Summary
Background
Daily and on-demand pre-exposure prophylaxis (PrEP) are effective at preventing HIV acquisition among men who have sex with men (MSM), but only daily PrEP is approved in the US. On-demand PrEP may improve uptake and adherence. We identify sub-groups of MSM who would benefit from on-demand PrEP and determine effectiveness achieved if individuals used their optimal regimens.
Methods
Using data from the HPTN 067 study (study period 2012–2014), we created an individual-based stochastic model of HIV risk in two synthetic MSM populations with parameters separately estimated using data from Harlem, US, and Bangkok, Thailand. Agents were assigned daily and on-demand PrEP for six months each. Two personalized PrEP assignments: optimal, based on improved predicted effectiveness and reduced pill burden, and adherence-based, using daily PrEP adherence, were simulated for another six months.
Findings
Simulated on-demand PrEP was optimal for approximately one-third of MSM. It was assigned mainly to those with low daily PrEP adherence (88% (Harlem), 95% (Bangkok) of MSM with daily PrEP adherence <40%). Mean effectiveness was slightly higher in the full synthetic population with optimal PrEP assignment compared to universal daily PrEP. Among MSM for whom on-demand PrEP was optimal, mean effectiveness improved by 18 (Harlem) and 7 percentage points (Bangkok). Comparable predicted effectiveness was achieved if on-demand PrEP was assigned to the population with daily PrEP adherence <50%. There was no advantage in assigning on-demand PrEP by sex act frequency.
Interpretation
On-demand PrEP could benefit many MSM by increasing effectiveness or decreasing pill burden with similar effectiveness. On-demand PrEP may be an effective alternative to daily PrEP for individuals with difficulty taking daily PrEP consistently. Results were similar for Harlem and Bangkok, indicating that these conclusions were robust in populations with different overall adherence levels and may inform future public-health policies.
Funding
US NIH grant UM1 AI068617.
Keywords: HIV, PrEP, On-demand PrEP, 2-1-1 PrEP, MSM, Mathematical model, US, Thailand
Research in context.
Evidence before this study
Pre-exposure prophylaxis (PrEP) with daily pill taking is an effective method to prevent HIV acquisition, but many individuals who are at high risk of HIV acquisition do not use daily PrEP. PrEP effectiveness depends on good adherence, which can be challenging for many users. On-demand PrEP, in which pills are only taken around sex acts, is also an effective method to prevent HIV in men who have sex with men (MSM) but is not currently FDA approved in the US and not as well known among potential users. On-demand PrEP may improve PrEP uptake, especially in individuals concerned about consistently taking daily pills or about side effects.
Added value of this study
We used detailed clinical trial data from a HIV Prevention Trials Network trial evaluating three PrEP regimens in Harlem, US, and Bangkok, Thailand, to inform an individual-based stochastic model of pill taking and sex frequency in order to model HIV risk with both daily and on-demand PrEP. We found that MSM who have poor adherence to daily PrEP are expected to have higher effectiveness and therefore lower risk of HIV acquisition when using on-demand PrEP. There was no advantage to assigning on-demand PrEP to MSM based on sex frequency.
Implications of all the available evidence
On-demand PrEP could benefit many MSM by increasing PrEP effectiveness or decreasing pill burden with similar effectiveness. On-demand PrEP should be offered to individuals with difficulty taking daily PrEP consistently.
Introduction
Despite promising advances in prevention, HIV remains a significant public health burden with 1.5 million new infections globally in 2020,1 disproportionately affecting men who have sex with men (MSM) in many areas. Pre-exposure prophylaxis (PrEP) with daily oral tenofovir disoproxil fumarate/emtricitabine (TDF-FTC) is effective for preventing HIV acquisition among MSM,2 but uptake remains low, especially among younger MSM and Black and Indigenous people of color (BIPOC) globally.3 Even among those using PrEP, effectiveness depends on continuous adherence, which is challenging for many.4,5 Indeed, challenges in uptake, persistence, and adherence have limited the impact of daily PrEP in decreasing HIV incidence.6, 7, 8
The availability of on-demand PrEP, where individuals align pill-taking with periods of sexual activity, may improve PrEP uptake, persistence, and adherence, particularly among those concerned about side effects or consistently adhering to daily pill taking,9, 10, 11, 12 or who prefer to take fewer pills. The best-supported on-demand PrEP regimen is “2-1-1,” in which individuals take two pills 2–24 h prior to sex, one on each day following day in which a sex act occurs, one 24 h after the final pre-sex act dose, and one 24 h after that.13 In a randomized controlled trial of MSM in France, on-demand 2-1-1 PrEP was found to reduce HIV incidence by 86% compared to placebo.13 Surveys of early adopters and demonstration projects have consistently found that MSM prescribed on-demand 2-1-1 PrEP report high use with sex acts,12,14 with adherence levels up to 81% and 88% in European trials.15,16 On-demand PrEP use is rarer in the United States (US) but one survey of US MSM who had taken on-demand PrEP (either as prescribed by a physician or self-modified from a daily PrEP prescription) found high levels of adherence (over 84%) for this regimen.11
The HPTN 067 study compared daily PrEP with two non-daily PrEP strategies: time-driven (one pill twice per week with a post-sex dose <2 h after sex) and event-driven PrEP (1 pill 24–48 h before and 1 pill <2 h after sex) among MSM in Harlem, New York, USA, and Bangkok, Thailand.17,18 The study collected data using real-time electronic drug monitoring pill bottles and self-reported data from weekly interviews on sex acts and when PrEP was ingested relative to pill bottle opening and sex acts.17 In Harlem, participants in the non-daily regimens had lower sex act coverage than those on daily PrEP, while participants in Bangkok had similar sex act coverage with each regimen. Blood concentrations of PrEP indicative of taking ≥2 pills/week were measured in >95% of visits when sex was reported in the prior week in all study arms in Bangkok, but in only 49%, 31%, and 17% of visits in Harlem in the daily, time-driven, and event-driven PrEP arms, respectively.17 Although they preferred on-demand PrEP, a sub-study of Harlem-based participants in HPTN 067 shared concerns about its effectiveness and their ability to adhere to more complicated regimens.19
In this study, we used mathematical modeling to: 1) simulate pill-taking and sex act frequency based on patterns observed in HPTN 067; 2) identify those who would benefit most from using on-demand 2-1-1 PrEP; and 3) report on different strategies of individualized PrEP assignment (to daily or on-demand 2-1-1 PrEP) based on improved effectiveness, reduced pill burden, and/or the likelihood of adhering to daily PrEP. We utilized observed data from HPTN 067 to predict associations between sexual behavior, ability to predict sex, and likelihood of taking regularly scheduled pills and pills before expected sex acts or after sex. This allowed us to develop a detailed model of pill-taking and sex act frequency and HIV risk to predict how individuals would respond to changes in their prescribed PrEP regimen and compare the effectiveness of different regimens in reducing risk of HIV acquisition. A key feature of our modeling framework is the ability to predict adherence when assigned to different PrEP regimens. While many MSM maintain high adherence when using on-demand PrEP, many more who could benefit from it had no chance to try it (91% of respondents in one survey had heard of PrEP, but only 23% and 17% of respondents had heard of non-daily PrEP and of taking PrEP only around sex acts, respectively20). We endeavored to determine which groups of MSM would benefit most from on-demand PrEP use to hopefully increase knowledge of and guide prescription of this regimen.
Methods
Based on the observed patterns in HPTN 067, we developed an agent-based stochastic model simulating pill taking and sex act frequency and used the model to create a distribution of these behaviors for model agents assigned to daily and on-demand 2-1-1 PrEP. First, we estimated model parameters which govern pill taking behavior and sexual activity separately for each PrEP regimen in HPTN 067 (daily, time-driven, and event-driven). We then used these parameters to simulate on-demand PrEP by modifying the event-driven PrEP regimen with 2-1-1 PrEP guidelines13. PrEP adherence was measured separately for patterns of “fixed” pills taken daily or weekly at regular intervals and “on-demand” pills taken before and after sex acts observed in HPTN 067. Next, we created a synthetic trial population to simulate daily and on-demand PrEP and predict PrEP adherence for each modelled agent. We calculated PrEP effectiveness for the synthetic trial population, measured as percent reduction in HIV risk, accounting for the predicted number of pills taken around agents’ sex acts. We determined an optimal PrEP regimen for each agent based on calculated effectiveness and number of pills taken. Finally, we evaluated the effectiveness of the optimal PrEP assignment and compared it to an adherence-based PrEP assignment in which only agents with low observed adherence to daily PrEP were assigned on-demand PrEP to determine the predicted impact of adding on-demand PrEP as an option. Lastly, we validated adherence for HPTN 067 participants based on observed pharmacokinetic data.
Panel 1: Model terms and definitions.
| Model terms | Definitions |
|---|---|
| Fixed regimen | PrEP pills taken at regular intervals (daily or weekly) |
| On-demand regimen | PrEP pills taken before and after sex acts |
| Optimal PrEP assignment | On-demand PrEP was assigned if it resulted in i) any improvement in effectiveness with fewer pills taken than daily PrEP (Criterion 1); ii) more than 10 percentage points (pp) improvement in effectiveness compared to daily PrEP (Criterion 2); or iii) less than 10 pp reduction in effectiveness compared to daily PrEP with fewer than half the number of pills taken (Criterion 3). In all other cases daily PrEP was assigned. |
| Adherence-based PrEP assignment | Agents with adherence to daily PrEP below 40, 50, or 60% were assigned on-demand PrEP. All other agents were assigned to daily PrEP. |
Modeling pill-taking and sex act frequency
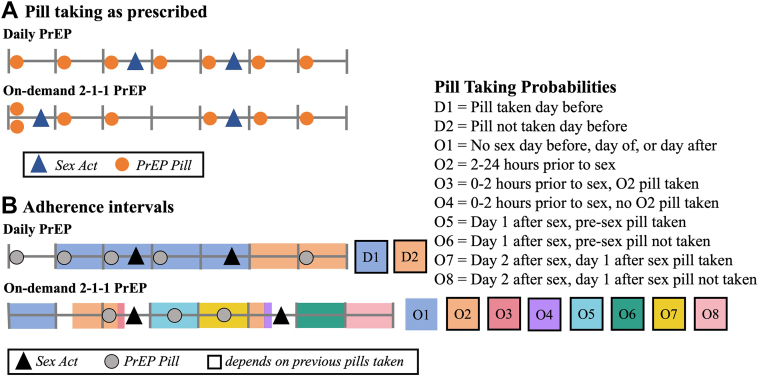
Using observed data from HPTN 067, we estimated individual pill-taking by dividing the study follow-up time into discrete adherence intervals during which a pill may or may not be taken. These intervals ranged from 2 to 44 h and depended on proximity to sex acts. Intervals were grouped into interval types, depending on the assigned PrEP regimen (daily or on-demand), recent pill-taking behavior, and proximity to sex acts (Fig. 1). refers to the probability of individual taking PrEP during interval . This depended on , the PrEP adherence parameter for individual and regimen ; had one entry per interval type and referred to the log-odds of taking a pill (see Fig. 1 for interval definitions). Its distribution was estimated from HPTN 067 data.
Fig. 1.
A: Diagram of PrEP regimens for a typical week: daily PrEP: one pill per day; on-demand PrEP: two pills 2–24 h before sex acts (only one pill if other pills taken in previous seven days), one pill 24 h after the last pre-sex pill, and one pill 24 h after that. B: Diagram of PrEP regimens' adherence interval types. Each regimen's adherence interval depended on previous pills taken (outlined label boxes) and on time before or after sex acts. Pill taking and sex acts here are to illustrate when each adherence interval occurs and do not reflect actual data.
The mean, , and covariance matrix, , describe the population distribution of the PrEP adherence parameters (see Table 1) for regimen and can be used to simulate a synthetic population. The number of modeled sex acts for each agent on each day was Poisson distributed with agent-specific mean . , , and were estimated from HPTN 067 data.17
Table 1.
Probability of pill taking within each adherence interval type.
| Interval type | Parameter | Pill taking probability: Harlem |
Pill taking probability: Bangkok |
|||
|---|---|---|---|---|---|---|
| Median | IQR | Median | IQR | |||
| A. Daily PrEP | Pill taken day before | D1 | 79% | 62–90% | 93% | 81–97% |
| Pill not taken day before | D2 | 46% | 28–65% | 79% | 53–92% | |
| B. On-demand PrEP | No sex act day before, day of, day after | O1 | 7% | 3–16% | 7% | 4–11% |
| 2–24 h prior to sex act | O2 | 29% | 21–40% | 36% | 32–40% | |
| 0–2 h prior to sex act, pill taken in 2–24 h window | O3 | 20% | 12–30% | 19% | 13–27% | |
| 0–2 h prior to sex act, pill not taken in 2–24 h window | O4 | 31% | 15–53% | 55% | 45–65% | |
| Day 1 after sex act, pre-sex act pill taken | O5 | 18% | 11–28% | 43% | 31–57% | |
| Day 1 after sex act, pre-sex act pill not taken | O6 | 13% | 9–20% | 6% | 3–11% | |
| Day 2 after sex act, day 1 after sex act pill taken | O7 | 90% | NA | 90% | NA | |
| Day 2 after sex act, day 1 after sex act pill not taken | O8 | 13% | 9–20% | 6% | 3–11% | |
A: Probabilities of daily PrEP use estimated from daily HPTN 067 arm data. B: Probabilities of on-demand PrEP use based on probabilities estimated from event-driven HPTN 067 arm data, with the exception of the second post-sex act pill, which was assigned 90% probability based on 2-1-1 adherence data.11
Daily PrEP
For daily PrEP, there were two interval types, D1 and D2, corresponding to days with or without a pill taken on the previous day. Pill taking probabilities were calculated from the observed daily arm of HPTN 067.
On-demand PrEP
We extended the probability estimates based on data from observed event-driven PrEP to inform adherence probabilities for on-demand 2-1-1 PrEP assuming individuals were as likely to adhere to the on-demand 2-1-1 regimen as they were to the event-driven regimen in HPTN 067. Therefore, we used pre-sex, post-sex, and make-up (an otherwise unneeded pill taken the day after a prescribed pill was missed) pill taking probabilities from the observed event-driven arm of HPTN 067 (see supplement for full details) to simulate on-demand 2-1-1 PrEP. The modeled pre-sex pill was doubled to two pills if there were no other pills taken in the previous seven days or current day, reflecting that 2-1-1 users are instructed not to double their first pill if they have taken pills in the preceding week. If sex acts occurred on multiple consecutive days, only one modeled pill would be taken on each subsequent day. The modeled make-up pill was doubled under the same conditions as the pre-sex pill, reflecting instructions to take two pills after sex if the pre-sex pills were missed.21 If the first post-sex pill was taken, the second modeled pill was taken on the following day with a 90% probability.11 An alternative scenario in which the second post-sex pill was independent of the first (with the same pill taking probability as the first post-sex pill) was also simulated. If the first post-sex pill was missed, the second post-sex pill was taken with the make-up pill probability.
Estimating PrEP adherence
Two measures of adherence were used for mapping between regimens: “fixed” pill adherence covering daily or weekly pills which were expected to be taken at regular intervals and “on-demand” pill adherence which were expected to be taken before and after sex acts. We evaluated the Pearson correlation coefficient between adherence to fixed and on-demand pills using data from the time-driven arm of HPTN 067 where participants took both fixed and on-demand pills so adherence to both types could be assessed in the same participants in the same time-period. We assumed agents retained the same fixed pill adherence quintile when assigned to time-driven PrEP or daily PrEP and the same on-demand pill adherence quintile when assigned to time-driven PrEP or on-demand PrEP. This allowed us to predict agent adherence levels when assigned to different regimens.
Creation of synthetic population
We created a synthetic population of 10,000 agents with defined pill taking and sex act frequency for each regimen = {,,,}. Given the different underlying distribution of pill taking behaviors, separate synthetic populations were created to represent the Bangkok and Harlem populations.
To create each of these populations, we first sampled 10,000 adherence parameter sets from each regimen and site-specific parameter distribution. Adherence parameter sets were stochastically combined.
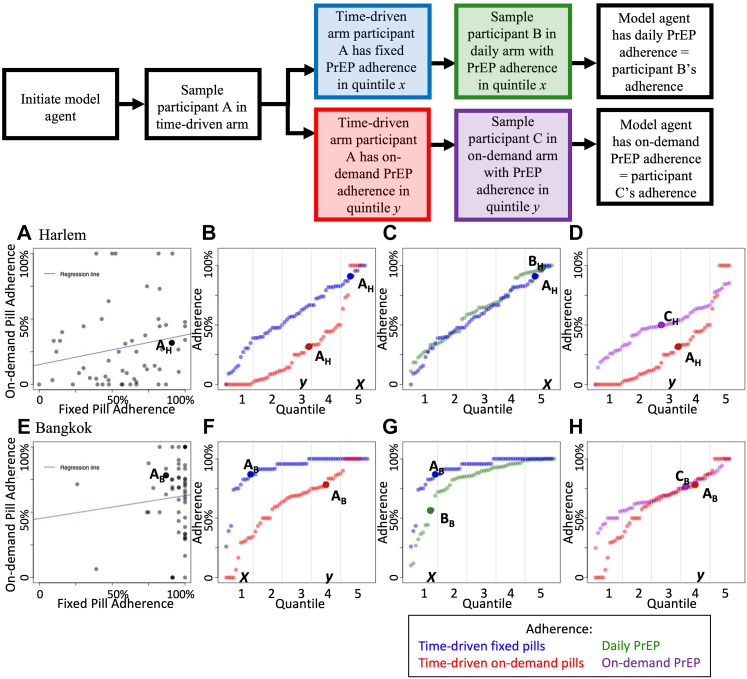
When an agent in the model was created, we sampled a participant from the time-driven arm of HPTN 067 (Fig. 2). That participant had both fixed and on-demand PrEP adherence values in quintiles x and y, respectively. For fixed adherence, a participant in the daily PrEP arm with adherence in quintile x was sampled and the modeled agent had daily PrEP adherence equal to that participant. For on-demand adherence, a participant in the on-demand PrEP arm with post-sex pill adherence in quintile y was sampled and the modeled agent had on-demand PrEP adherence equal to that participant. In this way, we directly used observed adherence data from the daily and event-driven arms of HPTN 067, linked by time-driven arm participants’ propensities to adhere to fixed and on-demand pills. Note that model agents may or may not have fixed and on-demand adherence in the same quintile. Pill taking behavior at the given adherence level was modeled as described above.
Fig. 2.
Bridging between PrEP regimens. Plots show data from the HPTN 067 trial. When a model agent is created, a participant from the time-driven arm of HPTN 067 is sampled. That participant has both fixed and on-demand PrEP adherence values (A & E) in quintiles x and y respectively (B & F). For fixed adherence, a participant in the daily PrEP arm with adherence in quintile x is sampled (C & G) and the modeled agent has daily PrEP adherence equal to that participant. For on-demand adherence, a participant in the event-driven PrEP arm with post-sex pill adherence in quintile y is sampled (D & H) and the modeled agent has on-demand PrEP adherence equal to that participant. In this way we use adherence data from the daily and event-driven arms of HPTN 067, linked by actual participants' propensities to adhere to fixed or on-demand pills. Participants may or may not have fixed and on-demand adherence in the same quintile as there was no statistical correlation found between these adherence types.
Estimating PrEP effectiveness
PrEP effectiveness was calculated on a per-sex act basis for each model agent. For sex act k, we added together the number of pills taken on the day of, the four days prior, and the two subsequent days. If at least two, four, or seven cumulative pills were taken, we assumed that the risk of HIV acquisition for that sex act was reduced by 76%, 96%, or 99%, respectively.4 If pills were taken both 2–48 h prior and 2 h after a sex act, HIV risk was reduced by 96% even if less than four pills were taken within the week of the sex act, reflecting perfect adherence to the event-driven regimen. A sensitivity analysis removing this assumption was also conducted.
Each sex act had an intrinsic untreated hazard, depending on condom use, sexual positioning, STI status of the agent, etc. This hazard for sex act k was reduced to during treatment. We defined the predicted effectiveness value for an agent to be the reduction in cumulative HIV hazard compared to no PrEP
We assumed the untreated intrinsic hazard was constant across all of an individual's sex acts or, equivalently, that their protection was uncorrelated with With this assumption, the effectiveness for an agent simplified to the mean level of protection across all sex acts. The population-level effectiveness was similarly the mean level of protection across all sex acts in the synthetic population.
Optimal PrEP assignment
The pill-taking and sex act frequency of each agent in the synthetic population were simulated separately for daily and on-demand PrEP for six months each. Effectiveness and number of pills taken were determined for each agent on each regimen. On-demand PrEP was identified as the optimal regimen over daily PrEP for an agent if it resulted in: i) any improvement in effectiveness with fewer pills taken than daily PrEP (Criterion 1); ii) > 10 percentage points (pp) higher effectiveness than daily PrEP (Criterion 2); or iii) < 10 pp lower effectiveness than daily PrEP with fewer than half the number of pills taken (Criterion 3) (see Fig. S3). In all other cases daily PrEP was identified as optimal. These criteria were chosen to reflect the potential preference of individuals to take fewer pills as long as effectiveness was not greatly reduced. We evaluated an optimal PrEP assignment in which each of the 10,000 agents in the synthetic population was assigned to their optimal regimen and simulated for six months. We considered alternate thresholds on the optimization criteria as part of a sensitivity analysis.
Adherence-based PrEP assignment
We evaluated a simplified, adherence-based PrEP assignment constructed on the simulated adherence to daily PrEP only. In this analysis, we simulated the entire synthetic population on daily PrEP for six months and calculated each agent's adherence (as the mean number of days a pill was taken). On-demand PrEP was assigned to agents with daily PrEP adherence below 50% while daily PrEP was assigned to all other agents. The synthetic population was simulated for another six months. Sensitivity analyses were conducted with on-demand PrEP assigned to agents with daily PrEP adherence between <40 and < 60%.
Pharmacokinetic validation of adherence
To determine whether observed real-time electronic drug monitoring pill bottles and self-reported pill taking in HPTN 067 was accurate, we examined pharmacokinetic data consisting of dried blood spot (DBS, Harlem) or peripheral blood mononuclear cell (PBMC, Bangkok) concentrations of tenofovir diphosphate (TVF-DP) to determine whether there were mismatches between reported pill taking and measured drug concentrations. Mismatched adherence was defined as a report in which two or more pills were reportedly taken in the past week, but drug concentration was measured as zero. We performed a sensitivity analysis eliminating participant data with mismatched adherence. In the supplement, we performed another sensitivity analysis eliminating participant data with an expanded definition of mismatched adherence including reports with two or more pills reportedly taken and measured drug concentration based on half-life <350 fmol/106 cells5,22 (DBS analysis, Harlem) or <3 fmol/106 cells4,23 (PBMC analysis, Bangkok).
Role of funding
The study funding source had no role in the design or interpretation of the study or in the writing of the manuscript.
Results
Analysis of the pill taking behavior in HPTN 067
In the daily arm of HPTN 067, participants were much more likely to take a pill if a pill was taken the day before than if no pill was taken (median probability Harlem: 33pp, Bangkok: 14pp higher, Table 1A). This resulted in sequences of successive or missed pill-taking days.
In the event-driven arm of HPTN 067 (which was assumed to have the same adherence probabilities as on-demand PrEP), pills were taken before a sex act with an approximately 30% median probability either in the prescribed 2–24 h window before a sex act, or 0–2 h before sex with no pill in the previous window in Harlem, while in Bangkok the probabilities were higher at 36% and 55%, respectively (Table 1B). Participants in Bangkok were also more likely to take post-sex act pills in the prescribed 0–2 h window after a sex act compared to participants in Harlem (Bangkok: 43%, Harlem: 18%), and participants in Harlem (compared to participants in Bangkok) were more likely to make up for a missed post-sex act pill the following day (Harlem: 13%, Bangkok: 6%).
In the time-driven arm of HPTN 067, participants were assigned to take both fixed and on-demand PrEP. There was no statistically significant correlation between a participant's adherence to fixed pills and their adherence to on-demand pills (Harlem: p = 0.14 and Bangkok: p = 0.53, Fig. S5).
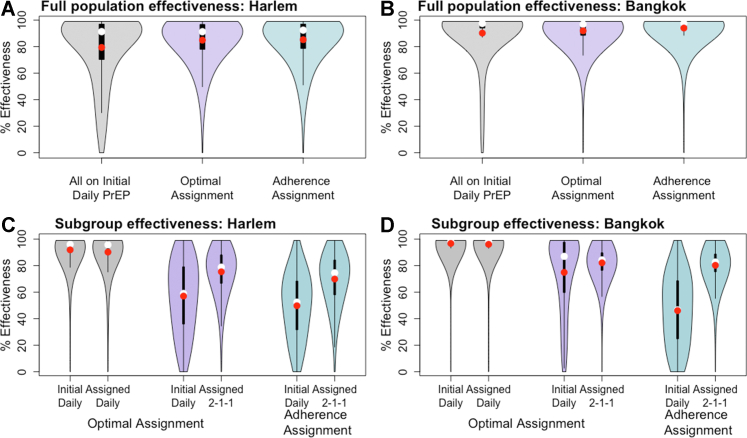
Predicted population effectiveness
Using the optimality criteria defined above, on-demand PrEP was optimal for 36% (Harlem) and 30% (Bangkok) of the population. In the adherence-based assignment, on-demand PrEP was assigned to 30% (Harlem) and 11% (Bangkok) of the population who had adherence to daily PrEP below 50%. The mean population predicted effectiveness improved slightly for both optimal and adherence-based PrEP assignments, with more significant improvement projected for Harlem. Mean population effectiveness improved from 79% to 85% (Harlem) and from 90% to 92% (Bangkok) when switching from universal daily PrEP to the optimal PrEP assignment (Fig. 3A and B). In comparison, mean effectiveness improved to 85% (Harlem) and 94% (Bangkok) when assessed based on daily PrEP adherence. As expected, taking more pills is associated with better effectiveness regardless of the regimen assignment (Fig. S6).
Fig. 3.
Predicted effectiveness of evaluated PrEP assignments for Harlem (A & C) and Bangkok (B & D). Red and white dots indicate mean and median values, respectively. Thick black bars show the interquartile range (IQR) and thin black lines show 1.5∗IQR. Shaded areas show the distribution of the data using kernel density estimation. A & B: Overall effectiveness for the whole population with agents on daily PrEP (gray), with optimal PrEP (purple), and adherence-based PrEP (blue). C & D: Effectiveness of daily and on-demand PrEP within the groups assigned to each regimen: with optimal PrEP assignment, daily PrEP optimal (gray), on-demand PrEP optimal (purple); with adherence-based PrEP assignment, daily PrEP assigned was qualitatively similar to daily PrEP optimal (not shown), on-demand PrEP assigned (blue).
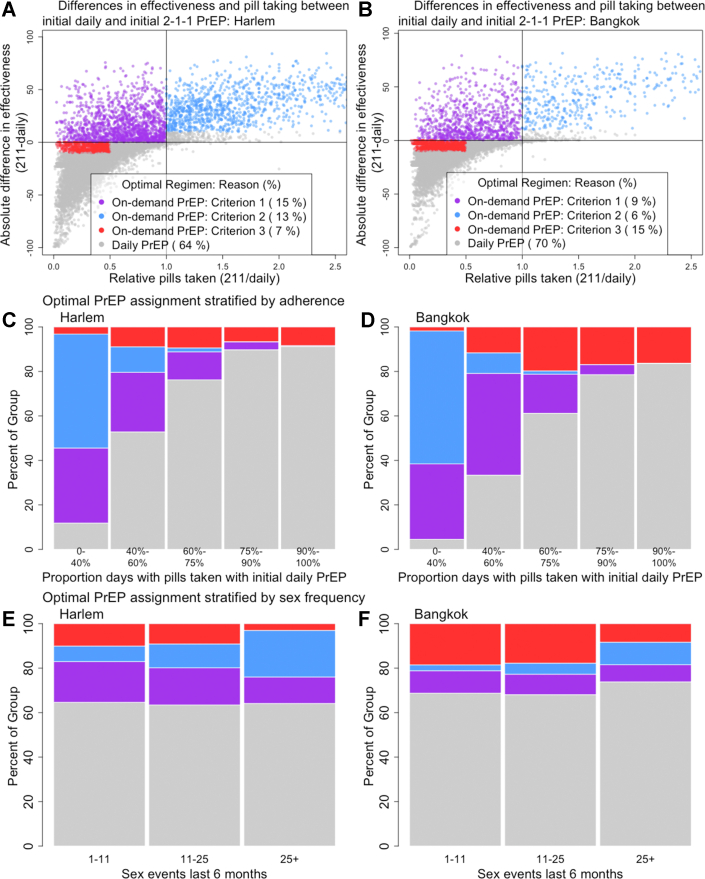
Restricted to the group of agents for whom on-demand PrEP was optimal in Harlem, mean effectiveness improved from 57% when using daily PrEP to 75% when using on-demand PrEP (Fig. 3C). Fewer pills were also required when this group switched to on-demand PrEP (daily PrEP pill count per week = 2.9, on-demand PrEP pill count = 2.3). Effectiveness increased for 80% of the group and pill taking decreased for 63% (Fig. 4A). In Bangkok, effectiveness improved less for the group of agents for whom on-demand PrEP was optimal: mean effectiveness on daily PrEP was 75% and mean effectiveness on on-demand PrEP was 82% (Fig. 3D). Substantially fewer pills were required when this group switched to on-demand PrEP (initial daily PrEP pill count per week = 4.4, on-demand PrEP pill count = 2). Effectiveness increased for 49% of the group and pill taking decreased for 81% (Fig. 4B).
Fig. 4.
Groups of agents for whom on-demand PrEP was optimal in Harlem (A, C, E) and Bangkok (B, D, F). A & B: Absolute percent difference in effectiveness and relative difference in pill taking between daily and on-demand PrEP. Colored dots represent agents for whom on-demand PrEP was optimal and gray dots represent agents for whom daily PrEP was optimal. C–F: Predicted proportion of agents for whom on-demand PrEP was optimal by adherence to daily PrEP (C & D) and sex frequency (E & F) and by optimality criteria. Criterion 1: any improvement in effectiveness with fewer pills taken than daily PrEP; Criterion 2: >10 percentage points (pp) higher effectiveness than daily PrEP; Criterion 3: <10 pp lower effectiveness than daily PrEP with fewer than half the number of pills taken. Note difference in size between adherence groups in Table 2.
There were substantial increases in effectiveness in the group of agents with on-demand PrEP assigned based on daily PrEP adherence in both locations. In Harlem, mean effectiveness on daily PrEP was 50% and was 70% on on-demand 2-1-1 PrEP (Fig. 3C). In Bangkok, mean effectiveness was 46% on daily PrEP and 80% on on-demand PrEP (Fig. 3D).
Who benefits from switching to on-demand PrEP?
On-demand PrEP was optimal mainly for those agents with low adherence to daily PrEP [for 88% (Harlem) and 95% (Bangkok) of those with low adherence (below 40%) to daily PrEP, Fig. 4C and D], while daily PrEP was mainly optimal for those with high adherence to daily PrEP [91% (Harlem) and 84% (Bangkok) of those with adherence above 90%]. Benefits from switching to on-demand PrEP varied by daily PrEP adherence. High daily PrEP adherers took fewer pills when assigned to on-demand PrEP. Among agents with daily PrEP adherence above 90% for whom on-demand PrEP was optimal, 95% (Harlem) and 99% (Bangkok) were assigned based on pill reduction (Criterion 3). In contrast, low daily PrEP adherers were more likely to have higher predicted effectiveness with on-demand PrEP. This was true for 96% (Harlem) and 98% (Bangkok) of those with daily PrEP adherence below 40% for whom on-demand PrEP was optimal. Notably, there were significant differences in the daily PrEP adherence profiles of the simulated MSM populations in Harlem and Bangkok based on HPTN 067 data (Table 2).
Table 2.
Predicted proportion of population in reported daily PrEP adherence and sex act frequency groups by simulated site.
| Adherence to daily PrEP | % in Group, Harlem | % 2-1-1 optimal, Harlem | % in Group, Bangkok | % 2-1-1 optimal, Bangkok |
|---|---|---|---|---|
| 0–40% | 21% | 88% | 8% | 95% |
| 40–60% | 19% | 47% | 8% | 67% |
| 60–75% | 18% | 24% | 10% | 39% |
| 75–90% | 24% | 10% | 21% | 21% |
| 90–100% | 18% | 9% | 53% | 16% |
| Sex Acts past 6 months | % in Group, Harlem | % 2-1-1 optimal, Harlem | % in Group, Bangkok | % 2-1-1 optimal, Bangkok |
| 0–11 | 32% | 35% | 38% | 31% |
| 11–25 | 31% | 37% | 32% | 32% |
| 25+ | 37% | 36% | 30% | 26% |
Adherence cut-offs were chosen to be approximately equivalent to quintiles in the Harlem group while sex frequency cut-offs were chosen to be approximately equal to tertiles in both populations.
There was little difference in sex act frequency of agents for whom on-demand or daily PrEP was optimal (Fig. 4E and F, S8). Agents with more frequent sex acts were less likely to have on-demand PrEP as their optimal regimen due to lower pill burden. Sex act frequency distribution was similar across Harlem and Bangkok populations (Table 2).
Sensitivity analyses
We conducted sensitivity analyses to test the effects of assumptions about efficacy and pill taking probabilities on the results of the analysis with optimal PrEP assignment. In the first alternative scenario we replaced the assumption of 96% PrEP efficacy with perfect adherence to the event-driven PrEP regimen with the effectiveness value assumed with 2+ pills taken (76%+). As a result of this change, the optimal effectiveness decreased 3.26 pp in Harlem and increased 0.4 pp in Bangkok. Similarly, we also added an assumption of 96% PrEP efficacy with perfect adherence to on-demand 2-1-1 PrEP and found optimal regimen PrEP effectiveness did not change in Harlem and decreased 0.15 pp in Bangkok. We conducted a further sensitivity analysis to determine the effect of the assumption that the second post-sex act pill for on-demand PrEP was taken with a probability of 90% if the first post-sex act pill was taken. Here, we changed the probability of the second post-sex act pill to the value for the first post-sex act pill. The optimal regimen PrEP effectiveness decreased 0.35 pp in Harlem and 0.14 pp in Bangkok.
We next explored a series of alternative criteria to define optimal PrEP. If we expanded criteria to include all agents for whom on-demand PrEP had higher effectiveness regardless of the number of pills taken, on-demand PrEP was optimal for an additional 2 pp (Harlem) and 1 pp (Bangkok) of agents, and the overall PrEP effectiveness increased by 0.52 pp and 0.04 pp, respectively. The effectiveness within the subgroup for whom on-demand PrEP was optimal increased by 2 pp in Harlem but remained the same in Bangkok. Under more restrictive criteria, in which on-demand PrEP was no longer optimal for agents who took more than twice as many pills as in daily PrEP but achieved less than 10 pp higher effectiveness (Criterion 3), on-demand PrEP was optimal for 5 pp (Harlem) and 3 pp (Bangkok) fewer agents. The overall PrEP effectiveness with optimal assignment decreased by 2.6 pp (Harlem) and 1.43 pp (Bangkok) while the effectiveness in the subgroup for whom on-demand PrEP was optimal decreased by 1 pp (Harlem) and remained the same (Bangkok).
We also conducted sensitivity analyses examining alternate daily PrEP adherence thresholds (40% and 60%) in the adherence-based assignment (Fig. S4). If all agents with <40% adherence to daily PrEP were assigned on-demand PrEP, on-demand PrEP would be assigned to 9.15 pp (Harlem) and 2.40 pp (Bangkok) fewer agents. Overall effectiveness would decrease by 0.62 pp (Harlem) and increase by 0.10 pp (Bangkok) and effectiveness for the subgroup assigned on-demand PrEP would increase by 9.58 pp (Harlem) and 11.45 pp (Bangkok). If all agents with <60% adherence to daily PrEP were assigned on-demand PrEP, on-demand PrEP would be assigned to 10.00 pp (Harlem) and 4.76 pp (Bangkok) more agents. Overall effectiveness would increase by 0.18 pp (Harlem) and 0.31 pp (Bangkok) and effectiveness for the subgroup assigned on-demand PrEP would decrease by 6.60 pp (Harlem) and 9.09 pp (Bangkok).
Pharmacokinetic analyses
In Harlem, 34/173 participants with pharmacokinetic data had mismatched adherence (reported 2+ pills taken in the past week but had zero drug detected, Fig. S7). These participants made 87 total reports, 50 of which were mismatched. In Bangkok, 2/178 participants had mismatched adherence. They had 6 total reports, 4 of which were mismatched. When participants with mismatched adherence were removed from the analysis, the population predicted effectiveness with optimal PrEP assignment increased by 1.08 pp in Harlem and decreased by 0.10 pp in Bangkok.
Discussion
Both daily oral and on-demand PrEP have shown effectiveness in reducing HIV risk in MSM.2,13 The latter regimen may have better adherence and uptake among some MSM, despite not currently being recommended by the US Food and Drug Administration (FDA).24 In this study, we used a simulation model to evaluate how many daily PrEP users would benefit from switching to on-demand PrEP and how much of a benefit they would have compared to daily PrEP. We applied our analysis to two different MSM populations, Harlem, US and Bangkok, Thailand with substantially different pill-taking behavior, based on data from HPTN 067 conducted at these sites. Our findings suggest that on-demand PrEP can improve effectiveness for individuals who have low adherence to daily PrEP. We estimated that, on an individual basis, on-demand PrEP will be more advantageous for about a third of the MSM population; for those agents it increased mean effectiveness considerably (by 18pp and 7pp in Harlem and Bangkok, respectively) while requiring fewer pills (by 0.6 and 2.4 per week in Harlem and Bangkok, respectively). We further tested a simple criterion for recommending on-demand PrEP, based on adherence to daily PrEP, which resulted in a comparable increase in mean effectiveness but may reduce the proportion of MSM who benefit from it in populations with high adherence to daily PrEP. Although the behavioral parameters we used are population specific and not easily generalizable, our main result – that individuals with low adherence to daily PrEP would likely benefit from on-demand PrEP- was robust across two different populations.
A key feature of our modeling framework is its ability to predict individuals’ pill taking behavior when assigned to different PrEP regimens. This was based on the premise that fixed adherence to daily or weekly pills differed from on-demand adherence around sex acts, which may lead to higher effectiveness for some individuals using on-demand PrEP. The time-driven arm of HPTN 067 study provided a unique set of data that combined both fixed and on-demand adherences for the same population,17 allowing us to establish connections that bridged fixed-pill and on-demand pill adherences. This was a strong assumption and real-world pill taking may not follow the patterns observed in HPTN 067 when moving between fixed and on-demand pills. Although the distribution of fixed and on-demand adherence among the Harlem and Bangkok populations was quite different, overall effectiveness was similar, giving us confidence in the validity of our key assumptions. Ideally, data from observational studies in which the same people are given a chance to try different options over extended periods of time should be used to make conclusions on expected behavior upon switching regimens.25 For comparison of products with different delivery routes where at least one is directly observable, such as oral pills vs. injectables, double-blinded studies in which each participant receives one placebo and one active product may provide useful bridging information.26 This study highlights the need for additional implementation studies to compare the usage of daily and non-daily PrEP to confirm our findings and increase accuracy.
Our analysis did not explicitly account for individual preference for either daily or on-demand PrEP, which may not always align with what is optimal. Our finding that one in three MSM may benefit from using on-demand PrEP due to improved adherence, fewer pills needed, or both is similar to the fraction of individuals who express a preference for on-demand PrEP and their indicated reasons for doing so. In demonstration projects in Amsterdam and Belgium, 26.7% and 23.5% of MSM chose on-demand over daily PrEP, respectively.27, 28, 29 Further, in two different surveys of Australian MSM, 20% chose on-demand PrEP and that preference was correlated with concerns over adherence and side effects.16,17 In contrast, in studies in Asia, 57%, 56%, and 39% of MSM using PrEP chose on-demand over daily PrEP (in China, Taiwan, and Hong Kong, respectively)14,30,31 and had full adherence 82% and 92% of the time (Taiwan and Hong Kong, respectively)14,31 Preference for on-demand PrEP also depends on the available alternatives. Although survey participants frequently state a willingness to use on-demand PrEP, they typically prefer long-acting injectable PrEP,32, 33, 34, 35, 36 which was recently approved for use in US.
One challenge for our analysis was that on-demand PrEP was not included in the HPTN 067 trial, so we do not have detailed pill-taking behavior data. Instead, adherence to on-demand PrEP was predicted based on observed adherence to event-driven PrEP. This may represent a conservative estimate of adherence because event-driven PrEP had a smaller window in which post-sex act pills could be taken (2 h in event-driven PrEP versus 24 h in on-demand PrEP). Adherence to on-demand PrEP was higher in the IPERGAY trial, with 45% of participants reporting use according to the 2-1-1 guideline at last sex act (although this does not include those who used a condom instead of PrEP),13 indicating that on-demand PrEP could be more beneficial than our analysis suggests. Our estimate of a 90% probability of taking the second post-sex act pill may be optimistic, though the sensitivity analysis with decreased probability did not substantially change results. A further limitation was the self-reported nature of the sex act and pill taking data in the HPTN 067 populations. These data were collected weekly, limiting recall bias, but may be subject to social desirability bias. Our optimal regimen criteria that allowed a large reduction in pills taken to be preferable even if it entailed a small reduction in effectiveness was designed to reflect that reduction in pill count may be a significant incentive to some PrEP users, but the precise levels used were arbitrary. We used cumulative pill counts around sex acts to determine PrEP effectiveness, which did not account for timing of pill taking within the four days before and two days after a sex act. We assumed that risk per exposure in each of an individual's sex acts remained consistent, which may not be accurate due to differing risk factors in different acts that we lacked data to incorporate into our model.
Having choices in HIV prevention is the key to reach more people at risk. It is equally important to offer guidance on who may benefit most from each option. Efficacy, while important, is not the deciding factor for many in choosing an HIV prevention method.25 As more methods of HIV prevention become available, good quantitative frameworks need to be used to inform providers and guide individuals in their selection of the prevention method that will be most effective for them based on preference, sexual behavior patterns, and likelihood of adherence. Low levels of knowledge of on-demand PrEP currently represent a barrier to its use among many MSM20; increasing provider recommendations of this regimen in those who have low adherence to daily PrEP has the potential to increase PrEP effectiveness in these individuals. On-demand PrEP should become more widely available to the many MSM who could benefit from it, especially those who have low adherence to daily PrEP.
Contributors
Conception of the research question: SES, MM, DTD. Data acquisition, analysis, and interpretation: MM, JPH, DJD. Model creation: MM. Model parameterization, coding, and simulation: SES, MM. Drafting of the manuscript: SES, MM, DTD. Critical input into draft manuscript: all authors. Read & approved final manuscript: all authors.
Data sharing statement
Model data is available on request to the authors.
Declaration of interests
DJD declares support from the National Institute for Allergy and Infectious Diseases (NIAID) and lecture honoraria from University of Pennsylvania. MCB declares grants or contracts from MRC Centre for Global Infectious Disease Analysis (reference MR/R015600/1), jointly funded by the UK Medical Research Council (MRC) and the UK Foreign, Commonwealth & Development Office (FCDO), under the MRC/FCDO Concordat agreement and is also part of the EDCTP2 program supported by the European Union. JH declares grants or contracts from the National Institute of Health (NIH). The remaining authors declare no competing interests.
Acknowledgments
The authors are grateful to Heather Angier, scientific writer at the Vaccine and Infectious Disease Division of the Fred Hutchinson Cancer Center for editing of the manuscript.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.eclinm.2022.101776.
Appendix A. Supplementary data
References
- 1.UNAIDS . UNAIDS; 2021. Global HIV & AIDS Statistics — Fact Sheet. [Google Scholar]
- 2.Grant R.M., Lama J.R., Anderson P.L., et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363:2587–2599. doi: 10.1056/NEJMoa1011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoots B., Finlayson T., Nerlander L., Paz-Bailey G., Group N.H.B.S.S. Willingness to take, use of, and indications for pre-exposure prophylaxis among men who have sex with men—20 US cities, 2014. Clin Infect Dis. 2016;63:672–677. doi: 10.1093/cid/ciw367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anderson P., Glidden D., Liu A., et al. Emtricitabine-tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Sci Transl Med. 2012;4 doi: 10.1126/scitranslmed.3004006. 151ra125–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu A., Glidden D., Anderson P., et al. Patterns and correlates of PrEP drug detection among MSM and transgender women in the global iPrEx study. JAIDS. 2014;67:528–537. doi: 10.1097/QAI.0000000000000351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sullivan P., Siegler A. Getting pre-exposure prophylaxis (PrEP) to the people: opportunities, challenges and emerging models of PrEP implementation. Sex Health. 2018;15:522–527. doi: 10.1071/SH18103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hess K., Crawford J., Eanes A., et al. Reasons why young men who have sex with men report not using HIV pre-exposure prophylaxis: perceptions of burden, need, and safety. AIDS Patient Care STDS. 2019;33:449–454. doi: 10.1089/apc.2019.0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huang Y., Tao G., Smith D., Hoover K. Persistence with human immunodeficiency virus pre-exposure prophylaxis in the United States, 2012-2017. Clin Infect Dis. 2021;72:379–385. doi: 10.1093/cid/ciaa037. [DOI] [PubMed] [Google Scholar]
- 9.Vaccher S.J., Gianacas C., Templeton D.J., et al. Baseline preferences for daily, event-driven, or periodic HIV pre-exposure prophylaxis among gay and bisexual men in the PRELUDE demonstration project. Front Public Health. 2017;5:341. doi: 10.3389/fpubh.2017.00341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chan C., Vaccher S., Fraser D., et al. Preferences for current and future PrEP modalities among PrEP-experienced gay and bisexual men in Australia. AIDS Behav. 2021;26(1):88–95. doi: 10.1007/s10461-021-03344-3. [DOI] [PubMed] [Google Scholar]
- 11.Camp C., Saberi P. Facilitators and barriers of 2-1-1 HIV pre-exposure prophylaxis. PLoS One. 2021;16 doi: 10.1371/journal.pone.0251917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hojilla J., Marcus J., Silverberg M., et al. Early adopters of event-driven human immunodeficiency virus pre-exposure prophylaxis in a large healthcare system in san francisco. Clin Infect Dis. 2020;71:2710–2712. doi: 10.1093/cid/ciaa474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Molina J.-M., Capitant C., Spire B., et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med. 2015;373:2237–2246. doi: 10.1056/NEJMoa1506273. [DOI] [PubMed] [Google Scholar]
- 14.Wu H., Wen-Wei K.S., Chang H., Li C., Ko N., Strong C. Imperfect adherence in real life: a prevention-effective perspective on adherence to daily and event-driven HIV pre-exposure prophylaxis among men who have sex with men - a prospective cohort study in taiwan. J Int AIDS Soc. 2021;24 doi: 10.1002/jia2.25733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jongen V., Hoornenborg E., van den Elshout M., et al. Adherence to event-driven HIV PrEP among men who have sex with men in amsterdam, The Netherlands: analysis based on online diary data, 3-monthly questionnaires and intracellular TFV-DP. J Int AIDS Soc. 2021;24 doi: 10.1002/jia2.25708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vuylsteke B., Reyniers T., De Baetselier I., et al. Daily and event-driven pre-exposure prophylaxis for men who have sex with men in Belgium: results of a prospective cohort measuring adherence, sexual behaviour and STI incidence. J Int AIDS Soc. 2019;22 doi: 10.1002/jia2.25407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grant R., Mannheimer S., Hughes J., et al. Daily and nondaily oral preexposure prophylaxis in men and transgender women who have sex with men: the human immunodeficiency virus prevention trials network 067/ADAPT study. Clin Infect Dis. 2018;66:1712–1721. doi: 10.1093/cid/cix1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bekker L.-G., Roux S., Sebastien E., et al. Daily and non-daily pre-exposure prophylaxis in African women (HPTN 067/ADAPT Cape Town Trial): a randomised, open-label, phase 2 trial. Lancet HIV. 2018;5(2):e68–e78. doi: 10.1016/S2352-3018(17)30156-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Franks J., Hirsch-Moverman Y., Loquere A.S., et al. Sex, PrEP, and stigma: experiences with HIV pre-exposure prophylaxis among New York City MSM participating in the HPTN 067/ADAPT Study. AIDS Behav. 2018;22:1139–1149. doi: 10.1007/s10461-017-1964-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sewell W., Powell V., Mayer K., Ochoa A., Krakower D., Marcus J. Nondaily use of HIV preexposure prophylaxis in a large online survey of primarily men who have sex with men in the United States. J Acquir Immune Defic Syndr. 2020;84:182–188. doi: 10.1097/QAI.0000000000002332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Foundation S.F.A. Q&a: PrEP 2-1-1. 2019. https://www.sfaf.org/resource-library/qa-prep-2-1-1-for-anal-sex/
- 22.Castillo-Mancilla J., Zheng J., Rower J., et al. Tenofovir, emtricitabine, and tenofovir diphosphate in dried blood spots for determining recent and cumulative drug exposure. AIDS Res Hum Retroviruses. 2013;29:384–390. doi: 10.1089/aid.2012.0089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hendrix C., Andrade A., Bumpus N., et al. Dose frequency ranging pharmacokinetic study of tenofovir-emtricitabine after directly observed dosing in healthy volunteers to establish adherence benchmarks (HPTN 066) AIDS Res Hum Retroviruses. 2016;32:32–43. doi: 10.1089/aid.2015.0182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Disease Control C for, Prevention On-demand PrEP [fact sheet]. CDC. 2022. https://www.cdc.gov/hiv/basics/prep/on-demand-prep.html
- 25.Ngure K., Nair G., Szydlo D., et al. Conference on retroviruses and opportunistic infections (CROI) 2022. Choice and adherence to dapivirine ring or oral PrEP by young african women in REACH. virtual. [Google Scholar]
- 26.Landovitz R., Donnell D., Clement M., et al. Cabotegravir for HIV prevention in cisgender men and transgender women. N Engl J Med. 2021;12:595–608. doi: 10.1056/NEJMoa2101016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Coyer L., van den Elshout M., Achterbergh R., et al. Understanding pre-exposure prophylaxis (PrEP) regimen use: switching and discontinuing daily and event-driven PrEP among men who have sex with men. EClinicalMedicine. 2020;29–30 doi: 10.1016/j.eclinm.2020.100650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reyniers T., Nöstlinger C., Laga M., et al. Choosing between daily and event-driven pre-exposure prophylaxis: results of a belgian PrEP demonstration project. J Acquir Immune Defic Syndr. 2018;79:186–194. doi: 10.1097/QAI.0000000000001791. [DOI] [PubMed] [Google Scholar]
- 29.Jongen V., Reyniers T., Ypma Z., et al. Choosing event-driven and daily HIV pre-exposure prophylaxis - data from two european PrEP demonstration projects among men who have sex with men. J Int AIDS Soc. 2021;24 doi: 10.1002/jia2.25768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang J., Xu J., Wang H., et al. Preference for daily versus on-demand pre-exposure prophylaxis for HIV and correlates among men who have sex with men: the China real-world oral PrEP demonstration study. J Int AIDS Soc. 2021;24 doi: 10.1002/jia2.25667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kwan T., Lui G., Lam T., et al. Comparison between daily and on-demand PrEP (pre-exposure prophylaxis) regimen in covering condomless anal intercourse for men who have sex with men in Hong Kong: a randomized, controlled, open-label, crossover trial. J Int AIDS Soc. 2021;24 doi: 10.1002/jia2.25795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hall E., Heneine W., Sanchez T., Sineath R., Sullivan P. Preexposure prophylaxis modality preferences among men who have sex with men and use social media in the United States. J Med Internet Res. 2016;18:e111. doi: 10.2196/jmir.5713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Patel R., Crane J., López J., et al. Pre-exposure prophylaxis for HIV prevention preferences among young adult african american men who have sex with men. PLOS ONE. 2018;13 doi: 10.1371/journal.pone.0209484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Clement M., Kofron R., Landovitz R. Long-acting injectable cabotegravir for the prevention of HIV infection. Curr Opin HIV AIDS. 2020;15:19–26. doi: 10.1097/COH.0000000000000597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Biello K., Mimiaga M., Santostefano C., al et MSM at highest risk for HIV acquisition express greatest interest and preference for injectable antiretroviral PrEP compared to daily, oral medication. AIDS Behav. 2018;22:1158–1164. doi: 10.1007/s10461-017-1972-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dubov A., Ogunbajo A., Altice F., Fraenkel L. Optimizing access to PrEP based on MSM preferences: results of a discrete choice experiment. AIDS Care. 2019;31:545–553. doi: 10.1080/09540121.2018.1557590. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.