Abstract
High healthcare utilizers are often chronically ill patients who require aggressive hospital and outpatient care. We describe a patient with septic shock who was stabilized in the intensive care unit, then transitioned to a virtual hybrid hospital‐at‐home to complete both inpatient care as well as outpatient wound and rehabilitation therapy.
Keywords: home hospital, home rehabilitation, hospital‐at‐home, telehealth, wound care
Mayo Clinic's Advance Care at Home program can deliver both inpatient‐level care as well as postacute, skilled nursing‐level wound care, and rehabilitative therapy. Decompensations were treated in the home setting, preventing escalations to the emergency department.
1. INTRODUCTION
High healthcare utilizers (HHUs) are a small group of individuals who place a disproportionately large burden on the healthcare system due to their high resource consumption and who frequently have unmet care needs or receive unneeded care. 1 HHU constitutes a public health challenge in several fields. For instance, several systems classify HHUs based on fiscal resources spend per patient which implies an economic problem for the health system. Additionally, HHUs represent other indirect problems such as the saturation of emergency services and hospitalization in brick‐and‐mortar (BAM) hospitals. Finally, the multiple hospitalizations of a patient mean a burden for both the family and the patient. Several programs have aimed to target this group of patients. The problem is that most of the interventions that have been tried have failed to fulfill goals in the treatment of this specific group of patients or were no longer functioning a few years later. 2
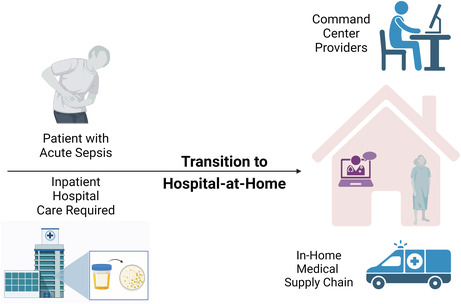
In July 2020, Mayo Clinic began implementing the Advanced Care at Home (ACH) program. ACH is a virtual hybrid hospital‐at‐home program that provides both acute and postacute care to patients in their homes. 3 Patients in Florida, Wisconsin, and Arizona are admitted to the ACH program and are virtually cared for by a single telemedicine command center. The command center performs virtual rounds on the patient and then directs a vendor‐mediated supply chain to deliver in‐home care. This program has shown in its 2 years that it has effectively managed the issue that HHUs represent. This case report aims to demonstrate that ACH is a feasible and effective solution for complex HHU patients.
2. CASE PRESENTATION
A 61‐year‐old lady with multiple medical comorbidities presented to the Emergency Department (ED) with dysuria and lightheadedness. She had a complex history of multiple hospitalizations due to her many chronic comorbidities which included morbid obesity (BMI: 56.18 kg/m2), congestive heart failure with reduced ejection fraction (EF 40%–45%), coronary artery disease status postcoronary artery bypass graft surgery (CABG) in 2013, pulmonary embolism in 2016, atrial fibrillation on warfarin, pulmonary hypertension with an estimated right ventricular systolic pressure of 57 mmHg, chronic obstructive pulmonary disease (COPD), systemic hypertension, diabetes mellitus type 2 on insulin therapy, chronic kidney disease stage 4 (CDK4), ureterolithiasis, chronic pain on chronic opioid therapy, peripheral vascular disease, chronic lymphedema with recurrent episodes of lower limb and sepsis.
In the ED, the patient reported pain with urination that began 3 days prior to her visit accompanied by decreased urine output. She described the urine as cloudy with a foul odor. She also described left lower extremity pain with an intensity of 4/10 on a verbal pain scale which had begun 7 days prior to her visit and had slowly worsened over that timeframe. She described that pain as occurring in the area of her chronic ulcers with no associated erythema or drainage, something she had seen with her previous episodes of lower extremity cellulitis. She denied chest pain, shortness of breath, abdominal pain, nausea, and vomiting. Physical examination revealed hypotension with a mean arterial pressure ranging from 50 to 55 mmHg, somnolent although arousable, and bradycardia with a heart rate of 50 beats per minute. An electrocardiogram was obtained which confirmed idioventricular bradycardia with an irregularly irregular rhythm concern for a complete heart block. Lab work showed an elevated BUN (69 mg/dl) and creatinine (3.66 mg/dl) with an estimated glomerular filtration rate of <15 ml/min/1.73m2 as well as hyperkalemia (6.8 mmol/L) and hyponatremia (131 mEq/L). The urinalysis showed the presence of protein, white blood cells, red blood cells, nitrates, and bacteria. A kidney ultrasound revealed nonobstructing nephrolithiasis of both kidneys with no hydronephrosis. Given the urinary symptoms, physical exam findings, and laboratory studies, a diagnosis of sepsis with shock from a urinary source was suspected.
The patient was admitted to the intensive care unit (ICU) for treatment of septic shock. She received an intervenous (IV) 0.9% normal saline bolus of 30 ml/kg and empiric IV antibiotics were started. IV meropenem was chosen due to her history of previous urinary tract infections with multidrug‐resistant (MDR) E. coli. Atropine was given to improve her heart rate and her hyperkalemia was immediately addressed with IV bicarbonate, calcium gluconate, and insulin with dextrose.
Due to continued hypotension despite IV fluid boluses, epinephrine infusion was started to maintain her MAP. Over the next 48 h, her blood pressure stabilized, and her mental status normalized. Her acute renal failure improved as her blood pressure stabilized and she began producing urine. Urine and blood cultures returned positive for MDR E. coli. After 5 days of treatment in the ICU, she was ready to be deescalated to a step‐down medical unit. The ongoing plan would be continued care in the medical ward for 5–7 days, then transition to a skilled nursing facility for rehabilitation and wound care for an additional 10–14 days. The patient and her family were given the option to continue inpatient care in the medical ward as outlined, or they could transition to the ACH hospital‐at‐home program to complete her acute medical care as well as postacute rehabilitative care. The ACH team evaluated the patient at the bedside to determine eligibility based on demographic, insurance, clinical, and social criteria to be admitted into the program. 4 The patient deemed eligible for the program and was consented to enroll. Instead of moving to the medical ward, the patient was transferred directly home from the ICU to continue her high‐acuity inpatient care including IV antibiotic therapy, daily laboratory studies, hemodynamic monitoring, and our care for her chronic ulcers in the lower extremities.
The technological kit consisting of a tablet two‐way video connection, a Wi‐Fi telephone to the centralized command center, and a personal emergency response system was set up and tested in the home. The patient and family member received virtual rounds with the virtual medical team coordinated by the single telemedicine command center located in Jacksonville, Florida, USA. Additionally, the patient had in‐home visits by a paramedic and registered nurse to perform physical examinations in conjunction with the virtual care team, change wound dressings, draw the laboratory studies, and administer the IV antibiotics. The patient's blood pressure slowly stabilized to her prehospitalization levels, and her home oral antihypertensive medications were slowly reintroduced. On ACH day 5 (hospital day #10), she was discharged from the inpatient acute phase to the postacute restorative phase of the program, and intense therapy including physical and occupational therapy began. The ACH medical team conducted a virtual consultation with the Orthopedic Surgery team to get further recommendations on wound care, physical therapy goals, and to set up postacute follow‐up care. The patient continued in the program recovering strength and mobility while completing her antibiotic treatment from the comfort of her home. During her recovery, she did have one instance of lightheadedness and 1 day of decreased urine output. On both occasions, the virtual medical team was able to conduct an assessment with the assistance of a visiting paramedic. On both occasions, the patient was reassured, and the medical care plan was adjusted, avoiding any escalation back to the ED or the hospital. As she approached being discharged from the entire ACH program, the virtual care team was able to contact her primary care provider and all subspecialist involved in her care and spent several days handing off her longitudinal care plan to these providers. The ACH team ensured that all home medications were filled, and any durable medical equipment was delivered. After all questions were answered for the patient and her family, she was discharged 21 days after originally being admitted to the BAM hospital.
3. DISCUSSION
Here we present a case of an HHU patient who required both prolonged hospitalization as well as postacute care due to septic shock. As opposed to spending 10 days in the BAM hospital followed by 11 days in a skilled nursing or rehab center, our patient was able to move out of the ICU after 5 days of care directly home, completing her inpatient care 5 days later, and then transitioning directly into postacute care in the home for an additional 11 days. She was able to be monitored, complete her IV antibiotics, have laboratory studies conducted, and receive wound care and physical therapy all under the supervision of her virtual care team. She was also able to connect to an orthopedic specialist in consultation as well as have a smooth care plan handoff with her primary care providers. In addition, we were able to escalate the care in her home during her recovery to avoid return visits to the ED or hospital. We believe that this type of innovation shows a strong promise in reducing the number of unnecessary healthcare visits in HHU patients. This holds especially true in the immunocompromised patient population who often are HHU due to their susceptibility to repeated infections. 4 What is more, these immunocompromised patients often require extended hospital stays for infection treatment, which may add to their risk of contracting a hospital‐acquired infection, 4 , 5
Existing studies often use an empirical threshold for the number of healthcare visits or associated expenses to define HHU. 6 Despite receiving extensive care from a variety of sources, crucial healthcare needs go unmet, and many people receive needless and ineffective treatment. 7 , 8 , 9 Healthcare use is considered preventable and/or needless when the occurrences are believed to be avoidable. Preventing avoidable encounters, especially in acute care settings like emergency departments and crucial care centers, are key in driving down healthcare utilization and the associated costs. In 2010, $64.4 billion, 19.6% of ED episodes, and 2.4% of national health expenditures were spent on potentially needless emergency department (ED) visits. 10 In our case, our patient had two occurrences in her restorative phase, where had she been unmonitored in the outpatient setting, she states that she would have sought emergency services. By being able to connect instantaneously with the virtual technology and escalate care right in her home, we were able to avoid unnecessary trips to the ED and the associated cost and resource use. This shows that HHU patients are an urgent target for cost‐cutting and quality improvement initiatives like ACH.
Because of their disproportionate spending, HHU patients garner a lot of attention in healthcare studies. According to the Agency for Healthcare Research and Quality (AHRQ), the top 10% of the health‐care‐using population accounted for 66% of all healthcare spending in the United States in 2012. 11 This very unequal spending trend is sometimes misinterpreted as an indicator of ineffective healthcare delivery. From a humanitarian standpoint, HHU patients deserve special attention, both because they have significant healthcare needs and because, due to their frequent interactions with the system, they are more likely than other patients to be affected by preventable healthcare quality and safety issues. Moreover, inadequacies in the hospital's physical environment and cultural atmosphere have been demonstrated to have a negative impact on patients' experiences of hospitalization and are used as evidence for the claim that those with palliative care needs should avoid admission to the hospital. 12 In ACH, we are able to deliver hospital‐level care in the patient's own environment. We can study their home environment, interact with their family and support system, and individualize a care plan that meets their needs. We have seen this approach lead to HHU patients being more willing to engage in their healthcare plan and longitudinal recovery. This may ultimately lead to better outcomes for HHU patients.
4. CONCLUSION
This case represents an HHU patient who was successfully treated for an extended period with high‐acuity care in the home setting. Continued efforts in treating HHU patients with the ACH hospital‐at‐home model of care may benefit the healthcare system by conserving the use of inpatient resources while providing a safe and desired care environment for our patients.
AUTHOR CONTRIBUTIONS
Margaret R. Paulson: Conceptualization; data curation; formal analysis; writing – review and editing. Ricardo A. Torres‐Guzman: Data curation; investigation; writing – original draft. Gautam V. Matcha: Conceptualization; formal analysis; investigation; writing – review and editing. Francisco R. Avila: Data curation; investigation; writing – original draft. Karla C. Maita: Data curation; investigation; writing – original draft. John P. Garcia: Data curation; investigation; writing – original draft. Antonio J. Forte: Resources; software; supervision; writing – original draft. Micheal J. Maniaci: Resources; supervision; validation; writing – review and editing.
FUNDING INFORMATION
No external funding sources were used for this study, only internal Mayo Clinic departmental funds.
CONFLICT OF INTEREST
None of the authors have any conflict of interest to report.
ETHICAL APPROVAL
This study conforms to all standards of the Mayo Clinic Ethics Committee.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
ACKNOWLEDGMENT
We would like to thank Abdullah Eldaly for his contributions to this case report.
Paulson MR, Torres‐Guzman RA, Matcha GV, et al. Treatment of a high healthcare utilizer with sepsis in a virtual hybrid hospital‐at‐home program. Clin Case Rep. 2023;11:e06806. doi: 10.1002/ccr3.6806
DATA AVAILABILITY STATEMENT
Access to data is restricted to keep the patient's privacy. However, if deemed necessary, data will be provided by the corresponding author upon reasonable request after approval from the needed institutional committee.
REFERENCES
- 1. Wammes JJG, van der Wees PJ, Tanke MAC, Westert GP, Jeurissen PPT. Systematic review of high‐cost patients' characteristics and healthcare utilisation. BMJ Open. 2018;8(9):e023113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Anderson GF, Ballreich J, Bleich S, et al. Attributes common to programs that successfully treat high‐need, high‐cost individuals. Am J Manag Care. 2015;21(11):e597‐e600. [PubMed] [Google Scholar]
- 3. Maniaci MJ, Torres‐Guzman RA, Garcia JP, et al. Overall patient experience with a virtual hybrid hospital at home program. SAGE Open Med. 2022;22(10):20503121221092589. doi: 10.1177/20503121221092589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Poutoglidis A, Tsetsos N, Vakouli S, Fyrmpas G. Necrotizing bacterial rhinitis in an immunocompromised patient. Ear Nose Throat J. 2022;101(10):637‐639. [DOI] [PubMed] [Google Scholar]
- 5. Centers for Disease Control and Prevention . CDC Healthcare‐associated Infections (HAI); HAI Data 2022. Accessed December 16, 2022. https://www.cdc.gov/hai/data/portal/index.html
- 6. Yang C, Delcher C, Shenkman E, Ranka S. Expenditure variations analysis using residuals for identifying high health care utilizers in a state Medicaid program. BMC Med Inform Decis Mak. 2019;19(1):131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Blumenthal D, Chernof B, Fulmer T, Lumpkin J, Selberg J. Caring for high‐need, high‐cost patients ‐ an urgent priority. N Engl J Med. 2016;375(10):909‐911. [DOI] [PubMed] [Google Scholar]
- 8. Bodenheimer T, Fernandez A. High and rising health care costs. Part 4: can costs be controlled while preserving quality? Ann Intern Med. 2005;143(1):26‐31. [DOI] [PubMed] [Google Scholar]
- 9. Wennberg JE, Bronner K, Skinner JS, Fisher ES, Goodman DC. Inpatient care intensity and patients' ratings of their hospital experiences. Health Aff (Millwood). 2009;28(1):103‐112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Galarraga JE, Pines JM. Costs of ED episodes of care in the United States. Am J Emerg Med. 2016;34(3):357‐365. [DOI] [PubMed] [Google Scholar]
- 11. Cohen SB. The concentration of health care expenditures and related expenses for costly medical conditions, 2012. Statistical Brief (Medical Expenditure Panel Survey (US)). Agency for Healthcare Research and Quality (US); 2001. [PubMed] [Google Scholar]
- 12. Robinson J, Gott M, Frey R, Gardiner C, Ingleton C. Predictors of patient‐related benefit, burden and feeling safe in relation to hospital admissions in palliative care: a cross‐sectional survey. Palliat Med. 2018;32(1):167‐171. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Access to data is restricted to keep the patient's privacy. However, if deemed necessary, data will be provided by the corresponding author upon reasonable request after approval from the needed institutional committee.


