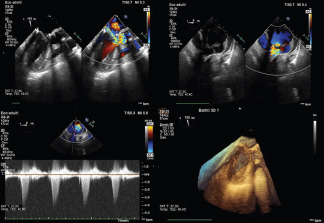
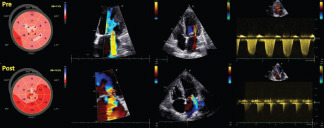
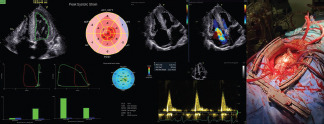
Introduction: Atrial functional mitral regurgitation (AFMR) remains poorly defined clinically. Aim: To compare clinical, echocardiographic characteristics and outcomes of severe AFMR to primary mitral regurgitation (PMR) after mitral valve annuloplasty (MVA) via right minithoracotomy approach (RMA)
Methods: Consecutive patients, who underwent MVA by RMA at our institution between 2016 and 2021 for severe mitral regurgitation with preserved left ventricular function, were screened. We excluded endocarditis, cardiomyopathy, prior mitral intervention. The absence of leaflet pathology defined AFMR. Outcomes included death and heart failure hospitalizations (HFH)
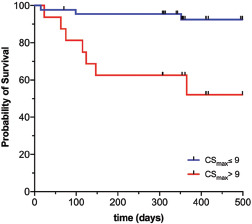
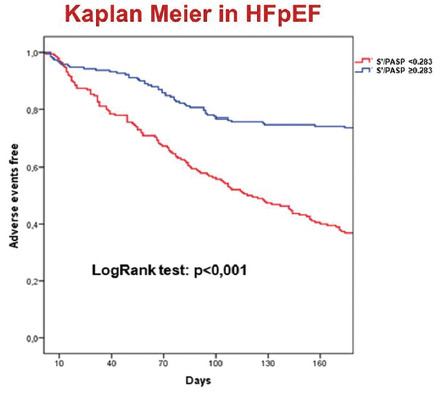
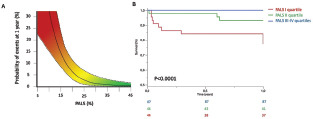
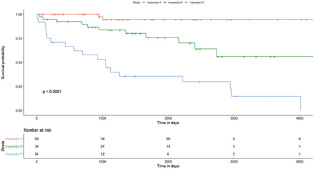
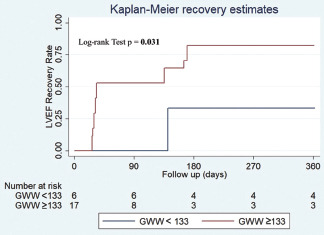
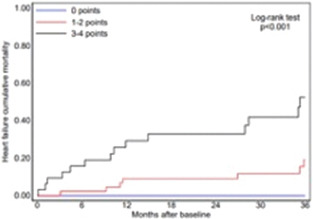
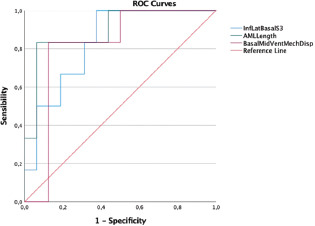
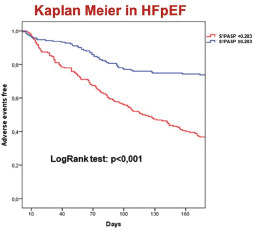
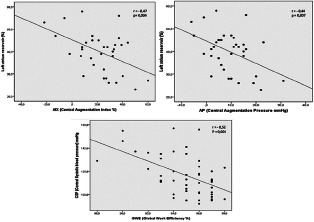
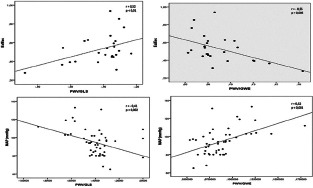
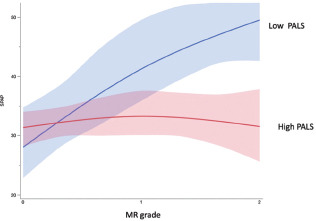
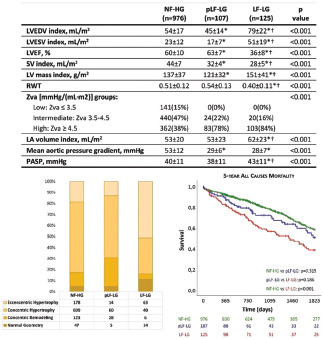
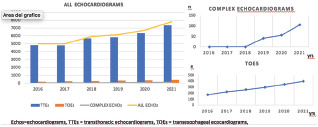
Results: 154 MVA were performed. After excluding 11 patients, among the remaining 143, AFMR were diagnosed in 24 patients, PMR in 119 patients. Compared to PMR, patients with AFMR were older (p 0,002), female (p 0,003), with worst New York Heart Association functional class (p 0,0072), with more comorbidities, including hypertension (p 0.00015) and atrial fibrillation (p 0.00001), higher left atrium volume (p 0,000004), higher average E/e' (p 0.0003) and more frequent severe tricuspid regurgitation (p 0,00001). During the follow up (38±13 mounths), 24 patients were lost and 5 patients died (4,3% in the AFMR group, 4% in PMR group). Patients with AFMR and PMR, treated by annuloplasty, had the same survival rate (log-rank p 0.09). No HFH were registered
Conclusions: AFMR is characterized by an unfavorable cardiovascular background. An early surgery correction could improve survival of these patients.
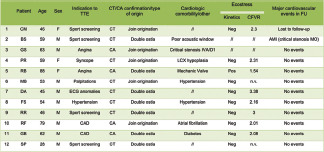
| All (n=143) | AFMR (n=24) | PMR (n=119) | P | |
|---|---|---|---|---|
| Baseline characteristics | ||||
| Age, Years | 63,7±11,5 | 70,2±9,2 | 62,3±11,5 | 0,02 |
| BMI, Kg/m2 | 25,8±4,0 | 26,5±5,0 | 25,7±3,7 | 0,43 |
| Female | 66 (46,2%) | 18(75%) | 48 (40,4%) | 0,003 |
| Smokers | 53 (37,1%) | 8 (33,3%) | 45 (37,8%) | 0,818 |
| NYHA class | 0,0072* | |||
| - I | 0 | 0 | 0 | - |
| - II | 46(32,2%) | 2 (8,3%) | 44(37,0%) | - |
| - III | 75 (52,4%) | 19 (79,2%) | 56 (47,0%) | - |
| - IV | 22 (15,4%) | 3 (12,5%) | 19(16,0%) | - |
| Atrial fibrillation | 37 (25,9%) | 19(79,2%) | 18(15,1%) | 0,00001 |
| Arterial Hypertension | 77 (53,8%) | 20 (83,3%) | 57 (47,9%) | 0,0015 |
| Dyslipidemia | 37 (25,9%) | 5 (20,8%) | 32 (26,9%) | 0,6183 |
| Coronary Artery Disease | 52 (36,4%) | 9(20,8%) | 43(36,1%) | 1 |
| Diabetes mellitus | 11 (7,7%) | 4(16,7%) | 7 (5,9%) | 0,0892 |
| Echocardiographic Characteristics | ||||
| Ejection fraction, % | 66,2±6,9 | 60,7±6,6 | 67,3±6,4 | 0,09 |
| End Diastolic Volume, ml | 140,6±39,8 | 125,0±29,7 | 146,0±41,5 | 0,02 |
| End systolic Volume, ml | 47,5±18,7 | 54,7±25,4 | 45,1±15,2 | 0,065 |
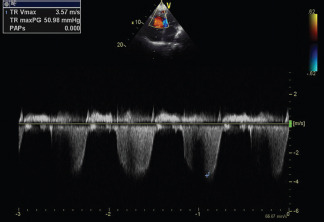
| Severe Tricuspide Regurgitation | 20 (14,0%) | 17 (70,8%) | 3 (2,5%) | 0,00001 |
| Anteroposterior Diameter of left atrium, mm | 47,4±8,3 | 51,9±8,6 | 46,5±7,9 | 0,002747 |
| Left atrium volume, ml | 73,4±31,4 | 93,3±15,8 | 69,7±32,2 | 0,000004 |
| E/e’ | 15,2±2,5 | 18,S±3,0 | 14,7±2,6 | 0,0003 |




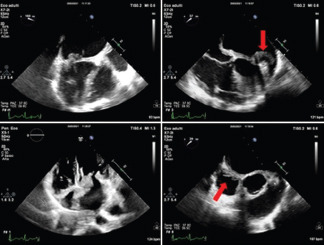
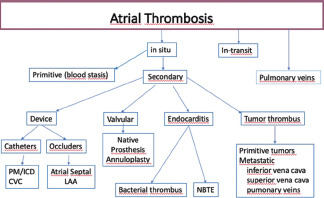
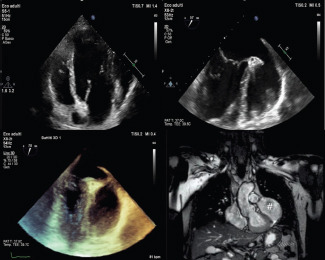
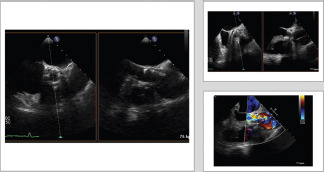
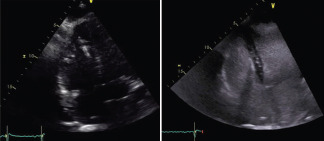
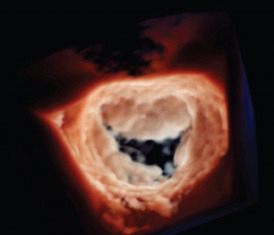
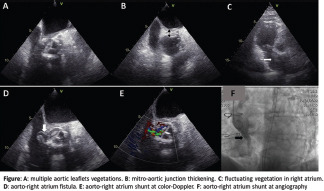
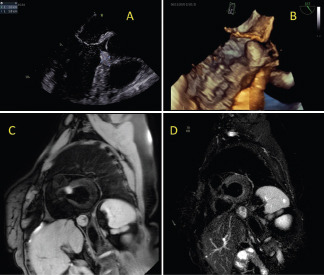
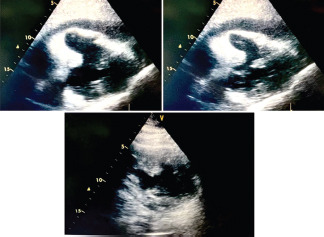


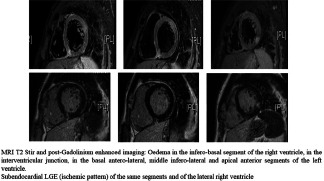
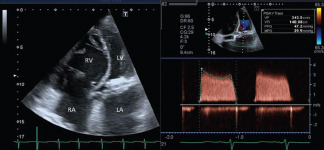
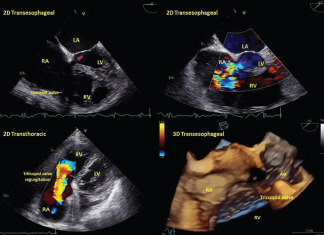
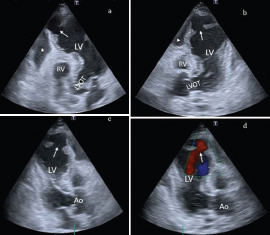


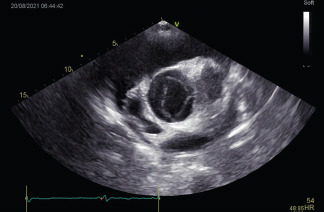
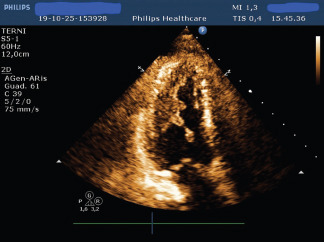
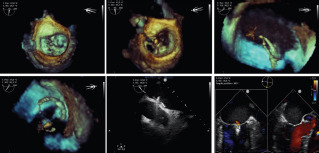
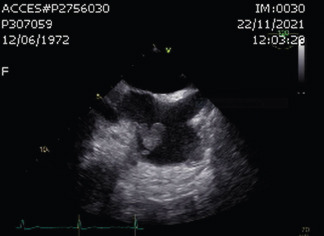
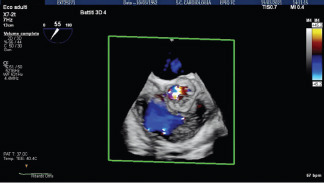
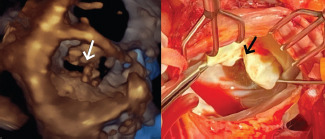

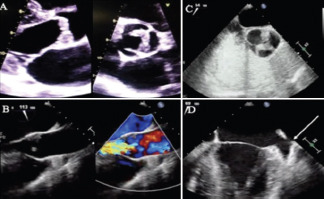

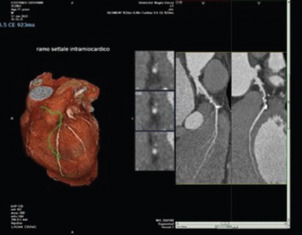
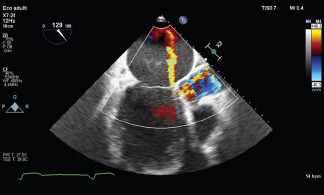
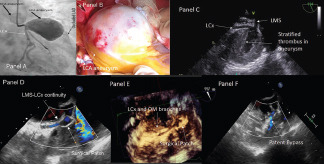
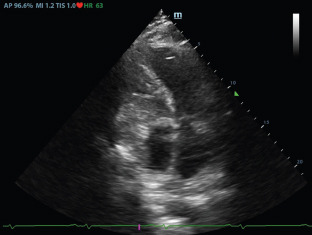
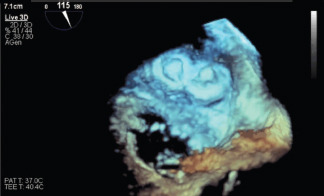
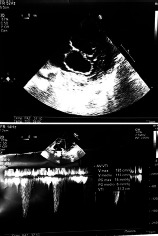
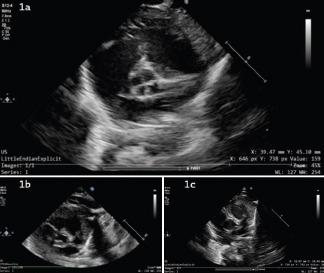


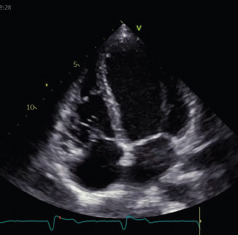
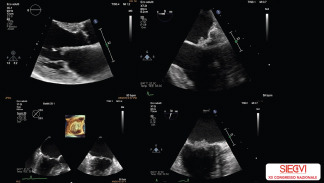
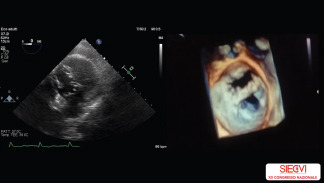

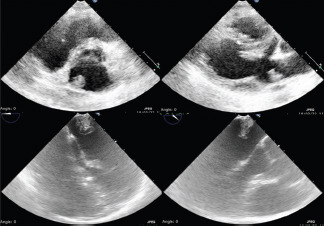

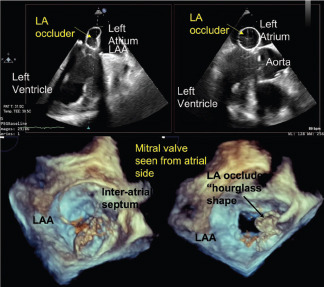
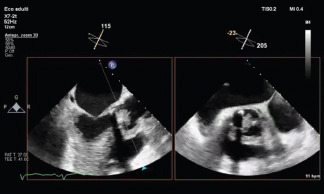

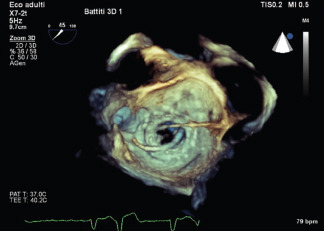
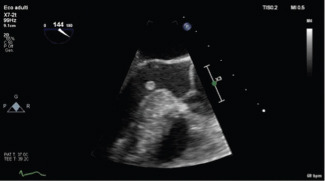

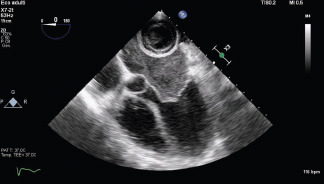
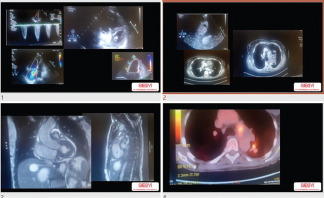
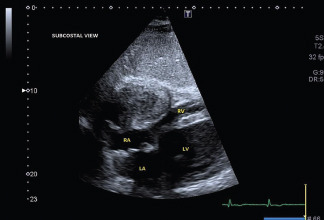
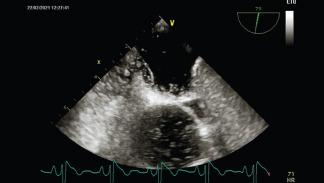
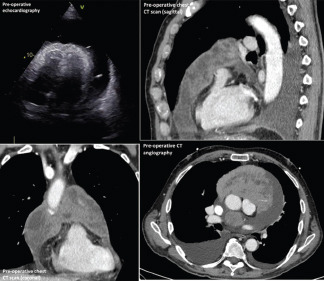
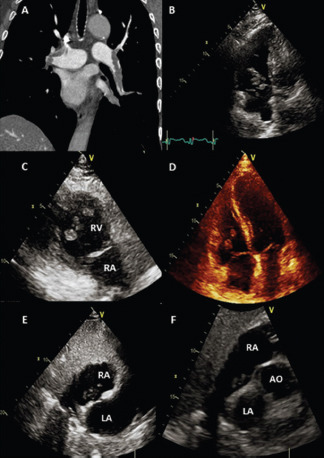
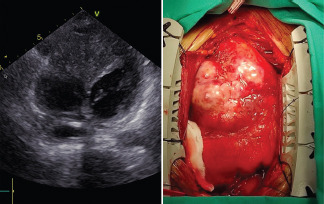

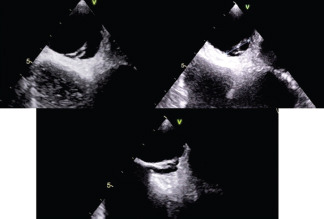

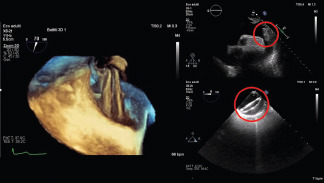
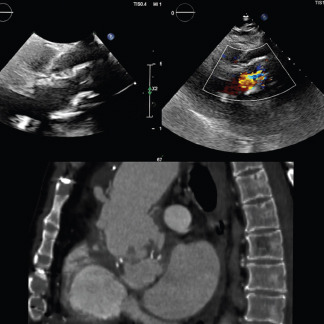
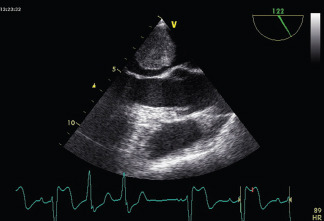


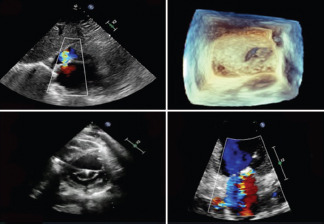
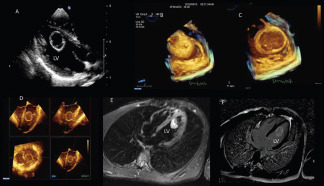
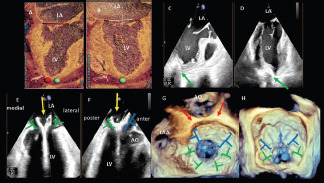
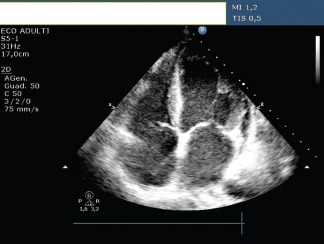
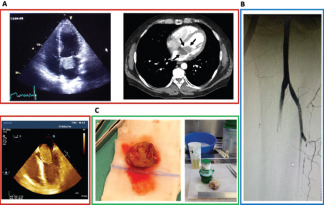
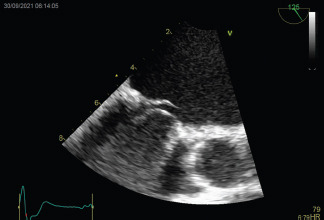
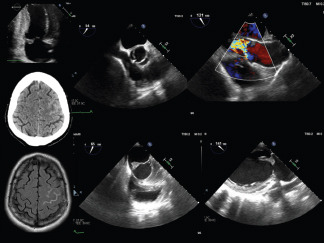
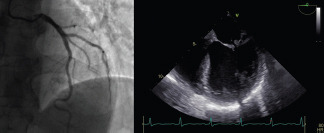
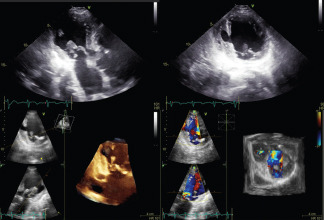
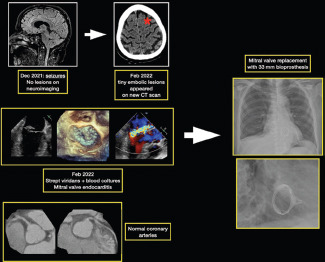
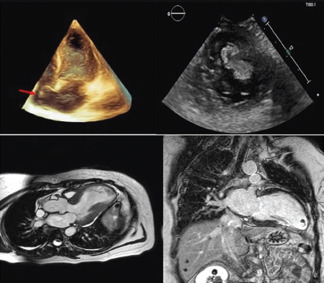
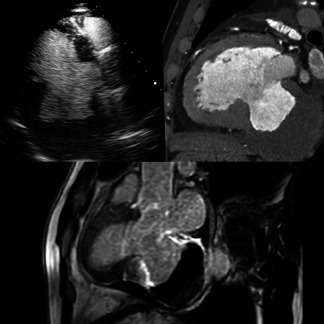
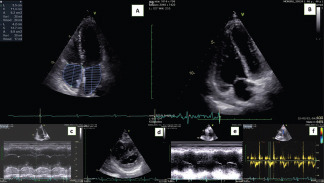
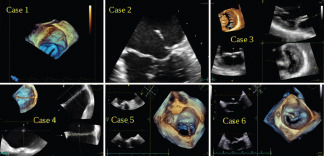
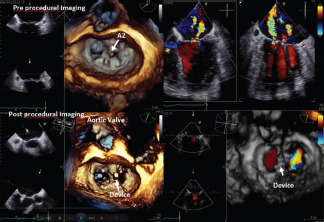
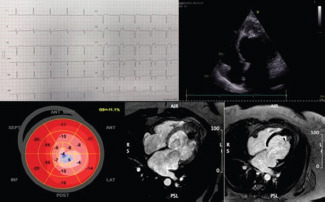
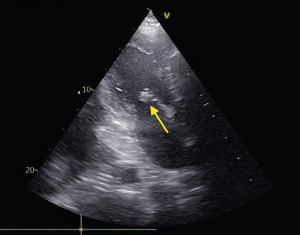
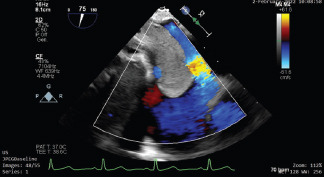
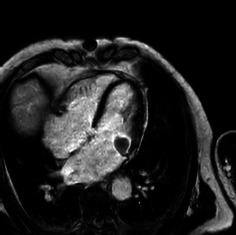
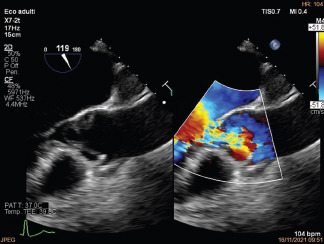
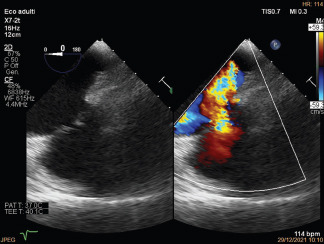
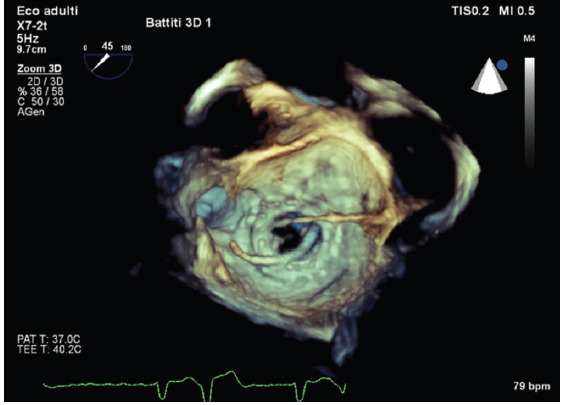
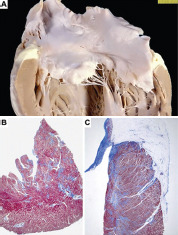
 An 11 year-old girl, who underwent an OS-ASD percutaneous closure with a 32 mm occluder, was diagnosed with a mild COVID19 a week after the procedure. After the recovery, at 1-month medical evaluation, transthoracic echocardiography (TTE) showed a large mobile mass attached to the right side of the well-positioned device, impinging on the tricuspid orifice, with no evidence of significant rigurgitation or functional stenosis. The patient was asymptomatic and on DAPT with aspirin and clopidogrel. She was hospitalized, clopidogrel was interrupted and warfarin was started. We excluded endocarditis. Transesophageal echocardiography (TEE) confirmed the diagnosis of intracardiac thrombosis, without evidence of residual interatrial shunt. Angio-pulmonary computed tomography excluded thromboembolism. Thrombophilic screening documented 3 heterozygote mutations (Factor V Leiden, MTHFR C677T/A1298C) and no pathogenetic CYP2C19 polymorphisms emerged. Because of clinical stability, we opted for a conservative approach, continuing warfarin (INR target 2-3) for at least 3 months and close follow-up. CONCLUSION
An 11 year-old girl, who underwent an OS-ASD percutaneous closure with a 32 mm occluder, was diagnosed with a mild COVID19 a week after the procedure. After the recovery, at 1-month medical evaluation, transthoracic echocardiography (TTE) showed a large mobile mass attached to the right side of the well-positioned device, impinging on the tricuspid orifice, with no evidence of significant rigurgitation or functional stenosis. The patient was asymptomatic and on DAPT with aspirin and clopidogrel. She was hospitalized, clopidogrel was interrupted and warfarin was started. We excluded endocarditis. Transesophageal echocardiography (TEE) confirmed the diagnosis of intracardiac thrombosis, without evidence of residual interatrial shunt. Angio-pulmonary computed tomography excluded thromboembolism. Thrombophilic screening documented 3 heterozygote mutations (Factor V Leiden, MTHFR C677T/A1298C) and no pathogenetic CYP2C19 polymorphisms emerged. Because of clinical stability, we opted for a conservative approach, continuing warfarin (INR target 2-3) for at least 3 months and close follow-up. CONCLUSION