Abstract
Purpose
To describe a case of corneal decompensation in the setting of a Descemet's membrane detachment that developed following aborted Hydrus minimally invasive glaucoma surgery (MIGS) that was successfully treated with a Descemet's stripping only procedure.
Observations
A 75 year-old female patient presented with symptomatic corneal decompensation following complicated Hydrus MIGS surgery. Ocular coherence tomography demonstrated an inferonasal Descemet's detachment with overlying edema. Specular microscopy revealed undetectable cells centrally but a peripheral cell density of 1446 cells/mm2. The Descemet's detachment did not respond to an intracameral air injection and a subsequent Descemet's stripping only procedure was performed. The corneal edema resolved by postoperative week 6. At postoperative month 2, best corrected visual acuity was 20/40 and specular microscopy demonstrated central cell density of 975 cells/mm2.
Conclusions and Importance
Descemet's stripping only can be an effective treatment for some cases of corneal decompensation that occur in the setting of a Descemet's membrane detachment from complicated intraocular surgery, such as in this case with MIGS surgery.
Keywords: Descemet stripping only, DSO, Descemetorrhexis without endothelial keratoplasty, DWEK, Minimally invasive glaucoma surgery, Hydrus
1. Introduction
Descemet stripping only (DSO) is emerging as an alternative treatment to Descemet membrane endothelial keratoplasty (DMEK) for Fuchs endothelial corneal dystrophy (FECD) with healthy peripheral endothelium. As endothelial cell function declines in Fuchs dystrophy, visually significant corneal edema can develop, leading to microcystic edema, bullae, subepithelial fibrosis, and vision loss.1 Rather than replacing endothelial cells with an allograft, DSO removes pathologic guttae via a central descemetorrhexis, thereby allowing healthy peripheral endothelial cells to migrate into the central void and clear the corneal edema.2
Beyond Fuchs dystrophy, DSO is a potential treatment for some cases of post-surgical corneal decompensation with healthy peripheral endothelium.3 Here, we describe a case of corneal edema following a complicated and eventually aborted Hydrus implantation that was successfully managed with DSO. This is the first reported case of DSO performed for corneal decompensation in the setting of a Descemet's membrane detachment that developed following a complicated MIGS surgery.
2. Case report
A 75 year-old woman was referred for visually significant corneal edema in her right eye following complicated Hydrus MIGS surgery 5 months prior. The Hydrus procedure was complicated by challenges with inserting the MIGS device and the Hydrus implant was eventually explanted. At the initial evaluation, uncorrected visual acuity was 20/100, improving to 20/60 with pinhole, and intraocular pressure was 18 mmHg. Slit lamp examination revealed moderate diffuse corneal edema, more pronounced inferonasally (Fig. 1A, 1B). No guttae were apparent in either eye. Central corneal thickness by ultrasound pachymetry (Pachmate 2, DGH Technology, Exton, PA) was 628 μm OD and 563 μm OS. A focal, inferonasal Descemet's detachment from 3:00 to 6:00 was observed on slit lamp examination and anterior segment optical coherence tomography (Visante, Carl Zeiss Meditec, Dublin, CA) (Fig. 2A) with a 4 mm × 5 mm area of overlying edema. Specular microscopy (Tomey EM-3000, Phoenix, AZ) in the right eye revealed no cells centrally (Fig. 3A) but a cell density of 1446 cells/mm2 in the superior mid-peripheral cornea (Fig. 3B).
Fig. 1.
A and B, Slit lamp photographs demonstrating diffuse corneal edema. C and D, Slit lamp photographs demonstrating resolution of corneal edema 2 months after DSO.
Fig. 2.
A, Visante anterior segment optical coherence tomography (ASOCT) revealed a Descemet's membrane detachment from 3:00 to 6:00 at presentation. B, One week after DSO, ASOCT shows no residual Descemet's detachment.
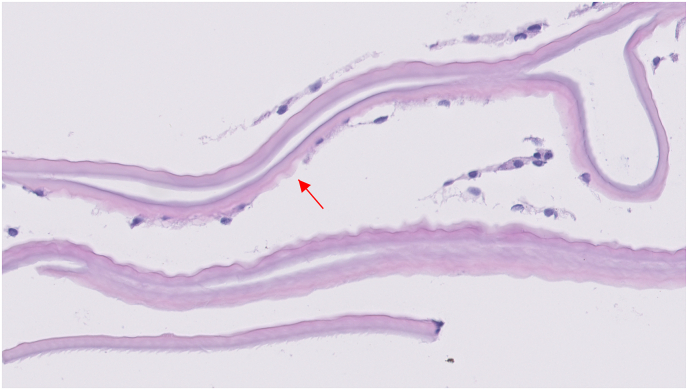
Fig. 3.
A, Specular microscopy at presentation demonstrates undetectable endothelial cells in the central cornea. B, Specular microscopy of the superior mid-peripheral cornea with a cell density of 1446 cells/mm2. C, Specular microscopy 2 months after DSO reveals repopulation of the central cornea with a cell density of 975 cells/mm2.
In an attempt to reattach the Descemet's detachment, intracameral air injection was performed and the patient positioned supine for 2 days. After 1 week, there was no clinical improvement in corneal edema, nor any improvement in the Descemet's detachment, confirmed by Visante OCT. DSO was then performed. The borders of the Descemet's detachment were identified and marked using intraoperative OCT guidance (Rescan 700, Carl Zeiss Meditec, Dublin, CA). Gorovoy DSO forceps (Moria Surgical, Doylestown, PA) were used to perform a 4 mm × 5 mm inferiorly decentered descemetorrhexis that encompassed the Descemet's detachment. Histopathology revealed endothelial cell atrophy and scattered guttata consistent with Fuchs dystrophy (Fig. 4).
Fig. 4.
Histopathology of Descemet's membrane showing endothelial cell atrophy and scattered guttata (red arrow). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
On postoperative day 1 visual acuity was 20/60 with overlying edema in the area of the descemetorrhexis, involving the inferior two-thirds of the entrance pupil. Gatifloxacin and prednisolone were administered 4 times daily in addition to the patient's glaucoma eyedrops. At postoperative week 1, uncorrected visual acuity remained stable at 20/60 but there was improved corneal edema over the area of the DSO, consistent with the Pentacam pachymetry map (Fig. 5A). Visante OCT showed no remaining Descemet's detachment (Fig. 2B). Prednisolone was tapered over 1 month.
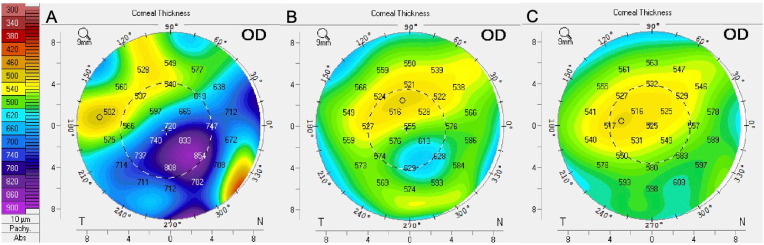
Fig. 5.
A, Pentacam pachymetry map 1 week after DSO demonstrates corneal edema concentrated inferonasally over the descemetorrhexis. B, Marked reduction in corneal thickness on Pentacam 6 weeks after DSO. C, Further recovery to relatively normal corneal thickness on the Pentacam pachymetry map 2 months after DSO.
By postoperative week 6, the corneal edema had nearly resolved, leaving a mild central subepithelial opacity on slit lamp examination. Uncorrected visual acuity was 20/60 and central corneal thickness by ultrasound pachymetry had improved to 527 μm. Significant improvement in the corneal edema was also seen on the Pentacam pachymetry map (Fig. 5B). Two months after the DSO, visual acuity and central corneal thickness by ultrasound pachymetry continued to improve, reaching 20/40 and 511 μm, respectively. The cornea appeared even clearer upon slit lamp examination (Fig. 1C, 1D) with resolution of the inferonasal edema on the Pentacam pachymetry map (Fig. 5C). Specular microscopy revealed a central cell density of 975 cells/mm2, indicating endothelial cell recovery centrally (Fig. 3C).
Six months following DSO, the patient's uncorrected visual acuity was 20/40. There was no corneal edema and the central corneal thickness by ultrasound pachymetry was 530 μm.
3. Discussion
This is the first case of DSO being successfully used to treat corneal decompensation with a Descemet's membrane detachment following a complicated MIGS procedure. Thus far, the primary indication for DSO has been Fuchs endothelial dystrophy4 with healthy peripheral endothelium. This case expands the indications for DSO to include some cases of post-surgical corneal edema, a category for which endothelial keratoplasty and penetrating keratoplasty have been the only therapeutic options for visual rehabilitation. The ideal cases would be sectoral corneal edema with healthy peripheral endothelium. Patients with surgically induced corneal edema often have or will develop other ophthalmic co-morbidities so the benefits of DSO - elimination of graft rejection risk and need for long-term topical corticosteroids - is particularly appealing. For glaucoma patients such as our patient, avoiding risk and optic nerve damage from steroid-induced glaucoma is a notable advantage.
In this case, the resolution of corneal edema 6 weeks postoperatively supports a generalized theory behind DSO: so long as there remains a sufficient reserve of healthy endothelial cells surrounding the area of injury, a descemetorrhexis can facilitate cellular migration and repopulation. Fuchs dystrophy may not need to be the underlying cause of corneal injury. Although this patient was later found to have underlying Fuchs dystrophy based on the presence of guttae on histopathology, we suspect that the severity of Fuchs was mild as there were no visible guttae present in either eye. Only scattered guttae were observed on histopathology. In addition, the corneal edema did not involve the entire central cornea as the superior one-third of the entrance pupil was relatively clear and accounted for the 20/60 pinhole vision. Had the Fuchs dystrophy been more advanced prior to the original Hydrus surgery, more extensive central corneal edema without such a sharp demarcation between edematous and normal cornea would have been expected. Moreover, the inferior peripheral location of the corneal edema is not where Fuchs dystrophy presents but rather contiguous with the site of the paracentesis through which the Hydrus procedure was performed.
Certainly, the underlying Fuchs dystrophy may lead to the cornea being more susceptible to surgical damage. A recent study found a significant correlation between an individual's genetic TCF4 allele repeat load and longer clearance times post-DSO.5 However, in this case, we don't ascribe much culpability to the underlying Fuchs dystrophy because peripheral endothelial cells are generally healthier in this disease. As such, even though this patient did have Fuchs dystrophy, we believe it is more appropriate to characterize this case as primarily a post-surgical corneal decompensation. It is worth noting that there have been reported cases of spontaneous resolution of Descemet's membrane detachment within a 5–6 month period.6,7 However, our patient presented 5 months following the aborted MIGS procedure without evidence of corneal clearance, making it reasonable to pursue surgical intervention. A persistent fibrotic Descemet detachment as visualized by the tense flat detachment in the Visante OCT probably prevented resolution. Removal of this mechanical barrier thus allowed healthy endothelial cells to migrate across the bare stroma to deturgesce the stroma.
Although there is not yet a standardized protocol for DSO, systematic review and meta-analysis by Franceschino et al. suggest that a central descemetorrhexis of 4 mm improves postoperative corneal clearing in Fuchs dystrophy.8 In FECD patients, corneal edema typically resolves 4–12 weeks following DSO.9 In our case, a decentered, inferonasally positioned, 4 × 5 mm descemetorrhexis was performed, indicating that the descemetorrhexis does not need to be located centrally for complete recovery. Corneal clearance was achieved in this case after 6 weeks. DSO with temporal, sectoral descemetorrhexis that successfully cleared in 10 weeks has also been reported.3 Both cases had recovery times comparable to DSO in FECD featuring a central descemetorrhexis. Compared to primary FECD cases, post-surgical or traumatic corneal edema and more likely to present with peripheral corneal decompensation. DMEK is more difficult to perform in such cases as it requires a larger graft and comfort with mobilizing the tissue towards the periphery. For some of these patients, DSO provides another option to those who might not be ideal candidates for DMEK.
Although not used in our case, topical rho kinase (ROCK) inhibitors such as ripasudil (not commercially available in the US) and netarsudil (used off-label for endothelial rejuvenation in the US) show promise as potential adjuvant therapies that can accelerate corneal deturgescence in the recovery period following DSO.10 Investigations on in vitro models suggest that ROCK inhibitors, specifically ripasudil, may act by enhancing the pump and barrier functions of corneal endothelium.11 In our case, the patient's corneal edema progressively cleared throughout the recovery period so we did not trial a ROCK inhibitor. There are several reports of successful DSO without a ROCK inhibitor with sustained corneal clearance for several years.9,12,13 The efficacy of ROCK inhibitors in corneal edema and DSO remains under investigation.
4. Conclusions
This is the first case report of a successful DSO for the treatment of a Descemet's detachment and corneal edema following a complicated and eventually aborted MIGS procedure. When considering DSO, imaging of the peripheral corneal endothelium can help identify suitable candidates by revealing sufficient endothelial reserve, as in our case. While DMEK remains the gold standard procedure for corneal edema, there are advantages to DSO – most notably eliminating the risk of graft rejection and the need for prolonged topical corticosteroid. Whether corneal endothelial damage is due to intrinsic factors such as FECD or external factors such as surgery or trauma, DSO is becoming a suitable option for more patients.
Patient consent
This case report does not contain any personal information that could lead to the identification of the patient.
CRediT author statement
Nergis C. Khan: Data Curation, Writing. Charles C. Lin: Conceptualization, Data Curation, Visualization, Writing, Supervision.
Declaration of competing interest
The authors have no conflicts of interest to disclose.
Acknowledgements
All authors attest that they meet the current ICMJE criteria for Authorship.
Footnotes
This work is supported by Research to Prevent Blindness and NIH-National Eye Institute Grant P30-EY026877. The sponsors had no role in the design or conduct of this report.
References
- 1.Ong Tone S., Kocaba V., Böhm M., Wylegala A., White T.L., Jurkunas U.V. Fuchs endothelial corneal dystrophy: the vicious cycle of Fuchs pathogenesis. Prog Retin Eye Res. 2021;80 doi: 10.1016/j.preteyeres.2020.100863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Garcerant D., Hirnschall N., Toalster N., Zhu M., Wen L., Moloney G. Descemet's stripping without endothelial keratoplasty. Curr Opin Ophthalmol. 2019;30(4):275–285. doi: 10.1097/ICU.0000000000000579. [DOI] [PubMed] [Google Scholar]
- 3.Hirabayashi K.E., Mark D., Lau J., Lin C.C. Descemet stripping only for a chronic Descemet detachment after cataract surgery. Cornea. 2020;39(3):379–381. doi: 10.1097/ICO.0000000000002195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang M.J., Kane S., Dhaliwal D.K. Descemetorhexis without endothelial keratoplasty versus DMEK for treatment of Fuchs endothelial corneal dystrophy. Cornea. 2018;37(12):1479–1483. doi: 10.1097/ICO.0000000000001742. [DOI] [PubMed] [Google Scholar]
- 5.Spiteri N., Hirnschall N., van Bysterveldt K., et al. Impact of TCF4 repeat number on resolution of corneal edema after Descemet's stripping only in Fuchs dystrophy: a pilot study. Vis Basel Switz. 2021;5(4):47. doi: 10.3390/vision5040047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang X., Chen Y., Yu G., Dang G. Spontaneous resolution of recurrent Descemet's membrane detachment after trabeculectomy: a case report. Am J Ophthalmol Case Rep. 2022;25 doi: 10.1016/j.ajoc.2022.101276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pan J.C.H., Au Eong K.G., A Eong K.G. Spontaneous resolution of corneal oedema after inadvertent “descemetorhexis” during cataract surgery. Clin Exp Ophthalmol. 2006;34(9):896–897. doi: 10.1111/j.1442-9071.2006.01360.x. [DOI] [PubMed] [Google Scholar]
- 8.Franceschino A., Dutheil F., Pereira B., Watson S.L., Chiambaretta F., Navel V. Descemetorhexis without endothelial keratoplasty in Fuchs endothelial corneal dystrophy: a systematic review and meta-analysis. Cornea. 2021 doi: 10.1097/ICO.0000000000002855. Published online December 8. [DOI] [PubMed] [Google Scholar]
- 9.Borkar D.S., Veldman P., Colby K.A. Treatment of Fuchs endothelial dystrophy by Descemet stripping without endothelial keratoplasty. Cornea. 2016;35(10):1267–1273. doi: 10.1097/ICO.0000000000000915. [DOI] [PubMed] [Google Scholar]
- 10.Moloney G., Garcerant Congote D., Hirnschall N., et al. Descemet stripping only supplemented with topical ripasudil for Fuchs endothelial dystrophy 12-month outcomes of the sydney eye hospital study. Cornea. 2021;40(3):320–326. doi: 10.1097/ICO.0000000000002437. [DOI] [PubMed] [Google Scholar]
- 11.Colby K. Descemet stripping only for Fuchs endothelial corneal dystrophy: will it become the gold standard? Cornea. 2022;41(3):269–271. doi: 10.1097/ICO.0000000000002796. [DOI] [PubMed] [Google Scholar]
- 12.Iovieno A., Moramarco A., Fontana L. Descemet stripping only in Fuchs' endothelial dystrophy without use of topical Rho-kinase inhibitors: 5-year follow-up. J Can Ophtalmol. 2021;17:S0008–S4182. doi: 10.1016/j.jcjo.2021.06.010. Published online July. (21)00217-9. [DOI] [PubMed] [Google Scholar]
- 13.Artaechevarria Artieda J., Wells M., Devasahayam R.N., Moloney G. 5-Year outcomes of Descemet stripping only in Fuchs dystrophy. Cornea. 2020;39(8):1048–1051. doi: 10.1097/ICO.0000000000002270. [DOI] [PubMed] [Google Scholar]