Abstract
Background
The coronavirus disease 2019 (COVID-19) disproportionately affects minority populations in the USA. Sweden — like other Nordic countries — have less income and wealth inequality but lacks data on the socioeconomic impact on the risk of adverse outcomes due to COVID-19.
Methods
This population-wide study from March 2020 to March 2022 included all adults in Stockholm, except those in nursing homes or receiving in-home care. Data sources include hospitals, primary care (individual diagnoses), the Swedish National Tax Agency (death dates), the Total Population Register “RTB” (sex, age, birth country), the Household Register (size of household), the Integrated Database For Labor Market Research “LISA” (educational level, income, and occupation), and SmiNet (COVID data). Individual exposures include education, income, type of work and ability to work from home, living area and living conditions as well as the individual country of origin and co-morbidities. Additionally, we have data on the risks associated with living areas. We used a Cox proportional hazards model and logistic regression to estimate associations. Area-level covariates were used in a principal component analysis to generate a measurement of neighborhood deprivation. As outcomes, we used hospitalization and death due to COVID-19.
Results
Among the 1,782,125 persons, male sex, comorbidities, higher age, and not being born in Sweden increase the risk of hospitalization and death. So does lower education and lower income, the lowest incomes doubled the risk of death from COVID-19. Area estimates, where the model includes individual risks, show that high population density and a high percentage of foreign-born inhabitants increased the risk of hospitalization.
Conclusions
Segregation and deprivation are public health issues elucidated by COVID-19. Neighborhood deprivation, prevalent in Stockholm, adds to individual risks and is associated with hospitalization and death. This finding is paramount for governments, agencies, and healthcare institutions interested in targeted interventions.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12916-022-02715-4.
Keywords: COVID-19, Socioeconomics, Population study, Cohort study, Stockholm, Epidemiology, Hospitalization, Mortality
Background
Globally, it is known that countries with high levels of income inequality have performed significantly worse when dealing with the coronavirus disease 2019 (COVID-19) outbreak in terms of cases and deaths [1, 2]. Moreover, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), causing COVID-19 disproportionately affects minority populations in the USA and in the UK [3–5].
During the 2009 H1N1, influenza reports in the USA of racial ethnic disparities with regard to complications and hospitalization [6] led to a national survey documenting the sources of these inequalities [7]. Increased risk of exposure to the virus and increased susceptibility to severe consequences of the infection combined with lack of health care access were important contributors.
In the rest of Western Europe and specifically in the Nordics, there is a paucity of data regarding the socioeconomic impact on the risk of infection, hospitalization, and mortality due to COVID-19. Even though the risk of COVID-19 varies enormously between geographical areas as well as between individuals with different sociodemographic characteristics, such as sex, age, and socioeconomic status, the relationship between geographical areas and individual risk factors is unknown.
The present study sought to address this knowledge gap with a population-wide study of all adult inhabitants in the Stockholm Region, excluding older adults living in nursing homes or receiving in-home care. We used the real-time COVID-19 monitoring framework in Region Stockholm to investigate the demographic and socioeconomic impact on the risk of hospitalization and mortality.
We hypothesized that demographic and socioeconomic factors contributed to the risk of hospitalization and death independently of other co-morbidity-related risk factors. We further wanted to assess if living areas carried additional risks of COVID hospitalization or death, even when adjusting for all individual factors.
Methods
Data sources
Stockholm’s administrative organization (Region Stockholm), responsible for all healthcare within the region, manages VAL (Swedish: Vård Analys Lager, the Stockholm Regional Healthcare Data Warehouse), a data warehouse of healthcare utilization. VAL contains complete hospital inpatient and hospital outpatient data, and primary care information, including consultations and diagnoses at the individual level. The coverage in VAL for inpatient care is over 99% [8] and the validity of the diagnostic coding is 85–95%, depending on the diagnosis [9]. The VAL database includes linkage to the Swedish National Tax Agency (death dates) and was also further linked to national population registers held by Statistics Sweden. This included the Total Population Register “RTB” (sex, age, birth country) [10]. RTB also contains Household Register data on geographical information, including street address and apartment data (size of household) and the Integrated Database For Labor Market Research ”LISA” (educational level, income, and occupation) [11]. In addition, we used data from SmiNet which is a national electronic surveillance system for reporting communicable diseases [12]. Since February 1, 2020, it is mandatory for the Swedish laboratories to report all PCR-confirmed cases of COVID-19 to SmiNet. All register linkage used the unique personal identity number given to each Swedish citizen [13].
Study population
The study population consisted of all individuals 18 years and older, residing in Stockholm County during a calendar year from March 1st, 2020, to February 28th, 2021, based on data from the Population Register [10]. Individuals permanently staying in nursing homes were excluded since they were mainly treated for COVID-19 in their facilities and hence did not contribute risk for hospitalization. Also, those with home-care services were excluded due to increased risk of infection, uncoupled to sociodemographic status.
Variables used as exposure and confounders in statistical models
Educational level: separated into low (pre-secondary education), medium (secondary-), and higher education (post-secondary education) based on LISA data.
Income: household disposable income (LISA data) was separated into quintiles, from the 20% with the lowest income to the 20% with the highest income defined as income including welfare, after taxation.
Work: using the “standard for Swedish occupational classifications” (SSYK), based on the “international standard classification of occupations” (ISCO), we dichotomized individuals based on the ability to work from home or not. Additionally, we have analyzed healthcare workers, and adults not working (full-time students, unemployed, on long-term sick leave, or retired) separately. These classifications were made by individually assessing the work characteristics of the different occupations.
Living area: the greater Stockholm area was divided into 164 neighborhoods with an average of 14,000 inhabitants. They were ranked after death due to COVID-19 per 10,000 people (excluding those living at nursing homes) and then grouped into quintiles. In other analyses, we introduce them separately, as baseline hazards.
Living condition: measured as the size of household (the number of people in the household).
Country of origin: data on country and region of origin is available, but for these analyses, we divided subjects into those born in Sweden and not born in Sweden.
Co-morbidities: the following ICD codes from the VAL database were chosen, based on previous risk factor publications [14, 15] heart failure (I50), ischemic heart disease (I20-25), diabetes (E10-14), obesity (E66), chronic kidney disease (N18), chronic obstructive pulmonary disease (J44), cancer (C00-97) and liver disease (I85–I85.9; I98.2; K79–K71, K71.3–K77.8; R16–R18.9; Z52.6; Z94.4). All individuals with one of these diagnoses within the last 5 years (or 2 years for cancer) or one hospitalization due to cardiovascular disease have been classified as having a co-morbidity.
Outcomes
The primary outcome was 30-day all-cause mortality after laboratory-confirmed COVID-19 infection. The secondary outcome was hospitalization with confirmed COVID-19 infection. Hospitalization as outcome was verified via SmiNet and validated if inpatient treatment included the emergency ICD10 codes for COVID-19 (issued by the WHO): U07.1–U07.2 as the main diagnosis.
Observation period
The observation period ran from the 1st of March 2020 to the 28th of February 2021. Follow-up ended at loss to follow-up (emigration from the Stockholm Region), end of study, or the date of outcomes.
Statistical analyses
Multivariate logistic regression model was used, fitted for each outcome. The modeling strategy consisted of analyzing a selection of individual covariates first, followed by the same individual covariates and a selection of area-level covariates. To avoid collinearity in the latter part of the modeling, each area-level covariate was included one at a time, always including the whole set of individual covariates. Area-level covariates outside of area percentages of children, percentages of elderly, density, and inhabitants born outside of Sweden were included in a principal component analysis to generate a composite neighborhood deprivation score (NDS), divided into three levels, from least (NDS 1) to most deprived (NDS 3).
In Additional file 1: Table S1 associations were estimated using a Cox proportional hazards model with income as exposure and adjusted for confounder variables as categorical variables and stratified for area effects, thus allowing for different baseline hazards in each area. In this analysis, individuals were censored at the date of death from other causes, emigration from the region, or at the end of follow-up, whichever came first. The potential confounders were added sequentially in order to show the confounding impact of different domains of the sociodemographic factors.
Ethical approval
The study has been approved by the Regional Ethical Review Board, Stockholm (2021–00810). All data were analyzed in a pseudonymized format and confidentiality was always maintained. Reporting follows the STrengthening the Reporting of OBservational studies in Epidemiology and the REporting of studies Conducted using Observational Routinely-collected health Data statements [16, 17].
Data sharing
Swedish privacy law prohibits us from making registered data publicly available.
Results
In all, 1.7 million people were followed from March 1st, 2020, to February 28th, 2021, during which time 10,495 hospitalizations and 1148 deaths due to COVID-19 were registered. Tables 1 and 2 detail the individual effect estimates on covid-19 hospital admission and mortality. Men had a higher risk of both hospitalization and death than women, with relative risk (RR) 1.6 (confidence interval (CI) 1.53–1.66) and RR 2.5 (CI 2.19–2.85), respectively. Increasing age was strongly associated with increasing risks, mainly regarding to mortality where a relative risk of 53 was seen in the ≥75 years age category. Immigrants to Sweden were generally at higher risks of both outcomes, with a RR for hospitalization of 2.11 (2.02–2.21) and RR for death was 1.68 (1.47–1.92). Lower education and lower income levels were significantly coupled with higher relative risks of mortality. The lowest income level was associated with a doubled risk of death from COVID-19, and the presence of co-morbidities more than quadrupled the mortality risk.
Table 1.
Frequency table for COVID-19 hospitalizations and mortality among a Stockholm Regions cohort of 1,782,125 persons followed between the 1st of March 2020 to the 28th of February 2021
| N (%) | Number of hospital admissions during follow-up (%) | Number of deaths during follow-up (%) | |
|---|---|---|---|
| Total | 1,782,125 | 10,495 | 1148 |
| Sex | |||
| Women | 890,223 (50%) | 4145 (39%) | 351 (31%) |
| Men | 891,902 (50%) | 6350 (61%) | 797 (69%) |
| Age groups | |||
| 18–44 years | 878,906 (49%) | 2021 (19%) | 31 (3%) |
| 45–59 years | 459,285 (26%) | 3065 (29%) | 110 (10%) |
| 60–74 years | 311,575 (17%) | 3239 (31%) | 335 (29%) |
| 75–110 years | 132,359 (7%) | 2170 (21%) | 672 (59%) |
| Region of origin (birth) | |||
| Sweden | 1,226.715 (69%) | 5225 (50%) | 658 (57%) |
| Not born in Sweden | 555,410 (31%) | 5270 (50%) | 490 (43%) |
| Living conditionsa | |||
| Single household | 367,841 (21%) | 2276 (22%) | 385 (34%) |
| Double | 524,238 (29%) | 3483 (33%) | 496 (43%) |
| Triple | 301,768 (17%) | 1538 (15%) | 113 (10%) |
| Quartet | 315,376 (18%) | 1382 (13%) | 54 (5%) |
| Multiple | 272,902 (15%) | 1816 (17%) | 100 (9%) |
| Education | |||
| High | 689,193 (39%) | 2957 (28%) | 252 (22%) |
| Medium | 761,873 (43%) | 4505 (43%) | 468 (41%) |
| Low | 226,960 (13%) | 2267 (22%) | 329 (29%) |
| Other | 56,279 (3%) | 411 (4%) | 71 (6%) |
| NA | 47,820 (3%) | 355 (3%) | 28 (2%) |
| Type of workb | |||
| Full-time home | 510,967 (29%) | 2725 (26%) | 114 (10%) |
| Part-time home | 475,712 (27%) | 1416 (13%) | 62 (5%) |
| Health worker | 117,788 (17%) | 837 (8%) | 26 (2%) |
| Otherb | 677,658 (38%) | 5520 (53%) | 946 (82%) |
| Income | |||
| Income Q5 (highest income) | 347,377 (19%) | 1528 (15%) | 116 (10%) |
| Income Q4 | 346,117 (19%) | 1531 (15%) | 114 (10%) |
| Income Q3 | 340,517 (19%) | 1832 (17%) | 174 (15%) |
| Income Q2 | 323,936 (18%) | 2382 (23%) | 359 (31%) |
| Income Q1 | 326,115 (18%) | 2698 (26%) | 351 (31%) |
| No info on income | 98,063 (6%) | 524 (5%) | 34 (3%) |
| Comorbidities | |||
| No | 1,447,390 (81%) | 4933 (47%) | 239 (21%) |
| Yes | 334,735 (19%) | 5562 (53%) | 909 (79%) |
aLiving conditions are measured as the size of the household (i.e., the number of people in the household)
bPossibility to work from home full-time or part-time. ‘Other’ includes full-time students, unemployed, on long-term sick leave, or retired
Table 2.
Relative risks1 with 95% confidence intervals for COVID-19 hospitalizations and mortality among a Stockholm Regions cohort of 1,782,125 persons followed between the 1st of March 2020 to the 28th of February 2021
| Hospital Admissions | Mortality | |
|---|---|---|
| RRc (95% CI) | RRc (95% CI) | |
| Sex | ||
| Women | 1.0 | 1.0 |
| Men | 1.60 (1.53–1.66) | 2.50 (2.19–2.85) |
| Age groups | ||
| 18–44 years | 1.0 | 1.0 |
| 45–59 years | 2.55 (2.40–2.70) | 5.97 (3.97–8.99) |
| 60–74 years | 3.47 (3.25–3.70) | 17.08 (11.54–25.28) |
| 75–110 years | 4.95 (4.57–5.36) | 53.78 (36.00–80.33) |
| Region of origin (birth) | ||
| Sweden | 1.0 | 1.0 |
| Not born in Sweden | 2.11 (2.02–2.21) | 1.68 (1.47–1.92) |
| Living conditionsa | ||
| Single household | 1.0 | 1.0 |
| Two person | 1.05 (0.99–1.11) | 0.85 (0.74–0.98) |
| Three person | 1.25 (1.17–1.33) | 1.08 (0.86–1.34) |
| Four person | 1.30 (1.21–1.40) | 0.84 (0.62–1.14) |
| >Four person | 1.46 (1.36–1.57) | 1.03 (0.79–1.35) |
| Education | ||
| High | 1.0 | 1.0 |
| Medium | 1.15 (1.10–1.21) | 1.16 (0.99–1.36) |
| Low | 1.38 (1.31–1.50) | 1.49 (1.25–1.77) |
| Other | 0.89 (0.84–0.94) | 1.35 (1.08–1.69) |
| Type of workb | ||
| Full-time | 1.0 | 1.0 |
| Part-time | 0.77 (0.72–0.83) | 0.94 (0.69–1.29) |
| Health worker | 1.45 (1.34–1.58) | 1.28 (0.83–1.97) |
| Otherb | 0.89 (0.84–0.94) | 1.35 (1.08–1.69) |
| Income | ||
| Income Q5 (highest income) | 1.0 | 1.0 |
| Income Q4 | 1.01 (0.94–1.09) | 1.10 (0.84–1.42) |
| Income Q3 | 1.09 (1.02–1.18) | 1.35 (1.06–1.72) |
| Income Q2 | 1.20 (1.11–1.28) | 1.75 (1.40–2.20) |
| Income Q1 | 1.34 (1.24–1.44) | 2.19 (1.73–2.79) |
| No info income | 1.10 (0.92–1.30) | 0.98 (0.42–2.28) |
| Comorbidities | ||
| No | 1.0 | 1.0 |
| Yes | 2.99 (2.86–3.13) | 4.38 (3.75–5.12) |
aLiving conditions are measured as the size of the household (i.e., the number of people in the household)
bPossibility to work from home full-time or part-time. Other includes full-time students. Unemployed, long-term sick leave, or retired
cOdds ratios (here presented as relative risks) derived from a logistic regression model; fully adjusted models included all variables presented in the table
Table 3 shows the contextual effect estimates on hospitalization and death. This model takes all the individual effect estimates — presented in Tables 1 and 2 — into account. The geographical area factors standing out include a high percentage of people not born in Sweden; mortality in such areas was elevated by over 50% compared to reference areas. We also found high population density and the age distribution in an area to be associated with increased risk of both hospital admission and mortality, where a high proportion of younger adults and a low proportion of older adults were associated with increased risks.
Table 3.
Frequency table of contextual effect estimates and variables used in model based on tertiles of percentage distributions of selected factors over geographical areas in Stockholm county
| Number of hospital admissions (%) | Number of deaths (%) | |
|---|---|---|
| Categories (tertiles) based on the percentage of Swedish born in a geographical area | ||
| High % born in Sweden | 2295 (22%) | 261 (23%) |
| Medium % born in Sweden | 3368 (32%) | 370 (32%) |
| Low % born in Sweden | 4832 (46%) | 517 (45%) |
| Categories (tertiles) based on population density in a geographical area | ||
| High population density | 4210 (40%) | 472 (41%) |
| Medium population density | 3848 (37%) | 375 (33%) |
| Low population density | 2437 (23%) | 301 (26%) |
| Categories (tertiles) based on the percentage of childrena in a geographical area | ||
| High % children | 3145 (30%) | 338 (29%) |
| Medium% children | 4504 (43%) | 460 (40%) |
| Low % children | 2846 (27%) | 350 (30%) |
| Categories (tertiles) based on the percentage of older adultsb in a geographical area | ||
| High % elderly | 2534 (24%) | 324 (28%) |
| Medium % elderly | 3971 (38%) | 455 (40%) |
| Low % elderly | 3990 (38%) | 369 (32%) |
| Index variable based on area covariate above (tertiles) | ||
| High | 2922 (28%) | 339 (30%) |
| Medium | 3891 (37%) | 408 (36%) |
| Low | 3682 (35%) | 401 (35%) |
aChildren = 0–15 years of age
bElderly = 70 years or older
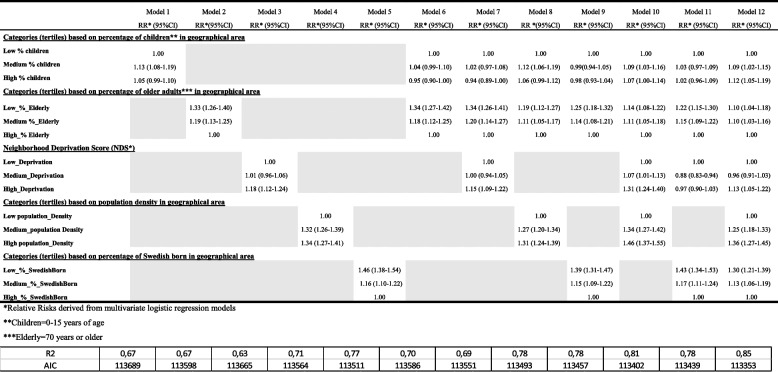
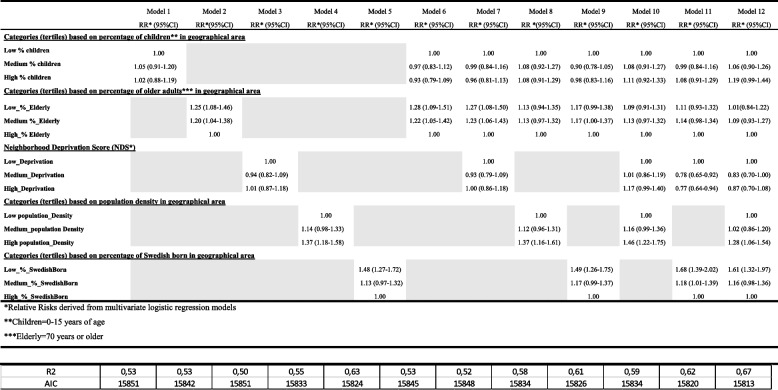
Tables 4 and 5 demonstrate the interface between area factors and individual effect estimates on the risk of hospital admission and death in a stepwise fashion. This model takes all the individual effect estimates — presented in Tables 1 and 2 — into account. Hospitalization is higher in areas with many children, fewer elderly people, high density, high area deprivation, and in areas with low percentages of Swedish-born inhabitants. Mortality is to a larger extent impacted by individual risk factors (Table 5) as demonstrated by non-significant relative risks. Important exceptions include areas with high density and low percentages of Swedish-born inhabitants. Neighborhood deprivation is explained in the methods section and the first principal component explained 42.22% of the total variability and it can be interpreted directly from Additional file1: Figure S1.
Table 4.
Relative risk* and 95% confidence intervals of COVID-19-related hospitalization for area-level covariates (based on tertiles of percentage distributions) and a principal component analysis to generate a composite neighborhood deprivation score (NDS). Area-level covariate was included one at a time (model 1 to 12, always including the whole set of individual covariates in the models)
Table 5.
Relative risk* and 95% confidence intervals of COVID-19-related deaths for area-level covariates (based on tertiles of percentage distributions) and a principal component analysis to generate a composite neighborhood deprivation score (NDS). Area-level covariate was included one at a time (model 1 to 12, always including the whole set of individual covariates in the models)
Additional file 1: Table S1 shows the crude risk of death depending on where you live and the risk after multiple adjustments. As mentioned in the methods, residential areas were divided into quintiles with the 20% most afflicted, i.e., the highest number of deaths, in quintile 1 and the 20% least afflicted in quintile 5. Crude data indicate a quadrupled death toll in the worst-off areas. Even after adjustments for sex, age, country of origin, education, type of work, income, living conditions, and co-morbid conditions; mortality is twice as high for people living in the most afflicted neighborhoods.
Discussion
To our knowledge, this large, population-based study is the first to assess the combination of individual- and area-level risk factors on outcomes of COVID-19 patients. Our key finding is that segregation and deprivation are strongly associated to detrimental outcomes of COVID-19.
Individual factors like lower income, lower education, and inability to work from home together with age, male sex, and co-morbid conditions increase the risk of hospitalization and death. Country of origin plays a part in the individual risk of severe outcomes, but we also demonstrate group-level effects. Residence in an area with a higher percentage of immigrants was independently associated with an increased risk of hospital admission. Living in affluent neighborhoods, with few immigrants, was associated with both lower risk of hospitalization and death. There were other signals in the contextual effect estimates; areas with low numbers of children and a high percentage of people over 70 years were associated with decreased risk of hospital admission. Living in the most deprived areas in Stockholm was an independent risk factor for hospitalization during the first year of the COVID-19 pandemic.
One ecological study from Germany, during the first wave, showed COVID-19 cases and death negatively associated with the share of schoolchildren and children in day care as well as physician density [18]. In contrast to that and other ecological studies, the present investigation combines individual- and area-related factors. A Norwegian study of immigrants indicated that crowded housing and low income at a group level were correlated with cases and hospitalization of COVID-19 [19]. A nationwide Swedish study [20], albeit lacking data on hospitalization and solely examining the first wave (less than 2 months of follow-up) of the pandemic, scrutinizes sociodemographic factors. Being male, low individual income, lower education, and not being married independently predict a higher risk of death from COVID-19 and from all other causes of death. Immigrants from low- or middle-income countries had a higher risk of COVID-19 mortality but not for other causes of death.
The Stockholm data presented here augments this base of knowledge. On top of adding very granular individual and group-level information, we include data on hospitalization with over two years of follow-up encompassing five distinct COVID-19 waves. The greater Stockholm area has been the epicenter of the pandemic in Sweden and indeed in all of Scandinavia [21]. This could partly be explained by the fact that the region shares many traits of other European large cities with regard to precarious employment, crowded housing, and foreign-born inhabitants. The fact that individual factors, such as older age, lower income, less education as well as contextual factors — the type of area one resides in — are all associated with increased risk of hospitalization or death is paramount for politicians, policy makers, and health care personnel. This knowledge allows for targeted outreach, when striving to contain potential new variants of the SARS-CoV-2 virus, or indeed other transmissible diseases. To be specific, exploring and explaining the intersection between risk factors at the geographical area level and individual risk factors has implications for our ability to intervene in an optimal way. If, for example, the individual age was the most important factor, interventions need to reach that demographic group independently of where they live. However, as clearly demonstrated here, certain geographic area traits carry independent additional risk; interventions need to be focused towards high-risk areas and especially on old people residing in such areas. Support focused on those not born in Sweden could have had significant health benefits during the first year of the pandemic and must be improved in the future.
This investigation has strengths. The Region Stockholm real-time COVID-19 monitoring framework makes a detailed analysis of risk factors for COVID-19-related mortality and hospitalization quite simple. We have complete coverage of the entire greater Stockholm area population and all deaths and hospitalizations due to COVID-19 for the whole study period. Data resolution is exceptional, with individual data on education, income, work situation, living area, and living condition as well as the country of origin and co-morbid conditions. Additionally, we present unique sociodemographic properties on an area level; including population density, average income, age groups and data on foreign-born inhabitants. The Stockholm Syndrome described here, with large swaths of low-income workers, unable to work from home, and residing in crowded households may, as mentioned above, be quite generalizable. These are conditions rampant in many larger cities across the continent and in the world. These findings and these circumstances are likely to have an impact beyond COVID-19. Yet, the findings should be interpreted with caution. Swedish data on COVID-19 deaths is considered accurate, the National Board of Health and Welfare reports all cases where the underlying cause of death was COVID-19, regardless of whether the diagnosis was laboratory-confirmed or not [22]. Persons ill enough to seek hospital care will be admitted (the Swedish health care system is not based on private insurance). However, it is impossible to rule out that inequalities in hospitalization due to COVID-19 might partly be affected by differences in health-seeking behavior. Certain individuals may have a lower bar for seeking medical attention. In contrast, others may have the ability to “navigate” the health care system more efficiently; one needs to be aware of this when using hospital admission as a proxy for the severity of the disease. With this said, it is not self-evident in which direction this would skew the risk estimates. Additionally, some findings, like the fact that areas with more elderly people had a lower risk of hospitalization may seem counterintuitive. We can only speculate, but the adherence to regional and national recommendations, such as avoiding shopping, avoiding crowds, and general stay-at-home-recommendations, is likely higher among the elderly. Dichotomizing Stockholm residents into born in Sweden vs not born in Sweden and not taking into account time spent in Sweden may blunt our ability to draw conclusions regarding this variable. Lastly, the risks of death in areas that were hit hard by the pandemic could — despite our best efforts to adjust for all individual factors — be driven by residual confounding. At the same time — for policy makers in the healthcare sector — that does not matter. Our findings clearly indicate where and to whom we should focus governmental resources.
Conclusions
segregation and deprivation are well-known public health issues. This study from Stockholm, Sweden shows that the risk of hospitalization and death from COVID-19 is increased by area factors, such as population density, the number of people born in Sweden on top of aspects like the inability to work from home and living in crowded housing. In combination, these add to known individual risk factors such as male sex, high age, and cardiac, renal, liver, and other comorbidities [15]. Even when correcting for all known individual risk factors, residing in the highest-risk areas is associated with a more than doubled risk of dying from COVID-19. This finding, in conjunction with the aforementioned individual risk factors, is paramount for governments, agencies, and healthcare institutions interested in targeted interventions such as vaccine outreach for the elderly residing in high-risk areas. The interaction between sociodemographic factors and the virus is very clear; an insight that can help how we deal with future strains of SARS-CoV-2 or other pandemics.
Supplementary Information
Additional file 1: Figure S1. Area level covariates for the principal components analysis, creating the neighborhood deprivation score. Table S1. Risk of covid-19 death among residents 18 years and older (n= 1 722 444) divided by residential area* in Stockholm Region. Follow-up between 1st of March 2020 to the 28th of February 2021, Individuals living in elderly care facilities or with home-care service excluded.
Acknowledgements
The authors wish to thank the staff at the Center for Epidemiology and Community Medicine, Region Stockholm.
Abbreviations
- CI
Confidence interval
- COVID-19
The coronavirus disease 2019
- ISCO
International standard classification of occupations
- LISA
Integrated Database For Labor Market Research
- NDS
Neighborhood deprivation score
- RR
Relative risk
- RTB
Total Population Register
- SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2
- SSYK
Standard for Swedish occupational classifications
- VAL
Swedish: Vård Analys Lager, the Stockholm Regional Healthcare Data Warehouse
Authors’ contributions
All authors read and approved the final manuscript. MB: Conceptualization of the project, methodology, project leading, writing, editing the manuscript, and expertise in the clinical field of COVID-19. MH: Conceptualization of the project, methodology, and writing the manuscript. SF: Data curation, study design, and data analysis. PT: Data curation, study design, and data analysis. AP: Data curation, study design, and data analysis. AL: Conceptualization, funding acquisition, methodology, and writing — review and editing.
Funding
Open access funding provided by Karolinska Institute.
Availability of data and materials
Swedish privacy law prohibits us from making registered data publicly available. The data supporting our findings were used under license and ethical approval for the current study. Readers interested in obtaining microdata or replicating our study may seek similar approvals and inquire through Statistics Sweden. For further advice see: https://www.scb.se/en/services/guidance-for-researchers-and-universities/, or contact Statistics Sweden at: mikrodata@scb.se.
Declarations
Ethics approval and consent to participate
Regional Ethical Review Board, Stockholm (2021–00810).
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wildman J. COVID-19 and income inequality in OECD countries. Eur J Health Econ. 2021;22(3):455–462. doi: 10.1007/s10198-021-01266-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Su D, Alshehri K, Pagan J. Income inequality and the disease burden of COVID-19: Survival analysis of data from 74 countries. Prev Med Rep. 2022;27:101828. doi: 10.1016/j.pmedr.2022.101828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and mortality among black patients and white patients with Covid-19. N Engl J Med. 2020;382(26):2534–2543. doi: 10.1056/NEJMsa2011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Webb Hooper M, Napoles AM, Perez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. 2020;323(24):2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel AP, Paranjpe MD, Kathiresan NP, Rivas MA, Khera AV. Race, socioeconomic deprivation, and hospitalization for COVID-19 in English participants of a national biobank. Int J Equity Health. 2020;19(1):114. doi: 10.1186/s12939-020-01227-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease C, Prevention 2009 pandemic influenza A (H1N1) virus infections - Chicago, Illinois, April-July 2009. MMWR Morb Mortal Wkly Rep. 2009;58(33):913–918. [PubMed] [Google Scholar]
- 7.Quinn SC, Kumar S, Freimuth VS, Musa D, Casteneda-Angarita N, Kidwell K. Racial disparities in exposure, susceptibility, and access to health care in the US H1N1 influenza pandemic. Am J Public Health. 2011;101(2):285–293. doi: 10.2105/AJPH.2009.188029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carlsson AC, Wandell P, Osby U, Zarrinkoub R, Wettermark B, Ljunggren G. High prevalence of diagnosis of diabetes, depression, anxiety, hypertension, asthma and COPD in the total population of Stockholm, Sweden - a challenge for public health. BMC Public Health. 2013;13(1):670. doi: 10.1186/1471-2458-13-670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim JL, Reuterwall C, Heurgren M, Olausson PO. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11:450. doi: 10.1186/1471-2458-11-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ludvigsson JF, Almqvist C, Bonamy AK, Ljung R, Michaelsson K, Neovius M, Stephansson O, Ye W. Registers of the Swedish total population and their use in medical research. Eur J Epidemiol. 2016;31(2):125–136. doi: 10.1007/s10654-016-0117-y. [DOI] [PubMed] [Google Scholar]
- 11.Ludvigsson JF, Svedberg P, Olen O, Bruze G, Neovius M. The longitudinal integrated database for health insurance and labour market studies (LISA) and its use in medical research. Eur J Epidemiol. 2019;34(4):423–437. doi: 10.1007/s10654-019-00511-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rolfhamre P, Jansson A, Arneborn M, Ekdahl K. SmiNet-2: description of an internet-based surveillance system for communicable diseases in Sweden. Euro Surveillance. 2006;11(5):103–107. [PubMed] [Google Scholar]
- 13.Ludvigsson JF, Otterblad-Olausson P, Pettersson BU, Ekbom A. The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol. 2009;24(11):659–667. doi: 10.1007/s10654-009-9350-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zadori N, Vancsa S, Farkas N, Hegyi P, Eross B, Group KS The negative impact of comorbidities on the disease course of COVID-19. Intensive Care Med. 2020;46(9):1784–1786. doi: 10.1007/s00134-020-06161-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hergens MP, Bell M, Haglund P, Sundstrom J, Lampa E, Nederby-Ohd J, Ostlund MR, Cars T. Risk factors for COVID-19-related death, hospitalization and intensive care: a population-wide study of all inhabitants in Stockholm. Eur J Epidemiol. 2022;37(2):157–165. doi: 10.1007/s10654-021-00840-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Initiative S. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 17.Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, Sorensen HT, von Elm E, Langan SM, Committee RW. The REporting of studies conducted using observational routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12(10):e1001885. doi: 10.1371/journal.pmed.1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ehlert A. The socio-economic determinants of COVID-19: a spatial analysis of German county level data. Socio Econ Plan Sci. 2021;78:101083. doi: 10.1016/j.seps.2021.101083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kjøllesdal M, Skyrud K, Gele A, Arnesen T, Kløvstad H, Diaz E, Indseth T. The correlation between socioeconomic factors and COVID-19 among immigrants in Norway: a register-based study. Scand J Public Health. 2022;50(1):52–60. 10.1177/14034948211015860. [DOI] [PMC free article] [PubMed]
- 20.Drefahl S, Wallace M, Mussino E, Aradhya S, Kolk M, Branden M, Malmberg B, Andersson G. A population-based cohort study of socio-demographic risk factors for COVID-19 deaths in Sweden. Nat Commun. 2020;11(1):5097. doi: 10.1038/s41467-020-18926-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Welfare NBoHa: Statistics on COVID-19. In.; 2021.
- 22.Welfare NBoHa. In.; 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Figure S1. Area level covariates for the principal components analysis, creating the neighborhood deprivation score. Table S1. Risk of covid-19 death among residents 18 years and older (n= 1 722 444) divided by residential area* in Stockholm Region. Follow-up between 1st of March 2020 to the 28th of February 2021, Individuals living in elderly care facilities or with home-care service excluded.
Data Availability Statement
Swedish privacy law prohibits us from making registered data publicly available. The data supporting our findings were used under license and ethical approval for the current study. Readers interested in obtaining microdata or replicating our study may seek similar approvals and inquire through Statistics Sweden. For further advice see: https://www.scb.se/en/services/guidance-for-researchers-and-universities/, or contact Statistics Sweden at: mikrodata@scb.se.