Abstract
Female entertainment and sex workers (FESW) have high rates of alcohol and amphetamine-type stimulant (ATS) use, increasing risk for HIV/sexually transmitted infections (STI), and other negative outcomes. A prospective cohort of 1,198 FESW in a HIV/ATS use prevention intervention in Cambodia was assessed for alcohol and stimulant use disorders (AUD and SUD) using the Alcohol and Substance Use Involvement (ASSIST) scale. STI history was measured by self-report at baseline and at quarterly follow-up visits. Participants were asked if they had been diagnosed with an STI by a medical provider in the past 3 months. Marginal structural models were used to estimate joint effects of AUD and SUD on recent STI. At baseline, one-in-four screened AUD positive and 7% screened positive for SUD. At 18-months, 26% reported ≥ 1 recent STI. Accounting for time-varying and other known confounders, the adjusted odds ratio (AOR) for recent STI associated with AUD alone and SUD alone were 2.8 (95% CI: 1.5–5.1) and 3.5 (95% CI:1.1–11.3), respectively. The AOR for joint effects of AUD and SUD was 5.7 (95% CI:2.2–15.2). AUD and SUD are independently and jointly associated with greater odds of STI among Cambodian FESW. Further research is critical for understanding how AUD and SUD potentiate biological and behavioural pathways that influence STI acquisition and to inform HIV riskreduction interventions in FESW.
Keywords: Sexually transmitted infections, sex workers, drug users, sexual behaviour, women, risk factors
Introduction
While significant progress has been made in reducing the HIV epidemic in Cambodia,1 some populations remain at high risk, notably women working in the entertainment and sex work sectors.2,3 In Cambodia, women engaged in high-risk and transactional sex are a heterogeneous group working in variety of environments and venues, whom collectively can be referred to as female entertainment and sex workers (FESW). HIV prevalence in Cambodian female entertainment and sex workers (FESW) decreased from 23% in 2007 to 9% in 2009, which could be attributed in part to effective HIV prevention interventions, but also to increasing challenges associated with reaching women at increased risk of HIV infection.2,3 In 2008, the Cambodian sex work landscape underwent major changes with the implementation of new anti sex-trafficking and sexual exploitation laws, greatly impacting FESW. Following the passage and implementation of the ‘Law on Suppression of Human Trafficking and Sexual Exploitation’, brothel-based sex work was banned, and the most direct effect was on direct sex trade, which went ‘underground’, or women moved into indirect work.3,4 Brothels were closed, as transactional sex was illegal, and many women were forced to engage in ‘hidden’ sexual transactions in streets and parks or in entertainment venues, such as clubs and karaoke bars.
FESW have high rates of alcohol consumption and drug use, which can lead to increased sexual risks, exposure to violence, HIV and STI acquisition, and other negative health outcomes.5-7 In Cambodia, FESW frequently work in entertainment settings, including bars, clubs, beer gardens and karaoke venues, where alcohol consumption is prevalent.3,6,8 Alcohol is often part of sexual transactions and consumed by both FESW and their male clients before sexual intercourse.9-11 According to global literature, prevalence of daily alcohol consumption by FESW ranges from 12–78%.5 Alcohol use in FESW, especially before sex with clients, has been associated with negative outcomes, including unprotected sex, violence victimization and higher risk of HIV and STI acquisition.10,12-14 In previous studies, we found that self-reported unhealthy alcohol use was prevalent among Cambodian FESW: 24% reported being drunk for more than 20 days in the month prior to interview.2 In another more recent study conducted in Cambodia, unhealthy alcohol use, including risky drinking and alcohol-use disorders,15 was reported by 85% of the FESW and by 47% of their male sex clients.8 The high prevalence of unhealthy alcohol consumption in sex work venues could potentially fuel transmission of HIV and STI in Cambodia.
Research has also identified drug use and, in particular, amphetamine-type stimulant (ATS) use as a serious problem associated with HIV risk among FESW in Southeast Asia16-21 which threatens to reverse downward trends in HIV infection rates in the region. ATS use has been associated with risky sexual behaviors and incident HIV and STI in many groups, including FESW.22-26 In Cambodia, our group found 26.3% of FESW reported recent ATS use (last 3 months).21 ATS use among Cambodian FESW was also associated with having a higher number of sex partners, incident STIs and experience of violence.21,27 In Vietnam, hepatitis C, HIV, and STI-risk increased with the use of non-injection drugs, specifically amphetamine-type stimulants.17,28-31 In China, drug-using FESWs had substantially higher HIV and STI prevalence.32-34
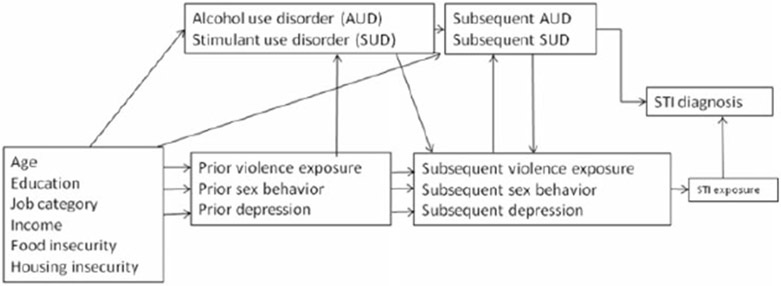
Taken together, alcohol consumption and ATS use have important negative health consequences for FESW, including increased sexual risk behaviors and experiencing violence victimization, which increase exposure to HIV and STI acquisition. Concomitant risk factors including depression, exposure to violence, and characteristics of sex work venue have been suggested as potential mediators in the relationship between substance use, and risky sexual behaviors and risk of STI acquisition.21,27,35 Furthermore, risk factors such as depression and exposure to violence are associated with having a history of prior alcohol consumption or drug use.36,37 Most studies have looked at the effects of alcohol and drug use on HIV and STI transmission separately and without considering concomitant risk factors. We hypothesized that both time-varying levels of alcohol and ATS use are subject to time-varying confounding and likely affected by prior exposure (Figure 1). Therefore, unbiased estimation of the joint effects of the alcohol and ATS use on STI acquisition likely requires the use of joint marginal structural models. We examined the joint effects of alcohol and ATS use on recent STI infection in FESW in 10 provinces in Cambodia. We hypothesized that FESW with alcohol use disorder (AUD) will have higher rates of recent STI infection and that concomitant ATS use disorder (SUD) will further increase rates of STI infection.
Figure 1.
Causal diagram for the effects of alcohol and ATS use disorders on STI diagnosis.
Methods
Study setting
Data for the present study were obtained from 1,198 FESW enrolled in a cluster randomized stepped-wedge trial of an HIV and ATS use prevention intervention conducted in 10 provinces in Cambodia (Phnom Penh, Battambang, Banteay Meanchey, Siem Reap, Kandal, Kampong Spueu, Kampong Chhnang, Kampong Cham, Sihanouk, and Pailin). The Cambodian Integrated HIV and Drug Prevention Implementation program (CIPI) study was implemented within an existing HIV-prevention program targeting FESW called “SMARTgirl”.38 Detailed descriptions of both the study and intervention protocol are described elsewhere.39,40 Data were collected at outcome assessment visits conducted at baseline, and every 6-months for a period of 18 months from June 2013 to November 2016. The study received ethical approvals from the Cambodian National Ethical Committee, University of California at San Francisco, University of New Mexico and FHI360.
Study population, recruitment and data collection
Eligibility criteria for study participation were: (1) being biologically female; (2) age ≥18 years; (3) reporting ≥2 different sexual partners and/or transactional sex within the last month; (4) understanding spoken Khmer language; and (5) able to provide voluntary informed consent. Participants were paid US$4 at the 6- and 12-month follow up visits, and US$8 at the 18-month visit. Remuneration of US$2 was offered for transportation, and refreshments and condoms were provided at all visits.
Participants were recruited in multiple venues including SMARTgirl clubs, entertainment establishments (karaoke bars, beer gardens, nightclubs, massage parlors), as well as other sex work venues (brothels, streets, parks and guest houses). Trained outreach workers described the study, answered questions, and invited interested women to attend the local study site to participate in the study. Eligibility screening was conducted at the local study site, usually a SMARTgirl Club. The intervention consisted of a 16-week conditional cash transfer and aftercare program delivered to women who screened positive for an ATS use disorder (i.e., moderate or high risk on this ASSIST and were positive on urine toxicology screening (ATS Tox+).39 A recruitment target of 120 women per province was set for baseline with an expected intervention eligibility rate of 25%. The study was powered to detect between small and medium effect sizes according to Cohen’s guidelines.40,41
A total of 1198 women completed the baseline assessment and 257 enrolled in the intervention. Up to 600 FESW were resampled from the baseline (preintervention) sample for follow-up assessments conducted at 6-months, 12-months, and 18-months. All intervention participants and convenience sample of 300 non-intervention participants were targeted for follow-up assessments. All assessment visits were included in the present analysis.
Measures
At baseline, women completed an interviewer-administered structured behavioural questionnaire covering socio-demographic factors including age, number of years of school completed and marital status. Women were also asked to report the number of days working as brothel-based, freelance, or entertainment-based sex workers in the past month. The primary sex work venue was then categorized as entertainment-based or brothel/freelance. Women were asked whether or not their workplace required drinking alcohol with customers. Sexual risk measures included number of sexual partners and number of new sexual partners in the past 3 months. Participants also provided a self-collected vaginal swab to measure prostate specific antigen (PSA) using OneStep ABAcard® p30 rapid PSA test (Abacus Diagnostics, Inc., West Hills, CA) as an indicator of recent unprotected vaginal sex.42 Inconsistent condom use was measured by self-report for the last 3 paying and non-paying sexual partners as well as a positive PSA test. For the purposes of multivariate modeling, condom use with paying partners was classified as ‘always protected’ for women reporting no paying partners. Women were also asked if they or their partner used ATS prior to or during sex with the last 3 partners. Alcohol and ATS use disorders (AUD and SUD) were assessed using the World Health Organization (WHO) Alcohol and Substance Use Involvement (ASSIST) scale.43 The ASSIST scales for alcohol use disorder and stimulant use disorder had scores ranging from 0–27, and were categorized into the following risk categories, (low risk: <4, moderate risk: 4–26, and high risk: 27). In the present analysis AUD and SUD were defined as high risk (27+) vs. low or moderate risk (0–26). Recent STI was self-reported and measured as “Has a doctor, nurse, or other health care provider told you in the last 3 months that you had a Sexually Transmitted Disease (STD) or infection?” Self-reported HIV status was assessed separately from self-reported STI and HIV test results were made by linking identifiers with the national surveillance data.44 The WHO Multi-Country Study of Women’s Health and Domestic Violence was used to assess recent exposure to sexual and physical violence.45 Psychological distress was assessed with the K10 Kessler Psychological Distress scale.46 Measures of economic wellbeing included self-reported monthly income, debt, housing instability, and food insecurity. Food insecurity was defined as reporting “sometimes”, “always”, or “usually” to “having no food to eat of any kind in your household because of lack of money or resources to get food in the last 3 months” (adapted from47). Housing instability was measured as “in the past 3 months, how often were you worried about having a place to stay for you or your family because of lack of resources or money for housing?” (adapted from48). Women were asked if they had a debt they were working to pay off. Participants completed the behavioral questionnaire and the PSA testing at baseline and six-month follow-up assessments.
Statistical analyses
Behavioral and health characteristics were assessed with frequencies and percentages for categorical variables and medians and interquartile ranges for continuous variables. Comparisons between groups were performed with the Chi-square test for categorical items and the Kruskal-Wallis test for continuous items.
Three logistic regression models were estimated: crude, adjusted, and a weighted marginal structural model (MSM). The marginal structural model was used to estimate the joint effects of AUD and SUD on self-reported STI in the past 3 months. We accounted for the impact of potential informative censoring occurring when participants were lost-to-follow-up due to reasons related to the study using inverse probability of censoring weighting methods.49 Censoring and probability weights were constructed using both baseline fixed characteristics (age, years of education, and sex work venue) and time-varying covariates (AUD, SUD, condom use with paying partners, positive PSA test result, psychological distress, income, required drinking alcohol in the workplace, ATS use with sex partners, number of sex partners, food insecurity, housing instability, and violence victimization). All visits were included and current and lagged values of each factor were used to construct weights. Censoring and probability weights were constructed separately for each outcome (AUD and SUD), and then multiplied together to create a joint weight using a two-step process.50 Weights were stabilized to reduce the range of values and were centered around 1.3.
All models accounted for clustering by province and adjusted for intervention participation. The crude model estimated the association between AUD and SUD and self-reported STI in the past 3 months. The adjusted model accounted for baseline condom use with paying partners, psychological distress, age, sex work venue, income, food insecurity, housing instability, number of sex partners, drug use with sex partners, work place drinking, PSA test results, recent sexual or physical violence victimization, and months followed in the study. Multivariable models excluded observations without complete case information. Missing data were relatively rare (<1%) on STI reports, baseline condom use with paying partners, housing instability, drug use with sex partners, and PSA test results. Complete case data were available for AUD, SUD, psychological distress, age, sex work venue, income, food insecurity, number of sex partners, and recent sexual or physical violence victimization. All analyses were conducted in Stata version 15, College Station, TX.
Results
Participants were recruited between November 2013, and July 2015. Follow-up data collection ended in November 2016. Of 1,559 women screened, 1,428 (92%) were eligible and 1,198 of those (84%) completed a baseline assessment. Follow-up assessments were completed by 596 participants at 6-months, 544 at 12-months, and 556 at 18-months.
At baseline 18% of the 1,198 FESW enrolled in the study reported a recent STI. Twenty-six percent reported ≥1 recent STIs during the 18-month follow-up. Most participants were ≥30 years of age (79%), did not have a primary partner (68%), currently worked in an entertainment venue (81%), and reported a median monthly income of US$200 (Interquartile Range [IQR] = 120, 300) (Table 1). Overall, women reported a median of seven male sex partners (IQR = 4, 17) in the past 3 months and a median of 4 (IQR = 1, 9) new partners (Table 2). Self-reported condom use was common with paying partners (77%) but less with non-paying partners (19%). At baseline, 25% and 7% screened positive for AUD and SUD respectively. Half (54%) reported that their job required drinking alcohol with customers. Approximately 18% of the women had moderate or severe risk of psychological distress. The proportion of STI reported during follow-up ranged from 23% in women without stimulant use disorder to 38% in those with both AUD and SUD. Women who were older, had lower monthly income, tested HIV positive, had debt, worked in brothels or freelance, and had AUD were significantly more likely to report a recent STI. In addition, women who tested positive for PSA, experienced food insecurity and housing instability were more likely to report a recent STI (Table 2).
Table 1.
Sociodemographic and workplace characteristics of FESW in 10 provinces in Cambodia (N = 1198).
| Total (n = 1198) |
STI reported at any study visit (n = 313) |
No STI report at any study visit (n = 885) |
|||||
|---|---|---|---|---|---|---|---|
| Characteristic | N | % | N | % | N | % | p-Value |
| Median age (in years) | 26 | (22,30) | 27 | (23,30) | 26 | (22,30) | 0.02 |
| Marital status | 0.10 | ||||||
| Married/Living together | 382 | 31.9 | 103 | 32.9 | 279 | 31.5 | |
| Separated/Divorced/Widowed | 494 | 41.2 | 140 | 44.7 | 354 | 40.0 | |
| Single | 322 | 26.9 | 70 | 22.4 | 252 | 28.5 | |
| Education (years of school completed) | 0.14 | ||||||
| None | 194 | 16.2 | 58 | 18.5 | 136 | 15.4 | |
| Primary (1–6) | 634 | 52.9 | 171 | 54.6 | 463 | 52.3 | |
| Secondary (≥7) | 370 | 30.9 | 84 | 26.8 | 286 | 32.3 | |
| Main sex work venue (past month) | 0.04 | ||||||
| Entertainment | 967 | 80.7 | 240 | 76.7 | 727 | 82.2 | |
| Brothel/freelance (eg., park, street, guest house) | 231 | 19.3 | 73 | 23.3 | 158 | 17.9 | |
| Currently work for employer, boss, manager, or supervisor (yes) | 872 | 72.8 | 234 | 74.8 | 638 | 72.1 | 0.36 |
| Monthly Income (US$) | <0.01 | ||||||
| <100 | 258 | 21.5 | 87 | 27.8 | 171 | 19.3 | |
| >100–250 | 534 | 44.6 | 127 | 40.6 | 407 | 46.0 | |
| >250 | 406 | 33.9 | 99 | 31.6 | 307 | 34.7 | |
| Have debt | 548 | 45.7 | 176 | 56.2 | 372 | 42.0 | <0.01 |
| Workplace requires drinking alcohol with customers (yes) | 642 | 53.6 | 172 | 55.0 | 470 | 53.1 | 0.57 |
Table 2.
Sexual behaviour, substance use, and health characteristics of FESW in 10 provinces in Cambodia (N = 1198).
| Total (n = 1198) |
STI reported at any study visit (n = 313) |
No STI report at any study visit (n = 885) |
|||||
|---|---|---|---|---|---|---|---|
| Characteristic | N | % | N | % | N | % | p-Value |
| Number of male sex partners (past 3 months) | |||||||
| Median | 7 | 4–17 | 6 | 4–14 | 8 | 4–18 | 0.06 |
| ≤3 | 279 | 23.3 | 71 | 22.7 | 208 | 23.5 | 0.11 |
| 4–15 | 607 | 50.7 | 173 | 55.3 | 434 | 49.0 | |
| ≥16 | 312 | 26.0 | 69 | 22.0 | 243 | 27.5 | |
| Number of new male sex partners (past 3 months) | |||||||
| Median | 4 | 1–9 | 3 | 1–7 | 4 | 2–10 | <0.01 |
| 0 | 181 | 15.1 | 56 | 17.9 | 125 | 14.1 | <0.01 |
| 1–5 | 582 | 48.6 | 166 | 53.0 | 416 | 47.0 | |
| ≥6 | 435 | 36.3 | 91 | 29.1 | 344 | 38.9 | |
| Prostate Specific Antigen result positive | 338 | 28.2 | 105 | 33.7 | 233 | 26.5 | 0.02 |
| HIV antibody result positive | 75 | 6.3 | 30 | 9.6 | 45 | 5.1 | <0.01 |
| Consistent condom use with paying partners;a (past 3 months) | 862 | 76.6 | 235 | 81.9 | 627 | 74.8 | 0.02 |
| Consistent condom use with non-paying partners;a (past 3 months) | 113 | 18.5 | 35 | 18.6 | 78 | 18.5 | 0.97 |
| ATS use with any sex partner in past 3 months (yes) | 257 | 21.8 | 77 | 24.6 | 180 | 20.5 | 0.13 |
| ATS use disorder (SUD) | 0.09 | ||||||
| Low (<4) | 790 | 65.9 | 200 | 63.9 | 590 | 66.7 | |
| Moderate (4–26) | 322 | 26.9 | 82 | 26.2 | 240 | 27.1 | |
| High (≥27) | 86 | 7.2 | 31 | 9.9 | 55 | 6.2 | |
| Alcohol use disorder (AUD) | <0.01 | ||||||
| Low (<11) | 292 | 24.4 | 60 | 19.2 | 232 | 26.2 | |
| Moderate (11–26) | 611 | 51.0 | 154 | 49.2 | 457 | 51.6 | |
| High (≥27) | 295 | 24.6 | 99 | 31.6 | 196 | 22.2 | |
| Psychological distress | 0.42 | ||||||
| No or low risk | 708 | 59.7 | 174 | 56.5 | 534 | 60.8 | |
| Mild risk | 260 | 21.9 | 74 | 24.0 | 186 | 21.2 | |
| Moderate risk | 112 | 9.4 | 34 | 11.0 | 78 | 8.9 | |
| Severe risk | 107 | 9.0 | 26 | 8.4 | 81 | 9.2 | |
| Food insecurity (past 3 months) | <0.01 | ||||||
| Never | 837 | 69.9 | 196 | 62.6 | 641 | 72.4 | |
| Rarely | 228 | 19.0 | 67 | 21.4 | 161 | 18.2 | |
| Sometimes | 66 | 5.5 | 20 | 6.4 | 46 | 5.2 | |
| Often/always | 67 | 5.6 | 30 | 9.6 | 37 | 4.2 | |
| Housing instability (past 3 months) | 0.03 | ||||||
| Never | 546 | 45.6 | 121 | 38.7 | 425 | 48.1 | |
| Rarely | 201 | 16.8 | 55 | 17.6 | 146 | 16.5 | |
| Sometimes | 144 | 12.0 | 44 | 14.1 | 100 | 11.3 | |
| Often/always | 306 | 25.6 | 93 | 29.7 | 213 | 24.1 | |
| Experience of sexual or physical violence in the past 3 months (yes) | 564 | 47.1 | 154 | 49.2 | 410 | 46.3 | 0.38 |
Condom use with paying partners was calculated for all participants who reported a paying partner (N = 1125); Condom use with non-paying partners was calculated for all participants who reported a non-paying partner (N = 610).
Crude estimates for the odds of reporting a recent STI with screening positive for AUD alone was 2.3 (95% CI: 1.3–4.0) (Table 3). The crude OR for SUD alone was 2.1 (95% CI: 1.1—4.0). The OR for the joint effect of AUD and SUD was 3.5 (95% CI: 2.1–5.6). After accounting for several known confounders including sexual risk behaviors, the adjusted odds ratio (AOR) for recent STI associated with AUD alone was 2.1 (95% CI: 1.3–3.4) and the AOR ratio for SUD alone was 1.8 (95% CI: 0.9–3.7). The AOR for the joint effect of AUD and SUD was 2.5 (95% CI: 1.6–4.0).
Table 3.
Crude, adjusted, and weighted estimates for joint effects of alcohol and ATS substance use disorder on STI acquisition among 1198 FESW in 10 provinces in Cambodia, 2013–2016.
| Crude |
Adjusteda |
Weighted |
|||||
|---|---|---|---|---|---|---|---|
| Alcohol use disorder | ATS use disorder | OR | 95% CI | AOR | 95% CI | AOR | 95% CI |
| 0–26 | 0–26b | 1.0 | 1.0 | 1.0 | |||
| 27+ | 2.1 | 1.1–4.0 | 1.8 | 0.9–3.7 | 3.5 | 1.1–11.3 | |
| 27+ | 0–26 | 2.3 | 1.3–4.0 | 2.1 | 1.3–3.4 | 2.8 | 1.5–5.1 |
| 27+ | 3.5 | 2.1–5.6 | 2.5 | 1.6–4.0 | 5.7 | 2.2–15.2 | |
| p-value for interaction term | 0.42 | 0.55 | 0.61 | ||||
Accounted for baseline condom use with paying partners, psychological distress, age, sex work venue, income, food insecurity, housing instability, number of sex partners, drug use with sex partners, work place drinking, prostate specific antigen results, recent sexual or physical violence victimization, intervention participation, and months followed in study.
Referent group.
In the joint marginal structural model, the AOR for recent STI associated with AUD alone was 2.8 (95% CI: 1.5–5.1). The AOR for SUD alone was 3.5 (95% CI: 1.1–11.3). The AOR for the joint effect of AUD and SUD was 5.7 (95% CI: 2.2–15.2). A test for trend in proportion reporting recent STI over the 18-month follow-up was not statistically significant. Tests for interaction in crude, adjusted and marginal structural models were not statistically significant.
Discussion
AUD and SUD were independently and jointly associated with greater odds of self-reported STI among Cambodian FESW even after accounting for sexual risk-taking behaviors, and concomitant factors including psychological distress, exposure to violence, and characteristics of sex work venue. Women with both AUD and SUD had the greatest odds of reporting a STI during follow-up. We found a strong association between AUD and STI in the absence of SUD, which support previous findings.10,12 The increase in the AOR for recent STI associated with AUD alone, SUD alone, and the joint effect of AUD and SUD in the MSM compared to the unadjusted odds, suggests the presence of time-dependent confounding. To our knowledge, this study is among the first to observe independent as well as joint effects of AUD and SUD on over five-fold greater odds of self-reported STI after adjusting for time-dependent confounding.
Many studies have shown that alcohol use is associated with prevalent and incident HIV and STI infection as well as risky sexual behaviors, such as unprotected sex, multiple partnerships and transactional sex.51-53 Also consistent with other studies is the magnitude of the association between SUD and STI.25 Unlike the present study, these studies are limited by the use of standard adjustment approaches. In our previous study, ATS use was associated with a five-fold increased risk of STI acquisition among Cambodia FESW.21 In the present study, the AOR for SUD in the absence of AUD was 3.5. ATS use has been shown to increase libido, lower inhibitions, enhance sexual pleasure and prolong sexual intercourse.54-56 ATS has also been associated with risky sexual behaviors including high number of sex partners, unprotected sex, and sexual intercourse with more risky partners; all increasing the risk of HIV and STI acquisition.21,56-59 In our qualitative study, Cambodian FESW reported that clients intoxicated with alcohol or ATS often requested unprotected sex.4
Although we found no evidence for an interaction between AUD and SUD on STI prevalence, women having both AUD and SUD had a higher risk of STI than women with only AUD or SUD or neither disorder. A possible explanation for the lack of interaction between AUD and SUD is that women who worked in entertainment venues represented the majority of the study sample and are more likely to drink alcohol and use ATS infrequently compared to brothel-based and freelance sex workers.4 Because brothel-based and freelance sex workers represented only 19% of the study sample, we may have failed to detect an interaction effect.
Our study has some limitations to consider when interpreting the results. Data on recent STI and alcohol and ATS use, were self-reported and may be subject to recall and social-desirability bias. As a result, the estimates of risk may be conservative and biased towards the null. However, self-report of alcohol and ATS use has been shown to be accurate in this population.8,60 The proportion of women reporting any STI at baseline was 18% and similar to our previous study where 15.4% of the FESW screened positive to STI tests (Chlamydia trachomatis and Neisseria gonorrhoeae).21 Secondly, because participants were not sampled probabilistically our results may not be generalizable to the larger population of FESW in Cambodia. Nevertheless, efforts were made to recruit women from multiple sex work venues in ten provinces in Cambodia, increasing the representativeness of our sample.
Despite these limitations, our findings are strengthened by the longitudinal study design and high retention rates at follow-up assessments. Adding to the strengths is the use of MSM methods, which allow for improved adjustment for confounding than standard adjustment approaches that can introduce biases.61 The MSM method assumes no unmeasured confounders and that the marginal structural model for the effect of AUD and SUD on STI is correctly specified. We also assume the models for inverse probability weights and censoring weights are correctly specified. Although strong assumptions, standard statistical methods also require the same assumptions in order to make a causal inference. The advantage of MSM methods over traditional methods is that this approach accounts for time dependent confounding by covariates that are affected by previous measurements of outcomes and covariates.50
ATS and alcohol use are critical public health issues with significant health consequences for FESW, including risky sexual behaviors and violence victimization, which increase exposure to STI, including HIV acquisition. The burden of unhealthy alcohol use and ATS use disorders in this vulnerable population demonstrates the importance of better understanding their influence on HIV and STI transmission to improve our fight against these epidemics. Our results also highlight the need to develop more comprehensive HIV and STI prevention programs addressing both alcohol and other drug use problems, but also other risks such as mental health issues, gender-based violence and economic insecurity that affect FESW. Given the independent effects of both AUD and SUD also observed in our study, prevention programs targeting FEWS may also benefit from integration of prevention interventions designed to specifically address the risks/harms associated with alcohol and stimulant use in this population. In Cambodia, women who work in entertainment venues are more likely to drink alcohol, whereas women working “freelance” or in brothels are more likely to use stimulants,3 supporting the need for interventions tailored to specific sex work settings and social milieus. Sex work context and risk have shifted among young FESW in Phnom Penh, following implementation of anti-prostitution and anti-trafficking laws. Compared to previous studies, the present study found a lower prevalence of sexual risk and HIV infection. Women engaging more directly in transactional sex have become harder to sample and access.3 Future prevention research and programs need to consider how new policies and demographic changes in FESW impact HIV transmission.
Our findings also underscore the need for further research to understand how AUD and SUD potentiate biological as well as behavioral vulnerability for STI acquisition in FESW. The findings suggest the presence of time-dependent confounding which was accounted for by the marginal structural model. Finally, there is a need to explore how interventions integrating evidence-based AUD and SUD treatments can optimize the effectiveness of existing HIV prevention activities for FESW.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Footnotes
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Vun MC, Fujita M, Rathavy T, et al. Achieving universal access and moving towards elimination of new HIV infections in Cambodia. J Int AIDS Soc 2014; 17: 18905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Couture M-C, Sansothy N, Sapphon V, et al. Young women engaged in sex work in Phnom Penh, Cambodia, have high incidence of HIV and sexually transmitted infections, and amphetamine-type stimulant use: new challenges to HIV prevention and risk. Sex Transm Dis 2011; 38: 33–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Page K, Stein E, Sansothy N, et al. Sex work and HIV in Cambodia: trajectories of risk and disease in two cohorts of high-risk young women in Phnom Penh, Cambodia. BMJ Open 2013; 3: e003095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maher L, Mooney-Somers J, Phlong P, et al. Selling sex in unsafe spaces: sex work risk environments in Phnom Penh, Cambodia. Harm Reduct J 2011; 8: 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li Q, Li X and Stanton B. Alcohol use among female sex workers and male clients: an integrative review of global literature. Alcohol Alcohol 2010; 45: 188–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Semple SJ, Pitpitan EV, Chavarin CV, et al. Prevalence and correlates of hazardous drinking among female sex workers in 13 Mexican Cities. eScholarship, University of California, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Do VT, Ho HT, Nguyen TM, et al. Sexual violence and the risk of HIV transmission in sexual partners of male injecting drug users in Tien Du district, Bac Ninh province of Vietnam. Health Care Women Int 2018; 39: 404–414. [DOI] [PubMed] [Google Scholar]
- 8.Couture M-C, Page K, Sansothy N, et al. High prevalence of unhealthy alcohol use and comparison of self-reported alcohol consumption to phosphatidylethanol among women engaged in sex work and their male clients in Cambodia. Drug Alcohol Depend 2016; 165: 29–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pitpitan EV, Wagner KD, Goodman-Meza D, et al. Context matters: the moderating role of bar context in the association between substance use during sex and condom use among male clients of female sex workers in Tijuana, Mexico. AIDS Behav 2013; 17: 2577–2587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang B, Li X, Stanton B, et al. Alcohol use, unprotected sex, and sexually transmitted infections among female sex workers in China. Sex Transm Dis 2010; 37: 629–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang C, Yang C, Latkin C, et al. Factors associated with drinking alcohol before visiting female sex workers among men in Sichuan province, China. AIDS Behav 2013; 17: 568–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen Y, Li X, Zhang C, et al. Alcohol use and sexual risks: use of the alcohol use disorders identification test (AUDIT) among female sex workers in China. Health Care Women Int 2013; 34: 122–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chiao C, Morisky DE, Rosenberg R, et al. The relationship between HIV_sexually transmitted infection risk and alcohol use during commercial sex episodes: Results from the study of female commercial sex workers in the Philippines. Substance Use Misuse 2006; 41: 1509–1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang C, Li X, Stanton B, et al. Alcohol use and client-perpetrated sexual violence against female sex workers in China. Psychol Health Med 2013; 18: 330–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kriston L, Hölzel L, Weiser A-K, et al. Meta-analysis: are 3 questions enough to detect unhealthy alcohol use? Ann Intern Med 2008; 149: 879–888. [DOI] [PubMed] [Google Scholar]
- 16.Gorbach PM, Sopheab H, Chhorvann C, et al. Changing behaviors and patterns among Cambodian sex workers: 1997–2003. J Acquir Immune Defic Syndr 2006; 42: 242–247. [DOI] [PubMed] [Google Scholar]
- 17.Ho HT, Le GM and Dinh TT. Female sex workers who use amphetamine-type stimulants (ATS) in three cities of Vietnam: use and sexual risks related to HIV/AIDS. Glob Public Health 2013; 8: 552–569. [DOI] [PubMed] [Google Scholar]
- 18.McKetin R, Kozel N, Douglas J, et al. The rise of methamphetamine in Southeast and East Asia. USA: Carfax Publishing, Taylor & Francis Group, 2008. [DOI] [PubMed] [Google Scholar]
- 19.Sopheab H, Morineau G, Neal JJ, et al. Sustained high prevalence of sexually transmitted infections among female sex workers in Cambodia: high turnover seriously challenges the 100% condom use programme. BMC Infect Dis 2008; 8: 167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.UNODC. The Challenge of synthetic drugs in East and South-East Asia: trends and patterns of amphetamine-type stimulants and new psychoactive substances. A report from the Global SMART Programme, UNODC, 2017. [Google Scholar]
- 21.Couture M-C, Evans JL, Sothy NS, et al. Correlates of amphetamine-type stimulant use and associations with HIV-related risks among young women engaged in sex work in Phnom Penh, Cambodia. Drug Alcohol Depend 2012; 120: 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Buavirat A, Page-Shafer K, van Griensven GJP, et al. Risk of prevalent HIV infection associated with incarceration among injecting drug users in Bangkok, Thailand: case-control study. Br Med J 2003; 326: 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Melbye K, Khamboonruang C, Kunawararak P, et al. Lifetime correlates associated with amphetamine use among Northern Thai men attending STD and HIV anonymous test sites. Drug Alcohol Depend 2002; 68: 245–253. [DOI] [PubMed] [Google Scholar]
- 24.Witte SS, Altantsetseg B, Aira T, et al. Reducing sexual HIV/STI risk and harmful alcohol use among female sex workers in Mongolia: a randomized clinical trial. AIDS Behav 2011; 15: 1785–1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Meade CS, Watt MH, Sikkema KJ, et al. Methamphetamine use is associated with childhood sexual abuse and HIV sexual risk behaviors among patrons of alcohol-serving venues in Cape Town, South Africa. Drug Alcohol Depend 2012; 126: 232–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beyrer C, Razak MH, Jittiwutikarn J, et al. Methamphetamine users in Northern Thailand: changing demographics and risks for HIV and STD among treatment-seeking substance abusers. Int J STD AIDS 2004; 15: 697–704. [DOI] [PubMed] [Google Scholar]
- 27.Draughon Moret JE, Carrico AW, Evans JL, et al. The impact of violence on sex risk and drug use behaviors among women engaged in sex work in Phnom Penh, Cambodia. Drug Alcohol Depend 2016; 161: 171–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Le L-VN, Nguyen TA, Tran HV, et al. Correlates of HIV infection among female sex workers in Vietnam: injection drug use remains a key risk factor. Drug Alcohol Depend 2015; 150: 46–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Le L-VN, O’Connor S, Tran TH, et al. High hepatitis C virus infection among female sex workers in Viet Nam: strong correlation with HIV and infection drug use. Western Pacific Surveillance and Response. Vol. 10. Geneva: World Health Organization. 2019, pp.9–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nguyen TV, Khuu N, Van Truong PH, et al. Correlation between HIV and sexual behavior, drug use, trichomoniasis and candidiasis among female sex workers in a Mekong Delta province of Vietnam. AIDS Behav 2009; 13: 873–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tran TN, Detels R, Long HT, et al. HIV infection and risk characteristics among female sex workers in Hanoi, Vietnam. J Acquir Immune Defic Syndr 1999; 39: 581–586. [PMC free article] [PubMed] [Google Scholar]
- 32.Xu JJ, Smith MK, Chu J, et al. Dynamics of the HIV epidemic in Southern China: sexual and drug-using behaviours among female sex workers and male clients in Yunnan. Int J STD AIDS 2012; 23: 670–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hail-Jares K, Choi S, Duo L, et al. Occupational and demographic factors associated with drug use among female sex workers at the China–Myanmar border. Drug Alcohol Depend 2016; 161: 42–49. [DOI] [PubMed] [Google Scholar]
- 34.Zhu J, Yuan R, Hu D, et al. HIV prevalence and correlated factors of female sex workers and male clients in a border region of Yunnan province, China. Int J STD AIDS 2018; 29: 424–434. [DOI] [PubMed] [Google Scholar]
- 35.Shen H, Zou H, Huang S, et al. Depression and HIV risk behaviors among female sex workers in Guangdong, China: a multicenter cross-sectional study. BioMed Res Int 2016; 2016: 6986173–6986178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hankin A, Smith LS, Daugherty J, et al. Correlation between intimate partner violence victimization and risk of substance abuse and depression among African-American women seen in an urban emergency department. West J Emerg Med 2010; 11: 252–256. [PMC free article] [PubMed] [Google Scholar]
- 37.Holden KB, McKenzie R, Pruitt V, et al. Depressive symptoms, substance abuse, and intimate partner violence among pregnant women of diverse ethnicities. J Health Care Poor Underserved 2012; 23: 226–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.FHI360/PRASIT. SMARTgirl program review: providing HIV/AIDS prevention and care for entertainment workers. Reporting period October 2008-Kime 2010. Phnom Penh, 2010. [Google Scholar]
- 39.Carrico AW, Nil E, Sophal C, et al. Behavioral interventions for Cambodian female entertainment and sex workers who use amphetamine-type stimulants. J Behav Med 2016; 39: 502–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Page K, Stein ES, Carrico AW, et al. Protocol of a cluster randomised stepped-wedge trial of behavioural interventions targeting amphetamine-type stimulant use and sexual risk among female entertainment and sex workers in Cambodia. BMJ Open 2016; 6: e010854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cohen J Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: L. Erlbaum Associates, 1988. [Google Scholar]
- 42.Evans JL, Couture M-C, Stein ES, et al. Biomarker validation of recent unprotected sexual intercourse in a prospective study of young women engaged in sex work in Phnom Penh, Cambodia. Sex Transm Dis 2013; 40: 462–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Humeniuk R, Ali R, Babor TF, et al. Validation of the alcohol, smoking and substance involvement screening test (ASSIST). Addiction 2008; 103: 1039–1047. [DOI] [PubMed] [Google Scholar]
- 44.Muth S, Len A, Evans JL, et al. HIV treatment Cascade among female entertainment and sex workers in Cambodia: impact of amphetamine use and an HIV prevention program. Addict Sci Clin Pract 2017; 12: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Garcia-Moreno C, Heise L, Jansen HAFM, et al. Public health. Violence against women. Science (New York) 2005; 310: 1282–1283. [DOI] [PubMed] [Google Scholar]
- 46.Kessler RC, Barker PR, Colpe LJ, Epstein JF, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry 2003; 60: 184–189. [DOI] [PubMed] [Google Scholar]
- 47.Coates J, Swindale A and Bilinsky P. Household Food Insecurity Access Scale (HFIAS) for measurement of household food access: indicator guide (v. 3). Washington, DC, www.fao.org/fileadmin/user_upload/eufao-fsi4dm/doc-training/hfias.pdf (accessed 23 September 2020). [Google Scholar]
- 48.Centers for Disease Control and Prevention. Behavioral risk factor surveillance system. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, 2012. [Google Scholar]
- 49.Cole SR and Hernán MA. Constructing inverse probability weights for marginal structural models. Am J Epidemiol 2008; 168: 656–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fewell Z, Hernan MA, Wolfe F, et al. Controlling for time-dependent confounding using marginal structural models. Stata J 2004; 4: 402–420. [Google Scholar]
- 51.Baliunas D, Baliunas D, Rehm J, et al. Alcohol consumption and risk of incident human immunodeficiency virus infection: a meta-analysis . Int J Public Health 2010; 55: 159–166. [DOI] [PubMed] [Google Scholar]
- 52.Kalichman SC, Simbayi LC, Kaufman M, et al. Alcohol use and sexual risks for HIV/AIDS in Sub-Saharan Africa: systematic review of empirical findings. Prev Sci 2007; 8: 141–151. [DOI] [PubMed] [Google Scholar]
- 53.Shuper PA, Neuman M, Kanteres F, et al. Causal considerations on alcohol and HIV/AIDS – a systematic review. Alcohol Alcohol 2010; 45: 159–166. [DOI] [PubMed] [Google Scholar]
- 54.Dixon TC, Ngak S, Stein E, et al. Pharmacology, physiology and performance: occupational drug use and HIV risk among female entertainment and sex workers in Cambodia. Harm Reduct J 2015; 12: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Volkow ND, Wang G-J, Fowler JS, et al. Stimulant-Induced enhanced sexual desire as a potential contributing factor in HIV transmission. Am J Psychiatry 2007; 164: 157–160. [DOI] [PubMed] [Google Scholar]
- 56.Semple SJ, Patterson TL and Grant I. The context of sexual risk behavior among heterosexual methamphetamine users. Addict Behav 2004; 29: 807–810. [DOI] [PubMed] [Google Scholar]
- 57.Bogart LM, Kral AH, Scott A, et al. Sexual risk among injection drug users recruited from syringe exchange programs in California. Sexually Transm Dis 2005; 32: 27–34. [DOI] [PubMed] [Google Scholar]
- 58.Cheng WS, Garfein RS, Semple SJ, et al. Differences in sexual risk behaviors among male and female HIV-Seronegative heterosexual methamphetamine users. Am J Drug Alcohol Abuse 2009; 35: 295–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rusch ML, Lozada R, Pollini Ra Vera A, et al. Polydrug use among IDUs in Tijuana, Mexico: correlates of methamphetamine use and route of administration by gender. eScholarship, University of California, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kab V, Evans J, Sansothy N, et al. Testing for amphetamine-type stimulant (ATS) use to ascertain validity of self-reported ATS use among young female sex workers in Cambodia. Addict Sci Clin Pract 2012; 7: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Robins JM, Hernán MÁ and Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology 2000; 11: 550–560. [DOI] [PubMed] [Google Scholar]