In this multi-institutional study of 9 Level 1 Pediatric Trauma Centers, there was an increased risk of pediatric injury during the first 6 months of the COVID-19 pandemic, with the most socially vulnerable children at greater risk of intentional injury.
KEY WORDS: Pediatric injury, COVID-19, social vulnerability, intentional injury, time series
BACKGROUND
The impact of the COVID-19 pandemic on pediatric injury, particularly relative to a community's vulnerability, is unknown. The objective of this study was to describe the change in pediatric injury during the first 6 months of the COVID-19 pandemic compared with prior years, focusing on intentional injury relative to the social vulnerability index (SVI).
METHODS
All patients younger than 18 years meeting inclusion criteria for the National Trauma Data Bank between January 1, 2016, and September 30, 2020, at nine Level I pediatric trauma centers were included. The COVID cohort (children injured in the first 6 months of the pandemic) was compared with an averaged historical cohort (corresponding dates, 2016–2019). Demographic and injury characteristics and hospital-based outcomes were compared. Multivariable logistic regression was used to estimate the adjusted odds of intentional injury associated with SVI, moderated by exposure to the pandemic. Interrupted time series analysis with autoregressive integrated moving average modeling was used to predict expected injury patterns. Volume trends and observed versus expected rates of injury were analyzed.
RESULTS
There were 47,385 patients that met inclusion criteria, with 8,991 treated in 2020 and 38,394 treated in 2016 to 2019. The COVID cohort included 7,068 patients and the averaged historical cohort included 5,891 patients (SD, 472), indicating a 20% increase in pediatric injury (p = 0.031). Penetrating injuries increased (722 [10.2%] COVID vs. 421 [8.0%] historical; p < 0.001), specifically firearm injuries (163 [2.3%] COVID vs. 105 [1.8%] historical; p = 0.043). Bicycle collisions (505 [26.3%] COVID vs. 261 [18.2%] historical; p < 0.001) and collisions on other land transportation (e.g., all-terrain vehicles) (525 [27.3%] COVID vs. 280 [19.5%] historical; p < 0.001) also increased. Overall, SVI was associated with intentional injury (odds ratio, 7.9; 95% confidence interval, 6.5–9.8), a relationship which increased during the pandemic.
CONCLUSION
Pediatric injury increased during the pandemic across multiple sites and states. The relationship between increased vulnerability and intentional injury increased during the pandemic.
LEVEL OF EVIDENCE
Prognostic and Epidemiological; Level III.
The SARS-CoV-2 (COVID-19) pandemic impacted children and their families across the globe, leading to unparalleled changes in lifestyle. The United States declared a state of national emergency on March 13, 2020, and stay-at-home orders were issued regionally in the subsequent weeks.1 These orders changed the daily lives of children across the nation as they no longer had access to schools, parks, and local community support programs. Simultaneously, as the United States reached an unemployment rate of 13%, many families experienced job loss and financial hardship.2
While hospital admissions at children's hospitals for medical conditions decreased the initial weeks of the pandemic, reports of pediatric injury varied, and the vast majority have been limited to single centers, single mechanisms of injury, or to emergency department (ED) visits alone.3–9 Furthermore, children are a vulnerable population and are at increased risk for poor health outcomes and violent injury when their social determinants of health are suboptimal.10–14 How the COVID-19 pandemic affected pediatric trauma and the relationship between social vulnerability and intentional injury in children has not been explored.
This study aims to compare pediatric injury during the first 6 months of the pandemic to historical controls; additionally, we sought to explore the association between intentional injury and social vulnerability and how that relationship changed in the setting of the pandemic. We hypothesized the COVID pandemic would be associated with a change in both pediatric injury mechanisms and intent. Furthermore, we hypothesized that there would be an increase in the strength of association between social vulnerability and intentional injury.
PATIENTS AND METHODS
Study Design, Setting, and Participants
Data were merged from institutional trauma registries at nine Level I pediatric trauma centers (PTCs) participating in the Midwest Pediatric Surgery Consortium (http://www.mwpsc.org) for the period from January 1, 2016, to September 30, 2020. All children younger than 18 years who met the National Trauma Data Bank (NTDB) criteria were included.15 Namely, these children sustained a traumatic injury within 14 days of the initial hospital encounter with at least one of the following International Classification of Disease, Tenth Revision (ICD-10) diagnosis codes documented: ICD-10-CM S00-S99, T07, T14, T20-T28, T30-T32, and T79.A1-T79.A9. To be included, the child had to be transferred and/or admitted to the hospital, or have died from their injuries.15 The study was approved by each institution's institutional review board with a waiver of consent. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines were followed for this observational cohort study (Supplementary Digital Content, http://links.lww.com/TA/C571).
Variables and Statistical Methods
Trends of overall pediatric injury volume and mechanism of injury were analyzed from the beginning of the study period, January 1, 2016, through the first 6 months of the pandemic, ending on September 30, 2020. The primary exposure of interest was the COVID-19 pandemic. Patients were assigned to the “COVID cohort” if they were injured after the start date of stay-at-home orders (or safer-at-home orders) associated with each site's region, as this was when the daily life of children began to change. The COVID cohort was compared with a historical cohort. To account for the possibility of outlying data from a single year, the historical cohort was averaged across years 2016 to 2019, using data from corresponding dates of the COVID cohort. A sensitivity analysis was completed comparing the COVID cohort to a 2019 cohort alone to evaluate the change between the exposed cohort to the nearest year prior, thus minimizing the effect of temporal changes (e.g., triage patterns, population changes, etc.) and is provided in eTables 1 and 2, http://links.lww.com/TA/C572. Demographic, injury characteristics, and outcomes were compared between cohorts. Injury type, mechanism, and intent were defined by the primary ICD-10 External Cause of Injury codes (E-codes). Outcomes included mortality, hospital disposition, intensive care unit (ICU) and hospital length of stay (LOS), and days on mechanical ventilation.
The relationship between the pandemic and intentional injury based on a child's “vulnerability,” as described by their geocoded social vulnerability index (SVI), was explored. The Agency for Toxic Substances and Disease Registry's Geospatial Research, Analysis & Services Program created the Centers for Disease Control and Prevention SVI, a metric that reflects the degree to which a community exhibits certain social conditions that may weaken their ability to prevent human suffering during times of external stress.16 The SVI ranks each census tract on 15 social factors compromising four subthemes: socioeconomic status, household composition and disability, minority status and language, and housing and transportation. The SVI tract rankings are based on percentiles and range from 0 to 1, with 1 indicating greatest vulnerability. Because SVI is assigned at the census tract level, a weighted value for zip code areas was created based on the relative proportion of residential addresses in the census tracts intercepting with each zip code.12 We investigated the association between SVI and its subthemes and intentional injury, as compared with unintentional injury, and the impact of the pandemic on these associations.
Raw and cumulative numbers of pediatric injuries averaged by month were presented. Day to day variation data were displayed with LOESS smoothing techniques. A two-sample Komogorov-Smirnov test comparing the two cohorts was performed. In addition, interrupted time series analysis with autoregressive integrated moving average modeling was used to estimate the expected pediatric injury during the pandemic while controlling for temporal variation.17 This was graphed against the observed trauma volume during the first 6 months of the pandemic, and a two-sample Kolmogorov-Smirnov test was used to test significance. For the time series analyses, an averaged date of March 23, 2020, was used as there was slight variation in Stay at Home and Safer at Home initiation dates between sites.
Descriptive statistics are presented for each cohort. Data were missing for key variables in less than 5% of cases, and are presented if missingness accounts for 5% or more of the variable. Pearson χ2 was used to compare categorical variables, and when significant a comparison of binomial proportions was utilized when more than two groups where present and then provided in the text. Student's t test and Wilcoxon rank-sum were used to compare mean values for normally distributed continuous variables and median values for non-parametric continuous variables, respectively. Fisher's exact tests were used if any category had less than 5 observations. Two-tailed significance was set at p less than 0.05.
To explore the relationship between the pandemic period and intentional injury (dichotomized and compared with unintentional injury), univariate logistic regression and multivariable logistic regression while controlling for clustering by hospital site were completed. To understand if the relationship between SVI and intentional injury was moderated by the pandemic, the COVID period and SVI was used as an interaction term. All analyses were performed using R statistical software (RStudio, version 1.4.1717 2009–2021 RStudio, PBC).18–24
RESULTS
Participants
Overall, 47,385 patients met inclusion criteria, 8,991 treated in 2020 and 38,394 treated in 2016 to 2019. The COVID cohort, limited to the pandemic period, included 7,068 patients. The averaged historical cohort for the matched time frame from years 2016 to 2019 included 5,891 (SD, 472) patients. There was a 20% increase in pediatric injury during the COVID cohort as compared with the historical cohort (Fig. 1, p = 0.031). Similar findings were appreciated in the sensitivity analysis of 2019 (eFig. 1, http://links.lww.com/TA/C572). Despite day-to-day variation, the average number of injured children treated per day increased from 31 to 37, also an increase of approximately 20% (eFig. 2, http://links.lww.com/TA/C572). Accounting for seasonal and yearly variation in the interrupted time series analysis, the number of observed injuries were significantly greater than the expected injuries during the first 6 months of the pandemic (p < 0.001, Fig. 2).
Figure 1.
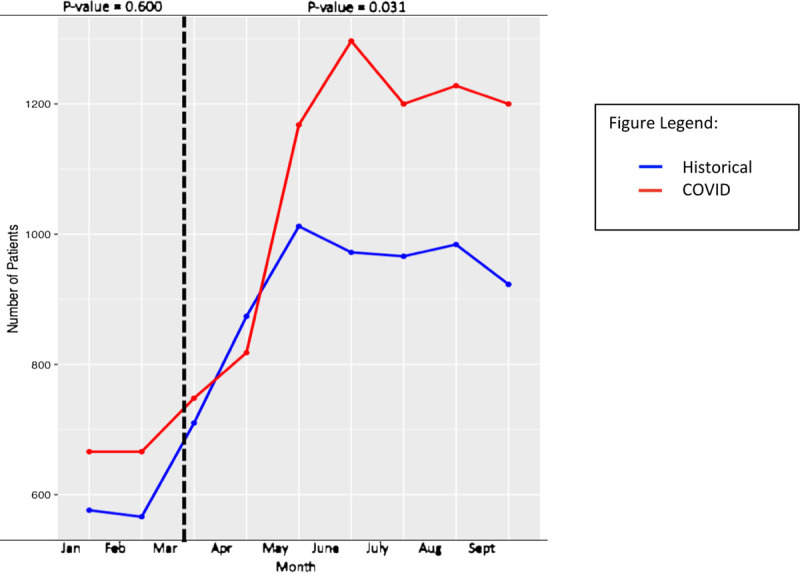
Number of pediatric injuries per month comparing COVID cohort (red) vs. the averaged 2016 to 2019 historical cohort (blue), with dashed line representing the beginning of the COVID period.
Figure 2.
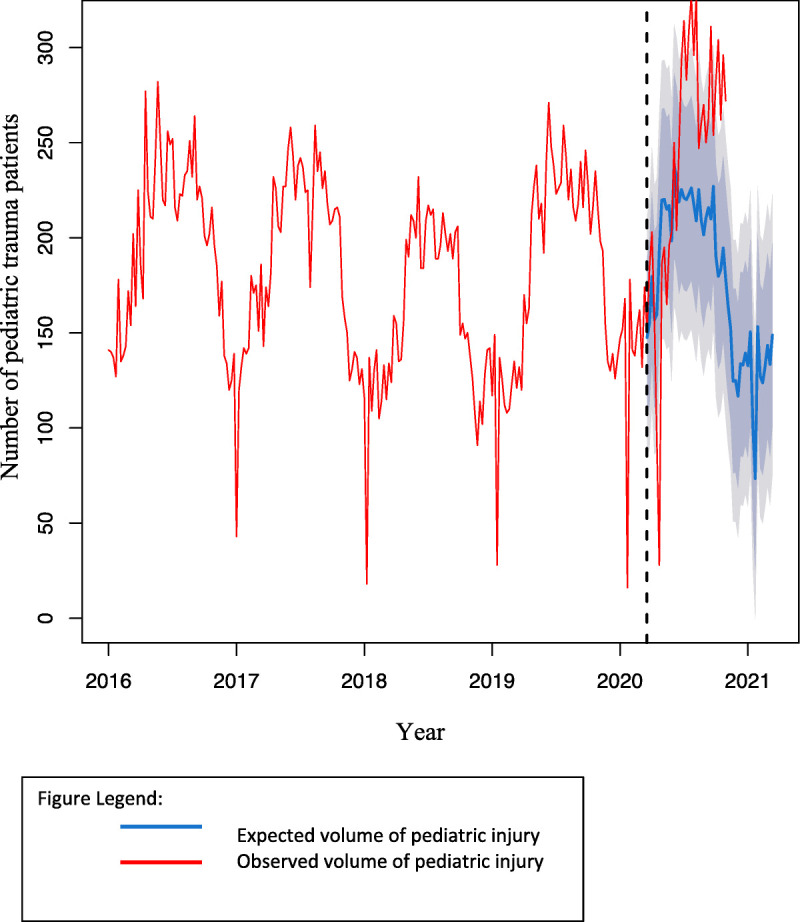
Interrupted time series analysis estimating expected number of pediatric injuries per week (blue), compared with observed number of pediatric injuries per week (red) from January 1, 2016, to September 30, 2020.
Descriptive Data, Outcome Data, and Main Results
Demographic and injury characteristics are presented in Table 1. There was a small increase in the proportion of children 10 years to 14 years of age (26.8% COVID cohort vs. 24.3% historical cohort, p = 0.002), with a corresponding decrease in injured children younger than 1 year (8.7% COVID cohort vs. 9.8% historical cohort, p = 0.036). Socioeconomic status as represented by US zip code-based median household income quintiles saw an increase in the proportion of injured children in the 5th quintile, representing the highest income (25.2% COVID cohort vs. 23.3% historical cohort, p = 0.009). Similarly, there was a decrease in the weighted mean of overall SVI and SVI subthemes in the COVID cohort, indicating slightly less vulnerability compared with historical controls (Table 1). Subthemes for socioeconomic status and housing/transportation met statistical significance (Table 1).
TABLE 1.
Demographic and Injury Characteristics of the Patient Population by Cohort, n (%)
| Historical Average 2016–2019, n = 5,891 | COVID 2020, n = 7,068 | p | |
|---|---|---|---|
| Male | 3,639 (61.8) | 4,289 (60.7) | 0.198 |
| Age, y | 0.005 | ||
| < 1 | 579 (9.8) | 618 (8.7) | |
| 1–4 | 1,232 (20.9) | 1,513 (21.4) | |
| 5–9 | 1,842 (31.3) | 2,155 (30.5) | |
| 10–14 | 1,434 (24.3) | 1,891 (26.8) | |
| 15–17 | 804 (13.7) | 891 (12.6) | |
| Race | 0.630 | ||
| White | 4,349 (75.7) | 5,222 (76.2) | |
| African American | 1,033 (18.0) | 1,199 (17.5) | |
| Asian | 86 (1.5) | 105 (1.5) | |
| Hawaiian/PI | 10 (0.2) | 8 (0.1) | |
| American Indian | 14 (0.2) | 27 (0.4) | |
| Other | 250 (4.4) | 294 (4.3) | |
| Ethnicity | <0.001 | ||
| Hispanic | 368 (6.3) | 478 (6.8) | |
| Non-Hispanic | 4,744 (80.5) | 6,384 (90.3) | |
| Unknown/missing | 778 (13.2) | 206 (2.9) | |
| Median household income | 0.034 | ||
| Quintile 1 (poorest) | 1,148 (19.6) | 1,291 (18.3) | |
| Quintile 2 | 1,180 (20.1) | 1,344 (19.1) | |
| Quintile 3 | 1,040 (17.7) | 1,295 (18.4) | |
| Quintile 4 | 1,135 (19.4) | 1,337 (19.0) | |
| Quintile 5 (richest) | 1,364 (23.3) | 1,778 (25.2) | |
| Weighted SVI, SD | 0.4640 (0.2213) | 0.4559 (0.2236) | 0.007 |
| SES | 0.4926 (0.2377) | 0.4824 (0.2411) | 0.002 |
| Household/disability | 0.5867 (0.2093) | 0.5825 (0.2079) | 0.133 |
| Minority/language | 0.3212 (0.2153) | 0.3179 (0.2138) | 0.262 |
| Housing/transportation | 0.4659 (0.1805) | 0.4608 (0.1856) | 0.037 |
| Injury type* | <0.001 | ||
| Blunt | 4,731 (80.5) | 5,568 (78.8) | |
| Penetrating | 475 (8.2) | 776 (11.0) | |
| Burn | 317 (5.3) | 475 (6.7) | |
| Unspecified | 122 (1.7) | 134 (1.9) | |
| Not applicable | 246 (3.4) | 115 (1.6) | |
| Injury mechanism* | <0.001 | ||
| Fall | 2,482 (42.2) | 2,652 (37.6) | |
| MVC | 1,437 (24.5) | 1,923 (27.3) | |
| Nontraffic | 124 (8.6) | 131 (6.8) | |
| Motorcycle | 22 (1.5) | 36 (1.9) | |
| MVC occupant | 496 (34.5) | 505 (26.3) | |
| MVC other | 5 (0.4) | 5 (0.3) | |
| MVC with cyclist | 64 (4.5) | 69 (3.6) | |
| MVC with pedestrian | 115 (8.0) | 75 (3.9) | |
| MVC unspecified | 24 (1.7) | 12 (0.6) | |
| Bicycle collision | 261 (18.2) | 505 (26.3) | |
| Pedestrian (including skateboarding, rollerblading) | 46 (3.2) | 60 (3.1) | |
| Land transportation (including ATV collisions) | 280 (19.5) | 525 (27.3) | |
| Struck by/against | 534 (9.1) | 494 (7.0) | |
| Firearm | 108 (1.8) | 215 (3.1) | |
| Cut/pierce | 182 (3.1) | 251 (3.6) | |
| Drown/submerge | 22 (0.4) | 28 (0.4) | |
| Burn | 316 (5.4) | 475 (6.7) | |
| Abuse | 228 (3.9) | 264 (3.8) | |
| Bites/stings | 186 (3.2) | 318 (4.5) | |
| Natural | 78 (1.3) | 64 (0.9) | |
| Other/not specified | 237 (4.0) | 354 (5.0) | |
| Intent of injury* | <0.001 | ||
| Unintentional | 5,374 (92.3) | 6,508 (92.1) | |
| Intentional, assault | 378 (6.5) | 459 (6.5) | |
| Intentional, suicide | 37 (0.6) | 44 (0.6) | |
| Intentional, other | 35 (0.6) | 49 (0.7) | |
| Unknown | 1 (0.0) | 1 (0.0) | |
| ISS | 0.888 | ||
| 0–15 | 5,132 (92.4) | 6,490 (92.2) | |
| 16–24 | 262 (4.7) | 336 (4.8) | |
| ≥25 | 158 (2.9) | 210 (3.0) |
*Primary external cause of injury code included only.
ISS, Injury Severity Score; PI, Pacific Islander; SES, socioeconomic status.
While many injury types and mechanisms increased (eFig. 3, http://links.lww.com/TA/C572), there was a statistically significant increase in relative proportion of penetrating injuries (10.2% COVID cohort vs. 8.0% historical cohort, p < 0.001) and burn injuries (6.7% COVID cohort vs. 5.3% historical cohort, p = 0.001), with a commensurate decrease in the proportion of blunt injuries. Notably, firearm injuries increased (2.3% COVID cohort vs. 1.8% historical cohort, p = 0.043), while falls (37.5% COVID cohort vs. 42% historical cohort, p < 0 .001), occupant motor vehicle collisions (MVCs) (26.3% COVID cohort vs. 34.5% historical cohort, p < 0.001), and car versus pedestrian collisions (3.9% COVID cohort vs. 8.0% historical cohort, p < 0.001) decreased. Bicycle collisions and collisions involving other land transportation vehicles (e.g., all-terrain vehicles [ATV]) increased (Table 1). While statistically significant, the relative proportions of injury intent did not change in a clinically meaningful way.
Among the outcomes studied (Table 2), there were changes in disposition from the ED, with a greater proportion of children discharged home in the COVID cohort (22.8% vs. 13.4% historical, p < 0.001). In addition, fewer went to the operating room in the COVID cohort (9.1% vs. 12.2% historical, p < 0.001). There were no significant changes in median ICU LOS, hospital LOS, or mechanical ventilation days.
TABLE 2.
Outcomes After Injury by Cohort, n (%)
| Historical Average 2016–2019, n = 5,891 | COVID 2020, n = 7,068 | p | ||
|---|---|---|---|---|
| Overall mortality | 57 (1.0) | 67 (0.9) | 0.732 | |
| ED disposition* | ||||
| Admit floor | 3426 (58.2) | 3501 (49.5) | <0.001 | |
| Admit ICU | 436 (7.4) | 425 (6.0) | ||
| Admit operating room | 720 (12.2) | 642 (9.1) | ||
| Discharged home | 790 (13.4) | 1612 (22.8) | ||
| Transferred out | 16 (0.2) | 14 (0.2) | ||
| Other (including AMA, jail, etc.) | 4 (0.1) | 10 (0.1) | ||
| Died in the ED | 17 (0.3) | 23 (0.3) | ||
| Unknown/missing | 482 (8.2) | 841 (11.9) | ||
| Hospital disposition | ||||
| Home without services | 4287 (84.7) | 4405 (81.4) | <0.001 | |
| Home with services | 47 (0.9) | 10 (0.2) | ||
| Rehab, SNF, LTC | 50 (1.0) | 66 (1.2) | ||
| Transferred out | 103 (2.0) | 107 (2.0) | ||
| Other (jail, AMA) | 11 (0.2) | 8 (0.2) | ||
| Died inpatient | 40 (0.8) | 44 (0.8) | ||
| Unknown/missing | 526 (10.4) | 769 (14.2) | ||
| Median vent days (IQR) | 3 (0.5–5.5) | 3 (0.5–5.5) | 0.660 | |
| Median LOS, ICU (IQR) | 2 (0.5– 3.5) | 2 (0–4) | 0.270 | |
| Median LOS, hospital (IQR) | 1 (0–2) | 1 (0–2) | 0.200 | |
*If ED disposition and hospital disposition were incongruent (e.g., ED disposition indicated as home, however, hospital disposition also home, rather than “not applicable” because the child was not admitted), then LOS was used to determine admission status and the discordant variables were considered “unknown” (see category).
AMA, against medical advice; wo, without; Rehab, rehabilitation; SNF, skilled nursing facility; LTC, long-term care facility; IQR, interquartile range.
Social Vulnerability and Intentional Injury
In univariate analyses, the COVID cohort was not associated with intentional injury. Race, ethnicity, age, median household income, and SVI were associated with intentional injury (Table 3). In the adjusted model, ethnicity was not included due to the high proportion of missingness and median household income was not included due to moderate collinearity with SVI (correlation coefficient = −0.84). Sex was included for face validity, and the COVID cohort was included to test the study aims. In adjusted models, the COVID cohort alone was not associated with intentional injury; however, the interaction between SVI and the COVID cohort was statistically significant (p = 0.017). Stratified analyses demonstrated the association between SVI and intentional injury increased during the pandemic across all SVI subthemes compared with the historical cohort (Fig. 3 and eFigure 4, http://links.lww.com/TA/C572).
TABLE 3.
Association of the COVID Pandemic and Intentional Injury, Univariate and Multivariable Models Controlling for Demographic Factors and for Clustering by Site
| OR (95% CI) | aOR (95% CI) | |
|---|---|---|
| Cohort | ||
| Historical average | Reference | Reference |
| COVID | 1.0 (0.9–1.1) | 1.1 (0.9–1.1) |
| Sex | ||
| Female | Reference | Reference |
| Male | 1.1 (1.0–1.2) | 1.0 (0.9–1.1) |
| Age, y | ||
| <1 | 19.0 (16.1–22.6) | 17.8 (15.0–21.3) |
| 1–4 | 3.5 (2.9–4.2) | 3.2 (2.7–3.9) |
| 5–9 | Reference | Reference |
| 10–14 | 2.3 (1.9–2.8) | 2.2 (1.8–2.6) |
| 15–17 | 7.4 (6.2–8.9) | 6.5 (5.4–7.9) |
| Race | ||
| White | Reference | Reference |
| African American | 4.0 (3.6–4.4) | 3.2 (2.9–3.6) |
| American Indian | 2.4 (1.1–4.5) | 2.5 (1.1–5.1) |
| Hawaiian/PI | 0.9 (0.1–2.9) | 1.3 (0.2–3.9) |
| Asian | 1.0 (0.6–1.5) | 0.9 (0.6–1.5) |
| Other | 1.4 (1.1–1.7) | 1.2 (0.9–1.5) |
| Ethnicity | ||
| Non-Hispanic | Reference | — |
| Hispanic | 1.0 (0.8–1.5) | — |
| Unknown/missing | 1.3 (1.2–1.5) | — |
| Median household income | ||
| Quintile 1 (poorest) | Reference | — |
| Quintile 2 | 0.7 (0.6–0.7) | — |
| Quintile 3 | 0.4 (0.4–0.5) | — |
| Quintile 4 | 0.4 (0.4–0.5) | — |
| Quintile 5 (richest) | 0.3 (0.2–0.3) | — |
| Weighted SVI | 7.9 (6.5–9.8) | 2.5 (2.0–3.2) |
95% CI, 95% confidence interval; Pacific Islander, PI; adjusted odds ratio, aOR; SVI, social vulnerability index.
Figure 3.
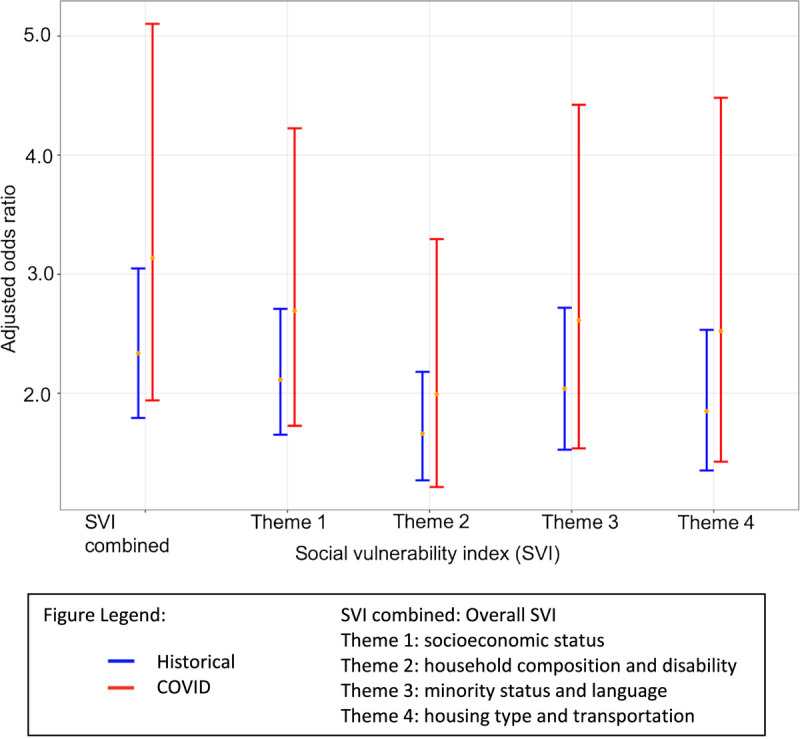
Adjusted odds of intentional injury as compared with unintentional injury in the COVID (red) and historical cohorts (blue) by combined SVI and by individual SVI subthemes.
DISCUSSION
In this multi-institutional study, an overall increase in pediatric injury was observed during the first 6 months of the pandemic as compared with historical controls. This affected children of all demographics and socioeconomic backgrounds, including children from higher income and overall less vulnerable zip codes. The mechanisms of injury changed during this period, with an increase in firearms, burns, bicycle collisions, and ATV-related injuries. Finally, higher SVI, indicating greater vulnerability, was associated with intentional injury, and this relationship was exacerbated during the pandemic.
The higher overall rate of injuries we identified differs from a number of reports in the published literature. While we saw an overall increase in trauma encounters starting as early as April 2020, Sanford and colleagues' retrospective review of trauma registry data at a single US-based Level I PTC between March 15 and May 15 saw a decline of about 16% in the 8 weeks following the US Emergency Declaration.7 Likewise, a 22% decrease in overall pediatric trauma early in the pandemic was found in an evaluation of pediatric trauma admissions 4 weeks after the pandemic began at a single center in Ireland and a 34% decrease in pediatric ED trauma encounters was identified in the first 6 weeks of the pandemic at another single PTC in the United States.3,8 A multi-institutional trauma registry study through June 30, 2020, also reported a decrease in trauma volumes.25 Pediatric Health Information Systems-based studies have demonstrated that both ED visits (through August 2020) and hospital admissions (through June 2020) for pediatric injury declined in 2020 compared with prior years and expected volumes.6,26 The differences in pediatric trauma volume between our study and that appreciated by the other studies described is likely due to differences in time frame of the data captured. Our data identified a rise in pediatric trauma volume beginning as early as April 2020; however, more demonstrable differences were observed between May and September.
Our study demonstrated differences in the type, mechanism, and intent of injury during the first 6 months of the pandemic. We found an increase in injures related to firearms, burns, and collisions involving bicycles and other forms of land transport like ATVs, with a decrease in the relative proportion of falls, MVCs, and other blunt injury compared with historical controls. These trends were similar to those identified by Sanford and colleagues'7 evaluation of a single institution's trauma registry, which identified a relative increase in penetrating trauma encounters and burn admissions, with a corresponding decline in blunt injuries. While the relative decrease in blunt injuries in our study was modest, the change in mechanisms most often associated with blunt injury were more pronounced.
For example, MVC occupant injuries decreased from 34.5% to 26.3%, while injuries from bicycle collisions increased from 18.3% to 26.3%. Concordant with our findings, Matthay et al.27 in a single institution study that captured both adult and pediatric injury, found a 71% decrease in pedestrian versus auto injuries and a 27% decrease in MVCs. Sandford et al. also found a decrease in MVCs while, akin to our findings, injuries due to ATV, bicycle, and skateboard collisions almost doubled.7 Findings from the National Electronic Injury Surveillance System data between March and September 2020 reported increases in injuries related to skateboards and scooters, ATVs and mopeds, and batteries, and decreases in sport-related injuries compared with 2019. We also saw a decrease in falls and struck by/against injuries, presumably related to fewer sports-related injuries and fewer injuries on playgrounds and schoolyards. On the other hand, fewer families were on the road, either for day to day activities or for travel, which may explain the decline in MVCs.
Our data identified a notable increase in pediatric firearm injuries, which almost doubled in the 6 months following the onset of the pandemic, compared with the historical average and compared with 2019 alone during the same period. While Matthay and colleagues27 found a consistent volume of violent-related traumatic injuries, they did find a trend toward increased gunshot wounds early in the pandemic (p = 0.10).27 Cohen et al.'s28 study using the Gun Violence Archive, found an increase in firearm injuries in children younger than 12 years (relative risk, 1.90; 95% confidence interval, 1.58–2.29) during the first 6 months of the pandemic, when compared with an averaged historical cohort similar to our study (2016–2019). While Sanford et al. did not identify an increase in firearms, the study period was limited to only the first 8 weeks of the pandemic, which may explain the discordant findings. While we did not see an increase in the relative proportion of children with an E-Code related to non-accidental trauma, it is important to note there was concern related to the welfare of children in this context and is thus explored in depth elsewhere.29 All together, these findings highlight the differential effect the COVID pandemic as a whole on injury patterns in children.
We found that injury increased in a similar fashion across sex and race, and with a slight decrease in proportion infants and an increase in the 10- to 14-year-old age group. Sanford et al. found no difference in sex or in median age, and a slight increase in proportion of children identifying as White race. Differences in findings are likely related to the longer timeframe and multi-institutional nature of our study. It is possible our finding that more 10-year to 14-year-old children were injured in the COVID cohort compared with the historical cohort may reflect a lack of structure or supervision normally provided by in-person attendance at school.
Interestingly, we appreciated an increase in injuries during COVID across all income quintiles; however, the most profound change, of just over 30%, was in the “richest” quintile. This is concordant with change in weighted SVI between the two cohorts. Overall, across the combined SVI and all the SVI subthemes, the weighted values were slightly lower in the COVID cohort as compared with the historical cohort, reflecting slightly less vulnerability overall. There are similar findings in the sensitivity analysis comparing the COVID cohort to 2019 alone, meaning the change is not simply a time-based improvement in socioeconomic status. These data indicate the COVID pandemic was associated with increased pediatric injury across all strata of society.
However, children who lived in zip codes with increased social vulnerability had increased odds of intentional injury compared with unintentional injury. This relationship was identified at baseline, and then was found to be exacerbated during the pandemic. All SVI domains (socioeconomic status, household composition and disability, minority status and language, and housing and transportation) reflected this relative increase in association with intentional injury in children during the pandemic. In unadjusted analyses, this was most pronounced for minority children and children who speak English “less well,” as compared with those with increased vulnerability related to socioeconomic status, household composition, or housing type and transportation. Hence, the SVI metric, which was created to identify communities with less “ability to prevent human suffering during times of external stress” appropriately identified children with a disproportionately increased risk for intentional injury during the pandemic. Exploration into these relationships is essential to further inform social service allocation during times of external stress, such as the COVID pandemic.
Our findings have several important limitations. First, the data are from institutional trauma registries, which do not capture all injuries that are treated at the hospital, including non-transferred ED discharged patients. Children dying before arrival or not treated at the trauma centers included in this study were not captured. While each Level I PTC in this study has a geographically large catchment area, this is not an epidemiologic study and thus population estimates cannot be made. Normalizing to population estimates was explored however census-based estimates for 2020 were not available. Likewise, a change in transfer patterns from adult centers to pediatric centers may explain a degree of the increased volume captured, as adult centers had increased need to treat COVID-positive adult patients. Social vulnerability index is a metric created by census tract, and use by zip code loses granularity and introduces risk for misclassification. Social vulnerability index uses 15 social factors from the 5-year American Community Survey data, which is released every 2 years by the US Census Bureau in December of the year following the Survey. While we used the most up-to-date SVI from 2018, reflecting the 2014 to 2018 survey data, there is risk in attributing the same SVI to the COVID cohort and the historical cohort, since SVI (and also median income) may have changed in the interim. We suspect any changes would lead to conservative estimates because vulnerability indices may have increased during the pandemic, indicating an even stronger relationship with intentional injury than we identified. We were also limited by the lack of a non-injured population, thus limiting analyses.
There were concurrent social unrest and potentially related tensions during the study period worth mentioning. Throughout the midwest, and much of the nation, there were protests related to high-profile police shootings. Some were peaceful and some involved looting and/or violence. It is impossible within the context of these data to parse out a causal relationship between the pandemic and pediatric injury compared with social unrest and pediatric injury. There are likely unmeasured confounders that may have disproportionally affected certain neighborhoods. For example, changes in disposable income may have affected children in lower income households more than higher income households. Changes in police presence, local isolation policies, regional healthcare and childcare programing, and relief payments to families and local businesses may have impacted different neighborhoods in different ways.
CONCLUSION
This study identified an increase in pediatric injuries associated with the COVID pandemic treated at Level I PTCs and examined the changes in the types of injuries seen across multiple sites and states. Importantly, we identified that the SVI was associated with intentional injury in children and that the relationship between increased vulnerability and intentional injury was even stronger during the pandemic, highlighting children most at risk of intentional injury during times of external stress. Collectively, these data suggest a child's social determinants of health, including the neighborhood in which they live, may be related to different injury patterns during the pandemic. These findings are critical to inform and guide resource allocation and tailored injury prevention methodologies for all children and families during times of family, community, and national stress.
AUTHORSHIP
K.T.F., A.T.C., M.F., M.E.F., P.C.M., K.E.S., K.V.A., and T.T.S. made substantial contributions to research design and idea development, data collection and analysis, data interpretation, article writing, and critical revisions. K.J.D., R.A.F., D.S.F., J.D.F., S.G., M.S.K., M.K., M.P.L., C.M.L., T.A.M., N.R., and S.D.S.P. made substantial contributions to data collection and analysis and article editing, including critical revisions. All authors give final approval of the enclosed article.
ACKNOWLEDGMENTS
We would like to thank the research coordinators and trauma registrars at each of the participating sites for their help in obtaining institutional data, including Sarah Fox, Jill Jaeger, Kristin Braun, Jane Riebe-Rodgers, Suzanne Moody, Taunya Kessler, Jessica Johnson, Carley Lutz, Michelle Bainter, Jodi Raymond, Pete Muenks, Elizabeth McClure, Jennifer Seay, Linda Cherney, Benjamin Eithun, Loran Zwiefelhofer, Connor Fairfax, and Amanda Truelove. Sarah Fox, the MWPSC Project Manager, for her efforts in helping the MWPSC to run smoothly and efficiently.
DISCLOSURE
The authors declared no conflicts of interest.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.jtrauma.com).
Contributor Information
Amelia T. Collings, Email: amroge@iu.edu.
Manzur Farazi, Email: mfarazi@mcw.edu.
Mary E. Fallat, Email: mary.fallat@louisville.edu.
Peter C. Minneci, Email: Peter.Minneci@nationwidechildrens.org.
K. Elizabeth Speck, Email: speckk@med.umich.edu.
Kyle Van Arendonk, Email: KVanArendonk@chw.org.
Katherine J. Deans, Email: Katherine.deans@nationwidechildrens.org.
Richard A. Falcone, Jr., Email: Richard.falcone@cchmc.org.
David S. Foley, Email: david.foley@louisville.edu.
Jason D. Fraser, Email: jdfraser@cmh.edu.
Samir Gadepalli, Email: samirg@med.umich.edu.
Martin S. Keller, Email: mskeller@wustl.edu.
Meera Kotagal, Email: Meera.kotagal@cchmc.org.
Matthew P. Landman, Email: landman@iu.edu.
Charles M. Leys, Email: leys@surgery.wisc.edu.
Troy A. Markel, Email: tmarkel@iupui.edu.
Nathan Rubalcava, Email: nathanrubalcava@gmail.com.
Shawn D. St. Peter, Email: sspeter@cmh.edu.
Thomas T. Sato, Email: ttsato@chw.org.
REFERENCES
- 1.United States. President (2016–2020: Trump). 2020. Declaring a National Emergency Concerning the Novel Coronavirus Disease (COVID-19) Outbreak, pursuant to 501(b) U.S.C. 5121–5207. Washington, U.S. 2020;85(53), 15337–15338. [Google Scholar]
- 2.Smith SM, Edwards R, Duong HC. Unemployment rises in 2020, as the country battles the COVID-19 pandemic. U.S. Bureau of Labor Stat; 2021: [June 2021:[Available at: https://www.bls.gov/opub/mlr/2021/article/unemployment-rises-in-2020-as-the-country-battles-the-covid-19-pandemic.htm. Accessed January 16, 2022. [Google Scholar]
- 3.Haddadin Z Blozinski A Fernandez K Vittetoe K Greeno AL Halasa NB, et al. Changes in pediatric emergency department visits during the COVID-19 pandemic. Hosp Pediatr. 2021;11(4):e57–e60. [DOI] [PubMed] [Google Scholar]
- 4.Kovler ML Ziegfeld S Ryan LM Goldstein MA Gardner R Garcia AV, et al. Increased proportion of physical child abuse injuries at a level I pediatric trauma center during the Covid-19 pandemic. Child Abuse Negl. 2021;116(Pt 2):104756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Markham JL Richardson T DePorre A Teufel RJ 2nd Hersh AL Fleegler EW, et al. Inpatient use and outcomes at children's hospitals during the early COVID-19 pandemic. Pediatrics. 2021;147(6):e2020044735. [DOI] [PubMed] [Google Scholar]
- 6.Pelletier JH, Rakkar J, Au AK, Fuhrman D, Clark RSB, Horvat CM. Trends in US pediatric hospital admissions in 2020 compared with the decade before the COVID-19 pandemic. JAMA Netw Open. 2021;4(2):e2037227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sanford EL, Zagory J, Blackwell JM, Szmuk P, Ryan M, Ambardekar A. Changes in pediatric trauma during COVID-19 stay-at-home epoch at a tertiary pediatric hospital. J Pediatr Surg. 2021;56(5):918–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sheridan GA Nagle M Russell S Varghese S O’Loughlin PF Boran S, et al. Pediatric trauma and the COVID-19 pandemic: a 12-year comparison in a Level-1 trauma center. HSS J. 2020;16(Suppl 1):92–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Swedo E Idaikkadar N Leemis R Dias T Radhakrishnan L Stein Z, et al. Trends in U.S. emergency department visits related to suspected or confirmed child abuse and neglect among children and adolescents aged <18 years before and during the COVID-19 pandemic—United States, January 2019-September 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1841–1847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fowler KA, Dahlberg LL, Haileyesus T, Gutierrez C, Bacon S. Childhood firearm injuries in the United States. Pediatrics. 2017;140(1):e20163486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jack SP Petrosky E Lyons BH Blair JM Ertl AM Sheats KJ, et al. Surveillance for violent deaths—National Violent Death Reporting System, 27 states, 2015. MMWR Surveill Summ. 2018;67(11):1–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morgan ME Horst MA Vernon TM Fallat ME Rogers AT Bradburn EH, et al. An analysis of pediatric social vulnerability in the Pennsylvania trauma system. J Pediatr Surg. 2020;55(12):2746–2751. [DOI] [PubMed] [Google Scholar]
- 13.Brokamp C, Beck AF, Goyal NK, Ryan P, Greenberg JM, Hall ES. Material community deprivation and hospital utilization during the first year of life: an urban population-based cohort study. Ann Epidemiol. 2019;30:37–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Convention on the rights of the child . Treaty no. 27531. United Nations Treaty Series, 1577; 1989:3–178 Available at: https://treaties.un.org/doc/Treaties/1990/09/19900902%2003-14%20AM/Ch_IV_11p.pdf. Accessed 10-22-2021. [Google Scholar]
- 15.American College of Surgeons Committee on Trauma . National Trauma Data Standard Data Dictionary: 2020 Admissions. Available at: https://www.facs.org/-/media/files/quality-programs/trauma/ntdb/ntds/data-dictionaries/ntds_data_dictionary_2021.ashx. Accessed 07-30-2021. [Google Scholar]
- 16.Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry/Geospatial Research, Analysis, and Services Program . CDC/ATSDR Social Vulnerability Index 2018 Database, United States. Available at: https://www.atsdr.cdc.gov/placeandhealth/svi/data_documentation_download.html. Accessed January 16, 2022.
- 17.Tiao GC, Box GEP. Intervention analysis with applications to economic and environmental problems. J Am Stat Assoc. 1975;70(349):70–79. [Google Scholar]
- 18.Wickham H Averick M Bryan J Chang W McGowan L François R Golemund G Hayes A Henry L Hester J, et al. Welcome to the Tidyverse. J Open Source Softw. 2019;4(43). [Google Scholar]
- 19.Hadley W, Francois R, Henry L, Muller K. dplyr: A Grammar of Data Manipulation. R package version 1.0.7 2021 [Available at: https://CRAN.R-project.org/package=dplyr.] Accessed July 30, 2021.
- 20.Grolemund G, Wickham H. Dates and Times Made Easy with lubridate. 2011. 2011;40(3):25. [Google Scholar]
- 21.Fox J, Weisberg S. An R Companion to Applied Regression. third ed. Thousand Oaks, CA: SAGE Publications; 2019. [Google Scholar]
- 22.Wickham H. ggplot2: Elegant Graphics for Data Analysis. second ed. Houston, TX: Springer; 2016. [Google Scholar]
- 23.Wickham H, Bryan J. readxl: Read Excel Files. 2019. [Available at: https://CRAN.R-project.org/package=readxl.] Accessed July 30, 2021.
- 24.Wickham H. stringr: Simple, Consistent Wrappers for Common String Operations. 2019. Available from: https://CRAN.R-project.org/package=stringr. Accessed July 30, 2021.
- 25.Bessoff KE Han RW Cho M Stroud M Urrechaga EM Thorson CM, et al. Epidemiology of pediatric trauma during the COVID-19 pandemic shelter in place. Surg Open Sci. 2021;6:5–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.DeLaroche AM Rodean J Aronson PL Fleegler EW Florin TA Goyal M, et al. Pediatric emergency department visits at US children’s hospitals during the COVID-19 pandemic. Pediatrics. 2021;147(4):e2020039628. [DOI] [PubMed] [Google Scholar]
- 27.Matthay ZA Kornblith AE Matthay EC Sedaghati M Peterson S Boeck M, et al. The DISTANCE study: determining the impact of social distancing on trauma epidemiology during the COVID-19 epidemic—an interrupted time-series analysis. J Trauma Acute Care Surg. 2021;90(4):700–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cohen JS Donnelly K Patel SJ Badolato GM Boyle MD McCarter R, et al. Firearms injuries involving young children in the United States during the COVID-19 pandemic. Pediatrics. 2021;148:e2020042697. [DOI] [PubMed] [Google Scholar]
- 29.Collings AT Farazi M Van Arendonk K Fallat ME Minneci PC Sato TT, et al. Impact of “stay-at-home” orders on non-accidental trauma: a multi-institutional study. J Pediatr Surg. 2022;57:1062–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]


