Abstract
Objective:
Identifying the potential pathways linking childhood abuse to depression and suicidal ideation is critical for developing effective interventions. This study investigated implicit self-esteem―unconscious valenced self-evaluation―as a potential pathway linking childhood abuse with depression and suicidal ideation.
Method:
A sample of youth aged 8–16 years (N = 240) completed a self-esteem Implicit Association Test (IAT) and assessments of abuse exposure, and psychopathology symptoms, including depression, suicidal ideation, anxiety, and externalizing symptoms. Psychopathology symptoms were re-assessed 1–3 years later.
Results:
Childhood abuse was positively associated with baseline and follow-up depression symptoms and suicidal ideation severity, and negatively associated with implicit self-esteem. Lower implicit self-esteem was associated with both depression and suicidal ideation assessed concurrently and predicted significant increases in depression and suicidal ideation over the longitudinal follow-up period. Lower implicit self-esteem was also associated with baseline anxiety, externalizing symptoms, and a general psychopathology factor (i.e. p-factor). We found an indirect effect of childhood abuse on baseline and follow-up depression symptoms and baseline suicidal ideation through implicit self-esteem.
Conclusion:
These findings point to implicit self-esteem as a potential mechanism linking childhood abuse to depression and suicidal ideation.
Keywords: childhood abuse, trauma, depression, suicide, implicit self-esteem
Exposure to childhood adversity is common and associated with a host of negative physical and mental health outcomes across the lifespan (Green et al., 2010; McLaughlin et al., 2012). Forms of adversity related to maladaptive functioning within the family have a particularly strong association with the onset of psychopathology (Kessler et al., 2010; McLaughlin et al., 2012). Of these types of maladaptive family functioning, exposure to childhood abuse is strongly related to risk for psychopathology, including depression and suicidal ideation and behaviors (Dunn, McLaughlin, Slopen, Rosand, & Smoller, 2013; Miller, Esposito-Smythers, Weismoore, & Renshaw, 2013; Norman, Byambaa, De, Butchart, Scott, & Vos, 2012). Childhood abuse is associated not only with higher risk for developing depression, but it also predicts the persistence of depression and greater resistance to treatment (Nanni, Uher, & Danese, 2012). Although the association of childhood abuse with depression and suicidal ideation is well supported, the mechanisms that underlie these strong relationships remain poorly understood.
One specific mediating pathway through which childhood abuse may contribute to risk for depression and suicidal ideation involves changes in how children evaluate themselves―their self-esteem. Self-esteem is widely conceived as a relatively stable trait, consisting of positive self-evaluations or attitudes towards the self (Rosenberg, 1965). Childhood abuse may negatively influence a child’s self-evaluations by providing the child with negative feedback, harsh criticism and insults, or continued exposure to physical harm from caregivers—all common experiences among children who have been abused (Teicher, Samson, Polcari, & McGreenery, 2006; Trickett & McBride-Chang, 1995).
Attitudes about the self can be broadly classified into those that are explicit and under conscious control, and those that are implicit, automatic, and not under conscious control (Greenwald & Banaji, 1995). Explicit self-evaluations, which can be measured through self-report, may be altered by conscious, reflective processes and are subjective by nature (Evans, 2008). These types of explicit self-construals are what is assessed in the common approaches used for measuring self-esteem (e.g., Blascovich & Tomaka, 1991). In contrast, implicit self-evaluations are not readily accessible to conscious self-reflection and introspection and are typically measured through Implicit Association Tests or name letter tasks (Greenwald & Banaji, 1995; Nuttin, 1985). These types of implicit tests have been used to examine implicit self-esteem in both children and adults (e.g., Creemers, Scholte, Engels, Prinstein, & Wiers, 2012; Cvencek, Greenwald, & Meltzoff, 2016) and allow self-evaluations to be measured behaviorally without relying on verbal responses, checklists, or other forms of reflective self-report.
To date, the link between childhood abuse and self-esteem has been explored exclusively through explicit self-report methods. Existing evidence indicates an association between childhood abuse and lower explicit self-esteem in childhood (Bolger, Patterson, & Kupersmidt, 1998; Leeson & Nixon, 2011) over and above the influence of neglect (Toth, Manly, & Cicchetti, 1992). Furthermore, the negative association between childhood abuse and explicit self-esteem persists into adulthood (Gross & Keller, 1992). Although the link between childhood abuse and explicit self-esteem has been observed, it is unknown whether childhood abuse influences implicit self-esteem.
While self-report measures provide valuable insights into explicit self-esteem, there are at least four measurement considerations that indicate a need for studying self-esteem with young children using implicit measurement methods. First, explicit measures are commonly influence by social desirability concerns. With the general understanding that self-esteem is a desirable trait, transparency in self-esteem questionnaires can result in these measures functioning more to reveal impression management strategies than self-esteem (Paulhus, 1991, 2002). In contrast, implicit measures have been found to be low in susceptibility to self-presentational distortion (Cvencek, Greenwald, Brown, Gray, & Snowden, 2010).
Second, little is known about how explicit and implicit processes may each uniquely contribute to cognitive vulnerability to depression and suicidal ideation. It is well known that negative self-esteem is a risk factor for depression. However, it is still unknown whether such negative self-evaluations are generated deliberately through conscious and introspective processing of self-relevant information, or whether they are generated automatically from non-conscious processing (Haeffel et al., 2007) or an interaction of the implicit and explicit systems (Cvenceck, Greenwald, McLaughlin, & Meltzoff, 2020).
Third, another potential reason that collecting implicit measures of self-esteem may be useful in clinical research concerns the extent to which participants accurately perceive their self-esteem. Accurate reporting on self-report measures requires awareness of and the ability to introspect upon one’s internal processes. This may be particularly difficult for children who have experienced abuse as there is evidence that childhood abuse is associated with lower self-awareness (Briere & Rickards, 2007). In addition, the target construct of affective self-regard may be unavailable to introspection in very young children. However, children as young as 5 years of age demonstrate positive self-esteem on implicit measures, and the strength of implicit self-esteem with young children matches that found in the previous studies with adult samples (Cvencek et al., 2016). Further study into alternative measurement methods of self-esteem, such as implicit measures, may provide a more complete picture of the role that self-esteem plays in the development of psychopathology following childhood abuse.
Fourth, prior research with adults has shown that explicit and implicit self-esteem are not always congruent, suggesting that they reflect at least somewhat distinct constructs (e.g., Bosson, Brown, Zeigler-Hill, & Swann, 2003; Greenwald & Farnham, 2000). Scholars have argued that environmental experiences early in development are likely to form and influence deeply-seated, automatic processes that contribute to implicit self-esteem (Cvencek et al., 2016; DeHart, Pelham, & Tennen, 2006; Greenwald & Banaji, 2017). If true, experiences of childhood abuse may exert a particularly strong influence on implicit self-esteem, although we are unaware of prior research directly examining this question.
Negative self-representations resulting from childhood abuse experiences may contribute to risk for depression and suicidal ideation, two forms of psychopathology that have been linked to low self-esteem. Lower explicit self-esteem has been associated with depression across the lifespan in numerous studies (Cai, 2003; van Tuijl, de Jong, Sportel, de Hullu, & Nauta, 2014). Shared measurement variance and overlapping items in the assessment of explicit self-esteem and depression may account for some of these findings, so extending research to include implicit measures of self-esteem is important for gaining new insights into the relationship between self-esteem and depression. Studies investigating the link between implicit self-esteem and depression have produced mixed results, however. While some studies have found associations between lower implicit self-esteem and depression in adults and adolescents (Franck, De Raedt, Dereu, & Van den Abbeele, 2007; Wu, Sun, Geng, & Ding, 2009), other studies of adults have not (Cai, 2003; De Raedt et al., 2006; Franck, De Raedt, & Houwer, 2007; van Tuijl et al., 2014). Most of this prior work has focused on adults (Cai, 2003; De Raedt et al., 2006; Franck, De Raedt, Dereu, & Van den Abbeele, 2007; van Tuijl et al., 2014), and it remains unclear whether low implicit self-esteem contributes to risk for depression specifically in children and adolescents. Identity development is in flux during childhood and adolescence, and implicit measures of self-esteem may be particularly useful indicators of self-esteem before explicit evaluations of the self have crystallized. We extend prior work on implicit self-esteem and depression by investigating these associations in a large sample of children and adolescents followed over several years. Although low explicit self-esteem has also been associated with other forms of psychopathology in children, including anxiety, internalizing psychopathology broadly (Isomaa, Väänänen, Fröjd, Kaltiala-Heino, & Marttunen, 2013; Lee & Hankin, 2009), and externalizing problems (Donnellan et al., 2005), we focus here on the role of implicit self-esteem as a pathway to depression and suicidal ideation given the central role of low self-esteem in the etiology of depression and prior research linking both implicit and explicit self-esteem to depression and suicidal ideation (Cai, 2003; Creemers et al., 2012; Franck, De Raedt, Dereu, & Van den Abbeele, 2007; van Tuijl et al., 2014; Wu et al., 2009).
Low explicit self-esteem has also been associated with suicidal ideation (Creemers et al., 2012) even after controlling for co-occurring depression (Bhar, Ghahramanlou-Holloway, Brown, & Beck, 2008). The relationship between implicit self-esteem and suicidal ideation is less clear in adults, with several studies finding no meaningful relationship (Creemers et al., 2012; Franck, De Raedt, Dereu, & Van den Abbeele, 2007). No prior studies have examined the relationship between implicit self-esteem and suicidal ideation in children and adolescents. However, research using implicit measures has demonstrated—in both adult and adolescent samples—that implicit links involving death and the self are associated with repeated thoughts of suicide and prospectively predict suicidal thoughts over time (Glenn et al., 2017; Nock & Banaji, 2007). These results suggest that assessment of implicit cognitions related to the self may potentially improve prediction of suicide risk.
Although studies examining implicit self-esteem as a potential mechanism linking childhood abuse with depression and suicidal ideation are currently lacking, two prior studies suggest that low explicit self-esteem may be a mediator of the association between childhood abuse and depression in adolescents (Arslan, 2016; Greger, Myhre, Klöckner, & Jozefiak, 2017). One prior study has also supported low explicit self-esteem as a potential mechanism linking abuse to suicidal ideation in young adults (Duprey, Oshri, & Liu, 2019). These studies have, however, focused on explicit self-esteem, and to our knowledge, similar work has not been conducted examining implicit self-esteem as a link between child abuse and depression and suicidal ideation.
Here, we examine whether lower implicit self-esteem—automatic negative self-representations—may be a mechanism linking childhood abuse to depression and suicidal ideation in children and adolescents. First, we hypothesized that childhood abuse would be associated with lower implicit self-esteem, assessed using a behavioral measure based on the Implicit Association Test (IAT), which has been validated with children (Cvencek et al., 2016). Second, we hypothesized that lower implicit self-esteem would be associated specifically with higher levels of depressive symptoms and suicidal ideation in children and adolescents based on the idea that implicit self-evaluations emerge early and therefore can begin to exert influence on the development of depression and suicidal ideation starting earlier in development than has been classically reported using explicit measures. Based on previous work supporting the distinctions between implicit self-esteem and explicit self-esteem, we hypothesized that implicit self-esteem would be associated with depression even after removing self-esteem related items from the depression measure. We hypothesized that low implicit self-esteem would be uniquely associated with depression and suicidal ideation, but not other forms of psychopathology, including anxiety, externalizing symptoms, and a general factor of psychopathology (i.e., p-factor). Finally, we expected that lower implicit self-esteem would mediate the association of childhood abuse with symptoms of depression and suicidal ideation.
Method
Sample
Children aged 8–16 years (Mage = 12.68 years; SD = 2.58 years) and a parent or guardian were recruited to participate in a study examining child trauma exposure, emotion regulation, and psychopathology. A total of 262 children aged 8–16 years were enrolled into the study. Children and caregivers were recruited for participation at schools, after-school and prevention programs, adoption programs, food banks, shelters, parenting programs, medical clinics, and the general community in Seattle, WA, between January 2015 and June 2017. Recruitment efforts were targeted at recruiting a sample with variation in exposure to maltreatment-related trauma. To do so, we recruited from neighborhoods with high levels of violent crime, from clinics that served a predominantly low-SES catchment area, and agencies that work with families who have been victims of violence (e.g., domestic violence shelters, programs for parents mandated to receive intervention by Child Protective Services). Recruitment was aimed at identifying a sample of 150 children with exposure to physical or sexual abuse or direct witnessing of domestic violence, along with an age-and sex-matched control group with no exposure to maltreatment or significant interpersonal violence for follow-up neuroimaging assessments that are not the focus of the current report. Exclusion criteria included IQ < 80, presence of pervasive developmental disorder, active psychotic symptoms or mania, and active substance abuse. Of the 262 children enrolled in the first study visit, three were excluded from all analyses due to low IQ (n = 1), presence of pervasive developmental disorder (n = 1), and presence of psychotic symptoms and drug abuse (n = 1). The IAT was not administered to 14 participants due to session time constraints, and 5 participants were excluded from the analyses due to poor performance on the IAT (see Implicit self-esteem section under ‘Measures’ below). These participants do not differ by gender, age, abuse exposure, depression, or suicidal ideation from participants who completed the IAT. The total sample size for the present analysis was 240 children and adolescents.
A longitudinal follow-up assessment was conducted approximately two years following the baseline assessments (M = 21.96 months, SD = 7.88 months) to assess symptoms of psychopathology and suicidal ideation. Implicit self-esteem was not assessed at follow-up. Abuse exposure was assessed at both time points using the same measures; however, given our research questions, we focus only on exposure to abuse occurring prior to the assessment of implicit self-esteem. A total of 198 children and adolescents of the 262 participants comprising the baseline sample (75.6%) completed a follow-up visit. Two participants at follow-up did not provide enough information about suicidal ideation to be included in analysis. Participants who completed the follow-up did not differ from those at baseline on abuse exposure, χ² = 0.78, p = .38, implicit self-esteem, t(93.64) = 0.29, p = .77, baseline depression, t(93.78) = 0.53, p = .60, or baseline suicidal ideation severity, t(155.41) = −0.06, p = .95.
All procedures were approved by the Institutional Review Board at the University of Washington. Written informed consent was obtained from legal guardians; children provided written assent. Maltreatment not previously reported to the relevant authorities was reported to Child Protective Services using standard clinical procedures. See Table 1 for socio-demographic characteristics of the sample.
Table 1.
Descriptive Statistics by Childhood Abuse
| No Abuse (N = 112) |
Abuse (N = 128) |
Total Sample (N = 240) |
||||||
|---|---|---|---|---|---|---|---|---|
| Measure | M | SD | M | SD | M | SD | t | P |
|
| ||||||||
| Baseline (T1) | ||||||||
| Implicit Self-Esteem | 0.60 | 0.37 | 0.47 | 0.40 | 0.53 | 0.39 | 2.79** | .006 |
| Depression Symptoms | 5.48 | 4.35 | 11.04 | 8.27 | 8.45 | 7.27 | −7 33*** | <.001 |
| Suicidal Ideation Severity | 0.09 | 0.41 | 0.92 | 2.04 | 0.53 | 1.57 | −4 75*** | <.001 |
| Age | 12.36 | 2.51 | 12.96 | 2.63 | 12.68 | 2.58 | −1.75 | .08 |
| Income to Needs Ratio | 4.67 | 2.68 | 2.31 | 2.22 | 3.42 | 2.72 | 7.49*** | <.001 |
|
| ||||||||
| Subject Demographic | N | % | N | % | N | % | X 2 | P |
|
| ||||||||
| Female | 47 | 41.96 | 69 | 53.91 | 116 | 48.33 | 4.17* | .04 |
| White | 64 | 57.14 | 35 | 27.34 | 99 | 41.25 | 8.50** | .004 |
| Black | 14 | 12.50 | 48 | 37.50 | 62 | 25.83 | 18.65*** | <.001 |
| Latino | 11 | 9.82 | 18 | 14.06 | 29 | 12.08 | 1.69 | .19 |
| Asian | 16 | 14.29 | 11 | 8.59 | 27 | 11.25 | 0.93 | .34 |
| Other | 7 | 6.25 | 16 | 12.50 | 23 | 9.58 | 3.52 | .06 |
| Below Poverty Line | 12 | 10.71 | 44 | 34.38 | 56 | 23.33 | 18.29*** | <.001 |
|
| ||||||||
| No Abuse (N = 90) |
Abuse (N = 88) |
Total Sample (N = 178) |
||||||
| Measure | M | SD | M | SD | M | SD | t | P |
|
| ||||||||
| Follow-Up (T2) | ||||||||
| Depression Symptoms | 5.72 | 5.10 | 10.48 | 8.61 | 8.07 | 7.43 | −4.84*** | <.001 |
| Suicidal Ideation Severity | 0.10 | 0.59 | 1.23 | 2.26 | 0.66 | 1.73 | −4 88*** | <.001 |
Note. t-value represents a two-sample t-test comparing means from children who experienced childhood abuse to children who has not experienced childhood abuse.
p < .05.
p < .01.
p < .001.
Measures
Abuse exposure.
We used a multi-informant, multi-method approach for assessing exposure to child maltreatment. Here, we focus specifically on children exposed to abuse, including physical, sexual, or emotional abuse. Children completed the Childhood Experiences of Care and Abuse (CECA) Interview (Bifulco, Brown, & Harris, 1994) with a trained member of our research team. The CECA assesses caregiving experiences, including physical and sexual abuse. Inter-rater reliability for maltreatment reports is excellent, and validation studies suggest high agreement between siblings on maltreatment reports (Bifulco, Brown, Lillie, & Jarvis, 1997). Children also completed two self-report measures: the Childhood Trauma Questionnaire (CTQ; Bernstein, Ahluvalia, Pogge, & Handelsman, 1997) and the UCLA PTSD Reaction Index (PTSD-RI; Steinberg, Brymer, Decker, & Pynoos, 2004). The CTQ is a 28-item scale that assesses the frequency of maltreatment during childhood, including physical, sexual, and emotional abuse. Validated thresholds for exposure to physical, sexual, and emotional abuse (Walker et al., 1999) were applied here in evaluating abuse exposure based on the CTQ. The CTQ has excellent psychometric properties including internal consistency, test-retest reliability, and convergent and discriminant validity with interviews and clinician reports of maltreatment (Bernstein et al., 1994, 1997). Internal consistency in our sample was good, α = .87. The PTSD-RI includes a trauma screen that assesses exposure to numerous traumatic events, including physical and sexual abuse and additionally assesses PTSD symptoms. The PTSD-RI has good internal consistency and convergent validity (Steinberg et al., 2013).
Caregivers completed three self-report measures: the Conflict Tactics Scale-Parent Child Version (CTS; Straus, Hamby, Finkelhor, Moore, & Runyan, 1998), the Juvenile Victimization Questionnaire (JVQ) lifetime caregiver report (Finkelhor, Hamby, Ormrod, & Turner, 2005), and the caregiver version of the PTSD-RI. The CTS includes 22 items assessing caregiver responses to child disobedience or misbehavior in the past year. Caregivers indicate how frequently they have used each strategy (e.g., shook him/her) on a Likert scale ranging from 0 (This has never happened) to 6 (More than 20 times in the past year) and can also indicate if they have used the strategy in the past but not in the last year. The CTS has adequate reliability and good discriminant and construct validity (Straus et al., 1998). The JVQ includes 34 items assessing exposure to crime, child maltreatment, peer and sibling victimization, sexual victimization, and witnessing indirect victimization and has excellent psychometric properties, including test-retest reliability and construct validity (Finkelhor et al., 2005). Caregivers endorsed whether their child had experienced each event in his/her lifetime. Caregivers also completed the trauma screen included in the PTSD-RI, described above.
We created a dichotomous abuse exposure variable based on both child and parent report of abuse experiences. Children were classified as experiencing physical or sexual abuse if abuse was endorsed by the child (on the CECA interview, PTSD-RI trauma screen, or above the validated CTQ threshold) or parent (on the CTS, JVQ, or PTSD-RI trauma screen). A total of 92 children (38.3%) experienced physical abuse and 56 children (23.3%) experienced sexual abuse. Inter-rater reliability was good for child and caregiver reports (82.0% agreement; kappa = 0.62). Exposure to emotional abuse was considered present if children scored above the validated threshold on the CTQ (Walker et al., 1999) or the CECA (Bifulco, Bernazzani, Moran, & Jacobs, 2005) and was determined based on child report only. A total of 82 children (34.2%) reported experiencing emotional abuse.
Neglect.
We measured neglect using the neglect subscale of the CECA interview (Bifulco et al., 1994). A sample item from the CECA neglect scale reads, “My parent neglected my basic needs (e.g. food and clothes).” The CECA neglect items (items 2, 3, 5, 7, 12, and 15) were rated by participants on a scale of 1 (Not at all) to 5 (Yes definitely). We created a sum score for the CECA neglect items and created a dichotomous neglect variable based on a validated cutoff score of 22 (Bifulco et al., 2005).
Socioeconomic status.
We measured socioeconomic status by calculating each family’s income to needs ratio. We assessed each family’s total yearly income through self-report. Then, we divided the family’s income by the poverty threshold income (adjusted for size of household).
Depression.
During the first study visit, children completed the Children’s Depression Inventory–2 (CDI-2), a widely used self-report measure of depressive symptoms in children and adolescents (Kovacs, 2011). The CDI-2 includes 28 items consisting of three statements (e.g., I am sad once in a while, I am sad many times, I am sad all the time) representing different levels of severity of a specific symptom of depression. The CDI-2 has sound psychometric properties, including internal consistency, test-retest reliability, and discriminant validity (Kovacs, 2011; Reynolds, 1994). The 28 items were summed to create a total score ranging from 0 to 56. The CDI-2 demonstrated good reliability in this sample (α = .89). The CDI-2 has a validated self-esteem subscale, which includes 6 items (items 2, 6, 7, 8, 13, 24; Kovacs, 2011). An example item is “I hate myself/I do not like myself/I like myself.” We used this subscale, excluding item 8—which assesses suicidal ideation— as a measure of explicit self-esteem in our analyses. At baseline assessments, 9% of participants had CDI-2 scores above a score of 19, indicating clinically significant levels of depression. At follow-up assessments, 11% of participants had CDI-2 scores indicating clinically significant levels of depression.
Suicidal ideation.
To assess suicidal ideation, interviewers conducted a shortened version of the Self-Injurious Thoughts and Behaviors Interview (SITBI), a widely utilized structured interview developed to assess presence, frequency, and characteristics of self-injurious thoughts and behaviors, including suicidal ideation, suicide plans, and suicide attempts (Nock et al., 2007). This interview has shown strong interrater reliability, test-retest reliability, and concurrent validity in a sample of adolescents aged 12–19 (Nock, Holmberg, Photos, & Michel, 2007). While we assessed both suicidal thoughts and behaviors during data collection, we focused exclusively on suicidal ideation in our analyses given low reported frequencies of self-injurious behaviors (12 participants reported any lifetime suicide attempts in our sample at baseline). The analyses in this study focused on lifetime presence (1) or absence (0) of suicidal ideation (“Have you ever had thoughts of killing yourself?”), and frequency of suicidal ideation for the participant’s lifetime, the past year, the past month, and the past week. The module also assesses the severity of suicidal ideation, both on average and at the worst point. For example, the severity of suicidal ideation on average is assessed using the question, “On average, how intense were your thoughts of killing yourself?” with response options ranging from 0 (low/little) to 4 (very much/severe). Following the approach by Miller et al. (2018), the suicidal ideation severity variable was calculated by taking standardized days of lifetime suicidal ideation added to standardized average intensity of the thoughts to capture severity of both frequency and intensity of suicidal thoughts. We also created a dichotomous suicidal ideation variable by examining whether a participant endorsed any lifetime suicidal ideation or not. At follow-up assessment, participants were asked the same questions covering the past year at the follow-up visit. We also created a dichotomous suicide ideation variable at follow-up by examining whether a participant endorsed suicidal ideation within a year of the follow-up assessment. Twenty percent of participants endorsed any lifetime suicidal ideation at baseline. Seventeen percent of participants endorsed any suicidal ideation in the year prior to the follow-up assessments.
Anxiety.
During the first study visit, children completed the Screen for Child Anxiety Related Disorders (SCARED), a widely used self-report measure of anxiety symptoms in children and adolescents (Birmaher et al., 1997). The SCARED includes 41 items assessing symptoms of five anxiety disorders: panic disorder, generalized anxiety disorder, separation anxiety, social anxiety disorder, and school avoidance. Each item is rated on a scale of 0 (Not True or Hardly Ever True) to 2 (Very True or Often True). The SCARED has sound psychometric properties, including internal consistency, test-retest reliability, and discriminant validity (Birmaher et al., 1997, 1999). The 41 items were summed to create a total score ranging from 0 to 82. The SCARED demonstrated excellent reliability in this sample (α = .94).
Externalizing symptoms.
Externalizing symptoms were assessed using both the child and caregiver reports on the Youth Self-Report (YSR) and Child Behavior Checklist (CBCL; Achenbach, 1991). The YSR and CBCL scales are among the most widely used transdiagnostic measures of internalizing and externalizing youth psychopathology. The higher raw score between the CBCL and YSR was used from the attention problems, rule-breaking behaviors, and aggressive behavior subscales to generate an externalizing psychopathology score for each participant.
General psychopathology factor (p-factor).
Based on the approach by Caspi and colleagues (2014), we calculated a general psychopathology factor, or p-factor, in our sample using confirmatory factor analysis (CFA) to test a bifactor model specifying a general psychopathology latent factor (“p”) using scores from externalizing scales of the YSR and CBCL, CDI-2, SCARED, and PTSD-RI (see Weissman et al., 2019, and Supplemental Materials for details on how p-factor scores were calculated in this sample). Standardized factor loadings for the latent p-factor (CDI-2, SCARED, PTSD-RI, externalizing problems) ranged from 0.44 to 0.80, all ps < .001. In the present analyses, we used the bifactor model of the p-factor because it is the most commonly reported general factor model of psychopathology in the existing literature (Caspi et al., 2014; Laceulle, Vollebergh, & Ormel, 2015) and our goal was not to estimate the structure of psychopathology in our sample but rather to generate a global measure of transdiagnostic psychopathology symptoms.
Implicit self-esteem.
Children completed a child friendly adaptation of the Implicit Association Test (IAT) in the first study visit. This “Child IAT” (Cvencek et al., 2016) is a validated tool used to assess implicit self-esteem—implicit evaluations of the self as good or bad—in young children. Following the standardized Child IAT procedures, participants were instructed to sort stimuli in four categories: self (e.g., me, I), other (e.g., they, them), positive (e.g., good, smart), and negative (e.g., bad, awful). The task was presented in seven blocks. Two practice blocks (20 trials each) oriented the participant to sorting stimuli into self versus other and good versus bad categories. One practice block (20 trials) and one test block (40 trials) was presented to each participant pairing: (a) self with positive versus other with negative (“congruent” pairing) or (b) self with negative versus other with positive (“incongruent” pairing). In line with published recommendations for reducing the effect of combined-task order on the estimated sample means of IAT measures (e.g., stronger association for category pairing that is presented first), the order of the congruent versus incongruent pairings was counterbalanced (Greenwald et al., 2003). There was one block between test blocks orienting the participant to the positive and negative words switching from their initial pairing (20 trials). Consistent with previous studies using the Child IAT (e.g., Cvencek et al., 2011), both text and audio stimuli were used to ensure that differences in reading ability did not impact performance. Faster sorting response times indicated a stronger association between the category pairings. For example, sorting self stimuli with positively valenced words such as “good” (and other stimuli with negatively valenced words) would indicate a positive implicit attitude toward self (me = good).
The self-esteem score was calculated using the scoring algorithm developed by Greenwald and colleagues (2003). Specifically, D is the difference between the mean response latencies for the two combined pairing blocks divided by the standard deviation of response latencies in all combined pairing blocks. This measure (D) had computational upper and lower bounds of +2 (me = good) and –2 (me = bad), with the value of 0 indicating equally strong association of self with both positive and negative valence. In other words, higher scores reflect a relatively more positive implicit self-esteem. Child IAT data for five participants were excluded based on previously published exclusion criteria for this test (e.g., excessively slow responding; Cvencek et al., 2011).
Statistical Analysis
We first examined whether race/ethnicity should be included as a potential confounder that should be adjusted for in our analysis because it was associated with abuse. Race/ethnicity (coded as White v. Non-White) was not significantly associated with implicit self-esteem, t(238) = −1.717, 95% CI [−0.19, 0.01], p = 0.09, and thus was not included as a covariate in models examining the association of abuse with implicit self-esteem or of implicit self-esteem with psychopathology.
We took several steps to determine the most appropriate regression distribution specifications (e.g., normal distribution gaussian specification). First, we visually inspected the distributions of our outcome variables to assess whether these distributions violated gaussian regression assumptions. Then, we inspected the distribution of model residuals to assess for normality. For outcomes and residuals that were right skewed, we fit regressions with negative binomial distribution specifications and inspected the distribution model residuals to assess for normality. We found that implicit self-esteem scores were normally distributed and thus retained a gaussian distribution specification for models predicting this outcome. Both depression and suicidal ideation severity were right skewed, with more scores on the lower end of the distribution than the higher end and our analysis indicated that a negative binomial distribution specification provided a better fit for these outcomes than a gaussian distribution. We have standardized all regression parameters and confidence intervals using the effectsize package in R (Ben-Shachar, Makowski & Lüdecke, 2020; R Core Team, 2019).
Next, we examined the association of abuse with depression and suicidal ideation using a negative binomial regression with abuse exposure as a predictor using the MASS package in R (Venables & Ripley, 2002). Additionally, we examined the association of abuse with a dichotomous suicidal ideation variable using a logistic regression with abuse exposure as a predictor using the stats package (Chambers, 1992) in R. Next, we examined the association between abuse and the implicit self-esteem scores using a linear regression using the stats package (Chambers, 1992) in R. We also evaluated whether implicit self-esteem was associated with SES and neglect. Additionally, we examined whether age, sex, or time between baseline and follow-up moderated the association between abuse and implicit self-esteem and whether each of the three types of abuse assessed in our sample (physical, sexual, and emotional abuse) were associated with implicit self-esteem.
In a third step, we evaluated whether performance on the self-esteem IAT was associated with depression and suicidal ideation at baseline as well as at the longitudinal follow-up, using a negative binomial regression. Additionally, we evaluated whether performance on the self-esteem IAT was associated with a dichotomous suicidal ideation variable at baseline as well as within a year of longitudinal follow-up assessments using a logistic regression. Further, we examined whether implicit self-esteem was associated with other forms of psychopathology, including anxiety, externalizing symptoms, and a general psychopathology factor (i.e., p-factor). In longitudinal analyses, we controlled for the time elapsed between baseline and follow-up assessments as well as the level of depressive symptoms or the presence or severity of lifetime suicidal ideation at baseline. Age and sex were included as covariates in all regression models.
Next, we ran several sensitivity analyses to investigate whether implicit self-esteem was associated with unique variance in predicting depression and suicidal ideation over and above explicit self-esteem. First, we examined the correlation of the self-esteem subscale of the CDI-2 with implicit self-esteem as assessed by the IAT. Second, we examined whether implicit self-esteem was associated with depression symptoms after removing the items on the CDI-2 that assess explicit self-esteem. Third, we evaluated whether implicit self-esteem was associated with depression symptoms and self-esteem in a model that controlled for explicit self-esteem. Finally, we examined whether implicit self-esteem mediated the association of childhood abuse and depression symptoms after excluding the CDI-2 self-esteem subscale from the total depression score. We conducted these analyses at both baseline and follow-up.
Finally, we investigated whether there was an indirect effect of abuse on depression and suicidal ideation through implicit self-esteem at baseline and follow-up. We used the PROCESS macro in SPSS (Hayes, 2017), a standard bootstrapping approach that provides confidence intervals for indirect effects. In both sets of models, we estimated 10,000 re-samples of the data to estimate the indirect effect. Confidence intervals that do not include 0 provide evidence for a statistically significant indirect effect. We have kept our mediation analyses within a gaussian framework, which is consistent with standards in the field. We have reported the results of gaussian linear regressions for each of the pathways contributing to the mediation model in Supplemental Table 1. Additionally, we examined if there was an indirect effect of abuse on the dichotomous suicidal ideation variable through implicit self-esteem at baseline and follow-up. We used the mediate package in R to conduct mediation analyses with a dichotomous outcome variable (Tingley, Yamamoto, Hirose, Keele, & Imai, 2014). These linear regressions produced weaker effects on average than the negative binomial models, but the direction of the effects remained consistent for both negative binomial regressions and gaussian regressions. Given the small amount of missing data on the IAT at baseline, missing data was handled with listwise deletion rather than imputing IAT scores.
Results
Descriptive Statistics
Table 1 provides the means and standard deviations of all measures separately for children with and without abuse. Table 2 provides the zero-order correlations among all measures, including abuse, implicit self-esteem, depression, suicidal ideation, and covariates. The majority of abuse exposed participants (86%) in our sample experienced abuse starting before age 8 (Mage = 6.00, SD = 2.59). The duration of physical or sexual abuse lasted 2 years on average (M = 2.08, SD = 2.76).
Table 2.
Correlations of Abuse, Implicit Self-Esteem, Depression, Suicidal Ideation, and Covariates
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| 1. Abuse | - | ||||||||
| 2. T1 CTQ Total Score | .57*** | - | |||||||
| 3. T1 Implicit Self-Esteem | −.21*** | −.01 | - | ||||||
| 4. T1 Depression | .38*** | .47*** | −.16* | - | |||||
| 5. T1 Suicidal Ideation | .27*** | .37*** | −.10 | .48*** | - | ||||
| 6. Age | .08 | .20** | .27*** | .28*** | .21** | - | |||
| 7. Sex | .15* | .18** | .08 | .18** | .03 | .09 | - | ||
| 8. T2 Depression | .32*** | .38*** | −.14 | .68*** | .39*** | .33*** | .20** | - | |
| 9. T2 Suicidal Ideation | .33*** | .43*** | −.11 | .50*** | .44*** | .24** | .16* | .62*** | - |
| Mean | - | 36.36 | 0.53 | 8.45 | 0.53 | 12.68 | - | 8.07 | 0.66 |
| SD | - | 14.05 | 0.39 | 7.27 | 1.57 | 2.58 | - | 7.43 | 1.73 |
Note. T1 = Time 1 (baseline); T2 = Time 2 (follow-up).
p < .05.
p <.01.
p < .001.
Abuse, Depression, and Suicidal Ideation
We first examined the associations of childhood abuse with symptoms of depression and severity of suicidal ideation. Children who experienced abuse had higher levels of depression symptoms at baseline (M = 11.04, SD = 8.27) than children who had never experienced abuse (M =5.48, SD = 4.35), β = 0.62, 95% CI [0.41,0.83], p < .001. A similar pattern was observed for suicidal ideation severity, such that children who were abused had higher suicidal ideation severity (M = 0.92, SD = 2.04) than children who were not abused (M = 0.09, SD = 0.41), β = 2.32, 95% CI [1.49, 3.23], p < .001. Additionally, the odds of children who were abused endorsing any lifetime suicidal ideation was significantly higher than for children who had not been abused, OR = 5.55, 95% CI [2.55, 13.49], p < .001. Child abuse was not associated with increases in depression symptoms over the follow-up period, β = 0.19, 95% CI [−0.06, 0.44], p = .14, but was associated with a significant increase in suicidal ideation severity after adjusting for baseline suicidal ideation, β = 2.32, 95% CI [1.35, 3.39], p < .001. Childhood abuse was also associated with the presence of suicidal ideation within a year of follow-up assessments after adjusting for the presence of any lifetime suicidal ideation at baseline, OR = 6.53, 95% CI [2.10, 25.32], p = .002.
We next examined whether the time that elapsed between baseline and follow-up assessments moderated the association between childhood abuse exposure and depression and suicidal ideation at follow-up. We found that time between baseline and follow-up assessments did not moderate the relationship between abuse exposure and follow-up depression, β = −0.02, 95% CI [−0.25, 0.22], p = .89, but that time between baseline and follow-up assessments moderated the relationship between abuse exposure and follow-up suicidal ideation, β = −1.27, 95% CI [−2.63, −0.12], p = .03 For participants who had not been exposed to abuse, those participants for whom more time elapsed between baseline and follow up assessments exhibited greater increases in SI at follow up. For participants who had been exposed to abuse, time between baseline and follow-up assessments was not associated with differences in suicidal ideation at follow-up.
Abuse and Implicit Self-Esteem
Next, we determined whether childhood abuse was associated with implicit self-esteem. We found significant differences in implicit self-esteem as a function of exposure to childhood abuse, β = −0.42, 95% CI [−0.66, −0.17], p < .001, such that children exposed to abuse had lower implicit self-esteem (M = 0.47, SD = 0.40) than children who had never been abused (M = 0.60, SD = 0.37). These differences persisted when controlling for neglect and socioeconomic status. Neither age, β = −0.11, 95% CI [−0.36, 0.13], p = .36, nor sex, β = −0.24, 95% CI [−0.74, 0.27], p = .36, interacted with abuse exposure to predict implicit self-esteem.
Critically, neither SES, β = 0.10, 95% CI [−0.02, 0.23], p = .11, nor neglect, β = 0.03, 95% CI [−0.09, 0.16], p = .58, was associated with implicit self-esteem, suggesting specificity to experiences of abuse.
Finally, we examined whether different types of abuse experiences were similarly associated with lower implicit self-esteem. Exposure to physical abuse was not associated with implicit self-esteem, β = −0.07, 95% CI [−0.20, 0.05], p = .23, whereas sexual abuse was marginally associated with lower implicit self-esteem, β = −0.12, 95% CI [−0.24, 0.01], p = .06, and emotional abuse exposure was significantly associated with lower implicit self-esteem, β = −0.17, 95% CI [−0.29, −0.04], p = .01.
Implicit Self-Esteem, Depression, and Suicidal Ideation
We next evaluated whether implicit self-esteem was associated with symptoms of depression and suicidal ideation at baseline as well as increases across the follow-up period (Table 3). Lower implicit self-esteem was associated with greater symptoms of depression at baseline, β = −0.22, 95% CI [−0.33, −0.10], p < .001, as well as with greater increases in depression symptoms across the follow-up period, controlling for baseline depression, β = −0.12, 95% CI [−0.25, −0.001], p = .043. Lower implicit self-esteem was also associated with more severe suicidal ideation at baseline, β = −0.50, 95% CI [−0.97, −0.07], p = .010, and was also associated with increases in the severity of suicidal ideation across the follow-up period, β = − 0.52, 95% CI [−1.04, −0.03], p = .028. Additionally, implicit self-esteem was inversely associated with the odds of endorsing lifetime suicidal ideation at baseline, OR = 0.32, 95% CI [0.13, 0.77], p = .010. In other words, at baseline, as implicit self-esteem increases, the odds of endorsing suicidal ideation decreases. Implicit self-esteem at baseline was not associated with the odds of endorsing suicidal ideation within a year of follow-up assessments after adjusting for the presence of lifetime suicidal ideation at baseline, OR = 0.64, 95% CI [0.18, 2.42], p = .51.
Table 3.
Regression Analyses: Implicit Self-Esteem and Psychopathology Outcomes
| Baseline |
Follow-Up |
|||||
|---|---|---|---|---|---|---|
| Symptom Severity | β | 95% CI | p | β | 95% CI | p |
|
| ||||||
| Depression | −0.22 | [−0.33, −0.10], | < .001 | −0.12 | [−0.25, −0.001] | .04 |
| Suicidal ideation | −0.50 | [−0.97, −0.07] | .01 | −0.52 | [−1.04, −0.03] | .03 |
| Anxiety | −0.14 | [−0.24, −0.04] | .003 | −0.09 | [−0.19, 0.01] | .08 |
| Externalizing | −0.17 | [−0.30, −0.04] | .01 | −0.02 | [−0.14, 0.09] | .69 |
| p-factor | −0.22 | [−0.35, −0.09] | .001 | −0.08 | [−0.20, 0.03] | .14 |
Note. Sex and age were included as covariates in all models. Baseline psychopathology and time elapsed between baseline and follow-up were included as covariates in models predicting follow-up psychopathology. CI = confidence interval.
Implicit Self-Esteem and Other Forms of Psychopathology
We assessed whether implicit self-esteem significantly predicted symptoms of other forms of psychopathology, including anxiety, externalizing problems, and a general psychopathology factor at both baseline and follow-up (Table 3). We found that lower implicit self-esteem was significantly associated with higher levels of baseline anxiety symptoms, β = − 0.14, 95% CI [−0.24, −0.04], p = .003, and was marginally associated with increased levels of anxiety symptoms at follow-up, β = −0.09, 95% CI [−0.19, 0.01], p = .08. Lower implicit self-esteem was also associated with higher levels of baseline externalizing symptoms, β = −0.17, 95% CI [−0.30, −0.04], p = .01, but was not associated with externalizing symptoms at follow-up controlling for baseline symptoms. Finally, lower implicit self-esteem was associated with higher p-factor scores at baseline, β = −0.22, 95% CI [−0.35, −0.09], p = .001, but was not associated with p-factor scores at follow-up controlling for baseline p-factor.
Indirect Effects
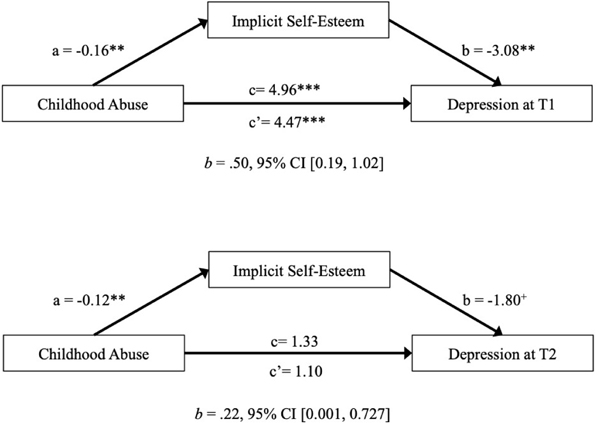
In a final step, we examined indirect effects of childhood abuse on depression and suicidal ideation through implicit self-esteem. There was a significant indirect effect of exposure to abuse on baseline depression symptoms through implicit self-esteem, b = .50, 95% CI [0.19, 1.02]. We also found a significant indirect effect of exposure to abuse on depression symptoms at the longitudinal follow-up through implicit self-esteem, when controlling for baseline depression severity, b = .22, 95% CI [0.001, 0.727] (see Figure 1). Given our finding that emotional abuse was more strongly associated with implicit self-esteem than either physical or sexual abuse, we examined the indirect effects of emotional abuse on depression and suicidal ideation through implicit self-esteem. Our findings for these mediation analyses were similar to those for exposure to childhood abuse. Although the magnitude of association of abuse with implicit self-esteem varied across different types of abuse, the indirect effect of childhood abuse on depression and suicidal ideation through implicit self-esteem was similar across these different types of childhood abuse exposure.
Figure 1.
Mediation models for implicit self-esteem mediating the relationship between childhood abuse and depression.
+p < .10. *p < .05. **p < .01. ***p < .001
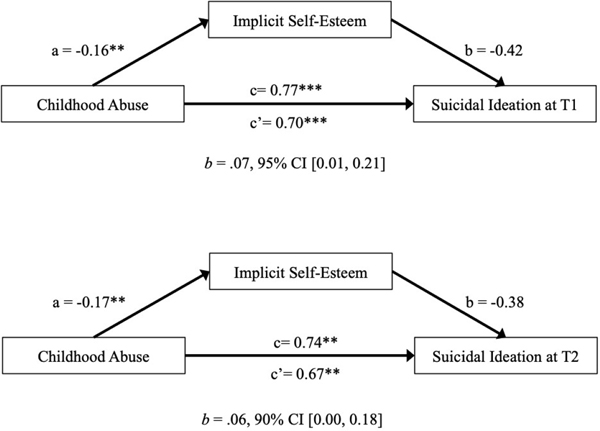
At baseline, we found a significant indirect effect of exposure to abuse on suicidal ideation severity through implicit self-esteem, b = .07, 95% CI [0.01, 0.21] (see Figure 2). We also found a marginally significant indirect effect of exposure to abuse on the presence of lifetime suicidal ideation through implicit self-esteem, b = .07, 95% CI [0.004, 0.25], p = .08. At follow-up, the indirect effect of exposure to abuse on suicidal ideation severity through implicit self-esteem, controlling for baseline suicidal ideation, was marginally significant, b = .06, 90% CI [0.00, 0.18] (see Figure 2), and the indirect effect of exposure to abuse on the presence of suicidal ideation within a year of follow-up assessments through implicit self-esteem, controlling for baseline lifetime suicidal ideation, was not significant, b = −.009, 95% CI [−0.23, 0.17], p = .88.
Figure 2.
Mediation models for implicit self-esteem mediating the relationship between childhood abuse and suicidal ideation.
+p < .10. *p < .05. **p < .01. ***p < .001.
Since lower implicit self-esteem was associated with higher levels of anxiety, externalizing symptoms, and the general psychopathology factor, we examined whether implicit self-esteem mediates the relationship between childhood abuse exposure and anxiety symptoms, externalizing symptoms, and general psychopathology. We found a marginally significant indirect effect of exposure to childhood abuse on anxiety symptoms through implicit self-esteem at baseline, b = .69, 90% CI [0.08, 1.47], but no indirect effect for externalizing symptoms, b = .23, 95% CI [−0.30, 0.84], nor a general psychopathology factor, b = .03, 95% CI [−0.001, 0.08]. We did not find a significant indirect effect of exposure to childhood abuse on anxiety, externalizing symptoms, or general psychopathology symptoms through implicit self-esteem at follow-up.
Explicit Self-Esteem Sensitivity Analysis
We ran several analyses to investigate whether implicit self-esteem is associated with unique variance when predicting depression and suicidal ideation compared to explicit self-esteem. First, we correlated the self-esteem subscale of the CDI-2 with implicit self-esteem. We found that explicit self-esteem and implicit self-esteem were not significantly correlated, r = − 0.05, 95% CI [−0.18, 0.08], p = .42. The lack of association between implicit and explicit self-esteem supports the notion that these are unique constructs.
Next, we examined whether implicit self-esteem predicts depression when excluding the self-esteem subscale from the CDI-2. At baseline, performance on the self-esteem IAT was associated with depression symptoms even after removing the items from the self-esteem subscale, β = −0.19, 95% CI [−0.31, −0.08], p < .001. Although the direction and effect size of the association between performance on the IAT and increases in depression symptoms over time were similar to our original model, this association was no longer significant once the items on the self-esteem subscale were removed, β = −0.09, 95% CI [−0.23, 0.05], p = .21.
Further, we examined whether implicit self-esteem predicts depression when excluding the self-esteem subscale from the CDI-2 and controlling for the self-esteem subscale. At baseline, performance on the self-esteem IAT was associated with depression symptoms after removing the items on self-esteem subscale and controlling for the self-esteem subscale in the analysis, β = −0.15, 95% CI [−0.24, −0.05], p = .002. Although the direction and effect size of the association between performance on the IAT and increases in depression symptoms over time were similar to our original model, this association was no longer significant once the items on the self-esteem subscale were removed and self-esteem was controlled for, β = −0.10, 95% CI [− 0.23, 0.04], p = .15.
We examined whether implicit self-esteem predicts suicidal ideation severity when controlling for the self-esteem subscale of the CDI-2. At baseline, performance on the self-esteem IAT was marginally associated with suicide ideation severity after controlling for the self-esteem subscale of the CDI-2, β = −0.32, 95% CI [−0.74, 0.08], p = .08. Performance on the self-esteem IAT was associated with increases in suicidal ideation severity over the two-year follow-up period after controlling for scores on the self-esteem subscale, β = −0.79, 95% CI [− 1.26, −0.37], p < .001.
In addition, we examined whether implicit self-esteem mediates the relationship between childhood abuse and depression symptoms (at both baseline and follow-up) after removing the self-esteem subscale items from the CDI-2 total score. Specifically, we observed a significant indirect effect of childhood abuse on baseline depression severity through implicit self-esteem even after removing the self-esteem subscale from the CDI-2, b = .31, 95% CI [0.04, 0.64]. The indirect effect of childhood abuse on follow-up depression severity through implicit self-esteem after removing the self-esteem subscale from the CDI-2 was no longer significant, b = .08, 95% CI [−0.11, 0.38].
Discussion
This study investigated the role of implicit self-esteem as a potential process linking exposure to childhood abuse with depression and suicidal ideation in children and adolescents. We provide novel evidence that children who have experienced abuse exhibit lower implicit self-esteem than children who have never been abused, using a behavioral paradigm that does not rely on self-report. Moreover, lower implicit self-esteem was associated with both depression and suicidal ideation assessed concurrently, as well as with increases in depression and suicidal ideation over a longitudinal follow-up period. Consistent with our hypotheses, lower implicit self-esteem significantly mediated the association of childhood abuse with depression, suicidal ideation, and increases in depression over time. These findings have implications with regard to screening and targets for early interventions aimed at preventing depression and suicidal ideation in children who have been maltreated.
Although prior studies have found that childhood abuse is associated with decreased self-esteem on explicit self-report measures (Bolger et al., 1998; Leeson & Nixon, 2011), we are unaware of previous research examining implicit self-esteem, which captures unconscious and automatic evaluations of the self. We demonstrate that children who experienced abuse had lower implicit self-esteem, indicating a less positive representation of the self. This association persisted after adjusting for other co-occurring forms of adversity—including both neglect and low SES—and was specific, such that low implicit self-esteem was associated with abuse but not to either neglect or low SES. This pattern is broadly consistent with recent conceptual models arguing that the mechanisms linking different forms of childhood adversity—specifically those involving threat and deprivation—with the emergence of psychopathology are at least partially distinct (McLaughlin & Sheridan, 2016; McLaughlin et al., 2014; Sheridan & McLaughlin, 2014). Moreover, these findings extend prior work demonstrating similar specificity in the association of childhood abuse with explicit self-esteem over and above the effects of child neglect (Toth et al., 1992).
Extending this prior work to include implicit measures is important, because measurements of explicit self-esteem rely on self-report, which makes them vulnerable to distortions due to desirability concerns by the participant and dependence on an ability to accurately perceive and report on attitudes about the self. Implicit Association Tests instead focus on unconscious and automatic behavioral responses, tapping into attitudes that may be less vulnerable to reporting biases (Greenwald & Banaji, 1995). Children who have been abused often experience insults and harsh criticism from caregivers, physical and emotional threats, overt physical violence, excessive punishment, and other forms of emotional, physical, and sexual harm (Teicher et al., 2006; Trickett & McBride-Chang, 1995; Wolfe & St. Pierre, 1989). Our examination of different types of abuse suggests that emotional abuse has a particularly strong association with implicit self-esteem. Intense negative feedback from caregivers during childhood and adolescence, a developmental period that is essential for identity formation (Boyes & Chandler, 1992), may have long-lasting negative effects on self-esteem. This pattern is consistent with prior work suggesting that emotional abuse is more strongly related to depression than other forms of abuse (Khan et al., 2015; Teicher et al., 2006). Our findings suggest that childhood abuse—and particularly emotional abuse—is associated with less positive implicit self-representations in childhood and adolescence.
These findings are also consistent with theories that implicit and automatic processes may be influenced by environmental experiences that occur early in development (Cvencek et al., 2016, 2020; DeHart et al., 2006; Greenwald & Banaji, 2017). In contrast, experiences occurring later in development are thought to influence more controlled, deliberate, and explicit processing (e.g., DeHart et al., 2004, 2006; Rudman, 2004; Rudman, Phelan, & Heppen, 2007), such as explicit self-esteem. These early experiences may contribute to lasting, deeply embedded, nonverbal representations of the self as less positive, and additionally may contribute to the emergence of psychopathology.
Given that explicit self-esteem is strongly related to depression symptoms and suicidal ideation, one might expect to find a similar pattern with implicit self-esteem. However, prior research using implicit measures with adults has produced inconsistent findings, with some studies finding an association (Franck, De Raedt, Dereu, & Van den Abbeele, 2007; Wu et al., 2009) but not others (Cai, 2003). To our knowledge, only three studies to date have examined implicit self-esteem longitudinally in relation to depressive symptoms in young children, finding either no relation between implicit self-esteem and depressive symptoms (Cvencek et al., 2020; Leeuwis, Koot, Creemers, & van Lier, 2015), or demonstrating very weak relations between the two (r = .05; van Tuijl et al., 2014). In the present study, we extend this work by showing that lower implicit self-esteem was consistently and moderately associated with depression symptoms and suicidal ideation severity at a baseline, and also moderately predicted increases in depression symptoms and suicidal ideation over time in children and adolescents. Children with less positive representations of the self, as measured by the self-esteem IAT, may experience increased feelings of worthlessness or guilt, which may contribute to higher depression severity. Lower implicit self-esteem may also contribute to attributions that negative events or experiences are the result of internal causes; these types of attributions are a well-established risk factor for depression in children, adolescents, and adults, particularly following exposure to life stressors (Alloy, Abramson, Metalsky, & Hartlage, 1988; Hankin, Abramson, & Siler, 2001; Joiner & Wagner, 1995).
These types of negative attributions have also been found to mediate the association between childhood maltreatment and the onset of depression in adulthood (Gibb et al., 2001), which may be an additional pathway through which lower self-esteem influences risk for depression following childhood abuse. It is important to note, however, that abuse exposure was not significantly associated with depression severity at follow-up assessments after adjusting for baseline levels of depression. This finding is surprising given the strong associations between childhood abuse and psychopathology across the lifespan (Green et al., 2010; McLaughlin et al., 2012). One possibility is that because participants who experienced abuse were already experiencing high levels of depression symptoms at baseline, the possibility for symptom increases was more constrained in these children relative to the children who had not been abused. Another possibility is that the younger participants in the study are aged 10–11 at follow-up, and they have not yet reached an age where risk for depression begins to increases in adolescence (Caspi et al., 2020; Kessler et al., 2005).
The degree to which implicit self-esteem is associated with depression and suicidal ideation above and beyond the role of explicit self-esteem remains unclear. While many studies in adolescents and adults have shown discrepancies between implicit and explicit self-esteem in their relationships to depression and suicidal ideation (e.g., Creemers et al., 2012; Cvencek et al., 2020; Franck, Raedt, & Houwer, 2007), our findings suggest that implicit self-esteem is directly related to both depression symptoms and suicidal ideation. This was true even after removing items on the depression scale that reflect explicit self-esteem and controlling for explicit self-esteem in the analysis. The difference in the pattern of associations in our sample relative to prior research might reflect that our sample was comprised of a high proportion of children who had been maltreated. Our findings suggest that greater research is needed to clarify the links between implicit self-esteem and psychopathology and how those associations might vary across development or as a function of environmental experience.
We also expected to find an association between lower implicit self-esteem and increased suicidal ideation and severity of suicidal ideation. People who have less positive self-representations may be more likely to appraise themselves to be less valuable or worthy and, in turn, more willing to harm themselves. Feeling worthless is one of the symptoms of depression most strongly associated with suicidal thoughts and behaviors (Liu et al., 2006; McGirr et al., 2007) and predicts lifetime suicide attempts in people with histories of trauma exposure (Jeon et al., 2014). Feelings of worthlessness may be an additional process contributing to the link from low implicit self-esteem to suicidal thoughts and behaviors.
We also examined whether lower implicit self-esteem was associated with other forms of psychopathology in addition to depression and suicidal ideation. Contrary to our predictions, we found that lower implicit self-esteem was associated with higher levels of anxiety, externalizing symptoms, and a general psychopathology factor, or p-factor. This suggests that low implicit self-esteem may be a transdiagnostic factor associated with many forms of psychopathology symptoms for children who have experienced abuse in the past. There have been several studies linking lower explicit self-esteem to diverse forms of psychopathology (e.g. Donnellan, Trzesniewski, Robins, Moffitt, & Caspi, 2005; Isomaa et al., 2013; Lee & Hankin, 2009). Lower implicit self-esteem, however, has primarily been associated with depression and suicidal ideation in past research, and has not been explored as a transdiagnostic risk factor.
We found support for lower implicit self-esteem as a mechanism linking childhood abuse to concurrent depression as well as to increases in symptoms of depression across a longitudinal follow-up spanning several years. Although an indirect effect of childhood abuse on suicidal ideation through implicit self-esteem was present in the baseline data, it was only marginally significant at the longitudinal follow-up and thus should be interpreted with caution given the difficulty in disentangling whether implicit self-esteem is predicting suicidal ideation or the reverse when measured concurrently. Prior research suggests that explicit self-esteem contributes to the relationship between childhood abuse and depression and suicidal ideation (Arslan, 2016; Duprey et al., 2019; Greger et al., 2017). We extend this prior work by demonstrating a role for implicit self-esteem as an additional pathway through which experiences of abuse may confer risk for depression and suicidal ideation in children and adolescents. Our mediation analysis also suggests that implicit self-esteem may be a pathway linking childhood abuse exposure to anxiety symptoms in addition to depression and suicidal ideation, but not externalizing symptoms or general psychopathology. This suggests that while implicit self-esteem may be linked to psychopathology transdiagnostically, it may act as a pathway linking childhood abuse to the emergence of internalizing symptoms, including anxiety, depression, and suicidal ideation.
The moderate positive association between age and implicit self-esteem (r = .27) is also noteworthy, because it indicates that, in this sample, older children had moderately higher self-esteem than younger children did. As mentioned earlier, only three studies examined the stability of implicit self-esteem longitudinally in children. One study examined implicit self-esteem in a sample of 11-year-olds over a 1-year follow-up (Leeuwis et al., 2015). The second study examined implicit self-esteem in a sample of 10-to 16-year-olds over a 2-year follow-up (van Tuijl et al., 2014). The third study examined implicit self-esteem in a sample of 5-year-olds over a 4-year follow-up (Cvencek et al., 2020). All three studies found that baseline and follow-up implicit self-esteem were positively correlated (rs ranging from .19 to .34), but no study reported any significant differences in magnitude of implicit self-esteem between baseline and follow-up. Based on the current demonstration of higher implicit self-esteem at older ages we speculate that implicit self-esteem may stay relatively stable during early and middle childhood, and then increase in magnitude during adolescence. This developmental pattern would be similar—but evident earlier—than a pattern obtained in previous research using explicit measures: Explicit self-esteem shows a general decline during late childhood and adolescence, followed by a gradual increase in early adulthood (Robins & Trzesniewski, 2005). The current findings of a gradual increase in implicit self-esteem already during adolescence is compatible with the prior theorizing that implicit self-esteem likely develops (or perhaps stabilizes) prior to the formation of explicit self-esteem (Cvencek et al., 2020; DeHart et al. 2006). Future research is needed to examine these possibilities empirically.
While this study had several strengths, including the large sample of youth who experienced childhood abuse, assessment of suicidal ideation through a structured interview, and the use of well-validated measures of depression and implicit self-esteem, our findings should be interpreted within the context of several limitations. First, we had a restricted range of suicidal ideation and measured suicidal ideation using number of days of suicidal ideation and intensity of suicidal ideation. There are validated measures that are designed specifically to assess suicidal ideation severity, like the Suicidal Ideation Questionnaire (Reynolds & Mazza, 1999), and future studies on may benefit from a stand-alone, well-validated suicidal ideation severity measure. Further, we focused exclusively on suicidal ideation given low reported frequencies of self-injurious behaviors. A future study that includes greater severity of self-injurious thoughts and behaviors may reveal a different pattern of results than the current study. Second, implicit measures may also have some limitations. Prior research has found stronger associations between self and positive compared to self and negative on implicit self-esteem measures in depressed samples (De Raedt et al., 2006), despite low self-esteem as a hallmark feature of depression. We have found this in our sample as well. As De Raedt and colleagues (2006) discussed, this may suggest that explicit and implicit approaches measure differentiable constructs, with implicit self-esteem better predicting automatic, affective processing (Greenwald & Banaji, 1995), and explicit self-esteem better predicting current, effortful, and conscious attitudes (Evans, 2008; see also Cvencek et al., 2016, for further discussion). Finally, this study did not include a stand-alone measure of explicit self-esteem. Though we were able to conduct several sensitivity analyses to examine whether implicit self-esteem was associated uniquely with the development of depression and suicidal ideation using the self-esteem subscale of the CDI-2, there were weaknesses to this method. We were unable to examine how the discrepancies between implicit and explicit self-esteem contributed to psychopathology in our study as our self-esteem measure was a subscale of our depression measure. Future studies on this topic would benefit from a well validated stand-alone measure of explicit self-esteem, such as the Rosenberg Self-esteem Scale (Rosenberg, 1986) of Lifespan Self-esteem Scale (Harris, Donnellan, & Trzesniewski, 2018). Examining congruence or discrepancies between implicit and explicit self-esteem measures—and whether the effect of implicit self-esteem depends on the levels of explicit self-esteem of an child—would be an interesting avenue for future research and may provide further insights into the role of implicit self-esteem in linking childhood abuse to depression and suicidal ideation (see Cvencek et al. 2020).
These findings warrant replication, but they could suggest that higher implicit self-esteem may be a potential protective factor against the development of depression and suicidal ideation following childhood abuse. Interventions designed to improve self-esteem and sense of self-worth in children who have been abused may be an effective strategy for treating psychopathology, particularly depression or suicidal ideation. Brief interventions that teach children that personal characteristics are not fixed but can be developed with effort (i.e., growth mindset; Yeager & Dweck, 2012) reflect one possible strategy for doing so. A one-session intervention of this type had lasting positive effects on depression symptoms in adolescents (Schleider & Weisz, 2018). Incorporating such techniques into existing evidence-based approaches, like trauma-focused cognitive behavioral therapy (Cohen, Mannarino, Berliner, & Deblinger, 2000; Dorsey et al., 2017), could potentially bolster the impact of such treatments on depression and suicidal ideation.
In addition to the potential for implicit self-esteem to be seen as a protective factor against depression and suicidal ideation following childhood abuse, implicit self-esteem may be useful for risk assessment for depression and suicidal ideation in children who have been abused. Recently, implicit measures have gained attention as potentially useful measurements of constructs that are difficult to measure accurately with self-report or clinical interviews, especially in children who may not be adept at intentional introspection and nuanced verbal report of their internal mental life. In particular, measuring suicidal thoughts and behaviors without relying on explicit reporting may have immense utility as a risk assessment tool, inasmuch as people are often hesitant to report suicidal thoughts or behaviors. The Death IAT, an Implicit Association Test in which participants sort self-other words with words associated with life and death, was developed to address this issue (Nock & Banaji, 2007). Research showing the predictive ability of the Death IAT to identify patients at risk of future suicide attempts points to implicit measures as potential markers of objective risk (Nock et al., 2010), although findings have been inconsistent across studies (Millner et al., 2019). While the self-esteem Child IAT (Cvencek et al., 2016) has not yet formally been used as a risk assessment tool, it is possible that this implicit measure may be able to detect suicidal ideation and link child abuse with suicidal ideation. Given that negative evaluations of the self can occur outside of conscious awareness and are captured by measures other than self-report, weaker unconscious me = good associations may signal that an individual is at greater risk of contemplating suicide even if individuals are unwilling (or unable) to verbally report their potential consideration of self-harm. The measurement of implicit self-esteem in child clinical samples may thus provide useful insight about risk of suicidal ideation during early development, and discrepancies between implicit and explicit forms of self-esteem, as well as the change in such discrepancies over time, may be particularly informative (Cvencek et al., 2020).
In conclusion, our findings suggest that low implicit self-esteem may be a pathway linking childhood abuse to depression and suicidal ideation. Lower self-esteem resulting from harsh punishment, physical or verbal threats, and violent behaviors from caregivers in childhood may increase risk for depressive symptoms and suicidal ideation. These findings suggest the value of further research into how implicit self-esteem may be used as a behavioral marker of risk for depression or suicidal ideation in children and adolescents, particularly those who have experienced childhood abuse, as well as a target for interventions aimed at preventing psychopathology among children who have been abused.
Supplementary Material
Acknowledgements
This research was funded by the National Institute of Mental Health (R01-MH103291 to McLaughlin; K01MH116325 to Miller), an Early Career Research Fellowship from the Jacobs Foundation (McLaughlin), a OneMind Institute Rising Star Award (McLaughlin), and the University of Washington I-LABS Innovative Research Fund (Meltzoff).
Footnotes
The authors declare that they have no conflict of interest.
References
- Achenbach T.(1991). Manual for the Child Behavior Checklist/4–18 and 1991 profile. University of Vermont, Department of Psychiatry. [Google Scholar]
- Alloy LB, Abramson LY, Metalsky GI, & Hartlage S.(1988). The hopelessness theory of depression: Attributional aspects. The British Journal of Clinical Psychology, 27(1), 5–21. 10.1111/j.2044-8260.1988.tb00749.x [DOI] [PubMed] [Google Scholar]
- Arslan G.(2016). Psychological maltreatment, emotional and behavioral problems in adolescents: The mediating role of resilience and self-esteem. Child Abuse & Neglect, 52, 200–209. 10.1016/j.chiabu.2015.09.010 [DOI] [PubMed] [Google Scholar]
- Ben-Shachar Makowski & Lüdecke (2020). Compute and interpret indices of effect size. Available from https://github.com/easystats/effectsize. [Google Scholar]
- Bernstein DP, Ahluvalia T, Pogge D, & Handelsman L.(1997). Validity of the Childhood Trauma Questionnaire in an adolescent psychiatric population. Journal of the American Academy of Child & Adolescent Psychiatry, 36(3), 340–348. 10.1097/00004583-199703000-00012 [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, Sapareto E, & Ruggiero J.(1994). Initial reliability and validity of a new retrospective measure of child abuse and neglect. The American Journal of Psychiatry, 151(8), 1132–1136. 10.1176/ajp.151.8.1132 [DOI] [PubMed] [Google Scholar]
- Bhar S, Ghahramanlou-Holloway M, Brown G, & Beck AT (2008). Self-esteem and suicide ideation in psychiatric outpatients. Suicide and Life-Threatening Behavior, 38(5), 511–516. 10.1521/suli.2008.38.5.511 [DOI] [PubMed] [Google Scholar]
- Bifulco A, Bernazzani O, Moran PM, & Jacobs C.(2005). The Childhood Experience of Care and Abuse Questionnaire (CECA.Q): Validation in a community series. British Journal of Clinical Psychology, 44(4), 563–581. 10.1348/014466505X35344 [DOI] [PubMed] [Google Scholar]
- Bifulco A, Brown GW, & Harris TO (1994). Childhood Experience of Care and Abuse (CECA): A retrospective interview measure. Journal of Child Psychology and Psychiatry, 35(8), 1419–1435. 10.1111/j.1469-7610.1994.tb01284.x [DOI] [PubMed] [Google Scholar]
- Bifulco A, Brown GW, Lillie A, & Jarvis J.(1997). Memories of childhood neglect and abuse: Corroboration in a series of sisters. Journal of Child Psychology and Psychiatry, 38(3), 365–374. 10.1111/j.1469-7610.1997.tb01520.x [DOI] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, & Baugher M.(1999). Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): A replication study. Journal of the American Academy of Child & Adolescent Psychiatry, 38(10), 1230–1236. 10.1097/00004583-199910000-00011 [DOI] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, & Neer SM (1997). The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child & Adolescent Psychiatry, 36(4), 545–553. 10.1097/00004583-199704000-00018 [DOI] [PubMed] [Google Scholar]
- Blascovich J, & Tomaka J.(1991). Measures of self-esteem. In Robinson JP, Shaver PR, & Wrightman LS (Eds.), Measures of personality and social psychological attitudes (pp.115–160). Academic Press. 10.1016/B978-0-12-590241-0.50008-3 [DOI] [Google Scholar]
- Bolger KE, Patterson CJ, & Kupersmidt JB (1998). Peer relationships and self-esteem among children who have been maltreated. Child Development, 69(4), 1171–1197. 10.2307/1132368 [DOI] [PubMed] [Google Scholar]
- Bosson JK, Brown RP, Zeigler-Hill V, & Swann WB Jr. (2003). Self-enhancement tendencies among people with high explicit self-esteem: The moderating role of implicit self-esteem. Self & Identity, 2(3), 169–187. 10.1080/15298860309029 [DOI] [Google Scholar]
- Boyes MC, & Chandler M.(1992). Cognitive development, epistemic doubt, and identity formation in adolescence. Journal of Youth and Adolescence, 21(3), 277–304. 10.1007/BF01537019 [DOI] [PubMed] [Google Scholar]
- Briere J, & Rickards S.(2007). Self-awareness, affect regulation, and relatedness: Differential sequels of childhood versus adult victimization experiences. The Journal of Nervous and Mental Disease, 195(6), 497–503. 10.1097/NMD.0b013e31803044e2 [DOI] [PubMed] [Google Scholar]
- Cai H.(2003). Explicit self-esteem, implicit self-esteem and depression. Chinese Mental Health Journal, 17(5), 331–336. [Google Scholar]
- Caspi A, Houts RM, Ambler A, Danese A, Elliott ML, Hariri A, Harrington H, Hogan S, Poulton R, Ramrakha S, Rasmussen LJH, Reuben A, Richmond-Rakerd L, Sugden K, Wertz J, Williams BS, & Moffitt TE (2020). Longitudinal assessment of mental health disorders and comorbidities across 4 decades among participants in the Dunedin Birth Cohort Study. JAMA Network Open, 3(4), e203221– e203221. 10.1001/jamanetworkopen.2020.3221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, Meier MH, Ramrakha S, Shalev I, Poulton R, & Moffitt TE (2014). The p factor: One general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science, 2(2), 119–137. 10.1177/2167702613497473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambers JM (1992). Linear models. In Chambers JM & Hastie TJ (Eds.), Statistical models in S (pp. 95–144). Wadsworth: & Brooks/Cole. [Google Scholar]
- Cohen JA, Mannarino AP, Berliner L, & Deblinger E.(2000). Trauma-focused cognitive behavioral therapy for children and adolescents: An empirical update. Journal of Interpersonal Violence, 15(11), 1202–1223. 10.1177/088626000015011007 [DOI] [Google Scholar]
- Creemers DHM, Scholte RHJ, Engels RCME, Prinstein MJ, & Wiers RW (2012). Implicit and explicit self-esteem as concurrent predictors of suicidal ideation, depressive symptoms, and loneliness. Journal of Behavior Therapy and Experimental Psychiatry, 43(1), 638–646. 10.1016/j.jbtep.2011.09.006 [DOI] [PubMed] [Google Scholar]
- Cvencek D, Greenwald AG, Brown AS, Gray NS, & Snowden RJ (2010). Faking of the Implicit Association Test is statistically detectable and partly correctable. Basic and Applied Social Psychology, 32(4), 302–314. 10.1080/01973533.2010.519236 [DOI] [Google Scholar]
- Cvencek D, Greenwald AG, McLaughlin KA, & Meltzoff AN (2020). Early implicit– explicit discrepancies in self-esteem as correlates of childhood depressive symptoms. Journal of Experimental Child Psychology, 200, 104962. 10.1016/j.jecp.2020.104962 [DOI] [PubMed] [Google Scholar]
- Cvencek D, Greenwald AG, & Meltzoff AN (2016). Implicit measures for preschool children confirm self-esteem’s role in maintaining a balanced identity. Journal of Experimental Social Psychology, 62, 50–57. 10.1016/j.jesp.2015.09.015 [DOI] [Google Scholar]
- Cvencek D, Meltzoff AN, & Greenwald AG (2011). Math–gender stereotypes in elementary school children. Child Development, 82(3), 766–779. 10.1111/j.1467-8624.2010.01529.x [DOI] [PubMed] [Google Scholar]
- De Raedt R, Schacht R, Franck E, & De Houwer J.(2006). Self-esteem and depression revisited: Implicit positive self-esteem in depressed patients? Behaviour Research and Therapy, 44(7), 1017–1028. 10.1016/j.brat.2005.08.003 [DOI] [PubMed] [Google Scholar]
- DeHart T, Pelham B, & Murray S.(2004). Implicit dependency regulation: Self-esteem, relationship closeness, and implicit evaluations of close others. Social Cognition, 22(1), 126–146. 10.1521/soco.22.1.126.30986 [DOI] [Google Scholar]
- DeHart T, Pelham BW, & Tennen H.(2006). What lies beneath: Parenting style and implicit self-esteem. Journal of Experimental Social Psychology, 42(1), 1–17. 10.1016/j.jesp.2004.12.005 [DOI] [Google Scholar]
- Donnellan MB, Trzesniewski KH, Robins RW, Moffitt TE, & Caspi A.(2005). Low self-esteem is related to aggression, antisocial behavior, and delinquency. Psychological Science, 16(4), 328–335. 10.1111/j.0956-7976.2005.01535.x [DOI] [PubMed] [Google Scholar]
- Dorsey S, McLaughlin KA, Kerns SEU, Harrison JP, Lambert HK, Briggs EC, Cox JR, & Amaya-Jackson L.(2017). Evidence base update for psychosocial treatments for children and adolescents exposed to traumatic events. Journal of Clinical Child & Adolescent Psychology, 46(3), 303–330. 10.1080/15374416.2016.1220309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn EC, McLaughlin KA, Slopen N, Rosand J, & Smoller JW (2013). Developmental timing of child maltreatment and symptoms of depression and suicidal ideation in young adulthood: Results from the National Longitudinal Study of Adolescent Health. Depression and Anxiety, 30(10), 955–964. 10.1002/da.22102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duprey EB, Oshri A, & Liu S.(2019). Childhood maltreatment, self-esteem, and suicidal ideation in a low-SES emerging adult sample: The moderating role of heart rate variability. Archives of Suicide Research, 23(2), 333–352. 10.1080/13811118.2018.1430640 [DOI] [PubMed] [Google Scholar]
- Evans JSBT (2008). Dual-processing accounts of reasoning, judgment, and social cognition. Annual Review of Psychology, 59, 255–278. 10.1146/annurev.psych.59.103006.093629 [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Hamby SL, Ormrod R, & Turner H.(2005). The Juvenile Victimization Questionnaire: Reliability, validity, and national norms. Child Abuse & Neglect, 29(4), 383–412. 10.1016/j.chiabu.2004.11.001 [DOI] [PubMed] [Google Scholar]
- Franck E, De Raedt R, Dereu M, & Van den Abbeele D.(2007). Implicit and explicit self-esteem in currently depressed individuals with and without suicidal ideation. Journal of Behavior Therapy and Experimental Psychiatry, 38(1), 75–85. 10.1016/j.jbtep.2006.05.003 [DOI] [PubMed] [Google Scholar]
- Franck E, De Raedt R, & De Houwer J.(2007). Implicit but not explicit self-esteem predicts future depressive symptomatology. Behaviour Research and Therapy, 45(10), 2448– 2455. 10.1016/j.brat.2007.01.008 [DOI] [PubMed] [Google Scholar]
- Gibb BE, Alloy LB, Abramson LY, Rose DT, Whitehouse WG, Donovan P, Hogan ME, Cronholm J, & Tierney S.(2001). History of childhood maltreatment, negative cognitive styles, and episodes of depression in adulthood. Cognitive Therapy and Research, 25(4), 425–446. 10.1023/A:1005586519986 [DOI] [Google Scholar]
- Glenn CR, Kleiman EM, Coppersmith DDL, Santee AC, Esposito EC, Cha CB, Nock MK, & Auerbach RP (2017). Implicit identification with death predicts change in suicide ideation during psychiatric treatment in adolescents. Journal of Child Psychology and Psychiatry, 58(12), 1319–1329. 10.1111/jcpp.12769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, & Kessler RC (2010). Childhood adversities and adult psychiatric disorders in the National Comorbidity Survey Replication I: Associations with first onset of DSM-IV disorders. Archives of General Psychiatry, 67(2), 113–123. 10.1001/archgenpsychiatry.2009.186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwald AG, & Banaji MR (1995). Implicit social cognition: Attitudes, self-esteem, and stereotypes. Psychological Review, 102(1), 4–27. 10.1037/0033-295X.102.1.4 [DOI] [PubMed] [Google Scholar]
- Greenwald AG, & Banaji MR (2017). The implicit revolution: Reconceiving the relation between conscious and unconscious. American Psychologist, 72(9), 861–871. 10.1037/amp0000238 [DOI] [PubMed] [Google Scholar]
- Greenwald AG, & Farnham SD (2000). Using the Implicit Association Test to measure self-esteem and self-concept. Journal of Personality and Social Psychology, 79(6), 1022–1038. 10.1037/0022-3514.79.6.1022 [DOI] [PubMed] [Google Scholar]
- Greenwald AG, Nosek BA, & Banaji MR (2003). Understanding and using the Implicit Association Test: I. An improved scoring algorithm. Journal of Personality and Social Psychology, 85(2), 197–216. 10.1037/0022-3514.85.2.197 [DOI] [PubMed] [Google Scholar]
- Greger HK, Myhre AK, Klöckner CA, & Jozefiak T.(2017). Childhood maltreatment, psychopathology and well-being: The mediator role of global self-esteem, attachment difficulties and substance use. Child Abuse & Neglect, 70, 122–133. 10.1016/j.chiabu.2017.06.012 [DOI] [PubMed] [Google Scholar]
- Gross AB, & Keller HR (1992). Long-term consequences of childhood physical and psychological maltreatment. Aggressive Behavior, 18(3), 171–185. [DOI] [Google Scholar]
- Haeffel GJ, Abramson LY, Brazy PC, Shah JY, Teachman BA, & Nosek BA (2007). Explicit and implicit cognition: A preliminary test of a dual-process theory of cognitive vulnerability to depression. Behaviour Research and Therapy, 45(6), 1155–1167. 10.1016/j.brat.2006.09.003 [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, & Siler M.(2001). A prospective test of the hopelessness theory of depression in adolescence. Cognitive Therapy and Research, 25(5), 607–632. 10.1023/A:1005561616506 [DOI] [Google Scholar]
- Harris MA, Donnellan MB, & Trzesniewski KH (2018). The Lifespan Self-Esteem Scale: Initial validation of a new measure of global self-esteem. Journal of Personality Assessment, 100(1), 84–95. 10.1080/00223891.2016.1278380 [DOI] [PubMed] [Google Scholar]
- Hayes AF (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford publications. [Google Scholar]
- Isomaa R, Väänänen J-M, Fröjd S, Kaltiala-Heino R, & Marttunen M.(2013). How low is low? Low self-esteem as an indicator of internalizing psychopathology in adolescence. Health Education & Behavior, 40(4), 392–399. 10.1177/1090198112445481 [DOI] [PubMed] [Google Scholar]
- Jeon HJ, Park J-I, Fava M, Mischoulon D, Sohn JH, Seong S, Park JE, Yoo I, & Cho MJ (2014). Feelings of worthlessness, traumatic experience, and their comorbidity in relation to lifetime suicide attempt in community adults with major depressive disorder. Journal of Affective Disorders, 166, 206–212. 10.1016/j.jad.2014.05.010 [DOI] [PubMed] [Google Scholar]
- Joiner TE, & Wagner KD (1995). Attribution style and depression in children and adolescents: A meta-analytic review. Clinical Psychology Review, 15(8), 777–798. 10.1016/0272-7358(95)00046-1 [DOI] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Kessler RC, McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Aguilar-Gaxiola S, Alhamzawi AO, Alonso J, Angermeyer M, Benjet C, Bromet E, Chatterji S, de Girolamo G, Demyttenaere K, Fayyad J, Florescu S, Gal G, Gureje O, Williams DR (2010). Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. The British Journal of Psychiatry, 197(5), 378–385. 10.1192/bjp.bp.110.080499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan A, McCormack HC, Bolger EA, McGreenery CE, Vitaliano G, Polcari A, & Teicher MH (2015). Childhood maltreatment, depression, and suicidal ideation: Critical importance of parental and peer emotional abuse during developmental sensitive periods in males and females. Frontiers in Psychiatry, 6, Article 42. 10.3389/fpsyt.2015.00042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M.(2011). Children’s Depression Inventory 2nd edition (CDI 2): Technical manual. Multi-Health Systems. [Google Scholar]
- Laceulle OM, Vollebergh WAM, & Ormel J.(2015). The structure of psychopathology in adolescence: Replication of a general psychopathology factor in the TRAILS Study. Clinical Psychological Science, 3(6), 850–860. 10.1177/2167702614560750 [DOI] [Google Scholar]
- Lee A, & Hankin BL (2009). Insecure attachment, dysfunctional attitudes, and low self-esteem predicting prospective symptoms of depression and anxiety during adolescence. Journal of Clinical Child & Adolescent Psychology, 38(2), 219–231. 10.1080/15374410802698396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeson FJ, & Nixon RDV (2011). The role of children’s appraisals on adjustment following psychological maltreatment: A pilot study. Journal of Abnormal Child Psychology, 39(5), 759–771. 10.1007/s10802-011-9507-5 [DOI] [PubMed] [Google Scholar]
- Leeuwis FH, Koot HM, Creemers DHM, & van Lier PAC (2015). Implicit and explicit self-esteem discrepancies, victimization and the development of late childhood internalizing problems. Journal of Abnormal Child Psychology, 43(5), 909–919. 10.1007/s10802-014-9959-5 [DOI] [PubMed] [Google Scholar]
- Liu X, Gentzler AL, Tepper P, Kiss E, Kothencnè VO, Tamás Z, Vetró Á, & Kovacs M.(2006). Clinical features of depressed children and adolescents with various forms of suicidality. The Journal of Clinical Psychiatry, 67(9), 1442–1450. 10.4088/JCP.v67n0917 [DOI] [PubMed] [Google Scholar]
- McGirr A, Renaud J, Seguin M, Alda M, Benkelfat C, Lesage A, & Turecki G.(2007). An examination of DSM-IV depressive symptoms and risk for suicide completion in major depressive disorder: A psychological autopsy study. Journal of Affective Disorders, 97(1), 203–209. 10.1016/j.jad.2006.06.016 [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, & Kessler RC (2012). Childhood adversities and first onset of psychiatric disorders in a national sample of US adolescents. Archives of General Psychiatry, 69(11), 1151–1160. 10.1001/archgenpsychiatry.2011.2277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, & Sheridan MA (2016). Beyond cumulative risk: A dimensional approach to childhood adversity. Current Directions in Psychological Science, 25(4), 239–245. 10.1177/0963721416655883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Sheridan MA, & Lambert HK (2014). Childhood adversity and neural development: Deprivation and threat as distinct dimensions of early experience. Neuroscience & Biobehavioral Reviews, 47, 578–591. 10.1016/j.neubiorev.2014.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AB, Esposito-Smythers C, Weismoore JT, & Renshaw KD (2013). The relation between child maltreatment and adolescent suicidal behavior: A systematic review and critical examination of the literature. Clinical Child and Family Psychology Review, 16(2), 146–172. 10.1007/s10567-013-0131-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AB, Linthicum KP, Helms SW, Giletta M, Rudolph KD, Hastings PD, Nock MK, & Prinstein MJ (2018). Reciprocal associations between adolescent girls’ chronic interpersonal stress and nonsuicidal self-injury: A multi-wave prospective investigation. Journal of Adolescent Health, 63(6), 694–700. 10.1016/j.jadohealth.2018.06.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millner AJ, Augenstein TM, Visser KH, Gallagher K, Vergara GA, D’Angelo EJ, & Nock MK (2019). Implicit cognitions as a behavioral marker of suicide attempts in adolescents. Archives of Suicide Research, 23(1), 47–63. 10.1080/13811118.2017.1421488 [DOI] [PubMed] [Google Scholar]
- Nanni V, Uher R, & Danese A.(2012). Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: A meta-analysis. The American Journal of Psychiatry, 169(2), 141–151. 10.1176/appi.ajp.2011.11020335 [DOI] [PubMed] [Google Scholar]
- Nock MK, & Banaji MR (2007). Prediction of suicide ideation and attempts among adolescents using a brief performance-based test. Journal of Consulting and Clinical Psychology, 75(5), 707–715. 10.1037/0022-006X.75.5.707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Holmberg EB, Photos VI, & Michel BD (2007). Self-Injurious Thoughts and Behaviors Interview: Development, reliability, and validity in an adolescent sample. Psychological Assessment, 19(3), 309–317. 10.1037/1040-3590.19.3.309 [DOI] [PubMed] [Google Scholar]
- Nock MK, Park JM, Finn CT, Deliberto TL, Dour HJ, & Banaji MR (2010). Measuring the suicidal mind: Implicit cognition predicts suicidal behavior. Psychological Science, 21(4), 511–517. 10.1177/0956797610364762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman RE, Byambaa M, De R, Butchart A, Scott J, & Vos T.(2012). The long-term health consequences of child physical abuse, emotional abuse, and neglect: A systematic review and meta-analysis. PLOS Medicine, 9(11), Article e1001349. 10.1371/journal.pmed.1001349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuttin JM (1985). Narcissism beyond Gestalt and awareness: The name letter effect. European Journal of Social Psychology, 15(3), 353–361. 10.1002/ejsp.2420150309 [DOI] [Google Scholar]
- Paulhus DL (1991). Measurement and control of response bias. In Robinson JP, Shaver PR, & Wrightman LS (Eds.), Measures of personality and social psychological attitudes (pp. 17–59). Academic Press. 10.1016/B978-0-12-590241-0.50006-X [DOI] [Google Scholar]
- Paulhus DL (2002). Socially desirable responding: The evolution of a construct. In Braun HI, Jackson DN, & Wiley DE (Eds.), The role of constructs in psychological and educational measurement (pp. 49–69). Lawrence Erlbaum Associates Publishers. [Google Scholar]
- Reynolds WM (1994). Assessment of depression in children and adolescents by self-report questionnaires. In Reynolds WM & Johnston HF (Eds.), Handbook of depression in children and adolescents (pp. 209–234). Springer. [Google Scholar]
- Reynolds WM, & Mazza JJ (1999). Assessment of Suicidal Ideation in Inner-City Children and Young Adolescents: Reliability and Validity of the Suicidal Ideation Questionnaire-JR. School Psychology Review, 28(1), 17–30. 10.1080/02796015.1999.12085945 [DOI] [Google Scholar]
- Robins RW, & Trzesniewski KH (2005). Self-esteem development across the lifespan. Current Directions in Psychological Science, 14(3), 158–162. 10.1111/j.0963-7214.2005.00353.x [DOI] [Google Scholar]
- Rosenberg M.(1965). Society and the adolescent self-image. Princeton University Press. [Google Scholar]
- Rosenberg M.(1986). Conceiving the self. R. E. Krieger. [Google Scholar]
- Rudman LA (2004). Sources of implicit attitudes. Current Directions in Psychological Science, 13(2), 79–82. 10.1111/j.0963-7214.2004.00279.x [DOI] [Google Scholar]
- Rudman LA, Phelan JE, & Heppen JB (2007). Developmental sources of implicit attitudes. Personality and Social Psychology Bulletin, 33(12), 1700–1713. 10.1177/0146167207307487 [DOI] [PubMed] [Google Scholar]
- Schleider J, & Weisz J.(2018). A single‐session growth mindset intervention for adolescent anxiety and depression: 9‐month outcomes of a randomized trial. Journal of Child Psychology and Psychiatry, 59(2), 160–170. 10.1111/jcpp.12811 [DOI] [PubMed] [Google Scholar]
- Sheridan MA, & McLaughlin KA (2014). Dimensions of early experience and neural development: Deprivation and threat. Trends in Cognitive Sciences, 18(11), 580–585. 10.1016/j.tics.2014.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg AM, Brymer MJ, Decker KB, & Pynoos RS (2004). The University of California at Los Angeles post-traumatic stress disorder reaction index. Current Psychiatry Reports, 6(2), 96–100. 10.1007/s11920-004-0048-2 [DOI] [PubMed] [Google Scholar]
- Steinberg AM, Brymer MJ, Kim S, Briggs EC, Ippen CG, Ostrowski SA, Gully KJ, & Pynoos RS (2013). Psychometric properties of the UCLA PTSD reaction index: Part I. Journal of Traumatic Stress, 26(1), 1–9. 10.1002/jts.21780 [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Finkelhor D, Moore DW, & Runyan D.(1998). Identification of child maltreatment with the Parent-Child Conflict Tactics Scales: Development and psychometric data for a national sample of American parents. Child Abuse & Neglect, 22(4), 249–270. 10.1016/s0145-2134(97)00174-9 [DOI] [PubMed] [Google Scholar]
- Teicher MH, Samson JA, Polcari A, & McGreenery CE (2006). Sticks, stones, and hurtful words: Relative effects of various forms of childhood maltreatment. American Journal of Psychiatry, 163(6), 993–1000. 10.1176/appi.ajp.163.6.993 [DOI] [PubMed] [Google Scholar]
- Tingley D, Yamamoto T, Hirose K, Keele L, & Imai K.(2014). Mediation: R package for causal mediation analysis. Journal of Statistical Software, 59(5). 10.18637/jss.v059.i05 [DOI] [Google Scholar]
- Toth SL, Manly JT, & Cicchetti D.(1992). Child maltreatment and vulnerability to depression. Development and Psychopathology, 4(1), 97–112. 10.1017/S0954579400005587 [DOI] [Google Scholar]
- Trickett PK, & McBride-Chang C.(1995). The developmental impact of different forms of child abuse and neglect. Developmental Review, 15(3), 311–337. 10.1006/drev.1995.1012 [DOI] [Google Scholar]
- van Tuijl LA, de Jong PJ, Sportel BE, de Hullu E, & Nauta MH (2014). Implicit and explicit self-esteem and their reciprocal relationship with symptoms of depression and social anxiety: A longitudinal study in adolescents. Journal of Behavior Therapy and Experimental Psychiatry, 45(1), 113–121. 10.1016/j.jbtep.2013.09.007 [DOI] [PubMed] [Google Scholar]
- Venables WN, & Ripley BD (2002). Modern applied statistics with S (4th ed.). Springer. [Google Scholar]
- Walker EA, Unutzer J, Rutter C, Gelfand A, Saunders K, VonKorff M, Koss MP, & Katon W.(1999). Costs of health care use by women HMO members with a history of childhood abuse and neglect. Archives of General Psychiatry, 56(7), 609–613. 10.1001/archpsyc.56.7.609 [DOI] [PubMed] [Google Scholar]
- Weissman DG, Bitran D, Miller AB, Schaefer JD, Sheridan MA, & McLaughlin KA (2019). Difficulties with emotion regulation as a transdiagnostic mechanism linking child maltreatment with the emergence of psychopathology. Development and Psychopathology, 31(3), 899–915. 10.1017/S0954579419000348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfe DA, & Pierre J St..(1989). Child abuse and neglect. In Ollendick TH & Hersen M.(Eds.), Handbook of child psychopathology (pp. 377–398). Springer. [Google Scholar]
- Wu M, Sun X, Geng K, & Ding Y.(2009). Stress-buffering effects of implicit self-esteem stability in a sample of adolescents. Psychological Science (China), 32, 1321–1324. [Google Scholar]
- Yeager DS, & Dweck CS (2012). Mindsets that promote resilience: When students believe that personal characteristics can be developed. Educational Psychologist, 47(4), 302–314. 10.1080/00461520.2012.722805 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.