Abstract
Introduction
Caffeine has long been vilified as a cause for urinary urgency incontinence (UUI) along with other potential bladder irritants such as carbonation, alcohol, and acidic juices. The objective of this study was to assess the fluid intake behavior of people with urgency, UUI, and those with lower urinary tract symptoms (LUTS) without UUI or urgency to assess if they avoided certain potential bladder irritants or had different fluid intake. We hypothesized that patients with UUI would avoid caffeine as a self‐management method more so than these other two groups.
Methods
Treatment‐seeking men and women with LUTS in the Symptoms of Lower Urinary Tract Dysfunction Research Network (LURN) Observational Cohort study completed a baseline 3‐day voiding and intake diary. “Complete” diaries had 3 days of data and no missing intake or voided volumes. Beverages with any caffeine, alcohol, carbonation, or acidic juice were identified and the total volume was recorded as well as the type of beverage containing caffeine to calculate the daily caffeine dose.
Results
Four hundred and ninety‐one participants (277 men and 214 women) with a median age of 63 had complete diaries. Urinary urgency was more prevalent in women than men (79% vs. 55%, p < 0.0001) as was UUI (84% vs. 47%, p < 0.0001). Total fluid intake over 3 days was lower among the urgency group versus the nonurgency group (median [interquartile range] 5.2 [4.0–6.8] L vs. 5.7 [4.3–7.0] L, p = 0.028) and the UUI group compared to the urgency without incontinence group were less likely to consume alcohol (26% vs. 37%, p = 0.04).
After adjusting for sex, BMI, age, and total intake volume, UUI participants had 54% lower odds of consuming any caffeine (odds ratio = 0.46, 95% confidence interval = 0.22–0.96, p = 0.04) than those without incontinence, but among those that did consume caffeine, no difference in the volume of caffeinated beverages or milligrams of caffeine consumed was detected between those with UUI and those with urgency without incontinence. No difference in carbonation or acidic juice intake was detected between groups.
Conclusions
Individuals with urgency consume a lower volume of fluid than those without urgency. UUI participants more often abstain from caffeine, but among those that consume caffeine, the dose is similar to those without UUI. One explanation for these results is that only a subset of individuals with urgency or UUI are caffeine sensitive.
Keywords: caffeine, fluid intake, urgency, urgency incontinence, voiding diary
1. INTRODUCTION
Caffeine and other dietary irritants have long been blamed as the cause of urinary urgency, frequency, and urgency incontinence. Providers have been giving the same advice to patients for decades, recommending fluid reduction, avoidance of alcohol, carbonated beverages, acidic drinks, and caffeinated beverages as a means of treating these urinary symptoms. However, it is unknown if this advice is effective in reducing lower urinary tract symptoms (LUTS). In addition, it is not clear whether all individuals are similarly sensitive to the urinary effects of these fluid choices or if there is an acceptable amount of consumption that does not affect LUTS for some. There is also the added burden to patients who may perceive themselves as failing behavioral therapy if they cannot comply with these instructions, resulting in discontinuation of care. Our prior systematic review of the literature on the impact of consumed substances on LUTS revealed mostly observational data of variable quality. 1 Fluid intake and caffeine were implicated in worsening frequency and urgency and modest alcohol intake was associated with a decrease in the diagnosis of benign prostatic hyperplasia. Hence, these beverages were specifically included in this analysis along with carbonated beverages and acidic juices since these are often included in patient instructions to improve LUTS. 2
The Symptoms of Lower Urinary Tract Dysfunction Research Network (LURN) Observational Cohort study participants completed a 3‐day voiding and fluid type/volume diary providing substantial, real‐world data on beverage consumption. We hypothesized that many patients would avoid caffeine and alcohol to control their symptoms as well as decreasing fluid intake since all participants were treatment‐seeking and had received care from a urologist or urogynecologist before study entry.
2. METHODS AND MATERIALS
2.1. Study design and population
The LURN completed a 1‐year prospective observational study that enrolled men and women seeking treatments for LUTS at six US tertiary care sites. The LURN study design has been previously reported. 3 Briefly, participants were required to be at least 18 years old and present to a LURN physician with at least one LUTS reported at moderate or greater severity, as assessed by the LUTS Tool using a 1‐month recall period. 4
2.2. Measures
The following data were collected during each participant's baseline study visit; demographic and medical history, including comorbidities, medication, and treatment history; a variety of patient‐reported symptoms; and physical exam data. This study used the LUTS Tool questionnaire, which is a 44‐item questionnaire assessing severity and bother of LUTS over the previous week to classify participants into urgency and urinary urgency incontinence (UUI) categories. Participants were classified as having urgency if they reported “sometimes” or greater in response to “having a feeling of a sudden rush to urinate.” Patients were further classified as having UUI if they also reported “sometimes” or greater in response to “leaking with a sudden rush to urinate.”
Bladder diaries, using a modified version of the International Consultation on Incontinence Questionnaire (ICIQ), were also collected from all participants as part of their baseline visit. 5 Participants were instructed to record beverage intake and voided volume over a course of 3 days. They also were instructed to include the timing of the intakes and voids, the type and volumes of beverages consumed, any bladder sensations at the time of voiding (e.g., none, normal, urgency), pad changes, and any incontinence episodes (“stress” or “urge” or “unknown”). Reports were also made on the time participants went to bed and woke up for the day. An assessment of the feasibility, reliability, and quality of these bladder diaries has been previously reported. 6
A systematic review of all beverage data was performed by LURN investigators, to identify potentially irritating beverages (PIBs). Beverages reported on participant bladder diaries were classified into categories of caffeinated, alcoholic, carbonated, and acidic beverages. The first two were included due to reports in prior publications, and the latter two because they are often included in patient instructions to improve LUTS. 7 Beverages noted as having caffeine were reviewed and estimates of caffeine levels were recorded. Beverages noted as having alcohol were reviewed and estimates of the total alcohol intake, in standard drinks (12 oz beer, 5 oz wine, 1.5 oz liquor are all classified as one standard drink) were recorded. Beverage consumption was coded as any use across the 3‐day diary, in addition to total volumes consumed across the 3 days, and total amount of caffeine and irritating beverages consumed across the 3 days. 7
2.3. Statistical methods
Data are reported as median and interquartile range (IQR) for continuous measures, and frequencies and percentages for categorical data. Statistical comparisons were made between urgency and nonurgency and UUI and urgency with no incontinence groups using the Wilcoxon Rank Sum test for continuous measures or χ 2 test for categorical measures.
Logistic regression models were used to test associations between group membership and the use of any caffeine, alcohol, carbonation, or acidic beverages. Linear regression models were used to assess differences between urgency groups and UUI groups for the volume of PIBs consumed and milligrams of caffeine consumed across the 3‐day diaries. Unadjusted and multivariable models were fitted, with the latter adjusting for participant sex, BMI, age, and total intake volume across the 3 days. All statistical analyses were completed using SAS 9.4.
3. RESULTS
The LURN Observational Cohort Study enrolled 1064 participants (519 men and 545 women). Among these participants, 162 did not complete a bladder diary. Among the 902 diaries that were submitted, 106 were excluded as unusable due to large amounts of missing data. An additional 295 diaries were deemed incomplete due to missing intake or voided volumes. An additional 11 participants were excluded from the urgency analyses for missing urgency data and 41 were excluded from the UUI analyses for missing either urgency or UUI data. This resulted in a total of 491 participants being included in analyses reporting on differences across urgency groups and 315 participants being included in analyses reporting on differences across UUI groups (Figure 1).
Figure 1.

STROBE diagram of participant inclusion
3.1. Urgency versus nonurgency comparisons
Four hundred and ninety‐one participants (277 men and 214 women) were included in the urgency analyses. The urgency group (n = 321) in comparison with the nonurgency group (n = 170) had a higher proportion of females (52% vs. 27%, p < 0.0001), a slightly higher BMI (median 29 vs. 28, p = 0.042), but was similar in age and race distributions. Total fluid intake over 3 days was lower among the urgency group compared to the nonurgency group (5.2 vs. 5.7 L, p = 0.028) as was the frequency of alcohol consumption (30% vs. 43%, p = 0.004) (Table 1).
Table 1.
Demographics, potential bladder irritants, and fluid intake on 3‐day intake and voiding diary
| N (%) or median [IQR] | Urgency | No urgency | p Value | UUI | UU | p Value |
|---|---|---|---|---|---|---|
| N = 321 | N = 170 | N = 210 | N = 105 | |||
| Gender | <0.001 | <0.001 | ||||
| Males | 153 (48%) | 124 (73%) | 71 (34%) | 79 (75%) | ||
| Females | 168 (52%) | 46 (27%) | 139 (66%) | 26 (24%) | ||
| Age | 63 [53–70] | 63 [52–70] | 0.778 | 63 [52–70] | 63 [53–70] | 0.975 |
| BMI | 29 [26–34] | 28 [25–31] | 0.042 | 30 [26–35] | 27 [25–31] | 0.003 |
| Race | 0.136 | 0.086 | ||||
| Black | 35 (11%) | 10 (6%) | 29 (14%) | 6 (6%) | ||
| White | 262 (82%) | 143 (84%) | 166 (79%) | 89 (85%) | ||
| Other race | 24 (7%) | 17 (10%) | 15 (7%) | 10 (10%) | ||
| Any caffeinea | 260 (81%) | 142 (84%) | 0.446 | 166 (79%) | 92 (88%) | 0.063 |
| Any alcohola | 95 (30%) | 72 (43%) | 0.004 | 54 (26%) | 39 (37%) | 0.036 |
| Any carbonationa | 181 (57%) | 95 (56%) | 0.941 | 116 (55%) | 60 (57%) | 0.748 |
| Any acidic juicea | 64 (20%) | 31 (18%) | 0.660 | 45 (21%) | 18 (17%) | 0.370 |
| Caffeine volume (L) a , b | 1.7 [0.9–2.4] | 1.6 [1.0–2.3] | 0.548 | 1.6 [0.9–2.6] | 1.7 [1.0–2.3] | 0.577 |
| Alcohol volume (L) a , b | 0.7 [0.4–1.3] | 0.6 [0.3–1.4] | 0.570 | 0.5 [0.4–1.1] | 0.9 [0.5–1.5] | 0.030 |
| Carbonation volume (L) a , b | 1.1 [0.4–1.8] | 0.9 [0.5–1.8] | 0.631 | 1.0 [0.4–1.8] | 1.1 [0.5–1.8] | 0.766 |
| Acidic juice volume (L) a , b | 0.5 [0.2–0.8] | 0.4 [0.3–0.7] | 0.750 | 0.5 [0.2–0.8] | 0.5 [0.2–0.7] | 0.636 |
| Total intake volume (L)a | 5.2 [4.0–6.8] | 5.7 [4.3–7.0] | 0.028 | 5.0 [4.0–6.4] | 5.5 [3.8–7.1] | 0.091 |
| Total amount of caffeine (mg) a , b | 400 [250–600] | 400 [250–600] | 0.567 | 400 [250–600] | 425 [220–650] | 0.666 |
| Total amount of alcohol (standard drinks) a , b | 3.6 [1.5–6.5] | 4.0 [1.7–7.8] | 0.979 | 3.5 [2.0–6.0] | 5.8 [2.0–8.3] | 0.178 |
Abbreviations: IQR, interquartile range; UU, urinary urgency; UUI, urinary urgency incontinence.
Across 3 days of completed bladder diaries.
Among those consuming that type of beverage.
After adjusting for sex, BMI, age, and total intake volume, urgency patients had a trend toward 32% lower odds of consuming any alcohol (odds ratio [OR] [95% confidence interval (CI)] = 0.68 (0.45, 1.03), p = 0.07), but among those that did consume alcohol, no difference was detected in the volume of alcohol consumed or the number of standard alcoholic drinks consumed (0.7 vs. 0.6 L, p = 0.57 and 3.6 drinks vs. 4.0 drinks, p = 0.98 across 3‐day diary, in urgency vs. nonurgency participants, respectively). In adjusted models, there was no difference detected between these groups in the consumption of any caffeine, carbonation, or acidic beverage consumption (Figure 2, Supporting Information: Table 1).
Figure 2.
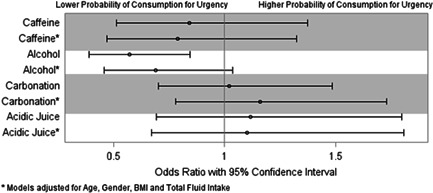
Urgency comparison for potentially irritating beverages
3.2. UUI versus urgency without incontinence comparison
Three hundred and fifteen participants (150 men and 165 women) were included in the UUI analysis. The UUI group (n = 210) in comparison with the urgency without incontinence group (n = 105) also had a higher proportion of females (66% vs. 24%, p < 0.0001) and a higher BMI (median 30 vs. 27, p < 0.0001), but was similar in age and race distributions. The frequency of alcohol consumption was lower among the UUI group compared to the urgency without incontinence group (26% vs. 37%, p = 0.04) and total volume intake trended toward lower (5.0 vs. 5.5 L, p = 0.09) (Table 1).
After adjusting for sex, BMI, age, and total intake volume, UUI participants had 54% lower odds of consuming any caffeine (OR [95% CI] = 0.46 (0.22, 0.96), p = 0.04), but among those that did consume caffeine, no difference was detected in the volume of caffeinated beverages consumed (1.6 vs. 1.7 L across 3 days in UUI vs. urgency without incontinence participants respectively, p = 0.58). There was also no difference detected in the milligrams of caffeine consumed (400 vs. 425 mg across 3 days in UUI vs. non‐UUI participants respectively, p = 0.62). Similar trends were reported for alcohol consumption, but the results were not statistically significant. No difference was found in the intake of carbonated beverages or acidic beverage consumption across either the unadjusted or adjusted models (Figure 3, Supporting Information: Table 2).
Figure 3.
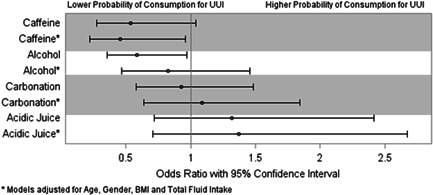
Urgency incontinence comparison for potentially irritating beverages
4. DISCUSSION
Among a large group of participants with various LUTS, those with urgency consumed a smaller volume of fluids daily compared to those without urgency. Those with urgency were more likely to abstain from alcohol consumption and those with UUI were more likely to abstain from caffeine, but in both cases, among those that did consume alcohol or caffeine, the daily consumption was no different between groups. After adjusting for total fluid volume intake, there were no differences in consumption between bladder symptom groups seen for carbonated beverages or acidic beverages suggesting these are not bladder irritants in a LUTS population without substantial bladder pain.
The benefits of increased water intake are sometimes exaggerated in the lay press and even by some health care providers. The literature is quite clear that other than for patients with urinary stone disease, there are no health benefits of overhydration and that patients with overactive bladder syndrome (OAB) have symptoms worsen when excess fluid is consumed. 8 In this study, these patients have likely noted worsening of their symptoms and have reduced their fluid intake accordingly to have more urinary symptom control. A person's daily volume of consumed fluids is an obvious predictor of the number of voids per day given that an individual's bladder volume is finite. This has been consistently seen in several studies on manipulating daily fluid intake. Decreasing daily fluid intake in a randomized trial including 30 women with urodynamic proven detrusor overactivity and OAB significantly reduced frequency, urgency, and incontinence. 9 In another OAB study of 67 men and women, decreasing fluid intake by 25% had a substantial impact on urgency, frequency, and nocturia, but greater reduction was not achievable by these patients even for only 4 days. 10 Other studies have also found it was very difficult to get people to eliminate PIBs from their diet. 11 In this study, the reduction in fluid intake for patients with UUI or urgency compared to those without these symptoms was modest with 500–233 ml less consumed fluids per day and was likely reduced over time which is likely why this was achievable. Advising to reduce fluid intake, particularly in those patients who overconsume fluids would be beneficial.
The results in this study that total mean caffeine intake was not different between those patients with UUI or urgency and those without was surprising, but closer analysis of the data revealed that a substantial number of patients with UUI abstain from caffeine completely. The results in randomized trials and other observational studies have yielded conflicting results with respect to caffeine. In some randomized trials, there was no change in symptoms when caffeinated beverages were replaced with decaffeinated substitutes, others have noted earlier urgency on urodynamics after consuming caffeinated water compared to the same study performed after drinking plain water. 9 , 12
In the Boston Area Community Health (BACH) Cohort (n = 4144) from 2002 to 2010, beverage intake was not associated with American Urological Association Symptom Index (AUASI) total score progression, but urgency alone was more likely to increase in those women drinking two or more cups of coffee a day compared to those who abstained, with a similar trend in men with all storage symptoms progressing in coffee drinkers. Total caffeine daily dose from all sources did not predict progression in women but did so in men. 13
In a study of 203 female university students, those with at least one episode of urgency per day consumed half a serving more of coffee per day and one more serving of bladder irritants daily than those without. The incontinence rate in this young population was only 1.4%. There was no difference in total caffeine intake or total fluid intake between the OAB and non‐OAB groups, and these were not a care seeking population. In addition, caffeine reduction may not have been deemed useful by these women to only improve minor urgency. 14 Advice for a trial without caffeine for patients with urgency or UUI to assess if their symptoms are sensitive to caffeine or not with the information that they can return to caffeine consumption if they do not respond would be beneficial.
Alcohol intake showed a similar trend to caffeine in that the total volume of alcohol consumed was not different between the patients with urgency compared to those without, but patients with urgency were more likely to completely abstain from alcohol. The data on alcohol intake and urgency and UUI are mixed in the literature. In the BACH Survey, intake amounts and symptoms were inconsistent with only a few groups having statistically significant associations between alcohol intake and OAB. 15 , 16 One interview study noted an increased odds of having urgency and frequency among current consumers of alcohol compared to nondrinkers, but other studies have not found any association with alcohol intake and UUI. 1 , 16 A trial without alcohol consumption would potentially be beneficial to assess the effects on urgency.
The intake of artificial sweeteners, citrus beverages, and carbonated beverages that were not caffeinated was not different between groups. There is sparse evidence in the literature that these have little to no impact on bladder symptoms and may actually be beneficial. 13 Of note, the LURN participants did not have interstitial cystitis/bladder pain syndrome as this was an exclusion criterion for the study and may only be an irritant in this specific condition. Advising patients with urgency and UUI to abstain from these beverages does not appear to be warranted. Advice for all patients with UUI or urgency, particularly those who overconsume fluids, should be to modestly reduce fluid intake. These same patients can undertake a trial of caffeine and alcohol avoidance and assess the benefit to their urinary symptoms since perhaps not all will be sensitive to these particular beverages.
This study has some limitations. This was an observational study of care‐seeking LUTS patients who all have access to bladder information from many sources including their medical provider, the lay press, family, and friends as well as any possible research they have undertaken into their condition. It is unknown if changes in fluid/irritant intake were undertaken as a result of the clinical visit or may have been a lifestyle change made before study entry. Also, given the observational nature of the study, it is unknown if these patients would be more symptomatic if they reintroduced fluids, caffeine, and alcohol or if they are simply avoiding the beverages based on the advice given. Also, some people avoid caffeine because of other health issues such as gastrointestinal upset, nervousness, sleeplessness, or cardiac irritability which may have nothing to do with their bladder but were not assessed in this study.
Although caffeine intake tends to be daily, alcohol intake is often more sporadic occurring at different volumes on weekends versus weekdays, hence a 3‐day voiding diary may not have reflected a person average intake. Alcohol is not typically contained in food, but caffeine is, and this study did not account for solid food intake of caffeine. Caffeine intake in the US population is however estimated to be 98% derived from fluids and not food sources. 17 The comparison groups for urgency and urgency incontinence patients were other participants who had LUTS hence there is not a control group without LUTS. Our conclusions are also based on the assumption that people may alter their behavior based on suggestion for fluid intake from providers, but if they tried a change and it had no effect, they would go back to their regular consumption.
5. CONCLUSION
In a large cohort of patients with LUTS, those with urgency consume a lower volume of fluids daily compared to those without urgency. Patients with urgency were more likely to abstain from alcohol, but among those that did consume alcohol, the volume was not different than those who did not have urgency. Patients with UUI are more likely to completely avoid caffeine than those without UUI, but those that did consume caffeine did not alter the amount consumed. Possible theories for this finding that deserve future study are that only a certain subset of people with UUI are caffeine sensitive.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Supporting information
Supporting information.
ACKNOWLEDGMENTS
The following individuals were instrumental in the planning and conduct of this study at each of the participating institutions: Duke University, Durham, North Carolina (DK097780): PIs: Cindy Amundsen, MD, Eric Jelovsek, MD; Co‐Is: Kathryn Flynn, PhD, Jim Hokanson, PhD, Aaron Lentz, MD, David Page, PhD, Nazema Siddiqui, MD, Kevin Weinfurt, PhD, Lisa Wruck, PhD; Study Coordinators: Paige Green, Magaly Guerrero. University of Iowa, Iowa City, IA (DK097772): PIs: Catherine S Bradley, MD, MSCE, Karl Kreder, MD, MBA; Co‐Is: Bradley A. Erickson, MD, MS, Daniel Fick, MD, Vince Magnotta, PhD, Philip Polgreen, MD, MPH; Study Coordinators: Sarah Heady, Chelsea Poesch, Shelly Melton, Jean Walshire. Northwestern University, Chicago, IL (DK097779): PIs: James W. Griffith, PhD, Kimberly Kenton, MD, MS, Brian Helfand, MD, PhD; Co‐Is: Carol Bretschneider, MD, David Cella, PhD, Sarah Collins, MD, Julia Geynisman‐Tan, MD, Alex Glaser, MD, Christina Lewicky‐Gaupp, MD, Margaret Mueller, MD, Devin Boehm; Study Coordinators: Sylwia Clarke, Melissa Marquez, Malgorzata Antoniak, Pooja Talaty, Francesca Moroni, Sophia Kallas. Dr. Helfand and Ms. Talaty are at NorthShore University Health System. University of Michigan Health System, Ann Arbor, MI (DK099932): PI: J. Quentin Clemens, MD, FACS, MSCI; Co‐Is: John DeLancey, MD, Dee Fenner, MD, Rick Harris, MD, Steve Harte, PhD, Anne P. Cameron, MD, Aruna Sarma, PhD, Giulia Lane, MD; Study Coordinators: Linda Drnek, Marissa Moore, Greg Mowatt, Sarah Richardson, Julia Chilimigras, Diana O'Dell. University of Washington, Seattle Washington (DK100011): PI: Claire Yang, MD; Co‐I: Anna Kirby, MD; Study Coordinators: Brenda Vicars, RN, Lauren Daniels. Washington University in St. Louis, St. Louis Missouri (DK100017): PI: H. Henry Lai, MD; Co‐Is: Gerald L. Andriole, MD, Joshua Shimony, MD, PhD, Fuhai Li, PhD; Study Coordinators: Linda Black, Vivien Gardner, Patricia Hayden, Diana Wolff, Aleksandra Klim, RN, MHS, CCRC. Arbor Research Collaborative for Health, Data Coordinating Center (DK099879): PI: Robert Merion, MD, FACS; Co‐Is: Victor Andreev, PhD, DSc, Brenda Gillespie, PhD, Abigail Smith, PhD; Project Manager: Melissa Fava, MPA, PMP; Clinical Monitor: Melissa Sexton, BA, CCRP; Research Analysts: Margaret Helmuth, MA, Jon Wiseman, MS, Jane Liu, MPH, Sarah Mansfield, MS. National Institute of Diabetes and Digestive and Kidney Diseases, Division of Kidney, Urology, and Hematology, Bethesda, MD: Project Scientist: Ziya Kirkali MD; Project Officer: Christopher Mullins PhD; Project Advisor: Julie Barthold, MD. Shauna Leighton, Medical Editor with Arbor Research Collaborative for Health, provided editorial assistance on this manuscript. This is publication number 34 of the Symptoms of Lower Urinary Tract Dysfunction Research Network (LURN). This study is supported by the National Institute of Diabetes & Digestive & Kidney Diseases through cooperative agreements (grants DK097780, DK097772, DK097779, DK099932, DK100011, DK100017, DK099879). Research reported in this publication was supported at Northwestern University, in part, by the National Institutes of Health's National Center for Advancing Translational Sciences, Grant Number UL1TR001422. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Cameron AP, Helmuth ME, Smith AR, et al. Total fluid intake, caffeine, and other bladder irritant avoidance among adults having urinary urgency with and without urgency incontinence: the Symptoms of Lower Urinary Tract Dysfunction Research Network (LURN). Neurourol Urodyn. 2023;42:213‐220. 10.1002/nau.25070
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- 1. Bradley CS, Erickson BA, Messersmith EE, et al. Evidence of the impact of diet, fluid intake, caffeine, alcohol and tobacco on lower urinary tract symptoms: a systematic review. J Urol. 2017;198:1010‐1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction . For Patients Overactive Bladder CCP. (sufuorg.com). Accessed December 10, 2021. https://sufuorg.com/resources/patients.aspx
- 3. Cameron AP, Lewicky‐Gaupp C, Smith AR, et al. Baseline lower urinary tract symptoms in patients enrolled in LURN: a prospective, observational cohort study. J Urol. 2018;199:1023‐1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Coyne KS, Barsdorf AI, Thompson C, et al. Moving towards a comprehensive assessment of lower urinary tract symptoms (LUTS). Neurourol Urodyn. 2012;31:448‐454. [DOI] [PubMed] [Google Scholar]
- 5. Bright E, Cotterill N, Drake M, Abrams P. Developing and validating the International Consultation on Incontinence Questionnaire bladder diary. Eur Urol. 2014;66(2):294‐300. 10.1016/j.eururo.2014.02.057 [DOI] [PubMed] [Google Scholar]
- 6. Cameron AP, Wiseman JB, Smith AR, et al. Are three‐day voiding diaries feasible and reliable? Results from the Symptoms of Lower Urinary Tract Dysfunction Research Network (LURN) cohort. Neurourol Urodyn. 2019;38:2185‐2193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. U.S. Department of Agriculture Agricultural Research Service . Food Data Central. Accessed December 1, 2021. https://fdc.nal.usda.gov/
- 8. Wood LN, Markowitz MA, Parameshwar PS, et al. Is it safe to reduce water intake in the overactive bladder population? A systematic review. J Urol. 2018;200:375‐381. [DOI] [PubMed] [Google Scholar]
- 9. Swithinbank L, Hashim H, Abrams P. The effect of fluid intake on urinary symptoms in women. J Urol. 2005;174:187‐189. [DOI] [PubMed] [Google Scholar]
- 10. Hashim H, Abrams P. How should patients with an overactive bladder manipulate their fluid intake? BJU Int. 2008;102:62‐66. [DOI] [PubMed] [Google Scholar]
- 11. Miller JM, Garcia CE, Hortsch SB, Guo Y, Schimpf MO. Does instruction to eliminate coffee, tea, alcohol, carbonated, and artificially sweetened beverages improve lower urinary tract symptoms? A prospective trial. J Wound Ostomy Continence Nurs. 2016;43:69‐79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lohsiriwat S, Hirunsai M, Chaiyaprasithi B. Effect of caffeine on bladder function in patients with overactive bladder symptoms. Urol Ann. 2011;3:14‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Maserejian NN, Wager CG, Giovannucci EL, Curto TM, McVary KT, McKinlay JB. Intake of caffeinated, carbonated, or citrus beverage types and development of lower urinary tract symptoms in men and women. Am J Epidemiol. 2013;177:1399‐1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Reisch R, Rutt R, Dockter M, Sanders S. Overactive bladder symptoms in female health profession students: bladder diary characteristics and impact of symptoms on health‐related quality of life. J Womens Health (Larchmt). 2018;27:156‐161. [DOI] [PubMed] [Google Scholar]
- 15. Kupelian V, Wei JT, O'leary MP, et al. Prevalence of lower urinary tract symptoms and effect on quality of life in a racially and ethnically diverse random sample: the Boston Area Community Health (BACH) Survey. Arch Intern Med. 2006;166:2381‐2387. [DOI] [PubMed] [Google Scholar]
- 16. Ikeda Y, Nakagawa H, Ohmori‐Matsuda K, et al. Risk factors for overactive bladder in the elderly population: a community‐based study with face‐to‐face interview. Int J Urol. 2011;18:212‐218. [DOI] [PubMed] [Google Scholar]
- 17. Fulgoni VL 3rd, Keast DR, Lieberman HR. Trends in intake and sources of caffeine in the diets of US adults: 2001–2010. Am J Clin Nutr. 2015;101:1081‐1087. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


