Abstract
Introduction
Home parenteral nutrition (HPN) is essential for patients with intestinal failure requiring long-term nutritional support. The Amerita Quality Improvement Project for HPN Patients (QIP-PN) explored the effect of a physician nutrition expert (PNE)-led multidisciplinary nutritional support team (MNST) on HPN care for patients under its service.
Objective
To determine an MNST effect on adherence to protocols, outcomes and quality of life (QOL) in HPN.
Methods
The study was divided into three phases: data review (phases 1a and 1b), observation (phase 2) and intervention (phase 3). Seven Amerita locations were selected as ‘study branches’ (population), from which all study patients and controls were drawn. The quality improvement project employed a quasi-experimental case-matched control group (control) design. Data were collected on demographics, treating physicians PNE status, HPN care variables, recommended interventions, quality-of-life assessment, adverse outcomes and hospitalisations. Paired t-test compared continuous data between phases 2 and 3. Comparisons between study and control groups used a negative binomial regression model.
Results
Thirty-four patients were reviewed in phase 1a and 197 in phase 1b. Forty study patients completed phase 2 and progressed into phase 3, of whom 30 completed ≥60 therapy days. Patients were lost to follow-up if they discontinued HPN for any reason. Improvements in weight, body mass index and QOL were seen in the study patients during intervention. Recommendations made and accepted by treating physicians differed based on PNE status. Study patients had fewer adverse outcomes and related hospitalisations than controls.
Conclusion
MNST recommendations improved clinical, biochemical parameters and patients’ self-reported overall health. MNST input reduced adverse outcomes, hospitalisation and the length of stay at the hospital. This study highlights the potential for MNST to have a significant impact on the quality and overall cost of HPN management.
Keywords: Nutrition assessment, Nutritional treatment, Malnutrition, Inflammatory bowel disease, Precision nutrition
WHAT IS ALREADY KNOWN ON THIS TOPIC.
Proper home parenteral nutrition (HPN) surveillance requires nutritional support team (NST) monitoring. In the USA, NST monitoring of HPN patients is often performed without the input of a physician nutrition expert (PNE). This study was needed to examine whether a PNE-led multidisciplinary NST (MNST) could improve measurable parameters of HPN care.
WHAT THIS STUDY ADDS
The study demonstrated that MNST recommendations improved clinical and biochemical parameters along with patients’ self-reported overall health. Furthermore, MNST input reduced adverse outcomes, hospitalisation and hospital length of stay.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
MNST input has the potential to significantly impact the quality, outcomes and overall cost of HPN management.
Introduction
Home parenteral nutrition (HPN) is a life-sustaining therapy for >25 000 US individuals (7.9/100 000) with intestinal failure (IF).1–3 HPN affords these patients functional lifestyles; avoiding hospital confinement4 5 while reducing overall cost of care.6 Appropriate HPN surveillance requires monitoring by a nurse, pharmacist and dietitian, who comprise a nutrition support team (NST).5 7–19 At advanced centres, NSTs may also include physician nutrition experts (PNE).20
US HPN patients are typically serviced by a home infusion company, whose NST members assist referring physicians in HPN management. The input of a PNE is not required to provide HPN.21 Implementation of HPN standards22–25 may rely on the treating physicians.26–28 This is concerning because the majority of HPN patients are managed by physicians without nutrition certification (internal data, Amerita].
This investigator-initiated study explored opportunities for quality improvement (QI) in HPN. Our objective was to determine the effect of a multidisciplinary NST (MNST), including a PNE, on adherence to protocols, outcomes of HPN care variables and quality of life (QOL) in HPN.
The primary hypothesis was that MNST intervention would improve HPN care variables. Another hypothesis was that MNST intervention would decrease adverse events such as unplanned hospitalisations. In this report, we detail our findings on MNST intervention on QI for HPN management.
Methods
Amerita, a national home infusion organisation (Amerita), established a QI project for HPN patients (QIP-PN). A MNST was created, consisting of a PNE, certified nutrition support clinicians (CNSC; Registered Dietitian (RD), Registered Nurse (RN), Registered Pharmacist (RPh)) and administrators. The QIP-PN study protocol examined multiple aspects of care for all HPN patients serviced by the organisation. The study Oversight and Safety Committee consisted of three non-affiliated PNEs.
Study design
Seven Amerita locations were selected as ‘study branches’ based on their case-load of long-term (>90 days) HPN patients. Amerita branches provide a variety of home infusion services other than HPN (ie, intravenous antibiotics, biologicals). The number of HPN patients at any given Amerita branch varies based on referral sources. Study branches were selected because they had a higher percentage of long-term HPN patients than non-study branches. Study branches tended to have more experienced HPN nurses, pharmacists and dietitians
All patients in the study were drawn from the population of long-term HPN patients at the study branches. As part of a QI project rather than a randomised controlled study, we employed a quasi-experimental design with a case-matched control group. The case-matched control group patients were randomly selected from long-term HPN patients at the study branches. This enabled us to compare MNST interventions to usual care.
The study was divided into three phases. Feasibility testing was conducted in phase 1a, in which patients at the study branches were randomly selected to determine that study parameters (table 1) could be extracted from medical records.
Table 1.
Study parameters examined in patients during phases 1a, 2 and 3
| Parameter | Data collection |
| Hospital | Name and initial discharge dates |
| PN prescriber characteristics | Degree, specialty, nutrition certification |
| Patient demographics | Age, gender, diagnoses, reason for home PN, CIRS Score |
| Patient QOL assessment | EQ-5D-3L |
| PN characteristics | Macronutrients, micronutrients, osmolarity, infusion cycle |
| Catheter Information | Catheter type, dressing type, insertion date, reinsertion date(S)/reason(S), infection type/dates, occlusions type/dates, other complications |
| Nursing | Agency, visit frequency |
| Lab draw | Frequency |
| Physician office visit | Frequency |
| PN Formula adjustment | Frequency |
| Visits to ED | Name, dates, reasons |
| Rehospitalisations | Name, dates, reasons |
| Payer(s) | Federal, commercial |
| Cost of PN formulation | Daily, weekly, monthly |
| MNST recommended changes | No of recommendations, accepted? Yes/No |
| Qualitative assessment of benefit | Grounded theory |
| Outcomes | Access device events, adverse drug reactions, ED use, unplanned hospitalisation |
CIRS, Cumulative Illness Rating Scale; ED, emergency department; EQ-5D-3L, Euroquol 5 Dimension-3 Level; MNST, multidisciplinary nutritional support team; PN, parenteral nutrition; QOL, quality of life.
HPN complications rates were collected in phase 1b as part of QI HPN outcome reporting. This data established the baseline complication rates for comparison to actively enrolled patients in phases 2 and 3. Acquisition of this data also permitted us to create a case-matched control group from within the phase 1b patients with similar characteristics to the study group.
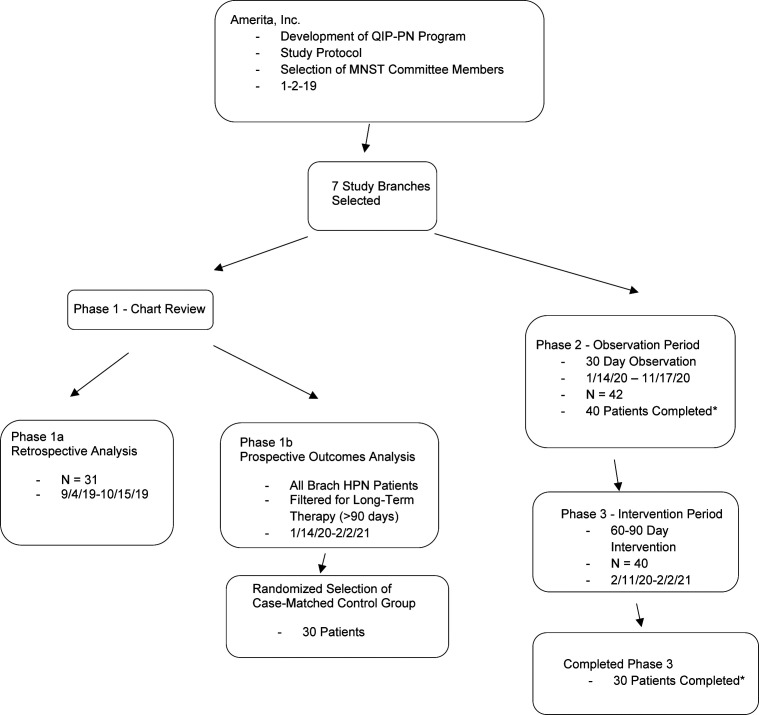
Consented study branch HPN patients were enrolled and monitored in phases 2 and 3. The same patients flowed through from phase 2 to 3 except for those lost to follow-up. In phase 2, data were collected during HPN care with observation only. In phase 3, the MNST made recommendations to the management team regarding HPN care (figure 1).
Figure 1.
Flowsheet of patient selection and participation in the Amerita QIP-PN Study. *Patients were lost to follow up if they discontinued HPN for any reason. HPN, home parenteral nutrition; MNST, multidisciplinary nutritional support team; QIP-PN, Quality Improvement Project for parenteral nutrition.
Study groups
The actual number of patients in any group varied because patients who were selected may have come off service before data collection was complete. Phase 1a was solely intended to confirm that study parameters (table 1) were retrievable from Amerita patient records. In phase 1b, all study branch long-term HPN patients were monitored for outcomes. All phase 1b patients were offered participation in phases 2 and 3. After providing informed consent, patients’ PN prescribing physicians were asked to sign physician study participation agreements. Patients from whom both informed consent and treating physician study participation agreements were obtained comprised the study group (figure 1).
The same patients were followed longitudinally through phases 2 and 3. The only difference between the phase 2 and 3 study population was the subtraction of patients who were lost to follow-up. The case-matched control group patients (controls) were randomly selected from phase 1b patients. Analysis of outcomes and PN management in the case–control group enabled us to establish a basis for these parameters under conditions of usual care.
Study components and timing
Phase 1a was conducted from 1 September 2019 to 15 October 2019. Phase 1b was conducted from January 2020 too February 2021. Phase was performed between January 2020 and November 2020. Phase 3 was conducted from February 2020 to February 2021. During phase 3, the MNST made management recommendations for adjustments in HPN care in accordance with established practice guidelines. These recommendations were provided to the patient’s treating physician by an Amerita branch clinician. The acceptance of MNST recommendations by the patient’s PN prescribing physician was recorded.
MNST interactions
Weekly telephonic MNST meetings were held as case conferences via indirect chart review. No patients were physically or virtually examined by the MNST members. The MNST functioned only as a consultancy service to the treating team based on data collected from the patient’s treatment team and homecare nurse.
The MNST recommendations were limited to those that related directly to the HPN process. The recommendations included macronutrient adjustments to conform to recommended guidelines, the addition or subtraction of micronutrients based on clinical and lab findings, changes in PN volume and rate based on patient responses, laboratory testing to conform to published standards and the frequency of home nursing and clinic visits.
For example, the MNST addressed noncompliance of specialised laboratory testing for micronutrients and essential fatty acids. When the MNST recommended additional lab testing the samples were obtained by the home healthcare nurse as part of usual patient care. The MNST also addressed instances in which laboratory or clinical findings were recorded but not acted on. Other issues, such as optimising intestinal rehabilitation, dietary adjustments and medication recommendations/adjustments were considered outside the scope of the MNST.
Data collection
In phase 1b, HPN outcomes were monitored prospectively in study branch patients as part of the National Home Infusion Foundation (NHIF) benchmark reporting process. In phases 2 and 3, data on the study parameters were prospectively collected on enrolled study patients during weekly virtual meetings of the MNST.
Statistical analysis
Comparisons between phase 2 and phase 3 patient data were performed by paired t-test, which was utilisable because the same patients were followed through both phases. Therefore, the study patients in the observation period (phase 2) served as their own controls for the intervention period (phase 3). For the comparison between the phase 3 study group and controls, an independent samples t-test was used only when the outcome variable is assumed to have normal distribution in the population. Comparison between the study and control groups used a negative binomial regression model for modelling outcome variable, rate of adverse events per 90-day period. A negative binomial regression model was needed for modelling rate of adverse events per 90-day period as it is a count variable inflated with zeros. Statistical analysis was conducted using R ( https://www.r-project.org/ ).
PNE status of treating physicians
HPN treating physicians were classified as being either PNE or non-PNE, defined as those who were either board certified by the National Board of Physician Nutrition Specialists or had CNSC designation.
Study instruments
Patient QOL assessment
The Euroquol 5 Dimension-3 Level (EQ-5D-3L) quality-of-life instrument was chosen for its simplicity, acceptance and prior application in HPN.29–31 The EQ-5D-3L system has five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Each dimension has three levels: no problems, some problems, extreme problems. Patients select the most appropriate statement in each dimension. A sixth dimension records the patient’s overall self-rated health state on a 0–100 scale where the endpoints are ‘Worst and Best Imaginable’. This was a quantitative reflection of the patient’s perception of health, scored as a Visual Analogue Scale (VAS).
The EQ-5D-3L was administered at the start of phase 2, start and end of phase 3. Due to COVID-19 restrictions on in-person contact, the EQ-5D-3L was administered via a telephone interview by an independent patient care coordinator who was not a member of the MNST, in accordance with the EQ-5D-3L guidelines.32 For this study, we used VAS score as a proxy for QOL.
Measure of multimorbidity and disease burden
We explored the use of multimorbidity scales for their application to HPN patients and elected to measure disease burden on study and control patients with the Cumulative Illness Rating Scale (CIRS).33 CIRS analyses multimorbidity by reviewing 14 body system categories, graded from 0 to 4.34–36 The CIRS approach has been validated as a predictor of hospitalisation, readmission and long-term mortality. CIRS scores range from 0 to 56.
Members of the MNST calculated comorbidity and illness severity, using the CIRS, based on information available in each patient’s electronic medical records. This included admission notes, medications, nursing notes, emergency department (ED) notes, imaging studies, physical and occupational therapy assessments, treatment/care plans and discharge summaries.
Results
Phase 1a/1b results
Phase 1a reviewed 34 patients. Phase 1b monitored 197 patients with 203 outcomes reported. Results for comparison in each outcome category were expressed in events per 1000 days of homecare service (the NHIF standard) and events per patient (table 2).
Table 2.
Phase 1b results
| Adverse outcome event | Events/1000 HPN days of service | Events/patient |
| Access device events | 0.384 | 0.09 |
| Adverse drug reactions | 0.021 | 0.07 |
| Emergency department visits | 0.277 | 0.01 |
| Unplanned hospitalisations | 3.647 | 0.87 |
| Therapy-related unplanned hospitalisations | 0.789 | 0.19 |
| Therapy unrelated unplanned hospitalisations | 2.858 | 0.68 |
| Overall adverse outcomes | 4.33 | 1.03 |
Note. Adverse outcomes in 197 long-term HPN patients at 7 study branches.
HPN, home parenteral nutrition.
Phase 2/3 results
Forty-two patients were enrolled in the study. Forty completed 30 days or more of observation in phase 2 and progressed into phase 3. Thirty patients completed 60 days or more in phase 3. Patient were lost to follow-up if HPN was discontinued for any reason.
Results among participants between phases 2 and 3 for monitored parameters (tables 3–6).
Table 3.
Descriptive statistics of continuous variables for patients in phases 2 and 3
| Characteristic | Phase 2 (M±SD), n=40 | Phase 3 (M±SD), n=30 |
| Weight (kg) | 59.93±17.16 | 61.0±16.85 |
| Weight with outliers removed (kg) | 52.77±17.24 | 54.55±17.18* |
| BMI | 20.20±5.27 | 20.49±5.31** |
| BMI with outliers removed | 18.9±5.23 | 19.6±5.23* |
| IBW (kg) | 60.15±9.66 | 60.15±9.66 |
| % IBW | 99.47±23.84 | 101.69±24.57 |
| % IBW with outliers removed | 98.72±23.78 | 102.38±24.30*** |
| PN formulation | ||
| Total Kcal/day | 1412±355.47 | 1405±387.10 |
| Total Kcal/kg/day | 25.10±8.56 | 24.91±10.04 |
| Non-protein Kcal/day | 1084±329.75 | 1074.37±363.71 |
| Non-protein Kcal/kg/day | 19.35±7.43 | 19.21±8.88 |
| Dextrose g/day | 218.14±81.88 | 218.95±79.87 |
| Dextrose g/kg/day | 3.83±1.63 | 3.85±1.77 |
| Amino acids g/day | 82.07±20.98 | 82.85±21.01 |
| Amino acids g/kg/day | 1.44±0.46 | 1.42±0.44 |
| Lipid g/day | 34.25±16.70 | 32.99±17.61 |
| Lipid g/kg/day | 0.63±0.41 | 0.62±0.41 |
| PN total volume | 1648.48±519.98 | 1611.43±530.22 |
| PN infusion duration (hours) | 13.20±3.56 | 12.86±3.06 |
| Infusion rate mL/hour | 130.41±47.59 | 129.41±45.89 |
| Osmolarity (mOsm) | 1569.63±338.63 | 1613±356.48 |
| Osmolar infusion rate mOsm/hour | 124.83±47.59 | 131.39±41.42 |
| Dextrose infusion rate g/hour | 17.22±7.28 | 17.79±7.47 |
| Amino acid infusion rate g/hour | 6.55±2.20 | 6.79±2.55 |
| Lipid infusion rate g/hour | 2.69±1.37 | 2.65±1.20 |
Note. Descriptive statistics for continuous variables. Nutritional parameters and PN formulation characteristics in study patients during phases 2 and 3. Nutritional parameters are presented with all study patients and with removal of three outlier patients (see text). PN intakes are express as g/day, g/kg/day and infusion rate.
*p<0.05, **p<0.01, ***p<0.001.
BMI, body mass index; IBW, ideal body weight; PN, parenteral nutrition.
Table 4.
Characteristic of study group patients in the context of PN cost
| PN formulation cost | No and percentage of study group patients (n=30) |
| Decreased | 11 patients (36.7%) |
| Unchanged | 5 patients (16.6%) |
| Increased | 14 patients (46.7%) |
| Range | −26.22% to +76.28% |
| Overall impact | −1.31% |
Note. Differences noted in cost of study patient PN therapy between the observation (phase 2) and intervention (phase 3). Costs were reduced when excess nutrients (ie, thiamine, ascorbic acid and zinc) were shown to be unnecessary. Costs increased when micronutrients (ie, selenium, zinc and others) were deficient and required additional supplementation. Unprecedented, industry-wide price increases in PN components confounded the impact of MNST interventions intended to reduce PN costs.
MNST, multidisciplinary nutritional support team; PN, parenteral nutrition.
Table 5.
PN order changes in study patients during phase 3
| PN order changes | PN modifications in study group patients (n=30) | Total PN modifications |
| Macronutrients | 21 (70%) | 104 |
| Electrolytes | 15 (50%) | 173 |
| Micronutrients | 25 (83.3%) | 42 |
| Thiamine | 5 | |
| Ergocalciferol | 5 | |
| Ascorbic acid | 1 | |
| Cyanocobalamin | 1 | |
| Zinc | 10 | |
| Chromium | 5 | |
| Selenium | 5 | |
| Manganese | 6 | |
| Copper | 2 | |
| Volume | 17 (56.6%) | 33 |
| Infusion rate | 6 (20%) | 11 |
| Total | 27 | 373 |
Note. Macronutrient orders were changed either because of inadequate weight gain, liver enzyme elevations or excessive weight gain. Electrolytes and micronutrient orders were changed based on lab results.
PN, parenteral nutrition.
Table 6.
Recommendations and acceptances by treating physicians
| Measurement | Recommendations made to treating physicians (per patient, n=30) | Recommendation acceptance (per patient, n=30) |
| Range | 1–11 | 0–11 |
| Mean | 5.23±2.20 | 4.56±2.82 |
| Mean if PNE | 3.09±1.92 | 2.36±2.42 |
| Mean if not PNE | 5.86±1.89* | 5.28±2.22* |
| Total | 157 | 137 (87.2%) |
Note. Study patient interventions recommended to and accepted by treating physicians. The MNST made recommendations for compliance to standards of care for study patients at weekly case review meetings. The treating physicians had final authority to either accept or reject the recommendations. Recommendations were significantly lower if the treating physician was a nutrition expert. Recommendation acceptances were significantly higher if the treating physician was not a nutrition expert.
*p<0.05.
MNST, multidisciplinary nutritional support team; PNE, physician nutrition expert.
Patient weight, body mass index (BMI) and percentage of ideal body weight (%IBW) (table 3). Average weight increased slightly between phases 2 and 3. However, three patients were outliers which altered these results. One was non-compliant. Two were obese and sought to lose weight while on parenteral nutrition (PN). All other patients sought weight gain or weight stabilisation. After excluding data for the outliers, the study group had statistically significant increases in weight, BMI and %IBW (via Hamwi method). Weight increased 1.78 kg; t(df=26) = −3.88, p=0.0006. BMI increased 0.7 kg/m2; t(df=26) = −2.08, p=0.047. The % IBW increased by 3.66%; t(df=26) = −2.26, p=0.0009.
Basic PN laboratory results (Complete Blood Count, Complete Metabolic Profile, magnesium, phosphate, triglycerides). Basic blood tests were performed regularly. Twenty-one patents received PN lab work weekly. Two received lab work every 2 weeks. Seven received lab work monthly. The frequency of lab work orders was based on the stability of the patient, but also varied by PNE status. Five of 7 that received monthly PN labs were followed by a PNE.
Specialised lab results. Specialised lab data on micronutrient levels was obtained in 27 of 30 patients (90%). Micronutrient levels were obtained prior to phase 3 in 9 of 30 (30%). Seven of these patients were cared for by a PNE. During phase 3, an additional 18 patients had micronutrient levels obtained. Three patients did not have micronutrient levels obtained either prior to or during phase 3.
PN component costs and modifications (tables 4–5). The overall cost of PN components decreased by 1.31% during phase 3. Costs ranged from a decrease of 26.22% to an increase of 76.28%. Costs were reduced when excess nutrients were found to be unnecessary (ie, thiamine, ascorbic acid and zinc from initial discharge orders). Costs increased when additional micromineral supplementation was required. Unprecedented, industry-wide price increases in specific components confounded MNST interventions to reduce PN costs. Product availability and shortages also impacted cost. Macronutrient orders were changed in 21 of 30 patients (70%), either because of inadequate weight gain, liver enzyme elevations or excessive weight gain. Electrolytes and micronutrient orders were changed based on lab results.
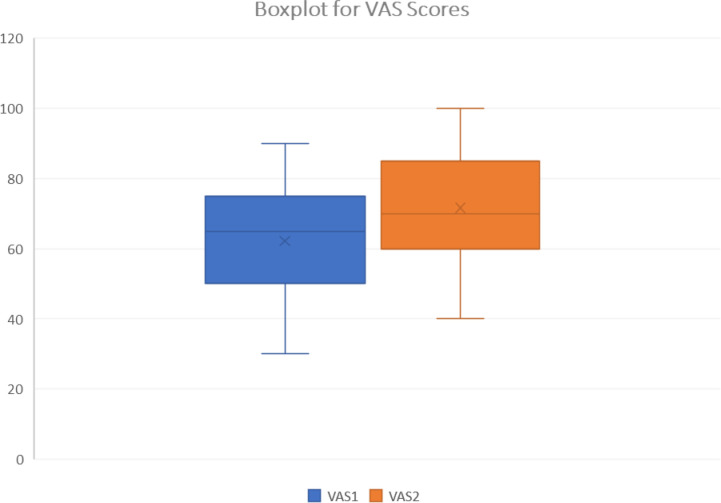
Patient QOL assessment (figure 2). The average EQ-5D-3L VAS score of overall health rose from 59.41 to 71.65 by the end of phase 3. This represents an increase of 12.24 points±10.0, or an improvement of 20.6% (t(df=28) = −4.10, p=0.0003).
Figure 2.
Boxplot of VAS scores. Boxplot representation of QOL EQ-5D 3L VAS scores before and after phase 3. EQ-5D 3L, Euroquol 5 Dimension-3 Level; QOL, quality of life; VAS, Visual Analog Scale.
Recommended interventions (table 6). The MNST made a total of 157 recommendations for compliance to standards of care in phase 3. Treating physicians had final authority to either accept or reject the recommendations. There were significantly fewer recommendations if the treating physician was a PNE (3.09±1.92 vs 5.86±1.89, p=0.0001). Recommendation acceptance was high (87.2%) but was significantly lower if the treating physician was a PNE (2.36±2.42 vs 5.28±2.22, p=0.0008). Impact on outcomes from non-accepted recommendations was not assessed.
Biochemical parameters. MNST recommendations resulted in improved electrolyte balance in 15 patients, improved liver function in 11 and reduced triglycerides in 3. Micronutrients were adjusted in 22 patients. Subsequent improvements were detected in zinc (10 patients), manganese (6), chromium (5), selenium (5) and copper (2) levels. Vitamin D was adjusted in five patients, thiamine in five, ascorbic acid in one and cyanocobalamin in one, with subsequent improvement of parameters.
Comparison between study patients and case-matched controls (tables 7–11).
Table 7.
Demographic characteristics of study patients and case-matched controls
| Characteristic | Study group (n=30) | Case-matched controls (n=30) |
| Male | 26.7% | 20% |
| Female | 73.3% | 80% |
| Age | 57.4±13.40 | 54.6±19.48 |
| Days on HPN therapy | 624.3±1084.27 | 589.76±1040.55 |
| CIRS Score | 17.4±3.81 | 16.5±3.82 |
| Federal payer | 56% | 73.33% |
| Prescriber PNE status | 36.6% | 23.3% |
| Prescriber non-PNE status | 63.4% | 73.33% |
Note. No significant demographic differences were identified between the groups.
CIRS, Cumulative Illness Rating Scale; HPN, home parenteral nutrition; PNE, physician nutrition expert.
Table 8.
Diagnostic categories of study patients and controls
| Primary diagnosis | Study group (n=30) | Case-matched controls (n=30) |
| Intestinal failure (IF) | 23 | 24 |
| Short bowel syndrome | 9 | 6 |
| Crohn’s disease-related intestinal failure | 4 | 4 |
| Complication of bariatric surgery | 3 | 2 |
| Gastroparesis | 3 | 4 |
| Chronic bowel obstruction | 2 | 6 |
| Coeliac disease | 1 | 1 |
| Colitis | 1 | 1 |
| Enteric fistula | 7 | 4 |
| Gastrointestinal cancers | 3 | 5 |
| Pancreatic cancer | 3 | 0 |
| Fallopian tube cancer | 1 | 1 |
Note. Principal diagnosis listed in the electronic medical record for study patients and case-matched controls. Most HPN patients in the study and case-matched control groups had IF as their reason for therapy (23). Intra-abdominal/pelvic cancer accounted for the remainder.
HPN, home parenteral nutrition.
Table 9.
Catheter characteristics of study patients and controls
| Catheter characteristics | Study group (n=30) | Case-Matched controls (n=30) |
| Type: | ||
| Infusion port | 11 | 9 |
| Tunnelled catheter | 10 | 5 |
| PICC | 6 | 16 |
| Groshong | 3 | 0 |
| Nursing care | ||
| Amerita | 25 | 7 |
| Home health agency nurses | 5 | 18 |
| Clinic staff | 0 | 5 |
| Dressings | ||
| Bio-occlusive | 21 | 29 |
| Hypoallergenic | 5 | 1 |
Note. Catheter type and care characteristics of study patients and case-matched controls. Most patients received catheter care on a weekly basis.
PICC, peripherally inserted central catheter.
Table 10.
PN order changes in study patients and controls
| PN order changes | Study group (n=30) | Case-matched controls (n=30) |
| Macronutrients | 104 | 73 |
| Electrolytes | 173 | 178 |
| Micronutrients | 42 | 12 |
| Volume | 33 | 24 |
| Infusion rate | 11 | 13 |
| Total PN order changes | 373 | 309 |
Note. PN orders for macronutrients were modified more often in study patients than in case-matched controls. Electrolytes, PN volume and duration were modified similarly among the study patients and case-matched controls. Micronutrients were modified in study patients more often than case-matched controls. The total number of PN formula changes were 20% higher in study patients than in case-matched controls.
PN, parenteral nutrition.
Table 11.
Adverse outcomes in study patients and controls
| Outcomes | Study group (n=30) | Case-matched controls (n=30) |
| Total adverse outcomes | 10 | 16 |
| Access device occlusion | 1 | 0 |
| Emergency room visits | 2 | 2 |
| Unplanned hospitalisation | 7 | 14 |
| PN-related hospitalisation | 3 | 3 |
| PN unrelated hospitalisation | 4 | 11 |
| Total hospital admissions | 11 | 20 |
| Single hospital admission | 3 | 8 |
| Double hospital admission | 4 | 5 |
| Triple hospital admission | 0 | 2 |
| Readmission rate | 0.13 | 0.23 |
| Hospitalisation rate per patient | 0.37 | 0.67 |
| Total hospital length of stay (LOS) days | 69 | 153 |
| Average LOS day | 6.27 | 7.65 |
Note. Study patients had fewer total adverse outcomes and unplanned hospitalisation than case-matched controls. Emergency department use was similar in both groups. Study group patients had a lower hospitalisation rate, readmission rate, total LOS and average LOS than case-matched controls.
PN, parenteral nutrition.
Patient characteristics (tables 7–8). Study patients and controls had similar demographics, comorbidity, payer mix, hospital referral source and PNE prescriber status.
Catheter Characteristics (table 9). Both groups had similar numbers of infusion ports. The study group had more tunnelled catheters (ie, Hickman, Broviac, Groshong catheters) whereas control patients had more peripherally inserted central catheter (PICC) lines. More study group patients were visited by Amerita staff nurses than by home health agency nurses. A similar number of patients in both groups had bio-occlusive catheter dressings.
PN order changes (table 10). PN formula changes were 20% more frequent among the study patients than controls. Macronutrients were modified 142.4% more often, micronutrients 350% more often and volume 137.5% more often in study patients than controls. Conversely, electrolytes were modified 97% as often and duration 84.6% as often in study patients than controls.
Adverse outcomes (table 11). There were 10 total outcomes reported among the phase 3 patients (0.33/patient), including seven unplanned hospitalisations. Three of the hospitalisations were therapy related. There were two ED visits among phase 3 study patients.
Phase 3 patients had fewer total adverse outcomes (3.64 vs 4.33 per 1000 therapy days), unplanned hospitalisations (2.54 vs 3.65 per 1000 therapy days) and access device events (0.338 vs 0.432 per 1000 therapy days) compared with phase 1b. ED use was higher in the study patients than phase 1b (0.338 vs 0.299 per 1000 therapy days).
There were 16 total adverse outcomes among the control patients (0.53/patient), with 14 unplanned hospitalisations. Three hospitalisations were therapy related. There were 2 ED visits among the control patients during the study period.
Total hospitalisations and length of stay (LOS). Seven study group patients were hospitalised 11 times during phase 3 (hospitalisation rate=0.37 admissions/patient). Three patients had only one hospitalisation, four had a second hospitalisation while none had a third. The readmission rate of study group patients was 0.13 (number of readmissions/number of patients). The total study group LOS was 69 days, average LOS (hospital days/number of hospitalisations) was 6.27 days.
Thirteen control group patients were hospitalised 20 times during the 90-day review (hospitalisation rate of 0.67). Eight had only one hospitalisation, five had a second hospitalisation and two had a third. The readmission rate of control group patients was 0.23. The total control group LOS was 153 days, average LOS was 7.65 days.
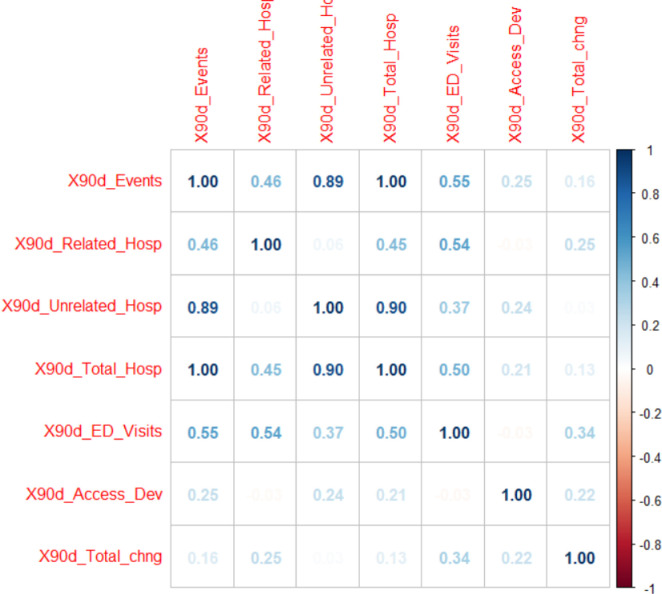
Statistical analysis of phase 3 study patients and controls (table 12). Comparison between the study and control group used a negative binomial regression model for modelling outcome variables. We used a negative binomial regression model to explain how this outcome is related with other possible predictors and to create a prediction model. Among the available count-data based predictors, 90-day related hospitalisations, 90-day access device events and 90-day total change were chosen as possible predictors because of their low correlation with 90-day events and with each other.
Table 12.
Results of modelling outcome variable, rate of adverse events per 90-day period, based on zero-inflated count data
| Estimate | SE | Z value | Pr(>|z|) | |
| (Intercept) | −5.12102 | 1.56044 | −3.282 | 0.00103** |
| Group | 1.26868 | 0.61553 | 2.061 | 0.03929* |
| CIRS Score | 0.15350 | 0.06872 | 2.234 | 0.02550* |
| X90d_Related_Hosp | 1.59514 | 0.48847 | 3.266 | 0.00109** |
| X90d_Access_Dev | 2.02450 | 1.40586 | 1.440 | 0.14986 |
| X90d_Total_chng | 0.02878 | 0.02795 | 1.030 | 0.30308 |
*p<0.05, **p<0.01.
CIRS, Cumulative Illness Rating Scale.
Figure 3 shows the Spearman correlation among these variables. In addition, we chose group (with control group as reference group), CIRS Score as other predictors. The results of negative binomial regression are displayed in table 5. Based on the results, group, CIRS score and 90-day hospitalisations, were significant predictors of 90-day (adverse) events at 5% alpha level. Specifically, rate of 90-day adverse events was significantly higher (3.56 times) for the control group than that for the study group, given all other predictors are in the model. Likewise, for a unit change in CIRS Score, the per cent change in expected incident rate of total 90-day events is by 16.6% (ie, exp(0.15350)–1), given all other predictors are in the model. For a unit change in 90-day unplanned hospitalisation—related to therapy (X90d_Related_Hosp), the per cent change in expected incident rate of total 90-day events is by 393% (ie, exp(1.59541)–1), given all other predictors are in the model.
Figure 3.
Correlation Plot. Correlation plot of Spearman correlation to show relationships of seven count variables in the data file (with only study and case–control group patients). X90d_Events = total 90-day adverse events, X90d_Related_Hosp = 90-day hospitalisations related to therapy, X90d_Unrelated_Hosp = 90-day hospitalisations unrelated to therapy, X90d_Total_Hosp = 90-day total number of hospitalisations, X90d_ED_Visits = 90-day emergency department visits, X90d_Access_Dev = 90-day access device complications. ED, emergency department.
Discussion
This study demonstrated that a PNE-led MNST could improve quality of care in long-term HPN. MNST interventions resulted in improved nutritional status, fewer adverse outcomes, hospitalisations, hospital LOS and better QOL.
MNST recommendations improved HPN through compliance to standards of care and attention to PN formula adaptation based on physical findings and biochemical parameters. PN macronutrient changes resulted in clinical improvement, measured by weight gain and BMI. Improved biochemical parameters were seen in electrolyte balance, liver function, micronutrient balance and triglyceride levels.
An important aspect of the QIP-PN study was the relationship of recommendations made and accepted by the treating physicians. The majority of HPN treating physicians were not nutrition specialists. The MNST made 157 recommendations for HPN management and 373 suggestions for formula changes during intervention. The vast majority (87.2%) of these were accepted by the treating physicians. Fewer recommendations were required if the patient’s physician was a PNE. PNEs were less willing to accept MNST recommendations.
The EQ-5D-3L QOL index was an important aspect of our study. Although other QOL indexes have been used in HPN, we found that the EQ-5D-3L was well suited because of its simplicity. The EQ-5D-3L was previously shown to be feasible and relevant for HPN patients.32 Other HPN QOL indexes employ up to 20 measured parameters compared with 5 for the EQ-5D-3L. In addition, we found that the VAS score provided an advantageous single point of reference for the patients overall perceived condition.
The study made use of a CIRS measure of multi-morbidity. To our knowledge this is the first real world application of the CIRS approach in the HPN population. CIRS scores documented the complexity of HPN patients with a moderately high value in both the study patients and controls.
Total hospitalisations and LOS
There were fewer hospitalisations in study patients versus controls. The average LOS was 1.38 days shorter and there were 84 fewer hospital days among study patients than controls. There were fewer hospital readmission in study patients. No study patient was readmitted more than twice, whereas two of the control patients were admitted three times. The reductions in hospitalisation, LOS and rehospitalisation could have a significant impact on overall cost for HPN care.
Adverse outcomes
Study patients had statistically significant differences in total outcomes and unplanned hospitalisations. CIRS Score and 90-day therapy-related hospitalisations were significant predictors of total outcomes at the 5% alpha level.
Limitations
Our study group was small (30 patients and 30 controls) and the duration of the intervention period was short (60–90 days). Considering these limitations, additional research should be performed with a larger number of patients and longer timeframes of monitoring to affirm our favourable results.
Furthermore, our results may have been biased by the differences between the study group and controls. Case-matched controls had a higher proportion of PICC lines and fewer surgically placed central lines than the study group (40% vs 80%). In addition, more of the case-matched controls were followed by agency nurses than Amerita staff (60% vs 16.6%). These differences may have contributed to the more favourable results observed in the study group.
Conclusion
This study demonstrated that a PNE-led, MNST produced measurable improvements in the care of long-term HPN patients. The MNST made numerous recommendations for HPN management, most of which were accepted by the treating physicians. MNST input improved patients’ self-assessed overall health, while reducing adverse outcomes, rehospitalisation and hospital LOS. If extended to the entire population of long-term HPN patients, we believe that MNSTs could have a significant impact on the quality and cost of HPN care.
Footnotes
Contributors: MR designed the study, served as principal investigator and is the author responsible for the overall content as the guarantor. MP reviewed the data and performed statistical analyses. RB collected data and participated on MNST weekly patient rounds and discussions. JH collected data and participated on MNST weekly patient rounds and discussions. FG participated on MNST weekly patient rounds and discussions and communicated recommendations to patients’ treating physicians. AT participated on MNST weekly patient rounds and discussions and communicated recommendations to patients’ treating physicians. DS participated on MNST weekly patient rounds and discussions and communicated recommendations to patients’ treating physicians. AD participated on MNST weekly patient rounds and discussions. MS participated on MNST weekly patient rounds and discussions. DR collected data for phase 1b of the study. VP served on the Study Oversight and Safety Committee. KS served on the Study Oversight and Safety Committee. NA served on the study oversight and safety committee.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: MR and MS are paid consultants for Amerita. RB, JH, FG, AT, DS, AD and DR are paid employees of Amerita. MP, VP, KS and NA have no conflicts.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available on reasonable request. Data are available in the form of multiple linked spreadsheets.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The protocol was granted Institutional Review Board (IRB) exemption under NIH guidelines (45CFR 46.104(d)(2)) by the Western IRB on 4 September 2019.
References
- 1. Winkler MF, Smith CE. The impact of long-term home parenteral nutrition on the patient and the family: achieving normalcy in life. J Infus Nurs 2015;38:290–300. 10.1097/NAN.0000000000000112 [DOI] [PubMed] [Google Scholar]
- 2. Mundi MS, Pattinson A, McMahon MT, et al. Prevalence of home parenteral and enteral nutrition in the United States. Nutr Clin Pract 2017;32:799–805. 10.1177/0884533617718472 [DOI] [PubMed] [Google Scholar]
- 3. Mullady DK, O'Keefe SJD. Treatment of intestinal failure: home parenteral nutrition. Nat Clin Pract Gastroenterol Hepatol 2006;3:492–504. 10.1038/ncpgasthep0580 [DOI] [PubMed] [Google Scholar]
- 4. Winkler MF, Smith CE. Clinical, social, and economic impacts of home parenteral nutrition dependence in short bowel syndrome. JPEN J Parenter Enteral Nutr 2014;38:32S–7. 10.1177/0148607113517717 [DOI] [PubMed] [Google Scholar]
- 5. Huisman-de Waal G, Schoonhoven L, Jansen J, et al. The impact of home parenteral nutrition on daily life-a review. Clin Nutr 2007;26:275–88. 10.1016/j.clnu.2006.10.002 [DOI] [PubMed] [Google Scholar]
- 6. Arhip L, Serrano-Moreno C, Romero I, et al. The economic costs of home parenteral nutrition: systematic review of partial and full economic evaluations. Clin Nutr 2021;40:339–49. 10.1016/j.clnu.2020.06.010 [DOI] [PubMed] [Google Scholar]
- 7. Maki DG, Kluger DM, Crnich CJ. The risk of bloodstream infection in adults with different intravascular devices: a systematic review of 200 published prospective studies. Mayo Clin Proc 2006;81:1159–71. 10.4065/81.9.1159 [DOI] [PubMed] [Google Scholar]
- 8. Buchman AL. Complications of long-term home total parenteral nutrition: their identification, prevention and treatment. Dig Dis Sci 2001;46:1–18. 10.1023/A:1005628121546 [DOI] [PubMed] [Google Scholar]
- 9. Compher CW, Kinosian BP, Evans-Stoner N, et al. Hyperhomocysteinemia is associated with venous thrombosis in patients with short bowel syndrome. JPEN J Parenter Enteral Nutr 2001;25:1–8. 10.1177/014860710102500101 [DOI] [PubMed] [Google Scholar]
- 10. Xu Z-W, Li Y-S. Pathogenesis and treatment of parenteral nutrition-associated liver disease. Hepatobiliary Pancreat Dis Int 2012;11:586–93. 10.1016/s1499-3872(12)60229-x [DOI] [PubMed] [Google Scholar]
- 11. Burden S, Hemstock M, Taylor M, et al. The impact of home parenteral nutrition on the burden of disease including morbidity, mortality and rate of hospitalisations. Clin Nutr ESPEN 2018;28:222–7. 10.1016/j.clnesp.2018.07.006 [DOI] [PubMed] [Google Scholar]
- 12. Winkler MF, Hagan E, Wetle T, et al. An exploration of quality of life and the experience of living with home parenteral nutrition. JPEN J Parenter Enteral Nutr 2010;34:395–407. 10.1177/0148607110362582 [DOI] [PubMed] [Google Scholar]
- 13. Baxter JP, Fayers PM, McKinlay AW. A review of the quality of life of adult patients treated with long-term parenteral nutrition. Clin Nutr 2006;25:543–53. 10.1016/j.clnu.2006.05.003 [DOI] [PubMed] [Google Scholar]
- 14. Winkler MF. Quality of life in adult home parenteral nutrition patients. JPEN J Parenter Enteral Nutr 2005;29:162–70. 10.1177/0148607105029003162 [DOI] [PubMed] [Google Scholar]
- 15. Wengler A, Micklewright A, Hébuterne X, et al. Monitoring of patients on home parenteral nutrition (HPN) in Europe: a questionnaire based study on monitoring practice in 42 centres. Clin Nutr 2006;25:693–700. 10.1016/j.clnu.2006.01.026 [DOI] [PubMed] [Google Scholar]
- 16. Pironi L, Steiger E, Brandt C, et al. Home parenteral nutrition provision modalities for chronic intestinal failure in adult patients: an international survey. Clin Nutr 2020;39:585–91. 10.1016/j.clnu.2019.03.010 [DOI] [PubMed] [Google Scholar]
- 17. Ritchey C. Is my patient non-compliant or do they have low literacy skills? A case report (2021), poster aAbstracts. J Parenter Enter Nutr;45:S44–240. 10.1002/jpen.2095 [DOI] [Google Scholar]
- 18. Kinnare K. Parenteral nutrition clinical interventions made by a home infusion nutrition support team (2021), poster a Abstracts. J Parenter Enter Nutr;45:S44–240. 10.1002/jpen.2095 [DOI] [Google Scholar]
- 19. Cuaresma J, et al. A multidisciplinary approach to reducing errors in total parenteral nutrition management (2021), poster aAbstracts. J Parenter Enter Nutr;45:S44–240. 10.1002/jpen.2095 [DOI] [Google Scholar]
- 20. Hurt RT, Steiger E. Early history of home parenteral nutrition: from hospital to home. Nutr Clin Pract 2018;33:598–613. 10.1002/ncp.10180 [DOI] [PubMed] [Google Scholar]
- 21. Accreditation Commission for Health Care . Accreditation standards -- DMEPOS and pharmacy [Accessed 02 Jan 2021].
- 22. Pironi L, Boeykens K, Bozzetti F, et al. ESPEN guideline on home parenteral nutrition. Clin Nutr 2020;39:1645–66. 10.1016/j.clnu.2020.03.005 [DOI] [PubMed] [Google Scholar]
- 23. Gillanders L, Angstmann K, Ball P, et al. AuSPEN clinical practice guideline for home parenteral nutrition patients in Australia and New Zealand. Nutrition 2008;24:998–1012. 10.1016/j.nut.2008.06.004 [DOI] [PubMed] [Google Scholar]
- 24. NICE guidelines . Nutrition support for adults: oral nutrition support, enteral tube feeding and parenteral nutrition, 2006. Available: https://www.nice.org.uk/guidance/cg32/chapter/1-Guidance#parenteral-nutrition-in-hospital-and-the-community [Accessed Aug 2017]. [PubMed]
- 25. Dreesen M, Foulon V, Vanhaecht K, et al. Guidelines recommendations on care of adult patients receiving home parenteral nutrition: a systematic review of global practices. Clin Nutr 2012;31:602–8. 10.1016/j.clnu.2012.02.013 [DOI] [PubMed] [Google Scholar]
- 26. Folwarski M, Kłęk S, Matras P, et al. Organizational issues of home parenteral nutrition during COVID-19 pandemic: results from multicenter, nationwide study. Nutrition 2021;86:111202. 10.1016/j.nut.2021.111202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Marshall JK, Gadowsky SL, Childs A, et al. Economic analysis of home vs hospital-based parenteral nutrition in Ontario, Canada. JPEN J Parenter Enteral Nutr 2005;29:266–9. 10.1177/0148607105029004266 [DOI] [PubMed] [Google Scholar]
- 28. Slye K, McKiernan M, Griffin A, et al. A comparison of a home parenteral nutrition service with the current European (ESPEN) guidelines on chronic intestinal failure in adults. Clin Nutr ESPEN 2022;50:289–306. 10.1016/j.clnesp.2022.04.029 [DOI] [PubMed] [Google Scholar]
- 29. van Hout B, Janssen MF, Feng Y-S, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 2012;15:708–15. 10.1016/j.jval.2012.02.008 [DOI] [PubMed] [Google Scholar]
- 30. Shaw JW, Johnson JA, Coons SJ. Us valuation of the EQ-5D health states: development and testing of the D1 valuation model. Med Care 2005;43:203–20. 10.1097/00005650-200503000-00003 [DOI] [PubMed] [Google Scholar]
- 31. Holst M, Ryttergaard L, Frandsen LS. Quality of life in HPN patients measured by EQ5D-3L including vas. J Clin Nutr Metab 2018;2. [Google Scholar]
- 32. Mulhern B, O'Gorman H, Rotherham N, et al. Comparing the measurement equivalence of EQ-5D-5L across different modes of administration. Health Qual Life Outcomes 2015;13:191. 10.1186/s12955-015-0382-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hudon C, Fortin M, Vanasse A. Cumulative illness rating scale was a reliable and valid index in a family practice context. J Clin Epidemiol 2005;58:603–8. 10.1016/j.jclinepi.2004.10.017 [DOI] [PubMed] [Google Scholar]
- 34. Nardi R, Scanelli G, Borioni D, et al. The assessment of complexity in internal medicine patients. The FADOI medicomplex study. Eur J Intern Med 2007;18:283–7. 10.1016/j.ejim.2006.12.006 [DOI] [PubMed] [Google Scholar]
- 35. Kittai AS, Gordon MJ, Mian A. Comorbidities predict inferior survival in patients receiving CAR T-cell therapy for relapsed/refractory DLBCL: a multicenter retrospective analysis. Transplant Cell Ther 2021;27:46–52. 10.1016/j.bbmt.2020.09.028 [DOI] [PubMed] [Google Scholar]
- 36. Ritt M, Ritt JI, Sieber CC, et al. Comparing the predictive accuracy of frailty, comorbidity, and disability for mortality: a 1-year follow-up in patients hospitalized in geriatric wards. Clin Interv Aging 2017;12:293–304. 10.2147/CIA.S124342 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available on reasonable request. Data are available in the form of multiple linked spreadsheets.