this report, we present a case of a 46-year-old female patient who was found to have pseudo–Mobitz II AV block secondary to His extrasystoles diagnosed on surface electrocardiogram (ECG) without requiring invasive electrophysiology study. We also demonstrated in this patient that flecainide can be an effective treatment for His extrasystoles.
Key Teaching Points.
-
•
Concealed His extrasystole can mimic second-degree Mobitz II atrioventricular (AV) block.
-
•
Concealed His extrasystole can be diagnosed using surface electrocardiogram.
-
•
Class IC antiarrhythmic agents are an effective treatment for pseudo–second-degree Mobitz II AV block secondary to concealed His extrasystole.
Case report
We present a case of a 46-year-old female patient with a history of anxiety and hypothyroidism who was referred to our clinic for possible pacemaker implantation. Her baseline 12-lead ECG showed normal sinus rhythm. She wore an ambulatory ECG monitor for 2 weeks after complaints of palpitation, during which time 156 episodes of second-degree Mobitz II AV block were observed (Figure 1). Lyme titer was negative. Transthoracic echocardiogram revealed normal left ventricle size and function without significant valvular heart disease. Cardiac magnetic resonance imaging showed normal biventricular size and function with no late gadolinium enhancement. She had good exercise capacity (9 METs) with no evidence of ischemia on treadmill exercise stress test. During stage I of the Bruce protocol, there was a single nonconducted P wave following the 10th QRS complex with fixed PR and P-P intervals, consistent with Mobitz II AV block (Figure 2). Sinus tachycardia with frequent likely junctional extrasystoles with a typical right bundle branch block (RBBB) configuration were also present. Closely following the blocked P wave was a small negative deflection, consistent with a retrograde P wave. The P wave is narrow and inverted in the inferior leads, consistent with retrograde septal activation, as would be expected to occur in association with a junctional extrasystole. While this could have been an opportunistic premature atrial extrasystole, the more likely explanation is that a junctional extrasystole conducted retrogradely through the AV node to the atrium and blocked antegradely in the His-Purkinje system (Figure 3). The timing of the extrasystole would have had to occur during inscription of the blocked antegrade P wave and engaged the AV node retrogradely, causing the oncoming antegrade P wave to block in the AV node. Furthermore, Mobitz II block is typically secondary to conduction disease below the AV node and tends to get worse at a faster heart rate, which was not observed here. All findings were supportive of pseudo-AV block secondary to His extrasystoles. She was started on flecainide, which was up titrated to 100 mg twice daily. A repeat ambulatory ECG recording at 5 months follow-up showed normal sinus rhythm with no AV block. A repeat treadmill exercise stress test revealed a peak heart of 153 beats per minute without evidence of ischemia or AV block.
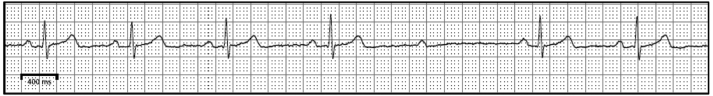
Figure 1.
A rhythm strip from ambulatory monitor. The P-P and PR intervals are constant before and after the blocked P wave, consistent with Mobitz II atrioventricular block.
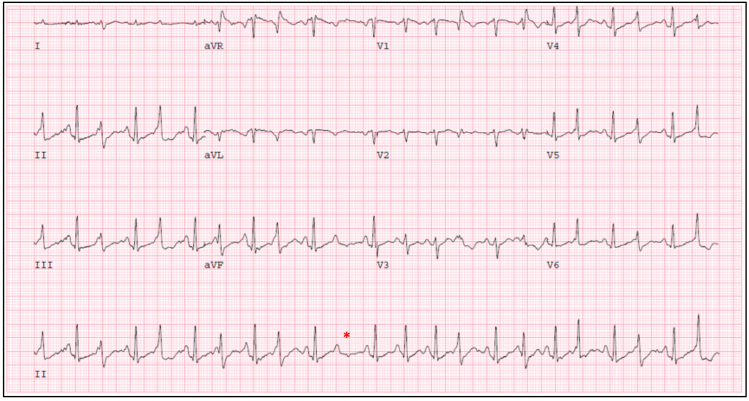
Figure 2.
Electrocardiogram during treadmill exercise stress test (stage I Bruce protocol). Sinus tachycardia with frequent junctional or ventricular premature complexes and Mobitz II atrioventricular block are present.
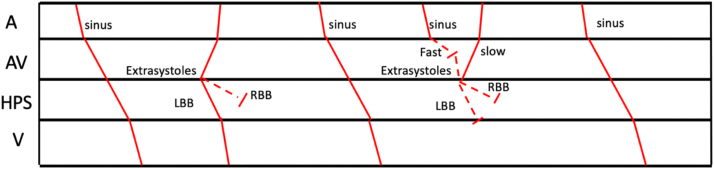
Figure 3.
Ladder diagram illustrates our proposed mechanism for intermittent right bundle branch (RBB) block and atrioventricular (AV) block seen on electrocardiogram. A His extrasystole that conducts retrogradely through the AV node to the atrium but blocks antegradely in the RBB will give rise to a QRS with RBB block. A shorter coupled His extrasystole that conducts retrograde into the slow AV node pathway to the atrium and into the fast AV node pathway, causing the preceding sinus beat to block in the AV node, will give rise to an inverted P wave without QRS, mimicking AV block.
Discussion
Concealed His extrasystoles mimicking AV block was first described by Langendorf and Mehlman1 in 1947. The mechanism was postulated to be secondary to His extrasystoles that fail to conduct to the ventricle but partially conduct into the AV junction. This was later confirmed in an electrophysiology study in 1970 by Rosen and colleagues.2 AV block secondary to His extrasystoles has been termed pseudo-AV block. This phenomenon was well documented in the 1970s.3, 4, 5 There have been few scattered case reports since then. In this case report, we present an otherwise healthy 46-year-old female patient who was found to have 156 episodes of second-degree Mobitz II AV block on ambulatory monitoring for palpitations. Evaluation for reversible causes with Lyme titers, transthoracic echocardiogram, cardiac magnetic resonance imaging, and treadmill exercise stress test were unremarkable. However, ECG during her stress test provided insight into the cause of her AV block. ECG (Figure 2) showed sinus tachycardia, junctional bigeminy with RBBB, and a blocked sinus P wave that was closely coupled to a small negative deflection, consistent with an atrial depolarization from a His extrasystole. This depolarization conducted retrogradely to the atrium but failed to conduct to the ventricle and partially conducted into the AV node, resulting in a pseudo-AV block. This occurrence was supported by the observation of frequent junctional bigeminy that conducted with RBBB. At a shorter coupling interval, a His extrasystole likely blocked antegrade in the His-Purkinje system and failed to depolarize the ventricles. In addition, it also conducted retrograde into the slow AV node pathway, resulting in retrograde atrial activation, and into the fast AV node pathway, causing the preceding sinus beat to block in the AV node (pseudo-AV block), as illustrated in Figure 3.
In 1973, Narula6 and Eugster and colleagues7 suggested that AV block from His extrasystoles could be a sign of conduction disease distal to the His bundle in some patients, indicating the need for a pacemaker. However, in 1976, Bonner and Zipes5 showed no evidence of distal conduction disease in some patients with pseudo-AV block. While we cannot rule out with absolute certainty the presence of distal conduction system disease in this case without an electrophysiology study, the likelihood of distal disease is low for the following reasons. At baseline, this patient had normal PR interval and QRS duration. Second, she had no AV block at peak exercise (153 beats/min). These findings along with her frequent ectopy were supportive of pseudo-AV block secondary to concealed His extrasystoles as opposed to distal conduction system disease. After a lengthy conversion with the patient, electrophysiology study was deferred and flecainide was started. While there have been no reported case studies of using class IC antiarrhythmics to treat His extrasystoles, we chose flecainide based on the results of previous studies using other class I antiarrhythmic agents, as shown in Table 1. Five months after initiation of flecainide, a repeat ambulatory ECG recording showed no AV block. Patch monitor showed rare premature atrial contractions and premature ventricular contractions. A repeat treadmill stress test showed rare junctional complexes without AV block.
Table 1.
Case studies on treatment of pseudo-atrioventricular block from His extrasystoles
| Authors | Year | Findings |
|---|---|---|
| Bonner and Zipes5 | 1976 | Lidocaine eliminated His extrasystoles |
| Dhurandhar et al8 | 1976 | Quinidine sulfate 200 mg 4 times a day completely suppressed His extrasystoles |
| Castellanos et al9 | 1977 | Xylocaine markedly reduced fascicular extrasystoles |
| Khan et al10 | 2011 | Procainamide suppressed His extrasystoles |
The findings in this patient underscore the fact that concealed His extrasystoles can be diagnosed from careful analysis of the surface electrocardiogram, and flecainide is an effective treatment for pseudo-AV block from concealed His extrasystoles. Treatment of pseudo-AV block from His extrasystoles with class I antiarrhythmic agents is summarized in Table 1.
Footnotes
Funding Sources: No funding. Disclosures: The authors have no conflicts to disclose.
References
- 1.Langendorf R., Mehlman J.S. Blocked (nonconducted) A-V nodal premature systoles imitating first and second degree A-V block. Am Heart J. 1947;34:500–506. doi: 10.1016/0002-8703(47)90528-0. [DOI] [PubMed] [Google Scholar]
- 2.Rosen K.M., Rahimtoola S.H., Gunnar R.M. Pseudo A-V block secondary to premature non-propagated His bundle depolarization. Documentation by His bundle electrocardiography. Circulation. 1970;42:367–373. doi: 10.1161/01.cir.42.3.367. [DOI] [PubMed] [Google Scholar]
- 3.Cannon D.S., Gallagher J.J., Goldreyer B.N., Damato A.N. Concealed bundle of His extrasystoles simulating nonconducted atrial premature beats. Am Heart J. 1972;83:777–779. doi: 10.1016/0002-8703(72)90209-8. [DOI] [PubMed] [Google Scholar]
- 4.El-Sherif N., Befeler B., Aranda J., Castellanos A., Lazzara R. Re-entry due to manifest and concealed His bundle ectopic systoles. Circulation. 1976;53:902–908. doi: 10.1161/01.cir.53.5.902. [DOI] [PubMed] [Google Scholar]
- 5.Bonner A.J., Zipes D.P. Lidocaine and His bundle extrasystoles. His bundle discharge conducted with functional right or left bundle branch block, or blocked entirely (concealed) Arch Intern Med. 1976;136:700–704. doi: 10.1001/archinte.136.6.700. [DOI] [PubMed] [Google Scholar]
- 6.Narula O.S. In: Cardiac Arrhythmias. Dreifus L.S., Likoff W., editors. Grune & Stratton Inc; New York: 1973. Conduction disorders in the A-V transmission system. 262. [Google Scholar]
- 7.Eugster G.S., Godfrey C.C., Brammell H.L., Pryor R. Pseudo A-V block associated with A-V and H-V conduction defects. Am Heart J. 1973;85:789–796. doi: 10.1016/0002-8703(73)90430-4. [DOI] [PubMed] [Google Scholar]
- 8.Dhurandhar R.W., Valen F.J., Phillips J. Pseudo second degree atrioventricular block with bradycardia. Successful treatment with quinidine. Br Heart J. 1976;38:1363–1366. doi: 10.1136/hrt.38.12.1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Castellanos A., Sung R., Mallon S.M., Ghahramani A., Moleiro F., Myerburg R.I. His bundle electrocardiography in manifest and concealed right bundle branch extrasystoles. Am Heart J. 1977;94:307–315. doi: 10.1016/s0002-8703(77)80473-0. [DOI] [PubMed] [Google Scholar]
- 10.Khan A., Ameen A., Maraj I., Turitto G., El-Sherif N.E. A His bundle extrasystole can both induce and reverse 2:1 atrioventricular block. J Interv Card Electrophysiol. 2011;32:121–123. doi: 10.1007/s10840-011-9542-8. [DOI] [PubMed] [Google Scholar]