Abstract
Background and study aims Endoscopic submucosal dissection (ESD) of pharyngeal cancers with conventional endoscopes often is difficult, not only because of the narrow working space, but also because endoscope maneuverability in the pharynx is poor due to interference from the endotracheal tube and/or hyoid bone. However, we hypothesized that those problems could possibly be resolved by use of an ultrathin endoscope for ESD of superficial pharyngeal cancer. The aim of this prospective interventional study was to investigate the feasibility of ESD for superficial pharyngeal cancer using an ultrathin endoscope.
Patients and methods This feasibility study was conducted at NTT Medical Center Tokyo between June 2020 and September 2021, and data from a total of 20 consecutively superficial pharyngeal cancers were analyzed. The primary outcome measure was the R0 resection rate. The ESD completion rate, en bloc resection rate, procedure time, and frequency of intraoperative and postoperative adverse events (AEs) were also evaluated as secondary outcome measures.
Results Data from 16 patients with 20 lesions were included in the analysis. All of the lesions were successfully resected by ultrathin endoscope ESD, and the en bloc and R0 resection rates were 100 % and 85.0 % (17/20), respectively; the procedure time was 37.8 ± 28.2 minutes. No intraoperative or postoperative AEs were encountered in any cases.
Conclusions ESD using an ultrathin endoscope is feasible for superficial pharyngeal cancers and has potential to be a safe and effective treatment option for these cancers.
Introduction
Pharyngeal cancers are often diagnosed at an advanced stage and, therefore, are considered to carry a poor prognosis 1 2 . Patients with advanced pharyngeal cancers require surgical resection or chemoradiation therapy, which often reduces their quality of life, in terms of both cosmetic problems and functional decline of the organ. However, with advances in endoscopic technologies in recent years such as magnifying endoscopy with narrow-band imaging (ME-NBI), the rate of detection of superficial pharyngeal cancers during routine upper gastrointestinal endoscopic examinations has increased 3 4 5 6 . Currently, there is no established treatment for superficial pharyngeal cancer, but in recent years, the trend has shifted from invasive surgical resection to minimally invasive local treatment, aimed at preserving organ function and maintaining patient quality of life. Muto et al. 7 and Satake et al. 8 reported that 5-year overall and disease-specific survival after transoral endoscopic treatment ranged from 71 % to 85 % and 97 % to 100 %, respectively. Among endoscopic treatments, endoscopic submucosal dissection (ESD) was developed as a novel technique for early-stage gastric cancer, with the technique potentially allowing even large lesions to be resected en bloc 9 . Although ESD requires a high level of skill, it has been widely performed for early-stage cancers of the gastrointestinal tract, and its usefulness for superficial pharyngeal cancers also has been reported by several researchers 10 11 12 13 14 . However, in the case of pharyngeal cancer, ESD using a conventional endoscope is often difficult, not only because of of the narrow working space in this region, but also because of poor maneuverability of the endoscope in the pharyngolarynx as a result of interference by the endotracheal tube and/or hyoid bone. Therefore, the procedure is challenging and an even higher level of skill is required for dissection.
In recent years, ultrathin endoscopes, with clearly improved brightness and resolution, have been widely used for screening endoscopic examinations 15 16 . We consider that the aforementioned problems with use of ESD for pharyngeal cancer using conventional scopes could possibly be overcome with an ultrathin endoscope. In fact, we have previously reported a case of successful ESD of superficial pharyngeal cancer using an ultrathin endoscope 17 . However, accumulation of more cases was needed to establish the efficacy and safety of ESD for superficial pharyngeal cancer using an ultrathin endoscope.
The aim of this prospective interventional study was to investigate the efficacy and safety of ESD for superficial pharyngeal cancers using an ultrathin endoscope to determine its feasibility.
Patients and methods
Study design and patients
This was a single-center, prospective feasibility study to investigate the efficacy and safety of ESD for superficial pharyngeal cancer using an ultrathin endoscope, which was conducted at NTT Medical Center Tokyo between June 2020 and September 2021. Data from a total of 20 consecutively diagnosed superficial pharyngeal cancers in Japanese patients were included in the analysis. Inclusion criteria were as follows: (1) histologically confirmed diagnosis of pharyngeal squamous cell carcinoma or high-grade intraepithelial neoplasia by preoperative endoscopic biopsy; (2) estimated depth of invasion by endoscopic examination limited to the epithelial or subepithelial layer; and (3) no lymph node metastasis or distant metastasis detected by whole-body CT. Patients with any of the following were excluded from the study: (1) estimated depth of invasion by endoscopic examination extending to the muscle layer; and (2) computed tomography evidence of lymph node metastasis or distant metastasis. Written informed consent was obtained from each patient. This study was conducted with the approval of the Ethics Committee of NTT Medical Center Tokyo (ID 20–72), and was registered in advance in the University Hospital Medical Information Network Clinical Trials Registry (UMIN000040961). All preoperative endoscopic workups, endoscopic treatments, and histopathological evaluations were performed at NTT Medical Center Tokyo.
Preoperative endoscopic examination
Preoperative endoscopic examination was performed using a magnifying endoscope (GIF-H290Z; Olympus, Tokyo, Japan) in all cases, and tumor size, location, and macroscopic type were assessed. Endoscopic diagnosis, including estimation of the depth of invasion of the tumor, was made by white-light imaging endoscopy and ME-NBI; however, only lesions with a biopsy-confirmed diagnosis of squamous cell carcinoma or high-grade intraepithelial neoplasia were considered as being eligible for this study. Clinical superficial pharyngeal cancer was defined as pharyngeal cancer with an estimated depth of invasion by endoscopic examination confined to the epithelial or subepithelial layer, with no suspected invasion of the muscular layer.
Settings for ultrathin endoscope ESD
We used EG-L580NW7 (FUJIFILM Medical Co., Ltd., Tokyo, Japan) as an ultrathin endoscope, which has a relatively smaller scope diameter of 5.8 mm, and working channel diameter of 2.4 mm. Even so, the multifunctional snare SOUTEN ( Fig. 1 ), and RAICHO (sheath diameter: 2.35 mm and 2.3 mm respectively, Kaneka Medics, Tokyo, Japan) were still usable as the cutting and hemostatic devices 18 19 20 . Distal attachments placed on the ultrathin endoscope tip were handmade using a transparent tape, as there were no special attachments available that fit the scope 21 . A 25G 3-mm local injection needle with a 1.9-mm sheath diameter was used (TOP, Tokyo, Japan), and a local injection was administrated using half Glyceol. The settings of the VIO300 D electrical unit (Erbe Elektromedizin, Tübingen, Germany) were “EndoCut mode I” (effect 2, duration 2, interval 2) for mucosal incision and “forced coagulation mode” (effect 2, 45 W) for dissection and vessel coagulation, just as in pharyngeal ESD using a conventional endoscope.
Fig. 1 .
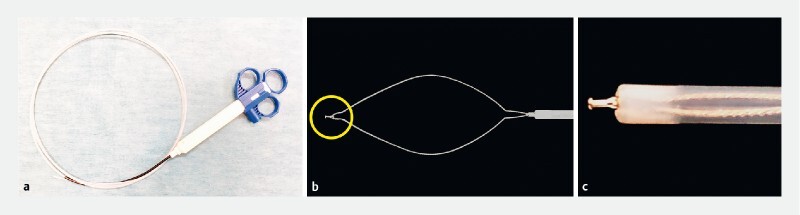
Details of the SOUTEN snare (Kaneka Medics, Tokyo, Japan). a A multifunctional snare, designed to achieve hybrid ESD. b, c A 1.5-mm needle-knife with a knob-shaped tip is attached to the top of the snare.
ESD procedure
Video 1 Pharyngeal endoscopic submucosal dissection using an ultrathin endoscope. Pharyngeal ESD using an ultrathin endoscope was performed to resect a superficial hypopharyngeal cancer measuring 30 mm in diameter located in the left pyriform sinus. Complete resection was achieved using the “SOUTEN” multifunctional snare, without any adverse events. English subtitles for video: A tumor was located in the left pyriform sinus adjacent to the hyoid bone. Marking was performed with the tip of SOUTEN. Local injection was administrated using half Glyceol. Mucosal flap was created with the tip of SOUTEN Dissection became difficult due to vertical approach. We switched to the transnasal approach. It became easy to dissect with a parallel approach to the lesion. Then, additional local injection was made. Mucosal incision and dissection on the posterior wall were performed. The manipulation of the endoscope became unstable due to interference by the hyoid bone. With the switch to the oral approach, dissection became possible. After additional injection, a circumferential incision and trimming were made. Switching to the transnasal approach again, the remaining subepithelial layer was dissected. The lesion was completely removed. Finally, the lesion was collected with SOUTEN.
All of the procedures were performed in an operating theater with the patient lying supine under general anesthesia with oral endotracheal intubation. To ensure sufficient working space, the anesthesiologist fixed the laryngoscope to the ventral side of the endotracheal tube while viewing the endoscopic image and lifted the larynx directly. The entire ESD procedure is shown in Fig. 2 and Video 1 . Marking around the lesion was performed using the tip of SOUTEN after clarifying the extent of the lesion with iodine dye. Next, after local injection, a mucosal incision was made and dissection was performed to create a mucosal flap. Finally, after confirming that the endoscope was stably positioned and capable of dissection of the subepithelial layer, local injection was added as appropriate, and the lesion was resected through a circumferential mucosal incision and dissection of the remaining subepithelial layer. Mucosal incision and subepithelial dissection were also all performed with the tip of SOUTEN. We tried to improve the field of view and stability of the endoscope by switching to the transnasal approach when it became difficult to dissect for the lesion via the oral approach due to poor maneuverability of the endoscope or when there was need for a vertical approach to the lesion. The resected lesion was retrieved using the snare part of the SOUTEN. All the procedures were performed by four skilled operators, each of whom had performed more than 100 ESDs in the upper gastrointestinal and/or lower gastrointestinal tract; only one of the four operators was experienced in ESD using an ultrathin endoscope.
Fig. 2 a.
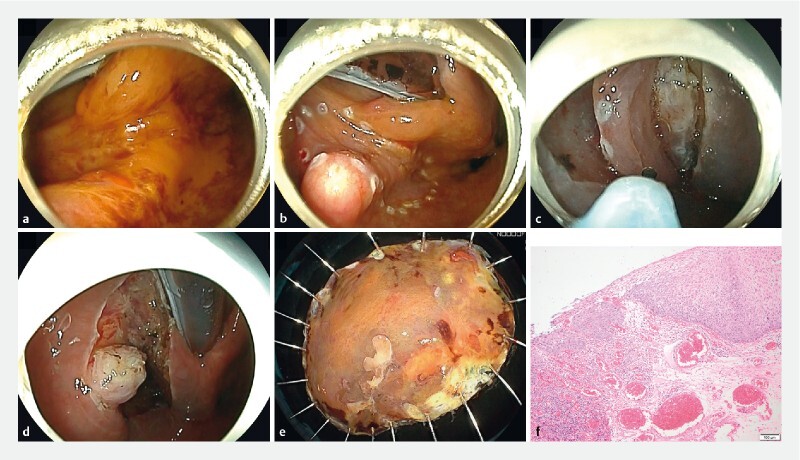
A superficial hypopharyngeal cancer measuring 30 mm in diameter was located in the left pyriform sinus adjacent to the hyoid bone. b Marking was performed with the tip of SOUTEN. c The subepithelial layer was dissected with the tip of SOUTEN. d The ulcer floor after endoscopic submucosal dissection. e The specimen resected en bloc. f Histological examination confirmed the diagnosis of squamous cell carcinoma with subepithelial invasion (tumor thickness 560 μm).
Histopathological examination
All the resected specimens were fixed in formalin for 24 hours, sectioned into 2-mm-thick slices, and stained with hematoxylin and eosin for detailed histopathological examination. Lesions with an intact basal layer and tumor cells confined to the epithelial layer were diagnosed as carcinoma in situ (CIS), whereas those in which the tumor cells showed subepithelial invasion were diagnosed as subepithelial cancer. In the case of subepithelial invasion, tumor thickness measurements were made (distance between the surface layer and deepest point), and immunostaining (D2–40, EVG) was performed to confirm or exclude lymphovascular invasion. R0 resection was defined as en bloc resection of a tumor with absence of tumor cells at the horizontal and vertical margins of the specimen on histopathological examination.
Outcome measurements
The primary outcome measure was assessment of R0 resection rates of pharyngeal ESD using an ultrathin endoscope. The completion rate, en bloc resection rate, procedure time, and frequency of intraoperative adverse events (AEs), such as perforation, and postoperative AEs within 14 days of the ESD, such as laryngeal edema and delayed bleeding, were evaluated as the secondary outcome measures.
Results
Characteristics of patients and lesions
Overall, 16 consecutive patients with 20 superficial pharyngeal cancers were enrolled in our study. The clinicopathological characteristics of the patients and lesions are summarized in Table 1 . The subject population consisted of 12 male and four female patients, and the age of the patients at the time of treatment was 69.2 ± 5.6 years. The mean tumor diameter of the 20 lesions was 19.3 ± 11.2 mm and the tumor was located in the pyriform sinus in 15 cases, posterior wall of the hypopharynx in two cases, posterior cricoid area in one case, posterior wall of the oropharynx in one case, and epiglottic vallecula in one case. In terms of the macroscopic type according to the Paris classification, 14 of 20 lesions were classified as flat type (IIb), 4 were classified as flat depressed type (IIc), and two were classified as flat elevated (IIa) type. As for the depth of tumor invasion on histopathology, 10 of 20 lesions were classified as CIS , and in 10, the tumor invaded the subepithelial layer.
Table 1. Clinicopathological characteristics of patients and lesions.
| Patients, n (lesion, n) | 16 (20) |
| Sex, n (male/female) | 12/ 4 |
| Age, years, mean ± SD | 69.2 ± 5.6 |
| History of esophageal cancer, n | 12 |
|
10 |
|
2 |
| History of pharyngeal cancer, n | 3 |
|
2 |
|
1 |
| Location, n (%) | |
|
18 (90) |
|
15 (75) |
|
2 (10) |
|
1 (5) |
|
2 (10) |
|
1 (5) |
|
0 (0) |
|
1 (5) |
| Tumor diameter, mm, mean ± SD | 19.3 ± 11.2 |
| Macroscopic type, n (%) | |
|
2 (10) |
|
14 (70) |
|
4 (20) |
| Depth of invasion, n (%) | |
|
10 (50) |
|
10 (50) |
| Tumor thickness, n (%) | |
|
16 (80) |
|
4 (20) |
| Positive lymphovascular involvement, n (%) | 0 (0) |
CRT, chemoradiotherapy; CIS, carcinoma in situ; SEP, subepithelial invasion.
Therapeutic outcomes
All of the lesions were successfully resected by ultrathin endoscope ESD. The therapeutic outcomes of pharyngeal ESD are summarized in Table 2 . The en bloc and R0 resection rates were 100 % (20/20) and 85.0 % (17/20), respectively, and the procedure time was 37.8 ± 28.2 minutes. The duration of postoperative fasting and postoperative hospitalization were 1.7 ± 0.9 days and 5.8 ± 1.1 days, respectively. The endoscopic approach to the lesion was oral alone in 13 cases (65.0 %), and both oral and transnasal in seven cases (35.0 %). There were no intraoperative AEs such as perforation or bleeding that necessitated the use of hemostatic forceps. In addition, there were no postoperative AEs within 14 days of the ESD such as laryngeal edema or delayed bleeding. As an addendum, the characteristics and therapeutic outcomes of all the enrolled patients are presented in detail in Table 3 .
Table 2. Therapeutic outcomes and adverse events.
| Ultrathin endoscope ESD (20 lesions) | |
| En bloc resection, n (%) | 20 (100) |
| R0 resection, n (%) | 17 (85.0) |
| Procedure time, min, mean ± SD | 37.8 ± 28.2 |
| Endoscopic approach, n (%) | |
|
13 (65) |
|
7 (35) |
| Adverse event, n (%) | |
|
0 (0) |
|
0 (0) |
|
0 (0) |
|
0 (0) |
|
0 (0) |
| Duration of postoperative fasting, day, mean ± SD | 1.7 ± 0.9 |
| Duration of postoperative hospitalization, day, mean ± SD | 5.8 ± 1.1 |
En bloc resection was defined as resection of the entire tumor in a single piece. R0 resection was defined as a complete resection with histologically negative lateral and vertical margins. Delayed bleeding was defined as overt bleeding occurring within 14 days of the ESD that necessitated an endoscopic hemostatic procedure using hemostatic forceps.
ESD, endoscopic submucosal dissection.
Table 3. Details of characteristics and therapeutic outcomes of enrolled patients.
| Patient | Age | Sex | Tumor location | Tumor diameter, mm | Macroscopic type | Procedure time, min | En bloc/R0 resection | Approach | Adverse events |
| 1 | 78 | M | Pyriform sinus (Lt) | 20 | IIb | 63 | Yes/Yes | Both | None |
| 2 | 62 | F | Pyriform sinus (Rt) | 17 | IIb | 27 | Yes/Yes | Both | None |
| 3 | 62 | F | Pyriform sinus (Rt) | 9 | IIb | 15 | Yes/Yes | Oral | None |
| 4 | 63 | M | Epiglottic vallecula | 7 | IIb | 50 | Yes/Yes | Both | None |
| 5 | 68 | M | Posterior hypopharyngeal wall | 7 | IIc | 12 | Yes/Yes | Both | None |
| 6 | 71 | M | Pyriform sinus (Lt) | 10 | IIa | 13 | Yes/Yes | Oral | None |
| 7 | 83 | M | Pyriform sinus (Rt) | 50 | IIb | 112 | Yes/No | Oral | None |
| 8 | 69 | F | Posterior oropharyngeal wall | 30 | IIb | 45 | Yes/Yes | Oral | None |
| 9 | 70 | M | Pyriform sinus (Rt) | 32 | IIc | 32 | Yes/No | Oral | None |
| 10 | 67 | M | Posterior hypopharyngeal wall | 10 | IIb | 23 | Yes/Yes | Oral | None |
| 11 | 70 | M | Pyriform sinus (Lt) | 25 | IIb | 73 | Yes/Yes | Oral | None |
| 12 | 73 | M | Pyriform sinus (Lt) | 17 | IIc | 18 | Yes/Yes | Oral | None |
| 13 | 73 | M | Pyriform sinus (Rt) | 8 | IIb | 11 | Yes/Yes | Oral | None |
| 14 | 73 | M | Pyriform sinus (Rt) | 15 | IIb | 15 | Yes/Yes | Oral | None |
| 15 | 73 | M | Pyriform sinus (Lt) | 15 | IIc | 43 | Yes/Yes | Both | None |
| 16 | 66 | M | Pyriform sinus (Rt) | 18 | IIb | 30 | Yes/Yes | Oral | None |
| 17 | 68 | M | Pyriform sinus (Rt) | 33 | IIb | 93 | Yes/No | Both | None |
| 18 | 76 | F | Pyriform sinus (Lt) | 10 | IIb | 21 | Yes/Yes | Oral | None |
| 19 | 64 | M | Pyriform sinus (Lt) | 28 | IIb | 40 | Yes/Yes | Both | None |
| 20 | 63 | F | Posterior cricoid area | 25 | IIa | 20 | Yes/Yes | Oral | None |
En bloc resection was defined as resection of the entire tumor in a single piece. R0 resection was defined as complete resection with histologically negative lateral and vertical margins.
Discussion
In this prospective feasibility study, we investigated the efficacy and safety of ESD for superficial pharyngeal cancer using an ultrathin endoscope. The primary endpoint was successfully achieved, with an R0 resection rate of 85.0 %. ESD using an ultrathin endoscope could be completed in all cases without interruption, and en bloc resection was obtained in all the cases. Furthermore, there were no cases of intraoperative AEs such as perforation, or postoperative AEs such as and laryngeal edema and delayed bleeding.
Pharyngeal cancer has been considered to carry a poor prognosis as it is often diagnosed at the advanced stage, but with the advent and widespread use of ME-NBI, early detection of pharyngeal cancer has become possible 1 2 3 4 5 6 . In addition, the detection rate of superficial pharyngeal cancer with upper gastrointestinal endoscopy is expected to increase further in the future because advances in endoscopic technologies in recent years have allowed brighter and clearer endoscopic images to be obtained. Although there is no established treatment for superficial pharyngeal cancer, the trend in recent years has shifted from invasive surgical resection to minimally invasive local treatment, aimed at preserving organ function and maintaining patient quality of life. Endoscopic laryngopharyngeal surgery (ELPS) is a minimally invasive procedure that is performed jointly by the otolaryngologist and endoscopist, the former using both hands to remove the lesion while viewing the monitor provided by the endoscopist; however, it has the disadvantage that it always requires two operators 22 23 . Similar to the case of early-stage cancers of the gastrointestinal tract, we believe that endoscopic resection is the optimal treatment for superficial pharyngeal cancer because it can be performed by a single operator and is minimally invasive and highly curative.
Endoscopic treatment can be broadly divided into endoscopic mucosal resection (EMR) and ESD; the latter, ESD, is more desirable in terms of the en bloc resection rate and control of local recurrence. Kinjo et al. and Okada et al. reported en bloc resection rates of ESD for superficial pharyngeal cancer of 100 % and 77.4 %, respectively. Meanwhile, Kinjo et al. and Okada et al. reported en bloc resection rates of EMR for superficial pharyngeal cancer of 60.2 % and 37.8 %, respectively 24 25 . In addition, Kinjo et al. reported local recurrence rates after ESD and EMR for superficial pharyngeal cancer of 0 % and 8.6 %, respectively 24 . The possibility of applying ESD to treatment of superficial pharyngeal cancer has been reported before, but unlike the case for ESD performed for other tumors of the gastrointestinal tract, the reports were mainly based on small studies conducted in a limited number of facilities 10 11 12 13 14 . This may be related to the fact that ESD for superficial pharyngeal cancer not only requires special arrangements for general anesthesia and laryngeal deployment using the laryngoscope absolutely, but also cooperation with the otorhinolaryngologist in the event that laryngeal edema occurs during treatment. Furthermore, pharyngeal ESD requires a higher level of skill for dissection, not only because of the small working space available for the endoscope, but also because of poor maneuverability of conventional endoscopes because of interference by the endotracheal tube and/or hyoid bone.
Endoscopy using ultrathin endoscopes, mainly screening endoscopy, has come to be widely used as a well-tolerated examination method, because the gag reflex can be suppressed by transnasal insertion, and the procedure is less invasive to patients in terms of changes in the respiratory and circulatory dynamics during the procedure 26 27 . Recently, brighter and clearer endoscopic imaging has become possible, making it very useful for detecting and diagnosing early-stage gastrointestinal cancers 15 28 . These ultrathin endoscopes have also been applied to endoscopic treatments. They are actively used in clinical practice, especially for inserting ileus tubes 29 . They have also reportedly been used as double endoscopes for ESD in cases of early gastric cancer 30 and for peroral endoscopic myotomy (POEM) in cases of achalasia 31 . Besides those indications, there are several reports suggesting that ESD using an ultrathin endoscope is very useful. The characteristics of an ultrathin endoscope make it effective for use in a transnasal approach to reduce the amount of sedation needed during the endoscopic treatment and to negotiate stricture that cannot be negotiated with a conventional endoscope. We have also previously experienced and reported cases of conscious transnasal hybrid ESD using an ultrathin endoscope for early gastric cancer in elderly patients 32 and cases of ESD using an ultrathin endoscope for early esophageal cancer with postoperative stricture 33 .
We conducted the present feasibility study based on the assumption that an ultrathin endoscope would be effective for pharyngeal ESD as well, which requires endoscope manipulation in an anatomically confined space. Even with use of an ultrathin endoscope for pharyngeal ESD, it is still possible to prepare all the necessary devices such as cutting device, hemostatic device, local injection needle, and distal attachments, as for pharyngeal ESD using a conventional endoscope. The primary endpoint, R0 resection rate, was 85 %, which is comparable or better than the previously reported rates of 54.8 % to 83.5 % 12 13 14 24 25 . Pharyngeal ESD using an ultrathin endoscope could be completed in all cases without interruption, and en bloc resection could be obtained. Furthermore, not only were there no AEs such as intraoperative perforation or delayed bleeding, but there was also no postoperative laryngeal edema or aspiration pneumonia, because the treatment could be completed within a relatively short time. On the other hand, there were four cases in the present study that required more than 60 minutes for treatment. Of these cases, two were cases in which the operator performed ESD using an ultrathin endoscope for the first time, and the other two were anatomic features such as a lesion located deep part of the pyriform sinus or a large lesion extending from pyriform sinus to the posterior wall with a narrow subepithelial layer, which may have contributed to the time consuming of treatment. Although there have been several reports on the usefulness of pharyngeal ESD with traction devices 13 34 35 , in the present study, ESD using an ultrathin endoscope was performed with the conventional method without using a traction device in any case. In these cases, it is highly likely that use of a traction device during dissection would have resulted in more efficient dissection, but the compatibility of traction devices with pharyngeal ESD using an ultrathin endoscope should also be evaluated in the future.
Based on the results of this study, pharyngeal ESD using an ultrathin endoscope is considered feasible in terms of the efficacy and safety. However, there are advantages and disadvantages of pharyngeal ESD using ultrathin endoscopes. The advantage using ultrathin endoscopes is good endoscope maneuverability within the narrow available space. In the case of pharyngeal ESD, no matter how much the laryngoscope is used to lift the larynx and secure a good field of view, the available space to manipulate the endoscope in the pyriform sinus and epiglottis is narrow, making it difficult to approach with a conventional endoscope and leaving the possibility that complete resection cannot be obtained. We believe that not only the endoscope's characteristic of being thin, but also its good maneuverability within the narrow available space synergizes to enable a rapid approach to the subepithelial layer. The other advantage is that the lesion can be approached by two routes: orally and transnasally. In the majority of cases, treatment is first initiated using an oral approach, but the stability of the endoscope and the manipulation of the endoscope due to interference by the hyoid bone occasionally may be compromised when dissecting the lesion in the pyriform sinus, although much less frequently than with a conventional endoscope. In addition, lesions located deep in the pyriform sinus can be difficult to dissect because it sometimes becomes necessary during the procedure to adopt a vertical approach. In such cases, switching to a transnasal approach can improve not only the endoscopic view by changing the endoscope's approach to the lesion, but also the stability due to the endoscope being fixed, which makes subepithelial dissection easy and safe. Another advantage of a transnasal approach is that lesions in the posterior oropharyngeal wall or epiglottis, which anatomically are often approached limited vertically with an oral approach, can be easily dissected by switching to a transnasal approach because the lesion can be approached horizontally. We believe that lesions located in such sites may offer a site-specific advantage when performing pharyngeal ESD using an ultrathin endoscope. However, there are also some disadvantages of ESD using thin endoscopes. A water jet cannot be used in case of bleeding and the sucking function is weak, which are disadvantages, although major bleeding is rarer in the pharynx as compared to the stomach. In fact, in this feasibility study, no case of major bleeding necessitating the use of hemostatic forceps was encountered. There are also few disadvantages to a transnasal approach, but if any, they include the possibility of epistaxis and the inability to insert an endoscope due to the narrowness of the nasal cavity caused by the skeletal structure, although these were not observed in this feasibility study.
The present study had several limitations. First, our results were based on the outcomes in a series of patients treated by skilled endoscopists. Therefore, any future studies should also include validation of the treatment by relatively inexperienced endoscopists. Second, most of the lesions were located in the hypopharynx, especially in the pyriform sinus, with only a few in the oropharynx. The locations of the lesions in the patients enrolled in the present study were not significantly different from those reported in previous studies of endoscopic treatment, in which about 75 % to 90 % of lesions were located in the hypopharynx 7 12 14 . In the present study, there were no cases of difficult approach in pharyngeal ESD using an ultrathin endoscope, and there seemed to be no disadvantage as a location for lesion. However, any future studies should also examine whether ESD using an ultrathin endoscope is possible for lesions located in various parts of the hypopharynx and oropharynx. Finally, this study was conducted at a single center that specializes in endoscopic treatment, in a relatively small sample. In order to standardize endoscopic ESD using an ultrathin endoscope for superficial pharyngeal cancer in the future, it is necessary to conduct large-scale prospective interventional multicenter studies.
Conclusions
In conclusion, ESD using an ultrathin endoscope for superficial pharyngeal cancer is feasible and has potential to be a safe and effective treatment option for superficial pharyngeal cancer in the future.
Acknowledgments
The authors thank all colleagues at NTT Medical Center Tokyo who supported the study. They also thank IMIC (https://www.imic.or.jp/) for editing a draft of this manuscript.
Footnotes
Competing interests The authors declare that they have no conflict of interest.
References
- 1.Eckel H E, Staar S, Volling P et al. Surgical treatment for hypopharynx carcinoma: feasibility, mortality, and results. Otolaryngol. Head Neck Surg. 2001;124:561–569. doi: 10.1067/mhn.2001.115060. [DOI] [PubMed] [Google Scholar]
- 2.Johansen L V, Grau C, Overgaard J. Hypopharyngeal squamous cell carcinoma–treatment results in 138 consecutively admitted patients. Acta Oncol. 2000;39:529–536. doi: 10.1080/028418600750013465. [DOI] [PubMed] [Google Scholar]
- 3.Muto M, Minashi K, Yano T et al. Early detection of superficial squamous cell carcinoma in the head and neck region and esophagus by narrow band imaging: a multicenter randomized controlled trial. J Clin Oncol. 2010;28:1566–1572. doi: 10.1200/JCO.2009.25.4680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Katada C, Tanabe S, Koizumi W et al. Narrow band imaging for detecting superficial squamous cell carcinoma of the head and neck in patients with esophageal squamous cell carcinoma. Endoscopy. 2010;42:185–190. doi: 10.1055/s-0029-1243963. [DOI] [PubMed] [Google Scholar]
- 5.Kikuchi D, Iizuka T, Yamada A et al. Utility of magnifying endoscopy with narrow band imaging in determining the invasion depth of superficial pharyngeal cancer. Head Neck. 2015;37:846–850. doi: 10.1002/hed.23683. [DOI] [PubMed] [Google Scholar]
- 6.Goda K, Dobashi A, Yoshimura N et al. Dual-focus versus conventional magnification endoscopy for the diagnosis of superficial squamous neoplasms in the pharynx and esophagus: a randomized trial. Endoscopy. 2016;48:321–329. doi: 10.1055/s-0035-1569644. [DOI] [PubMed] [Google Scholar]
- 7.Muto M, Satake H, Yano T et al. Long-term outcome of transoral organ-preserving pharyngeal endoscopic resection for superficial pharyngeal cancer. Gastrointest Endosc. 2011;74:477–484. doi: 10.1016/j.gie.2011.04.027. [DOI] [PubMed] [Google Scholar]
- 8.Satake H, Yano T, Muto M et al. Clinical outcome after endoscopic resection for superficial pharyngeal squamous cell carcinoma invading the subepithelial layer. Endoscopy. 2015;47:11–18. doi: 10.1055/s-0034-1378107. [DOI] [PubMed] [Google Scholar]
- 9.Gotoda T, Yamamoto H, Soetikno R M. Endoscopic submucosal dissection of early gastric cancer. J Gastroenterol. 2006;41:929–942. doi: 10.1007/s00535-006-1954-3. [DOI] [PubMed] [Google Scholar]
- 10.Iizuka T, Kikuchi D, Hoteya S et al. Endoscopic submucosal dissection for treatment of mesopharyngeal and hypopharyngeal carcinomas. Endoscopy. 2009;41:113–117. doi: 10.1055/s-0028-1119453. [DOI] [PubMed] [Google Scholar]
- 11.Kuwabara T, Hiyama T, Oka S et al. Clinical features of pharyngeal intraepithelial neoplasias and outcomes of treatment by endoscopic submucosal dissection. Gastrointest Endosc. 2012;76:1095–1103. doi: 10.1016/j.gie.2012.07.032. [DOI] [PubMed] [Google Scholar]
- 12.Hanaoka N, Ishihara R, Takeuchi Y et al. Clinical outcomes of endoscopic mucosal resection and endoscopic submucosal dissection as a transoral treatment for superficial pharyngeal cancer. Head Neck. 2013;35:1248–1254. doi: 10.1002/hed.23106. [DOI] [PubMed] [Google Scholar]
- 13.Yoshio T, Tsuchida T, Ishiyama A et al. Efficacy of double-scope endoscopic submucosal dissection and long-term outcomes of endoscopic resection for superficial pharyngeal cancer. Dig Endosc. 2017;29:152–159. doi: 10.1111/den.12712. [DOI] [PubMed] [Google Scholar]
- 14.Iizuka T, Kikuchi D, Suzuki Y et al. Clinical relevance of endoscopic treatment for superficial pharyngeal cancer: feasibility of techniques corresponding to each location and long-term outcomes. Gastrointest Endosc. 2021;93:818–827. doi: 10.1016/j.gie.2020.07.039. [DOI] [PubMed] [Google Scholar]
- 15.Kawai T, Yanagizawa K, Naito S et al. Evaluation of gastric cancer diagnosis using new ultrathin transnasal endoscopy with narrow-band imaging: preliminary study. J Gastroenterol Hepatol. 2014;29:33–36. doi: 10.1111/jgh.12797. [DOI] [PubMed] [Google Scholar]
- 16.Suzuki T, Kitagawa Y, Nankinzan R et al. Early gastric cancer diagnostic ability of ultrathin endoscope loaded with laser light source. World J Gastroenterol. 2019;25:1378–1386. doi: 10.3748/wjg.v25.i11.1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Muramoto T, Sakai E, Ohata K. Endoscopic submucosal dissection for superficial hypopharyngeal cancer with thin endoscope. Dig Endosc. 2020;32:e13–14. doi: 10.1111/den.13544. [DOI] [PubMed] [Google Scholar]
- 18.Ohata K, Muramoto T, Minato Y et al. Usefulness of a multifunctional snare designed for colorectal hybrid endoscopic submucosal dissection (with video) Endosc Int Open. 2018;6:E249–E253. doi: 10.1055/s-0043-124364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kobara H, Mori H, Masaki T. Effective and economical endoscopic resection using a novel multifunctional snare for small-sized gastric neoplasms. Dig Endosc. 2018;30:800–801. doi: 10.1111/den.13232. [DOI] [PubMed] [Google Scholar]
- 20.Arimoto J, Ohata K, Chiba H et al. Evaluation of colorectal endoscopic submucosal dissection using a multifunctional snare: a prospective clinical feasibility study (with videos) Gastrointest Endosc. 2021;93:671–678. doi: 10.1016/j.gie.2020.09.019. [DOI] [PubMed] [Google Scholar]
- 21.Kurebayashi M, Sakai E, Suzuki Y et al. Usefulness of a handmade distal endoscope attachment with a transparent tape. VideoGIE. 2020;5:226–228. doi: 10.1016/j.vgie.2020.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tateya I, Muto M, Morita S et al. Endoscopic laryngo-pharyngeal surgery for superficial laryngo-pharyngeal cancer. Surg Endosc. 2016;30:323–329. doi: 10.1007/s00464-015-4213-y. [DOI] [PubMed] [Google Scholar]
- 23.Watanabe A, Taniguchi M, Kimura Y et al. Synopsis of transoral endoscopic laryngopharyngeal surgery for superficial pharyngeal cancers. Head Neck. 2017;39:1779–1787. doi: 10.1002/hed.24839. [DOI] [PubMed] [Google Scholar]
- 24.Kinjo Y, Nonaka S, Oda I et al. The short-term and long-term outcomes of the endoscopic resection for the superficial pharyngeal squamous cell carcinoma. Endosc Int Open. 2015;3:E266–E273. doi: 10.1055/s-0034-1392094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Okada K, Tsuchida T, Ishiyama A et al. Endoscopic mucosal resection and endoscopic submucosal dissection for en bloc resection of superficial pharyngeal carcinomas. Endoscopy. 2012;44:556–564. doi: 10.1055/s-0032-1309720. [DOI] [PubMed] [Google Scholar]
- 26.Yagi J, Adachi K, Arima N et al. A prospective randomized comparative study on the safety and tolerability of transnasal esophagogastroduodenoscopy. Endoscopy. 2005;37:1226–1231. doi: 10.1055/s-2005-921037. [DOI] [PubMed] [Google Scholar]
- 27.Kawai T, Miyazaki I, Yagi K et al. Comparison of the effects on cardiopulmonary function of ultrathin transnasal versus normal diameter transoral esophagogastroduodenoscopy in Japan. Hepatogastroenterology. 2007;54:770–774. [PubMed] [Google Scholar]
- 28.Suzuki T, Kitagawa Y, Nankinzan R et al. Early gastric cancer diagnostic ability of ultrathin endoscope loaded with laser light source. World J Gastroenterol. 2019;25:1378–1386. doi: 10.3748/wjg.v25.i11.1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sato R, Watari J, Tanabe H et al. Transnasal ultrathin endoscopy for placement of a long intestinal tube in patients with intestinal obstruction. Gastrointest Endosc. 2008;67:953–957. doi: 10.1016/j.gie.2008.01.043. [DOI] [PubMed] [Google Scholar]
- 30.Ogata K, Yanai M, Kuriyama K et al. Double endoscopic intraluminal operation (DEILO) for early gastric cancer: outcome of novel procedure for endoscopic submucosal dissection. Anticancer Res. 2017;37:343–347. doi: 10.21873/anticanres.11327. [DOI] [PubMed] [Google Scholar]
- 31.Grimes K L, Inoue H, Onimaru M et al. Double-scope per oral endoscopic myotomy (POEM): a prospective randomized controlled trial. Surg Endosc. 2016;30:1344–1351. doi: 10.1007/s00464-015-4396-2. [DOI] [PubMed] [Google Scholar]
- 32.Minato Y, Sakai E, Ohata K. Conscious transnasal hybrid endoscopic submucosal dissection enables safe and painless en bloc resection in elderly patients with early gastric cancer. VideoGIE. 2019;4:157–158. doi: 10.1016/j.vgie.2018.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Muramoto T, Sakai E, Ohata K. Thin-endoscope endoscopic submucosal dissection for early esophageal cancer with postoperative stricture. Dig Endosc. 2020;32:e11–e12. doi: 10.1111/den.13537. [DOI] [PubMed] [Google Scholar]
- 34.Iizuka T, Kikuchi D, Hoteya S et al. A new technique for pharyngeal endoscopic submucosal dissection: Peroral countertraction (with video) Gastrointest Endosc. 2012;76:1034–1038. doi: 10.1016/j.gie.2012.07.013. [DOI] [PubMed] [Google Scholar]
- 35.Matsuno K, Miyamoto H, Tanaka M. Novel traction method for pharyngeal endoscopic submucosal dissection using ring-shaped thread and grasping forceps. Dig Endosc. 2020;32:e120–e121. doi: 10.1111/den.13718. [DOI] [PubMed] [Google Scholar]


