Abstract
Purpose:
Prior cancer research is limited by inconsistencies in defining rurality. The purpose of this study was to describe the prevalence of cancer risk factors and cancer screening behaviors across various county-based rural classification codes, including measures reflecting a continuum, to inform our understanding of cancer disparities according to the extent of rurality.
Methods:
Using an ecological cross-sectional design, we examined differences in cancer risk factors and cancer screening behaviors from the Behavioral Risk Factor Surveillance System and National Health Interview Survey (2008–2013) across rural counties and between rural and urban counties using four rural-urban classification codes for counties and county-equivalents in 2013: U.S. Office of Management and Budget, National Center for Health Statistics, USDA Economic Research Service’s rural-urban continuum codes, and Urban Influence Codes.
Results:
Although a rural-to-urban gradient was not consistently evident across all classification codes, the prevalence of smoking, obesity, physical inactivity, and binge alcohol use increased (all ptrend<0.03), while colorectal, cervical and breast cancer screening decreased (all ptrend<0.001) with increasing rurality. Differences in the prevalence of risk factors and screening behaviors across rural areas were greater than differences between rural and urban counties for obesity (2.4% vs. 1.5%), physical activity (2.9% vs. 2.5%), binge alcohol use (3.4% vs. 0.4%), cervical cancer screening (6.8% vs. 4.0%), and colorectal cancer screening (4.4% vs. 3.8%).
Conclusions:
Rural cancer disparities persist across multiple rural-urban classification codes, with marked variation in cancer risk factors and screening evident within rural regions. Focusing only on a rural-urban dichotomy may not sufficiently capture subpopulations of rural residents at greater risk for cancer and cancer-related mortality.
Keywords: cancer screening, rural, obesity, physical activity, alcohol, smoking, risk factors, health disparities
Introduction
Effective strategies to modify cancer risk factors and increase cancer screening in under-resourced rural settings are needed. The incidence of many preventable cancers, including cancers related to smoking (e.g., lung and laryngeal cancers) and cancers that can be prevented by screening (i.e., colorectal and cervical cancers), are higher in America’s rural vs. urban regions.1–3 Moreover, improvements in cancer survival rates over the last several decades have not occurred equally across the United States (U.S.). 4 Indeed, rural cancer disparities are widening, as cancer death rates decreased more slowly from 2006 to 2016 in U.S. rural (−1.0% per year) versus urban (−1.6% per year) counties.1
Compared to urban residents, individuals residing in rural areas of the U.S. are more likely to die after a cancer diagnosis, and this is particularly evident for lung, oropharyngeal, kidney, colorectal, and cervical cancers.2 Underlying causes of rural cancer disparities are likely multifactorial and have been largely attributed to geographic isolation, distance, and lack of access to specialty healthcare and technologies in rural settings.5 These obstacles may limit access to cancer screening services, and thereby contribute to lower screening rates observed in rural populations.6–11 Moreover, differences in modifiable cancer risk factors (e.g., smoking, obesity, physical activity, and alcohol use)12–14 and social determinants of health (e.g., poverty, literacy, social support, educational attainment)15 may also contribute to poor cancer outcomes among persons residing in rural areas.
To effectively address rural disparities in cancer outcomes, researchers need to adequately categorize and measure rural populations.16 Yet, prior research has been hampered by inconsistent measures of rurality across studies, each with limitations, and there is no consensus regarding how to best define rural regions.7,17–21 In fact, over 15 definitions of rurality are currently used by federal programs in the U.S. 22 These classifications are typically defined at either the county- or census tract-level and are largely based on population size, population density, and proximity to urban centers.23 As such, current rural designations do not consider important compositional, collective and contextual characteristics of rural individuals and places that may affect health (e.g., sociodemographic factors, shared norms, and built environment).20,24 While rurality is multidimensional and thereby difficult to define and measure, research on rural disparities has typically relied on pragmatic classifications of rural areas using discrete threshold-based measures (e.g. Office of Management and Budget’s metro (urban)/nonmetro (rural) county-level differentiation).23 This dichotomization of rural vs. urban areas may also reflect the small rural sample size, which limits the ability to assess variation within rural regions.25
Reliance on the rural-urban dichotomy to examine disparities neglects the complexity of the rural to urban continuum and may fail to capture important variability within each of these entities. Indeed, investigating disparities according to the degree of rurality may be critical to elucidate the person-level and area-level drivers of rural cancer disparities and to strategically prioritize resources to address these disparities. Several classification schemes have been proposed to assess the degree of rurality of U.S. counties and county-equivalents, including the USDA Economic Research Services’ rural-urban continuum codes (RUCC), urban influence codes (UIC),26 and the National Center for Health Statistics (NCHS) codes. However, it is unclear how cancer risk factors and screening behaviors differ across these classification codes, which reflect a continuum, and how this differentiation contrasts with dichotomous rural-urban measures. Measurement limitations hamper data interpretation and create biased conclusions which may lead to inequitable distribution of resources and beneficial interventions to address disparities. Additionally, this ambiguity makes it difficult to compare findings across studies of rural cancer disparities when different definitions of rurality are used.
Given the elevated burden of cancer in rural regions1–3 and limited cancer research in rural settings,2 the National Cancer Institute and other federal offices have emphasized the importance of research to better characterize and address rural cancer disparities, including understanding how rural residence should be defined in cancer control research. While rural-urban cancer disparities have been described in prior studies, the degree to which rurality is associated with prevalence of cancer risk factors and screening behaviors is unclear. Moreover, it is uncertain whether observed disparities vary based on the rural classification codes used. Thus, the aim of this study was to describe the prevalence of cancer risk factors and cancer screening behaviors across various county-based rural classification codes, including measures reflecting a continuum, to inform our understanding of cancer disparities according to the extent of rurality.
Materials and Methods
Study population
We examined data on county-level rurality, cancer risk factors, and cancer screening behaviors from multiple public datasets. Here, we use the term “county” to refer to both counties and county-equivalent areas like boroughs in Alaska and parishes in Louisiana. All U.S. counties with information on selected cancer risk factors, and cancer screening utilization were considered for inclusion in this study. The Federal Information Processing Standard Publication (FIPS) county codes, census regions, and standard federal regions were obtained from the 2016 U.S. Census reference files.27 A total of 3,143 counties and county-equivalents in the 50 states and District of Columbia, excluding Puerto Rico were identified in 2016. Because of county code changes, information was missing on the majority of indicators for the following 7 counties; Clifton Forge County, VA; Dade, FL; Hoonah-Angoon Census Area, AK; Prince of Wales-Outer-Ketchikan Census Area, AK; South Boston City, VA; Wrangell-Petersburg Census Area, AK; and Yellowstone National Park, WY. Thus, these counties were excluded, leaving 3,135 counties included in this analysis. For analysis of smoking and cancer screening behaviors, analyses were limited to the 3,108 counties with this information available.
Measures of rurality
We examined four county-level rural classification codes for the most recent year available (2013): U.S. Office of Management and Budget (OMB), National Center for Health Statistics (NCHS),28 U.S. Department of Agriculture, Economic Research Service’s rural-urban continuum codes (RUCC), and Urban Influence Codes (UIC), as described in Supplementary Table 1. The rural classification codes evaluated in this study were selected because they were defined at the county-level; other federal rural designation codes defined at the census-tract level were not included. Briefly, the OMB codes define metropolitan (urban) areas as those containing one or more central counties with urbanized areas, and nonmetropolitan (rural) counties as those outside the boundaries of metropolitan areas. Inherent in the OMB definition of rural is the combination of open countryside, rural towns (clusters of dense population with fewer than 2,500 people), and urban clusters with populations ranging from 2,500 to 49,999.26
The remaining coding schemas (NCHS, RUCC and UIC) subdivide the OMB metropolitan and nonmetropolitan counties into multiple categories to reflect a continuum. These codes use lower values to indicate highly urbanized areas and higher values to represent highly rural areas. NCHS codes consist of a six-level urban-rural classification scheme, with codes 1–4 reflecting urban, and 5–6 indicating rural counties. The most urban NCHS category designates central counties of large metropolitan areas (1), followed by large fringe metro (2; suburbs), medium metro (3), small metro (4), micropolitan (5) and nonmetropolitan “noncore” counties (6). RUCC codes (also called Beale codes) categorize counties based on population size, degree of urbanization, and proximity to a metropolitan area, and range from 1–9 where 1–3 represent urban and 4–9 are rural counties. UIC codes represent a 12-level classification system, which was developed by researchers at the Economic Research Service of the United States Department of Agriculture to better describe characteristics of rural areas with consideration of adjacency.29 UICs subdivide the OMB metropolitan and nonmetropolitan categories into 2 metropolitan groups (based on population size of 1 million) and non-metropolitan categories (based on adjacency to metropolitan or micropolitan areas and whether they have their “own town” [incorporated city or town or Census Designated Place of at least 2,500 residents]). This categorization relies on the assumption, derived from central place theorem, that adjacency to a town confers economic integration through access to larger economic centers of information, communication, trade, and finance, which enable local economies to connect to national and international marketplaces.30 Finally, we assessed the percentage of the county’s population that is rural based on population data from the U.S. Census Bureau in 2010, across rural-urban classification codes.
Cancer risk factors and screening behaviors
We examined the county-level prevalence of the following modifiable cancer risk factors; smoking,31 obesity, 32–34 physical inactivity,35 alcohol consumption,36–38 and preventive cancer screening participation (breast, cervical and colorectal). County-level modeled estimates of smoking and cancer screening participation from 2008–2010 were obtained from the State Cancer Profiles website.39 Estimates reflected combined results from the Behavioral Risk Factor Surveillance System (BRFSS) and the National Health Interview Survey (NHIS), both sponsored by the Centers for Disease Control (CDC). BRFSS is a large ongoing telephone survey of U.S. households, and NHIS is a smaller survey conducted via in-person interviews. The model-based county-level estimates for prevalence correct for potential non-coverage bias and nonresponse in BRFSS and reduce the variability in the estimates due to small sample sizes.40–42
Smoking status was defined as the percent of current smokers among adults 18 years and older. Screening behaviors were defined based on categorizations reported by the State Cancer Profiles surveillance dataset.39 Consistent with a prior study with similar methodology, breast cancer screening was defined as the percentage of women ages 40 years and older who had a mammogram within 2 years; cervical cancer screening as the percentage of women 18 years and older who had a Pap smear in the past 3 years (based on screening guidelines at the time) and had not reported ever having a hysterectomy; and colorectal cancer screening as the percentage of adults ages 50 years and older who ever had colorectal endoscopy (colonoscopy or sigmoidoscopy).41 County-level estimates of obesity and physical inactivity in 2013 were obtained from BRFSS and from the U.S. Census Bureau’s Population Estimates Program,43 and were based on indirect model-dependent estimates using Bayesian multilevel modeling techniques. The percentage of adults aged 18 years or older who were obese (BMI of 30.0 or higher; weight in kg/height in m2) was derived from self-reported weight and height. Individuals were considered physically inactive if they answered “no” to the question, “During the past month, other than your regular job, did you participate in any physical activities or exercises such as running, calisthenics, golf, gardening, or walking for exercise?” Information on obesity and physical activity was missing for a single county (Bedford City, VA) in 2013; estimates from 2012 were used for this county. Alcohol use prevalence by U.S. county in 2012, including age-standardized estimates for any drinking and binge drinking, were ascertained from the Institute for Health Metrics and Evaluation (IHME), and were produced by applying small area models to the 2012 Behavioral Risk Factor Surveillance System (BRFSS) data. Any alcohol use was defined as adults reporting at least one drink of alcohol within the past 30 days, and binge drinking was defined as consumption of 5 or more drinks for men and 4 or more drinks for women on a single occasion in the past 30 days.
Statistical Analysis
Using an ecological cross-sectional study design, we examined the distribution of cancer risk factors, and cancer screening behaviors according to the rural-urban dichotomy (OMB codes) using a chi-square test. Mean differences in cancer risk factors across the rural-urban codes reflecting a continuum (NCHS, RUCC, UIC) were estimated using an analysis of variance (ANOVA) model. We used the ANOVA model to estimate the p-values for trend in cancer risk factor and screening behavior prevalence across the rural-urban codes reflecting a continuum.49 We calculated differences in prevalence of cancer risk factors and screening behaviors between rural-urban counties overall, and across rural counties for each of the rural-urban classification schemes. For each classification code reflecting a continuum (NCHS, RUCC, and UIC), we calculated the greatest difference in prevalence of cancer risk factors and screening behaviors across rural counties (NCHS codes 5 & 6; RUCC codes 4–9; and UIC codes 3–12) and compared differences across rural counties to prevalence differences between OMB-designated rural vs. urban counties overall. All analyses were conducted using STATA 13 software (StataCorp, 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LLC).
Results
Demographic Characteristics Across Rural-Urban Classification Codes
Overall, 1,976 (62.9%) U.S. counties included in this study were rural and 1,167 (37.1%) were urban according to the OMB rural-urban dichotomy in 2013. In OMB-designated urban counties, 39.2% of the population were considered rural, while 70.1% of the population in OMB-designated rural counties were considered rural based on population data from the U.S. Census Bureau. (Table 1). The percentage of the population considered rural increased incrementally across the NCHS urban-rural codes from 2.1% in the large central metro counties to 78.9% in the most rural noncore regions. While the percentage of the population considered rural generally increased with increasing rurality across the RUCC and UIC codes, the positive trend was not incremental. For example, 34.6% of the population in rural counties (RUCC 5) were considered rural, which is lower than the 45.6% of rural populations in counties considered urban (RUCC 3). According to the UIC codes, the percentage of rural population was higher across all rural counties compared to urban counties but did not increase incrementally with increasing rurality. Similar trends in population size across the rural-urban classification codes were observed, with incremental increases observed for the OMB and NCHS codes and non-incremental increases in population size observed with increasing rurality according to the RUCC and UIC codes.
Table 1:
Mean prevalence of county-level cancer risk factors among U.S. adults, across rural classification codes
| N | Obesity | Physical Inactivity | Smoking | Alcohol Use | Binge Alcohol Use | |
|---|---|---|---|---|---|---|
|
| ||||||
| OMB | ||||||
| Urban | 1164 | 30.1 (4.4) | 24.4 (5.0) | 22.9 (5.6) | 52.4 (10.7) | 17.7 (4.2) |
| Rural | 1971 | 31.6 (4.5) | 26.9 (5.1) | 26.4 (5.0) | 48.1 (11.9) | 18.1 (5.6) |
| pdiff<0.001 | pdiff<0.001 | pdiff<0.001 | pdiff<0.001 | pdiff=0.02 | ||
| NCHS | ||||||
| 1 | 67 | 26.2 (4.7) | 21.0 (4.4) | 17.9 (4.2) | 58.5 (6.0) | 19.0 (2.6) |
| 2 | 367 | 29.6 (4.4) | 23.9 (5.0) | 22.1 (5.9) | 54.7 (10.0) | 17.9 (3.9) |
| 3 | 373 | 30.7 (4.4) | 24.9 (4.9) | 23.4 (5.4) | 50.8 (10.6) | 17.2 (4.1) |
| 4 | 357 | 30.7 (4.0) | 24.9 (4.9) | 24.0 (5.0) | 50.6 (11.3) | 17.7 (4.7) |
| 5 | 641 | 31.5 (4.6) | 26.2 (5.5) | 25.3 (4.7) | 49.1 (11.4) | 17.8 (4.9) |
| 6 | 1330 | 31.6 (4.4) | 27.2 (4.9) | 26.9 (5.1) | 47.7 (12.1) | 18.3 (5.8) |
| ptrend<0.001 | ptrend<0.001 | ptrend<0.001 | ptrend<0.001 | ptrend<0.03 | ||
| RUCC | ||||||
| 1 | 430 | 29.1 (4.6) | 23.5 (5.0) | 21.5 (5.9) | 55.2 (9.6) | 18.1 (3.7) |
| 2 | 379 | 30.7 (4.4) | 24.9 (4.9) | 23.4 (5.3) | 51.0 (10.6) | 17.2 (4.1) |
| 3 | 355 | 30.8 (4.0) | 25.0 (4.9) | 24.0 (5.0) | 50.6 (11.3) | 17.7 (4.7) |
| 4 | 214 | 31.4 (4.5) | 25.7 (5.1) | 25.2 (4.1) | 50.6 (10.5) | 17.9 (4.5) |
| 5 | 92 | 31.0 (5.3) | 24.9 (5.6) | 24.4 (4.5) | 51.3 (11.0) | 18.8 (4.8) |
| 6 | 593 | 32.3 (4.1) | 27.8 (4.9) | 27.0 (4.5) | 46.4 (10.6) | 17.3 (4.9) |
| 7 | 433 | 31.2 (4.8) | 26.5 (5.5) | 26.4 (4.7) | 48.7 (12.6) | 18.3 (5.5) |
| 8 | 220 | 31.9 (4.5) | 27.7 (4.6) | 27.1 (5.1) | 46.0 (12.9) | 17.8 (6.7) |
| 9 | 419 | 30.9 (4.3) | 26.8 (4.6) | 26.2 (6.0) | 49.2 (12.6) | 19.4 (6.2) |
| ptrend<0.001 | ptrend<0.001 | ptrend<0.001 | ptrend<0.001 | ptrend<0.001 | ||
| UIC | ||||||
| 1 | 431 | 29.1 (4.6) | 23.5 (5.0) | 21.5 (5.9) | 55.2 (9.6) | 18.1 (3.7) |
| 2 | 734 | 30.7 (4.2) | 24.9 (4.9) | 23.7 (5.2) | 50.8 (10.9) | 17.4 (4.4) |
| 3 | 129 | 31.7 (4.3) | 26.4 (5.3) | 25.5 (4.3) | 49.5 (10.2) | 17.3 (3.9) |
| 4 | 149 | 31.6 (3.7) | 27.6 (4.3) | 26.8 (4.6) | 46.2 (9.3) | 16.6 (4.4) |
| 5 | 242 | 31.9 (4.5) | 26.3 (5.1) | 25.5 (4.7) | 48.5 (10.9) | 17.7 (5.0) |
| 6 | 344 | 32.6 (4.3) | 28.0 (4.9) | 27.2 (4.3) | 46.3 (11.4) | 17.5 (5.4) |
| 7 | 162 | 31.8 (4.4) | 27.8 (4.9) | 27.8 (4.9) | 46.3 (13.4) | 18.2 (6.8) |
| 8 | 269 | 31.2 (4.9) | 26.0 (5.9) | 25.1 (4.8) | 49.5 (12.3) | 18.3 (5.3) |
| 9 | 184 | 32.1 (4.0) | 27.9 (4.8) | 27.2 (4.6) | 46.3 (11.8) | 17.5 (5.5) |
| 10 | 187 | 31.2 (4.6) | 27.2 (5.0) | 26.0 (5.7) | 48.8 (13.0) | 19.3 (6.4) |
| 11 | 124 | 30.4 (4.7) | 25.2 (4.9) | 26.0 (5.0) | 51.6 (12.4) | 19.5 (5.4) |
| 12 | 180 | 30.2 (4.6) | 25.8 (4.4) | 26.5 (6.4) | 50.3 (12.5) | 20.0 (6.0) |
| ptrend<0.001 | ptrend<0.001 | ptrend<0.001 | ptrend<0.001 | ptrend<0.001 | ||
National Center for Health Statistics (NCHS): Urban (1–4) Rural (5–6). USDA Economic Research Services’ rural-urban continuum codes (RUCC): Urban (1–3) Rural (4–9). Urban Influence Codes (UIC): Urban (1–2) Rural (3–12).
Numbers reflect mean prevalence (standard deviations)
Cancer Risk Factors Across Rural-Urban Classification Codes
Rural vs. urban counties based on the OMB dichotomy had significantly higher prevalence of obesity (31.6% vs. 30.1%), physical inactivity (26.9% vs. 24.4%), and smoking (26.4% vs. 22.9%). While the prevalence of alcohol use was lower in rural compared to urban counties (48.1% vs. 52.4%), rural counties had a higher percentage of binge alcohol use (18.1% vs. 17.7%). Although observed rural-urban differences in cancer risk factors and screening behaviors in this study were statistically significant, the absolute rural-urban difference was somewhat small, ranging from 0.4% for binge alcohol use to 3.5% for smoking prevalence.
Across the rural classification codes reflecting a continuum, the prevalence of obesity, physical inactivity, and smoking increased (all ptrend<0.001) with increasing rurality; although a consistent rural-to-urban gradient was not evident across RUCC and UIC codes (Table 2). Trends of increasing obesity, physical inactivity, and smoking with increasing rurality were consistent across the NCHS codes with the largest differences observed between the most urban and the most rural counties. Interestingly, the prevalence of alcohol use overall tended to decline with increasing rurality across all classification codes (all ptrend<0.001), with the highest percentage of alcohol use in the most urban counties for NCHS category 1 (58.5%), RUCC category 1 (55.2%) and UIC category 1 (55.2%). Patterns of binge alcohol use varied across the rural classification codes. For example, the highest prevalence of binge alcohol use was observed in the most urban NCHS counties (19.0%), while according to both the RUCC and UIC codes, binge alcohol use was highest in the most rural counties (RUCC code 9=19.4%, UIC code 12 =20.0%).
Table 2:
Mean prevalence of county-level cancer screening among U.S. adults, across rural classification codes
| N | Breast Cancer Screening | Cervical Cancer Screening | Colorectal Cancer Screening | |
|---|---|---|---|---|
|
| ||||
| OMB | ||||
| Urban | 1164 | 69.8 (6.5) | 75.2 (5.4) | 58.5 (6.8) |
| Rural | 1971 | 66.5 (7.5) | 71.2 (5.9) | 54.7 (6.7) |
| pdiff<0.001 | pdiff<0.001 | pdiff<0.001 | ||
| NCHS | ||||
| 1 | 67 | 71.9 (5.4) | 77.9 (4.6) | 58.8 (7.4) |
| 2 | 367 | 70.9 (6.5) | 76.9 (5.0) | 59.9 (6.9) |
| 3 | 373 | 69.1 (6.3) | 74.4 (5.5) | 57.7 (6.8) |
| 4 | 357 | 68.8 (6.6) | 73.6 (5.2) | 57.8 (6.4) |
| 5 | 641 | 67.4 (6.2) | 73.0 (5.2) | 56.1 (5.9) |
| 6 | 1330 | 66.1 (8.0) | 70.3 (6.1) | 54.0 (6.9) |
| ptrend<0.001 | ptrend<0.001 | ptrend<0.001 | ||
| RUCC | ||||
| 1 | 430 | 71.1 (6.4) | 77.1 (4.9) | 59.8 (7.0) |
| 2 | 379 | 69.2 (6.3) | 74.5 (5.5) | 57.8 (6.8) |
| 3 | 355 | 68.7 (6.5) | 73.6 (5.2) | 57.8 (6.4) |
| 4 | 214 | 67.7 (5.2) | 73.8 (4.1) | 57.2 (5.2) |
| 5 | 92 | 68.2 (6.1) | 74.7 (4.6) | 57.2 (6.2) |
| 6 | 593 | 66.3 (6.5) | 72.0 (4.7) | 54.7 (5.8) |
| 7 | 433 | 66.8 (7.1) | 71.8 (5.3) | 54.7 (6.3) |
| 8 | 220 | 66.5 (8.0) | 69.7 (5.8) | 53.7 (7.0) |
| 9 | 419 | 65.4 (9.7) | 67.9 (7.5) | 53.3 (8.3) |
| ptrend<0.001 | ptrend<0.001 | ptrend<0.001 | ||
| UIC | ||||
| 1 | 431 | 71.1 (6.4) | 77.1 (4.9) | 59.8 (7.0) |
| 2 | 734 | 69.0 (6.4) | 74.1 (5.4) | 57.8 (6.6) |
| 3 | 129 | 68.1 (5.0) | 74.1 (3.8) | 57.2 (5.2) |
| 4 | 149 | 67.5 (6.8) | 72.1 (4.9) | 54.7 (5.7) |
| 5 | 242 | 67.0 (5.8) | 72.9 (4.5) | 55.8 (5.9) |
| 6 | 344 | 65.9 (6.5) | 71.4 (4.7) | 54.3 (5.9) |
| 7 | 162 | 65.9 (8.4) | 69.5 (6.1) | 53.8 (7.1) |
| 8 | 269 | 67.3 (6.9) | 72.5 (6.3) | 55.7 (6.2) |
| 9 | 184 | 66.0 (7.5) | 70.8 (5.1) | 53.6 (6.5) |
| 10 | 187 | 65.5 (9.0) | 68.7 (7.2) | 53.8 (7.7) |
| 11 | 124 | 66.9 (7.1) | 71.9 (5.4) | 55.1 (7.0) |
| 12 | 180 | 65.5 (10.8) | 67.6 (7.8) | 52.8 (8.9) |
| ptrend<0.001 | ptrend<0.001 | ptrend<0.001 | ||
National Center for Health Statistics (NCHS): Urban (1–4) Rural (5–6). USDA Economic Research Services’ rural-urban continuum codes (RUCC): Urban (1–3) Rural (4–9). Urban Influence Codes (UIC): Urban (1–2) Rural (3–12).
Numbers reflect mean prevalence (standard deviations)
Cancer Screening Across Rural-Urban Classification Codes
Results for cancer screening participation across rural classification codes are shown in Table 3. Prevalence of breast, cervical and colorectal cancer screening were lower in OMB-designated rural vs. urban counties (all pdiff<0.001) overall, with the largest rural-urban difference observed for cervical cancer and the lowest screening prevalence for colorectal cancer. Colorectal, cervical, and breast cancer screening also decreased (all ptrend<0.001) with increasing rurality across all classification codes. However, a consistent rural-to-urban gradient was only observed for breast and cervical cancer screening using the NCHS codes. Breast cancer screening prevalence was highest in the most urban counties (71.9% NCHS category 1, 71.1% RUCC category 1, and 71.1% UIC category 1) and lowest in the most rural counties (66.1% NCHS category 6, 65.4% RUCC category 9, and 65.5% UIC category 12) across the rural classification codes. Likewise, cervical cancer screening prevalence was also highest in the most urban counties (77.9% NCHS category 1, 77.1% RUCC category 1, and 77.1% UIC category 1) and lowest in the most rural counties (70.3% NCHS code 6, 67.9% RUCC code 9, and 67.6% UIC category 12). Prevalence of colorectal cancer screening was highest in the most urban counties according to both the RUCC and UIC codes, and lowest in the most rural counties across all codes (54.0% NCHS category 6, 53.3% RUCC category 9, and 52.8% UIC category 12).
Rural-Urban and Within Rural Differences in Cancer Risk Factors and Screening
As shown in Figure 1a, overall rural vs. urban differences in cancer risk factors based on the OMB dichotomy were greatest for alcohol use (48.1% vs. 52.4%; difference = 4.3%), followed by smoking (26.4% vs. 22.9%; difference=3.5%), physical inactivity (26.9% vs. 24.4%; difference=2.5%), obesity (31.6% vs. 30.1%; difference=1.5%), and binge alcohol use (18.1% vs. 17.7%; difference=0.4%). Observed variation in the prevalence of cancer risk factors was also evident within rural regions and across classification codes. Indeed, differences in the prevalence of cancer risk factors across rural-designated counties were greater than differences between rural and urban counties overall for obesity, physical activity, and binge alcohol use. For example, prevalence of physical inactivity was 2.5% higher in OMB-designated rural vs. urban counties overall, while physical inactivity prevalence was 2.9% higher in rural counties with RUCC of 6 (27.8%) vs. RUCC of 5 (24.9%). Greater differences in risk factors across rural regions were observed using the RUCC and UIC codes compared to the NCHS codes. As shown in Figure 1b, rural-urban differences in cancer screening were similar across cancer sites (3.3% lower for breast, 4.0% lower for cervical, and 3.8% lower for colorectal in rural vs. urban counties). Differences in screening across rural counties using both the RUCC and UIC codes were greater than rural-urban differences overall for cervical (6.8%) and colorectal cancer screening (4.4%), but similar to rural-urban differences for breast cancer screening. Both the RUCC and UIC codes were better suited to differentiate cancer risk factors and screening behaviors across rural counties, given the larger number of categories for rural counties compared to the NCHS codes which largely reflect urban county differentiation.
Figure 1a:
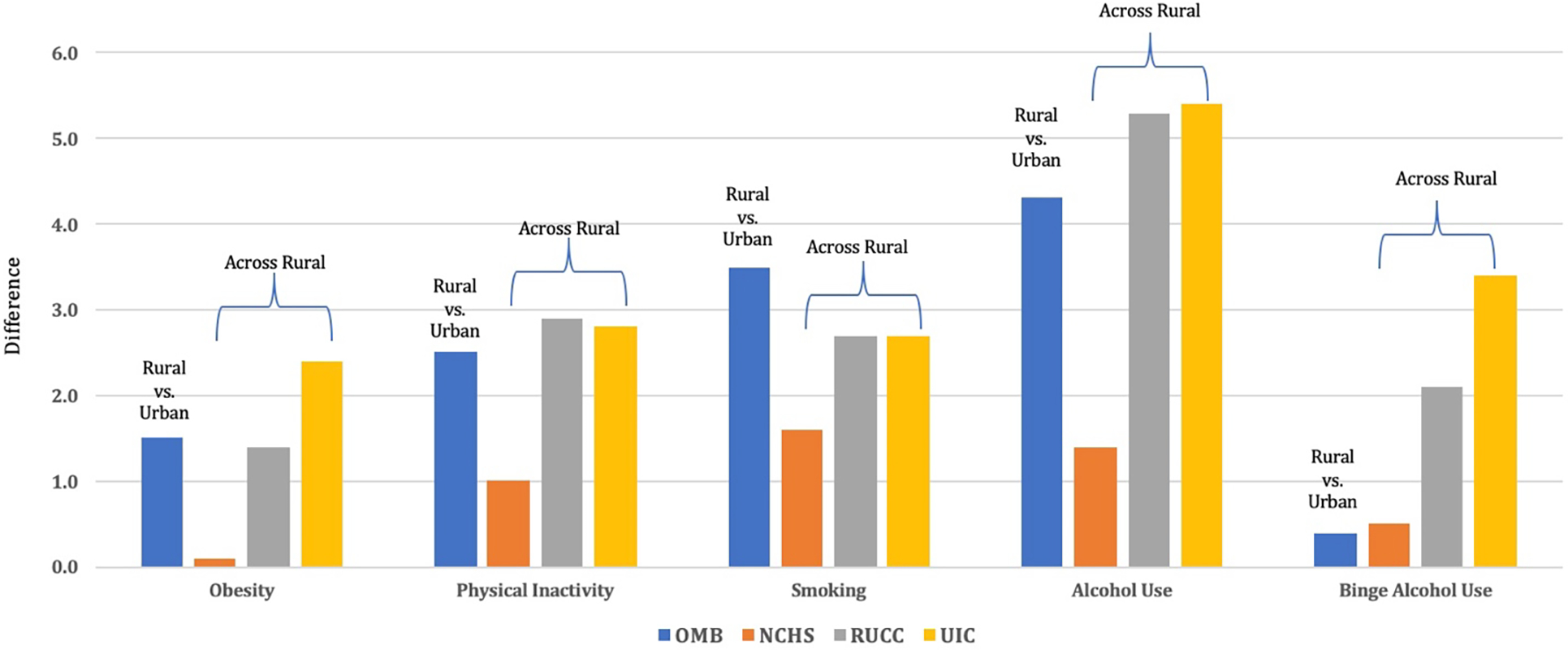
Differences in county-level cancer risk factors among U.S. adults between rural and urban counties and across rural counties
OMB=U.S. Office of Management and Budget codes, NCHS=National Center for Health Statistics, RUCC=USDA Economic Research Service’s rural-urban continuum codes, UIC=Urban Influence Codes
Figure 1b:
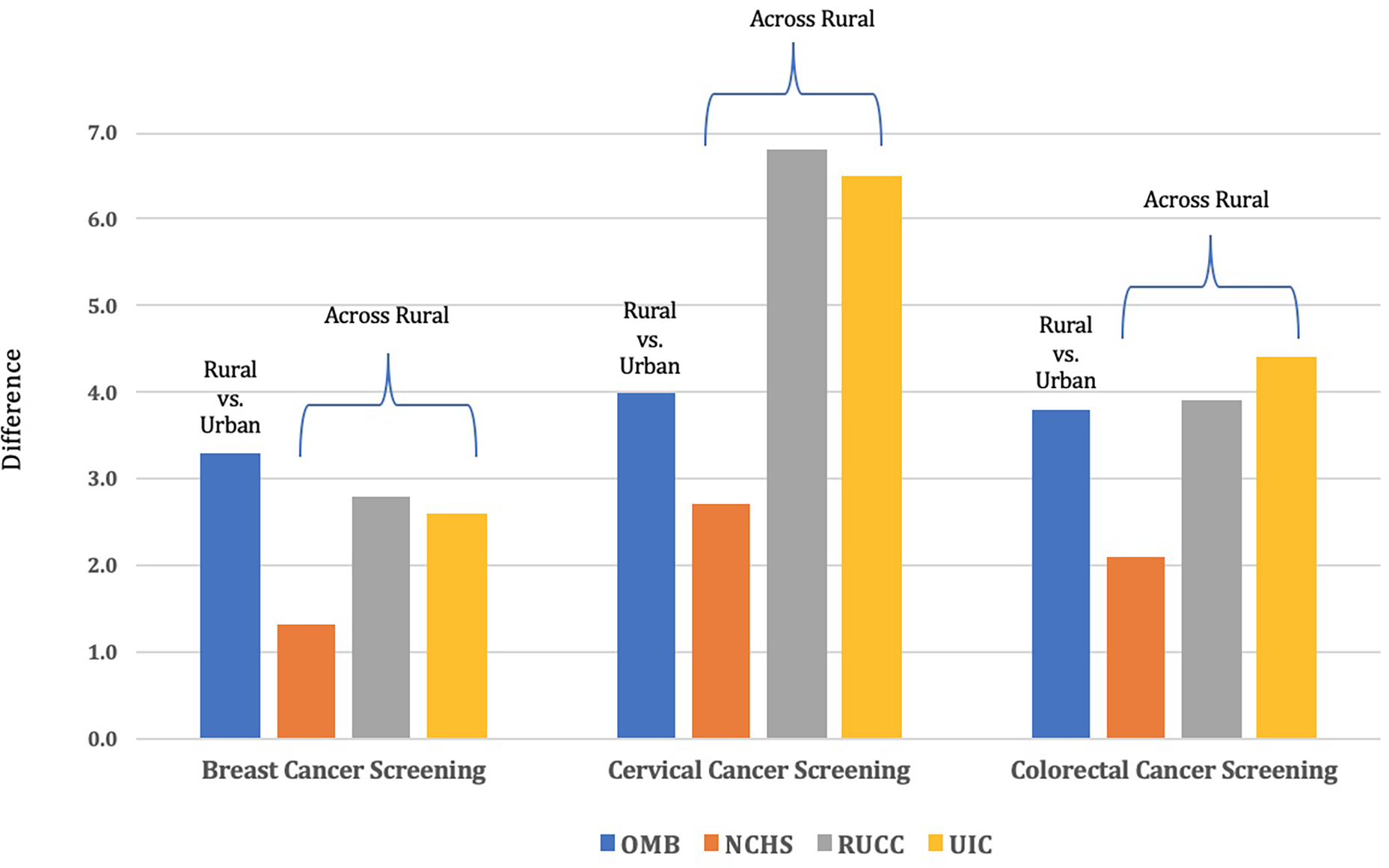
Differences in county-level cancer screening among U.S. adults between rural and urban counties and across rural counties
OMB=U.S. Office of Management and Budget codes, NCHS=National Center for Health Statistics, RUCC=USDA Economic Research Service’s rural-urban continuum codes, UIC=Urban Influence Codes
Discussion
In this large ecologic study, disparities in cancer risk factors and screening behaviors persisted across all county-level rural-urban classification codes evaluated. However, a rural-to-urban gradient in cancer risk factors and screening with increasing rurality was not evident across all classification codes. Moreover, differences in certain cancer risk factors (obesity, physical inactivity, alcohol use, and binge alcohol use) and cancer screening (cervical and colorectal) were greater across rural counties (using both RUCC and UIC codes) than between OMB-designated rural and urban counties overall. Both the RUCC and UIC codes were better suited to differentiate cancer risk factors and screening behaviors across rural counties, given the larger number of categories for rural counties compared to the NCHS codes which largely reflect urban county differentiation.
Results from this study align with findings from prior studies focusing on rural-urban comparisons, with higher prevalence of obesity,32,50 physical inactivity,51 smoking,52 and binge alcohol consumption,53 and lower prevalence of breast, cervical and colorectal cancer screening 6–11 observed in U.S. rural vs. urban settings. Differences in rural-urban prevalence of cancer risk factors and screening were largest for smoking (higher in rural vs. urban), overall alcohol use (lower in rural vs. urban), and for both cervical and colorectal cancer screening (lower in rural vs. urban). Findings from this study extend current knowledge by describing cancer risk factors and screening behaviors across multiple measures of rurality. The rural-urban codes evaluated in this study reflect a continuum and more finely represented differences in cancer risk factors across the rural-urban landscape, with larger differences observed between the most rural and most urban counties, most notably using the NCHS codes for cancer risk factors and breast cancer screening, and the UIC codes for cervical and colorectal cancer screening. These findings are consistent with results from prior studies examining health measures across rurality codes, suggesting that rural-urban status is both a continuum and multidimensional and that distinct elements of rural-urban status may influence health in nuanced ways.19,54
In this study, we observed larger differences in the prevalence of obesity, physical inactivity, binge alcohol use, and cervical and colorectal cancer screening across rural counties than differences observed between rural and urban counties overall. Thus, focusing on a rural-urban dichotomy may fail to identify subpopulations of rural residents at greater risk for certain cancer and cancer-related mortality within rural settings. This heterogeneity should be considered in future research to inform the development of targeted policies and strategies to address rural cancer disparities. While the National Cancer Institute advocates for use of the RUCC codes, much of the recently published cancer research utilizing RUCC continues to dichotomize the RUCC scale into rural and urban categories,55–58 ignoring potential variation within both rural and urban settings. Indeed, the dichotomization of a rural-urban transition is the prevailing paradigm in cancer disparities research, and may contribute to imprecise measurement and mixed findings in the literature.59 The reliance on the rural-urban dichotomy to characterize rural cancer disparities masks variability within the continuum and assumes that cancer risk behaviors follow a step function where the risk within groups is homogenous, leading to statistical power loss and inaccurate and unstable estimation.60–62 Results from this study suggest that cancer risk factors and screening behaviors do not necessarily follow a consistent stepwise change across the rural to urban continuum. Thus, policy implications based on crude categorization of rural and urban regions can lead to potentially inappropriate and imprecise provision of services. However, methodological challenges related to small sample size in categories reflecting a rural-urban continuum often limit the ability to produce stable estimates, particularly for rural settings with a small overall population size. Indeed, small sample sizes often preclude use of rigorous statistical methods,63 including multivariable analyses to characterize the multi-level factors contributing to rural health disparities. Innovative statistical methodologies to address analytic issues related to small samples, with particular emphasis on addressing health disparities in small population groups are needed.64
While the purpose of this study was not necessarily to identify an ideal coding scheme, our results can provide insights to guide future research focused on rural cancer disparities. Overall, disparities in cancer risk factors and screening behaviors persisted across all county-level rural-urban classification codes evaluated in this study. Importantly, the degree of differentiation of rural counties varies across classification codes, with the NCHS codes only including 2 categorizations of rural counties, while the RUCC and UIC codes divide rural counties into 6 and 10 categories, respectively. Therefore, both the RUCC and UIC codes are potentially better suited to differentiate cancer risk factors and screening behaviors across rural counties, given the larger number of categories for rural counties compared to the NCHS codes, which largely reflect urban county differentiation. Importantly, rural classification codes defined at the county-level do not account for marked variability within counties with regard to population size, population density, and proximity to urban centers.23 Thus, research to effectively address rural cancer disparities may need to target specific geographic regions and populations within rural counties, including consideration of rural census tracts within metro counties. Future studies are needed to compare the differentiation power of multiple rural-urban classification coding schemes to inform recommendations and ensure consistencies of rural-urban definitions in future research. Nonetheless, our findings suggest that the specific research question should be used to guide the choice of rural-urban classification designation in future studies.
Strengths of this study include the large sample size, including nearly all U.S. counties. An additional study strength was the characterization of disparities both within and across rural and urban settings. While our analysis focused on commonly used county-level indicators that are simple to understand, have boundaries that are relatively stable over time, and can be linked to national health datasets, there are limitations to this approach. For example, county size varies substantially across the U.S. with some counties covering large geographic regions, which include both very urbanized and very rural areas. Indeed, 30 million Census Bureau-defined rural residents live in OMB-defined urban areas and 20 million urban residents live in rural areas. Thus, use of county-level rural-urban designations ignores potential within-county variation. Likewise, the reliance on county-level data in this study introduces the potential for ecologic bias, whereby individual-level differences in cancer risk factors and screening behaviors are inferred based on aggregate county-level data. Further, observed differences in the prevalence of cancer risk factors and cancer screening participation in this study might not be clinically relevant. Finally, this analysis was purely descriptive and we were unable to account for other contributing factors fueling observed disparities, including differences in access to care, healthcare shortage areas, travel barriers, and other factors that may impact cancer prevention, screening, diagnosis, and treatment. Future studies are needed to assess the relative contribution of access to care and social determinants to observed rural cancer disparities, including use of the social vulnerability index to inform a more nuanced understanding of cancer disparities in the rural context.65
In conclusion, rural disparities in cancer risk factors and screening persist across multiple county-level rural-urban classification codes, with marked variation apparent across rural regions. Thus, focusing only on a rural-urban dichotomy may not sufficiently capture subpopulations of rural residents at greater risk for cancer and cancer-related mortality. Observed differences in cancer risk factors across rural counties speak to the need for using measures that better differentiate sub-populations within rural counties, including the RUCC and UIC codes. These findings advance our understanding of the causes of rural cancer disparities, adding precision and nuance to the narrative of a dichotomous rural-urban disparity and informing future targeted interventions.
Supplementary Material
Acknowledgements
The authors assume full responsibility for analyses and interpretation of these data. Dr. Nemeth is funded by National Cancer Institute career development grant 1K07CA216321-01A1.
No funding was received to assist with the preparation of this manuscript. Dr. Nemeth is funded by NCI career development grant 1K07CA216321-01A1.
Footnotes
Compliance with Ethical Standards
The authors declare no potential conflicts of interest
The authors have no relevant financial or non-financial interests to disclose
All authors contributed to the study conception and design. Material preparation and data collection were performed by Kelly A. Hirko. Data analyses were performed by Huiwen Xu. The first draft of the manuscript was written by Kelly A. Hirko and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript and assume full responsibility for analyses and interpretation of these data.
The datasets analyzed during the current study are available in the State Cancer Profiles website, https://statecancerprofiles.cancer.gov/
Ethics approval
This is an observational descriptive study using publicly available county-level data. The Michigan State University Institutional Review Board has confirmed that no ethical approval is required.
References
- 1.Henley SJ, Anderson RN, Thomas CC, Massetti GM, Peaker B, Richardson LC. Invasive Cancer Incidence, 2004–2013, and Deaths, 2006–2015, in Nonmetropolitan and Metropolitan Counties - United States. Morb Mortal Wkly Rep Surveill Summ Wash DC 2002 2017;66:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blake KD, Moss JL, Gaysynsky A, Srinivasan S, Croyle RT. Making the Case for Investment in Rural Cancer Control: An Analysis of Rural Cancer Incidence, Mortality, and Funding Trends. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol 2017;26:992–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zahnd WE, James AS, Jenkins WD, Izadi SR, Fogleman AJ, Steward DE, Colditz GA, Brard L. Rural-Urban Differences in Cancer Incidence and Trends in the United States. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol 2018;27:1265–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin 2020;70:7–30. [DOI] [PubMed] [Google Scholar]
- 5.Charlton M, Schlichting J, Chioreso C, Ward M, Vikas P. Challenges of Rural Cancer Care in the United States. Oncol Williston Park N 2015;29:633–40. [PubMed] [Google Scholar]
- 6.Agency for Healthcare Research and Quality. 2014 national healthcare quality and disparities report chartbook on rural health care. AHRQ Pub. No. 15–0007-9-EF [Internet]. 2015;Available from: https://www.ahrq.gov/research/findings/nhqrdr/2014chartbooks/ruralhealth/index.htmlexternalicon
- 7.Meilleur A, Subramanian SV, Plascak JJ, Fisher JL, Paskett ED, Lamont EB. Rural residence and cancer outcomes in the United States: issues and challenges. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol 2013;22:1657–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bennett KJ, Probst JC, Bellinger JD. Receipt of cancer screening services: surprising results for some rural minorities. J Rural Health Off J Am Rural Health Assoc Natl Rural Health Care Assoc 2012;28:63–72. [DOI] [PubMed] [Google Scholar]
- 9.Nuño T, Gerald JK, Harris R, Martinez ME, Estrada A, García F. Comparison of breast and cervical cancer screening utilization among rural and urban Hispanic and American Indian women in the Southwestern United States. Cancer Causes Control CCC 2012;23:1333–41. [DOI] [PubMed] [Google Scholar]
- 10.Fan L, Mohile S, Zhang N, Fiscella K, Noyes K. Self-reported cancer screening among elderly Medicare beneficiaries: a rural-urban comparison. J Rural Health Off J Am Rural Health Assoc Natl Rural Health Care Assoc 2012;28:312–9. [DOI] [PubMed] [Google Scholar]
- 11.Doescher MP, Jackson JE. Trends in cervical and breast cancer screening practices among women in rural and urban areas of the United States. J Public Health Manag Pract JPHMP 2009;15:200–9. [DOI] [PubMed] [Google Scholar]
- 12.Colditz GA, Wolin KY, Gehlert S. Applying what we know to accelerate cancer prevention. Sci Transl Med 2012;4:127rv4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garcia MC, Faul M, Massetti G, Thomas CC, Hong Y, Bauer UE, Iademarco MF. Reducing Potentially Excess Deaths from the Five Leading Causes of Death in the Rural United States. Morb Mortal Wkly Rep Surveill Summ Wash DC 2002 2017;66:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Matthews KA, Croft JB, Liu Y, Lu H, Kanny D, Wheaton AG, Cunningham TJ, Khan LK, Caraballo RS, Holt JB, Eke PI, Giles WH. Health-Related Behaviors by Urban-Rural County Classification - United States, 2013. Morb Mortal Wkly Rep Surveill Summ Wash DC 2002 2017;66:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bolin JN, Bellamy GR, Ferdinand AO, Vuong AM, Kash BA, Schulze A, Helduser JW. Rural Healthy People 2020: New Decade, Same Challenges. J Rural Health Off J Am Rural Health Assoc Natl Rural Health Care Assoc 2015;31:326–33. [DOI] [PubMed] [Google Scholar]
- 16.Brawley OW. Cancer Disparities: The Scope of the Problem and Possible Solutions. In: Cancer Disparities. 2011. [Google Scholar]
- 17.Woods Michael. Conceptualizing Rural Areas in Metropolitan Society: A Rural View. 2015;
- 18.Bennett KJ, Borders TF, Holmes GM, Kozhimannil KB, Ziller E. What Is Rural? Challenges And Implications Of Definitions That Inadequately Encompass Rural People And Places. Health Aff Proj Hope 2019;38:1985–92. [DOI] [PubMed] [Google Scholar]
- 19.Long JC, Delamater PL, Holmes GM. Which Definition of Rurality Should I Use?: The Relative Performance of 8 Federal Rural Definitions in Identifying Rural-Urban Disparities. Med Care 2021;59:S413–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zahnd WE, Mueller-Luckey GS, Fogleman AJ, Jenkins WD. Rurality and Health in the United States: Do Our Measures and Methods Capture Our Intent? J Health Care Poor Underserved 2019;30:70–9. [DOI] [PubMed] [Google Scholar]
- 21.Hart LG, Larson EH, Lishner DM. Rural definitions for health policy and research. Am J Public Health 2005;95:1149–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coburn AF, MacKinney AC, McBride TD, Mueller KJ, Slifkin RT, Wakefield MK. Choosing rural definitions: implications for health policy. [Internet]. 2007;Available from: Issue Brief 2:1–8 [Google Scholar]
- 23.Waldorff B, Kim A. Defining and Measuring Rurality in the US: From Typologies to Continuous Indices. 2015; [Google Scholar]
- 24.Macintyre S, Ellaway A, Cummins S. Place effects on health: how can we conceptualise, operationalise and measure them? Soc Sci Med 2002;55:125–39. [DOI] [PubMed] [Google Scholar]
- 25.Zahnd WE, Askelson N, Vanderpool RC, Stradtman L, Edward J, Farris PE, Petermann V, Eberth JM. Challenges of using nationally representative, population-based surveys to assess rural cancer disparities. Prev Med 2019;129S:105812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cromartie John. Historical Development of ERS Rural-Urban Classification Systems [Internet]. Available from: https://sites.nationalacademies.org/cs/groups/dbassesite/documents/webpage/dbasse_169814.pdf
- 27.U.S. Census. 2016. U.S. Census reference files [Internet]. Available from: https://www.census.gov/geographies/reference-files/2016/demo/popest/2016-fips.html
- 28.Ingram DD, Franco SJ. 2013 NCHS urban-rural classification scheme for counties. 2014; [PubMed]
- 29.Baer LD, Johnson-Webb KD, Gesler WM. What is rural? A focus on urban influence codes. J Rural Health Off J Am Rural Health Assoc Natl Rural Health Care Assoc 1997;13:329–33. [DOI] [PubMed] [Google Scholar]
- 30.Economic Research Service USDA. ERS/USDA Urban Influence Codes Documentation [Internet]. 2003;Available from: https://www.ers.usda.gov/data-products/urban-influence-codes/documentation/
- 31.U.S. Department of Health and Human Services. The Health Consequences of Smoking - 50 Years of Progress: A Report of the Surgeon General. 2014;
- 32.Befort CA, Nazir N, Perri MG. Prevalence of obesity among adults from rural and urban areas of the United States: findings from NHANES (2005–2008). J Rural Health Off J Am Rural Health Assoc Natl Rural Health Care Assoc 2012;28:392–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Davis AM, Bennett KJ, Befort C, Nollen N. Obesity and related health behaviors among urban and rural children in the United States: data from the National Health And Nutrition Examination Survey 2003–2004 and 2005–2006. J Pediatr Psychol 2011;36:669–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Johnson JA, Johnson AM. Urban-rural differences in childhood and adolescent obesity in the United States: a systematic review and meta-analysis. Child Obes Print 2015;11:233–41. [DOI] [PubMed] [Google Scholar]
- 35.Patterson PD, Moore CG, Probst JC, Shinogle JA. Obesity and physical inactivity in rural America. J Rural Health Off J Am Rural Health Assoc Natl Rural Health Care Assoc 2004;20:151–9. [DOI] [PubMed] [Google Scholar]
- 36.Gfroerer JC, Larson SL, Colliver JD. Drug use patterns and trends in rural communities. J Rural Health Off J Am Rural Health Assoc Natl Rural Health Care Assoc 2007;23 Suppl:10–5. [DOI] [PubMed] [Google Scholar]
- 37.Borders TF, Booth BM. Rural, suburban, and urban variations in alcohol consumption in the United States: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. J Rural Health Off J Am Rural Health Assoc Natl Rural Health Care Assoc 2007;23:314–21. [DOI] [PubMed] [Google Scholar]
- 38.Jackson JE, Doescher MP, Hart LG. Problem drinking: rural and urban trends in America, 1995/1997 to 2003. Prev Med 2006;43:122–4. [DOI] [PubMed] [Google Scholar]
- 39.National Cancer Institute, Centers for Disease Control. State Cancer Profiles [Internet]. [[cited 2021 Dec 13];Available from: https://statecancerprofiles.cancer.gov/
- 40.Raghunathan TE, Dawei X, Schenker N, Parsons VL, Davis WW, Dodd KW, Feuer EJ. Combining information from two surveys to estimate county-level prevalence rates of cancer risk factors and screening. Journal of the American statistical association 2007;102. [Google Scholar]
- 41.Liu B, Parsons V, Feuer EJ, Pan Q, Town M, Raghunathan TE, Schenker N, Xie D. Small Area Estimation of Cancer Risk Factors and Screening Behaviors in US Counties by Combining Two Large National Health Surveys. Prev Chronic Dis 2019;16:E119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.National Cancer Institute. Small Area Estimates for Cancer-Related Measures [Internet]. Available from: sae.cancer.gov
- 43.U.S. Census Bureau’s Population Estimates Program (https://www.cdc.gov/diabetes/data/countydata/countydataindicators.html).
- 44.Rao JNK. Small Area Estimation. Hoboken, New Jersey: John Wiley & Sons, Inc, 2003. [Google Scholar]
- 45.Cadwell BL, Thompson TJ, Boyle JP, Barker LE. Bayesian small area estimates of diabetes prevalence by U.S. county, 2005. J Data Sci 8:173–88. [PMC free article] [PubMed] [Google Scholar]
- 46.Barker LE, Thompson TJ, Kirtland KA, Boyle JP, Geiss LS, McCauley MM, Albright AL. Bayesian Small Area Estimates of Diabetes Incidence by United States County, 2009. J Data Sci JDS 2013;11:269–80. [PMC free article] [PubMed] [Google Scholar]
- 47.Institute for Health Metrics and Evaluation. United States Alcohol Use Prevalence by County 2002–2012. 2015;
- 48.Dwyer-Lindgren L, Flaxman AD, Ng M, Hansen GM, Murray CJL, Mokdad AH. Drinking Patterns in US Counties From 2002 to 2012. Am J Public Health 2015;105:1120–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Park C, Hsiung JT, Soohoo M, Streja E. Choosing Wisely: Using the Appropriate Statistical Test for Trend in SAS [Internet]. [[cited 2022 Apr 25];Available from: https://www.lexjansen.com/wuss/2019/175_Final_Paper_PDF.pdf
- 50.Lundeen EA, Park S, Pan L, O’Toole T, Matthews K, Blanck HM. Obesity Prevalence Among Adults Living in Metropolitan and Nonmetropolitan Counties - United States, 2016. MMWR Morb Mortal Wkly Rep 2018;67:653–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Whitfield GP, Carlson SA, Ussery EN, Fulton JE, Galuska DA, Petersen R. Trends in Meeting Physical Activity Guidelines Among Urban and Rural Dwelling Adults - United States, 2008–2017. MMWR Morb Mortal Wkly Rep 2019;68:513–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Doogan NJ, Roberts ME, Wewers ME, Stanton CA, Keith DR, Gaalema DE, Kurti AN, Redner R, Cepeda-Benito A, Bunn JY, Lopez AA, Higgins ST. A growing geographic disparity: Rural and urban cigarette smoking trends in the United States. Prev Med 2017;104:79–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dixon MA, Chartier KG. Alcohol Use Patterns Among Urban and Rural Residents: Demographic and Social Influences. Alcohol Res Curr Rev 2016;38:69–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cohen SA, Cook SK, Sando TA, Sabik NJ. What Aspects of Rural Life Contribute to Rural-Urban Health Disparities in Older Adults? Evidence From a National Survey. J Rural Health Off J Am Rural Health Assoc Natl Rural Health Care Assoc 2018;34:293–303. [DOI] [PubMed] [Google Scholar]
- 55.Shete S, Deng Y, Shannon J, Faseru B, Middleton D, Iachan R, Bernardo B, Balkrishnan R, Kim SJ, Huang B, Millar MM, Fuemmler B, et al. Differences in Breast and Colorectal Cancer Screening Adherence Among Women Residing in Urban and Rural Communities in the United States. JAMA Netw Open 2021;4:e2128000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lutgendorf SK, Ramirez E, Schrepf A, Valentine MC, Charlton M, Zimmerman MB, Goodheart MJ, Zia S, Sood AK, Thaker PH. Rural residence is related to shorter survival in epithelial ovarian cancer patients. Gynecol Oncol 2021;163:22–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Thomson MD, Williams AR, Sutton AL, Tossas KY, Garrett C, Sheppard VB. Engaging rural communities in cancer prevention and control research: Development and preliminary insights from a community-based research registry. Cancer Med 2021;10:7726–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Johnson KJ, Wang X, Barnes JM, Delavar A. Associations between geographic residence and US adolescent and young adult cancer stage and survival. Cancer 2021;127:3640–50. [DOI] [PubMed] [Google Scholar]
- 59.Yaghjyan L, Cogle CR, Deng G, Yang J, Jackson P, Hardt N, Hall J, Mao L. Continuous Rural-Urban Coding for Cancer Disparity Studies: Is It Appropriate for Statistical Analysis? Int J Environ Res Public Health 2019;16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bennette C, Vickers A. Against quantiles: categorization of continuous variables in epidemiologic research, and its discontents. BMC Med Res Methodol 2012;12:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hall SA, Kaufman JS, Ricketts TC. Defining urban and rural areas in U.S. epidemiologic studies. J Urban Health Bull N Y Acad Med 2006;83:162–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cossman RE, Cossman JS, Cosby AG, Reavis RM. Reconsidering the Rural-Urban Continuum in Rural Health Research: A Test of Stable Relationships Using Mortality as a Health Measure. Popul Res Policy Rev 2008;27:459–76. [Google Scholar]
- 63.Kenny DA, Mannetti L, Pierro A, Livi S, Kashy DA. The statistical analysis of data from small groups. J Pers Soc Psychol 2002;83:126–37. [PubMed] [Google Scholar]
- 64.Fok CCT, Henry D, Allen J. Maybe Small Is Too Small a Term: Introduction to Advancing Small Sample Prevention Science. Prev Sci Off J Soc Prev Res 2015;16:943–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry/Geospatial Research Analysis, and Services Program. CDC/ATSDR Social Vulnerability Index 2020 [Internet]. 2020. [[cited 2022 Feb 2];Available from: https://www.atsdr.cdc.gov/placeandhealth/svi/data_documentation_download.html#:~:text=Our%20suggested%20citation%20for%20use,%5BInsert%20US%20or%20State%5D.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


