Abstract
Background:
Hip fractures are the most common orthopedic condition in elderly patients. In this patient group, efficient preoperative analgesia that reduces the requirement for opioids and their negative side effects is crucial. This study aims for evaluating the efficiency of fascia iliaca compartment block (FICB) and pericapsular nerve group (PENG) in providing the appropriate analgesia before positioning patients for spinal anesthesia (SA).
Methods:
Ninety participants undergoing hip surgeries under SA were selected randomly to receive PENG block (n = 45) using 20 mL 0.25% bupivacaine or FICB using 30 mL of 0.25% bupivacaine. The blinded observer assessed Visual Analog Scale (VAS) scores at rest, with passive leg raise to 15° before and after 30 min of the block. The blinded observer also recorded hemodynamic parameters including noninvasive blood pressure respiratory rate and heart rate. The data were analyzed using SPSS version 19. Using the appropriate statistical methodology, continuous and categorical data were analyzed, and P ≤ 0.05 was considered statistically significant.
Results:
At rest and with a passive leg raise to 15°, VAS scores in the PENG and FICB groups decreased significantly (P < 0.0001). After 30 minutes of performing the PENG block, the VAS scores at rest and passive leg raise were 2.16±0.67 and 3.29±0.73 respectively, whereas with the fascia iliaca block the VAS scores at rest and passive leg raise were 4.07±0.69 and 5.11±0.71 with the p = 0.001, which is highly significant.
Conclusion:
PENG block outperforms fascia iliaca block in providing effective analgesia before positioning patients undergoing hip surgery under SA.
Keywords: Anesthesia, fascia iliaca block, hip fractures, pericapsular nerve group block
INTRODUCTION
Hip fracture is a common orthopedic condition in geriatric population which is associated with severe pain that impedes positioning for spinal anesthesia (SA).[1] As elderly patients have associated comorbidities, regional anesthesia is preferred over general anesthesia.[2] In fracture hip surgeries, regional anesthesia is linked with lower mortality and morbidity than a general anesthesia.[3] Positioning the patient for SA is extremely painful, requires higher doses of sedatives and opioids and which is unfavorable in geriatric patients.[4] In these cases, pain management should begin as soon as the fracture occurs to facilitate tests, radiological investigations, and transportation.[5]
The most often utilized treatment for orthopedic pain was opioids. However, using opioids in older individuals has been linked to numerous complications, such as hypotension, delirium, prolonged hospitalization, respiratory depression, or postdischarge adverse effects such as dependence or addiction.[6] Hip fracture pain may be efficiently managed with regional nerve blocks, providing quick onset, site-specific analgesia that is more successful in comparison to normal systemic analgesia alone. In addition, the assertions that nerve blocks reduce hospital stays are supported by certain data and decrease morbidity and mortality as well as delirium rates.[7] Regional analgesia thus offers better analgesia and fewer side effects than opioids, making it a safer choice. In addition to being utilized in operating rooms, regional analgesia may also be used in emergency rooms to assist with patient evaluation, transportation, and radiological tests.[8] Local anesthetic is injected between the fascia iliaca and the psoas muscle using the fascia iliaca compartment block (FICB), a typical local analgesic method used by anesthesiologists to block the obturator, femoral, and lateral cutaneous nerves.[9] The research implies that the accessory obturator nerve is not blocked since these blocks only provide modest analgesia.
In 2018, Girón-Arango et al. developed the pericapsular nerve group (PENG) block utilizing ultrasonography for blocking the articular branches that go to the anterior capsule of the hip where they cross the iliopectineal eminence, recognizing the anterior capsule as the hip joint's most nerve-rich region.[10] However, there have not been any studies that compare FICB to PENG. This study's goal is to assess the effectiveness of FICB and PENG block in delivering appropriate analgesia before positioning patients having hip surgery under SA.
MATERIALS AND METHODS
Before the first patient recruitment, the current trial has been listed with the “Clinical Trials Registry of India” (CTRI/2020/07/026782). Ethical committee approval was taken (XXX; SNMC/IECHSR/2019–20/A-12/1.2) on November 12, 2019. Between January 2020 and June 2021, a total of 90 individuals were recruited [Figure 1]. We selected 90 patients for hip surgery after receiving written informed consent. The following were the inclusion criteria: age range of 18–80 years, a physical status Class I and II as per “American Society of Anesthesiologists” (ASA), and a body mass index below 35 kg.m−2. The following exclusion criteria applied: infection at injection site, allergy to local anesthetics, patients receiving opioids for chronic analgesic treatment, coagulopathy, and patients with an inguinal hernia on the same side of hip pathology.
Figure 1.
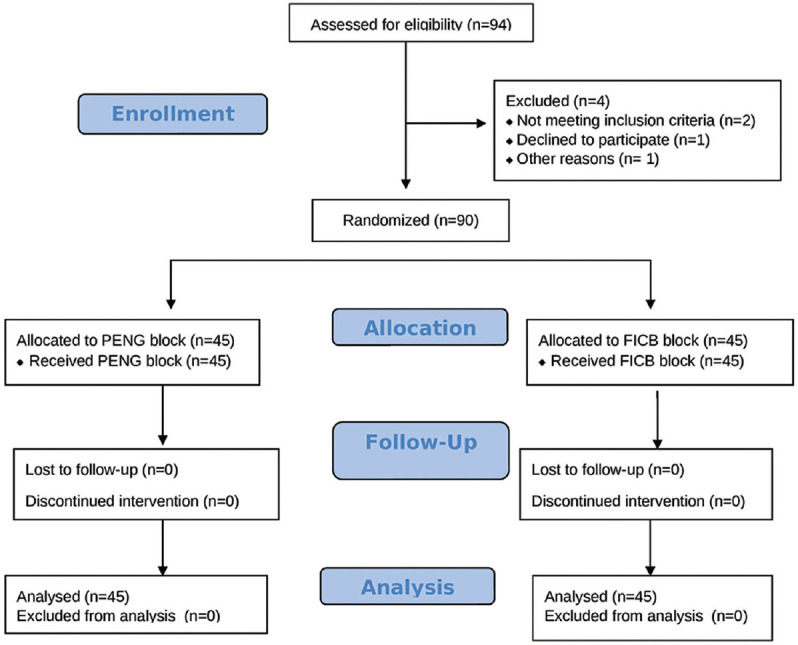
CONSORT diagram. FICB = Fascia iliaca compartment block, PENG = Pericapsular Nerve Group
Upon entering the operating room, subjects were randomly selected to take an ultrasound-guided PENG block (n = 45) or FICB (n = 45) utilizing a computer-generated random number sequence and a closed opaque envelope approach. Here, a research associate, who was not engaged in the trial, made the randomization list and opaque envelopes. After shifting the patients to the operating room, a pulse oximeter, noninvasive blood pressure, and an electrocardiogram (ECG) were attached and “systolic blood pressure” (SBP), “diastolic blood pressure” (DBP), and “heart rate” were recorded. Before the administration of the block, the patient explained the visual analog score (VAS). Preprocedure pain was assessed at rest and with passive leg rise to 15°. For passive leg raise, with a patient in supine position, the affected limb was gently raised to approximately 15° with slight flexion of hip and knee in extension. This VAS was considered a baseline score.
The ultrasonographic machine (GE Logiq e, GE Healthcare, Wisconsin, United States), 4–13 MHz linear transducer, 2–5MHz curvilinear transducer, 100 mm, 20-gauge, short-beveled block needles (Stimuplex Ultra 360, B Braun Medical, Melsungen, Germany) were used during the procedure. For PENG blocks, patients were positioned in a supine posture. A curvilinear probe was placed in transverse plane so as to identify anterior inferior iliac spine. It was then rotated about 45° anticlockwise so as to align with pubic ramus. Iliopsoas muscle and tendon, femoral artery (FA), the pectineus muscle, and the iliopubic eminence were all evident. For this procedure, a 22-gauge 100 mm needle was inserted from the lateral to the medial plane, where it was placed in the musculofascial plane between the anterior psoas tendon and the posterior pubic rami. To ensure appropriate dispersion of the local anesthetic solution (20 mL of 0.25% bupivacaine) in this plane, 5 mL increments were administered [Figure 2].
Figure 2.
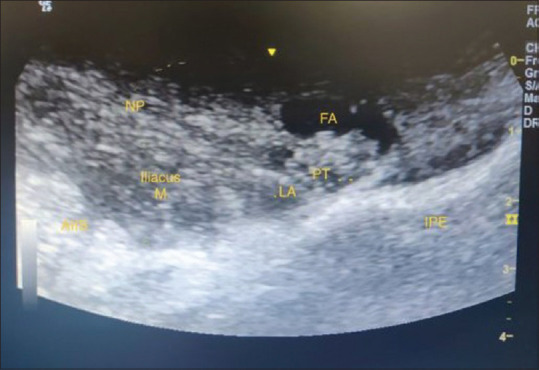
Sonoanatomy PENG block, PT=Psoas tendon, AIIS=Anterior inferior iliac spine, IPE=Iliopubic eminence, FA=Femoral artery, iliacus muscle, LA=Local anesthetic, NP=Needle path
For FICB's patients were positioned supine, a linear ultrasound probe was positioned in the inguinal crease, and a scan was carried out to identify the sartorius muscle, the FA, and nerve in the inguinal crease and following the sartorius muscle until its origin at the anterior superior iliac spine. The drug was injected below the fascia iliaca, in the lateral part of the iliacus muscle. Bupivacaine 30 mL, 0.25% was administered under the fascia iliac plane in 5 mL increments after negative aspiration [Figure 3].
Figure 3.

Sonoanatomy FICB, FI=Fascia iliaca, FA=Femoral artery, SM=Sartorius muscle, NP=Needle path, iliopsoas muscle
Patients were continually monitored for SBP, DBP, heart rate, pulse oximetry and continuous ECG, and local anesthetic toxicity symptoms for 30 min after the block. Thirty min after the blocks, VAS score was reassessed at rest and with passive leg rise to 15°. Another anesthesiologist who was not aware of the regional block's administration made all of the observations. Intravenous (i.v.) fentanyl 0.5–1 μg.kg− 1 was used in case if any patient had a VAS score of more than 3 and then they were allowed to sitting position to receive SA. Under the aseptic precaution, SA was administered utilizing a 25-gauge Quincke's spinal needle and 2 mL of 0.5% bupivacaine. We did not use any other introperative additional analgesia except 1g i.v. paracetamol at the end of surgery and thereafter every 8 h as institutional postoperative analgesia protocol. The primary outcome measures were VAS scores at rest and after a passive leg rise to 15°, as well as VAS scores 30 min after the block. The secondary outcome measures were cardiovascular stability and block-related complications.
Statistical analysis
Using OpenEpi software 2.3.1 (CDC, Atlanta, Georgia, USA) version, a sample size estimate was performed with a 95% degree of confidence and an 80% study power. According to the trial conducted by Girón-Arango et al.[10] and Shariat et al.,[11] the percentage of hip fractures patients with a complete sensory blockade in PENG block is 99.9% and with fascia iliaca block is 38%. The sample size estimated was 41 rounded off to 45 in each group, that is, 45 patients in Group A in whom PENG block was given and 45 patients in Group B in whom fascia iliaca block was given. The following formula is utilized to identify sample size: N = 2 (Zα + Zβ)2 δ2/d2, Z is a critical value for given α and β, α is type-I error (0.05), β is type-II error probability, and d is the absolute difference of two means.
Microsoft Excel was used to enter the data, and SPSS version 19.2.1 (IBM Corp., Armonk, N.Y., USA) was used to analyze it. Mean and standard deviation were computed for quantitative data, whereas percentages and proportions were utilized for qualitative data. Both qualitative and quantitative data were analyzed with the Chi-square and unpaired t-test. P = 0.05 was deemed statistically significant.
RESULTS
In both the groups, the demographic characteristics, surgical procedures, and surgery time were comparable [Table 1]. The mean VAS scores were comparable in both the groups at rest and passive leg rise before the block (P = 0.88 and 0.126, respectively) [Table 2]. VAS scores were significantly lower 30 min after block in both the groups, at rest and during movement (P = 0.001). The mean VAS scores before block with passive leg raise in PENG was 7.78 ± 0.82 and in FICB was 7.55 ± 0.50 (P = 0.126) whereas the reduction in VAS scores after block with passive leg raise PENG was 3.29 ± 0.73 and FICB 5.11 ± 0.71. This difference is statistically significant [Table 3] (P = 0.001).
Table 1.
Comparison of the group’s demographic characteristics, the surgery type, and the length of the procedure
| Variables | PENG (n=45) | FICB (n=45) | P |
|---|---|---|---|
| Age (years) | 64.62±12.13 | 64.95±8.72 | 0.881* |
| Gender (male/female) | 26/19 | 24/21 | 0.671 |
| Procedure: IT/arthroplasty/CRIF | 31/12/2 | 27/18/0 | 0.772 |
*P>0.05 (not significant). IT=Intertrochanteric, CRIF=Closed reduction internal fixation, FICB=Fascia iliaca compartment block, PENG=Pericapsular nerve group
Table 2.
Comparing the patients in the pericapsular nerve group block and fascia iliaca compartment block group’s preblock and 30-min postblock visual analog score measurements
| Groups | Mean±SD | |||
|---|---|---|---|---|
|
| ||||
| Preblock VAS | Postblock VAS | |||
|
|
|
|||
| Rest | Movement | Rest | Movement | |
| PENG (n=45) | 6.49±0.84 | 7.78±0.82 | 2.16±0.67 | 3.29±0.73 |
| FICB (n=45) | 6.47±0.50 | 7.55±0.50 | 4.07±0.69 | 5.11±0.71 |
| P | 0.88 | 0.126 | 0.001* | 0.001* |
*P<0.05 (significant). VAS=Visual analog score, SD=Standard deviation, FICB=Fascia iliaca compartment block, PENG=Pericapsular nerve group
Table 3.
Preblock and 30-min postblock hemodynamic comparison among patients in the pericapsular nerve group block and fascia iliaca compartment block groups
| Groups | Mean±SD | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Preblock hemodynamics | Postblock hemodynamics | |||||
|
|
|
|||||
| HR | SBP | DBP | HR | SBP | DBP | |
| PENG | 92.38±7.06 | 142.02±10.17 | 86.16±5.98 | 83.49±8.06 | 124.71±8.98 | 76.96±7.15 |
| FICB | 94.58±5.79 | 141.64±8.79 | 86.27±4.85 | 84.69±5.25 | 131.29±7.20 | 86.04±4.91 |
| P | 0.11 | 0.851 | 0.923 | 0.001* | 0.01* | 0.001* |
*P<0.05 (significant). DBP=Diastolic blood pressure, SBP=Systolic blood pressure, HR=Heart rate, FICB=Fascia iliaca compartment block, PENG=Pericapsular nerve group, SD=Standard deviation
At rest and during passive leg raise prior to the block, the mean heart rate, SBP, and DBP were comparable in both the groups (P = 0.11, 0.851, and 0.923, respectively) [Table 3]. There was a significant reduction in hemodynamic variables 30 min after the block in both the groups (all P = 0.001) [Table 4]. We did not encounter any block-related complications.
Table 4.
Comparison of the pericapsular nerve group block and fascia iliaca compartment block group patient’s passive leg raise hemodynamics at preblock and 30-min postblock times
| Groups | Mean±SD | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Preblock hemodynamics | Postblock hemodynamics | |||||
|
|
|
|||||
| HR | SBP | DBP | HR | SBP | DBP | |
| PENG | 97.49±8.24 | 146.58±19.04 | 90.4±7.08 | 86.04±7.95 | 130.11±7.05 | 80.99±6.38 |
| FICB | 100.02±5.75 | 150.22±9.06 | 92.30±5.28 | 92.42±5.19 | 138.96±8.96 | 89.2±5.11 |
| P | 0.094 | 0.249 | 0.826 | 0.001* | 0.001* | 0.001* |
*P<0.05 (significant). DBP=Diastolic blood pressure, SBP=Systolic blood pressure, PENG=Pericapsular nerve group, HR=Heart rate, FICB=Fascia iliaca compartment block, SD=Standard deviation
DISCUSSION
This study demonstrates that both PENG and fascia iliaca blocks provided a substantial decline in VAS scores at rest and with passive leg raise. However, PENG block provided better pain relief than FICB in positioning of patients for SA as evidenced by reduced VAS scores with passive leg raise. Moreover, in our study, we also found out that there was a significant decrease in SBP, DBP, and heart rate after PENG block compared to FICB. These changes in hemodynamic parameters can be attributed to a better reduction in pain score (VAS) with PENG block.
Proper positioning is a prerequisite for smooth conduct of SA in hip fracture patients which requires adequate analgesia. As most of the patients are elderly with comorbidities, peripheral nerve blocks are preferred for providing pain relief and avoiding systemic use of opioids. FICB and PENG blocks are common analgesic blocks used during spinal positioning. This study aims for assessing the analgesic effectiveness of the FICB and PENG block for optimal spinal positioning because both the PENG block and FICB provide efficient analgesia for patient positioning, but there are very few studies in literature in the form of case series and reports.
Fascia iliaca block is a 3-in-1 block that involves the femoral nerve, obturator nerve, and lateral femoral cutaneous nerve, but obturator nerve sparing is common. According to Shariat et al.,[11] there was no noticeable difference between the FICB with 0.5% ropivacaine and the sham block with 0.9% normal saline in terms of postoperative pain scores or 24-h opioid intake in THA patients. Kacha et al.[12] conducted a randomized, controlled, double-blind prospective trial with 100 patients scheduled for hip or proximal femoral surgery. They reported a significant reduction in VAS scores with FICB with 30 mL of 0.25% ropivacaine when compared to SHAM block with 30 mL normal saline. In our study, we also found a significant reduction in pain scores after FICB.
The PENG block, a new regional analgesic block based on cadaveric research, targets the articular branches to the anterior part of the hip joint with a single injection. This study demonstrates the accessory obturator nerve's contribution to the anterior hip joint. Giron Arango et al.[10] conducted a case series on five patients with hip fractures. PENG block was given in all five patients which showed a decline in pain scores in all five individuals even at rest, and also with passive leg raise, the maximum reported VAS score was 2. The case series study by Sahoo et al.[13] included nine patients who had been scheduled for hip fracture surgery. The VAS ratings at rest and during passive leg raise were significantly reduced for all 9 patients who had PENG block. Our study also got similar results; there was an effective reduction in VAS scores after the PENG block.
Only a few studies have compared FICB to PENG block. PENG block had better postoperative analgesic efficacy compared to FICB, according to Senthil et al.[14] The PENG block had a significantly longer first time of analgesic requirement postsurgery than the FICB (P = 0.007). The overall quantity of morphine consumed in the PENG block was considerably less (P = 0.008) as compared to the FICB group. Forty patients with hip fracure were randomized to receive either PENG or FICB blocks by Senthil et al.,[14] and they observed that there was no significant difference in duration of postoperative analgesia and dynamic pain scores. But they found significant difference between VAS and quadriceps motor power, which indicates the potency of sensory block and quadriceps motor sparing in PENG block compared to FICB.
In 66 patients, Jadon et al.[15] compared suprainguinal FICB with PENG block for positioning for SA. They reported that the NRS score after 30 min of a block at rest with S-FICB was 4, whereas with PENG block, it was 3. NRS score with passive leg raise with S-FICB was 5, whereas with PENG block, it was 4, but they used a suprainguinal approach for FICB. Bhattacharya et al.[16] conducted a controlled study on 50 patients with fracture neck femur. Twenty-five patients from each arm of the study had a PENG block or FICB with 20 mL of 0.25% levobupivacaine. The author concluded that both FICB and PENG blocks are nearly equally effective, with PENG providing pain relief more quickly in patients with fractures of the neck of the femur. In our study, we found that PENG block provided better analgesic efficacy than fascia iliaca block. The strength of our study was that a good number of cases were analyzed in this study, a visual analog score was used to assess the pain which is a sensitive indicator of pain assessment, and double blinding was done in this study to reduce the bias. The hemodynamic response was also noted in this study.
Our study has a few limitations: first, postoperative analgesia and opioid consumption were not assessed. Second, assessing motor function in the postoperative period would have revealed quadriceps weakness. Third, only ASA PS classes I and II patients were included in this study.
CONCLUSION
PENG block is superior to fascia iliaca block in providing effective analgesia prior to positioning of patients posted for hip surgeries under SA.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Parker M, Johansen A. Hip fracture. BMJ. 2006;333:27–30. doi: 10.1136/bmj.333.7557.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kowark A, Rossaint R, Coburn M. General versus spinal anesthesia for the elderly hip fractured patient. Curr Opin Anaesthesiol. 2019;32:116–9. doi: 10.1097/ACO.0000000000000679. [DOI] [PubMed] [Google Scholar]
- 3.Neuman MD, Silber JH, Elkassabany NM, Ludwig JM, Fleisher LA. Comparative effectiveness of regional versus general anesthesia for hip fracture surgery in adults. Anesthesiology. 2012;117:72–92. doi: 10.1097/ALN.0b013e3182545e7c. [DOI] [PubMed] [Google Scholar]
- 4.Yun MJ, Kim YH, Han MK, Kim JH, Hwang JW, Do SH. Analgesia before a spinal block for femoral neck fracture: Fascia iliaca compartment block. Acta Anaesthesiol Scand. 2009;53:1282–7. doi: 10.1111/j.1399-6576.2009.02052.x. [DOI] [PubMed] [Google Scholar]
- 5.Morrison SR, Magaziner J, McLaughlin MA, Orosz G, Silberzweig SB, Koval KJ, et al. The impact of post-operative pain on outcomes following hip fracture. Pain. 2003;103:303–11. doi: 10.1016/S0304-3959(02)00458-X. [DOI] [PubMed] [Google Scholar]
- 6.Helmerhorst GT, Vranceanu AM, Vrahas M, Smith M, Ring D. Risk factors for continued opioid use one to two months after surgery for musculoskeletal trauma. J Bone Joint Surg Am. 2014;96:495–9. doi: 10.2106/JBJS.L.01406. [DOI] [PubMed] [Google Scholar]
- 7.Scurrah A, Shiner CT, Stevens JA, Faux SG. Regional nerve blockade for early analgesic management of elderly patients with hip fracture – A narrative review. Anaesthesia. 2018;73:769–83. doi: 10.1111/anae.14178. [DOI] [PubMed] [Google Scholar]
- 8.Curatolo M. Regional anesthesia in pain management. Curr Opin Anaesthesiol. 2016;29:614–9. doi: 10.1097/ACO.0000000000000353. [DOI] [PubMed] [Google Scholar]
- 9.Haines L, Dickman E, Ayvazyan S, Pearl M, Wu S, Rosenblum D, et al. Ultrasound-guided fascia Iliaca compartment block for hip fractures in the emergency department. J Emerg Med. 2012;43:692–7. doi: 10.1016/j.jemermed.2012.01.050. [DOI] [PubMed] [Google Scholar]
- 10.Girón-Arango L, Peng PW, Chin KJ, Brull R, Perlas A. Pericapsular nerve group (PENG) block for hip fracture. Reg Anesth Pain Med. 2018;43:859–63. doi: 10.1097/AAP.0000000000000847. [DOI] [PubMed] [Google Scholar]
- 11.Shariat AN, Hadzic A, Xu D, Shastri U, Kwofie K, Gandhi K, et al. Fascia lliaca block for analgesia after hip arthroplasty: A randomized double-blind, placebo-controlled trial. Reg Anesth Pain Med. 2013;38:201–5. doi: 10.1097/AAP.0b013e31828a3c7c. [DOI] [PubMed] [Google Scholar]
- 12.Kacha NJ, Jadeja CA, Patel PJ, Chaudhari HB, Jivani JR, Pithadia VS. Comparative study for evaluating efficacy of fascia iliaca compartment block for alleviating pain of positioning for spinal anesthesia in patients with hip and proximal femur fractures. Indian J Orthop. 2018;52:147–53. doi: 10.4103/ortho.IJOrtho_298_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sahoo RK, Jadon A, Sharma SK, Nair AS. Pericapsular nerve group (PENG) block for hip fractures: Another weapon in the armamentarium of anesthesiologists. J Anaesthesiol Clin Pharmacol. 2021;37:295–6. doi: 10.4103/joacp.JOACP_295_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Senthil KS, Kumar P, Ramakrishnan L. Comparison of pericapsular nerve group block versus fascia iliaca compartment block as postoperative pain management in hip fracture surgeries. Anesth Essays Res. 2021;15:352–6. doi: 10.4103/aer.aer_119_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jadon A, Mohsin K, Sahoo RK, Chakraborty S, Sinha N, Bakshi A. Comparison of supra-inguinal fascia iliaca versus pericapsular nerve block for ease of positioning during spinal anaesthesia: A randomised double-blinded trial. Indian J Anaesth. 2021;65:572–8. doi: 10.4103/ija.ija_417_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bhattacharya A, Bhatti T, Haldar M. ESRA19-0539 pericapsular nerve group block is it better than the rest for pain relief in fracture neck of femur? Reg Anesth Pain Med. 2019;44:A116. [Google Scholar]


