A 70-year-old woman with acute cholangitis was referred to our unit for treatment. Complex choledocholithiasis with impacted stones prevented endoscopic retrograde cholangiopancreatography (ERCP) and the patient underwent biliary drainage by endoscopic ultrasound (EUS)-guided choledochoduodenostomy (CDS) using a cautery-enhanced 8 × 8-mm lumen-apposing metal stent (LAMS) over a guidewire.
After LAMS release, EUS imaging revealed maldeployment of the distal flange of the LAMS between the common bile duct (CBD) and duodenal wall. This was probably due to an angled scope tip and difficulty in manipulating the guidewire (stripping of the guidewire occurred) ( Video 1 ).
Video 1 Maldeployment of lumen-apposing metal stent during endoscopic ultrasound choledochoduodenostomy managed by advancing a guidewire directly through the choledochal breach followed by endoscopic retrograde cholangiopancreatography rendezvous with transpapillary biliary stent placement and clips to seal the perforation.
Passage of purulent fluid was visible through the LAMS endoscopically. The EUS scope was replaced with a gastroscope to easily inject contrast through the LAMS. The fluoroscopic view showed a subhepatic leak and quick opacification of the biliary tree ( Fig. 1 ).
Fig. 1.
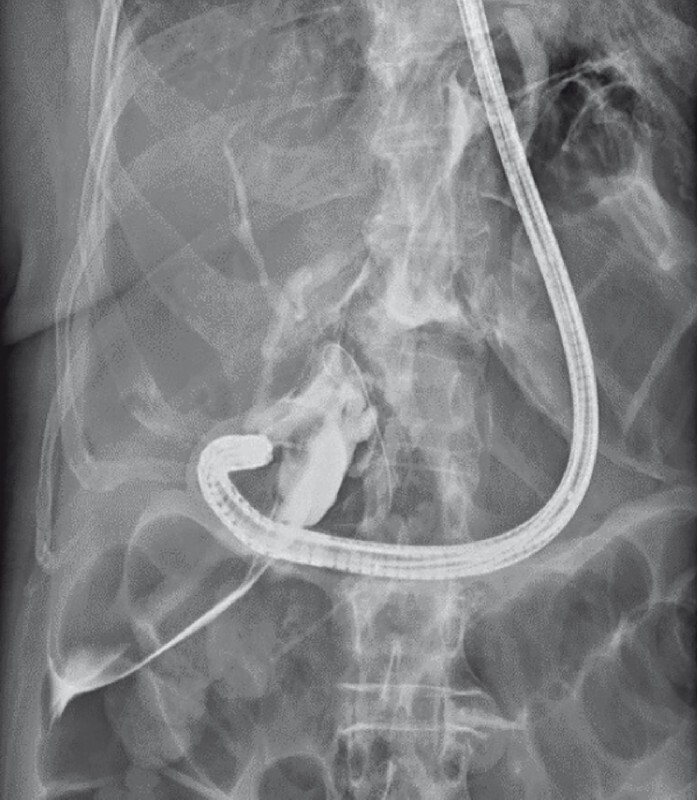
Evidence of gross biliary leak and bile duct opacification.
Careful inspection through the LAMS lumen using the front view gastroscope enabled us to identify the breach in the CBD: a guidewire was advanced antegrade through a 5-Fr biliary catheter into the CBD to the duodenum. This allowed transpapillary insertion of a guidewire with a sphincterotome using a duodenoscope. Then a fully covered metal stent was inserted to enable biliary drainage and closure of the perforation. The LAMS was removed, and the duodenal perforation was closed using two clips ( Fig. 2 ).
Fig. 2.

Biliary stent and clip closure of the duodenal defect.
The post-procedure period was uneventful and the patient was discharged after 6 days of hospitalization. Four weeks later the biliary stent was removed, choledochal stone clearance was completed, and the occlusion cholangiogram confirmed that the biliary leak was sealed ( Fig. 3 ).
Fig. 3.

Final occlusion cholangiogram showed no calculi or biliary leak.
Maldeployment of a LAMS during EUS-CDS can lead to a double perforation and requires prompt recognition and management 1 . When feasible, endoscopic rescue therapies are effective in managing this serious adverse event 2 3 4 5 ; endoscopists should be aware of possible solutions to a serious complication that would otherwise require a surgical approach.
Endoscopy_UCTN_Code_CPL_1AK_2AD
Footnotes
Competing interests The authors declare that they have no conflict of interest.
Endoscopy E-Videos : https://eref.thieme.de/e-videos .
Endoscopy E-Videos is an open access online section, reporting on interesting cases and new techniques in gastroenterological endoscopy. All papers include a high quality video and all contributions are freely accessible online. Processing charges apply (currently EUR 375), discounts and wavers acc. to HINARI are available. This section has its own submission website at https://mc.manuscriptcentral.com/e-videos
References
- 1.Fabbri C, Coluccio C, Binda C et al. Lumen-apposing metal stents: How far are we from standardization? An Italian survey. Endosc Ultrasound. 2022;11:59–67. doi: 10.4103/EUS-D-21-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Di Mitri R, Amata M, Mocciaro F et al. EUS-guided biliary drainage with LAMS for distal malignant biliary obstruction when ERCP fails: single-center retrospective study and maldeployment management. Surg Endosc. 2022;36:4553–4569. doi: 10.1007/s00464-021-08808-0. [DOI] [PubMed] [Google Scholar]
- 3.Sanchez-Ocana R, de Benito Sanz M, Nájera-Muñoz R et al. Rendezvous ERCP via endoscopic ultrasound-guided gallbladder drainage to salvage a dislodged lumen-apposing metal stent during choledochoduodenostomy. Endoscopy. 2022;54:65–67. doi: 10.1055/a-1368-3985. [DOI] [PubMed] [Google Scholar]
- 4.Fugazza A, Fabbri C, Di Mitri R et al. EUS-guided choledochoduodenostomy for malignant distal biliary obstruction after failed ERCP: a retrospective nationwide analysis. Gastrointest Endosc. 2022;95:896–904. doi: 10.1016/j.gie.2021.12.032. [DOI] [PubMed] [Google Scholar]
- 5.Graves M, Krafft M, Nasr J. EUS-guided choledochoduodenostomy creation using a biliary fully covered self-expanding metal stent after maldeployment of lumen-apposing metal stent. VideoGIE. 2021;6:234–235. doi: 10.1016/j.vgie.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]


