Abstract
The emergence of COVID-19 spurred the fastest development of a vaccine in history. Yet, a large proportion of Americans remain hesitant to receive it. Our paper investigates how the social networks we inhabit might explain persistent vaccine hesitancy. We argue that the COVID-19 vaccination status of respondents’ closest associates inhibits or motivates their decision to receive a COVID-19 vaccine. To test our argument, we conduct an original survey asking respondents a battery of questions about the people with whom individuals most frequently discuss vaccines and COVID-19. Our survey reports that individuals’ discussion networks are polarized by vaccination status. Concurrently, there is a strong association between the social network’s vaccination status and the respondent’s vaccination status. This association is so robust that partisanship does not moderate the association between discussants’ vaccination status and respondents’ vaccination status. Together, our results imply that unvaccinated individuals remain hesitant because they face reinforcing social pressure from their closest associates. The unique timing of our survey, during an unprecedented vaccination campaign against a novel disease, offers a snapshot of how relationships may affect attitudes.
Keywords: COVID-19, vaccine hesitancy, egocentric networks, political discussions, survey research
Introduction
On January 7, 2020, Chinese health officials reported the first known case of COVID-19. After record development speed, the United States administered its first COVID-19 vaccine on December 14, 2020. Yet, after an initial boom, vaccination rates stalled by July 2021. As of October 2022, only 68% of Americans received either the Johnson & Johnson vaccine or both doses of the Moderna and Pfizer vaccine and only a third have received a COVID-19 booster (The New York Times, 2020). Public health experts agree these numbers are extremely concerning (Trogen & Pirofski, 2021; Troiano & Nardi, 2021). Evidence shows that receiving a vaccine reduces deaths and hospitalization from COVID-19 (World Health Organization, 2021). Scientists warn that without mass vaccination, COVID-19 will burden healthcare systems, deaths will increase, and variants that pose a greater risk may be more likely to evolve. Yet, receiving a COVID-19 vaccine has been at the center of political debates since their inception. Our paper explores the factors explaining individuals’ decisions to receive a COVID-19 vaccine and what may continue to inhibit Americans willingness to receive it?
We utilize the unique situation of a rapidly developed vaccine to provide a snapshot of how an individual’s closest associates influence their decision to receive a COVID-19 vaccine. The role of social influence in political opinion and behavior is well established (Berelson, Paul et al., 1954; Huckfeldt & Sprague, 1987; Lupton & Thornton, 2017; McClurg, 2006), but the COVID-19 pandemic highlights the consequences and responsibility of interconnectedness. Not only do our interpersonal connections spread the virus but our connections can also encourage potentially lifesaving behaviors, like mask wearing and receiving a vaccine. We argue that mass inoculation does not simply take place on television or on front pages, but through the connections we hold with individuals in our immediate social circles. To support our argument, we examine the vaccination status among individuals’ core discussion networks to determine whether individuals live in “vaccine bubbles.” We then consider how the level of vaccine network homogeneity relates to individuals’ vaccine status. Our paper extends the literature on why individuals are hesitant to receive vaccines (Konstantinou et al. 2021) and previous literature on forces driving vaccination status during the COVID-19 pandemic (Fridman et al., 2021) by going by beyond the individual, politics, or political actors and focusing our paper on the core social networks that individuals trust in times of crisis to make decision. Additionally, we speak to issue polarization on COVID-19 vaccines and show that partisan polarization exists in attitudes and behaviors among individuals’ core social networks but is not exclusively charactered by partisanship.
In late July 2021, at the most critical point of vaccine administration in the United States, we conducted an original survey on a nationally representative sample of Americans. Our survey asks respondents to report their vaccination status and attitudes towards COVID-19 vaccines, along with those of their core social network – the group of friends, family and associates with whom they have discussions about COVID-19 vaccines. Using this novel data, we build an egocentric map of vaccination statuses and attitudes among a representative sample of Americans. Our data provides a window into the formation of attitudes and the relationship between individuals vaccination status and that of their core network.
Our data collection efforts uncovered novel insights about the interaction between individuals’ social networks and COVID-19 vaccines during a time when vaccination efforts were beginning to wane. First, we find that individuals’ discussion networks are polarized by vaccination status. Unvaccinated individuals have unvaccinated discussants, and vaccinated individuals have vaccinated discussants. Second, for each vaccinated person in a respondent’s social network the probability that the respondent is vaccinated increases. Finally, we find that partisanship does not moderate the effect of discussion networks on vaccination decisions, which suggests the force that respondents’ social networks exert might be strong enough to overcome partisanship’s influence on individuals’ vaccination decisions. Together, these results suggest that the vaccination status of an individual’s closest associates is highly associated with their decision to receive a COVID-19 vaccine. Consequently, these results are representative of network homophily that characterizes similar vaccine networks (Konstantinou et al. 2021). Importantly, while the data we present is the only one of its kind to be collected during this time, it cannot disentangle the causal effects of how social networks influence vaccination decisions. Our results simply suggest a remarkably strong association between vaccination status and what people hear from their closest friends. We hope scholars will use our paper as a useful starting place in pin down the precise mechanisms involved. Nevertheless, our results suggest that social bubbles may play an important role in ongoing resistance to vaccination.
This study contributes to research on social networks and vaccinations in at least three ways. First, we examine the relationship between social networks and COVID-19 vaccinations status. Previous studies examine HPV, H1N1, childhood immunization and seasonal flu vaccines (see Konstantinou et al., 2021 for an extensive list). However, these vaccines have been available for long periods of time and the relationship between close social networks and vaccination status has been well-studied. The COVID-19 pandemic provided a key opportunity for scholars to be able to see social networks and vaccines develop together in real time. All individuals had to make health decisions at the same time. In addition, the timing of the COVID-19 illness is different than other illnesses examined in previous studies. Vaccines went into quick production using a brand-new technology – unlike anything we have seen in the United States in recent years. Studies on COVID-19 vaccines tend to examine how individual characteristics are related to hesitancy and acceptance of the vaccine (Argote Tironi et al., 2021). Given the novelty of COVID-19 vaccines, scholars do not know if social contagion theory still applies to COVID-19, especially given the issue polarization associated with COVID-19 vaccines. This paper provides evidence that the effects of social contagion on vaccination attitudes can emerge rapidly when a novel vaccine is introduced.
Second, we use social networks to describe the mechanism underling the political polarization of COVID-19 vaccines. Contemporary studies illustrate a sharp divide between Democrats and Republicans in their likelihood of receiving a COVID-19 vaccine (Motta, 2021; Pink et al., 2021; Weisel, 2021). However, these studies are limited since they examine the effect of partisanship on vaccine hesitancy in isolation. We account, not only for respondents’ partisanship, but also how reinforcing pressures by co-partisans or vaccinated/unvaccinated peers influence the social context individuals face when deciding whether to get a vaccine. We argue that this context is a powerful motivator or inhibitor of vaccination status, not solely partisanship alone. Our paper broadens current literature that exclusively focuses on partisanship as a driver of vaccine hesitancy.
Third, our paper employs a reliable research design on a representative sample during a novel moment in American history. Past research on the spread of vaccines through social networks focus exclusively on a single social strata and examines how vaccine attitude proliferate through that social group (Edge et al., 2015, 2019; Fu et al., 2019). For example, Edge et al. (2015) and Edge et al., (2019) examines influenza vaccination uptake amongst medical students and doctors, respectively. However, influenza vaccines should be more likely to spread among medical students and doctors since their career path primes pro-vaccine beliefs.
Therefore, studies focusing exclusively on specific social groups are likely not representative of the U.S. population generally. Our study employs a nationally representative survey with a social network battery that captures egocentric attitudes about COVID-19 vaccines. By using established survey methodology (Butters & Hare, 2020; Huckfeldt & Sprague, 1995; Laumann, 1973) built to examine a representative sample, we can gain a broader picture of how social groups motivate COVID-19 vaccination among Americans generally. To our knowledge, our study is the only one to utilize an egocentric survey to examine issue polarization related to COVID-19 vaccines.
In total, our paper raises alarms about how social networks contribute to issue politization of COVID-19 vaccines and their impact of such polarization on public health. The rapid formation of networks that isolate individuals from vaccination pressures are likely to be a significant impediment to any future vaccination campaign.
Attitude Formation and Polarization in Social Networks
The literature suggests that social networks influence the attitudes and behaviors of their members (Christakis & Fowler., 2007; Edge et al., 2019). This influence can take place through several possible mechanisms: learning from members, social contagion, and relying on trusted close contacts. Learning from discussants occurs when individual gather enough information from their network to decide whether to get vaccinated. Alternatively, social contagion occurs when individuals encounter others who have already been vaccinated and they choose to do so as well. In other words, an individual need simply to perceive network behaviors and adjust their behavior in response. The latter can be understood as an information shortcut model while the former requires an explicit exchange of information. Finally, trusted contacts mean that individuals rely on specific people in their social network for information, not everyone. We argue that together, these mechanisms likely explain how social networks affect individuals’ decision to receive a COVID-19 vaccine and why these decisions may build polarized attitudes.
Linkages between social networks and behavioral outcomes through learning, in the form of information exchange, underlies much of the literature in political science. The key argument in these works is that networks offer opportunities to learn about politics via political talk that can influence opinions and behaviors. Lab experiments and observational studies agree that disagreement in social networks enhances tolerance and political participation (e.g., Mutz, 2006). More recent work suggests that individuals’ psychological traits also play a role in how individuals learn from their social networks. In fact, some individuals might increase their political activity when confronted with disagreeable friends, family, and close associates (Klar, 2014; Lyons et al., 2016), while others will not (Djupe et al., 2018). Scholars also suggest that the amount individuals learn from their social networks depends on socially supplied expertise (e.g., Ahn & Barry, 2015). This expertise is understood as information held by discussants and can be shared with an ego or discussant.
An alternative explanation suggests that attitudes and behaviors of individuals are contagious throughout a social network (Konstantinou et al., 2021). The relationship between social networks and vaccine uptake may constitute networks behaving as “clarifying cues” rather than in-depth learning opportunities. Research in political science suggests that this relationship may be the case for political behavior and participation. Sokhey &McClurg (2012) find that the role of networks in “correct voting” was more likely due to networks serving as a place where people could check their position in relation to others without having to exchange additional information in the traditional sense. Similarly, a simple cue indicating a potential discussant’s ideology has been shown to impact an individual’s willingness to communicate with that discussant for both political and non-political topics (Settle & Carlson, 2019).
In addition to social networks acting as cues, they may provide the pressure needed for socially desired outcomes. Gerber et al., 2008 shows that social pressure effectively encourages political participation. In that study, the threat of being out of step with the rest of one’s social circle counteracts one’s willingness to abstain from voting (Panagopoulos, 2010) takes this idea a step further by examining different types of social pressure which may motivate individuals to do the socially desirable activity: namely shame and pride. The author finds that shame is the most effective type of social pressure for motivating altruistic social behavior. Other authors suggest that these types of pressure and the prosocial behavior they illicit may be related to social proximity (Bicchieri et al., 2022). Thus, close social networks provide a space where social pressure, whether through shame or pride, can encourage or discourage those within that network to adhere to prosocial behavior. Research in health psychology has shown that behaviors related to health, such as taking a vaccine, are related to a variety of factors: perceived risk, what others think about the behavior, and how much the behavior is done by others (Bicchieri, 2016; Fishbein & Icek, 2011). These factors, which generally support social contagion theory, also relate to people’s social networks. Christakis and Fowler (2008) show that the likelihood of individuals quitting smoking increases with exposure to multiple contacts who also attempted to quit. The authors identify normative social pressure from others as one of the reasons respondents chose to quit themselves (see also Kuhlman et al., 2011). Using an experimental design, Centola (2011) present evidence that increasing similarity between online contacts is related to the use of an online dieting tool. Through this study, the author shows that network homophily was a significant predictor of the spread of health behaviors.1 Furthermore, Konstantinou et al., 2021 identify the effects of network homophily as a significant factor driving broad findings of the importance of social networks on vaccination uptake for past vaccination efforts. Taken together, these studies suggest that there is an important link between social networks, and health outcomes.
The literature suggests that individuals rely on a close group of friends, family, and associates to acquire information, formulate opinions, and make choices about political matters (Huckfeldt, Johnson, & Sprague, 2004; Sinclair, 2012).2 Therefore, not all members of a social network are equally influential in persuading their members' behavior. At the nexus of social networks and health-related behavior is research that suggests only relevant peers’ choices are informative for helping individuals judge a behavior’s credibility, feasibility, and social desirability (Christensen et al., 2004; Cialdini, 2007; Paluck et al., 2016). Li and Zhang (2015) find that close social networks – that is family, friends, and neighbors – are significant in promoting physical health behaviors. Thus, we argue that the behaviors and attitudes of individuals’ core social network (i.e., friends and family) with whom they discuss COVID-19 and vaccinations are important to their decision to receive a COVID-19 vaccine.Through learning, social contagion, and trusted allies, social networks may influence individuals' behavior at the individual level and may exert polarizing effects at the aggregate level (Butters & Hare, 2020). At the individual level, the literature finds that our core social networks provide a steady flow of information that can shape attitudes and behaviors (Berelson, Paul et al., 1954; Huckfeldt, Mendez, et al., 2004; Sokhey & McClurg, 2012). These networks provide a space where intimate exposure to cross-cutting political viewpoints may occur (Klofstad et al., 2013) but intimate social networks tend to be marked with political agreement (Mutz, 2006). At the aggregate level, individuals who have regular and selective exposure to homogeneous social networks on a given political topic harbor more passionate and narrow-minded preferences (Huckfeldt & Sprague, 1995; Knoke, 1990; McPherson et al., 2001). As homogeneous networks proliferate, clusters of networks with distinct and polarized attitudes have become more common (Butters & Hare, 2020). Scholarly attention to the effects of such political “echo chambers” tend to focus on trends in media consumption (Lelkes et al., 2017; Prior, 2007) and online social network segregation (Jiang et al., 2020) rather than voters' immediate political discussion networks. In this work, we anticipate that this type of polarization exists in individuals’ everyday discussions they have with their close friends and family about COVID-19 vaccinations.
H1
As overall attitudes towards COIVD-19 vaccines becomes more vaccine supportive in social network, the number of vaccinated discussants increases – leading to polarization in attitudes and vaccination status within a social network.
H2
As the number of vaccinated discussants in a respondent’s core social network increases, the likelihood that the respondent is vaccinated also increases.
We also test the effects of partisanship across levels of vaccination in social networks. Literature suggests that partisanship is the unmoved mover (Green et al., 2004), that individuals view issues through a perceptual screen (Campbell et al., 1960), and that partisanship can cloud an individual’s objective understanding of the world (Bartels, 2002; Gaines et al., 2007).
From this literature we expect partisanship to drive people’s attitudes on issues surrounding pandemic. Recent literature on Democrats and Republicans’ attitudes shows partisans are divided on pandemic-related issues. Particularly, scholars find that Democrats are more likely to adopt COVID-19 precautions than Independents or Republicans, such as social distancing measures (Gollwitzer et al., 2020; Roberts & Utych, 2021), masking wearing (Kahane, 2021; Shin et al., 2022), and receiving a vaccine (Albrecht, 2022; Galston, 2021; Jones & McDermott, 2022). Therefore, we expect Democrats to have a higher vaccination rate than Independents and Republicans in our study examining what drives individual’s vaccination status.
However, if our theory is correct and those with whom respondents discuss vaccines and politics shape individuals’ attitudes about vaccination, then we expect that as the number of vaccinated discussants in a respondent’s social network increases, so should the likelihood that the respondents is vaccinated as well – irrespective of their partisanship.
We ask to what extent does partisanship moderate the effect of respondent’s discussion network on their propensity to receive a COVID-19 vaccine. On the one hand, partisanship literature suggests that party identification exerts a strong force, pushing respondents closer to their respective party’s positions on vaccination (Druckman et al., 2013). On the other hand, social contagion theory suggests that the respondent is more likely to be vaccinated if individuals in the respondent’s social network are also vaccinated, irrespective of partisanship (Konstantinou et al., 2021).
H3
Partisanship will not moderate the association between discussants’ vaccination status and respondents’ vaccination status.
Methodology
To examine the effect that social networks have on individuals’ propensity to receive a COVID-19 vaccine and to what extent attitudes within them are polarized, we conducted an original nationally representative survey through Lucid over two waves in July and August of 2021.3
Our survey’s timing allows us to collect unique data about our question. Since it was administered during a tipping between vaccine supportive individuals (those who had received a vaccine before July 2021) and vaccine resistant individuals (those unwilling to receive a vaccine before July 2021), our data includes useful variation in the vaccination status of individuals and of their closest associates. This variation provides important statistical leverage that surveys too early or too late in the year would lack.
Together, both waves yield more than 2560 high quality respondents.4 The median survey completion time was 13 minutes. The study was approved by the institutional review board at University of California, Davis; all subjects provided written and informed consent.
To build our egocentric discussion network, we ask respondents to provide the first name of three individuals (called discussants) with whom they “discuss COVID-19, vaccines, and politics.” Our questions define the context of respondents’ interactions with their closest discussants by asking individuals about their perception of their discussants’ vaccine-related behavior.5
Health and political communication networks use egocentric design regularly (Berelson, Lazarsfeld et al., 1954; Butters & Hare, 2020; Huckfeldt & Sprague, 1987; Lupton & Thornton, 2017; McClurg, 2006) and it appears in nationally representative surveys such as the ANES and CCES.6 Though this design censors respondents who might list more than three people (Eveland et al., 2013), (Marsden, 2004) finds that name generating procedures lets respondents report discussants with whom they have the closest ties and who may be the most influential in their network. Scholars find that while individuals may report a large network (Lupton & Thornton, 2017), the inner circle of people they rely on for support tends to be smaller (Dunbar & Spoors, 1995; Hill & Dunbar, 2003). In addition, in recent studies, name generators have also been shown to capture an individual’s discussion network, “quite well” (Djupe & Sokhey, 2014). Therefore, the literature suggests that our egocentric networks are a subset of a larger network but an important and influential subset at that.
We find that respondents are generous in naming discussants in their social networks. Our survey reports that 92.9% of respondents provides three names, 3.8% provides only two names, and 3.3% provide only one name. After respondents provide a name, we ask about the respondent’s and their social network’s vaccination status and attitudes about COVID-19 vaccines.
Our key independent variable is the number of discussants in respondents’ social network who received a COVID-19 vaccine.7 In our survey, respondents report the vaccination status of each discussant. We derive our measure by counting the number of vaccinated discussants in respondents’ discussion network. Our independent variable ranges from 0 to three discussants. 0 (3) means that no (all) discussants in respondents’ social network received a COVID-19 vaccine.
Figure 1 illustrates the distribution of the number of people in respondents’ self-reported social network who are vaccinated. We find that a plurality of respondents are members of a completely vaccinated network (i.e., three vaccinated discussants). However, a majority of respondents report being members of a network with at least one unvaccinated discussant.
Figure 1.
Distribution of vaccination status in respondents’ social network.
Our key dependent variable is whether the respondent received a COVID-19 vaccine.8 We create this variable by asking for respondents’ self-reported COVID-19 vaccination status.9 At the time of survey (July and August 2021), 63.8 (70.4) percent of respondents in wave 1 (wave 2) report receiving a COVID-19 vaccine. Between wave 1 and 2, our sample reports a 6.6% increase in vaccinated Americans. Given the marginal increase in vaccinations during our sample, our survey reports a unique cross-section of the pandemic as a transition between widespread willingness to receive a vaccination to widespread appeals to convince people to receive a vaccination.
We employ a linear probability model to assess the relationship between the vaccination rate in respondents’ social network and their propensity to receive a COVID-19 vaccine.10 The additive term, Number of Vaccinated Discussants in Respondent’s Social Network, represents our key independent variable. The variable Xi represents our model’s control variables. We control for the average vaccine support in the respondent’s social network, network sophistication, network size, demographic information about the respondent: education level, age, gender, and ethnicity.11 We also control for political variables, such as their three-point party identification and their political ideology. We include county fixed effects to control for fixed observed and unobserved heterogeneity across counties σc. Lastly, we include a wave fixed effect variable to control for fixed observed and unobserved heterogeneity between survey times.12
Social Network Results
We begin by examining the distribution of discussants’ attitudes towards COVID-19 vaccines across the number of vaccinated discussants: zero, one, two, or three. Figure 2 reports an association that suggests that as discussants’ attitudes towards COVID-19 vaccines become more supportive as the number of vaccinated discussants in respondents social network increases.
Figure 2.
Distribution of attitudes towards vaccination in social network.
In the survey, we asked respondents to rate each discussants’ attitude towards COVID-19 vaccines on a 11-point scale from high vaccine resistance to high vaccine support. Then, we take the average attitude across discussants in each respondents’ network and bin these averages into five groups. We find that social networks with zero (three) vaccinated individuals are more likely to display vaccine resistant (supportive) attitudes. 52% of respondents with no vaccinated discussants report highly resistant vaccine attitudes, compared with 0% of respondents with all vaccinated discussants. Contrastingly, 76% of respondents with all vaccinated discussants report highly supportive vaccine attitudes, compared with only 5% of respondents with no vaccinated discussants. Concurrently, we find that supportive attitudes toward the vaccine increase as the number of vaccinated discussants increases. This result suggests polarization in attitudes towards COVID-19 vaccines across the number of vaccinated discussants.
Figure 3 reports that vaccinated (unvaccinated) individuals tend to exist in social networks with other vaccinated (unvaccinated) individuals. It illustrates respondents’ COVID-19 vaccination status (vaccinated/unvaccinated) and the number of discussants inside their core social network who received a COVID-19 vaccine. It shows that 57% of vaccinated respondents report three discussants in their immediate network are also vaccinated, 46% of unvaccinated respondents report zero vaccinated discussants, and even fewer respondents reporting discussants with a vaccination status different from their own. The figure suggests (1) vaccinated and unvaccinated individuals are less likely to discuss COVID-19 vaccines when compared to members with the same vaccination status and (2) that discussants’ vaccination status is closely associated with respondents’ vaccination status.
Figure 3.
Distribution of vaccination in respondents’ social network conditional on respondents’ vaccination status.
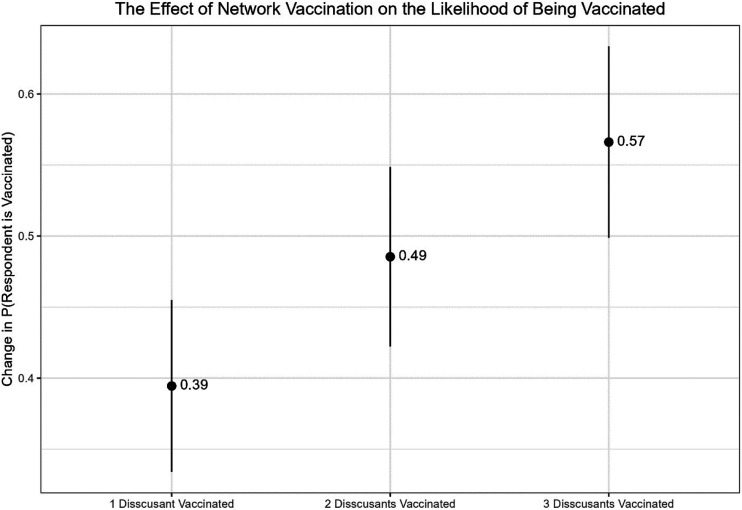
Figure 4 shows a strong relationship between the number of vaccinated discussants and respondents’ vaccination status. It illustrates the results of our key model of interests, fixed effects model. The model reports a positive and significant (p < .05) association between the number of discussants in the respondent’s social network who are vaccinated and the probability that the respondent is vaccinated. Compared to the base category, individuals in a network with zero vaccinated discussants, the model reports that one, two, and three vaccinated discussants increase the probability that the respondent is vaccinated by 39, 49 and 57%, respectively. The results suggest that vaccine discussion networks may be influential in individuals’ decisions to get a COVID-19 vaccination.13
Figure 4.
The effect of network vaccination on the likelihood of being vaccinated.
Taken together, our results provide clues as to why those who are unvaccinated remain hesitant: they face reinforcing social pressure from their closest associates. We cannot say for certain that social networks cause individuals to receive or refuse vaccination, but these results do establish a remarkably strong association between individuals’ network composition and vaccination status. More rigorous testing is needed to pin down the precise mechanisms involved, but our results are highly suggestive that social bubbles play an important role in ongoing vaccine hesitancy.
Despite our best efforts to control for potential confounding variables the threat of omitted variable bias remains. As a robustness check, we conduct a sensitivity analysis that measures the strength of a confounder necessary to decrease the size of our estimates to a range where they would not be statistically significant (Cinelli & Chad, 2020). The sensitivity analysis suggests that a confounder three times as strong as the respondent’s own vaccine hesitancy coefficient would not be strong enough to overturn the significance of any factor level in our social network coefficient. The results imply that our social network coefficient is robust against observed and unobserved confounders. We report these results in the Appendix Figure 5(A)
Partisanship Results
To test our competing partisanship hypothesis, we pool data from wave one and two of our study and employ a linear probability model. We interact respondents’ three-point party identification with the number of vaccinated discussants in respondents’ social network.14 We control for ideology on a 7-point scale, respondents’ education, household income, age, gender, ethnicity, and wave fixed effects. We report the results of the control model.15 If partisanship is the main mover, we expect that it should moderate the effect of discussants’ vaccination status on respondent’s vaccination status. However, if discussants’ vaccination status moves respondent’s vaccination status, then partisanship should be inconsequential in its ability to determine vaccination status.
We find that partisanship does not moderate the association between discussants’ vaccination status and respondents’ vaccination status. The results in Figure 5 suggest that the number of vaccinated discussants in respondents’ social network has a positive and significant effect on respondents’ propensity to receive a COVID-19 vaccine, despite the respondent’s partisanship. As the number of vaccinated discussants in respondents’ network increases, the respondent’s propensity to receive a COVID-19 vaccine increases as well – irrespective of the respondent’s party identification. These results imply that knowing other vaccinated individuals may overcome initial partisan tendencies associated with being vaccine avoidant and illustrates a more complex story that involves the discussions of social networks in determining vaccination status, not merely party alone.
Figure 5.
Predicted probabilities of partisanship and network vaccination on the likelihood of being vaccinated.
As the figure illustrates, Republicans and Democrats with zero vaccinated individuals in their discussion network have a 17% and 30% chance of receiving a vaccine.
However, when Republicans and Democrats know three vaccinated individuals in their discussion network both have an 88% chance of receiving a vaccine. Moving between zero and three vaccinated individuals, Republicans and Democrats experience a 71 and a 58% increase in the likelihood of being vaccinated, respectively.
Therefore, the effect of the number of vaccinated discussants on receiving a vaccine works equally well in motivating or inhibiting vaccination across partisanship. These results are particularly compelling for Republicans, whose lower initial likelihood of receiving a vaccine compared to Democrats when they report zero vaccinated respondents, is virtually negated when compared to Democrats when both sets of partisans report three vaccinated discussants.
Our findings lead to several conclusions about partisanship’s role in vaccination decisions. First, partisanship does not moderate the effect of discussion networks on vaccination decisions. Second, partisanship does not exclusively explain the respondent’s vaccination status as past literature might suggest. Third, issue polarization on decisions to receive a COVID-19 vaccine are not exclusively split along partisan lines. Instead, vaccination statuses in respondents’ social networks explain issue polarization on vaccination decisions better than partisanship. Finally, the force that respondents’ social networks exert might be strong enough to overcome the perceptual screen that partisanship confers on vaccination decisions.
Discussion
Our paper examines how individuals discuss COVID-19 vaccines to understand persistent vaccine hesitancy in the United States. The unique timing of our survey provides data on the development of attitudes surrounding a novel vaccine rapidly developed for a relatively new disease. Understanding what drives decisions to receive a COVID-19 vaccine is instrumental in navigating the current and future public health crises.
We examine vaccinated and unvaccinated individuals’ egocentric networks using an original survey. We find that vaccination networks are grounded in homophily, where unvaccinated and vaccinated individuals cluster together and hold polarizing attitudes about vaccines. Further, we provide evidence that the density of such vaccinations in individuals’ social networks is highly predictive of their vaccination status. As a byproduct, we anticipate that the influence of individuals’ closest associates may contribute to polarization in attitudes toward COVID-19 vaccines. Finally, we provide evidence that discussants’ vaccination status is associated with increasing vaccination rates, irrespective of the respondent’s party affiliation. Together, these findings suggest that social pressure may encourage an individual to receive a COVID-19 vaccine.
These findings contribute to our understanding of health and vaccine networks (Konstantinou et al., 2021). Our study provides another layer of evidence suggesting that the flow of information in one’s close social network helps to shape attitudes and behaviors (Berelson, Lazarsfeld et al., 1954; Huckfeldt & Sprague, 1995; Mutz, 2006). We also shed light on how issue polarization contributes to mass level political polarization (Abramowitz & Saunders, 2008; Fiorina & Abrams, 2008). Indeed, political polarization has become part of our everyday social lives (Butters & Hare, 2020), including in response to the pandemic (Allcott et al., 2020; Kerr et al., 2021). As we have shown, issue polarization on COVID-19 vaccines exists in attitudes and behaviors among individuals’ core social networks but is not exclusively charactered by partisanship.
Despite our rigorous and robust efforts, our study is not without its limits. First, the analysis we present in this paper does not establish causality. Given the cross-sectional nature of our data, we cannot say with certainty that the network’s vaccination status caused respondents to receive a COVID-19 vaccine. However, we can say that our paper uncovers an important association. This association suggests that networks may play a role in determining vaccination status. Further, it also shows that during the heart of a pandemic, with a novel disease, and an unprecedented vaccination campaign, individuals are not making vaccination decisions in isolation but instead, their decision may be the sum-total of their own perceptions and their perceptions of their networks’ behavior.
Second, we concede that we cannot determine the causal direction of our finding. Individuals with pre-existing vaccine-supportive attitudes may cluster with like-minded individuals, or their social network may influence their decision to receive a COVID-19 vaccine. Concurrently, this paper also does not pin down how social networks influence vaccination status. However, we find correlational evidence that the amount of encouragement a respondent receives predicts their decision to receive or forgo a COVID-19 vaccine. Figure 6 reports that the more discussants who encourage or discourage vaccination, the more likely the respondent is to receive or forgo a COVID-19 vaccine, respectively. This figure offers correlational evidence that networks attempt to influence their members’ behavior and that network encouragement may be a potential mechanism driving vaccination decisions.16 We encourage future scholars to examine this mechanism further.
Figure 6.
Distribution of encouragement and respondents vaccination status.
Instead, our paper narrows in on an important association: the actions of an individual’s social network is correlated with the individual’s behavior. Parallel with network studies on obesity (Christakis & Fowler. 2007) and HIV (Cortopassi et al., 2019), we provide suggestive evidence that the likelihood of receiving a COVID-19 vaccine may depend on the composition of an individual’s social network and whether their social network is vaccinated. The correlation we find extends to the most dramatic public health crisis of a generation and to the important lifesaving actions to redress it. While we do not provide causal evidence, our study shows future research designed to demonstrate causal relationships is likely to be promising. Further work should deploy a causal inference design that can demonstrate the link we show is likely to exist.
Despite any limit to our study, our findings have implications for the future of the COVID-19 pandemic. First, we expect COVID-19 outbreaks will be concentrated among unvaccinated individuals and spread quickly through their unvaccinated social networks. Since variants of concerns will be more transmissible than the initial strain, and unvaccinated social networks are densely populated, areas with large numbers of unvaccinated individuals should expect a significant increase in caseload and hospitalization.
Second, we expect slow vaccination uptake among remaining unvaccinated individuals, given that unvaccinated social networks are insulated from vaccinated ones and the social pressure to receive a COVID-19 vaccine. Our findings suggest that social pressure may be a key factor in the decision to receive (not receive) a COVID-19 vaccine. So long as unvaccinated individuals remain insulated, the social pressure to forgo vaccination will be strong.
Third, policymakers and healthcare officials should allocate resources and target unvaccinated clusters. Our research suggests that even if one person in the respondent’s social network is vaccinated, the probability the respondent received a COVID-19 vaccine is significant and positive, relative to zero vaccinated respondents. Efforts to target unvaccinated individuals may have spillover effects, such as encouraging the rest of their social network to receive a COVID-19 vaccine as well.
Finally, new updates to COVID-19 vaccines or attempts to make vaccination a yearly event like the flu shot might only be as successful as the pressure and follow-through an individual receives from their social network.
Supplemental Material
Supplemental Material for Polarization in COVID-19 Vaccine Discussion Networks by Sharif Amlani, Spencer Kiesel, and Ross Butters in American Politics Research
Acknowledgements
We are very grateful to the journal editor and anonymous reviewers for their thorough reading and helpful suggestions. We thank and appreciate the support and suggestions given by Chris Hare and Lauren Peritz throughout our work on this project.
Author Biographies
Sharif Amlani is a Ph.D. candidate at the University of California, Davis. His research interests focus on advancing public policy in American politics, including examining the relationship between campaign finance activity and legislative behavior. His research has been published in Political Behavior, Electoral Studies, and Election Law Journal.
Spencer Kiesel is a PhD candidate at UC Davis whose research focuses on the representation of nonreligious persons in the US. He also works on political polarization and vaccine hesitancy utilizing an array of methodological tools including experimental design, conjoint analysis, machine learning modeling (MLE, GLM, etc.), coding in R and Stata, and data visualization.
Ross Butters is an Adjunct Assistant Professor at the University of California Center Sacramento. His research focuses on the impact of social factors on individual political attitudes and behavior. Specifically, he is interested in understanding how the composition of political communication networks, and the information therein, influences political attitudes and participation of individuals.
Notes
Homophily is defined as “the tendency of individuals to associate with others who share similar traits” (Smirnov & Thurner, 2017)
Core social networks are developed from an individual’s larger environmental context. These networks are where informal interactions and conversations with close associates, such as family, friends, and coworkers, occurs. These networks allow for more frequent interactions on a wider range of topics than would be possible with mere acquaintances (Hays, 1989).
Because of concerns over Lucid’s respondent pool we include multiple attention check questions (Aronow et al., 2020). We include a cut question that filters out respondents who fail the attention check question. We use attention check questions from (Aronow et al., 2020). In addition, we eliminate speeders from our sample.
High quality refers to respondents who passed three attention check questions, passed speeding checks, and who were in the lower 95% of individuals with missing answers.
Some suggest that artificially limiting a political name generator may impact the number or type of contacts a respondent reports. However, Eveland et al. (2018) suggest that doing so, “did not prohibit the majority of respondents from reporting as many alters as they were willing.” (p. 194). Indeed, the majority of respondents reported in that work were not able to name the full number of names available to them.
See the 2000 ANES and 2016 CCES, among other similar, but not exactly matching data collection tools.
Instead of the number of individuals, scholars may be more interested in the proportion of a respondent’s social network that are vaccinated. The correlation between the number and the proportion is greater than >.95. In addition, the advantage to using the number is we can omit the special scale where 50% of an individual’s social network is vaccinated. This special case occurs when an individual lists two people but only 1 is vaccinated. This occurs in our dataset but is rare. It leads to a sparse cell problem leading to incorrect inferences for these cases. For interested scholars, we include a model using the proportion in the appendix Table 2A the results are the same.
The wordings to each of these questions can be found in the appendix.
We define vaccination as whether a respondent has received at least 1 dose of an available COVID-19 vaccine.
While using a linear probability model to access the propensity to receive a vaccine does not follow the traditional methodological procedure for a binary dependent variable (i.e., using a logistic regression), Figure 1(a) in the appendix illustrates the functional form of the relationship between the number of people who are vaccinated in the respondent’s network and the propensity of receiving a COVID-19 vaccine. The figure includes a LOESS line that is more linear than logistic. Thus, a linear model better captures the functional form of the relationship between our key independent and dependent variables. We include estimates using a logistic regression in appendix Table 1A as a robustness check – the results are the same.
Average vaccine support is measured by asking respondents to rate each discussants’ attitudes towards COVID-19 vaccines on an eleven-point scale ranging from vaccine resistant to vaccine supportive with vaccine hesitant as the median response. Then, we take the average level of support across each respondent’s discussants and call it the respondents’ average vaccine support in their social network. Network sophistication is measured by averaging respondents’ perception of how much each of discussant knows about COVID-19 vaccines on a three-point scale (from not much at all to a great deal). Network size is measured as the number of discussants the respondents report.
In addition to these controls, the appendix includes models exclusive to wave two that controls for respondents’ vaccine hesitancy, generated from a scale using questions from the World Health Organization (2013), and we control for the respondents’ political knowledge, generated from our own scale. The vaccine hesitancy scale and the political knowledge scale have a Cronbach alpha of 0.85 and 0.71, respectively.
In the Appendix, we include the full table for the wave 1 and 2 fixed effects model. Additionally, we include a base model, a model including only the control variables, and models exclusive to wave 2 that control for political knowledge and vaccinate hesitancy as control variables.
We code independent leaners (both Democrats and Republicans) into their respective parties.
We include a base, control and the full model specification for the fixed effects model in Appendix Table 5A.
In Appendix Figure 8(a) – 12(a) and Appendix Tables 6A – 9A, we offer additional correlational evidence reporting an association between network encouragement and their members behavior on COVID-19 vaccines.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Replcation material: https://doi.org/10.7910/DVN/ECT4DL
Supplemental Material: Supplemental material for this article is available online.
ORCID iD
Spencer Kiesel https://orcid.org/0000-0003-1722-4409
References
- Abramowitz A. I., Saunders K. L. (2008). Is polarization a myth? The Journal of Politics, 70(2), 542–555. [Google Scholar]
- Ahn T. K., Barry J. R. (2015). The overvaluing of expertise in discussion partner choice. Journal of Tropical Pediatrics, 27(3), 380–400. 10.1177/0951629814531672 [DOI] [Google Scholar]
- Albrecht D. (2022). Vaccination, politics and COVID-19 impacts. BMC Public Health, 22(1), 1–12. 10.1186/s12889-021-12432-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allcott H., Boxell L., Conway J., Gentzkow M., Thaler M., Yang D. (2020). Polarization and public health: Partisan differences in social distancing during the coronavirus pandemic. Journal of Public Economics, 191, 104254. 10.1016/j.jpubeco.2020.104254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Argote Tironi Pa., Barham E., Zuckerman Daly S., Gerez J. E., Marshall J., Pocasangre O., Pocasangre O. (2021). Messages that increase COVID-19 vaccine acceptance: Evidence from online experiments in six Latin American countries. Plos One, 16(10), Article e0259059. 10.1371/journal.pone.0259059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aronow P. M., Kalla J., Orr L., Ternovski J. (2020). Evidence of rising rates of inattentiveness on Lucid in 2020. Preprint. SocArXiv. 10.31235/osf.io/8sbe4. [DOI] [Google Scholar]
- Bartels L. M. (2002). Beyond the running tally: Partisan bias in political perceptions. Political Behavior, 24(2), 117–150. 10.1023/A:1021226224601 [DOI] [Google Scholar]
- Berelson B. R., Lazarsfeld P. F., McPhee W. N. (1954. a). Voting: A study of opinion formation in a presidential campaign. University of Chicago Press. [Google Scholar]
- Berelson B., Paul L., Mcphee W. (1954. b). Democratic practice and democratic theory. In Bachrach P. (Ed), Political elites in a democracy (pp. 27–48). Routledge. [Google Scholar]
- Bicchieri C. (2016). Norms in the wild: How to diagnose, measure, and change social norms. Oxford University Press. [Google Scholar]
- Bicchieri C., Dimant E., Gächter S., Nosenzo D. (2022). Social proximity and the erosion of norm compliance. Games and Economic Behavior, 132, 59–72. 10.1016/j.geb.2021.11.012. [DOI] [Google Scholar]
- Butters R., Hare C. (2020). Polarized networks? New evidence on American voters’ political discussion networks. Political Behavior, 44(3), 1079–1103. 10.1007/s11109-020-09647-w [DOI] [Google Scholar]
- Campbell A., University of Michigan Survey Research Center. Converse P. E., Miller W. E., Stokes D. E. (1960). The American voter. University of Chicago Press. [Google Scholar]
- Centola D. (2011). An experimental study of homophily in the adoption of health behavior. Science, 334(6060), 1269–1272. 10.1126/science.1207055 [DOI] [PubMed] [Google Scholar]
- Christakis N. A., Fowler J. H. (2007). The spread of obesity in a large social network over 32 years. New England Journal of Medicine, 357(4), 370–379. 10.1056/NEJMsa066082 [DOI] [PubMed] [Google Scholar]
- Christakis N. A., Fowler J. H. (2008). The collective dynamics of smoking in a large social network. New England Journal of Medicine, 358(21), 2249–2258. 10.1056/NEJMsa0706154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen P. N., Rothgerber H., Wood W., Matz D. C. (2004). Social norms and identity relevance: A motivational approach to normative behavior. Personality & Social Psychology Bulletin, 30(10), 1295–1309. 10.1177/0146167204264480 [DOI] [PubMed] [Google Scholar]
- Cialdini R. B. (2007). Descriptive social norms as underappreciated sources of social control. Psychometrika, 72(2), 263–268. 10.1007/s11336-006-1560-6 [DOI] [Google Scholar]
- Cinelli Carlos, Chad Hazlett. (2020). Making Sense of Sensitivity: Extending Omitted Variable Bias. Journal of the Royal Statistical Society: Series B (Statistical Methodology), 82(1), 39–67. 10.1111/rssb.12348. [DOI] [Google Scholar]
- Cortopassi A. C., Driver R, Eaton L. A., Kalichman S. C., Kalichman S. C. (2019). A new era of HIV risk: It’s not what you know, it’s who you know (and how infectious). Annual Review of Psychology, 70(1), 673–701. 10.1146/annurev-psych-010418-102927 [DOI] [PubMed] [Google Scholar]
- Djupe P., Scott M., Edward Sokhey A. (2018). The political consequences of gender in social networks. British Journal of Political Science, 48(3), 637–658. 10.1017/S0007123416000156 [DOI] [Google Scholar]
- Djupe P. A., Sokhey A. E. (2014). The distribution and determinants of socially supplied political expertise. American Politics Research, 42(2), 199–225. 10.1177/1532673x13486924 [DOI] [Google Scholar]
- Druckman J. N., Peterson E., Slothuus R. (2013). How elite partisan polarization affects public opinion formation. American Political Science Review, 107(1), 57–79. 10.1017/S0003055412000500 [DOI] [Google Scholar]
- Dunbar R., Spoors M. (1995). Social networks, support cliques, and kinship. Human Nature (Hawthorne, N.Y.), 6(3), 273–290. 10.1007/BF02734142 [DOI] [PubMed] [Google Scholar]
- Edge R., Heath J., Rowlingson B., Keegan T. J., Isba R. (2015). Seasonal influenza vaccination amongst medical students: A social network analysis based on a cross-sectional study” edited by N. Masuda. Plos One, 10(10), Article e0140085. 10.1371/journal.pone.0140085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edge R., Keegan T., Isba R., Peter D. (2019). Observational study to assess the effects of social networks on the seasonal influenza vaccine uptake by early career doctors. BMJ Open, 9(8), Article e026997. 10.1136/bmjopen-2018-026997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eveland W. P., Hutchens M. J., Morey A. C. (2013). Political network size and its antecedents and consequences. Political Communication, 30(3), 371–394. 10.1080/10584609.2012.737433 [DOI] [Google Scholar]
- Eveland W. P., Jr, Appiah O., Beck P. A. (2018). Americans are more exposed to difference than we think: Capturing hidden exposure to political and racial difference. Social Networks, 52, 192–200. 10.1016/j.socnet.2017.08.002 [DOI] [Google Scholar]
- Fiorina M. P., Abrams S. J. (2008). Political polarization in the American public. Annual Review of Political Science, 11(1), 563–588. 10.1146/annurev.polisci.11.053106.153836 [DOI] [Google Scholar]
- Fishbein M., Icek A. (2011). Predicting and changing behavior: The reasoned action approach. Psychology press. [Google Scholar]
- Fridman A., Gershon R., Gneezy A. (2021). COVID-19 and vaccine hesitancy: A longitudinal study. PloS one. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu L. Y., Zimet G. D., Latkin C. A., Joseph J. G. (2019). Social networks for human papillomavirus vaccine advice among african American parents. Journal of Adolescent Health, 65(1), 124–129. 10.1016/j.jadohealth.2019.01.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaines B. J., Kuklinski J. H., Quirk P. J., Peyton B., Verkuilen J. (2007). Same facts, different interpretations: Partisan motivation and opinion on Iraq. Journal of Politics, 69(4), 957–974. 10.1111/j.1468-2508.2007.00601.x [DOI] [Google Scholar]
- Galston W. A. (2021). For covid-19 vaccinations, party affiliation matters more than race and ethnicity. Brookings Institution. https://www.brookings_edu/blog/fixgov [Google Scholar]
- Gerber A. S., Green D. P., Larimer C. W. (2008). Social pressure and voter turnout: Evidence from a large-scale field experiment. American Political Science Review, 102(1), 33–48. 10.1017/s000305540808009x [DOI] [Google Scholar]
- Gollwitzer A., Martel C., Brady W. J., Pärnamets P., Freedman I. G., Knowles E. D., Van Bavel J. J. (2020). Partisan differences in physical distancing are linked to health outcomes during the COVID-19 pandemic. Nature Human Behaviour, 4(11), 1186–1197. 10.1038/s41562-020-00977-7 [DOI] [PubMed] [Google Scholar]
- Green D. P., Bradley P., Schickler E. (2004). Partisan hearts and minds: Political parties and the social identities of voters. Yale University Press. [Google Scholar]
- Hays R. B. (1989). The day-to-day functioning of close versus casual friendships. Journal of Social and Personal Relationships, 6(1), 21–37. 10.1177/026540758900600102 [DOI] [Google Scholar]
- Hill R. A., Dunbar R. I. M. (2003). Social network size in humans. Human Nature, 14(1), 53–72. 10.1007/s12110-003-1016-y [DOI] [PubMed] [Google Scholar]
- Huckfeldt R., Johnson P. E., Sprague J. (2004. a). Political disagreement: The survival of diverse opinions within communication networks. Cambridge University Press. [Google Scholar]
- Huckfeldt R., Mendez J. M., Osbornb T. (2004. b). Disagreement, ambivalence, and engagement: The political consequences of heterogeneous networks. Political Psychology, 25(1), 65–95. 10.1111/j.1467-9221.2004.00357.x [DOI] [Google Scholar]
- Huckfeldt R., Sprague J. (1987). Networks in context: The social flow of political information. American Political Science Review, 81(4), 1197–1216. 10.2307/1962585 [DOI] [Google Scholar]
- Huckfeldt R. R., Sprague J. (1995). Citizens, politics and social communication: Information and influence in an election campaign. Cambridge University Press. [Google Scholar]
- Jiang J., Chen E., Shen Y., Lerman K., Ferrara E. (2020). Political polarization drives online conversations about COVID-19 in the United States. Human Behavior and Emerging Technologies, 2(3), 200–211. 10.1002/hbe2.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones D. R., McDermott M. L. (2022). Partisanship and the politics of COVID vaccine hesitancy. Polity, 54(3), 408–434. 10.1086/719918. [DOI] [Google Scholar]
- Kahane L. H. (2021). Politicizing the mask: Political, economic and demographic factors affecting mask wearing behavior in the USA. Eastern Economic Journal, 47(2), 1–21. 10.1057/s41302-020-00186-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr J., Panagopoulos C., van der Linden S. (2021). Political polarization on COVID-19 pandemic response in the United States. Personality and Individual Differences, 179, 110892. 10.1016/j.paid.2021.110892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klar S. (2014). Partisanship in a social setting. American Journal of Political Science, 58(3), 687–704. 10.1111/ajps.12087 [DOI] [Google Scholar]
- Klofstad C. A., Edward Sokhey A., McClurg S. D. (2013). Disagreeing about disagreement: How conflict in social networks affects political behavior. American Journal of Political Science, 57(1), 120–134. 10.1111/j.1540-5907.2012.00620.x [DOI] [Google Scholar]
- Knoke D. (1990). Networks of political action: Toward theory construction*. Social Forces, 68(4), 1041–1063. 10.1093/sf/68.4.1041 [DOI] [Google Scholar]
- Konstantinou P., Georgiou K., Kumar N., Kyprianidou M., Nicolaides C., Karekla M., AngelosKassianos P. (2021). Transmission of vaccination attitudes and uptake based on social contagion theory: A scoping review. Vaccines, 9(6), 607. 10.3390/vaccines9060607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhlman C., Kumar V., Marathe M., Ravi S., Rosenkrantz D., Swarup S., Tuli G. (2011). A Bi-threshold model of complex contagion and its application to the spread of smoking behavior. Proceedings of the workshop on social network mining and analysis (SNA-KDD 2011),San Diego, California. Citeseer. [Google Scholar]
- Laumann E. O. (1973). Bonds of pluralism: The form and substance of urban social networks. J. Wiley. [Google Scholar]
- Lelkes Y., Sood G., Iyengar S. (2017). The hostile audience: The effect of access to broadband internet on partisan affect: Effect of broadband internet access on partisan affect. American Journal of Political Science, 61(1), 5–20. 10.1111/ajps.12237 [DOI] [Google Scholar]
- Li T., Zhang Y. (2015). Social network types and the health of older adults: Exploring reciprocal associations. Social Science & Medicine, 130, 59–68. 10.1016/j.socscimed.2015.02.007. [DOI] [PubMed] [Google Scholar]
- Lupton R., Thornton J. (2017). Disagreement, diversity, and participation: Examining the properties of several measures of political discussion network characteristics. Political Behavior, 39(3), 585–608. 10.1007/s11109-016-9371-7 [DOI] [Google Scholar]
- Lyons J., Sokhey A. E., McClurg S. D., Drew S. (2016). Personality, interpersonal disagreement, and electoral information. The Journal of Politics, 78(3), 806–821. 10.1086/685734 [DOI] [Google Scholar]
- Marsden P. V. (2004). Recent Developments in Network Measurement. Vol. Models and methods in social network analysis. : Cambridge University Press. [Google Scholar]
- McClurg S. D. (2006). The electoral relevance of political talk: Examining disagreement and expertise effects in social networks on political participation. American Journal of Political Science, 50(3), 737–754. 10.1111/j.1540-5907.2006.00213.x [DOI] [Google Scholar]
- McPherson M., Smith-Lovin L., JamesCook M. (2001). Birds of a feather: Homophily in social networks. Annual Review of Sociology, 27(1), 415–444. 10.1146/annurev.soc.27.1.415 [DOI] [Google Scholar]
- Motta M. (2021). Republicans, not Democrats, are more likely to endorse anti-vaccine misinformation. American Politics Research, 49(5), 428–438. 10.1177/1532673X211022639 [DOI] [Google Scholar]
- Mutz D. C. (2006). Hearing the other side: Deliberative versus participatory democracy. Cambridge University Press. [Google Scholar]
- Paluck E. L., Shepherd H., Aronow P. M. (2016). Changing climates of conflict: A social network experiment in 56 schools. Proceedings of the National Academy of Sciences, 113(3), 566–571. 10.1073/pnas.1514483113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panagopoulos C. (2010). Affect, social pressure and prosocial motivation: Field experimental evidence of the mobilizing effects of pride, shame and publicizing voting behavior. Political Behavior, 32(3), 369–386. 10.1007/s11109-010-9114-0 [DOI] [Google Scholar]
- Pink S. L., Chu J., Druckman J. N., Rand D. G., Robb Willer., Willer R. (2021). Elite party cues increase vaccination intentions among Republicans. Proceedings of the National Academy of Sciences, 118(32), Article e2106559118. 10.1073/pnas.2106559118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prior M. (2007). Post-broadcast democracy: How media choice increases inequality in political involvement and polarizes elections. Cambridge University Press. [Google Scholar]
- Roberts D. C., Utych S. M. (2021). Polarized social distancing: Residents of republican-majority counties spend more time away from home during the COVID- 19 crisis. Social Science Quarterly, 102(6), 2516–2527. 10.1111/ssqu.13101 [DOI] [Google Scholar]
- Settle J. E., Carlson T. N. (2019). Opting out of political discussions. Political Communication, 36(3), 476–496. 10.1080/10584609.2018.1561563 [DOI] [Google Scholar]
- Shin J., Yang A., Liu W., Kim H. M., Zhou A., Sun J. (2022). Mask- wearing as a partisan issue: Social identity and communication of party norms on social media among political elites. Social Media + Society, 8(1), 20563051221086230. 10.1177/20563051221086233 [DOI] [Google Scholar]
- Sinclair B. (2012). The social citizen: Peer networks and political behavior. University of Chicago Press. [Google Scholar]
- Smirnov I., Thurner S. (2017). formation of homophily in academic performance: Students change their friends rather than performance. Plos One, 12(8), Article e0183473. 10.1371/journal.pone.0183473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sokhey A. E., McClurg S. D. (2012). Social networks and correct voting. The Journal of Politics, 74(3), 751–764. 10.1017/S0022381612000461 [DOI] [Google Scholar]
- The New York Times (2020). See how vaccinations are going in your county and state (December 17). The New York Times. [Google Scholar]
- Trogen B., Pirofski L-A. (2021). Understanding vaccine hesitancy in COVID-19. Med (New York, N.y.), 2(5), 498–501. 10.1016/j.medj.2021.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troiano G., Nardi A. (2021). Vaccine hesitancy in the era of COVID-19. Public Health, 194, 245–251. 10.1016/j.puhe.2021.02.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisel O. (2021). Vaccination as a social contract: The case of COVID-19 and US political partisanship. Proceedings of the National Academy of Sciences, 118(13), Article e2026745118. 10.1073/pnas.2026745118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2013). The Determinants of Vaccine Hesitancy: Sample Survey Questions. World Health Organization. https://www.who.int/immunization/sage/meetings/2013/april/4_survey_questionsRevised.pdf. [Google Scholar]
- World Health Organization (2021). Statement for healthcare professionals: How COVID-19 vaccines are regulated for safety and effectiveness (revised march 2022). World Health Organization. Retrieved June 4, 2022https://www.who.int/news/item/17-05-2022-statement-for-healthcare-professionals-how-covid-19-vaccines-are-regulated-for-safety-and-effectiveness [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Polarization in COVID-19 Vaccine Discussion Networks by Sharif Amlani, Spencer Kiesel, and Ross Butters in American Politics Research