Abstract
Background
The impact of screen time on mental health, including depression, has attracted increasing attention from not only children and adolescents but also the elderly. Thus, we conducted a meta-analysis of cohort studies to evaluate the association between screen time and depression risk.
Methods
The PubMed, Embase, Web of Science, and China National Knowledge Infrastructure databases were searched for cohort studies up to May 2022, and the reference lists of the included studies were also retrieved. A random-effect model was used to estimate the combined effect size. Heterogeneity was assessed with the I2 statistic. Potential publication bias was evaluated using a funnel plot and Begg’s and Egger’s tests.
Results
The final analysis included 18 cohort studies with a combined total of 241,398 participants. The pooled risk ratio (RR) was 1.10 (95% confidence interval: 1.05–1.14), with significant heterogeneity (I2 = 82.7%, P < 0.001). The results of subgroup analyses showed that the pooled RRs varied according to geographic locations, gender, age group, screen time in the control group, depression at the baseline, and whether the study was conducted during the COVID-19 pandemic. No obvious evidence of publication bias was found.
Conclusion
This study indicates that screen time is a predictor of depressive symptoms. The effects of screen time on depression risk may vary based on the participant’s age, gender, location, and screen time duration. The findings could have important implications for the prevention of depression.
Keywords: screen time, depression, meta-analysis, mental health, epidemiology
1 Background
Depression is a common and disabling psychiatric condition worldwide (1). According to estimates of the Global Burden of Diseases (GBD), injuries, risk factors study, depressive disorders accounted for 170.8 million cases in 1990 and 279.6 million cases in 2019, representing a 63.7% increase in prevalence (2). Depressive etiology is complex and results from interactions between biological vulnerabilities and environmental factors (3). According to the GBD (2), depression has been among the three top causes of non-fatal health losses for the past 30 years. Furthermore, research shows that depression is expected to be the leading global cause of disability-adjusted life year by 2030 (4). Depressive and anxiety disorders account for between one-quarter and one-third of all primary healthcare visits worldwide, and the World Health Organization (WHO) has estimated that neuropsychiatric disorders account for 1.2 million deaths annually, not including suicides (5). Moreover, social crises such as the coronavirus disease 2019 (COVID-19) pandemic can also lead to an epidemic of depression. WHO estimated that the cases of the major depressive disorder increased by 53.2 million (27.6%) globally because of the COVID-19 pandemic in 2020 (6). As one of the most widespread diseases affecting human physical and mental health, depression is receiving increasing attention.
With the popularization of modern information and communication technology, time spent using screens on devices, such as mobile phones, laptops, tablets, computers, and televisions, is becoming a core component of daily life (7), online studying, or work. People’s use of display screen equipment (DSE) during their free time has substantially increased in recent years (8, 9). With the increased screen time, both sedentary behavior and exposure to radiofrequency electromagnetic fields (RF-EMF) increase (10). Poitras et al. (11) and Carson et al. (12) indicated that screen time is associated with unfavorable health outcomes, and Canada, Australia, and USA have developed the “Sedentary Behavior Guidelines” to provide guidance and motivate people to reduce their screen time (13–15). Several studies have indicated that increased screen time duration could be associated with lagged development (16), psychosocial symptoms (10, 17), obesity (18, 19), sleep disorders (20, 21), and cardiovascular disease (22, 23). Thus, active or passive screen use has become a common issue among both adolescents and adults.
The relationship between screen time and depression remains controversial, and the biological mechanisms underlying this possible association are unclear. Some studies have reported an independent and interactive relationship between screen time and physical activity (21, 23–26). Tremblay et al. (27) suggested that, independent of physical activity levels, screen time-based sedentary behaviors were associated with an increased risk of various physiological and psychological problems. Furthermore, previous studies indicated that RF-EMF exposure may increase the risk of headaches, fatigue, sleep problems, chronic tinnitus, and depression (10, 28). Liu et al. (7) and Wang et al. (29) conducted meta-analyses in 2015 and 2019, respectively, to investigate the relationship between screen time-based sedentary behavior and depression. Although screen time is the time spent using devices with display screens (30), some studies have combined DSE use with other behaviors requiring low energy expenditure, such as sitting, driving, and reading, when defining the total duration of sedentary behavior, which should also be given attention. Considering the influence of RF-EMF on psychological problems, we summarized the available evidence and performed a meta-analysis of longitudinal studies to investigate the effects of screen time on depression risk. To achieve our goal, we applied the patients, intervention, comparison, and outcome (PICO) framework as follows: human being (P), time spent on screen-based equipment (I), no or little time spent on screen-based equipment (C), and increased depression prevalence (O).
2 Methods
2.1 Literature search strategy
This meta-analysis was conducted following the checklist of the Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines (31) and the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) statement (Supplementary File 1) (32). We systematically searched the PubMed, Embase, Web of Science, and China National Knowledge Infrastructure (CNKI) databases from their inception to May 2022 for studies describing an association between screen time and depression risk regardless of language or publication status. We used the following keywords: “screen time,” “video game,” “computer use,” “watching television,” “television view,” “internet use,” “electronic game,” “smartphone use,” “tablets,” or “iPads” in combination with “depression” or “depressive symptom” as search terms. In addition, all listed references were reviewed.
2.2 Inclusion and exclusion criteria
Studies were included if they fulfilled the following criteria: (1) the exposure of interest was screen time, (2) the outcome of interest was depression, (3) the study design was longitudinal, and (4) provided risk estimates such as hazard ratios (HR), relative risks (RR), or odds ratios (OR) with corresponding 95% confidence intervals (CIs) or sufficient data to calculate them. Studies were excluded if they were as follows: (1) publications that were not full reports, (2) duplicate studies, (3) studies on screen time addiction, (4) studies with inadequate information to calculate risk estimates, or (5) studies reporting time spent on other behaviors as well, causing difficulty in separating only screen time. Two reviewers (QZ and DY) independently reviewed all identified studies by title and abstract or full text. Disagreements were resolved through consultation with a third reviewer (CW).
2.3 Data extraction
The following information was extracted for each included study: first author’s name, publication year, study source, country, follow-up years, participants’ age range or mean age at the baseline, participants’ gender, sample size, screen equipment, depression measurement, depression definition, depression at baseline, study period, source of participates, screen time measurement, screen time in exposure group, screen time in the control group, depression at the baseline or adjusted, adjusted covariates, and effect estimates with their corresponding 95% CIs. Data extraction was conducted independently by two authors (JZG and QZ). Interobserver agreement was assessed using Cohen’s kappa (κ), and any disagreements were resolved by discussion with a third author (ZL).
2.4 Quality assessment
The methodological quality of the included studies was independently assessed by two reviewers (LL and GZ) using the Newcastle–Ottawa Scale (NOS) (33), which assesses the quality of cohort studies. The NOS includes eight items grouped into categories of selection, comparability, and outcome. Each study is assigned a score ranging between 0 and 9, and NOS scores over six indicate relatively high quality, five and six indicate medium quality, and less than five indicate low quality.
2.5 Statistical analysis
The RR was considered the common measure of the association between screen time and depression. The ORs were transformed into RRs using the formula where P0 indicates the incidence of the outcome of interest in the non-exposed group (34) and then synthesized with the RRs and the HRs into pooled RRs. The multivariable-adjusted RRs were preferentially pooled when such estimates were reported. If no adjusted analysis was available, the unadjusted estimate would be pooled. A fixed-effect model was applied when heterogeneity was not detected; otherwise, a random-effect model was used to summarize RRs for the association between screen time and depression. For further assessment of the association between screen time and depression risk, a subgroup analysis was conducted to explore sources of potential heterogeneity and examine the robustness of the primary results. This difference among subgroups was tested using meta-regression analysis (STATA “metareg” command). In sensitive analysis, we conducted a leave-one-out analysis to observe the magnitude of influence on the pooled RR of each study. Statistical heterogeneity among studies was evaluated using I2 statistics where values of 25, 50, and 75% represented the cutoff points for low, moderate, and high degrees of heterogeneity, respectively. Potential publication bias was evaluated using a funnel plot and Begg’s and Egger’s tests.
3 Results
3.1 Literature search
Figure 1 shows all steps and reasons for study exclusion. The process of screening studies on databases retrieved 7,329 studies in total, of which 3,558 were from the Web of Science, 2,102 were from PubMed, 894 were from Embase, and 775 were from the CNKI. After eliminating reviews and duplicate publications, 2,924 articles were excluded. After screening studies by titles and abstracts, 51 remained. At the full-text review stage, 28 articles were excluded for having a cross-sectional design. Of the remaining 23 longitudinal studies, five provide insufficient data for calculating risk estimates. Ultimately, 18 studies were included in the meta-analysis.
FIGURE 1.
Flow chart of study selection.
3.2 Study characteristics
Table 1 and Supplementary File 2 show the characteristics of the 18 included studies (35–52). Overall, the studies included 241,398 individuals, with sample sizes ranging from 435 (51) to 100,517 (49). All included studies were observational studies. Half were conducted in Europe (35, 40, 44, 45, 47, 49–52), while five (38, 41, 42, 46, 48) and four (36, 37, 39, 43) were in Asia and North America, respectively. Two studies (43, 46) only included female participants, while four (36, 44, 45, 47) reported the results for male and female participants, respectively. Most of the included studies had been published since 2010, with only one study published in 2009 (41). The follow-up durations ranged from 2 (48, 52) to 144 months (51). Only one study (46) used a physician’s diagnosis or medication history as the assessment tool for depression, while the others used self-report questionnaires or scales. Eleven studies (35–38, 41, 44–46, 49–51) excluded baseline cases of depression, while seven (39, 40, 42, 43, 47, 48, 52) studies did not. In all included studies, screen time duration was based on self-report. Table 2 shows the results of the quality assessment. Based on NOS scores, 14 studies (35–39, 41–46, 49–51) were of moderate or high quality, and four (40, 47, 48, 52) were of weak quality.
TABLE 1.
Characteristics of included studies in the meta-analysis.
| First author | Study name | Country | Sample size | Age at baseline (years) | Gender | Study period | Screen equipment | Depression measurement | Depression at baseline | Follow-up time (months) | Covariates adjustment |
| Primack et al. (41) | Add Health | America | 4,142 | Mean 21.8 ± 1.82 | M/F | General | TV, videocassettes, computer games | CES-D | Excluded | 84 | Sex, age, race, ethnicity, maternal educational level, the participants’ marital status and highest level of educational attainment at follow-up |
| Lucas et al. (46) | the Nurses’ Health Study | USA | 49,821 | Range 30–55 | F | General | TV | Both depression diagnosis and use of antidepressants | Excluded | 120 | Age, time interval, current postmenopausal hormonal use, body mass index, marital status, involvement in a social or community group, smoking status, total energy intake, coffee intake, reported diagnosis of diabetes mellitus, cancer, myocardial infarction or angina, high blood pressure, rheumatoid arthritis, osteoarthritis, asthma, emphysema, categories of television watching, categories of physical activity, physical limitations in 1992, five-item Mental Health Index score in 1992 |
| Thomée et al. (44) | None | Sweden | 4,156 | Range 20–24 | M/F | General | Mobile phone | Two items from Prime-MD | Excluded | 12 | Relationship status, educational level, and occupation |
| Thomée et al. (45) | None | Sweden | 4,163 | Range 20–24 | M/F | General | Computer | Two items from Prime-MD | Excluded | 12 | Relationship status, educational level, and occupation |
| Grøntved et al. (51) | EYHS | Danish | 435 | Mean 15.6 ± 0.4 | M/F | General | TV and computer | MDI | Excluded | 144 | Age at baseline, follow-up time, sex, parental education level, parental marital status, smoking status, and alcohol intake in adolescence, and with school id treated as a random effect, BMI in adolescence, cardiorespiratory fitness in adolescence |
| Sui et al. (38) | ACLS | America | 4,802 | Range 18–80; mean 48.4 ± 9.8 | M/F | General | TV | CES-D | Excluded | 464 | Age, gender, education, marital status, employment status, current smoker, body mass index, diabetes, and MVPA (hours/week) |
| Padmapriya et al. (43) | GUSTO | Asia | 1,144 | Mean 30.7 ± 5.1 | F | During pregnancy | TV | EPDS | Included | 17 | Age, education, working during pregnancy, household income, smoking history, parity during pregnancy, and pregnancy BMI |
| Wu et al. (39) | China | 2,521 | Mean 18.43 ± 0.96 | M/F | General | Video; computer, TV/video programs | CES-D | Included | 14 | Sex, age, residential background, BMI, perceived family economy, sleep quality, smoking, alcohol intake, exercise after school and physical activity | |
| Khouja et al. (40) | the Avon Longitudinal Study of Parents and Children, a UK-based prospective cohort study | UK | 1,869 | 16 | M/F | General | TV, computer, texting | CIS-R | Included | 24 | Sex, maternal age, anxiety at age 15, maternal anxiety and depression, maternal education, parental socioeconomic position, also adjusted for child IQ, parental conflict, presence of the child’s father, number of people living in the child’s home, bullying and family TV use in early life, time spent alone (weekdays or weekends, as applicable) |
| Liu et al. (37) | China | 3,396 | Range 14–24; mean 18.3 ± 1.7 | M/F | General | Mobile phone | BDI | Excluded | 8 | Age, sex, and other sociodemographics with significant associations with LTMPU at baseline; lifestyle practice and health conditions with significant associations with LTMPU at baseline | |
| Zink et al. (42) | H&H | USA | 2,525 | Range 13–16; mean 14.6 | M/F | General | TV, computer/ videogame |
RCADS | Included | 12 | Demographic characteristics of sex, age, race, ethnicity, and highest parental education, SES, BMI percentile based on self-reported height and weight using the age- and sex-normed CDC standardized guideline, baseline Major Depressive Disorder, baseline computer/videogame use, baseline television viewing |
| Choi et al. (49) | Phenotypic and genomic data from over 100,000 UK Biobank participants | British | 100,517 | Range 18+ | M/F | General | TV, computer | PHQ-9 | Excluded | 96 | Participant characteristics (sex, age, assessment center), sociodemographic factors (socioeconomic deprivation, employment status, household income, completion of higher education, urbanicity, household size), and physical health factors (BMI and reported physical illness or disability) |
| Meyer et al. (48) | the COVID-19 and Well-being Study | USA | 2,327 | Range 18+ | M/F | During COVID-19 pandemic | Screen not specific | BDI | Included | 2 | Age and sex, public health guidelines, time point (nine time points; weeks 0–8), and the interaction of time with each factor |
| Sarris et al. (35) | the UK Biobank | UK | 31,343 | Range 37–73; mean 56.7 ± 8.1 | M/F | General | TV, computer | An item from PHQ-9 | Excluded | 120 | Age, gender, ethnicity, social deprivation, education, and BMI |
| Ayuso-Mateos et al. (52) | the Edad con Salud project | Spain | 1,103 | Range 18+ mean 54.8 ± 16.4 | M/F | During COVID-19 pandemic | Screen not specific | CIDI | Excluded | 2 | Age, sex, education level, whether the participant lived alone (both before and during the lockdown), whether the participant had co-habited/was co-habiting with a relative isolated by COVID-19, whether the participant had been/was concerned about a relative/friend infected by COVID-19, whether the participant had been infected with COVID-19 and its severity, whether the participant had enough quietness at home to get proper rest, whether the house-hold economic situation had worsened due to the COVID-19 emergency, whether the participant had been unemployed due to the COVID-19 emergency, time a day spent in front of screens during the lockdown (working and non-working), pre- and post-measure levels of physical activity |
| Kandola et al. (47) | the Millennium Cohort Study | UK | 7,701 | 11 | M/F | General | Video games, social media and leisure-time internet use | sMFQ | Included | 36 | Gender, socioeconomic position (household income), baseline emotional symptoms, self-reported maternal history of a depression or anxiety diagnosis, the self-reported experience of bullying, self-reported physical activity, and standardized, BMI |
| Liu et al. (36) | MABC | China | 2,490 | 0 | M/F | General | TV, electronic products (mobile phones, tablets, computers and others) | SDQ | Excluded | 48 | Age, gender, number of siblings, delivery model, birth weight, maximum educational level of parents, family income, passive smoking, outdoor activities |
| Pimenta et al. (50) | the SUN Project | Spanish | 12,691 | Mean 36.7 ± 11.5 | M/F | General | TV, computer | DSM-IV | Excluded | 21 | Gender, marital status, years of university education, working hours, living status, hanging out with friends, smoking, physical activity, total energy intake, Mediterranean diet score, baseline self-perception of competitiveness, anxiety, and dependence levels, baseline BMI, use of tranquilizers or anxiolytics, insomnia, sleeping hours |
USA, the United States; UK, the United Kingdom; F, female; M, male; Add Health, the National Longitudinal Survey of Adolescent Health; EYHS, the Danish cohorts of the European Youth Heart Study; ACLS, Aerobics Center Longitudinal Study; GUSTO, the growing up in Singapore toward healthy outcomes; H&H, the Happiness and Health study; MABC, the Ma’anshan Birth Cohort prospective cohort study; SUN, the “Seguimiento Universidad de Navarra” project; TV, television; CES-D, the Center for Epidemiological Studies Depression scale; Prime-MD, Primary care evaluation of mental disorders; MDI, the Major Depression Inventory; EPDS, the Edinburgh Postnatal Depression Scale; CIS-R, self-administered, computerized version of the revised Clinical Interview Schedule; BDI, the Beck Depression Inventory; RCADS, the Revised Children’s Anxiety and Depression Scale; PHQ-9, the Patient Health Questionnaire-9; CIDI, the Chinese version of the computerized Composite International Diagnostic Inventory; sMFQ, short Moods and Feelings Questionnaire; SDQ, the Strengths and Difficulties Questionnaire; DSM-IV, the Diagnostic and Statistical Manual of Mental Disorders; BMI, body mass index; SES, socioeconomic status; MVPA, moderate and vigorous physical activity; LTMPU, long-time mobile phone use; CDC, the Centers for Disease Control and Prevention; SES, socioeconomic status; COVID-19, coronavirus disease 2019; IQ, intelligence quotient.
TABLE 2.
Quality assessment of included cohort studies.
| Original studies | Selection | Comparability | Outcome | Total score | |||||
| (1) Representa-tiveness of the exposed cohort | (2) Selection of the non-exposed cohort | (3) Ascertainment of exposure | (4) Demonstration that outcome of interest was not present at start of study | (1) Comparability of cohorts on the basis of the design or analysis | (1) Assessment of outcome | (2) Was follow-up long enough for outcomes to occur | (3) Adequacy of follow up of cohorts | ||
| Primack et al. (41) | 1 | 1 | 0 | 1 | 2 | 0 | 1 | 1 | 7 |
| Lucas et al. (46) | 0 | 1 | 0 | 1 | 2 | 0 | 1 | 1 | 6 |
| Thomée et al. (44) | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 5 |
| Thomée et al. (45) | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 5 |
| Grøntved et al. (51) | 0 | 1 | 0 | 1 | 2 | 0 | 1 | 0 | 5 |
| Sui et al. (38) | 1 | 1 | 0 | 1 | 2 | 0 | 0 | 0 | 5 |
| Padmapriya et al. (43) | 1 | 1 | 0 | 0 | 2 | 0 | 0 | 1 | 5 |
| Wu et al. (39) | 1 | 1 | 0 | 0 | 2 | 0 | 0 | 1 | 5 |
| Khouja et al. (40) | 1 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | 4 |
| Liu et al. (26) | 1 | 1 | 0 | 1 | 2 | 0 | 0 | 1 | 6 |
| Zink et al. (42) | 1 | 1 | 0 | 0 | 2 | 0 | 0 | 1 | 5 |
| Choi et al. (49) | 1 | 1 | 0 | 1 | 2 | 0 | 1 | 1 | 7 |
| Meyer et al. (48) | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 1 | 4 |
| Sarris et al. (35) | 1 | 1 | 0 | 1 | 2 | 0 | 1 | 0 | 6 |
| Ayuso-Mateos et al. (52) | 1 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | 4 |
| Kandola et al. (47) | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 3 |
| Liu et al. (36) | 1 | 1 | 0 | 1 | 2 | 0 | 0 | 1 | 6 |
| Pimenta et al. (50) | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 6 |
3.3 Quantitative synthesis
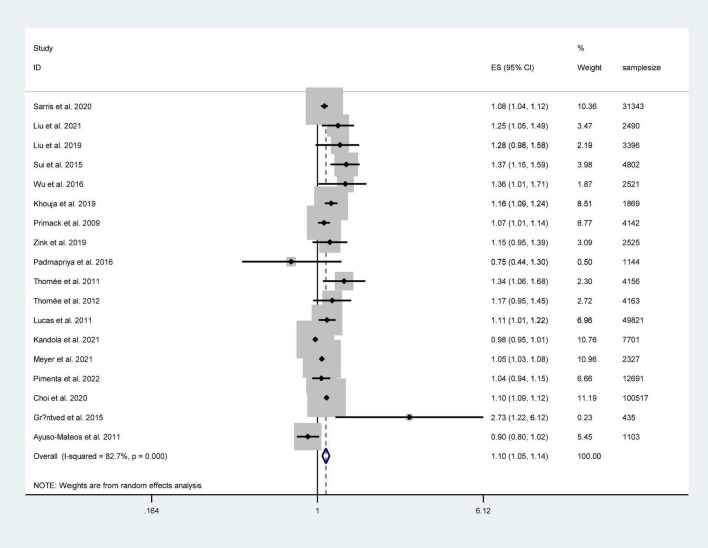
Figure 2 shows the pooled results from the random-effect model. Among these studies, 12 reported a positive relationship between screen time and depression risk. The pooled RR was 1.10 (95% CI: 1.05–1.14). The results showed a positive association between screen time and depression risk with a high level of heterogeneity (I2 = 82.7%, P < 0.001).
FIGURE 2.
Forest plot of the association between screen time and the risk of depression.
3.4 Subgroup analysis
Subgroup analyses were conducted by study location, age, gender, sample size, study quality, depression at baseline, depression definition, follow-up time, screen equipment, whether during the COVID-19 pandemic, screen time in the control group, and physical activity controlled for or absent in the models (Table 3). When stratified by gender, the results showed a positive association between screen time and depression in female participants (RR = 1.15, 95% CI: 1.01–1.31, I2 = 76.2%); however, this association was not statistically significant in male participants (RR = 1.12, 95% CI: 0.89–1.42, I2 = 77.4%). Screen time was significantly associated with an increased risk of depression in participants who watched television (RR = 1.13, 95% CI: 1.06–1.21, I2 = 65.0%) and used mobile phones (RR = 1.13, 95% CI: 1.01–1.25, I2 = 57.7%). A significant association between screen time and increased depression risk was observed among participants from Asia (RR = 1.24, 95% CI: 1.07–1.43, I2 = 21.7%). The pooled results of studies that excluded baseline depression in their analyses suggested a significantly positive association between screen time and depression risk (RR = 1.11, 95% CI: 1.06–1.16, I2 = 66.0%).
TABLE 3.
Subgroup analysis of odd ratios for the association between screen time and depression.
| No of studies | RR (95% CI) | I2 (%) | P-value for heterogeneity | P-value between groups | ||
| Study location | 0.648 | |||||
| Asia | 4 | 1.24 (1.07, 1.43) | 21.7 | 0.280 | ||
| North America | 9 | 1.07 (1.01, 1.14) | 89.4 | <0.001 | ||
| Europe | 5 | 1.11 (1.04, 1.18) | 67.7 | 0.015 | ||
| During COVID-19 pandemic | 0.101 | |||||
| Not | 16 | 1.12 (1.07, 1.18) | 82.6 | <0.001 | ||
| Yes | 2 | 0.98 (0.85, 1.14) | 83.2 | 0.015 | ||
| Depression at baseline | 0.530 | |||||
| Excluded | 12 | 1.11 (1.06, 1.16) | 66.0 | 0.001 | ||
| Included | 6 | 1.07 (1.00, 1.15) | 85.4 | <0.001 | ||
| Sample size | 0.221 | |||||
| <5,000 | 13 | 1.14 (1.07, 1.22) | 73.4 | <0.001 | ||
| >5,000 | 5 | 1.06 (1.00, 1.13) | 92.5 | <0.001 | ||
| Study quality | 0.287 | |||||
| Low quality | 4 | 1.03 (0.96, 1.10) | 90.6 | <0.001 | ||
| Medium quality | 12 | 1.17 (1.09, 1.25) | 56.8 | 0.008 | ||
| High quality | 2 | 1.10 (1.06, 1.12) | 0 | 0.397 | ||
| Follow-up time | 0.580 | |||||
| <60 months | 12 | 1.09 (1.03, 1.15) | 79.4 | <0.001 | ||
| >60 months | 6 | 1.11 (1.06, 1.16) | 64.2 | 0.016 | ||
| Screen time in the control group | 0.037 | |||||
| Continuous | 4 | 1.05 (1.01, 1.09) | 64.8 | 0.036 | ||
| ≤1 h/day | 7 | 1.12 (1.06, 1.18) | 50.3 | 0.060 | ||
| >1 h/day | 4 | 1.22 (1.09, 1.36) | 0 | 0.722 | ||
| Physical activity adjusted | ||||||
| Yes | 8 | 1.11 (1.01, 1.22) | 83.4 | 0.001 | 0.774 | |
| No | 10 | 1.10 (1.06, 1.14) | 68.3 | <0.001 | ||
| Sex | 0.867 | |||||
| Mix | 12 | 1.10 (1.06, 1.14) | 74.6 | <0.001 | ||
| Female | 7 | 1.15 (1.01, 1.31) | 76.2 | 0.001 | ||
| Male | 5 | 1.12 (0.89, 1.42) | 77.4 | 0.004 | ||
| Gender | 0.429 | |||||
| 0–20 | 7 | 1.18 (1.04, 1.34) | 86.0 | <0.001 | ||
| 20–44 | 8 | 1.08 (1.05, 1.12) | 61.0 | 0.012 | ||
| >44 | 3 | 1.09 (0.92, 1.30) | 88.4 | <0.001 | ||
| Screen equipment | 0.689 | |||||
| Screen not specific | 6 | 1.06 (1.00, 1.13) | 70.5 | 0.005 | ||
| Using mobile phone | 4 | 1.13 (1.01, 1.25) | 57.7 | 0.069 | ||
| Watching TV | 8 | 1.13 (1.06, 1.21) | 65.0 | 0.006 | ||
| Using computer | 8 | 1.09 (0.99, 1.20) | 89.1 | <0.001 | ||
3.5 Sensitivity analysis
Sensitivity analysis was adopted to identify the potential sources of heterogeneity in the association between screen time and depression risk. This helped us to examine the influence of various exclusions on the combined RRs and test the stability of the quantitative synthesis results. The pooled RRs ranged from 1.09 (95% CI: 1.05–1.14) to 1.11 (95% CI: 1.06–1.16) when one study was omitted. The leave-one-out analysis indicated that none of the individual studies significantly influenced the overall results.
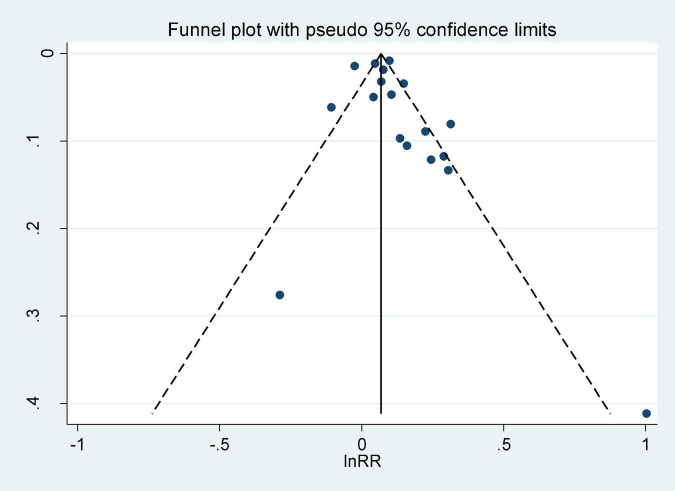
3.6 Publication bias
Visual inspection of the funnel plot did not reveal any significant asymmetry (Figure 3). Egger’s and Begg’s tests showed no obvious publication bias across studies (Egger’s test t = 1.10, P = 0.272; Begg’s test z = 1.08, P = 0.296).
FIGURE 3.
Funnel plot for studies of screen time in relation to the risk of depression.
4 Discussion
We conducted a meta-analysis of 18 longitudinal studies to investigate the association between screen time and depression risk. The pooled results showed that screen time was associated with an increased risk of depression with an RR value of 1.10 (95% CI: 1.05–1.14; I2 = 82.7%).
All included studies were observational, with few conducting experimental validations, and the research value of observational studies will be affected if they are not rigorously designed. Experimental studies may provide an important proof of concept for intervention efficacy; however, they can sometimes be limited by factors, such as ethical or experimental conditions (53, 54). Although high heterogeneity was observed in the meta-analysis, subgroup and meta-regression analyses showed that study location, whether depression was excluded at baseline, screen time in the control group, and study quality could explain the potential heterogeneity. Heterogeneity moderately decreased when grouped by age and screen time category; thus, in addition to screen time duration, future studies should investigate the influence of screen time on different age groups and the effects of different screen mediums on mental health. Heterogeneity declined significantly as study quality improved. When studies that did not exclude depression at baseline were excluded, heterogeneity decreased to 54%. The original study’s design had a significant impact on the results, and future studies should consider study design rigor. In the subgroup analysis by screen equipment, watching television and using mobile phones increased the incidence of depression.
In the subgroup based on age, the association between screen time and depression was not statistically significant in the elders. Wang et al. (55) found that the elders who reported internet use had lower depression levels compared with those who did not. Another study on different types of internet use and depressive symptoms indicated that using the internet for social contact and entertainment decreased depression scores in the elderly, but when using the internet for learning, working, or commercial activity, the effect of relieving depressive symptoms disappeared (56). Elders spend more time online for recreational and leisure activities (56, 57). However, one study of internet use and mental health suggested that internet use affects mental health and increases the incidence of depressive symptoms in elders who may even experience feelings of technological panic (58). Future research should consider technological fear as an important influencing factor.
In the subgroup analysis by gender, screen time was significantly associated with an increased risk of depression in women; however, this association was not statistically significant in men. In general, screen time is considered a sedentary behavior, and this finding was consistent with previous meta-analyses on the association between sedentary behavior and mental health and screen time-based sedentary behavior on depression (29, 59). One explanation might be that women were more likely to be influenced by intimate social relationships that contribute to depression and thus would experience greater depressive symptoms than men. Kawachi et al. (60), Wirback et al. (61), and Altemus et al. (62) found that gender differences in support derived from social network participation may partly account for the higher prevalence of psychological distress among women compared with men, and smaller social networks, fewer close relationships, and lower perceived adequacy of social support have been linked to depressive symptoms (60–62). When screen time increases, women may have less time to communicate with others, which could result in developing fewer intimate relationships and smaller social networks, ultimately leading to mental disorders, such as depression.
Subgroup stratification according to whether a study was conducted during the COVID-19 pandemic showed that while screen time increased the risk of depression during the normal period, the opposite association was found during the COVID-19 pandemic (52). This may be because watching television and using mobile phones or computers could relieve an individual’s negative mood during lockdown conditions. Most of the subgroup effects were statistically significant. The population from Asia was at a higher risk than those from North America or Europe. An investigation of sitting time trends in 27 countries found that time spent on sedentary behaviors may not be increasing in the European region (8), and among these countries, the prevalence of depression has decreased steadily.
Electronic devices have become an integral part of many people’s lives, even among retired adults who do not need to work or study. In our study, we observed a significant effect of screen time on depression in youth (aged 0–20 years), although heterogeneity was high. Our findings support limiting screen time for adolescents. The results regarding the effect of screen time on depression in the elderly were not statistically significant, and our findings did not confirm if the relationship was positive or negative. Insufficient information in the original studies and the wide age range of participants made it difficult to perform a more detailed age group study. Future studies should focus on the effect of age and analyze the effect of screen time on depression risk separately for different age groups. Notably, the results stratified by subgroup, whether the study was conducted during the COVID-19 pandemic, suggested that screen time may alleviate depressive symptoms during lockdowns. Thus, the government should encourage people to use electronic devices to distract themselves and relieve their negative emotions during lockdown situations.
The underlying mechanisms of the relationship between screen time and depression risk remain unclear. With the increasing prevalence of depression, depression prevention has become a widespread public health concern. Therefore, identifying modifiable risk factors to aid in depression prevention is an important task. Several hypotheses may explain the impact of screen time on depression. First, increased screen time led to curtailed physical activity, which has been beneficial for reducing depression risk (63, 64). However, when stratified by physical activity regardless of if it was adjusted, the pooled results still indicated that screen time was a risk factor for depression. Tremblay et al. (27) suggested that independent of physical activity levels, screen time-based sedentary behaviors are associated with increased depression risk. As sedentary behavior and physical activity are both common human experiences, future studies are needed to explore the relationship between both behaviors and depression. Second, screen time, such as watching television and using mobile phones or computers, has been associated with sleep disorders, which could lead to sleep problems and increase the risk of depression (46, 65). Third, according to the causal model of social networks and social supports, social ties have protective effects on mental health and direct communication helps individuals build intimacy (60). Screen time can cause a reduction in social interactions and narrow social networks, and a lack of social networks may lead to social solitude and lower perceived adequacy of social support; thus, such changes could result in depressive symptoms. Fourth, RF-EMF may provide another explanation. With the rapid development and widespread use of electronic devices, health authorities have recognized the possible effects of long-term exposure to RF-EMF. Recent studies reported that RF-EMF may be linked to adverse health consequences, and several countries have made proposals to reduce the use of electronic devices. However, research findings on the relationship between EMFs and health problems have been inconsistent. Therefore, future studies should consider potential confounding or interactive effects, explore the underlying biological mechanism, and demonstrate an independent effect of screen time on depression risk.
4.1 Strengths and limitations
This meta-analysis highlights the synthesized effects of screen time on depression risk. First, our research was based on cohort studies, which provided much stronger and more sufficient evidence. Second, it included a total of 237,146 participants from seven countries across Europe, Asia, and North America. The large sample size and wide range of locations significantly increased the statistical power and generalizability of the findings on the association between screen time and depression risk. Third, no obvious publication bias was detected in our study, which indicates that the combined results are reliable and convincing overall. Finally, our study excluded mixed sedentary behavior and screen time that could not be separated.
Some of this study’s potential limitations should also be discussed. First, recall bias and measurement errors are unavoidable when using self-report questionnaires to assess screen time. Electronic devices, such as mobile phones, computers, and smart televisions, can record time spent using the device in detail, thereby allowing for screen time to be measured objectively and conveniently. Researchers should obtain as much detailed information as possible and use objective measurements in future studies. Second, although included studies had adjusted for confounding factors, some of the included studies did not adjust for potential confounders, such as age, gender, and physical activity level, which might influence the association between screen time and depression risk. Future studies should pay more attention to these important covariates and measure and adjust for key variables. Third, the information in the included original studies was limited; therefore, we were unable to conduct dose-response analyses. Objective measurements of screen time are recommended, so we can easily collect more definite and detailed information about exposure to screen time and further analyze the dose-response effects.
5 Conclusion
This meta-analysis demonstrates that screen time is likely to increase the risk of depression. The high heterogeneity may be the result of a less rigorous original study design across the included studies. The effects of screen time on depression risk may vary widely, and the determinants or the benefits of screen time were shown to differ based on duration and individual characteristics (e.g., age, gender, and location). Among young and female populations, screen time was found to significantly increase depression risk. Compared with less screen time, screen time exceeding 1 h/day was associated with a higher risk of depression. Our findings support the recommendations to limit the prolonged use of electronic devices. Objective measures are recommended to use in future studies to explore complex relationships and specific time constraints of screen time. Considering the increasing prevalence of depression in modern society and the increasing number of people exposed to screens for long periods, our findings have important implications for depression prevention.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
CW and LL conceived the study. GZ, HH, JZ, XK, SY, DY, and ZC were responsible for the collection and cleaning of the data and assisted in the writing of the manuscript. LL and QZ wrote the manuscript. LZ, YG, and ZL contributed to the review and revision of the study. CW was the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Science and Technology Research Project of Education Department of Jiangxi Province (GJJ190814).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.1058572/full#supplementary-material
The PRISMA checklist.
Details of included articles.
References
- 1.Whiteford H, Degenhardt L, Rehm J, Baxter A, Ferrari A, Erskine H, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global burden of disease study 2010. Lancet. (2013) 382:1575–86. 10.1016/S0140-6736(13)61611-6 [DOI] [PubMed] [Google Scholar]
- 2.Gbd 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the Global burden of disease study 2019. Lancet Psychiatry. (2022) 9:137–50. 10.1016/S2215-0366(21)00395-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Izaki Y. Depression among adolescents: clinical features and interventions. J Med Invest. (2021) 68:22–8. 10.2152/jmi.68.22 [DOI] [PubMed] [Google Scholar]
- 4.Lopez A, Mathers C. Measuring the global burden of disease and epidemiological transitions: 2002-2030. Ann Trop Med Parasitol. (2006) 100:481–99. 10.1179/136485906X97417 [DOI] [PubMed] [Google Scholar]
- 5.Mathers C, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. (2006) 3:e442. 10.1371/journal.pmed.0030442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Covid-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. (2021) 398:1700–12. 10.1016/S0140-6736(21)02143-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu M, Wu L, Yao S. Dose-response association of screen time-based sedentary behaviour in children and adolescents and depression: a meta-analysis of observational studies. Br J Sports Med. (2016) 50:1252–8. 10.1136/bjsports-2015-095084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Milton K, Gale J, Stamatakis E, Bauman A. Trends in prolonged sitting time among European adults: 27 country analysis. Prev Med. (2015) 77:11–6. 10.1016/j.ypmed.2015.04.016 [DOI] [PubMed] [Google Scholar]
- 9.Ten Broeke P, Olthof M, Beckers D, Hopkins N, Graves L, Carter S, et al. Temporal dynamics of sitting behavior at work. Proc Natl Acad Sci USA. (2020) 117:14883–9. 10.1073/pnas.2001284117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Redmayne M, Smith E, Abramson M. The relationship between adolescents’ well-being and their wireless phone use: a cross-sectional study. Environ Health. (2013) 12:90. 10.1186/1476-069X-12-90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Poitras V, Gray C, Janssen X, Aubert S, Carson V, Faulkner G, et al. Systematic review of the relationships between sedentary behaviour and health indicators in the early years (0-4 years). BMC Public Health. (2017) 17(Suppl. 5):868. 10.1186/s12889-017-4849-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carson V, Hunter S, Kuzik N, Gray C, Poitras V, Chaput J, et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth: an update. Appl Physiol Nutr Metab. (2016) 41(6 Suppl. 3):S240–65. 10.1139/apnm-2015-0630 [DOI] [PubMed] [Google Scholar]
- 13.Tremblay M, Carson V, Chaput J, Connor Gorber S, Dinh T, Duggan M, et al. Canadian 24-hour movement guidelines for children and youth: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. (2016) 41(6 Suppl. 3):S311–27. 10.1139/apnm-2016-0151 [DOI] [PubMed] [Google Scholar]
- 14.Virgara R, Phillips A, Lewis L, Richardson M, Maher C. Physical activity and screen time in outside school hours care services across Australia: current versus best practice. BMC Public Health. (2022) 22:680. 10.1186/s12889-022-13135-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hollman H, Updegraff J, Lipkus I, Rhodes R. Perceptions of physical activity and sedentary behaviour guidelines among end-users and stakeholders: a systematic review. Int J Behav Nutr Phys Act. (2022) 19:21. 10.1186/s12966-022-01245-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yu Y, Hsieh T, Lin G, Lee S, Huang C, Chen K. High levels of screen time were associated with increased probabilities of lagged development in 3-year-old children. Acta Paediatr. (2022) 111:1736–42. 10.1111/apa.16373 [DOI] [PubMed] [Google Scholar]
- 17.Niiranen J, Kiviruusu O, Vornanen R, Saarenpää-Heikkilä O, Paavonen E. High-dose electronic media use in five-year-olds and its association with their psychosocial symptoms: a cohort study. BMJ Open. (2021) 11:e040848. 10.1136/bmjopen-2020-040848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mitchell J, Rodriguez D, Schmitz K, Audrain-McGovern J. Greater screen time is associated with adolescent obesity: a longitudinal study of the BMI distribution from ages 14 to 18. Obesity (Silver Spring). (2013) 21:572–5. 10.1002/oby.20157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reyna-Vargas M, Parmar A, Lefebvre D, Azad M, Becker A, Turvey S, et al. Longitudinal associations between sleep habits, screen time and overweight, obesity in preschool children. Nat Sci Sleep. (2022) 14:1237–47. 10.2147/NSS.S363211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sakamoto N, Kabaya K, Nakayama M. Sleep problems, sleep duration, and use of digital devices among primary school students in Japan. BMC Public Health. (2022) 22:1006. 10.1186/s12889-022-13389-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hale L, Guan S. Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep Med Rev. (2015) 21:50–8. 10.1016/j.smrv.2014.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ford E, Caspersen C. Sedentary behaviour and cardiovascular disease: a review of prospective studies. Int J Epidemiol. (2012) 41:1338–53. 10.1093/ije/dys078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jingjie W, Yang L, Jing Y, Ran L, Yiqing X, Zhou N. Sedentary time and its association with risk of cardiovascular diseases in adults: an updated systematic review and meta-analysis of observational studies. BMC Public Health. (2022) 22:286. 10.1186/s12889-022-12728-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Feng Q, Zhang Q, Du Y, Ye Y, He Q. Associations of physical activity, screen time with depression, anxiety and sleep quality among Chinese college freshmen. PLoS One. (2014) 9:e100914. 10.1371/journal.pone.0100914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li X, Buxton O, Lee S, Chang A, Berger L, Hale L. Sleep mediates the association between adolescent screen time and depressive symptoms. Sleep Med. (2019) 57:51–60. 10.1016/j.sleep.2019.01.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu M, Zhang J, Hu E, Yang H, Cheng C, Yao S. Combined patterns of physical activity and screen-related sedentary behavior among Chinese adolescents and their correlations with depression, anxiety and self-injurious behaviors. Psychol Res Behav Manag. (2019) 12:1041–50. 10.2147/PRBM.S220075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tremblay M, LeBlanc A, Kho M, Saunders T, Larouche R, Colley R, et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. Int J Behav Nutr Phys Act. (2011) 8:98. 10.1186/1479-5868-8-98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Belyaev I, Dean A, Eger H, Hubmann G, Jandrisovits R, Kern M, et al. EUROPAEM EMF Guideline 2016 for the prevention, diagnosis and treatment of EMF-related health problems and illnesses. Rev Environ Health. (2016) 31:363–97. 10.1515/reveh-2016-0011 [DOI] [PubMed] [Google Scholar]
- 29.Wang X, Li Y, Fan H. The associations between screen time-based sedentary behavior and depression: a systematic review and meta-analysis. BMC Public Health. (2019) 19:1524. 10.1186/s12889-019-7904-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Diler F, Başkale H. The influence of sleep patterns and screen time on the sleep needs of infants and toddlers: a cross-sectional study. J Pediatr Nurs. (2022) 67:e201–7. 10.1016/j.pedn.2022.07.014 [DOI] [PubMed] [Google Scholar]
- 31.Stroup D, Berlin J, Morton S, Olkin I, Williamson G, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. (2000) 283:2008–12. 10.1001/jama.283.15.2008 [DOI] [PubMed] [Google Scholar]
- 32.Moher D, Liberati A, Tetzlaff J, Altman D. Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wells G, Shea B, O’Connell D. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Ottawa, ON: Ottawa Hospital Research Institute; (2011). [Google Scholar]
- 34.Zhang J, Yu K. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. (1998) 280:1690–1. 10.1001/jama.280.19.1690 [DOI] [PubMed] [Google Scholar]
- 35.Sarris J, Thomson R, Hargraves F, Eaton M, de Manincor M, Veronese N, et al. Multiple lifestyle factors and depressed mood: a cross-sectional and longitudinal analysis of the UK Biobank (N = 84,860). BMC Med. (2020) 18:354. 10.1186/s12916-020-01813-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu W, Wu X, Huang K, Yan S, Ma L, Cao H, et al. Early childhood screen time as a predictor of emotional and behavioral problems in children at 4 years: a birth cohort study in China. Environ Health Prev Med. (2021) 26:3. 10.1186/s12199-020-00926-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu S, Wing Y, Hao Y, Li W, Zhang J, Zhang B. The associations of long-time mobile phone use with sleep disturbances and mental distress in technical college students: a prospective cohort study. Sleep. (2019) 42:zsy213. 10.1093/sleep/zsy213 [DOI] [PubMed] [Google Scholar]
- 38.Sui X, Brown W, Lavie C, West D, Pate R, Payne J, et al. Associations between television watching and car riding behaviors and development of depressive symptoms: a prospective study. Mayo Clin Proc. (2015) 90:184–93. 10.1016/j.mayocp.2014.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wu X, Tao S, Zhang S, Zhang Y, Chen K, Yang Y, et al. Impact of screen time on mental health problems progression in youth: a 1-year follow-up study. BMJ Open. (2016) 6:e011533. 10.1136/bmjopen-2016-011533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Khouja J, Munafò M, Tilling K, Wiles N, Joinson C, Etchells P, et al. Is screen time associated with anxiety or depression in young people? Results from a UK birth cohort. BMC Public Health. (2019) 19:82. 10.1186/s12889-018-6321-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Primack B, Swanier B, Georgiopoulos A, Land S, Fine M. Association between media use in adolescence and depression in young adulthood: a longitudinal study. Arch Gen Psychiatry. (2009) 66:181–8. 10.1001/archgenpsychiatry.2008.532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zink J, Belcher B, Kechter A, Stone M, Leventhal A. Reciprocal associations between screen time and emotional disorder symptoms during adolescence. Prev Med Rep. (2019) 13:281–8. 10.1016/j.pmedr.2019.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Padmapriya N, Bernard J, Liang S, Loy S, Shen Z, Kwek K, et al. Association of physical activity and sedentary behavior with depression and anxiety symptoms during pregnancy in a multiethnic cohort of Asian women. Arch Womens Ment Health. (2016) 19:1119–28. 10.1007/s00737-016-0664-y [DOI] [PubMed] [Google Scholar]
- 44.Thomée S, Härenstam A, Hagberg M. Mobile phone use and stress, sleep disturbances, and symptoms of depression among young adults–a prospective cohort study. BMC Public Health. (2011) 11:66. 10.1186/1471-2458-11-66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Thomée S, Härenstam A, Hagberg M. Computer use and stress, sleep disturbances, and symptoms of depression among young adults–a prospective cohort study. BMC Psychiatry. (2012) 12:176. 10.1186/1471-244X-12-176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lucas M, Mekary R, Pan A, Mirzaei F, O’Reilly E, Willett W, et al. Relation between clinical depression risk and physical activity and time spent watching television in older women: a 10-year prospective follow-up study. Am J Epidemiol. (2011) 174:1017–27. 10.1093/aje/kwr218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kandola A, Owen N, Dunstan D, Hallgren M. Prospective relationships of adolescents’ screen-based sedentary behaviour with depressive symptoms: the Millennium cohort study. Psychol Med. (2021) 19:1–9. 10.1017/S0033291721000258 [DOI] [PubMed] [Google Scholar]
- 48.Meyer J, O’Connor J, McDowell C, Lansing J, Brower C, Herring M. High sitting time is a behavioral risk factor for blunted improvement in depression across 8 weeks of the COVID-19 pandemic in April-May 2020. Front Psychiatry. (2021) 12:741433. 10.3389/fpsyt.2021.741433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Choi K, Stein M, Nishimi K, Ge T, Coleman J, Chen C, et al. An exposure-wide and mendelian randomization approach to identifying modifiable factors for the prevention of depression. Am J Psychiatry. (2020) 177:944–54. 10.1176/appi.ajp.2020.19111158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pimenta A, Mendonça R, Lahortiga-Ramos F, Fernandez-Lazaro C, Martínez-González M, Sánchez-Villegas A. Sedentary behaviors and risk of depression in the Seguimiento Universidad de Navarra cohort: the SUN Project. Cadernos de Saúde Pública [online]. (2022) 38:e00076621. 10.1590/0102-311X00076621 [DOI] [Google Scholar]
- 51.Grøntved A, Singhammer J, Froberg K, Møller N, Pan A, Pfeiffer K, et al. A prospective study of screen time in adolescence and depression symptoms in young adulthood. Prev Med. (2015) 81:108–13. 10.1016/j.ypmed.2015.08.009 [DOI] [PubMed] [Google Scholar]
- 52.Ayuso-Mateos J, Morillo D, Haro J, Olaya B, Lara E, Miret M. Changes in depression and suicidal ideation under severe lockdown restrictions during the first wave of the COVID-19 pandemic in Spain: a longitudinal study in the general population. Epidemiol Psychiatr Sci. (2021) 30:e49. 10.1017/S2045796021000408 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 53.Liu Y, Liu X, Wang Y, Wang D, Ma P. [Interpretation of guidelines for controlling confounding factors and reporting results in causal inference studies]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. (2021) 33:113–6. 10.3760/cma.j.cn121430-20201127-00734 [DOI] [PubMed] [Google Scholar]
- 54.Sargeant J, Kelton D, O’Connor A. Study designs and systematic reviews of interventions: building evidence across study designs. Zoonoses Public Health. (2014) 61(Suppl. 1):10–7. 10.1111/zph.12127 [DOI] [PubMed] [Google Scholar]
- 55.Wang Y, Zhang H, Feng T, Wang H. Does internet use affect levels of depression among older adults in China? A propensity score matching approach. BMC Public Health. (2019) 19:1474. 10.1186/s12889-019-7832-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yang H, Zhang S, Zhang S, Xie L, Wu Y, Yao Y, et al. Internet use and depressive symptoms among older adults in China. Front Psychiatry. (2021) 12:739085. 10.3389/fpsyt.2021.739085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhang H, Wang H, Yan H, Wang X. Impact of internet use on mental health among elderly individuals: a difference-in-differences study based on 2016-2018 CFPS data. Int J Environ Res Public Health. (2021) 19:101. 10.3390/ijerph19010101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Xie L, Yang H, Lin X, Ti S, Wu Y, Zhang S, et al. Does the internet use improve the mental health of Chinese older adults? Front Public Health. (2021) 9:673368. 10.3389/fpubh.2021.673368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhang J, Yang S, Wang L, Han L, Wu X. The influence of sedentary behaviour on mental health among children and adolescents: a systematic review and meta-analysis of longitudinal studies. J Affect Disord. (2022) 306:90–114. 10.1016/j.jad.2022.03.018 [DOI] [PubMed] [Google Scholar]
- 60.Kawachi I, Berkman L. Social ties and mental health. J Urban Health. (2001) 78:458–67. 10.1093/jurban/78.3.458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Barnett P, Gotlib I. Psychosocial functioning and depression: distinguishing among antecedents, concomitants, and consequences. Psychol Bull. (1988) 104:97–126. 10.1037/0033-2909.104.1.97 [DOI] [PubMed] [Google Scholar]
- 62.Nolen-Hoeksema S. Sex differences in unipolar depression: evidence and theory. Psychol Bull. (1987) 101:259–82. [PubMed] [Google Scholar]
- 63.Rodriguez-Ayllon M, Cadenas-Sánchez C, Estévez-López F, Muñoz N, Mora-Gonzalez J, Migueles J, et al. Role of physical activity and sedentary behavior in the mental health of preschoolers, children and adolescents: a systematic review and meta-analysis. Sports Med. (2019) 49:1383–410. 10.1007/s40279-019-01099-5 [DOI] [PubMed] [Google Scholar]
- 64.Biddle S, Asare M. Physical activity and mental health in children and adolescents: a review of reviews. Br J Sports Med. (2011) 45:886–95. 10.1136/bjsports-2011-090185 [DOI] [PubMed] [Google Scholar]
- 65.Sun L, Li K, Zhang L, Zhang Y. Distinguishing the associations between evening screen time and sleep quality among different age groups: a population-based cross-sectional study. Front Psychiatry. (2022) 13:865688. 10.3389/fpsyt.2022.865688 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The PRISMA checklist.
Details of included articles.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.