Abstract
Inorganic arsenic is a known human carcinogen and is routinely detected in US community water systems (CWSs). Inequalities in CWS arsenic exist across broad sociodemographic subgroups. Our objective was to evaluate the county-level association between socioeconomic vulnerability and CWS arsenic concentrations across the US. We evaluated previously developed, population-weighted CWS arsenic concentrations (2006–2011) and three socioeconomic domains (the proportion of adults with a high school diploma, median household income, and the Centers for Disease Control and Prevention’s overall socioeconomic vulnerability score) for 2,604 conterminous US counties. We used spatial lag models and evaluated the adjusted geometric mean ratio (GMR) of CWS arsenic concentrations per higher socioeconomic domain score corresponding to the interquartile range, and also evaluated flexible quadratic spline models. We also stratified by region and by United States Department of Agriculture Rural-Urban Continuum Codes to assess potential effect measure modification by region and rurality. Associations between socioeconomic vulnerability and CWS arsenic were modified by region and rurality and specific to socioeconomic domain. The fully adjusted GMR (95% CIs) of CWS arsenic per interquartile range higher proportion of adults with a high school education was 0.83 (0.71, 0.98) in the Southwest (corresponding to 17% lower arsenic with higher education), 0.82 (0.71, 0.94) in the Eastern Midwest (18% lower), and 0.65 (0.31, 1.36) in New England (35% lower). Associations between median household income and CWS arsenic were largely null. Higher overall socioeconomic vulnerability was significantly associated with lower CWS arsenic, but only in counties in the Central Midwest and those with total populations less than 20,000. Findings may reflect regional/local differences in both socioeconomic/socio-cultural context and public drinking water regulatory efforts. Across the US, individual domains of socioeconomic vulnerability (especially educational attainment) are more strongly associated with inequalities in CWS arsenic than the complex overall socioeconomic vulnerability index.
Keywords: arsenic, drinking water, environmental justice, socioeconomic status
INTRODUCTION
Inorganic arsenic is a known human carcinogen associated with numerous adverse health outcomes including respiratory disease, adverse birth outcomes, metabolic disease and diabetes.1–7 Even at low- to moderate levels of exposure common in the US population, inorganic arsenic is associated with incident and fatal cardiovascular disease.8,9 In general US populations, the majority of inorganic arsenic exposure occurs through diet (especially rice and rice products) and drinking water.10 Public water systems, including community water systems (CWSs) which serve the same populations year-round, are regulated by the US Environmental Protection Agency. Over 90% of US residents receive at least some water from CWSs.11 The current maximum contaminant level (MCL) for arsenic is 10 μg/L (the US EPA sets the maximum contaminant goal level to 0 μg/L for arsenic and other known carcinogens). Arsenic is frequently detected in CWSs (approximately 45% of CWS monitoring records), and MCL violations are more common than violations for most other regulated contaminants.12 Modeling studies suggest that drinking water is the most significant source of inorganic arsenic exposure when water concentrations are above the MCL, although large epidemiologic studies robustly quantifying relative exposure sources across diverse US populations are currently lacking.13
There are major regional and sociodemographic inequalities in CWS arsenic concentrations across the US. The factors likely driving inequalities in drinking water contaminant exposures are complex and interrelated, but include differences in the natural environment (e.g. geochemistry, climate), inequalities in the built environment (e.g. infrastructure and planning, land-use patterns), and sociopolitical forces (e.g. structural racism, classism, regulatory policy).14 Previous work at the CWS-level found higher arsenic concentrations for CWSs located in the Central Midwest and Southwest, for CWSs serving tribal communities, Rural American Indian populations, and Semi-Urban Hispanic populations, and CWSs serving incarcerated populations in the Southwest.15,16 In one nationwide study at the county-level, higher proportions of Hispanic/Latino and American Indian/Alaskan Native residents were associated with higher CWS arsenic concentrations, independent of educational attainment, household income, and overall socioeconomic vulnerability.17 Similarly, at the Census block level in California, higher CWS arsenic concentrations were associated with higher proportions of Latinx residents but not with a higher proportion of residents who rent their homes (i.e. tenancy).18 However, no nationwide studies have yet specifically evaluated the association between community socioeconomic vulnerability and CWS arsenic concentrations independent of racial/ethnic composition. Identifying specific domains of community sociodemographic characteristics associated with higher public water contaminant concentrations (e.g., racial/ethnic composition, socioeconomic vulnerability, language, rurality, etc.) can identify specific mechanisms underlying exposure disparities and can inform public health interventions and regulatory actions to eliminate exposure disparities.14
Our objective was to evaluate the county-level association between three domains of community socioeconomic vulnerability (the proportion of adults with a high school diploma, median household income, and overall socioeconomic vulnerability score) and CWS arsenic concentrations across the conterminous US in geospatial models. We predicted that higher socioeconomic vulnerability (i.e. lower proportions of high school educational attainment, lower median household income, and higher socioeconomic vulnerability scores) would be associated with higher CWS arsenic concentrations. We also predicted that region and rurality would modify this association because both socio-cultural systems impacting socioeconomic vulnerability and public drinking water arsenic concentrations differ across regions and by rurality, but we had no a priori predictions about subgroup-specific associations.15,19 Our analysis focused on regulated CWSs only (not unregulated domestic wells), and we were unable to evaluate the association nationwide at finer geographic resolutions (e.g., Census block) because there are currently no nationwide estimates of CWS arsenic concentrations available at these alternative spatial resolutions.
MATERIALS AND METHODS
Dependent variable: County-level CWS arsenic concentrations
We used previously developed county-level, population-weighted CWS arsenic concentrations (2006–2011) which have been described in detail.15 Briefly, CWS arsenic concentrations were derived from the most recent nationwide, publicly available routine compliance monitoring records collected by the US EPA for the Third Six Year Review. Compliance monitoring records contained in the Third Six Year Review database represent over 95% of public water systems and over 92% of US residents reliant on public water systems nationwide.20,21 Mean arsenic concentrations at the county-level were developed considering the frequency of EPA’s compliance monitoring requirements. These county-level estimates reflect treated water distributed to consumers, and were calculated by weighing the average concentration for each CWS within the county by the size of the population served by each CWS. 2006–2011 CWS arsenic estimates were available for a total of 2,639 counties. County-level CWS arsenic concentrations were only estimated for counties when at least 50% of the population reliant on public drinking water was represented by available CWS arsenic records in the Third Six Year Review. No compliance monitoring records were submitted for the Third Six Year Review for CWSs from Colorado, Delaware, Georgia, Mississippi, and tribal CWSs from EPA regions 2, 6, 7, and 10.
Independent variables: measures of socioeconomic vulnerability
The Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry (CDC/ATSDR) publishes five county-level ranked indices of social vulnerability, including indices for socioeconomic vulnerability, household composition and diversity vulnerability, minority status and language vulnerability, and housing type and transportation vulnerability, and a sum total social vulnerability score (derived by ranking the sum of the rankings of the other four indices).22 We used the county-level socioeconomic vulnerability index published in 2014 as we were primarily interested in domains of vulnerability captured by the socioeconomic status index. The socioeconomic status vulnerability index is derived from 2010–2014 US Census American Community Survey estimates of median household income and the percent of adults who are unemployed, living below the poverty line, and without a high school diploma (higher scores indicate higher socioeconomic vulnerability). We did not assess the sum social vulnerability index because one component includes aspects of racial/ethnic composition (the minority status and language index), which we have evaluated separately and intended to control for in this analysis.17 We also downloaded the proportion of adults with a high school diploma (derived from the US Census American Community Survey) and median household income (derived from the Small Area Income and Poverty Estimates and National Center for Education Statistics data) prepared by the University of Wisconsin Population Health Institute and Robert Wood Johnson Foundation for the 2013 County Health Rankings Database in order to consider these individual components of the overall socioeconomic vulnerability index separately.23,24
Additional county-level covariates
We selected county-level variables reflecting the time period overlapping with the county-level CWS arsenic concentration estimates (2006–2011) and socioeconomic vulnerability variables (2010–2014). We derived the following county-level variables from the 2010 decennial US Census: total population, population density (population per square mile), and racial/ethnic composition (including the total number and proportion of residents who identified as American Indian or Alaskan Native (hereafter referred to as American Indian/Alaskan Native), non-Hispanic Asian, Native Hawaiian or Other Pacific Islander, Hispanic/Latino of any race, non-Hispanic Black or African American (hereafter referred to as non-Hispanic Black), and non-Hispanic White).25 We estimated the percent of public drinking water supplied by groundwater sources (versus surface water) from estimates of total groundwater and surface water withdrawn for public drinking water calculated by the US Geological Survey for 2010, as previously described.17,26,27 To assess potential effect measure modification by rurality, we also downloaded the United States Department of Agriculture’s Rural Urban Continuum Codes for 2013.28 Counties are categorized as metropolitan or non-metropolitan, and are further assigned to one of nine rural-urban categories (three metropolitan and six non-metropolitan categories) reflecting population size (but not density), degree of urbanization, labor force commuting, and adjacency to a metropolitan area. Finally, we assigned counties to US regions using categories previously developed based on similar water arsenic patterns (states included in each region are listed in the table footnote for Table 2): Central Midwest, Eastern Midwest, Mid-Atlantic, New England, Pacific Northwest, Southeast, and Southwest.15
Table 2.
Geometric mean ratio (GMR) and 95% CI of mean community water system (CWS) arsenic (2006–2011per increase in measures of socioeconomic vulnerability corresponding to the interquartile range (proportion of adults with a high school diploma, median household income, and CDC/ATSDR’s overall socioeconomic vulnerability score), nationwide and stratified by region and metropolitan vs non-metropolitan counties (N= 2,604 counties.
| Proportion of adults with a high school diploma | Median household income | Overall socioeconomic vulnerability score | |
|---|---|---|---|
| Unit of change (nationwide IQR) | 0.15 | $11,552 | 0.5 |
| Nationwide (N= 2,604) | |||
| Model 1 | 1.02 (0.98, 1.06) | 1.01 (0.99, 1.04) | 0.95 (0.91, 0.99) |
| Model 2 | 1.00 (0.96, 1.04) | 1.01 (0.98, 1.04) | 0.93 (0.88, 0.98) |
|
| |||
| Metropolitan versus non-metropolitan counties | |||
| Non-metropolitan counties (N= 1,634) | |||
| Model 1 | 1.03 (0.97, 1.09) | 1.09 (1.04, 1.15) | 0.88 (0.83, 0.93) |
| Model 2 | 1.01 (0.95, 1.07) | 1.09 (1.03, 1.15) | 0.85 (0.79, 0.92) |
| Metropolitan counties (N= 970) | |||
| Model 1 | 1.02 (0.95, 1.09) | 1.01 (0.97, 1.05) | 0.97 (0.90, 1.04) |
| Model 2 | 1.00 (0.92, 1.07) | 0.99 (0.95, 1.04) | 0.95 (0.87, 1.03) |
|
| |||
| By region | |||
| Central Midwest (N= 401) | |||
| Model 1 | 1.05 (0.94, 1.18) | 0.97 (0.88, 1.06) | 0.85 (0.75, 0.95) |
| Model 2 | 1.13 (0.99, 1.29) | 0.98 (0.89, 1.08) | 0.74 (0.64, 0.85) |
| Eastern Midwest (N= 555) | |||
| Model 1 | 0.80 (0.70, 0.91) | 1.06 (0.98, 1.15) | 1.03 (0.92, 1.17) |
| Model 2 | 0.82 (0.71, 0.94) | 1.07 (0.98, 1.17) | 0.99 (0.86, 1.13) |
| Mid-Atlantic (N=157) | |||
| Model 1 | 1.04 (0.85, 1.26) | 0.99 (0.92, 1.06) | 1.09 (0.89, 1.34) |
| Model 2 | 0.95 (0.76, 1.18) | 1.02 (0.94, 1.12) | 1.11 (0.88, 1.41) |
| New England (N= 53) | |||
| Model 1 | 0.65 (0.34, 1.26) | 0.93 (0.72, 1.19) | 1.61 (1.09, 2.39) |
| Model 2 | 0.65 (0.31, 1.36) | 0.97 (0.74, 1.28) | 1.60 (1.00, 2.57) |
| Pacific Northwest (N= 198) | |||
| Model 1 | 1.05 (0.90, 1.23) | 0.95 (0.81, 1.11) | 1.18 (0.94, 1.46) |
| Model 2 | 1.10 (0.94, 1.30) | 0.96 (0.81, 1.13) | 1.06 (0.79, 1.43) |
| Southeast (N= 849) | |||
| Model 1 | 0.99 (0.94, 1.03) | 1.01 (0.98, 1.04) | 0.95 (0.91, 1.01) |
| Model 2 | 0.98 (0.93, 1.02) | 0.99 (0.96, 1.03) | 0.98 (0.92, 1.04) |
| Southwest (N=390) | |||
| Model 1 | 0.84 (0.73, 0.97) | 0.98 (0.89, 1.06) | 1.17 (0.98, 1.39) |
| Model 2 | 0.83 (0.71, 0.98) | 1.00 (0.90, 1.11) | 1.17 (0.94, 1.47) |
CDC/ATSDR = Centers for Disease Control and Prevention (CDC) and Agency for Toxic Substances and Disease Registry (ATSDR). IQR = interquartile range. Spatial autocorrelation was modeled in Lagrange models with autoregressive correlation structure. Model 1 adjusts for the percentage of public water drawn from groundwater sources and population density. Model 2 further adjusts for county racial/ethnic composition (the proportion of residents who are non-Hispanic Black, American Indian/Native Alaskan, non-Hispanic Asian, non-Hispanic White, and Hispanic/Latino. Findings were also similar when models were further adjusted for either metropolitan versus non-metropolitan county status or county Rural-Urban Continuum Code. States included in each region are as follows: Central Midwest (North Dakota, South Dakota, Nebraska, Kansas, and Missouri), Eastern Midwest (Wisconsin, Illinois, Indiana, Michigan, Ohio, Minnesota, and Iowa), Mid-Atlantic (Pennsylvania, Maryland, District of Columbia, Delaware, New York, New Jersey, Connecticut, and Rhode Island), New England (Massachusetts, Vermont, New Hampshire, and Maine), Pacific Northwest (Washington, Oregon, Montana, Wyoming, and Idaho), Southeast (Oklahoma, Arizona, Louisiana, Mississippi, Alabama, Florida, Georgia, Tennessee, Kentucky, South Carolina, North Carolina, Virginia, and West Virginia), and Southwest (California, Nevada, Utah, Colorado, Arizona, New Mexico, and Texas).
Exclusion criteria
We restricted our analysis to conterminous US counties/county equivalents because counties in Alaska and Hawaii have few neighboring counties and unique geologic contexts impacting groundwater arsenic concentrations. A total of 2,639 conterminous US counties had CWS arsenic concentration estimates available. We further excluded 34 counties missing the percentage of public water sourced from groundwater sources, and 1 county missing population density for a final sample size of 2,604 counties.
Statistical analysis: County characteristics by socioeconomic vulnerability
We first described differences in county sociodemographic characteristics across tertiles of overall socioeconomic vulnerability. Across tertiles of the CDC/ATSDR’s overall socioeconomic vulnerability score, we compared mean CWS arsenic concentration estimates, total population and population density, percentage of public water sourced from groundwater, the proportion of adults with a high school diploma, median household income, the percent of residents living in rural areas, the percent of counties classified as metropolitan, and racial/ethnic composition (the percent of residents belonging to each Census-defined racial/ethnic group).
Statistical analysis: Geometric mean ratios of CWS arsenic by socioeconomic vulnerability
Because prior studies identified significant spatial autocorrelation in county-level CWS arsenic concentrations, we evaluated the county-level association between domains of socioeconomic vulnerability (proportion of adults with a high school diploma, median household income, and CDC/ATSDR overall socioeconomic vulnerability score) and mean CWS arsenic concentration in spatial regression models.17 We used a simple contiguity first order queen weighting matrix with binary values identifying neighbors (i= 1) and non-neighbors (i= 0), and used spatial lag models with an autoregressive correlation structure using the lagsarlm function from the “spatialreg” package in R.29,30 Lagrange Multiplier diagnostic tests via the lm.LMtest function in the R package “spatialreg” indicated both significant spatial lag and spatial error terms, and we proceeded with spatial lag models because model estimates were larger.
To quantify the association between county-level socioeconomic vulnerability and CWS arsenic concentrations, spatial lag models evaluated the geometric mean ratio (GMR) and 95% confidence intervals (CI) of county-level CWS arsenic concentrations per a higher socioeconomic vulnerability metric corresponding the interquartile range (IQR). The IQR was 0.15 for the proportion of adults with a high school diploma, $11,552 for median household income, and 0.5 for the CDC/ATSDR’s overall socioeconomic vulnerability index (vulnerability index scores ranged from 0–1). Model 1 adjusted for the percentage of public water drawn from groundwater sources and population density. Model 2 further adjusted for county racial/ethnic composition (the proportion of residents who are non-Hispanic Black, American Indian/Native Alaskan, non-Hispanic Asian, non-Hispanic White, and Hispanic/Latino). To evaluate potential effect measure modification, we repeated our nationwide analyses stratified by region and by metropolitan versus non-metropolitan counties. We also evaluated these associations via flexible quadratic spline models with knots at the 10th and 90th percentile of the socioeconomic vulnerability distribution (e.g., a flexible function of space). Alternative models with knots at the 50th and 75th percentiles yielded similar findings. We also further assessed flexible splines for models stratified by the nine Rural-Urban Continuum Codes to assess if rurality (as defined by population size, degree of urbanization, labor force commuting patterns, and adjacency to metro areas) further modified the association between overall socioeconomic vulnerability and CWS arsenic concentrations.
We conducted several additional sensitivity analyses. First, we repeated our main analyses using county-level 95th percentile CWS arsenic concentrations (rather than mean arsenic concentrations), which reflect the most highly exposed populations. Second, we also repeated our main analyses (nationwide, stratified by metropolitan versus non-metropolitan counties, and stratified by region) comparing GMRs across tertiles of CDC/ATSDR overall socioeconomic vulnerability score (setting tertile 1 as the reference) to evaluate the potential dose-response relationship.
RESULTS
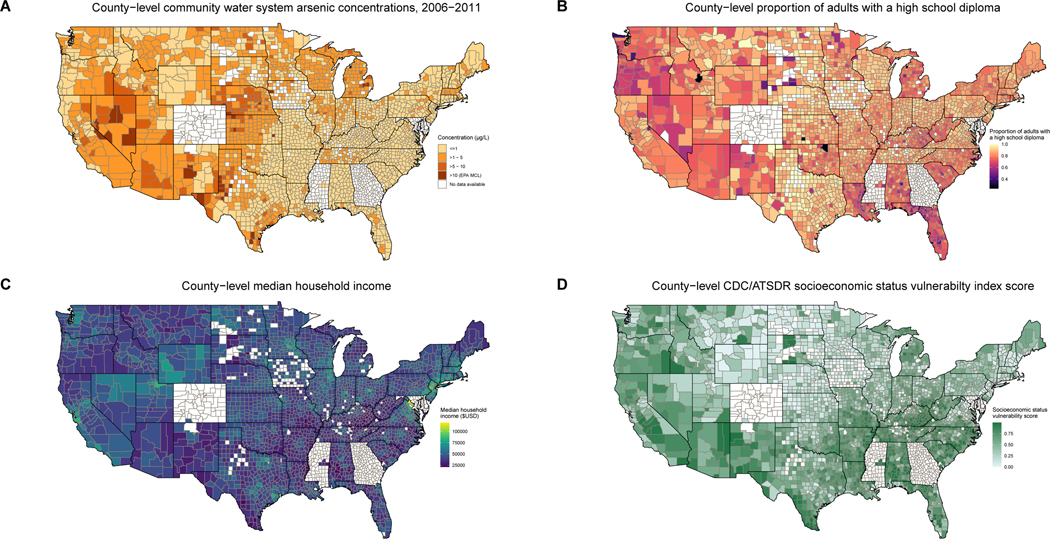
County-level domains of socioeconomic vulnerability and CWS arsenic concentrations are mapped in Figure 1. County-level CWS arsenic concentrations are generally highest in the southwest, west, and Great Plains regions of the US. The proportion of adults with a high school diploma and median household income appeared to follow similar spatial patterns, with higher income and high school educational attainment near large urban centers and cities. Counties with the highest CDC/ATSDR overall socioeconomic vulnerability scores were generally located in the southern, western, and Appalachian regions of the US.
Figure 1. Distribution of and county-level community water system (CWS) arsenic concentrations (2006–2011, Panel A), proportion of adults with a high school diploma (Panel B), median household income (Panel C), and CDC/ATSDR’s overall socioeconomic status vulnerability index (Panel D) across the conterminous US for N=2,604 counties included in the present analysis.
Counties shown in white were not included in the present analysis because CWS arsenic concentrations were not available for these counties. CDC/ATSDR = Centers for Disease Control and Prevention (CDC) and Agency for Toxic Substances and Disease Registry (ATSDR).
Table 1 presents county characteristics overall and stratified by tertile of CDC/ATSDR overall socioeconomic vulnerability score. Compared to counties in the first and second tertile of overall socioeconomic vulnerability, counties in the highest tertile of overall socioeconomic vulnerability (scores above 0.64) had lower mean CWS arsenic concentrations, smaller mean population size and smaller population density, lower percentages of public water sourced from groundwater sources, and higher percentages of non-Hispanic Black residents, American Indian/Alaskan Native residents, and Hispanic/Latino residents, although these differences did not appear to be significant.
Table 1.
County-level mean community water system (CWS) arsenic concentrations and sociodemographic characteristics (N= 2,604 counties), overall and stratified by tertile of the CDC/ATSDR’s socioeconomic status vulnerability index score.
| Overall | Tertile 1 (<= 0.33) | Tertile 2 (0.33–0.64 ) | Tertile 3 (<0.64) | |
|---|---|---|---|---|
| N counties | 2,604 | 859 | 859 | 886 |
| Mean CWS arsenic, 2006–2011 (mean, SD)a | 1.45 (2.29) | 1.78 (2.12) | 1.34 (2.36) | 1.24 (2.34) |
| Population size (mean, SD)b | 102,720 (332394) | 109,755 (223297) | 128,754 (371789) | 70,659 (375339) |
| Population density (per square mile, mean, SD)b | 179 (600) | 218 (727) | 197 (514) | 125 (533) |
| % public water from groundwater (mean, SD)c | 62 (42) | 71 (39) | 58 (42) | 57 (44) |
| % population living in a rural area (mean, SD)d | 58 (31) | 57 (34) | 53 (30) | 65 (28) |
| N (%) classified as non-metropolitane | 1,634 (63) | 472 (55) | 492 (57) | 670 (76) |
| Racial/ethnic composition (mean, SD) b | ||||
| % non-Hispanic Black | 7 (12) | 3 (5) | 6 (9) | 13 (17) |
| % American Indian/Alaskan Native | 2 (7) | 1 (2) | 1 (4) | 3 (11) |
| % Hispanic/Latino | 9 (14) | 5 (7) | 9 (13) | 11 (19) |
| % non-Hispanic White | 80 (19) | 88 (10) | 81 (16) | 71 (24) |
| % non-Hispanic Asian | 1 (2) | 1 (3) | 1 (2) | 1 (1) |
| Domains of socioeconomic vulnerability | ||||
| % of adults with a high school diploma (mean, SD)d | 84 (9) | 88 (7) | 83 (9) | 80 (9) |
| Median household income (mean, SD)d | 43,842 (10370) | 52,503 (11071) | 43,697 (5729) | 35,586 (4959) |
| CDC/ATSDR Social Vulnerability Index Scores (median and interquartile range)f | ||||
| Sum social vulnerability index | 0.48 (0.25 , 0.73) | 0.17 (0.08 , 0.28) | 0.49 (0.37 , 0.62) | 0.80 (0.67 , 0.90) |
| Overall socioeconomic vulnerability index | 0.49 (0.26 , 0.72) | 0.17 (0.09 , 0.25) | 0.48 (0.4 , 0.56) | 0.80 (0.72 , 0.90) |
CDC/ATSDR = Centers for Disease Control and Prevention (CDC) and Agency for Toxic Substances and Disease Registry (ATSDR).
Previously developed and described in detail (Nigra et al. 2020).
Derived from the 2010 US Census.
Estimates were calculated by the US Geological Survey for 2010 (Maupin et al. 2014).
Previously developed and published in the 2013 County Health Ranking database by the University of Washington Population Health Institute (ref).
Classified as “non-metropolitan” via United States Department of Agriculture Rural Urban Continuum codes.
The overall socioeconomic status vulnerability index is derived from 2010–2014 American Community Survey estimates of median household income and the percent of adults who are unemployed, living below the poverty line, and without a high school diploma. The index ranges from 0–1 and ranks counties nationwide (higher scores indicate lower socioeconomic status and higher socioeconomic vulnerability). The sum social vulnerability index sums CDC/ATSDR sub-indices for socioeconomic status, household composition and disability, minority status and language, and housing type and transportation.
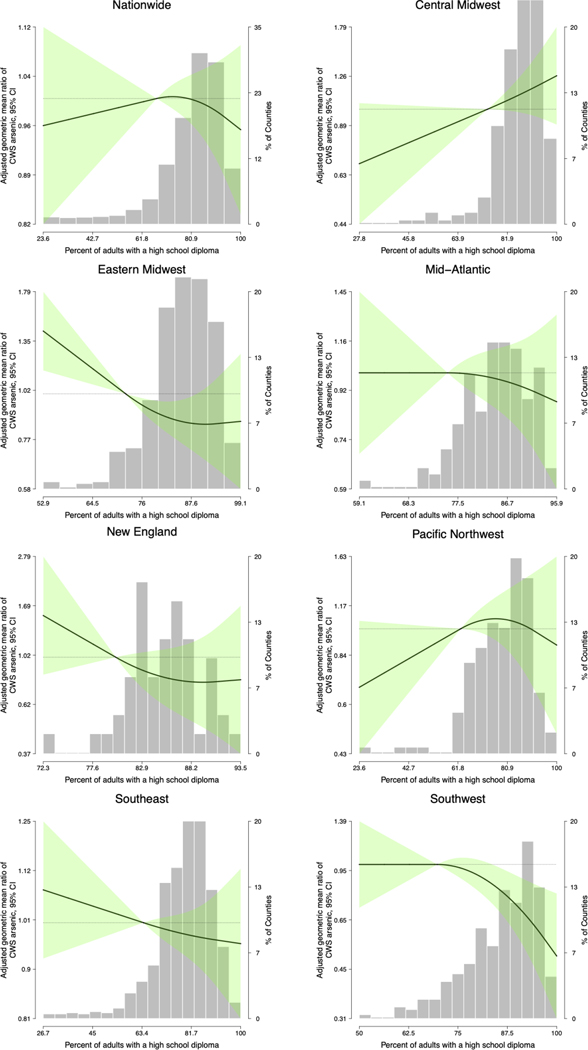
Table 2 presents nationwide and stratified (by region and metropolitan versus non-metropolitan counties) spatial lag model GMRs (95% CIs) of mean CWS arsenic per higher socioeconomic vulnerability domain corresponding to the interquartile range. In nationwide analyses evaluating the association between high school educational attainment and CWS arsenic concentrations, the fully adjusted GMR (95% CI) of CWS arsenic per 0.15 higher proportion of adults with a high school diploma was 1.00 (0.96, 1.04). The association remained null in analyses stratified by non-metropolitan counties versus metropolitan counties, but was modified by region. A higher proportion of adults with a high school diploma was associated with lower CWS arsenic concentrations in the Eastern Midwest (0.82, 95% CI 0.71, 0.94, corresponding to a 18% decrease) and Southwest (0.83, 95% CI 0.71, 0.98, corresponding to a 17% decrease). Fully adjusted, flexible quadratic spline models for the nationwide and region-specific associations between high school educational attainment and CWS arsenic concentrations are displayed in Figure 2. A higher proportion of adults with a high school diploma was also significantly associated with lower CWS arsenic concentrations in fully adjusted, flexible quadratic spline models for the Eastern Midwest and the Southwest regions (Figure 2). Associations were also inverse but not significant in New England. In the Central Midwest, the proportion of adults with a high school diploma was positively but not significantly associated with higher CWS arsenic concentrations (Table 2, Figure 2). In analyses evaluating the association between median household income and CWS arsenic concentrations, associations were null in nationwide analyses, among metropolitan counties, and in all region-specific analyses, although median household income was positively and significantly associated with CWS arsenic concentrations among non-metropolitan counties (GMR 1.09, 95% CI 1.03, 1.15, corresponding to a 9% increase Table 2).
Figure 2. Geometric mean ratios (95% CI) of community water system (CWS) arsenic concentrations per higher percent of adults with a high school diploma, based on spatial lag quadratic spline models with knots at the 10th and 90th percentiles of the socioeconomic vulnerability score distribution.
Lines represent the geometric mean and green shaded areas surrounding the lines represent 95% confidence intervals. Shaded gray bars represent the county-level distribution of socioeconomic status vulnerability scores and are shown as “% of Counties” in the right y-axis. Models adjust for the percentage of public water drawn from groundwater sources, population density, median household income, and county racial/ethnic composition (the proportion of residents who are non-Hispanic Black, American Indian/Native Alaskan, non-Hispanic Asian, non-Hispanic White, and Hispanic/Latino). The reference was set to the 5th percentile of the distribution of the percent of adults with a high school diploma. Models considering spline knots at other percentiles (50th, 75th) yielded similar findings. Spatial neighbors were identified via a simple queen contiguity matrix for neighbors (i=1) versus non-neighbors (i=0).
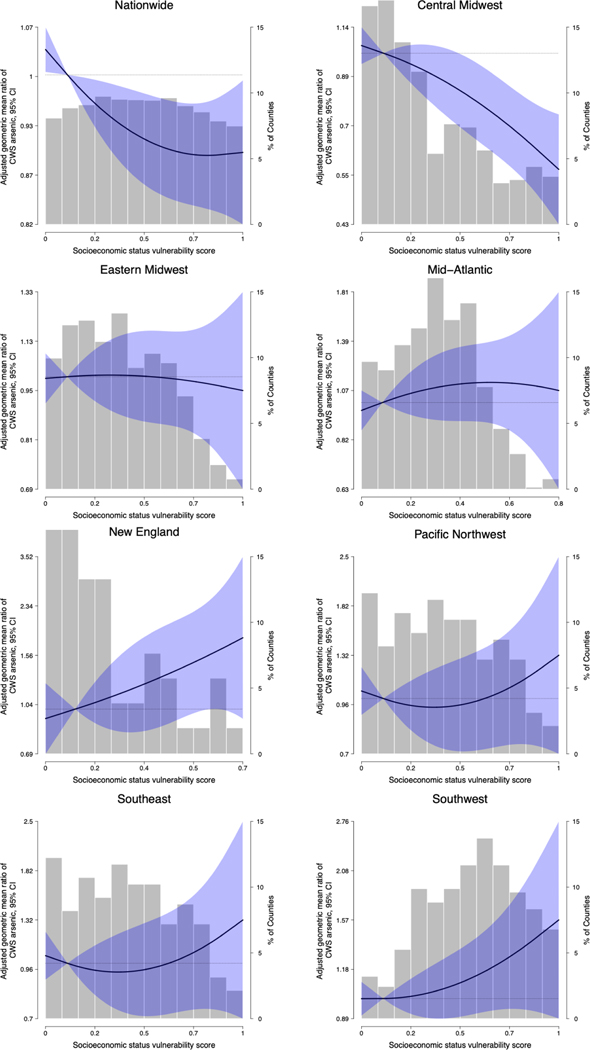
In nationwide analyses considering the CDC/ATSDR’s overall socioeconomic vulnerability score, the fully adjusted GMR (95% CI) of CWS arsenic per 0.5 unit higher overall socioeconomic vulnerability score was 0.93 (0.88, 0.98), corresponding to a 7% decrease (Table 2). Among non-metropolitan counties, the fully adjusted GMR per 0.5 unit increase in social vulnerability score was 0.85 (0.79, 0.92) (similar to findings for median household income). Associations were similar but not significant in metropolitan counties (GMR 0.95, 95% CI 0.87, 1.03). In analyses stratified by region, the fully adjusted GMR of CWS arsenic per 0.5 unit higher overall socioeconomic vulnerability score was 0.74 (0.64, 0.85) in the Central Midwest, and 1.60 (1.00, 2.57) in New England (Table 2). Associations between socioeconomic vulnerability and CWS arsenic were positive but not significant in the Mid-Atlantic (1.11, 95% CI 0.88, 1.41), Pacific Northwest (1.06, 95% CI 0.79, 1.43), and Southwest (1.17, 95% CI 0.94, 1.47), and close to the null in the Eastern Midwest and Southeast. Adjustment for racial ethnic composition attenuated effect estimates in the Pacific Northwest and strengthened effect estimates in the Central Midwest (Model 1 versus Model 2).
Fully adjusted, flexible quadratic spline models for the nationwide and region-specific associations between overall socioeconomic vulnerability and CWS arsenic concentrations are displayed in Figure 3. Associations were inverse, significant, and relatively linear in nationwide analysis and in the Central Midwest. Associations were positive but not statistically significant in New England, the Pacific Northwest, the Southeast, and the Southwest. In analyses stratified by metropolitan versus non-metropolitan counties, the association between socioeconomic vulnerability and CWS arsenic was inverse for both metropolitan and non-metropolitan counties, but appeared linear and was significant for non-metropolitan counties only (Supplemental Figure 1). Wider confidence intervals for metropolitan counties may reflect the smaller sample size. In sensitivity analyses further stratified by USDA Rural Urban Continuum Codes, associations were only inverse and significant for non-metropolitan counties with populations less than 20,000, regardless of adjacency to a metropolitan area (Supplemental Figure 2).
Figure 3. Geometric mean ratios (95% CI) of community water system (CWS) arsenic concentrations per higher CDC/ATSDR overall socioeconomic vulnerability score, based on spatial lag quadratic spline models with knots at the 10th and 90th percentiles of the socioeconomic vulnerability score distribution.
CDC/ATSDR = Centers for Disease Control and Prevention (CDC) and Agency for Toxic Substances and Disease Registry (ATSDR). Lines represent the geometric mean and blue shaded areas surrounding the lines represent 95% confidence intervals. Shaded gray bars represent the county-level distribution of socioeconomic status vulnerability scores and are shown as “% of Counties” in the right y-axis. Models adjust for the percentage of public water drawn from groundwater sources, population density, and county racial/ethnic composition (the proportion of residents who are non-Hispanic Black, American Indian/Native Alaskan, non-Hispanic Asian, non-Hispanic White, and Hispanic/Latino). Models considering spline knots at other percentiles (50th, 75th) yielded similar findings. Spatial neighbors were identified via a simple queen contiguity matrix for neighbors (i=1) versus non-neighbors (i=0).
Findings were largely similar when evaluating 95th percentile CWS arsenic concentrations, with significant inverse associations in the Central Midwest, significant positive associations in New England, and positive but non-significant associations in the Mid-Atlantic and Southwest (Supplemental Table 1). In sensitivity analyses assessing associations across tertiles of CDC/ATSDR overall socioeconomic vulnerability index, findings were similar to those in the main analyses assessing an increase corresponding to the interquartile range (Supplemental Table 2).
DISCUSSION
In this county-level analysis of the association between socioeconomic vulnerability and regulated CWS arsenic concentrations, associations were modified by region, driven by individual components of the overall socioeconomic vulnerability index, and differed for counties with populations less than 20,000 residents. Independent of county racial/ethnic composition, higher proportions of residents with high school diplomas was associated with lower CWS arsenic concentrations in the Southwest, New England, and Eastern Midwest, highlighting environmental justice concerns for communities in these regions with low high school educational attainment. Given that associations were modified by region and specific to educational attainment, nationwide associations and those considering the overall socioeconomic vulnerability score are not appropriate measures of the association between socioeconomic vulnerability and CWS arsenic. Interpretations should be made considering region, population size, and specific domains of socioeconomic vulnerability.
Socioeconomic status is a complex construct with various definitions, including, for example, “the relative position… on a hierarchical social structure, based on access or control over wealth, prestige, and power,” and “the capacity to create or consume goods.”31,32 The CDC/ATSDR’s socioeconomic vulnerability index was specifically developed to reflect community level income, poverty, employment, and education in the context of resilience to disasters and disaster management (e.g., high income households are more likely to have insurance policies, financial investments, and stable employment to mitigate household losses).33 In the context of drinking water disparities, these specific domains of socioeconomic status (income, poverty, employment, and education) are likely associated with both the sociopolitical and built environment at the household, community, and regional levels.14,19
The current study adds to a growing body of evidence identifying inequalities in regulated CWS arsenic concentrations across US populations, by racial/ethnic composition, region, broad sociodemographic characteristics, and now socioeconomic vulnerability and education levels.15–18,27 Prior studies on US drinking water metal concentrations by community socioeconomic vulnerability are sparse. One prior study in California found no significant association between home ownership and regulated public water arsenic concentrations.18
Although higher overall socioeconomic vulnerability was associated with lower CWS arsenic concentrations in both metropolitan and non-metropolitan counties in nationwide analyses, these associations were only significant for counties with populations less than 20,000, regardless of adjacency to metropolitan counties. Moreover, specific associations with both median household income and the proportion of adults with a high school diploma were null for both metropolitan and non-metropolitan counties. Therefore, other components of the overall socioeconomic vulnerability index not evaluated in this analysis (i.e., the percent of adults who are unemployed and living below the poverty line) are likely driving the observed nationwide association between higher socioeconomic vulnerability and lower CWS arsenic concentrations.
These nationwide findings for non-metropolitan counties and those with populations less than 20,000 might be explained by differences in drinking water infrastructure and unregulated domestic well use in rural areas. While the county-level measures of socioeconomic vulnerability evaluated in the current study reflect the overall county population, residents of lower socioeconomic status (with lower household incomes, or those without a high school diploma) might be more often served by unregulated domestic wells in non-metropolitan areas compared to metropolitan areas.26 Although characteristics of the population reliant on public drinking water systems may be most relevant to the association between community socioeconomic vulnerability and CWS arsenic concentrations, the measures of community socioeconomic vulnerability used in our analysis did not differentiate between community members using unregulated domestic wells versus regulated CWSs, and these findings may therefore be confounded by the proportion and sociodemographic characteristics of community members using unregulated domestic wells (i.e., even in rural or sparsely population counties with overall high socioeconomic vulnerability, only the highest income residents may be served by CWSs).
Across several complementary analyses, higher socioeconomic vulnerability (especially lower high school diploma attainment) was associated with higher CWS arsenic concentrations in the Eastern Midwest, Southwest, and New England, while higher socioeconomic vulnerability appeared to be associated with lower CWS arsenic concentrations in the Central Midwest. Taken together, our findings indicate that the differing relationship between domains of socioeconomic vulnerability and CWS arsenic concentrations across US regions potentially reflects regional/local differences in both socioeconomic context (e.g. distribution of household income and educational attainment, relevance of high school level educational attainment for social and political capitol, etc.) and drinking water infrastructure (e.g. prevalence of unregulated domestic wells, state level financial and technical support for regulated CWSs, etc.), as we predicted. The observed effect measure modification by region may also reflect differences across states and tribal agencies in enforcement of both monitoring and health-related violations, monitoring requirements and policies, and the availability of financial and technical aid to support CWSs to lower contaminant concentrations (typically achieved through either switching or mixing source water, or installing/improving treatment systems). These considerations underscore the importance of further assessing these associations at finer geographic resolutions (e.g., Census tract, zip code) within specific states and regions of the US, especially those that share the same CWS regulatory oversight and provide similar financial and technical support to reduce water contaminant levels (e.g., states, tribal authorities). Regardless, our findings raise environmental justice concerns for socioeconomically vulnerable communities in the Eastern Midwest, Southwest, and New England regions, especially communities with a high percentage of adults without high school diplomas.
Our analysis has several limitations. We were unable to assess the association at finer geographic resolutions (e.g., Census tract) because nationwide estimates of CWS arsenic concentrations at these resolutions are not yet available. This knowledge gap persists because only some states make public water system distribution boundary maps publicly available. The region and rurality-specific associations with domains of socioeconomic vulnerability observed here at the county-level may differ from those that could be estimated at the Census tract- or zip code-level in future analyses. Our county-level analysis was also limited by a small sample size, especially for stratified analyses. Further, although our current analysis attempted to isolate the association between socioeconomic vulnerability and CWS arsenic concentrations independent of racial/ethnic composition, future analyses should consider interactions between these two community sociodemographic characteristics, which interact with each other and with other domains of marginalization and social vulnerability (e.g., linguistic isolation, racial segregation, age structure, occupation, etc.). Although this study only assessed public drinking water arsenic concentrations, prior indicate that soil metal concentrations are elevated in some low-income communities and communities of color, especially in the southern US.34 Future studies should assess whether community socioeconomic vulnerability is associated with arsenic exposure from multiple sources (e.g. drinking water, air pollution, soil, etc.). Although social vulnerability may also be related to poor drinking water quality in other countries, findings from this analysis are only relevant to the US. Future studies can assess differences and similarities in the association between social vulnerability and water arsenic concentrations across the globe. Further work should also assess the associations between estimated CWS arsenic concentrations and related health outcomes across diverse US populations.
CONCLUSIONS
Our findings indicate that educational attainment, but not complex summary vulnerability indices, are more relevant for explaining inequalities in regulated CWS arsenic concentrations in the US. Moreover, associations between educational attainment and regulated CWS arsenic concentrations differed by region. Lower high school diploma attainment was associated with higher CWS arsenic concentrations in the Eastern Midwest, Southwest, and New England, while higher socioeconomic vulnerability – but not educational attainment - appeared to be associated with lower CWS arsenic concentrations in the Central Midwest.
Supplementary Material
HIGHLIGHTS.
We evaluated the association between socioeconomic status and public water arsenic
Lower high school diploma attainment was associated with higher public water arsenic concentrations
Significant associations were specific to the Southwest and Eastern Midwest
Complex indices of socioeconomic status are not relevant for inequalities in US public water arsenic
Funding:
This study was supported by NIEHS grants P30ES009089 and R01ES028758, and NIH/NIDCR grant DP5OD031849 (Office of the Director, NIH and NIDCR).
Footnotes
Declaration of competing interests:
The authors declare that they have no actual or potential competing financial interests.
REFERENCES
- 1.Sanchez TR, Powers M, Perzanowski M, George CM, Graziano JH, Navas-Acien A. A meta-analysis of arsenic exposure and lung function: Is there evidence of restrictive or obstructive lung disease? Current Environmental Health Reports. Jun 2018;5(2):244–254. doi: 10.1007/s40572-018-0192-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Powers M, Sanchez TR, Grau-Perez M, et al. Low-to-Moderate Arsenic Exposure and Respiratory Health in American Indian Communities. Annals of the American Thoracic Society. Apr 2018;15(Supplement_2):S128–s129. doi: 10.1513/AnnalsATS.201708-636MG [DOI] [Google Scholar]
- 3.Milton AH, Hussain S, Akter S, Rahman M, Mouly TA, Mitchell K. A review of the effects of chronic arsenic exposure on adverse pregnancy outcomes. International Journal of Environmental Research and Public Health. May 23 2017;14(6)(6):556. doi: 10.3390/ijerph14060556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Quansah R, Armah FA, Essumang DK, et al. Association of arsenic with adverse pregnancy outcomes/infant mortality: A systematic review and meta-analysis. Environmental Health Perspectives. May 2015;123(5):412–21. doi: 10.1289/ehp.1307894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grau-Perez M, Kuo CC, Gribble MO, et al. Association of low-moderate arsenic exposure and arsenic metabolism with incident diabetes and insulin resistance in the Strong Heart Family Study. Environmental Health Perspectives. Dec 20 2017;125(12):127004. doi: 10.1289/ehp2566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kuo C-C, Moon KA, Wang S-L, Silbergeld E, Navas-Acien A. The association of arsenic metabolism with cancer, cardiovascular disease, and diabetes: A systematic review of the epidemiological evidence. Environmental Health Perspectives. 2017;125(8)(8):087001–087001. doi: 10.1289/EHP577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pinchoff J, Monseur B, Desai S, Koons K, Alvero R, Hindin MJ. Is living in a region with high groundwater arsenic contamination associated with adverse reproductive health outcomes? An analysis using nationally representative data from India. International Journal of Hygiene and Environmental health. Jan 2022;239:113883. doi: 10.1016/j.ijheh.2021.113883 [DOI] [PubMed] [Google Scholar]
- 8.Moon KA, Oberoi S, Barchowsky A, et al. A dose-response meta-analysis of chronic arsenic exposure and incident cardiovascular disease. International Journal of Epidemiology. Apr 25 2018;46(6):1924–1939. doi: 10.1093/ije/dyy073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nigra AE, Moon KA, Jones MR, Sanchez TR, Navas-Acien A. Urinary arsenic and heart disease mortality in NHANES 2003–2014. Environmental Research. Sep 2021;200:111387. doi: 10.1016/j.envres.2021.111387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nachman KE, Punshon T, Rardin L, et al. Opportunities and Challenges for Dietary Arsenic Intervention. Environmental Health Perspectives. Aug 2018;126(8):84503. doi: 10.1289/ehp3997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.United States Environmental Protection Agency. Report on the Environment: Drinking Water. 11 January 2022. file:///Users/aen2136/Downloads/drinking-water.pdf [Google Scholar]
- 12.Ravalli F, Yuanzhi Y, Bostick BC, et al. Sociodemographic inequalities in uranium and other metals in community water systems across the US, 2006–2011. In press at Lancet Planetary Health. 2022; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kurzius-Spencer M, Burgess JL, Harris RB, et al. Contribution of diet to aggregate arsenic exposures: An analysis across populations. Journal of Exposure Science & Environmental Epidemiology. Mar-Apr 2014;24(2)(2):156–62. doi: 10.1038/jes.2013.37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Balazs CL, Ray I. The drinking water disparities framework: on the origins and persistence of inequities in exposure. Am J Public Health. Apr 2014;104(4):603–11. doi: 10.2105/ajph.2013.301664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nigra AE, Chen Q, Chillrud SN, et al. Inequalities in public water arsenic concentrations in counties and community water systems across the United States, 2006–2011. Environmental Health Perspectives. 2020;128(12):127001. doi: 10.1289/EHP7313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nigra AE, Navas-Acien A. Arsenic in US correctional facility drinking water, 2006–2011. Environmental Research. Jun 12 2020;188:109768. doi: 10.1016/j.envres.2020.109768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martinez-Morata I, Bostick BC, Conroy-Ben O, et al. Nationwide geospatial analysis of county-level racial/ethnic composition and public drinking water arsenic and uranium. Under review at Nature Communications. 2022; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pace C, Balazs C, Bangia K, et al. Inequities in Drinking Water Quality Among Domestic Well Communities and Community Water Systems, California, 2011‒2019. Am J Public Health. Jan 2022;112(1):88–97. doi: 10.2105/ajph.2021.306561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Deziel NC, Warren JL, Bravo MA, Macalintal F, Kimbro RT, Bell ML. Assessing community-level exposure to social vulnerability and isolation: spatial patterning and urban-rural differences. Journal of Exposure Science & Environmental Epidemiology. Apr 6 2022;doi: 10.1038/s41370-022-00435-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.United States Environmental Protection Agency. The analysis of regulated contaminant occurrence data from public water systems in support of the Third Six-Year Review of National Primary Drinking Water Regulations: Chemical Phase Rules and Radionuclides Rules. Accessed 20 July 2020, https://www.epa.gov/sites/production/files/2016-12/documents/810r16014.pdf
- 21.United States Environmental Protection Agency. The data management and quality assurance/quality control process for the Third Six-Year Review Information Collection Rule Dataset. Accessed 20 July 2020, https://nepis.epa.gov/Exe/ZyNET.exe/P100QO9Q.TXT?ZyActionD=ZyDocument&Client=EPA&Index=2016+Thru+2020&Docs=&Query=&Time=&EndTime=&SearchMethod=1&TocRestrict=n&Toc=&TocEntry=&QField=&QFieldYear=&QFieldMonth=&QFieldDay=&IntQFieldOp=0&ExtQFieldOp=0&XmlQuery=&File=D%3A%5Czyfiles%5CIndex%20Data%5C16thru20%5CTxt%5C00000001%5CP100QO9Q.txt&User=ANONYMOUS&Password=anonymous&SortMethod=h%7C-&MaximumDocuments=1&FuzzyDegree=0&ImageQuality=r75g8/r75g8/x150y150g16/i425&Display=hpfr&DefSeekPage=x&SearchBack=ZyActionL&Back=ZyActionS&BackDesc=Results%20page&MaximumPages=1&ZyEntry=1&SeekPage=x&ZyPURL
- 22.Centers for Disease Control and Prevention/ Agency for Toxic Substances and Disease Registry/ Geospatial Research Analysis and Services Program. CDC/ATSDR Social Vulnerability Index, 2014. Database US. Accessed 4 April 2022, https://www.atsdr.cdc.gov/placeandhealth/svi/data_documentation_download.html
- 23.Remington PL, Catlin BB, Gennuso KP. The County Health Rankings: rationale and methods. Population Health Metrics. 2015/04/17 2015;13(1):11. doi: 10.1186/s12963-015-0044-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.The University of Wisconsin Population Health Institute and Robert Wood Johnson Foundation. National Data & Documentation: 2010–2019: 2013 County Health Rankings,. Accessed 4 April 2022, https://www.countyhealthrankings.org/explore-health-rankings/rankings-data-documentation/national-data-documentation-2010-2019
- 25.United States Census Bureau. USA Counties: 2011. Accessed 4 April 2022, https://www.census.gov/library/publications/2011/compendia/usa-counties-2011.html
- 26.Maupin MA, Kenny JF, Hutson SS, Lovelace JK, Barber NL, Linsey KS. Estimated use of water in the United States in 2010. Accessed 20 July 2020, https://pubs.usgs.gov/circ/1405/pdf/circ1405.pdf
- 27.Spaur M, Lombard MA, Ayotte JD, et al. Associations between private well water and community water supply arsenic concentrations in the conterminous United States. The Science of the Total Environment. Sep 15 2021;787:147555. doi: 10.1016/j.scitotenv.2021.147555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.United States Department of Agriculture. Rural-Urban Continuum Codes. Accessed 4 April 2022, https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/
- 29.Bivand R, Piras G. Comparing implementations of estimation methods for spatial econometrics. Journal of Statistical Software. 2015;63:1–36. [Google Scholar]
- 30.Bivand RS, Pebesma EJ, Gómez-Rubio V, Pebesma EJ. Applied spatial data analysis with R. vol 747248717. Springer; 2008. [Google Scholar]
- 31.Mueller CW, Parcel TL. Measures of socioeconomic status: Alternatives and recommendations. Child development. 1981:13–30. [Google Scholar]
- 32.Miech RA, Hauser RM. Socioeconomic status and health at midlife: a comparison of educational attainment with occupation-based indicators. Annals of epidemiology. 2001;11(2):75–84. [DOI] [PubMed] [Google Scholar]
- 33.Flanagan BE, Gregory EW, Hallisey EJ, Heitgerd JL, Lewis B. A social vulnerability index for disaster management. Journal of homeland security and emergency management. 2011;8(1) [Google Scholar]
- 34.Jones DH, Yu X, Guo Q, Duan X, Jia C. Racial Disparities in the Heavy Metal Contamination of Urban Soil in the Southeastern United States. International Journal of Environmental Research and Public Health. Jan 19 2022;19(3)doi: 10.3390/ijerph19031105 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.