Abstract
Introduction
Lockdown restrictions due to the COVID-19 pandemic have reduced the number of injuries recorded. However, little is known about the impact of easing COVID-19 lockdown restrictions on the nature and outcome of injuries. This study aims to compare injury patterns prior to and after the easing of COVID-19 lockdown restrictions in Saudi Arabia.
Method
Data were collected retrospectively from the Saudi TraumA Registry for the period between March 25, 2019, and June 21, 2021. These data corresponded to three periods: March 2019–February 2020 (pre-restrictions, period 1), March 2020–June 2020 (lockdown, period 2), and July 2020–June 2021 (post easing of restrictions, period 3). Data related to patients’ demographics, mechanism and severity of injury, and in-hospital mortality were collected and analysed.
Results
A total of 5,147 traumatic injury patients were included in the analysis (pre-restrictions n = 2593; lockdown n = 218; post easing of lockdown restrictions n = 2336). An increase in trauma cases (by 7.6%) was seen in the 30–44 age group after easing restrictions (n = 648 vs. 762, p < 0.01). Motor vehicle crashes (MVC) were the leading cause of injury, followed by falls in all the three periods. MVC-related injuries decreased by 3.1% (n = 1068 vs. 890, p = 0.03) and pedestrian-related injuries decreased by 2.7% (n = 227 vs. 143, p < 0.01); however, burn injuries increased by 2.2% (n = 134 vs. 174, p < 0.01) and violence-related injuries increased by 0.9% (n = 45 vs. 60, p = 0.05) post easing of lockdown restrictions. We observed an increase in in-hospital mortality during the period of 12 months after easing of lockdown restrictions—4.9% (114/2336) compared to 12 months of pre-lockdown period—4.3% (113/2593).
Conclusion
This is one of the first studies to document trauma trends over a one-year period after easing lockdown restrictions. MVC continues to be the leading cause of injuries despite a slight decrease; overall injury cases rebounded towards pre-lockdown levels in Saudi Arabia. Injury prevention needs robust legislation with respect to road safety measures and law enforcement that can decrease the burden of traumatic injuries.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-023-14981-9.
Keywords: Covid-19, Pandemic, Easing restrictions, Injury, Major trauma, Motor Vehicle Crashes
Introduction
Coronavirus disease 2019 (COVID-19) was discovered in December 2019 in Wuhan, China [1]. Since then, the virus has spread rapidly worldwide. On January 30, 2020, the World Health Organization (WHO) announced the outbreak as a public health emergency of international concern and declared it a global pandemic on March 11, 2020 [2]. This outbreak of COVID-19 has forced many countries worldwide to enforce societal lockdowns and policies to contain the rapid infection spread. In Saudi Arabia, the first case of COVID-19 was reported on March 2, 2020, and cases soon increased exponentially [3]. The government of Saudi Arabia initiated restrictions from early March 2020; such restrictions included suspension of schools, universities, social events and international flights. Furthermore, on April 6, 2020, a stay at home order was introduced in the capital city of Saudi Arabia, Riyadh [3]. On June 21, 2020, the lockdown restrictions were lifted from all regions across the country and life returned to near-normal, with adherence to health instructions and maintenance of social distancing [3].
Traumatic injury is a leading cause of death and disability worldwide [4, 5]. The COVID-19 pandemic and the government’s restriction policies designed to fight this pandemic have undoubtedly affected the incidence of injury. For example, recent evidence showed that mandated lockdown restrictions resulted in significant reduction in injury-related road trauma by 42.6%, but increased household and assault injuries by 9.9% and 7%, respectively [6–8]. In Saudi Arabia, traumatic injuries, particularly injuries arising from motor vehicle crashes (MVC), are a major public health problem [9–12]. A recently published study reported a significant reduction in injuries by 26.8% during the country-wide lockdown [13]. A reduction in injury incidence was also seen in other countries such as Australia [14], Ireland [15], New Zealand [16] and South Africa [17].
There are limited studies describing the impact of lifting COVID-19 lockdown restrictions on traumatic injuries. It is anticipated that injury cases would rebound towards pre-lockdown levels because people will travel more and practice sports after lockdowns end. The patterns and outcome of injuries after easing lockdown restrictions in the Middle East, and specifically in Saudi Arabia, are unknown. This study aims to assess the impact of easing COVID-19 lockdown restrictions on traumatic injuries in Saudi Arabia.
Materials and methods
Data were extracted retrospectively from King Saud Medical City (KSMC) trauma registry known as the Saudi TraumA Registry (STAR). KSMC is located in Riyadh and is one of the few major trauma centres in Saudi Arabia with a bed capacity of 1,400. Approximately 350 visits are recorded per day to the emergency department (ED) and more than 300 trauma cases are seen per month [18]. The registry collects data of injury patients meeting any of the following criteria:
1. Principal diagnosis of injury, and
2. Death in the ED after injury, or
3. Inpatient admission ≥ 3 calendar days, or
4. Inpatient death following injury, or
5. Admission to the Intensive Care Unit (ICU)
This study included all traumatic injury patients who met the KSMC registry criteria and presented to the ED or admitted to the hospital between March 25, 2019, and June 21, 2021. These data correspond to three periods: March 25, 2019–March 24, 2020 (pre-restrictions, period 1, 12 months), March 25, 2020–June 21, 2020 (lockdown, period 2, 3 months) and June 22, 2020–June 21, 2021 (post easing of restrictions, period 3, 12 months). Data regarding injury events and patients’ characteristics such as demographics, time and place of injury, mechanism and severity of injury, definitive care mode of arrival were extracted from the STAR. Other variables included prehospital and in-hospital vital signs such as systolic blood pressure (SBP), heart rate (HR) and respiratory rate (RR). Furthermore, ED and in-hospital outcomes were included in the data analyses.
Although the focus of this study is comparing one year of injury data before and after easing of the lockdown restrictions, our data was extracted continuously from March 2019 to June 2021, including a three-month lockdown period. Therefore, injury data during the lockdown phase were included in this study as phase 2 (March 25, 2020–June 21, 2020).
Statistical analyses
Statistical analyses were performed using the R program for statistical computing, version R-4.1.1. Frequencies and percentages in each time period and for the total study population are reported for categorical variables such as age group, mechanism of injury, place of injury, type of injury and mode of arrival. Continuous variables such as prehospital and in-hospital vital signs are reported with mean and standard deviation (SD) or with median and interquartile range where appropriate. ICU admissions and in-hospital mortality are presented as frequencies and percentages. The significance of changes in variable distributions and/or means between periods 1 (pre restrictions) and 3 (post easing of restrictions), Chi-square test was used and the Student's t-test for independent samples or Mann–Whitney U test for continuous variables as appropriate. The three-month lockdown data are only presented as descriptive data; the comparison of injury characteristics, pattern, volume and outcome focused more on pre and post easing of COVID-19 restrictions. We did not focus on the lockdown phase because this period was previously studied in Riyadh, Saudi Arabia [13].
In this study, univariate analyses were performed to identity predictors of in-hospital mortality for time periods 1 and 3. Factors associated significantly with the dependent variable were entered into a multivariable logistic regression model. Furthermore, multivariable logistic regression modelling was also used to predict ICU admissions (dependent variable (DV)) by the mechanism of injury (including motor vehicle, motorcycle/pedal cyclist, pedestrian, fall, assault, burn and penetrating—independent variables (IV)) for periods 1 (pre restrictions) and 3 (post easing of restrictions). The two regression models are presented individually for the periods of pre and post easing of restrictions and adjusted for covariates including age and gender. The adjusted odds ratios (AOR) and 95% confidence intervals (CIs) were calculated with respect to the likelihood of difference between periods 1 and 3. The level for statistical significance was a p value of < 0.05 in all analyses. This study was approved by the Institutional Review Board Committee at King Saud Medical City (H1RI-20–June21-01).
Results
Demographic and clinical characteristics
A total of 5,147 traumatic injury patients were admitted over the study period: March 25, 2019–June 21, 2021. During the periods that were investigated, of the 5,147 patients; 2,593 (50.3%) patients were in the pre-restrictions group (period 1), 218 (4.3%) patients were in the lockdown group (period 2), and 2,336 (45.4%) patients were in post easing of lockdown restrictions group (period 3). Table 1 shows the characteristics of the study population in each of the three time periods and overall. Tests of significance of change were only undertaken for comparisons of periods 1 and 3.
Table 1.
Demographic and presentation characteristics of traumatic injury patients of pre-restrictions, restrictions/lockdown, and after easing the restrictions
| Variables | Total | Pre-restrictions | Lockdown$ | After easing restrictions | % changes | P value |
|---|---|---|---|---|---|---|
| Period 1 12 months |
Period 2 3 months |
Period 3 12 months |
P1 to P3 | |||
| N = 5147 | N = 2593 | N = 218 | N = 2336 | -5.2 | ||
| Mean age in years (SD) | 33 (17.5) | 32.6 (17.6) | 32 (16.2) | 34 (17.5) | ||
| Age group, n (%) | 5147 | 2593 | 218 | 2336 | ||
| 0–14 | 462 (9) | 252 (9.7) | 22 (10.1) | 188 (8) | -1.7 | 0.05* |
| 15–29 | 2097 (40.7) | 1160 (44.7) | 77 (35.3) | 860 (36.8) | -7.9 | < 0.01* |
| 30–44 | 1488 (28.9) | 648 (25) | 78 (35.7) | 762 (32.6) | + 7.6 | < 0.01* |
| 45–59 | 631 (12.3) | 302 (11.6) | 24 (11) | 305 (13.1) | + 1.5 | 0.14 |
| ≥ 60 | 469 (9.1) | 231 (8.9) | 17 (7.8) | 221 (9.5) | + 0.6 | 0.53 |
| Gender n (%) | 5147 | 2593 | 218 | 2336 | ||
| Male | 4337 (84.3) | 2170 (83.7) | 190 (87.1) | 1977 (84.6) | + 0.9 | 0.38 |
| Female | 810 (15.7) | 423 (16.3) | 28 (12.8) | 359 (15.4) | -0.9 | |
| Injury time, n (%) | 2540 | 1335 | 99 | 1106 | ||
| AM | 1138 (44.8) | 588 (44) | 43 (43.4) | 507 (45.8) | + 1.8 | 0.39 |
| PM | 1402 (55.2) | 747 (56) | 56 (56.6) | 599 (54.2) | -1.8 | |
| Mechanism of injury, n (%) | 5147 | 2593 | 218 | 2336 | ||
| Motor Vehicle | 2043 (39.7) | 1068 (41.2) | 85 (38.9) | 890 (38.1) | -3.1 | 0.03* |
| Motorcycle | 182 (3.5) | 91 (3.5) | 1 (0.5) | 90 (3.9) | + 0.4 | 0.57 |
| Pedal cyclist | 20 (0.4) | 7 (0.3) | 3 (1.4) | 10 (0.4) | + 0.1 | 0.48 |
| Pedestrian | 381 (7.4) | 227 (8.8) | 11 (5) | 143 (6.1) | -2.7 | < 0.01* |
| Fall > 1 m | 827 (16.1) | 384 (14.8) | 40 (18.3) | 403 (17.3) | + 2.5 | 0.02* |
| Fall ≤ 1 m | 832 (16.2) | 435 (16.8) | 30 (13.8) | 367 (15.7) | -1.1 | 0.33 |
| Assault/violence | 107 (2.1) | 45 (1.7) | 2 (0.9) | 60 (2.6) | + 0.9 | 0.05* |
| Burn | 333 (6.5) | 134 (5.2) | 25 (11.5) | 174 (7.4) | + 2.2 | < 0.01* |
| Accidental | 260 (5.1) | 121 (4.7) | 12 (5.5) | 127 (5.4) | + 0.7 | 0.24 |
| Penetrating | 154 (2.9) | 77 (2.9) | 9 (4.1) | 68 (2.9) | 0 | 0.97 |
| Other | 8 (0.2) | 4 (0.2) | 0 (0) | 4 (0.2) | 0 | |
| Injury place n (%) | 3367 | 1742 | 124 | 1501 | ||
| Farm | 25 (0.7) | 19 (1.1) | 0 (0) | 6 (0.4) | -0.7 | 0.03* |
| Home | 583 (17.3) | 252 (14.5) | 22 (17.7) | 309 (20.6) | + 6.1 | < 0.01* |
| Industrial | 111 (3.3) | 64 (3.7) | 2 (1.6) | 45 (3) | -0.7 | 0.23 |
| School | 9 (0.3) | 7 (0.4) | 0 (0) | 2 (0.1) | -0.3 | 0.23 |
| Road | 2606 (77.4) | 1379 (79.1) | 100 (80.6) | 1127 (75.1) | -4 | < 0.01* |
| Sports | 33 (1) | 21 (1.2) | 0 (0) | 12 (0.8) | -0.4 | 0.27 |
| Injury type, n (%) | 9582 | 4891 | 430 | 4261 | ||
| Head | 1350 (14.1) | 707 (14.5) | 66 (15.3) | 577 (13.5) | -1 | 0.04* |
| Face | 939 (9.8) | 492 (10.1) | 46 (10.7) | 401 (9.4) | -0.7 | 0.11 |
| Neck | 33 (0.3) | 19 (0.4) | 1 (0.2) | 13 (0.3) | -0.1 | 0.55 |
| Thorax | 1235 (12.9) | 631 (12.9) | 63 (14.6) | 541 (12.7) | -0.2 | 0.35 |
| Abdomen & pelvic | 461 (4.8) | 243 (4.9) | 17 (4) | 201 (4.7) | -0.2 | 0.37 |
| Spine | 1597 (16.7) | 773 (15.8) | 76 (17.7) | 748 (17.6) | + 1.8 | 0.09 |
| Upper extremities | 1306 (13.6) | 694 (14.2) | 50 (11.6) | 562 (13.2) | -1 | 0.03* |
| Lower extremities | 2246 (23.4) | 1135 (23.2) | 86 (20) | 1025 (24.1) | -0.9 | 0.96 |
| Other trauma | 415 (4.3) | 197 (4) | 25 (5.8) | 193 (4.5) | + 0.5 | 0.42 |
| Prehospital physiological assessment, mean (SD) | ||||||
| First systolic BP | 124.8 (21.6) | 125.2 (21.8) | 122.3 (22.9) | 124.5 (21.3) | 0.59 | |
| First heart rate | 93.1 (18.3) | 94.7 (19.2) | 93.6 (18.2) | 91 (1) | < 0.01* | |
| First RR | 17.8 (3.7) | 18.1 (4) | 18.2 (3.2) | 17.3 (3.4) | < 0.01* | |
| Definitive Care Mode of Arrival, n (%) | 4456 | 2268 | 183 | 2005 | ||
| Red Crescent ambulance | 1272 (28.5) | 632 (27.9) | 46 (25.1) | 594 (29.6) | + 1.7 | 0.41 |
| Private ambulance | 87 (1.9) | 58 (2.5) | 4 (2.2) | 25 (1.2) | -1.3 | < 0.01* |
| Government ambulance | 2032 (45.6) | 963 (42.5) | 105 (57.4) | 964 (48.1) | + 5.6 | < 0.01* |
| Helicopter | 52 (1.2) | 35 (1.5) | 0 (0) | 17 (0.8) | -0.7 | 0.05* |
| Private/police vehicle | 1013 (22.7) | 580 (25.6) | 28 (15.3) | 405 (20.2) | -5.4 | |
| Trauma Team Activation, n (%) | 5126 | 2583 | 217 | 2326 | ||
| Yes | 358 (7) | 221 (8.6) | 26 (12) | 111 (4.8) | -3.8 | < 0.01* |
| No | 4768 (93) | 2362 (91.4) | 191 (88) | 2215 (95.2) | + 3.8 | < 0.01* |
| Blood transfusion in ED, n (%) | 5139 | 2591 | 217 | 2331 | ||
| Yes | 192 (3.7) | 112 (4.3) | 11 (5.1) | 69 (2.9) | -1.4 | 0.02* |
| No | 4947 (96.3) | 2479 (95.7) | 206 (94.9) | 2262 (97.1) | -1.4 | |
| On arrival at the ED, mean (SD) | ||||||
| First systolic BP | 126.4 (21.8) | 126.8 (22.7) | 126.5 (22.3) | 126 (20.8) | -1.9 | 0.23 |
| First heart rate | 94 (19.2) | 94.3 (19.8) | 94.7 (20.7) | 93.7 (18.4) | -1.4 | 0.22 |
| First RR | 19.9 (3) | 20 (3) | 19.9 (2.8) | 19.8 (2.9) | -0.1 | 0.20 |
| First O2 saturation | 98 (2) Μ | 98 (3) Μ | 98 (2) Μ | 98 (2) Μ | ||
| Respiratory assistance, n (%) | 5052 | 2533 | 215 | 2304 | ||
| Assisted respiration | 768 (15.2) | 445 (17.6) | 33 (15.3) | 290 (12.6) | -5 | < 0.01* |
| Unassisted respiration | 4284 (84.8) | 2088 (82.4) | 182 (85.1) | 2014 (87.4) | + 5 | < 0.01* |
Period 1 = March 25, 2019 – March 24, 2020; Period 2 = March 25 – June 21, 2020; Period 3 = June 22, 2020 – June 21, 2021
IQR Interquartile Range, BP Blood Pressure, RR Respiratory Rate
% changes = change in value After easing restrictions compared to Pre-restrictions
P-value: Represent a calculation between period 1 and 3 groups
*Significant P-value
ΜMedian
$The lockdown column is just there for completeness
Comparing period 1 (pre restrictions, 12 months) and period 3 (post easing of restrictions, 12 months), there was a reduction in the total number of trauma cases by 5.2% post easing of restrictions. There were also changes in the distribution of cases by age group; we observed a reduction of 1.7% with respect to the proportion of trauma cases in the age group of < 14 years (n = 252 (9.7%) vs 188 (8%), p = 0.05), and of 7.9% with respect to the age group of 15–29 years (n = 1160 (44.7%) vs 860 (36.8%), p < 0.01); however, a significant increase of 7.6% was seen in those aged 30–44 years, post easing of restrictions (n = 648 (25%) vs 762 (32.6%), p < 0.01). The post easing of restrictions group saw a reduction in trauma team activation by 3.8% (n = 221 (8.6%) vs 111 (4.8%), p < 0.01). There was no significant difference between the numbers of prehospital and in-hospital physiological assessments conducted in the ED or hospital admissions between the two periods; however, the proportion of patients requiring respiratory assistance decreased by 5% post lockdown (n = 445 (17.6%) vs 290 (12.6%), p < 0.01). Incidences of private/police vehicles as modes of arrival decreased by 5.4% (n = 580 (25.6%) vs 405 (20.2%), p < 0.01) post lockdown. We observed a change in the type of injury, including a reduction in head injury by 1% (n = 707 (14.5%) vs 577 (13.5%), p = 0.04) and injury to upper extremities by 1% (n = 694 (14.2%) vs 562 (13.2%), p = 0.03).
Mechanism of injury
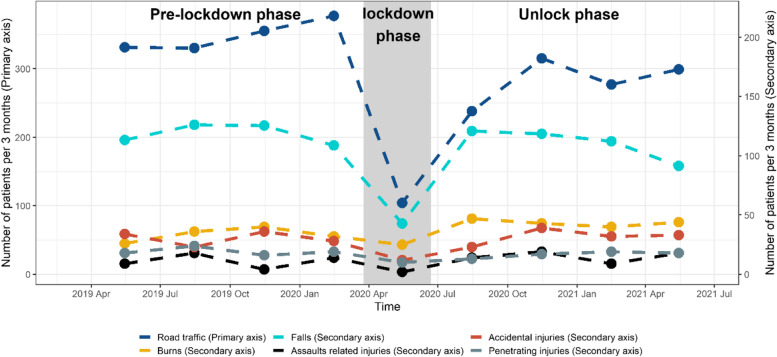
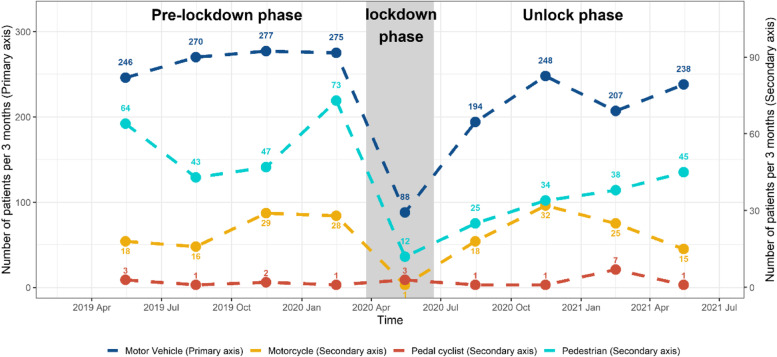
Overall, 1,402 (55.2%) injury events occurred in PM time, while 1,138 (44.8%) injury cases occurred in AM time. The definition of PM and AM is referring to clock times between noon and midnight and midnight to noon, respectively. The main mechanism of injury over the whole study period was MVC (n = 2043, 39.7%), followed by falls (n = 1659, 32.3%). Comparing injury mechanisms between pre and post lockdown periods, incidences of MVC-related injury reduced by 3.1% (n = 1068 (41.2%) vs 890 (38.1%), p = 0.03) and pedestrian injury decreased by 2.7% (n = 227 (8.8%) vs 143 (6.1%), p < 0.01). However, burn and home-related injuries increased by 2.2% (n = 134 (5.2%) vs 174 (7.4%), p < 0.01) and 6.1% (n = 252 (14.5%) vs 309 (20.6%), p < 0.01), respectively, after easing of lockdown restrictions. There was an increase of 2.5% in fall injuries > 1 m (n = 384 (14.8%) vs 403 (17.3%), p = 0.02) and a rise of 0.9% in assault/violence-related injuries (n = 45 (1.7%) vs 60 (2.6%), p = 0.05) post easing of lockdown restrictions (Figs. 1 and 2).
Fig. 1.
The mechanism of injury across the three periods
Fig. 2.
The mechanism of injury by road trauma across the three periods
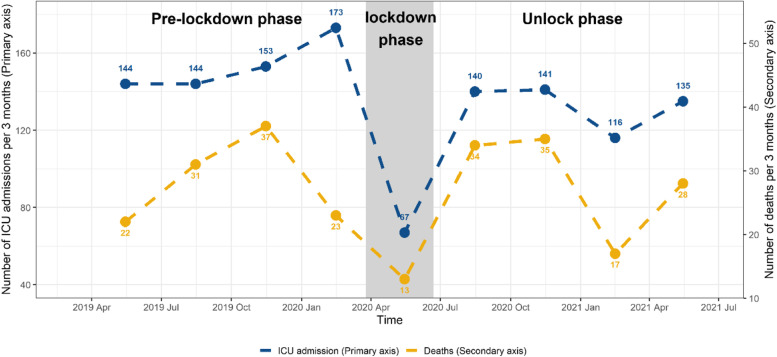
Patient outcomes
The median injury severity score (ISS) was nine, and ICU admission was seen in 1,213 cases (23.6% of the study population) (Fig. 3). There was a reduction in cases of low level of consciousness, indicated by a Glasgow Coma Scale (GCS) score of 3 to 8 by 3.7% (n = 245 (13.1%) vs 174 (9.4%), p < 0.01) and a reduction in the severity of injury (ISS > 40) by 0.7% (n = 42 (1.6%) vs 21 (0.9%), p = 0.03) after lifting of the lockdown restrictions. Transfer of patients from the ED to the operating theatre reduced by 2.2% (n = 137 (5.3%) vs 72 (3.1%), p < 0.01) after easing of the lockdown restrictions. There was no change in the length of ICU stay between the two periods (median was nine days); however, the length of hospital stay (LOHS) increased by a day compared with pre restrictions (median was eight days compared to nine days for the post lifting of restrictions group). The overall in-hospital mortality was 4.7% (240/5147). We observed an increase in in-hospital mortality in the 12 months after easing of lockdown restrictions compared to the 12 months before the lockdown, i.e., 4.9% (114/2336) and 4.3% (113/2593) p = 0.42, respectively. Table 2 shows patient outcomes following injury events.
Fig. 3.
The number of ICU admissions and deaths across the three periods
Table 2.
Level of consciousness, injury severity, and patient outcome following injury events
| Variables and outcomes | Total | Pre-restrictions | Lockdown$ | After easing restrictions | % changes P1 to P3 | P value |
|---|---|---|---|---|---|---|
| Period 1 12 months |
Period 2 3 months |
Period 3 12 months |
||||
| N = 5147 | N = 2593 | N = 218 | N = 2336 | -5.2 | ||
| GCS score, n (%) | 3869 | 1866 | 142 | 1861 | ||
| 13 − 15 | 3325 (85.9) | 1553 (83.2) | 117 (82.4) | 1655 (88.9) | + 5.7 | < 0.01* |
| 9 − 12 | 106 (2.7) | 68 (3.6) | 6 (4.2) | 32 (1.7) | -1.9 | < 0.01* |
| 3 − 8 | 438 (11.3) | 245 (13.1) | 19 (13.4) | 174 (9.4) | -3.7 | < 0.01* |
| ISS, Median (IQR) | 9 (12) | 9 (10) | 9 (14) | 9 (10) | 0.39 | |
| ISS, n (%) | 5140 | 2591 | 217 | 2332 | ||
| ≤ 15 | 3854 (71.1) | 1957 (75.5) | 147 (67.7) | 1750 (75) | -0.5 | 0.72 |
| 16–25 | 886 (16.4) | 432 (16.7) | 43 (19.8) | 411 (17.6) | + 0.9 | 0.39 |
| 26–40 | 331 (6.4) | 160 (6.2) | 21 (9.7) | 150 (6.4) | + 0.2 | 0.75 |
| > 40 | 69 (1.3) | 42 (1.6) | 6 (2.8) | 21 (0.9) | -0.7 | 0.03* |
| Disposition from ED, n (%) | 5122 | 2582 | 217 | 2323 | ||
| Ward | 3939 (76.9) | 1972 (76.4) | 155 (71.4) | 1812 (78) | + 1.6 | 0.22 |
| ICU | 965 (18.8) | 473 (18.3) | 53 (24.4) | 439 (18.8) | + 0.5 | 0.64 |
| Operating theatre | 218 (4.2) | 137 (5.3) | 9 (4.1) | 72 (3.1) | -2.2 | < 0.01* |
| ICU admission, n (%) | 5140 | 2591 | 217 | 2332 | 0.50 | |
| Yes | 1213 (23.6) | 614 (23.7) | 65 (30) | 534 (22.9) | -0.8 | |
| No | 3927 (76.4) | 1977 (76.3) | 152 (70) | 1798 (77.1) | + 0.8 | |
| Days in ICU (in days)** | ||||||
| Median (IQR) | 9 (14) | 9 (14) | 6 (14) | 9 (14) | 0.47 | |
| Days in hospital (in days) | ||||||
| Median (IQR) | 8 (12) | 8 (13) | 8 (12) | 9 (12) | 0.76 | |
| In-hospital mortality, n (%) | 240 (4.7) | 113 (4.3) | 13 (6) | 114 (4.9) | + 0.6 | 0.42 |
Period 1 = March 25, 2019 – March 24, 2020; Period 2 = March 25 – June 21, 2020; Period 3 = June 22, 2020 – June 21, 2021
GCS Glasgow Coma Scale, ISS Injury Severity Score, ED Emergency Department, ICU Intensive Care Unit, IQR Interquartile Range
P-value: Represent a calculation between period 1 and 3 groups
*Significant P-value
**Patients who spent 1 day or more in ICU
$The lockdown column is just there for completeness
Risk factors for ICU admission and/ or mortality
The results of unadjusted predictors of in-hospital mortality following injury events are shown in supplementary file, Appendix 1. The results of the multivariable logistic regression models show that age ≥ 60 was associated with an increased risk of mortality for both pre and post easing of restrictions (AOR = 12.85, 95% CIs 3.77–46.74, p < 0.01) and (AOR = 10.47, 95% CIs 2.88–43.90, p < 0.01), respectively. Patients who required operation on arrival were more likely to die in phase 1 (AOR = 4.65, 95% CIs 2.24–9.65, p < 0.01), but not in phase 3. Shorter length of stay in the ICU was significantly associated with mortality in phase 1 (AOR = 0.95, 95% CIs 0.91–0.97, p = 0.01) but not in phase 3 (Table 3).
Table 3.
Multivariable logistic regression model predicting in-hospital mortality
| Independent variable | Pre-restrictions Period 1 |
After easing restrictions Period 3 |
|---|---|---|
| Mortality | Mortality | |
| AOR (95% CI) P value | AOR (95% CI) P value | |
| Age | ||
| 0–14 | Ref | Ref |
| 15–29 | 0.84 (0.31 – 2.43) 0.741 | 0.93 (0.29 – 3.34) 0.910 |
| 30–44 | 2.43 (0.84 – 7.55) 0.112 | 1.06 (0.32 – 3.95) 0.927 |
| 45–59 | 1.62 (0.44 – 5.90) 0.461 | 1.19 (0.28 – 5.12) 0.808 |
| ≥ 60 | 12.85 (3.77 – 46.74) < 0.01 | 10.47 (2.88 – 43.90) < 0.01 |
| Physiological assessment | ||
| Hospital Pulse/heart rate | 1.01 (1.00 – 1.03) 0.021 | 0.99 (0.98 – 1.01) 0.741 |
| Hospital RR | 1.06 (1.00 – 1.11) 0.012 | 1.02 (0.96 – 1.08) 0.020 |
| Assisted respiration | 0.61 (0.25 – 1.44) 0.255 | 0.25 (0.08 – 0.75) 0.013 |
| Injury type | ||
| Head injury | 1.68 (0.77 – 3.72) 0.194 | 0.89 (0.36 – 2.17) 0.806 |
| Thorax injury | 0.87 (0.44 –1.72) 0.701 | 0.69 (0.33 – 1.43) 0.328 |
| Other trauma | 1.00 (0.23 – 3.55) 0.999 | 0.48 (0.11 – 2.25) 0.358 |
| Mechanism of injury | ||
| Fall | 2.28 (1.04 – 4.95) 0.038 | 1.81 (0.77 – 4.21) 0.168 |
| Burn | 9.97 (1.79 – 57.13) 0.01 | 27.33 (5.12 – 136.68) < 0.01 |
| Mode of arrival | ||
| Government Ambulance | 0.85 (0.42 – 1.75) 0.660 | 0.71 (0.33 – 1.53) 0.391 |
| Private police vehicle | 0.32 (0.07 – 1.06) 0.090 | 0.63 (0.21 – 1.65) 0.371 |
| GCS score | 0.74 (0.67 – 0.81) < 0.01 | 0.815 (0.73 – 0.90) < 0.01 |
| ISS | 1.05 (1.02 – 1.08) 0.01 | 1.06 (1.03 – 1.10) < 0.01 |
| Length of stay in ICU | 0.95 (0.91 – 0.97) 0.01 | 1.01 (0.98 – 1.03) 0.690 |
| Require operation | 4.65 (2.24 – 9.65) < 0.01 | 0.79 (0.24 – 2.21) 0.673 |
Period 1 = March 25, 2019 – March 24, 2020; Period 2 = March 25 – June 21, 2020; Period 3 = June 22, 2020 – June 21, 2021
RR Respiratory Rate, GCS Glasgow Coma Scale, ISS Injury Severity Score, ICU Intensive Care Unit
The mechanisms of injury significantly associated with ICU admission in period 1 were MVCs (AOR = 2.41, 95% CIs 1.72–3.45, p < 0.01), motorcycle/cyclists (AOR = 1.68, 95% CIs 1.05–2.68, p = 0.03), falls (AOR = 1.93, 95% CIs 1.30–2.92, p < 0.01), pedestrians (AOR = 0.70, 95% CIs 0.49–1.02, p = 0.05), burns (AOR = 5.76, 3.91–8.66, p < 0.01) and penetrating injuries (AOR = 1.69, 1.02–2.78, p = 0.04). However, only MVCs (AOR = 2.36, 95% CIs 1.47–3.99, p = 0.01) and burns (AOR = 5.56, 95% CIs 3.22–9.97, p < 0.01) were significantly associated with ICU admissions in period 3. Furthermore, burns were also significantly associated with in-hospital mortality in both periods, period 1 (AOR = 6.12, 95% CIs 3.18–13.02, p < 0.01) and period 3 (AOR = 8.58, 95% CIs 3.28–29.49, p < 0.01) (Table 4).
Table 4.
Adjusted predictors for ICU admission and in-hospital mortality by mechanism of injury
| Mechanism of injury, n (%) | Pre-restrictions Period 1 |
After easing restrictions Period 3 |
||
|---|---|---|---|---|
| ICU admission | Mortality | ICU admission | Mortality | |
| AOR (95% CI) P value | AOR (95% CI) P value | AOR (95% CI) P value | AOR (95% CI) P value | |
| Motor Vehicle | 2.41 (1.72–3.45) < 0.01 | 1.31 (0.71–2.71) 0.431 | 2.36 (1.47–3.99) 0.01 | 1.54 (0.61–5.19) 0.419 |
| Motorcycle/ cyclist | 1.68 (1.05–2.68) 0.030 | 0.28 (0.04–1.09) 0.107 | 1.57(0.80–3.09) 0.190 | No estimates due to small number |
| Fall | 1.93 (1.30–2.92) < 0.01 | 1.14 (0.52–2.63) 0.744 | 1.61(0.87–3.02) 0.133 | 1.24 (0.35–4.97) 0.742 |
| Pedestrian | 0.70 (0.49–1.02) 0.054 | 0.70 (0.36–1.48) 0.310 | 0.71 (0.42–1.23) 0.200 | 0.86 (0.32–2.99) 0.785 |
| Assault | 1.60 (0.90–2.79) 0.102 | 0.49 (0.07–1.90) 0.363 | 1.39 (0.61–3.03) 0.419 | 0.54 (0.03–3.76) 0.586 |
| Burn | 5.76 (3.91–8.66) < 0.01 | 6.12 (3.18–13.02) < 0.01 | 5.56 (3.22–9.97) < 0.01 | 8.58 (3.28–29.49) < 0.01 |
| Penetrating | 1.69 (1.02–2.78) 0.040 | 0.53 (0.12–1.78) 0.347 | 1.18 (0.53–2.56) 0.675 | 1.54 (0.30–7.19) 0.582 |
Discussion
To our knowledge, this is the first study that seeks to understand the impact of easing of COVID-19 lockdown restrictions on injuries in Saudi Arabia using clinical data and one of the first such studies internationally. Accessing data from a major trauma centre, this study explored a large number of injury variables such as demographics, mechanisms of injury, severity of injury and patient outcomes before and after easing of COVID-19 lockdown restrictions. Our study has observed a change in the demographics, the mechanisms of injury and the outcomes of the trauma after easing of restrictions. A reduction of 5.2% was observed in the overall volume of all injury admissions during the first 12 months post lifting of lockdown restrictions. A reduction in the proportion of cases resulting in an ICU admission and patients requiring surgery on arrival was seen in the post easing of restrictions period. This decrease might be attributed to a lower number of patients in the post restrictions period presenting with severe trauma and/or decreased level of consciousness.
Despite this, with respect to the risk of in-hospital mortality according to the mechanism of injury, there was no difference between the pre and post lockdown periods; however, we identified that motorcycle/pedal cycle, pedestrian, fall, and penetrating injuries were associated significantly with ICU admission in period 1 but not in period 3. Furthermore, we found that there was a 5% decrease in the odds of mortality for each additional day in ICU in period 1. We also witnessed a general decrease in the LOHS post easing of COVID-19 restrictions, but there was no change in the length of ICU stay in the two periods. It should be noted that the change in LOHS could be the result of COVID-19 infections, as hospitals possibly limited admissions during the COVID-19 outbreak and/or altered patient preferences, in addition to hastening patient discharge in order to limit potential exposure to the virus [19, 20].
Not surprisingly, the rates of injury at home and incidences of assault/violence increased significantly during the post lockdown period. Our findings are consistent with other studies that demonstrate the adverse psychological impact of COVID-19 on the global population [21, 22] which may have led to an increase in violence-related injuries [23, 24]. This psychological impact is expected to be long-lasting, persisting beyond the lockdown phase, because people may have lost family members, jobs or businesses during the virus outbreak [25]. These findings suggest that the causes of increased violence-related injuries should be investigated in future studies.
In this study, 45.6% of the patients arrived at the hospital by government ambulance; such patients are more likely to be referral patients because Saudi Red Crescent is the primary prehospital care provider in the country. However, transferring of patients between hospitals is usually undertaken by the Ministry of Health (MOH) ambulances (government ambulances). As a mode of arrival, there was no difference between Red Crescent ambulances and MOH ambulances between periods 1 and 3; however, a reduction in private vehicle/ police vehicle arrival was noted in period 3. One potential explanation for this decrease is the widespread COVID-19 infections, as the general public as well as the policymakers were cautious about transporting patients using their vehicles. There has also been a notable decrease in the ISS, suggesting that the overall injury burden was slightly lower in the pre as well as post lockdown groups.
In Saudi Arabia, road injuries are a major public health problem [9, 11]. With regard to the different etiologies of road trauma, although road trauma decreased post easing of restrictions, it is still the leading cause of injury across the three periods, causing around 50% of total trauma. We also reviewed the MOH statistics and indicators to identify the rate of road traffic mortality. The mortality was 5,754 cases in 2019 and 4,618 cases in 2020, which further shows that the burden of road traffic injury was significant even during the country-wide lockdown [26]. Given that an all-inclusive trauma system plays an essential part in decreasing mortality arising from road injuries [27, 28], there are opportunities to extend and strengthen the trauma care system in Saudi Arabia [9]. Moreover, injury prevention needs a robust community programme and legislation around road safety measures, including strict enforcement that can decrease the burden of traumatic injuries in the country.
Interestingly, there has been a significant increase in burn-related injuries both during and post lockdown periods. This could be the result of extended home schooling for several months after easing of lockdown restrictions as children spent more time at home [3]. We also found that the incidence of injury at home increased significantly in the post lockdown group. Hence, we are led to believe that lockdown prompted more cooking and dining activities at home, which is another possible contributor to the increased burn-related injuries.
With respect to the mechanism of injury, our study found that the most significant reduction was identified in the pedestrian population. Primary school students (years 1–6) are yet to return to on-site learning as of October 2021, which is a possible explanation for this significant drop, particularly when pedestrian injuries represent 71% of the total road injuries among children in Saudi Arabia [29]. Therefore, promotion of road safety is recommended around school zones together with traffic law enforcement.
This study has several limitations. First, we compared a period of 12 months before and a period of 12 months after lifting of COVID-19 restrictions; the duration of these two periods were marginally different (by three months) because we compared April 2019–March 2020 (phase 1) to July 2020–June 2021 (phase 2). We were interested in revealing the early impact of lifting policy restrictions. Nevertheless, our study also observes a one-year period of injury data covering all seasons. Second, although most of the restrictions were lifted by the end of June 2020, some protocols were in place for a longer time, such as limits on participants for social and religious gatherings. However, no lockdown policies or restrictions on travelling between regions were in effect beyond July 2020. Third, the population included in this study represents a single-centre experience. Thus, this limits the generalisability of our findings to different cities and regions in Saudi Arabia.
Conclusion
This retrospective study of a major trauma centre demonstrated a significant change in the mechanisms of injury and outcomes of the trauma population. MVC continues to be the leading cause of injury in Saudi Arabia. These findings suggest that the causes of increased violence-related injuries should be investigated. Although the overall injury cases decreased in the first 12 months after easing of COVID-19 restrictions, injury cases rebounded towards pre-lockdown levels with increased in-hospital mortality. Injury prevention needs a robust community programme and legislation with respect to road safety measures together with strict enforcement to decrease the burden of traumatic injuries in Saudi Arabia.
Supplementary Information
Additional file 1: Appendix 1. Univariatepredictors of in-hospital mortality following injury by different variables.
Acknowledgements
The authors extend their appreciation to the King Salman Center for Disability Research for funding this work through Research Group no KSRG-2022-069.
Abbreviations
- COVID-19
Coronavirus Disease 2019
- WHO
World Health Organization
- MVC
Motor Vehicle Crashes
- KSMC
King Saud Medical City
- STAR
Saudi TraumA Registry
- ED
Emergency Department
- ICU
Intensive Care Unit
- SBP
Systolic Blood Pressure
- HR
Heart Rate
- RR
Respiratory Rate
- SD
Standard Deviation
- DV
Dependent Variable
- IV
Independent Variables
- AOR
Adjusted Odds Ratios
- CIs
Confidence Intervals
- ISS
Injury Severity Score
- GCS
Glasgow Coma Scale
- LOHS
Length Of Hospital Stay
Authors’ contributions
This study was developed by all authors. Rayan Jafnan Alharbi, Rami Al-Jafar, Sharfuddin Chowdhury, Ateeq Almuwallad, and Abdullah Alshibani had substantial contribution to the conception or design of the study. Rami Al-Jafar and Rayan Jafnan Alharbi contributed to the data analyses. Rami Al-Jafar cleaned and analysed the data, Rayan Jafnan Alharbi planned and interpreted the data. Rayan Jafnan Alharbiprepared the first draft of this paper and revised critical comments and feedback from Muhammad Aziz Rahman, Ateeq Almuwallad, Abdullah Alshibani, and Virginia Lewis. All authors approved the final version of the manuscript.
Funding
This study was funded by the King Salman Center for Disability Research.
Availability of data and materials
The datasets used during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board Committee at King Saud Medical City, Riyadh, Saudi Arabia (IRB Reference number H1RI-20–June21-01). This study waived the need for obtaining informed consent, according to the regulations approved by the Institutional Review Board Committee at King Saud Medical City, Riyadh, Saudi Arabia because this study used non-identifiable data from an existing data set. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Eng J Med. 2020;382:1199. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Rolling updates on coronavirus disease (COVID-19). 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen. Accessed 6 Oct 2021.
- 3.MOH. Saudi Arabia’s experience in health preparedness and response to COVID-19 pandemic. Saudi Arabia: Ministry of Health Portal; 2020. Available online https://www.moh.gov.sa/en/Ministry/MediaCenter/Publications/Documents/COVID-19-NATIONAL.pdf. Accessed 6 Oct 2021.
- 4.Alharbi R, Mosley I, Miller C, Hillel S, Lewis V. Factors associated with physical, psychological and functional outcomes in adult trauma patients following road traffic crash: a scoping literature review. Transp Res Interdiscip Perspect. 2019;3:100061. [Google Scholar]
- 5.Alharbi RJ, Lewis V, Miller C. A state-of-the-art review of factors that predict mortality among traumatic injury patients following a road traffic crash. Australas Emerg Care. 2021;25:13. doi: 10.1016/j.auec.2021.01.005. [DOI] [PubMed] [Google Scholar]
- 6.Rajput K, Sud A, Rees M, Rutka O. Epidemiology of trauma presentations to a major trauma centre in the North West of England during the COVID-19 level 4 lockdown. Eur J Trauma Emerg Surg. 2021;47(3):631–6. doi: 10.1007/s00068-020-01507-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garude K, Natalwala I, Hughes B, West C, Bhat W. Patterns of adult and paediatric hand trauma during the COVID-19 lockdown. J Plast Reconstr Aesthetic Surg. 2020;73(8):1575. doi: 10.1016/j.bjps.2020.05.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rhodes HX, Petersen K, Biswas S. Trauma trends during the initial peak of the COVID-19 pandemic in the midst of lockdown: experiences from a rural trauma center. Cureus. 2020;12(8):e9811. doi: 10.7759/cureus.9811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alharbi RJ, Lewis V, Mosley I, Miller C. Current trauma care system in Saudi Arabia: a scoping literature review. Accid Anal Prev. 2020;144:105653. doi: 10.1016/j.aap.2020.105653. [DOI] [PubMed] [Google Scholar]
- 10.Alharbi RJ, Lewis V, Othman O, Miller C. Exploring factors that influence injured patients’ outcomes following road traffic crashes: a multi-site feasibility study. Trauma Care. 2022;2(1):35–50. doi: 10.3390/traumacare2010004. [DOI] [Google Scholar]
- 11.Alghnam S, Palta M, Hamedani A, Remington PL, Alkelya M, Albedah K, et al. In-hospital mortality among patients injured in motor vehicle crashes in a saudi arabian hospital relative to large US trauma centers. Injury Epidemiol. 2014;1(1):21. doi: 10.1186/s40621-014-0021-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alghnam S, Alkelya M, Al-Bedah K, Al-Enazi S. Burden of traumatic injuries in Saudi Arabia: lessons from a major trauma registry in Riyadh, Saudi Arabia. Ann Saudi Med. 2014;34(4):291. doi: 10.5144/0256-4947.2014.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hakeem FF, Alshahrani SM, Ghobain MA, Albabtain I, Aldibasi O, Alghnam S. The impact of CoViD-19 lockdown on injuries in Saudi Arabia: results from a level-I trauma center. Front Public Health. 2021;9:704294. doi: 10.3389/fpubh.2021.704294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jacob S, Mwagiru D, Thakur I, Moghadam A, Oh T, Hsu J. Impact of societal restrictions and lockdown on trauma admissions during the COVID-19 pandemic: a single‐centre cross‐sectional observational study. ANZ J Surg. 2020;90(11):2227–31. doi: 10.1111/ans.16307. [DOI] [PubMed] [Google Scholar]
- 15.Fahy S, Moore J, Kelly M, Flannery O, Kenny P. Analysing the variation in volume and nature of trauma presentations during COVID-19 lockdown in Ireland. Bone & Joint Open. 2020;1(6):261–6. doi: 10.1302/2633-1462.16.BJO-2020-0040.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Christey G, Amey J, Campbell A, Smith A. Variation in volumes and characteristics of trauma patients admitted to a level one trauma centre during national level 4 lockdown for COVID-19 in New Zealand. NZ Med J. 2020;133(1513):81–8. [PubMed] [Google Scholar]
- 17.Navsaria P, Nicol A, Parry C, Matzopoulos R, Maqungo S, Gaudin R. The effect of lockdown on intentional and non-intentional injury during the COVID-19 pandemic in Cape Town, South Africa: a preliminary report. South Afr Med J. 2021;111(2):110–3. doi: 10.7196/SAMJ.2021.v111i2.15318. [DOI] [PubMed] [Google Scholar]
- 18.Alqahtani AS, Abuzinada SA, Cameron PA, Fitzgerald MC, Alenizi AS, Farjou D. Experience gained from the implementation of the saudi TraumA Registry (STAR) BMC Health Serv Res. 2020;20(1):1–7. doi: 10.1186/s12913-019-4881-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jeffery MM, D’Onofrio G, Paek H, Platts-Mills TF, Soares WE, Hoppe JA, et al. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID-19 pandemic in the US. JAMA Intern Med. 2020;180(10):1328–33. doi: 10.1001/jamainternmed.2020.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boserup B, McKenney M, Elkbuli A. The impact of the COVID-19 pandemic on emergency department visits and patient safety in the United States. Am J Emerg Med. 2020;38(9):1732–6. doi: 10.1016/j.ajem.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rahman MA, Islam SMS, Tungpunkom P, Sultana F, Alif SM, Banik B, et al. COVID-19: factors associated with psychological distress, fear, and coping strategies among community members across 17 countries. Globalization Health. 2021;17(1):1–19. doi: 10.1186/s12992-021-00768-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Di Blasi M, Gullo S, Mancinelli E, Freda MF, Esposito G, Gelo OCG, et al. Psychological distress associated with the COVID-19 lockdown: a two-wave network analysis. J Affect Disord. 2021;284:18–26. doi: 10.1016/j.jad.2021.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mittal S, Singh T. Gender-based violence during COVID-19 pandemic: a mini-review. Front Global Women’s Health. 2020;1:4. doi: 10.3389/fgwh.2020.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Holland KM, Jones C, Vivolo-Kantor AM, Idaikkadar N, Zwald M, Hoots B, et al. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic. JAMA psychiatry. 2021;78(4):372–9. doi: 10.1001/jamapsychiatry.2020.4402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fegert JM, Vitiello B, Plener PL, Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc Psychiatry Mental Health. 2020;14:1–11. doi: 10.1186/s13034-020-00329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.MOH. Statistics and indicators: road traffic injuries and deaths. Saudi Arabia: Ministry of Health Portal; 2020. Available online: https://www.moh.gov.sa/en/Ministry/Statistics/Pages/Traffic-accidents.aspx. Accessed 12 Oct 2021.
- 27.Alharbi RJ, Shrestha S, Lewis V, Miller C. The effectiveness of trauma care systems at different stages of development in reducing mortality: a systematic review and meta-analysis. World J Emerg Surg. 2021;16(1):1–12. doi: 10.1186/s13017-021-00381-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gabbe BJ, Lyons RA, Fitzgerald MC, Judson R, Richardson J, Cameron PA. Reduced population burden of road transport–related major trauma after introduction of an inclusive trauma system. Ann Surg. 2015;261(3):565. doi: 10.1097/SLA.0000000000000522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Albedewi H, Al-Saud N, Kashkary A, Al-Qunaibet A, AlBalawi SM, Alghnam S. Epidemiology of childhood injuries in Saudi Arabia: a scoping review. BMC Pediatr. 2021;21(1):1–14. doi: 10.1186/s12887-021-02886-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Appendix 1. Univariatepredictors of in-hospital mortality following injury by different variables.
Data Availability Statement
The datasets used during the current study are available from the corresponding author on reasonable request.