Abstract
Summary
The role of exercise in preventing osteoporotic fractures is vague, and further recommendations for optimized exercise protocols are very rare. In the present work, we provided positive evidence for exercise effects on the number of osteoporotic fractures in adults, albeit without observing any significant relevance of intensity progression or study duration.
Introduction
Osteoporotic fractures are a major challenge confronting our aging society. Exercise might be an efficient agent for reducing osteoporotic fractures in older adults, but the most promising exercise protocol for that purpose has yet to be identified. The present meta-analysis thus aimed to identify important predictors of the exercise effect on osteoporotic fractures in adults.
Methods
We conducted a systematic search of six literature databases according to the PRISMA guideline that included controlled exercise studies and reported the number of low-trauma major osteoporotic fractures separately for exercise (EG) and control (CG) groups. Primary study outcome was incidence ratio (IR) for major osteoporotic fractures. Sub-analyses were conducted for progression of intensity (yes vs. no) during the trial and the study duration (≤ 12 months vs. > 12 months).
Results
In summary, 11 studies with a pooled number of 9715 participant-years in the EG and 9592 in the CG were included. The mixed-effects conditional Poisson regression revealed positive exercise effects on major osteoporotic fractures (RR: 0.75, 95% CI: 0.54–0.94, p = .006). Although studies with intensity progression were more favorable, our subgroup analysis did not determine significant differences for diverging intensity progression (p = .133) or study duration (p = .883). Heterogeneity among the trials of the subgroups (I2 ≤ 0–7.1%) was negligible.
Conclusion
The present systematic review and meta-analysis provided significant evidence for the favorable effect of exercise on major osteoporotic fractures. However, diverging study and exercise characteristics along with the close interaction of exercise parameters prevented the derivation of reliable recommendations for exercise protocols for fracture reductions.
PROSPERO ID: CRD42021250467.
Keywords: Exercise training, Intensity progression, Major osteoporotic fractures, Study duration
Introduction
Low-trauma fractures related to osteoporosis are a major problem in our aging society. Considering the demographic change in Europe, the number of osteoporotic fractures will quite likely increase by about 25% during the next 10–15 years [1]. A large variety of pharmaceutic agents target osteoporosis, most of which are very cost intensive, have potential negative adverse effects, and focus predominately on the bone. In contrast, physical exercise is a low-cost approach providing positive effects on fall risk [2] and bone strength [3, 4] without causing relevant adverse effects [5]. Thus, exercise might be an excellent strategy for combatting fractures in older adults. Reviewing the literature shows that there is indeed some evidence for a fracture-preventing effect of exercise in older adults [6–9]. However, with the exception of an older systematic review and meta-analysis that focused on low-trauma overall fractures [7], all the other studies [6, 8, 9] focused on data regarding fall-related fractures. In a recent systematic review and meta-analysis, we determined significant positive effects of exercise on overall and major osteoporotic fracture incidence [10]. Nevertheless, due to the considerable heterogeneity between the trial results, it is important to identify key components of promising exercise protocols. While their close interaction might prevent a meaningful sub-analysis of many exercise parameters (e.g., exercise intensity), we focus on intensity progression during the trial and study duration, as these may well be more independent training parameters. Thus, besides providing evidence for a (osteoporotic) fracture-preventing effect of exercise, we concentrated on the corresponding effect of (1) the progression of intensity during exercise intervention and (2) the duration of the study intervention,1 in order to derive reliable exercise recommendations.
Methods
This systematic review and meta-analysis is part of the Austria/German/Swiss (DACH) S3 Guideline “körperliches Training zur Frakturprophylaxe” (AWMF: 183—002).
Literature search
We adopted the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [11]. Briefly, we checked six electronic databases (PubMed, Scopus, Web of Science, Cochrane, Science Direct, and ERIC) without language restrictions for articles published from January 1, 2013 (last search [7]) to May 2021. We applied keywords and their synonyms around the queries “Bone mass” or “Osteopenia” or “Bone turnover” or “Bone metabolism” or “Bone mineral content” or “Skeleton” or “Bone Mineral Density” or “BMD” or “Bone Density” or “Osteoporoses” or “Osteoporosis” or “Bone structure” or “Bone status” or “Bone Tissue” or “bone”) AND (“Bone fracture” or “Fracture” or “fragility fracture” or “Broken Bone”) AND (“Exercise” or “physical activity” or “Physical training” or “Exercise training”) AND (“clinical trial”) AND (“45 years and older”). We also checked reference lists of eligible studies and systematic reviews/meta-analysis that focused on fracture and fall reduction and bone-related outcomes (e.g., BMD). Studies without full texts were not considered.
Eligibility criteria
Briefly, randomized and non-randomized clinical studies were included that fulfilled the following eligibility criteria: (a) exercise studies on fracture prevention, fall reduction, and bone strength with (b) at least one exercise (EG) versus one control group (CG) that (c) reported the number of hip, lumbar spine, forearm, and/or humerus fractures (d) separately for EG and CG, independently of (e) whether fractures were defined as primary or secondary outcome, observation, or adverse event, and (e) female and male cohorts older than 50 years on average that were observed (f) for at least 3 months (i.e., study length ≥ 3 months).
Studies that supplied (a) pharmaceutic agents (e.g., glucocorticoids, bisphosphonates) or treatments (e.g., chemo- and/or radiotherapy) with relevant impact on bone metabolism, (b) trials/study groups with mixed interventions other than exercise and low-dosed calcium/cholecalciferol were excluded. We also excluded review articles, case reports, editorials, conference abstracts, letters, preliminary data, or duplicate studies. For the present subgroup analyses, studies (i.e., [12–14]) that terminated their intervention 6 months ago and longer were not considered.
Data extraction
During the first step, two reviewers (IH, MS) independently reviewed the titles and abstracts for eligible articles. Subsequently, full-text articles were reviewed by IH and WK. Eligible articles were extracted by IH and WK using a detailed extraction form that asked for study characteristics, study protocol, participant and exercise characteristics, supplementation, and fractures in the EG and CG. In the case of missing information, the authors in question were contacted (n = 6).
Outcome measures
As per FRAX [15], low-trauma fractures of the arm, forearm, or wrist and hip and vertebral fractures were summarized into major osteoporotic fracture as the primary study outcome of the present study. Fractures induced by falls from levels higher than standing and car or bicycle accidents were not included. However, in a minor variation from FRAX, all types of humerus and vertebral fractures were included.
Quality assessment
The Physiotherapy Evidence Database (PEDro) scale risk of bias tool [16] and the TESTEX (Tool for the assEssment of Study qualiTy and reporting in Exercise) score [17] specifically dedicated to evaluate the methodologic quality of physiotherapy and exercise trials was used to rate methodologic quality of the exercise trials.
Data synthesis
Of importance, we pooled the three different exercise groups of Karinkanta et al. [18] into one exercise group. With respect to the study of Bischoff-Ferrari et al. [19], we included the isolated exercise group (without vitamin D) with data provided by the authors. As stated, we focused on two research issues, intensity progression and duration of the exercise study in the sub-analyses. Two reviewers (IH, WK) independently categorized the trials into the subgroups, with full consensus for classification.
Statistical analysis
We used the mixed-effects conditional Poisson regression model suggested by Stijnen et al. [20] for our analysis. We applied R packages metafor [21] included in the statistical software R [22]. The incidences were transformed into incidence rate ratios (IR) along with 95% confidence intervals (95% CI). Heterogeneity between studies was checked using I2 statistics2 [23] in combination with a Wald and likelihood ratio test, respectively. Funnel plots with Kendall’s τ statistic were applied to explore potential small study/publication bias. Subgroup analyses were applied for subgroups as described in data synthesis above. All tests were 2-tailed, and significance was accepted at p < 0.05.
Results
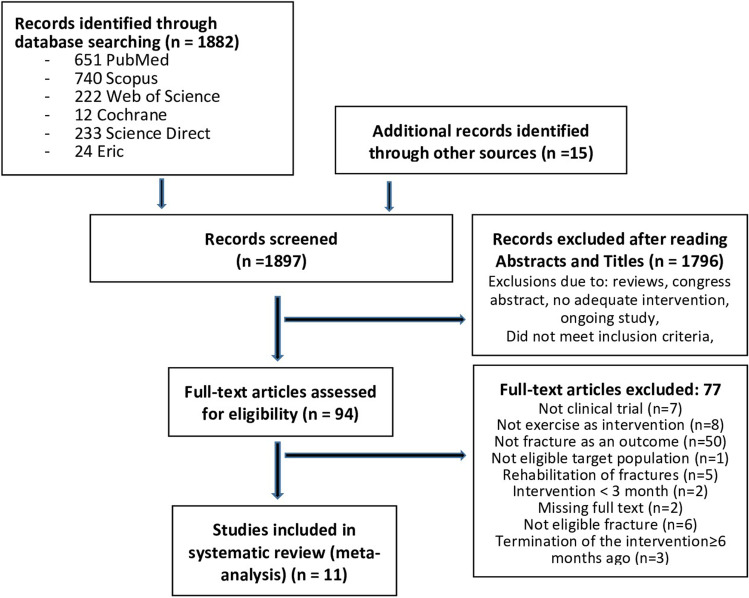
Our search identified 11 eligible studies [18, 19, 24–32] (Fig. 1) with a pooled number of participant years of n = 9715 in the EG and n = 9592 in CG. All studies included community dwelling middle-aged to older cohorts.
Fig. 1.
Flow-chart of the present systematic review according to PRISMA [11]
Table 1 gives a summary of the study and participant characteristics. In summary, no relevant between group differences (EG vs. CG) were observed for baseline participant characteristics of the individual studies. Initial sample sizes varied from 27 to 3279 participants/group. All but two studies [24, 32] included Caucasian cohorts on average between 54 ± 3 {Chan, 2004 #8453} and 80 ± 4 {Sakamoto, 2013 #15970} years of age. Seven studies focused exclusively on women. Six studies defined fracture risk as the primary outcome (Table 1).
Table 1.
Study and participant characteristics of the included studies
| First author, year, study-type | Study length [months] | Age [years], status | Female gender | Body Mass Index, [kg/m2] | Initial sample size [n] | Dropout [%] | Specific characteristics of the study group | Medication (%)a | Fracture as the primary outcome |
|---|---|---|---|---|---|---|---|---|---|
| Bischoff-Ferrari et al. 2020, RCT | 36 |
75 ± 4 cdw |
EG: 62% CG: 62% |
26.3 ± 4.2 26.4 ± 4.4 |
EG: 267 GC: 270 |
Total: 12 | No major health events, sufficiently mobile, good cognitive status, ≥ 40% with fall history |
EG: ≥ 48 CG: ≥ 51 |
Yes |
| Chan et al. 2004, RCT | 12 |
54 ± 3 cdw |
EG: 100% CG: 100% |
24.1 ± 4.7 23.5 ± 4.6 |
EG: 67 GC: 65 |
EG: 19 GC: 17 |
Early-postmenopausal healthy women without a history of fractures | none | No |
| Ebrahim et al. 1997, RCT | 24 |
67 ± 8 n.g |
EG: 100% CG: 100% |
n.g |
EG: 81 GC: 84 |
Total: 41 | Women with upper limb fractures during the last 2 years | n.g | No |
| Gill et al. 2016, RCT | 31 |
79 ± 5 n.g |
EG: 67% CG: 67% |
30.1 ± 5.7 30.3 ± 6.2 |
EG: 818 CG: 817 |
n.g | Functional limitations (SPPB ≤ 9; but 400 m ≤ 15 min) |
EG: 5.3b CG: 5.4 |
Yes?c |
| Karinkanta et al., 2007, RCT | 12 |
70–79 cdw |
EG: 100% CG: 100% |
28.1 ± 3.8 29.6 ± 3.7 |
EG: 112 CG: 37 |
EG: 4 GC: 3 |
No diseases or medication relevantly affecting falls or bone strength, no osteoporosis | none | No |
| Kemmler et al., 2010, RCT | 18 |
69 ± 4 cdw |
EG: 100% CG: 100% |
26.1 ± 4.0 26.9 ± 4.3 |
EG: 123 CG: 124 |
EG: 7 CG: 9 |
No diseases or medication relevantly affecting falls or bone strength | none | No |
| Kemmler et al., 2015, CT | 16 yrs |
55 ± 3 cdw |
EG: 100% CG: 100% |
25.7 ± 3.4 25.3 ± 4.2 |
EG: 86 GC: 51 |
EG: 31 CG: 9 |
Early-postmenopausal (1–8 y) women with osteopenia; no diseases/medication relevantly affecting falls or bone strength | none | Yes |
| Korpelainen et al., 2006, RCT | 30 |
70–73 cdw |
EG: 100% CG: 100% |
25.7 ± 3.4 25.5 ± 3.5 |
EG: 84 CG: 76 |
EG: 18 GC: 12 |
Low BMD at the proximal femur or distal radius (< -2 SD-T-score) | n.g | No |
| Lamb et al., 2020, cluster-RCT | 18 |
78 ± 6 cdw |
EG: 53% CG: 52% |
27 ± 5 26 ± 5 |
EG: 3279 GC: 3223 |
EG1: 16 CG: 14 |
People at increased risk for falls (falls risk screening questionnaire) | n.g | Yes |
| Preisinger et al. 1996d, RCT | 48 |
61 ± 7 cdw |
EG: 100% CG: 100% |
n.g |
EG: 27 GC: 31 |
EG: 56 GC: 0 |
Moderate back complaints, no medication relevantly affecting bone strength | n.g | No |
| Sakamoto et al., 2012, RCT | 6 |
ca. 80 ± 4 cdw |
EG: 79% CG: 83% |
23.2e 23.2 |
EG:714 GC: 651 |
EG: 43 CG: 30 |
Subjects with leg standing time ≤ 15 s; no other conditions relevantly affecting fall risk | n.g | Yes |
Cdw community dwelling, CT controlled trial, FaME fall management exercise, n.g. not given, OEP Otago Exercise Program, RCT randomized controlled trial
aOnly medication with moderate impact on falls or bone strength
bOverall number of drugs
cSerious fall injury: “fall resulting in a clinical non-vertebral fracture or that led to hospital admission”
dWe included the “fully compliant subgroup”
e…calculated from body height and mass
Exercise characteristics
Table 2 displays exercise characteristics of the included studies. The exercise program of three studies focused predominately on combined fall prevention/bone strengthening [25, 27, 28] or fall prevention protocols [26, 30, 32], while four studies [18, 24, 29, 31] concentrated on bone strengthening only. Length of the exercise intervention ranged from 6 months [32] to 16 years [28]. Unfortunately, not all of the studies reported the exercise intensity applied for the respective training component adequately and comprehensively (Table 2). With respect to physical interventions in the control group, at least three studies [19, 25, 27] implemented an “active control group.”
Table 2.
Exercise characteristics of the included studies
| First author, year | Fracture prevention strategy | Design, supervision | Length of intervention [months] | Type of exercise in the EG; supplementation | Exercise/strain composition | Progression of Intensity | Attendance rate | Intervention in the CG |
|---|---|---|---|---|---|---|---|---|
| Bischoff-Ferrari et al., 2020 | n.g.a | IE-PNS | 36 | DRT; no supplements | 3 × 30 min/week, 5 resistance type exercises (sit-to-stand, one-leg stance, pull backs, and external shoulder rotation against elastic resistance, steps); no details on strain composition given | No | n.g.b | Flexibility, 5 exercises, 3 × 30 min/ week |
| Chan et al., 2004 | Bone Strength | JE-PS | 12 | Tai Chi Chun: Yang style; no supplements | 5 × 50 min/week; all main muscle groups, no details on strain composition given | No | 84% | No intervention |
| Ebrahim et al., 1997 | Bone strength and fall reduction | IE-PNS | 24 | Brisk walking; no supplements | 3 × 40 min/week brisk walking presumably with moderate intensity (details n.g.) | No | 100% | Exercises for the upper limb; (details n.g.) study nurse-visits |
| Gill et al., 2016 | Fall prevention | IE-PNS | 26 | Multi-component: walking, lower extremity DRT, flexibility exercises for major muscle groups, balance; no supplements | In total: 5–6 × ≈30 min/week; presumably 2–3 × 30 min/week walking at RPE 13 (Borg CR-20), 3 × week 5 DRT exercises 2 sets × 10 reps at RPE 15–16 (Borg CR-20), 10 min of balance exercise and 3–5 min of stretching | Yes | 63% | No physical intervention, health education program |
| Karinkanta et al., 2007 | Bone strength | JE-PS | 12 | DRT for all main muscle groups vs. balance and high Impact exercise vs. multi-component: (DRT, impact, balance); no supplements | 3 × 45–50 min/week; DRT: 7 exercises, 3 sets, reps 8–10 reps at 75–80% 1RM | Yes | 67% | No intervention |
| Kemmler et al., 2010 | Bone strength/fall prevention | JE/IE-PS | 18 |
Multi-component: aerobic dance, DRT, functional gymnastics, isometric exercise; Up to 500 IU Vit-D/d; 1000 mg/d Ca |
In total 4 sessions/week; 2 × 60 min/week JE-S, aerobic dance at 70–85% HRmax, static/dynamic balance exercises, isometric/floor exercises at RM, 3 upper body exercises with 2–3 sets, 10–15 reps of with elastic bands at RM-2 reps; 3 leg exercises with 2 sets with 8 reps at RM-2reps; IE-NS: 2 × 25 min/week, 8 isometric and dynamic strength exercises | Yes |
60% JE-S: 77% IE-NS: 42% |
Wellness protocol. 4 × 10 week/18 1 × 60 min of mobility and flexibility exercise |
| Kemmler et al., 2015 | Bone strength/fall prevention | JE/IE-PS | 16 yrs | Multi-component: High impact aerobic dance, jumping, DRT, functional gymnastics, balance (last 4 years); up to 500 IU/d Vit-D, 1000 mg Ca/d | In total 4 sessions/week; 2 × 60 min/week JE-S, 20 min of HI aerobic dance at 70–85% HRmax, 4 × 15 different jumps; periodized DRT 9–13 exercises up to 90% 1RM with periods of high velocity; IE-NS: 2 × 25 min, 8 isometric and dynamic strength exercise; 5–6 flexibility exercises | Yes |
57% JE-S: 83% IE-NS:31% |
No intervention |
| Korpelainen et al., 2006 | Bone strength | JE/IE-PNS | 30 | Multi-component: HI aerobic exercises, jumps, balance, DRT; no supplements | JE-S for 6 months/year: 1 × 60 min + 6 × 20 min/week IE-NS intermitted by IE-NS (7 × 20 min/week); HI exercises, DRT in circuit mode ≥ 4 exercises, 3 sets of 30 s of exercise—30 s of rest, focus on maximum reps/30 s, shorter version during IE-NPS | Yes |
< 50% JE-S: 75% IE-NS:43% |
No physical intervention, social interaction, health information |
| Lamb et al., 2020 | Fall prevention | IE-PNS | 18 |
Multi-component: Otago Exercise Program (OEP); no supplements |
In total ≥ 3 × 30 min/week; 5 DRT-exercises with 4 intensity levels up to 2 sets of 10 reps; and 12 balance exercises with 4 levels; up to 4 sets of 10 steps; 2 × 30 min walking with habitual speed | No | n.g | Advice by mail |
| Preisinger et al., 1996 | Bone strength/back pain | IE-PNS | 48 | Physiotherapy incl. postural stability, motor control, coordination, functional DRT, flexibility; no supplements | ≥ 3 × 20 min/week; resistance exercises with elastic bands on unstable surface/seat | No | n.a.c | No exercise intervention partially massage, electro-therapy in EG and CG |
| Sakamoto et al., 2012 | Fall prevention | IE-PNS | 6 | Balance; no supplements | 7 × week, 3 sessions/d × 60 s one leg stand without holding on an object (when possible) | No | n.g | No intervention |
Ca calcium, DRT dynamic resistance exercise, IE individual exercise (predominately home-based), JE joint exercise (predominately facility-based), n.a. not applicable, n.g. not given, PNS predominately non-supervised, PS predominately supervised, RM repetition maximum, RPE rate of perceived exertion, Vit-D cholecalciferol
aThe intervention is more indicative of bone strength, but since bone parameters were not determined, we are unable to decide this issue
b70% of the participants carried out at least twice per week, 62% carried out at least 3 sessions/week
cIncluded were participants that exercised ≥ 3 × 20 min/week (44%)
Supplementation with vitamin D and/or calcium
Two studies [27, 28] provided calcium (up to 1000 mg/d) supplements for the EG and CG.
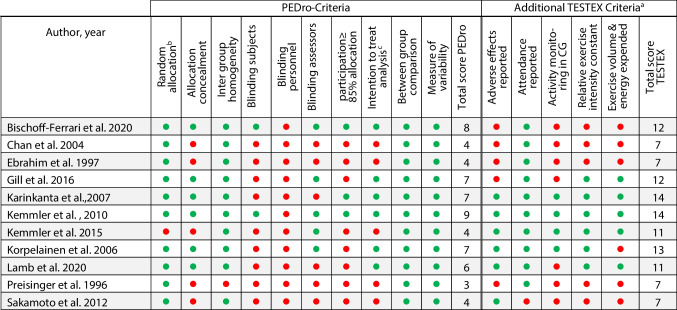
Methodological quality
The methodological quality is listed in Table 3. Score points applying PEDro vary between 3 and 9 from a maximum of 10 (9) points and 6–14 from a maximum of 15 when applying the TESTEX score. Of importance, blinding of instructors (i.e., treatment providers) is not applicable in exercise studies; consequently, the maximum score for PEDro should be considered 9 points. In contrast, TESTEX did not score blinding of treatment providers and participants.
Table 3.
Methodologic quality of the exercise studies
aTESTEX awards one point for listing the eligibility criteria and, also in contrast to PEDro, a further point for the between group comparison of at least one secondary outcome
bStudies that either have not randomly assigned participants to the groups (-) or retrospectively analyze for training frequency (n.a.)
c….. or all subjects received treatment or control as allocated (…or were retrospectively analyzed)
Altogether we observed 151 major osteoporotic fractures (MOF) in the exercise and 196 fractures in the control group. Excluding the follow-up studies, 126 MOF were observed in the EG versus 162 MOF in the CG. In detail, 44 versus 58 hip fractures were recorded in the EG vs. CG; in parallel 62 (EG) vs. 52 (CG) forearm and wrist fractures were reported. Unfortunately, some studies did not report vertebral fractures; thus, the number of 25 fractures in the EG vs. 49 in the CG might be considerably underreported.
Meta-analysis results
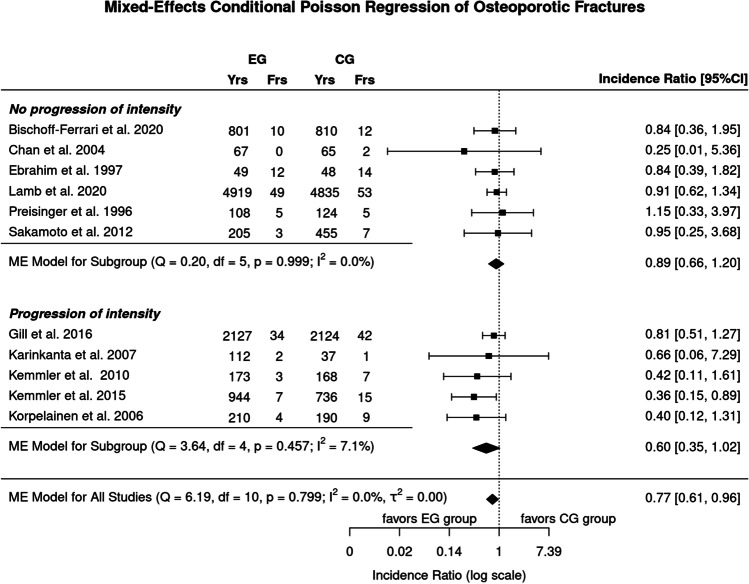
The meta-analysis demonstrated a significant (p = 0.006) effect of exercise on major osteoporotic fractures (IR: 0.75; 95% CI: 0.59–0.94) (Figs. 2 and 3, lower part). Heterogeneity between the trials (I2 < 1%) was negligible, and funnel plots and tests for funnel plot asymmetry indicate no relevant evidence for publication/small study bias.
Fig. 2.
Forest plot of data on the effect of “intensity progression during the trial” on exercise effects on major osteoporotic fracture risk
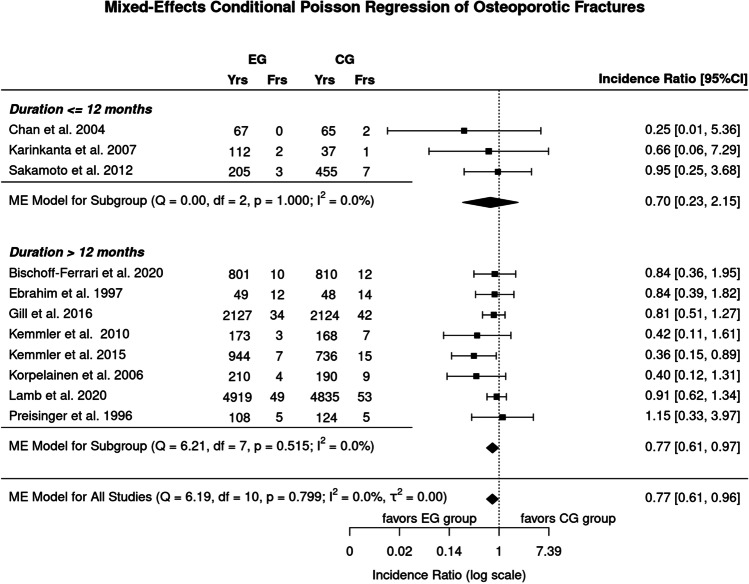
Fig. 3.
Forest plot of data on the effect of “study/intervention duration” on exercise effects on major osteoporotic fracture risk
Subgroup analysis on exercise components
Progression of intensity during the exercise trial
Five studies provided intensity progression in their exercise protocols [18, 26–29], while another six studies did not change exercise intensity during the intervention (Table 2, Fig. 2). While we observed more favorable effects in the subgroups that applied progression of intensity, in summary, we did not determine a significant difference between the two subgroups (p = 0.133) (Fig. 2). Heterogeneity between the trials was negligible for both subgroups (I2 = 0% and 7.1%).
Duration of the intervention protocol of the exercise trial
Only three studies applied study protocols ≤ 12 months [18, 24, 32], while another eight studies exercised > 12 months to 16 years (Table 2, Fig. 3). In contrast to the shorter studies/exercise interventions (IR: 0.70; 95% CI: 0.23 to 2.15), we observed significant effects for the exercise trials of longer duration (IR: 0.77; 95% CI: 0.61 to 0.97); however, in summary, no relevant differences between the two subgroups (p = 0.883) (Fig. 3) were observed. Heterogeneity between the trials was negligible for both subgroups (I2 = 0%).
Discussion
Apart from generating evidence for the fracture-preventing effect of exercise on low-trauma, major osteoporotic fractures [15], the present systematic review and meta-analysis aimed to determine parameters that might explain the effectiveness of exercise in reducing fractures related to osteoporosis in middle-aged to older adults. In summary the study provided evidence for a significant (major osteoporotic) fracture reducing effect of exercise; however, the sub-analysis on the relevance of intensity progression and exercise duration on this positive interaction did not significantly support the relevance of these important exercise parameters/principles.
Due to the close interaction of exercise parameters [33] and the few exercise trials that focus on definite outcomes of fracture reduction, it is a daunting task to identify key (exercise) parameters for generating meaningful recommendations for promising exercise protocols. This refers especially to the area of fracture reduction with its fundamentally different training strategies on bone strengthening and/or fall reduction [34]. As most exercise parameters (e.g., type of exercise, exercise intensity, training frequency) were confounded by the aspects described above, we focused on the principle of (intensity) progression and the duration of the study intervention because these can be considered superordinate variables of exercise training protocols.
Progression, i.e., the frequent adaptation of training load to persistently apply the overload principle [33], can be realized by changing several parameters including exercise frequency and/or intensity, type of exercise, or exercise duration. However, with few exceptions [27, 28], most of the included exercise trials focused (if at all) on the progression of exercise intensity. In summary, we observed more favorable effects of studies that applied intensity progression (vs. non-progression) on major osteoporotic fracture numbers; nevertheless, differences between the subgroups remained non-significant (Fig. 2). One may argue that progression might be negligible in studies of short duration, but the only study to which this could applied is the 6-month study of Sakamoto et al. [32]. Another reason for our finding might be that progression in particular of balance protocols was rarely reported and the corresponding studies were thus not correctly classified by our approach.
Although this aspect is not negligible for fall prevention studies [2] either, it is outweighed by duration of the study/intervention in exercise programs on bone strengthening due to the length of bone adaptation in adults [35, 36]. Furthermore, along with high sample sizes, study duration is important for generating enough statistical power to address fracture number as a clinical outcome [28]. Of importance only three studies applied exercise protocols of 6 [32] to 12 months [18, 24]. Comparing the latter studies with longer studies (Fig. 3), we observed comparable effects sizes for the two categories.
In summary, we provided further evidence for the (osteoporotic) fracture-reducing effect of exercises; however, we failed to determine key parameters of promising exercise parameters or training principles in this area. We predominately attribute this unfavorable result to the fact that due to participant characteristics,3 two fundamentally different exercise strategies, i.e., bone strengthening or fall reduction (or both), can be applied for reducing fracture risk. Considerable differences in addressing the two training aims confounded a joint analysis for meaningful exercise parameters and training principles. In parallel, against our expectation, with its close interaction of exercise parameters, the complexity of exercise might have also confounded our analysis of intensity progression and study duration. Since the methodologically correct approach for addressing this problem, i.e., trials with two exercise arms that differ only in the given component of interest (e.g., exercise frequency; [37]), was not available4 in the domain of fracture reduction, corresponding exercise recommendations have to be derived from more dedicated meta-analyses in the area of osteoporosis [38–40] or fall reduction [2, 41] or even better: from randomized controlled trials with similar or comparable training aims and cohorts.
Due to higher evidence standards, more dedicated inclusion criteria, higher fracture risk, and diverging fracture outcomes, it is difficult to set our results into perspective with data on pharmaceutic studies. However, a (very) rough overview on bisphosphonate (risedronate[42],5 zoledronate [43], denosumab [44], and teriparatide [45]) effects on fragility fracture incidence indicates results in the area of 20% (risedronate, non-vertebral fractures) to 54% (teriparatide, overall fragility fractures). Our result falls at the lower range; however, it should be borne in mind that all of these pharmaceutic studies focus on secondary preventions, i.e., subjects with a much higher fracture prevention potential. Evidence for a fracture preventing effect in the area of primary prevention is much lower to negligible (e.g., [42]). From a socioeconomic point of view, on the other hand, it would be wrong to conclude that exercise might be a true alternative to pharmaceutical therapy. A large proportion of frail elderly persons, the most vulnerable group for fractures, demonstrate low affinity to exercise [46] and will be hard to persuade to start exercising frequently. Nevertheless, the combination of bone strengthening drugs and fall prevention exercise will definitely be the most promising fracture reduction strategy for this cohort.
Apart from problems described above, other limitations and/or particularities of the present work might have affected our results. (1) We focused on low-trauma fractures and thus excluded fractures caused, for example, by bicycle or car accidents, or falls from levels higher than standing. However, due to unavailable data, we might have not included only “low-trauma fractures.” However, considering that in osteoporosis not only fragility fractures but also all forms of fractures, including high-impact trauma fractures, occur quite frequently, this limitation might be negligible. (2) We further subsume all types of vertebral and humerus fractures under “major osteoporotic fractures,” which is not consistent with FRAX [15]. (3) We included studies with “active control groups” (Table 3) which might have diluted our exercise effects on fracture reduction slightly. (4) We included one non-randomized controlled trial [28]. Although fully aware of potential sources of bias,6 we included this study due to its long duration (16 years), the sufficient power to address fracture as an outcome, and “fracture reduction” being stated as the primary outcome. (5) The latter aspect might be highly relevant since studies that focus on BMD effects (“bone-strength,” Table 3) in older people, for example, did not adequately address all the relevant fracture determinants and thus may have generated suboptimum results. (6) Heterogeneity between the trials was consistently negligible (i.e., I2: 0 to 7.1%) among the subgroups (Figs. 2 and 3). Further funnel plot analyses did not indicate evidence for publication/small-study bias. This finding is noteworthy because the studies vary widely with respect to participant (Table 1) and exercise characteristics (Table 2). (7) Finally, the statistical power to address differences between the subgroups can be considered moderate at best. Nevertheless, a recent (meta-)analysis on major osteoporotic fracture reduction that focused on supervision of the exercise program revealed significant differences in favor of supervised exercise protocols {Hoffmann, 2022 #16145}. Thus, the present analysis does not seem to be “hopelessly underpowered.”
Conclusion
Our systematic review and meta-analysis showed a 23% reduction in major osteoporotic fracture incidence, thus providing further evidence for the significant favorable effect of exercise on (low-trauma) fracture reduction. On the other hand, our joint analysis of exercise protocols that focus on bone strengthening, fall reduction, or both did not indicate high relevance of intensity progression or study duration. Along with others [47], we feel that meta-analyses might not be the best choice for deriving promising exercise recommendations, at least for the area of fracture reduction due to the complexity of exercise and the close interaction of exercise parameters. Well-designed and adequately powered randomized controlled trials might be more suitable to address this issue.
Acknowledgements
We acknowledge the support of the Elsbeth Bonhoff Stiftung, Berlin, Germany and the Dachverband Osteologie (DVO) e.V. We are also very grateful to all authors who provided missing information for the present work. The article was performed in (partial) fulfillment of the requirements for Isabelle Hoffmann’s obtaining the degree Dr. med. dent.
Author contribution
All authors conceived and designed this systematic review and meta-analysis and drafted and revised the manuscript. Article search, screening, data extraction, and rating were performed by IH, MS, SvS, DS, HBF, and WK, and formal analysis was conducted by WK and MK. All authors read the final version of the manuscript. WK accepts direct responsibility for the work.
Funding
Open Access funding enabled and organized by Projekt DEAL. This research received no external funding; however, the project S3-Guideline “körperliches Training zur Frakturprophylaxe” was supported by the Elsbeth Bonhoff Foundation.
Data availability
The data that support the findings of this study are available from the corresponding author (WK), upon reasonable request.
Declarations
Statement of human rights
This article does not cover any studies with human participants or animals performed by any of the authors.
Conflicts of interest
None.
Informed consent
Not applicable.
Footnotes
More precisely, the studies listed the length of the intervention as “study duration.” Since no included study reported a delay between baseline or follow-up assessment and start or end of the intervention, we consistently use the term “study duration.”.
0–40%, low; 30–60%, moderate; 50–90%, substantial; 75–100%, considerable heterogeneity.
E.g., early-postmenopausal osteopenic women with high bone turnover and low risk of falls versus vulnerable older people with manifest osteoporosis, pharmaceutic therapy, and high fall risk.
Certainly due to the need to generate an enormous power (ie number of participant years) to address fracture number as an outcome considering further the potentially small differences between the groups….
In the area of secondary prevention; effects on primary prevention were much lower.
While we do not observe differences in prognostic outcome measures, adherence rates were higher compared to most comparable RCTs.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kanis JA, Norton N, Harvey NC, et al. SCOPE 2021: a new scorecard for osteoporosis in Europe. Arch Osteoporos. 2021;16:82. doi: 10.1007/s11657-020-00871-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sherrington C, Michaleff ZA, Fairhall N, et al. Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med. 2017;51:1750–1758. doi: 10.1136/bjsports-2016-096547. [DOI] [PubMed] [Google Scholar]
- 3.Shojaa N, von Stengel S, Schoene D, et al. Effect of exercise training on bone mineral density in postmenopausal women: a systematic review and meta-analysis of intervention studies. Front Physiol. 2020;11:1427–1444. doi: 10.3389/fphys.2020.00652. [DOI] [Google Scholar]
- 4.Mages M, Shojaa M, Kohl M, et al. Exercise effects on bone mineral density in men. Nutrients. 2021;13:4244. doi: 10.3390/nu13124244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kunutsor SK, Leyland S, Skelton DA, et al. Adverse events and safety issues associated with physical activity and exercise for adults with osteoporosis and osteopenia: a systematic review of observational studies and an updated review of interventional studies. J Frailty Sarcopenia Falls. 2018;3:155–178. doi: 10.22540/JFSF-03-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Souto BP, Rolland Y, Vellas B, Maltais M. Association of long-term exercise training with risk of falls, fractures, hospitalizations, and mortality in older adults: a systematic review and meta-analysis. JAMA Intern Med. 2019;179:394–405. doi: 10.1001/jamainternmed.2018.5406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kemmler W, Haberle L, von Stengel S. Effects of exercise on fracture reduction in older adults: a systematic review and meta-analysis. Osteoporos Int. 2013;24:1937–1950. doi: 10.1007/s00198-012-2248-7. [DOI] [PubMed] [Google Scholar]
- 8.Wang Q, Jiang X, Shen Y, et al. Effectiveness of exercise intervention on fall-related fractures in older adults: a systematic review and meta-analysis of randomized controlled trials. BMC Geriatr. 2020;20:322. doi: 10.1186/s12877-020-01721-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhao R, Feng F, Wang X. Exercise interventions and prevention of fall-related fractures in older people: a meta-analysis of randomized controlled trials. Int J Epidemiol. 2017;46:149–161. doi: 10.1093/ije/dyw142. [DOI] [PubMed] [Google Scholar]
- 10.von Stengel S, Becker C, Gosch M, Jakob F, Kerschan-Schindl K, Kladny B, Clausen J, Lange U, Middeldorf S, Peters S, Schoene D, Sieber C, Tholen R, Thomasius F, Bischoff-Ferrari HA, Uder M, Kemmler W (2022) Exercise reduces the number of overall and major osteoporotic fractures in adults. Does supervision make a difference? Systematic review and meta-analysis. J Bone Miner Res. 10.1002/jbmr.4683. Online ahead of print [DOI] [PubMed]
- 11.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karinkanta S, Kannus P, Uusi-Rasi K, Heinonen A, Sievanen H. Combined resistance and balance-jumping exercise reduces older women’s injurious falls and fractures: 5-year follow-up study. Age Ageing. 2015;44:784–789. doi: 10.1093/ageing/afv064. [DOI] [PubMed] [Google Scholar]
- 13.Korpelainen R, Keinanen-Kiukaanniemi S, Nieminen P, Heikkinen J, Vaananen K, Korpelainen J. Long-term outcomes of exercise: follow-up of a randomized trial in older women with osteopenia. Arch Intern Med. 2010;170(17):1548–1556. doi: 10.1001/archinternmed.2010.311. [DOI] [PubMed] [Google Scholar]
- 14.Sinaki M, Itoi E, Wahner HW, et al. Stronger back muscles reduce the incidence of vertebral fractures: a prospective 10 year follow-up of postmenopausal women. Bone. 2002;30:836–841. doi: 10.1016/S8756-3282(02)00739-1. [DOI] [PubMed] [Google Scholar]
- 15.Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E. FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int. 2008;19:385–397. doi: 10.1007/s00198-007-0543-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sherrington C, Herbert RD, Maher CG, Moseley AM. PEDro. A database of randomized trials and systematic reviews in physiotherapy. Man Ther. 2000;5:223–226. doi: 10.1054/math.2000.0372. [DOI] [PubMed] [Google Scholar]
- 17.Smart NA, Waldron M, Ismail H, et al. Validation of a new tool for the assessment of study quality and reporting in exercise training studies: TESTEX. Int J Evid Based Healthc. 2015;13:9–18. doi: 10.1097/XEB.0000000000000020. [DOI] [PubMed] [Google Scholar]
- 18.Karinkanta S, Heinonen A, Sievanen H, et al. A multi-component exercise regimen to prevent functional decline and bone fragility in home-dwelling elderly women: randomized, controlled trial. Osteoporos Int. 2007;18:453–462. doi: 10.1007/s00198-006-0256-1. [DOI] [PubMed] [Google Scholar]
- 19.Bischoff-Ferrari HA, Vellas B, Rizzoli R, et al. Effect of vitamin D supplementation, omega-3 fatty acid supplementation, or a strength-training exercise program on clinical outcomes in older adults: the DO-HEALTH randomized clinical trial. JAMA. 2020;324:1855–1868. doi: 10.1001/jama.2020.16909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stijnen T, Hamza TH, Ozdemir P. Random effects meta-analysis of event outcome in the framework of the generalized linear mixed model with applications in sparse data. Stat Med. 2010;29:3046–3067. doi: 10.1002/sim.4040. [DOI] [PubMed] [Google Scholar]
- 21.Viechtbauer W. Conducting meta-analyses in R with the metafor Package. J Stat Softw. 2010;36:1–48. doi: 10.18637/jss.v036.i03. [DOI] [Google Scholar]
- 22.R-Core-Team (2021) R. A language and environment for statistical computing. In R Foundation for Statistical Computing (ed), stij edn. https://www.R-project.org/. Vienna, Austria
- 23.Higgins J, Thomas J, Chandler J et al (2021) Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2021). Cochrane, 2021
- 24.Chan K, Qin L, Lau M, et al. A randomized, prospective study of the effects of Tai Chi Chun exercise on bone mineral density in postmenopausal women. Arch Phys Med Rehabil. 2004;85:717–722. doi: 10.1016/j.apmr.2003.08.091. [DOI] [PubMed] [Google Scholar]
- 25.Ebrahim SB, Thompson PW, Baskaran V, Evans K. Randomized placebo controlled trial of brisk walking in the prevention of postmenopausal osteoporosis. Age Aging. 1997;26:252–260. doi: 10.1093/ageing/26.4.253. [DOI] [PubMed] [Google Scholar]
- 26.Gill TM, Pahor M, Guralnik JM, et al. Effect of structured physical activity on prevention of serious fall injuries in adults aged 70–89: randomized clinical trial (LIFE Study) BMJ. 2016;352:i245. doi: 10.1136/bmj.i245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kemmler W, von Stengel S, Engelke K, Haberle L, Kalender WA. Exercise effects on bone mineral density, falls, coronary risk factors, and health care costs in older women: the randomized controlled senior fitness and prevention (SEFIP) study. Arch Intern Med. 2010;170(2):179–185. doi: 10.1001/archinternmed.2009.499. [DOI] [PubMed] [Google Scholar]
- 28.Kemmler W, Bebenek M, Kohl M, Von Stengel S. Exercise and fractures in postmenopausal women. Final results of the controlled Erlangen Fitness and Osteoporosis Prevention Study (EFOPS) Osteoporos Int. 2015;26:2491–2499. doi: 10.1007/s00198-015-3165-3. [DOI] [PubMed] [Google Scholar]
- 29.Korpelainen R, Keinanen-Kiukaanniemi S, Heikkinen J, Vaananen K, Korpelainen J. Effect of exercise on extraskeletal risk factors for hip fractures in elderly women with low BMD: a population-based randomized controlled trial. J Bone Miner Res. 2006;21:772–779. doi: 10.1359/jbmr.060116. [DOI] [PubMed] [Google Scholar]
- 30.Lamb SE, Bruce J, Hossain A, et al. Screening and intervention to prevent falls and fractures in older people. N Engl J Med. 2020;383:1848–1859. doi: 10.1056/NEJMoa2001500. [DOI] [PubMed] [Google Scholar]
- 31.Preisinger E, Alacamlioglu Y, Pils K, et al. Exercise therapy for osteoporosis: results of a randomised controlled trial. Br J Sports Med. 1996;30:209–212. doi: 10.1136/bjsm.30.3.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sakamoto K, Endo N, Harada A, et al. Why not use your own body weight to prevent falls? A randomized, controlled trial of balance therapy to prevent falls and fractures for elderly people who can stand on one leg for </=15 s. J Orthop Sci. 2013;18:110–120. doi: 10.1007/s00776-012-0328-3. [DOI] [PubMed] [Google Scholar]
- 33.Weineck J. Optimales training. Erlangen: Spitta-Verlag; 2019. [Google Scholar]
- 34.Kemmler W, Stengel V, editors. The role of exercise on fracture reduction and bone strengthening. London: Avademic Press; 2019. [Google Scholar]
- 35.Erben RG. Hypothesis: coupling between resorption and formation in cancellous bone remodeling is a mechanically controlled event. Front Endocrinol (Lausanne) 2015;6:82. doi: 10.3389/fendo.2015.00082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eriksen EF. Cellular mechanisms of bone remodeling. Rev Endocr Metab Disord. 2010;11:219–227. doi: 10.1007/s11154-010-9153-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zitzmann AL, Shojaa M, Kast S, et al. The effect of different training frequency on bone mineral density in older adults. A comparative systematic review and meta-analysis. Bone. 2021;154:116230. doi: 10.1016/j.bone.2021.116230. [DOI] [PubMed] [Google Scholar]
- 38.Beck BR, Daly RM, Singh MA, Taaffe DR. Exercise and Sports Science Australia (ESSA) position statement on exercise prescription for the prevention and management of osteoporosis. J Sci Med Sport. 2016;20:438–445. doi: 10.1016/j.jsams.2016.10.001. [DOI] [PubMed] [Google Scholar]
- 39.Daly RM, Dalla Via J, Duckham RL, Fraser SF, Helge EW. Exercise for the prevention of osteoporosis in postmenopausal women: an evidence-based guide to the optimal prescription. Braz J Phys Ther. 2019;23:170–180. doi: 10.1016/j.bjpt.2018.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Giangregorio LM, McGill S, Wark JD, et al. Too fit to fracture: outcomes of a Delphi consensus process on physical activity and exercise recommendations for adults with osteoporosis with or without vertebral fractures. Osteoporos Int. 2015;26:891–910. doi: 10.1007/s00198-014-2881-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sibley KM, Thomas SM, Veroniki AA, et al. Comparative effectiveness of exercise interventions for preventing falls in older adults: a secondary analysis of a systematic review with network meta-analysis. Exp Gerontol. 2021;143:111151. doi: 10.1016/j.exger.2020.111151. [DOI] [PubMed] [Google Scholar]
- 42.Wells GA, Hsieh SC, Zheng C, Peterson J, Tugwell P, Liu W. Risedronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2022;5:CD004523. doi: 10.1002/14651858.CD004523.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Black DM, Delmas PD, Eastell R, et al. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med. 2007;356(18):1809–1822. doi: 10.1056/NEJMoa067312. [DOI] [PubMed] [Google Scholar]
- 44.McCloskey EV, Johansson H, Oden A, et al. Denosumab reduces the risk of osteoporotic fractures in postmenopausal women, particularly in those with moderate to high fracture risk as assessed with FRAX. J Bone Miner Res. 2012;27:1480–1486. doi: 10.1002/jbmr.1606. [DOI] [PubMed] [Google Scholar]
- 45.Neer RM, Arnaud CD, Zanchetta JR. Effect of parathyroid hormone (1–34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med. 2001;344:1434–1441. doi: 10.1056/NEJM200105103441904. [DOI] [PubMed] [Google Scholar]
- 46.Carlson SA, Fulton JE, Schoenborn CA, Loustalot F. Trend and prevalence estimates based on the 2008 Physical Activity Guidelines for Americans. Am J Prev Med. 2010;39:305–313. doi: 10.1016/j.amepre.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 47.Gentil P, Arruda A, Souza D, et al. Is there any practical application of meta-analytical results in strength training? Front Physiol. 2017;8:1. doi: 10.3389/fphys.2017.00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author (WK), upon reasonable request.