Abstract
Sleep disturbance is associated with elevated suicidal ideation and negative affect. To date, however, no study has investigated the temporal relationship between sleep and suicidality among those diagnosed with borderline personality disorder (BPD). This preregistered (https://osf.io/4vugk) study tested whether nightly sleep (self-reported sleep duration, sleep onset latency, and subjective sleep quality) represents a (within-person) short-term risk factor for affective dysregulation and increases in suicide risk from day-to-day, as well as whether between-person differences in sleep, negative affect, and suicidality were associated. We used a 21-day ecological momentary assessment protocol in a sample of 153 people diagnosed with BPD, 105 of which had a history of serious suicide attempts, and 52 healthy controls (N = 4076 days). We found a within-person association between worse subjective sleep quality and greater next-day negative affect. At the between-person level, we found positive relationships between sleep latency and suicidal ideation, and a negative association between subjective sleep quality and negative affect. BPD severity did not significantly moderate the strength of any within-person associations, although BPD was positively associated with average levels of suicidal ideation, sleep latency, and negative affect, and negatively related to subjective sleep quality. These findings suggest that the association of sleep with suicidal ideation and BPD exists largely at the between-persons rather than the within-person level. Disturbed sleep, therefore, seems to largely coincide, rather than specifically contribute to, the exacerbation of suicidal crises in BPD.
Keywords: suicidal ideation, ecological momentary assessment, borderline personality disorder, multilevel structural equation modeling, sleep
Research suggests that the association between sleep disturbances and suicidal ideation may be potentiated by borderline personality disorder (BPD; Winsper & Tang, 2014; Winsper et al., 2017). Previous work, however, has returned contradictory results (Oltmanns & Oltmanns, 2015), and the temporal, within-person link of sleep and suicidal ideation in BPD has received limited clinical and research attention (Winsper & Tang, 2014; see Liu et al. [2020] for a recent systematic review and meta-analysis of longitudinal studies). In this study, we address this gap in the literature by asking: Are sleep disturbances contributing factors to exacerbating short-term suicide risk, or an epiphenomenal aspect of BPD? Our analyses are based on a preregistered study protocol (https://osf.io/4vugk), and a 21-day ambulatory assessment procedure, in a carefully sampled population of suicide attempters and nonattempters diagnosed with BPD.
Meta-analytic (Winsper et al., 2017) and narrative reviews (Oltmanns & Oltmanns, 2015) present strong evidence that BPD is linked to sleep disturbance (Oltmanns, 2019; Winsper et al., 2017). Compared with healthy controls, people diagnosed with BPD experience shorter sleep duration, worse sleep efficiency, and reduced REM latency (Akiskal et al., 1985; McNamara et al., 1984; Reynolds et al., 1985; Simor & Horváth, 2013). Yet, inconsistent results within this set of studies make it difficult to articulate clear conclusions regarding the relationship of BPD and individual sleep parameters (Hafizi, 2013; Oltmanns & Oltmanns, 2015; Winsper et al., 2017). These discrepancies could potentially be attributed to the fact that previous related research has been methodologically diverse and conducted in small samples of phenotypically heterogenous groups of individuals with BPD (Harty et al., 2010; Winsper et al., 2017).
One reason why it is important to understand sleep in BPD is that suicidal ideation, suicidal attempts, and even death by suicide have been linked to a variety of indicators of poor sleep, including insomnia, nightmares, poor subjective sleep quality, short self-reported sleep duration, or low sleep efficiency (Bromundt et al., 2013; Grove et al., 2020; Hafizi, 2013; Oltmanns et al., 2014; Sansone et al., 2010; Selby, 2013; Wall et al., 2020).
Conventionally, poor sleep has been viewed to be reflective of psychiatric burden, rather than representing a stable risk factor of psychopathology. This view, however, is amended by findings suggesting that sleep disturbance may uniquely contribute to the exacerbation of psychopathological symptoms (Nutt et al., 2008; Tkachenko et al., 2014), which is based on the notion that the successful treatment of primary psychopathology does not automatically seem to improve sleep problems (Carney et al., 2007). Some cross-sectional evidence also suggests that elevated insomnia symptoms may account for the link between BPD traits and an increased risk for suicide (DeShong & Tucker, 2019).
Relatedly, a recent set of findings implies that sleep disruption potentially charts the progression of BPD symptom severity and suicidality by impairing emotional functioning (Balestrieri et al., 2006; Fleischer et al., 2012; Grove et al., 2017; Lereya et al., 2017; Morales-Muñoz et al., 2020; Sjöström et al., 2009; Wall et al., 2020; Wojnar et al., 2009). On a conceptual level, the emotional cascade model (Selby & Joiner, 2009) provides one plausible explanatory framework for this relationship. The model suggests that upsetting emotional experiences may be potentiated via poor affect regulatory skills that, in turn, may exacerbate in the context of poor sleep in those with a BPD diagnosis. This positive feedback loop contributes to the escalation of negative affect, which then results in exceptionally aversive emotional states that are met by impulsive and self-harming behaviors in attempts to soothe those affective experiences. Therefore, understanding the clinical significance of sleep for affective dysregulation is particularly relevant to BPD, because cumulative evidence implies that the within-person association between negative affective states and the severity of suicidal ideation is particularly pronounced in BPD (Kaurin et al., 2020; Links et al., 2007; Mou et al., 2018).
What cannot be ascertained from previous, largely cross-sectional studies, however, is whether sleep problems precede, thus exacerbate affective dysregulation and suicidal ideation in BPD, or whether sleep problems largely coincide with BPD. Moreover, correlates obtained from cross-sectional designs may further be driven by individual differences or comorbidity rather than dynamical within-person processes, and cannot be ruled out as concomitants to or epiphenomena of suicidal ideation (Liu et al., 2020). To disambiguate both possibilities, longitudinal studies are needed that are designed to characterize temporal aspects of the relationship between sleep and suicidality (Bernert et al., 2015; Littlewood et al., 2019), both of which fluctuate over time and may influence each other (Ben-Zeev et al., 2012; Kleiman et al., 2017; Lemola et al., 2013; Vallières et al., 2005).
A few longitudinal studies have sought to address this issue, but none of them in BPD samples in particular. For instance, Ribeiro et al. (2012) found that insomnia predicted greater suicidal ideation one month later in a sample of young military recruits, but not vice versa. These findings were replicated by Zuromski et al. (2017) in an online sample of individuals endorsing lifetime experience of suicidal behavior. Additionally, a 1-week-long ecological momentary assessment study reported that subjective and actigraphic sleep duration as well as subjective sleep quality predicted next day ideation (Littlewood et al., 2019). Again, suicidal ideation did not predict next night sleep. Finally, a unidirectional relationship was reported in which nightmares significantly predicted postsleep self-harm via increased daytime negative affect in a sample of university students (Hochard et al., 2015).
Although it appears from this brief review that disturbed sleep is prospectively linked to elevated levels of suicide risk, it should be noted that the majority of studies assessed sleep disturbance as a long-term risk factor (Liu et al., 2020). Thus, these studies generally provide limited insight into the temporal association between sleep, suicidal ideation, and negative affect, and do not permit disentangling individual difference level associations from the estimates of temporal associations (e.g., person-centering day-level predictors; Bolger & Laurenceau, 2013). In fact, a recent meta-analysis concluded that sleep disturbance prospectively predicts suicide outcomes, but more work is needed to examine sleep as a short term risk factor and to differentiate the associations of acute from chronic sleep disturbance (Liu et al., 2020). Therefore, it remains unclear to what degree disrupted sleep predicts short-term suicide risk. Narrowing this gap is of substantial clinical importance, because clinical risk assessments are focused on determining if individuals may engage in suicidal behavior in the near future (Liu et al., 2020).
To this end, the present study expands upon prior research by disentangling, and then separately estimating the day-level and person-level associations among sleep, negative affect, and suicidal ideation. Such methodological distinction is key to the question whether poor sleep largely coincides with BPD, or significantly contributes to the short-term exacerbation of BPD symptoms (including negative affectivity and suicidality) from day to day. As such, we aim to contribute to a better understanding of whether temporal changes in sleep predict short-term changes of suicide risk, and whether that relationship is accounted for by negative affect.
Preregistered Analyses
Although previous research has found sleep disturbance to contribute to elevated negative affect, and suicidal ideation, no study has investigated the temporal relationship between sleep and suicidality in BPD, whether negative affect accounts for this relationship, nor directly examined the separate day-level and person-level associations. The current preregistered (https://osf.io/4vugk) study responds to a recent call for more methodologically rigorous studies of the sleep–suicidal ideation relationship (Bernert et al., 2015; Littlewood et al., 2019; Liu et al., 2020) by investigating the temporal relationships among sleep, negative affect, and suicidal ideation using a 21-day ecological momentary assessment protocol in a sample of 142 people diagnosed with BPD, 98 of which had a history of serious suicide attempts, and 49 healthy controls. This sampling approach increases the likelihood of participants reporting suicidal ideation during the study period, because past suicide attempts represent the most reliable predictors of future suicide attempts (O’Connor & Nock, 2014). Moreover, the design of this study allows to improve limitations in the suicide literature by utilizing a brief follow-up period and focusing on sleep as a less studied short-term risk factor for suicidal ideation in BPD.
Based on previous work reviewed above, we set out to disambiguate whether sleep problems antecede and potentially aggravate short-term suicidal ideation in BPD, or whether disturbed sleep and suicidal ideation largely coincide with BPD. We tested a series of hypotheses related to whether nightly sleep predicted next-day suicidal ideation or negative affect, and whether BPD severity moderated the dynamic links among those variables as they fluctuate, within-person, from day to day. Specifically, our hypotheses were as follows:
Tests of Within-Person Associations:
Hypothesis 1a: Worse nightly sleep would predict greater next-day suicidal ideation.
Hypothesis 1b: Worse nightly sleep would predict greater next-day negative affect.
Hypothesis 1c: The within-person association between worse sleep and next-day suicidal ideation would be accounted for by the next-day negative affect.
Cross-Level Interaction Effects:
Hypothesis 2a: BPD features would magnify the within-person association between sleep disturbance and suicidal ideation.
Hypothesis 2b: BPD features would magnify the within-person association between sleep disturbance and negative affect.
Our hypotheses are presented in simplified form for clarity. Estimated models included covariates (i.e., between-level: age, gender; within-level: day in study, and weekday vs. weekend). Sleep onset latency, shorter sleep duration, and worse subjective quality were examined each night and models were conducted separately for each sleep parameter to avoid multicollinearity. Of note, we have tested the association between negative affect and suicidality at both, the within- and between-person level in previous analyses. Results from these analyses revealed that negative affect significantly predicts daily levels of suicidality as operationalized in the models below (Kaurin et al., 2020).
Recent meta-analytic evidence suggests that the link between disturbed sleep and BPD features is likely independent of comorbid depression (Winsper et al., 2017). However, given the importance of persistent negative affectivity for the prediction of suicidal behavior (Zanarini et al., 2016), we exploratorily probed the robustness of our analyses by controlling for current depressive symptoms at the between-person level (osf.io/cxy9b).
Method
All study procedures were approved by the Institutional Review Boards of the University of Pittsburgh (STUDY19050210), and all data and analyses have been made publicly available at the OSF.
Sample
Participants were drawn from a longitudinal study and were recruited from in- and outpatient clinics as well as from the nearby community by advertisement. At enrollment, participants had to be between 18 and 45 years and discharged from any inpatient treatment setting. Exclusion criteria included a lifetime diagnosis of any psychotic or bipolar disorder, clinical evidence of organic brain disease, physical disorders or treatments with known psychiatric consequence (e.g., lupus, steroids), and IQ < 70 measured by the WTAR (Wechsler Test of Adult Reading; Wechsler, 2001). A more detailed description of the parent study protocol has been reported elsewhere (Soloff & Chiappetta, 2017). The sample comprised 153 individuals diagnosed with BPD and 52 healthy control participants (Mage 33.64, SD = 9.50; range 20–60 years; 80% female; 74% Caucasian, 12% African American, 5% Asian, 5% Multi-Race, 4% Pacific Islander, or nonspecified). Of the 153 BPD patients, n = 35 had a history of high-lethality, n = 70 had past low-lethality past suicide attempts, and n = 48 reported no past suicide attempts. As preregistered, to increase the consistency of our EMA measurements, participants with less than 5 days of sleep were excluded from data analyses. Moreover, data on bed and waketime variables were excluded from analyses if identified as an outlier at 4 SD from the mean. This resulted in a final sample size of N = 201 participants, which did not significantly differ from the original sample in key outcomes.
The diagnosis of BPD was based on the International Personality Disorder Examination (IPDE; Loranger et al., 1996), and participants had to meet probable or definite criteria for a lifetime diagnosis. Participants diagnosed with BPD were further divided into two groups based on history of reported suicide attempts. Suicide attempters were required to have clinically significant attempts, defined by a score of >1 on the Beck Lethality Scale (Beck et al., 1975). For participants with multiple attempts, data for the highest-lethality attempt were used.
Participants of the healthy control group and were required to have no lifetime Axis I or II diagnoses determined by the Structured Clinical Interview for DSM–IV or IPDE. As preregistered, participants from the three groups were merged to represent a range of symptom severity, which was further specified with the Personality Assessment Inventory-Borderline Scale (PAI-BOR; Morey, 1991), which demonstrated excellent (α =.81) reliability in our sample. The PAI-BOR contains four subscales that tap core features of BPD: Affective Instability, Identity Problems, Negative Relationships, and Self-Harm. The Self-Harm subscale taps impulsivity and impulsive behaviors more broadly and is not limited to self-harm behaviors.
Momentary Assessments
Participants completed a 21-day EMA protocol within predefined time windows, using the MetricWire smartphone application, which randomly reminded them to complete surveys via push notifications approximately six times per day. This resulted in N = 4,086 days (based on N = 24,916 momentary assessments), with an average number of 19.9 days per participant, ranging from 1–22 days overall. Based on data preregistered exclusion procedures detailed above, the final sample comprised N = 4,076 days and an average number of 20 days per participant.
Each morning, participants reported on last night’s sleep characteristics. Specifically, they reported what time they went to bed the prior night, how long it took them to fall asleep (i.e., sleep onset latency), what time they woke up, and the quality of the prior night sleep (i.e., subjective sleep quality).
Sleep duration was calculated from bedtime, waketime, and sleep onset latency reports. First, bedtime and waketime reports were checked for reporting errors (e.g., participants reporting a bedtime of 10:00 instead of 22:00) and either transformed to their appropriate time or were removed from the data. After addressing potential bed and waketime reporting errors, sleep duration was calculated by the difference, in hours, between self-reported waketime and bedtime.
To calculate sleep duration, we added 24 hr to the waketime and subtracted bedtime from the transformed waketime variable. To illustrate, if a participant reported a bedtime of 23:00 and a waketime of 8:00, the waketime of 8:00 would be transformed to 32:00 by adding 24 hr. Then, the bedtime of 23:00 was subtracted from 32:00 to calculate a sleep duration of 9 hr.
Sleep onset latency was reported on a scale in which each response was a 15 chunk of time (e.g., 1 = “under 15 min,” 2 = “15–30 min”). This Sleep Onset Latency Scale ranged from “under 15 min” to “1 hr 45 min to 2 hr.” Sleep onset latency was recoded so that participant responses reflected the mean of the selected response option (e.g., responses of between 15 and 30 min were recoded to equal 22.5 min). Note that the 15-min interval of 1 hr 30 min to 1 hr 45 min was erroneously left out of the scale during data collection. Subjective sleep quality was measured with the question “Last night my sleep quality was…,” based on a 5-point rating scale, ranging from 1 (very poor) 5 (very good). Participants reported how strongly they experienced negative emotion (i.e., nervous, sad, irritated, angry; ωwithin-person = .81; ωbetween-person = .91) derived from the Positive and Negative Affect Schedule (Watson et al., 1988), on a scale from 0 (not at all) to 100 (extremely) for each adjective.
Suicidal ideation was assessed with six dichotomous items (1 = yes, 0 = no; range: 0–5.4) derived from the Suicidal Ideation subscale of the Columbia-Suicide Severity Rating Scale (C-SSRS; Posner et al., 2008). All items were used to form a daily mean score of suicidal intent severity, and read as follows: “Have you wished you were dead or wished you could go to sleep and not wake up?,” “Have you actually had any thoughts of killing yourself?,” “Have you been thinking about how you might do this?,” “Have you had these thoughts and had some intention of acting on them?,” “Have you started to work out or worked out the details of how to kill yourself?,” “Do you intend to carry out this plan?” (ωwithin = .67; ωbetween = .83). The examination of intraclass correlation returned that approximately 60% of the variability in ratings of suicidal ideation was explained by between-person differences (ICC = .601).
On 11.4% of days participants reported suicidal ideation at least once during the day. More specifically, participants in the BPD group endorsed suicidal ideation on 6.2%, and suicide attempters, on 19.5% of all study days. Among the healthy controls, one participant endorsed a single episode of suicidal ideation.
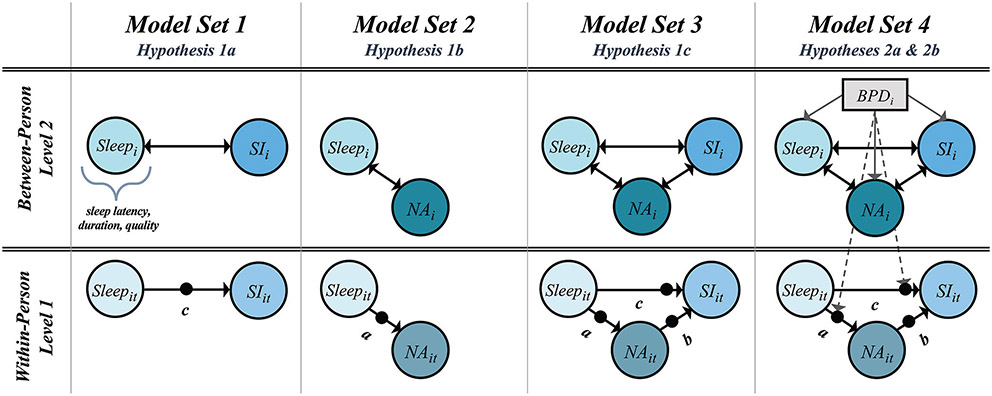
Data Analysis
As preregistered, multilevel structural equation models (MSEMs) were used to test our hypotheses of the links between daily sleep, affect, and suicidal ideation. All models were estimated in Mplus (Version 8.4; Muthén & Muthén, 2019). We used Bayesian estimation because it provides a true latent decomposition into within- and between-person variance for both the predictors and outcome variables when random effects are specified. Significance for all model parameters was based on 95% Credibility Intervals (CIs), with CIs that excluded zero indicative of a parameter that differed significantly from zero. Figure 1 provides a hypothesis-by-hypothesis schematic overview of the estimated models, along with path annotations as referenced in the results section.
Figure 1. Overview of Quantitative Model Specifications Used to Test Preregistered Hypotheses, Including Decomposition of Observed Daily Variables Into Between- (Subscript i) and Within-Person (Subscript t) Variance.
Note. Not all parameters are diagrammed. All models controlled for age and gender at the between-person level, and for time and weekday at the within-person level. Coefficients for covariates are not presented for parsimony. Single headed arrows indicate regression paths. Solid lines represent paths for Hypotheses 1a–c, and dashed for Hypotheses 2a and b. Filled dots represent random effects. NA = negative affect; SI = suicidal ideation.
Total variance in the observed variables of sleep and suicidal ideation was decomposed into their constituent pieces. Because sleep is a daily level variable nested within people, it was decomposed into its day-level and person-level variables using latent decomposition. Accordingly, both assessments of suicidal ideation and negative affect were averaged over each day, and decomposed into their day-level, and person-level latent variables. This decomposition is akin to the partitioning of variance that occurs with the outcome variable in standard multilevel modeling; however, in MSEM it is conducted for both outcomes and predictors that have repeated observations within a person. The between person-level latent variables are an estimate of an individual’s average (i.e., random intercepts) and resemble the portion of variance that is usually captured in cross-sectional studies. The day-level variables reflect the deviations from their average on a given day, for that person, respectively.
Based on our preregistered hypotheses, two sets of models were estimated with nightly sleep (i.e., latency, duration, quality) predicting daily suicidal ideation or negative affect. Model Set 1 (Hypothesis 1a) regressed daily suicidal ideation on nightly sleep at Level 1 (i.e., sleep and daily suicidal ideation), and Level 2 (i.e., associations among individual differences in average sleep parameters and suicidal ideation). Model Set 2 (Hypothesis 1b) regressed daily negative affect on nightly sleep at both levels. To test Hypothesis 1c, Model Set 3 combined Models 1 and 2 by introducing negative affect as intermediate variable for the relationship between sleep and suicidal ideation at Level 1 and Level 2.
To test the second set of hypotheses, Models 4 (Hypothesis 2a) and 5 (Hypothesis 2b) introduced BPD symptom severity as moderator of the link between sleep and suicidal ideation, or sleep and negative affect (i.e., cross-level interactions), while also predicting individual differences in ratings of one’s nightly sleep, negative affect, and suicidal ideation.
Age and gender (0 = female; 1 = male) were modeled as covariates at the between-person level, and random slopes and intercepts were regressed on these covariates. Study day and weekend (vs. weekday) were modeled as covariates at the within-person level to control for any confounding influence of time and weekend effects. No prior information about parameter values were specified (i.e., we used noninformative/diffuse priors that are the default in MPlus). Missing data were assumed to be missing at random. A Bayesian approach to SEM uses all available data in estimation: With increasingly large samples, it provides similar results to full information maximum likelihood to address missing data (Asparouhov & Muthén, 2010).
Along with other parameters not reported in the tables (e.g., residual variances), covariances among between-persons variables are not depicted in the diagrams, but full specifications and detailed output from all models can be found online at osf.io/cxy9b. Table 1 summarizes pooled within-person correlations among the variables along with correlations among the random intercepts (i.e., person averages) at the between-person level.
Table 1.
Correlations Among Study Variables at Within and Between-Person Levels
| Quality | Latency | Duration | Negative affect | Suicidal ideation | BPD | |
|---|---|---|---|---|---|---|
| Within-person | ||||||
| Quality | — | |||||
| Latency | −.34 | — | ||||
| Duration | .30 | −.31 | — | |||
| Negative affect | −.06 | .02 | −.06 | — | ||
| Suicidal ideation | −.03 | .07 | −.04 | .15 | — | — |
| Between-person | ||||||
| Quality | ||||||
| Latency | −.46 | |||||
| Duration | .21 | −.14 | ||||
| Negative affect | −.04 | .32 | .10 | |||
| Suicidal ideation | .07 | .30 | .06 | .23 | ||
| BPD | −.52 | .46 | −.12 | .37 | .21 | |
| M | 3.18 | 22.63 | 7.36 | 1.78 | .11 | 39.19 |
| SD | 1.01 | 22.67 | 1.85 | 0.07 | .04 | 19.50 |
Note. N = 201 (between), N = 4,076 (within). Bolded values indicate the credibility interval does not contain zero. BPD = borderline personality disorder.
Results
Model Set 1: Does Nightly Sleep Predict Next-Day Suicidal Ideation?
Results for models examining the effects of sleep (i.e., sleep latency, duration, and quality) on next-day suicidal ideation can be found in the first column of Table 2. None of the three model specifications returned a significant link between sleep and next day suicidal ideation at the within-person level. That is, on days when participants reported worse than average nightly sleep, they did not also report greater suicidal ideation. At the between-person level, however, we found a relationship between sleep latency and suicidal ideation suggesting that participants who reported taking a longer time to fall asleep also reported higher average levels of suicidal ideation.
Table 2.
Key Estimates From Three Individual Multilevel Structural Equation Models Showing Associations Among Sleep, Negative Affect, and Suicidal Ideation
| Model Set 1 Hypothesis 1a |
Model Set 2 Hypothesis 1b |
Model Set 3 Hypothesis 1c |
||||
|---|---|---|---|---|---|---|
| Est (CI) | β | Est (CI) | β | Est (CI) | β | |
| Sleep Latency | ||||||
| Within-person | ||||||
| Sleep → Suicidal ideation (c) | .00 [−.00, .01] | .14 | — | — | .00 [00, .00] | .13 |
| Sleep → NA (a) | — | — | .00 [−.00, .01] | .06 | .00 [−.00, .00] | .02 |
| NA → Suicidal ideation (b) | — | — | — | — | .14 [.08, .20] | .45 |
| Indirect effect | — | — | — | — | .00[−.00, −.01] | — |
| Between-person | ||||||
| Sleep ↔ Suicidal ideation | .01 [.00, .01] | .24 | — | — | .99 [.38, 1.70] | .24 |
| Sleep ↔ NA | — | — | .02 [.01, .02] | .44 | 3.92 [2.50, 5.60] | .44 |
| NA ↔ Suicidal ideation | — | — | — | — | .06 [.04, .10] | .36 |
| Sleep duration | ||||||
| Within-person | ||||||
| Sleep → suicidal ideation (c) | −.00 [−.01, .01] | −.04 | — | — | −.01 [−02, .01] | −.07 |
| Sleep → NA (a) | — | — | −.01 [−.02, .01] | −.10 | −.02 [−03, .00] | −.15 |
| NA → suicidal ideation (b) | — | — | — | — | .15 [.09, .20] | .48 |
| Indirect effect | — | — | — | — | .00 [−.01, .01] | — |
| Between-person | ||||||
| Sleep ↔ suicidal ideation | .02 [−.03, .07] | .06 | — | — | .01 [−.04, .07] | .04 |
| Sleep ↔ NA | — | — | −.03 [−.12, .06] | −.07 | −.04 [−.16, .08] | −.05 |
| NA ↔ suicidal ideation | — | — | — | — | .07 [.04, .10] | .37 |
| Subjective sleep quality | ||||||
| Within-person | ||||||
| Sleep → suicidal ideation (c) | −.01 [−.03, .00] | −.16 | — | — | −.01 [−.03, .00] | −.21 |
| Sleep → NA (a) | — | — | −.05 [−.08, −.02] | −.33 | −.08 [−.11, −.05] | −.49 |
| NA → suicidal ideation (b) | — | — | — | — | .13 [.08, .19] | .45 |
| Indirect effect | — | — | — | — | −.01 [−.02, .01] | — |
| Between-person | ||||||
| Sleep ↔ suicidal ideation | −.03 [−.10, .03] | −.06 | — | — | .00 [−.03, .03] | .00 |
| Sleep ↔ NA | — | — | −.24 [−.37, −.12] | −.29 | −.13 [−.20, −.07] | −.32 |
| NA ↔ suicidal ideation | — | — | — | — | .07 [.04, .10] | .36 |
Note. N = 201 (between), N = 4,076 (within); → indicates regression; β parameter estimates are standardized. 95% credibility intervals of unstandardized parameter estimates are in parentheses. Bolded values indicate the credibility interval does not contain zero; CI = credibility interval; NA = negative affect.
Model Set 2: Does Nightly Sleep Predict Next-Day Negative Affect?
Key estimates for models testing the effects of sleep (i.e., sleep latency, duration, and quality) on next-day negative affect are detailed in the central column of Table 2. Overall, we only found a significant positive within-person link between subjective sleep quality and next day negative affect. Thus, on average, when individuals reported worse nightly subjective sleep quality, they also tended to report elevated levels of negative affect on the subsequent day.
At the between-persons level, a positive relationship emerged for negative affect and sleep latency, and a negative association for subjective sleep quality and negative affect. That is, those who generally tended to report longer sleep onset latency and worse subjective sleep quality, also reported higher levels of negative affect on average.
Model 3: Does Negative Affect Explain the Relation Between Nightly Sleep and Next-Day Suicidal Ideation?
As noted in our preregistration, our aim was to combine both Model 1 and Model 2 to test whether negative affect would account for the relationship between poor nightly sleep and suicidal ideation. Unsurprisingly given the nonsignificant direct associations between sleep variables and suicidal ideation at the within-person level, negative affect did not statistically mediate these associations (see right column of Table 2, Model 3).
Model 4: Does BPD Severity Moderate the Associations Among Sleep, Negative Affect, and Suicidal Ideation?
Finally, we tested whether BPD severity features moderated the paths of the within-person Models 1 and 2. All within-person paths exhibited significant variability across individuals. Individual differences in the strength of these within-person paths were regressed on BPD severity, sex, and age. Coefficients from these models are displayed in Table 3, organized by sleep variables. Results indicated that BPD severity had no significant effect on any within-person pathway, although it did have associations with between-person differences.
Table 3.
Key Estimates From Multilevel Models With Sleep Predicting Suicidal Ideation or Negative Affect and Moderation of These Within-Person Effects by BPD Severity
| Model Set 4 | ||||
|---|---|---|---|---|
| Hypothesis 2a |
Hypothesis 2b |
|||
| Est (CI) | β | Est (CI) | β | |
| Sleep latency | ||||
| BPD → Sleep | .31 [.21,.42] | .42 | .32 [.22, .43] | .42 |
| BPD → NA | — | — | .02 [.01, .02] | .48 |
| BPD → Suicidal ideation | .00 [.00, 00] | .14 | — | — |
| BPD × (Sleep → Suicidal Ideation) | .00 [.00,.00] | .06 | — | — |
| BPD × (Sleep → NA) | — | — | .00 [.00, .00] | −.01 |
| Sleep duration | ||||
| BPD → Sleep | −.01 [−.02, .01] | −.09 | −.01 [−.02 .00] | −.12 |
| BPD → NA | — | — | .02 [.01 .02] | .58 |
| BPD → Suicidal ideation | .00 [.00, .01] | .22 | — | — |
| BPD × (Sleep → Suicidal Ideation) | .00 [−.00, .00] | −.05 | — | — |
| BPD × (Sleep → NA) | — | — | −.00 [.00 .00] | −.10 |
| BPD × (NA → Suicidal Ideation) | — | — | — | — |
| Subjective sleep quality | ||||
| BPD → Sleep | −.02 [−.02, −.01] | −.50 | −.02 [−.02, −.01] | −.50 |
| BPD → NA | — | — | .02 [.01, .02] | .56 |
| BPD → Suicidal ideation | .01 [.00, .01] | .25 | — | — |
| BPD × (Sleep → Suicidal Ideation) | .00 [−.00, .00] | −.01 | — | — |
| BPD × (Sleep → NA) | — | — | −.00 [−.00, .00] | −.15 |
| BPD × (NA → Suicidal Ideation) | — | — | — | — |
Note. N = 201 (between), N = 4,076 (within); → indicates regression; β parameter estimates are standardized. 95% credibility intervals of unstandardized parameter estimates are in parentheses. Bolded values indicate the credibility interval does not contain zero; BPD = borderline personality disorder; CI = credibility intervals; NA = negative affect.
Specifically, BPD severity was positively associated with individual differences in suicidal ideation, except for the model where suicidal ideation was regressed on sleep latency. BPD severity was also positively related to sleep latency and negatively to subjective sleep quality. Additionally, in models were negative affect was regressed on sleep, we found that BPD severity was associated with greater negative affect (see Table 3 for an overview).
Discussion
Whereas previous studies reported long-term associations between disturbed sleep and suicide risk, it remained unclear whether these associations were driven by individual differences or dynamic within-person processes. Therefore, sleep disturbances could not be ruled out as concomitant to or an epiphenomenon of BPD, and to what degree disrupted sleep predicts short-term suicide risk in contrast (see Liu et al., 2020 for a systematic review and meta-analysis of longitudinal studies). To narrow this gap in the literature, we obtained data from a large, well-characterized BPD sample over-sampled for past suicide attempts, and preregistered our analyses.
In contrast to our first set of preregistered hypotheses, we did not find a significant within-person association between daytime suicidal ideation and self-reports of how a participant slept the night before. Overall, this pattern contrasts with sparse previous evidence that prior sleep disruption predicts suicidal ideation (Hochard et al., 2015; Ribeiro et al., 2012; Zuromski et al., 2017). It particularly contrasts with Littlewood and colleagues (2019) who found that both self-reported sleep duration and subjective sleep quality predicted greater next-day suicidal ideation. One explanation may be that these prior studies did not appear to explicitly disentangle and separately model within-person and between-person associations between sleep and suicidal ideation. Moreover, the use of community or non-BPD samples in these studies limits the ability to generalize results to BPD samples, like the sample reported in this study. It is also worth noting that the current study collected substantially more repeated assessments per person than most prior studies, and obtained a significantly larger sample size (Hochard et al., 2015; Littlewood et al., 2019; Ribeiro et al., 2012), affording more accuracy when approximating links between BPD, suicidal ideation, and sleep (Oltmanns, 2019).
At the between-person level, however, we found that people who generally take longer to fall asleep also tended to report greater suicidal ideation. The relationship between sleep latency and suicidal ideation could be reflective of more general, aberrant self-regulatory processes in BPD that are shared, potentially etiological and maintaining factors of poor subjective sleep quality in BPD. However, because these links emerged at the between-rather than the within-person level, sleep disturbances likely reflect concomitants or epiphenomena of BPD rather than a stable risk factor (Liu et al., 2020). In that regard, it is reasonable to assume that effects of sleep on BPD symptom exacerbation unfold over longer periods of time, and thus more likely resemble stable predispositions to affective dysregulation.
Accordingly, tests of the second set of hypotheses revealed that at the between-person level, people with greater average negative affect had longer sleep onset latency and worse subjective sleep quality on average. Moreover, a significant within-person link between subjective sleep quality and negative affect emerged, wherein a night of better quality of sleep than typical predicted less than usual next-day negative affect. Importantly, this effect may be interpreted as a check of our study’s ability to detect within-person relationships in general. Overall, these findings generally replicate findings that sleep and negative affect are linked at both the within- and between-person level (Kahn et al., 2013; Palmer & Alfano, 2017). They also converge with evidence that a number of symptoms and behaviors central to BPD are known to disrupt sleep patterns (Fleischer et al., 2012; Winsper & Tang, 2014). Relatedly, Harvey et al. (2011) proposed that it is important to address both sleep disturbance and emotion dysregulation in treatment to produce durable treatment gains. For instance, helping to stabilize sleep prior to addressing emotion regulation skills might facilitate skill acquisition and improve overall treatment outcome (see also Nutt et al., 2008).
Regarding our third hypothesis, we did not find that negative affect accounted for the within-person link between sleep and suicidal ideation. Wall et al. (2020) reported a similar pattern in cross-sectional data, where adolescent BPD and affective dysregulation were significantly related to sleep disturbance, but affective dysregulation did not account for the link between sleep disturbance and BPD.
Finally, tests of our second set of hypotheses revealed that none of the significant within-person links was moderated by BPD severity. In line with previous work (Winsper et al., 2017), however, we found that BPD severity was generally positively associated with suicidal ideation, and sleep latency, while it was negatively associated with subjective sleep quality. Additionally, in models where negative affect was regressed on sleep, we found that BPD severity was positively related to negative affect. Thus, people with greater severity of BPD had worse sleep, greater negative affect, and greater suicidal ideation on average. However, these participants did not have stronger within-person links among these variables. Moreover, these effects were unique to BPD, even after controlling for depression, which we demonstrated in an exploratory, not preregistered set of analyses (osf.io/cxy9b).
Overall, these findings suggest that the associations of sleep with suicidal ideation and BPD largely reside at the individual difference level rather than the within-person level. Those who experience more negative affect in general also tend to report lower subjective sleep quality or greater sleep latency. Additionally, those who reported longer average sleep latency also endorsed higher levels of suicidal ideation. In addition, poor sleep and greater suicidal ideation tended to characterize individuals higher in BPD severity rather than poor sleep exacerbating suicidal ideation and negative emotions in BPD patient populations. It is possible that the pattern of results reported in this study reflects more general self-regulatory impairments in BPD that have the potential to spill over into disturbed nightly sleep (Harty et al., 2010; Selby, 2013) that may largely coincide, though not specifically contribute to the exacerbation of suicidal crises in BPD.
Study Limitations
The current research has limitations that are important to consider. First, findings are based upon self-report data which may upwardly bias associations due to common method variance (Podsakoff et al., 2003). Additionally, self-reports of sleep demonstrate moderate convergence with actigraphy and polysomnographic measures of sleep, and future research should strive to use other methods to measure sleep. Along these lines, participant raw reports of bedtime and waketime, which were used to calculate sleep duration, had reporting errors (a frequent, yet infrequently discussed problem with self-reports of bed and waketimes) that either had to be corrected or resulted in data loss. Using an actigraphic measure of sleep would avoid such reporting errors (though it is still prone to other data cleaning problems, see Fekedulegn et al., 2020). Despite the limitation of using self-reported sleep data, it should be noted that subjective sleep quality is a unique sleep characteristic that can only be measured by self-report and which is an important, distinct element of sleep that is tied to health and functioning (Buysse, 2014).
Even in real world, every day contexts and representative, high-risk populations, the base rate of momentary endorsements of suicidal ideation is low, and the levels reported in this sample were slightly higher than averages reported in previous studies (7.8% of reports in Husky et al., 2014). This low variance in suicidal ideation likely reduced the ability to detect and downwardly biased associations between sleep and suicidal ideation. Thus, to increase the reliability of our statistical models, we averaged momentarily assessed suicidal ideation over each day. This allowed us to create a detailed measure of suicidal ideation severity, encompassing a wide range of suicidal thoughts and potential behaviors that no previous momentary study has assessed. Future studies could, therefore, explore whether different item and scaling choices would affect response rates, and also, which temporal resolution would yield most reliable estimates.
Further, our findings at the between-person level are cross-sectional in nature and therefore preclude causal conclusions. Thus, although an individual’s BPD severity and average levels of sleep, negative affect, and suicidal ideation all tended to be associated with each other, it is unclear whether any of these characteristics precede or cause one another. There is limited evidence supporting the notion that sleep problems may be evident before the development of BPD and contribute to its etiology (Lereya et al., 2017; Selby, 2013; Wall et al., 2020). There is also tentative evidence to suggest that ongoing sleep problems can contribute to the chronicity of the disorder (Plante et al., 2013). Intensive longitudinal studies focused on more chronic levels of these characteristics across different developmental stages are needed to determine how poor sleep and short-term fluctuations in suicidal ideation relate to each other in daily life.
Although we have probed and illustrated the robustness of our study results via sensitivity analyses controlling for concurrent depression (osf.io/cxy9b), the present study is—to some extent—limited by a comprehensive control strategy of important confounders of sleep disturbances, such as other relevant comorbid disorders or socioeconomic features (e.g., working status). Data derived from ambulatory assessment protocols allow to characterize temporal aspects of the relationship between sleep, affect, and suicidality as they fluctuate over time as well as their reciprocal influence. Cross-sectional analyses, in contrast, focus on epiphenomena of suicidal ideation. Thus, although it is plausible to assume that it is predominantly the latter relationship that is more susceptible to biases by unobserved confounds, future studies should investigate whether the dynamic coupling between variables of interest may be weakened or enhanced in the context of theoretically justifiable control variables.
Finally, it is important to note that our set of sleep measures did not include an indicator of nightmares, which are known to occur frequently in BPD (Winsper et al., 2017). This is a critical limitation, because preliminary evidence suggests a prospective association between nightmares and BPD symptoms based on intensive longitudinal data in a small sample (Selby, 2013) as well as over longer developmental periods (Lereya et al., 2017). There is also growing evidence showing that nightmares are associated with increased risk of suicidal behavior or self-harm in clinical and community samples (Hochard et al., 2015; Russell et al., 2018), independently of a history of traumatic experience (Sandman et al., 2017). Possibly, nightmares aggravate daytime affective dysregulation which may manifest in symptom exacerbation; alternatively, nightmares may also be reflective of daily affect dysregulatory experiences (Selby, 2013). Thus, more research is needed to clarify the direction and magnitude of the relationship between nightmares and affect-regulatory processes in daily life, and how each of these processes as well as their interactive effects may contribute to states of heightened risk for death by suicide.
Conclusion
This is the first preregistered study examining sleep as a short-term risk factor of suicidal ideation in a well-characterized BPD sample. We believe that it represents an important first step toward rigorous research on how sleep and suicide are related on a narrow timescale in BPD (see also Oltmanns, 2019) and emphasize the importance of disentangling within- and between-person associations in this context. Because our results suggest that the link between sleep disturbance and suicidal ideation in BPD largely exists at the individual difference level rather than the within-person level, it is reasonable to assume that sleep disturbance generally emerges as part of the disorder. Those who experience generally elevated levels of negative affect also tend to report lower subjective sleep quality or greater sleep latency, whereas those who experience generally more pronounced levels of sleep latency also endorse higher levels of suicidal ideation. In other words, poor sleep and greater suicidal ideation tend to characterize individuals higher in BPD severity rather than poor sleep exacerbating suicidal ideation and negative emotions in BPD. Possibly, effects of sleep on BPD symptom exacerbation unfold over longer periods of time, which is why they phenomenologically resemble stable predispositions to affective dysregulation, and more general self-regulatory impairments likely manifest as disturbed nightly sleep in BPD.
Disturbed sleep, therefore, seems to largely coincide, rather than specifically contribute to the exacerbation of suicidal crises in BPD.
Acknowledgments
This study was supported by the National Institute of Mental Health (R01 MH048463).
Footnotes
The authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest, or nonfinancial interest in the subject matter or materials discussed in this article. We are grateful to the patients who took part in this study and to the clinical and research teams who made this work possible.
References
- Akiskal HS, Yerevanian BI, Davis GC, King D, & Lemmi H (1985). The nosologic status of borderline personality: Clinical and polysomnographic study. The American Journal of Psychiatry, 142(2), 192–198. 10.1176/ajp.142.2.192 [DOI] [PubMed] [Google Scholar]
- Asparouhov T, & Muthén B (2010). Bayesian analysis of latent variable models using Mplus. https://www.statmodel.com/download/BayesAdvantages18.pdf [Google Scholar]
- Balestrieri M, Rucci P, Sbrana A, Ravani L, Benvenuti A, Gonnelli C, Dell'osso L, & Cassano GB (2006). Lifetime rhythmicity and mania as correlates of suicidal ideation and attempts in mood disorders. Comprehensive Psychiatry, 47(5), 334–341. 10.1016/j.comppsych.2006.01.004 [DOI] [PubMed] [Google Scholar]
- Beck AT, Beck R, & Kovacs M (1975). Classification of suicidal behaviors: I. Quantifying intent and medical lethality. The American Journal of Psychiatry, 132(3), 285–287. 10.1176/ajp.132.3.285 [DOI] [PubMed] [Google Scholar]
- Ben-Zeev D, Young MA, & Depp CA (2012). Real-time predictors of suicidal ideation: Mobile assessment of hospitalized depressed patients. Psychiatry Research, 197(1–2), 55–59. 10.1016/j.psychres.2011.11.025 [DOI] [PubMed] [Google Scholar]
- Bernert RA, Kim JS, Iwata NG, & Perlis ML (2015). Sleep disturbances as an evidence-based suicide risk factor. Current Psychiatry Reports, 17(3), Article 554. 10.1007/s11920-015-0554-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolger N, & Laurenceau JP (2013). Intensive longitudinal methods: An introduction to diary and experience sampling research. Guilford Press. [Google Scholar]
- Bromundt V, Wirz-Justice A, Kyburz S, Opwis K, Dammann G, & Cajochen C (2013). Circadian sleep-wake cycles, well-being, and light therapy in borderline personality disorder. Journal of Personality Disorders, 27(5), 680–696. 10.1521/pedi_2012_26_057 [DOI] [PubMed] [Google Scholar]
- Buysse DJ (2014). Sleep health: Can we define it? Does it matter? Sleep, 37(1), 9–17. 10.5665/sleep.3298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carney CE, Edinger JD, Manber R, Garson C, & Segal ZV (2007). Beliefs about sleep in disorders characterized by sleep and mood disturbance. Journal of Psychosomatic Research, 62(2), 179–188. [DOI] [PubMed] [Google Scholar]
- DeShong HL, & Tucker RP (2019). Borderline personality disorder traits and suicide risk: The mediating role of insomnia and nightmares. Journal of Affective Disorders, 244, 85–91. 10.1016/j.jad.2018.10.097 [DOI] [PubMed] [Google Scholar]
- Fekedulegn D, Andrew ME, Shi M, Violanti JM, Knox S, & Innes KE (2020). Actigraphy-based assessment of sleep parameters. Annals of Work Exposures and Health, 64(4), 350–367. 10.1093/annweh/wxaa007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleischer M, Schäfer M, Coogan A, Häßler F, & Thome J (2012). Sleep disturbances and circadian CLOCK genes in borderline personality disorder. Journal of Neural Transmission, 119(10), 1105–1110. 10.1007/s00702-012-0860-5 [DOI] [PubMed] [Google Scholar]
- Grove JL, Smith TW, Carlson SE, Bryan CJ, Crowell SE, Czajkowski L, Williams PG, & Parkhurst K (2020). Prospective association between suicide cognitions and emotional responses to a laboratory stressor: The mediating role of nightly subjective sleep quality. Journal of Affective Disorders, 265, 77–84. 10.1016/j.jad.2020.01.060 [DOI] [PubMed] [Google Scholar]
- Grove JL, Smith TW, Crowell SE, & Ellis JH (2017). Preliminary evidence for emotion dysregulation as a mechanism underlying poor sleep quality in borderline personality disorder. Journal of Personality Disorders, 31(4), 542–552. 10.1521/pedi_2016_30_261 [DOI] [PubMed] [Google Scholar]
- Hafizi S (2013). Sleep and borderline personality disorder: A review. Asian Journal of Psychiatry, 6(6), 452–459. 10.1016/j.ajp.2013.06.016 [DOI] [PubMed] [Google Scholar]
- Harty L, Duckworth R, Thompson A, Stuewig J, & Tangney JP (2010). Are inmates’ subjective sleep problems associated with borderline personality, psychopathy, and antisocial personality independent of depression and substance dependence? Journal of Forensic Psychiatry and Psychology, 21(1), 23–39. 10.1080/14789940903194095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey AG, Murray G, Chandler RA, & Soehner A (2011). Sleep disturbance as transdiagnostic: Consideration of neurobiological mechanisms. Clinical Psychology Review, 31(2), 225–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hochard KD, Heym N, & Townsend E (2015). The unidirectional relationship of nightmares on self-harmful thoughts and behaviors. Dreaming, 25(1), 44–58. 10.1037/a0038617 [DOI] [Google Scholar]
- Husky M, Olié E, Guillaume S, Genty C, Swendsen J, & Courtet P (2014). Feasibility and validity of ecological momentary assessment in the investigation of suicide risk. Psychiatry Research, 220(1–2), 564–570. 10.1016/j.psychres.2014.08.019 [DOI] [PubMed] [Google Scholar]
- Kahn M, Sheppes G, & Sadeh A (2013). Sleep and emotions: Bidirectional links and underlying mechanisms. International Journal of Psychophysiology, 89(2), 218–228. 10.1016/j.ijpsycho.2013.05.010 [DOI] [PubMed] [Google Scholar]
- Kaurin A, Dombrovski A, Hallquist M, & Wright AG (2020, July 22). Daily suicidal surge and attempted suicide in borderline personality disorder. 10.31234/osf.io/hswea [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleiman EM, Turner BJ, Fedor S, Beale EE, Huffman JC, & Nock MK (2017). Examination of real-time fluctuations in suicidal ideation and its risk factors: Results from two ecological momentary assessment studies. Journal of Abnormal Psychology, 126(6), 726–738. 10.1037/abn0000273 [DOI] [PubMed] [Google Scholar]
- Lemola S, Ledermann T, & Friedman EM (2013). Variability of sleep duration is related to subjective sleep quality and subjective well-being: An actigraphy study. PLoS ONE, 8(8), Article e71292. 10.1371/journal.pone.0071292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lereya ST, Winsper C, Tang NK, & Wolke D (2017). Sleep problems in childhood and borderline personality disorder symptoms in early adolescence. Journal of Abnormal Child Psychology, 45(1), 193–206. 10.1007/s10802-016-0158-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Links PS, Eynan R, Heisel MJ, Barr A, Korzekwa M, McMain S, & Ball JS (2007). Affective instability and suicidal ideation and behavior in patients with borderline personality disorder. Journal of Personality Disorders, 21(1), 72–86. 10.1521/pedi.2007.21.1.72 [DOI] [PubMed] [Google Scholar]
- Littlewood DL, Kyle SD, Carter LA, Peters S, Pratt D, & Gooding P (2019). Short sleep duration and poor sleep quality predict next-day suicidal ideation: An ecological momentary assessment study. Psychological Medicine, 49(3), 403–411. 10.1017/S0033291718001009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu RT, Steele SJ, Hamilton JL, Do QBP, Furbish K, Burke TA, Martinez AP, & Gerlus N (2020). Sleep and suicide: A systematic review and meta-analysis of longitudinal studies. Clinical Psychology Review, 81, Article 101895. 10.1016/j.cpr.2020.101895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loranger A, Sartorius N, & Janca A (1996). Assessment and diagnosis of personality disorders: The International Personality Disorder Examination (IPDE). Cambridge University Press. [Google Scholar]
- McNamara E, Reynolds CF III, Soloff PH, Mathias R, Rossi A, Spiker D, Coble PA, & Kupfer DJ (1984). EEG sleep evaluation of depression in borderline patients. The American Journal of Psychiatry, 141(2), 182–186. 10.1176/ajp.141.2.182 [DOI] [PubMed] [Google Scholar]
- Morales-Muñoz I, Broome MR, & Marwaha S (2020). Association of parent-reported sleep problems in early childhood with psychotic and borderline personality disorder symptoms in adolescence. JAMA Psychiatry, 77(12), 1211–1256. 10.1001/jamapsychiatry.2020.1875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morey LC (1991). Personality assessment screener. Psychological Assessment Resources. [Google Scholar]
- Mou D, Kleiman EM, Fedor S, Beck S, Huffman JC, & Nock MK (2018). Negative affect is more strongly associated with suicidal thinking among suicidal patients with borderline personality disorder than those without. Journal of Psychiatric Research, 104, 198–201. 10.1016/j.jpsychires.2018.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L, & Muthén B (2019). Mplus user’s guide. [Google Scholar]
- Nutt D, Wilson S, & Paterson L (2008). Sleep disorders as core symptoms of depression. Dialogues in Clinical Neuroscience, 10(3), 329–336. 10.31887/DCNS.2008.10.3/dnutt [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor RC, & Nock MK (2014). The psychology of suicidal behaviour. The Lancet Psychiatry, 1(1), 73–85. 10.1016/S2215-0366(14)70222-6 [DOI] [PubMed] [Google Scholar]
- Oltmanns JR (2019). Personality disorders, maladaptive personality traits, and sleep problems: Findings and future directions. In Križan Z (Ed.), Sleep, personality, and social behavior (pp. 239–254). Springer. 10.1007/978-3-030-30628-1_13 [DOI] [Google Scholar]
- Oltmanns JR, & Oltmanns TF (2015). Borderline personality pathology, polysomnography, and self-reported sleep problems: A review. Current Sleep Medicine Reports, 1(2), 141–149. 10.1007/s40675-015-0011-2 [DOI] [Google Scholar]
- Oltmanns JR, Weinstein Y, & Oltmanns TF (2014). Borderline personality pathology and insomnia symptoms in community-dwelling older adults. Personality and Mental Health, 8(3), 178–187. 10.1002/pmh.1259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer CA, & Alfano CA (2017). Sleep and emotion regulation: An organizing, integrative review. Sleep Medicine Reviews, 31, 6–16. 10.1016/j.smrv.2015.12.006 [DOI] [PubMed] [Google Scholar]
- Plante DT, Frankenburg FR, Fitzmaurice GM, & Zanarini MC (2013). Relationship between maladaptive cognitions about sleep and recovery in patients with borderline personality disorder. Psychiatry Research, 210(3), 975–979. 10.1016/j.psychres.2013.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podsakoff PM, MacKenzie SB, Lee JY, & Podsakoff NP (2003). Common method biases in behavioral research: A critical review of the literature and recommended remedies. The Journal of Applied Psychology, 88(5), 879–903. 10.1037/0021-9010.88.5.879 [DOI] [PubMed] [Google Scholar]
- Posner K, Brent D, Lucas C, Gould M, Stanley B, Brown G, & Mann J (2008). Columbia-Suicide Severity Rating Scale (C-SSRS). Columbia University Medical Center. [Google Scholar]
- Reynolds CF III, Soloff PH, Kupfer DJ, Taska LS, Restifo K, Coble PA, & McNamara ME (1985). Depression in borderline patients: A prospective EEG sleep study. Psychiatry Research, 14(1), 1–15. 10.1016/0165-1781(85)90084-8 [DOI] [PubMed] [Google Scholar]
- Ribeiro JD, Pease JL, Gutierrez PM, Silva C, Bernert RA, Rudd MD, & Joiner TE Jr. (2012). Sleep problems outperform depression and hopelessness as cross-sectional and longitudinal predictors of suicidal ideation and behavior in young adults in the military. Journal of Affective Disorders, 136(3), 743–750. 10.1016/j.jad.2011.09.049 [DOI] [PubMed] [Google Scholar]
- Russell K, Rasmussen S, & Hunter SC (2018). Insomnia and nightmares as markers of risk for suicidal ideation in young people: Investigating the role of defeat and entrapment. Journal of Clinical Sleep Medicine, 14(5), 775–784. 10.5664/jcsm.7104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandman N, Valli K, Kronholm E, Vartiainen E, Laatikainen T, & Paunio T (2017). Nightmares as predictors of suicide: An extension study including war veterans. Scientific Reports, 7(1), Article 44756. 10.1038/srep44756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sansone RA, Edwards HC, & Forbis JS (2010). Sleep quality in borderline personality disorder: A cross-sectional study. Primary Care Companion to the Journal of Clinical Psychiatry, 12(5), PCC.09m00919. 10.4088/PCC.09m00919bro [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selby EA (2013). Chronic sleep disturbances and borderline personality disorder symptoms. Journal of Consulting and Clinical Psychology, 81(5), 941–947. 10.1037/a0033201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selby EA, & Joiner TE Jr. (2009). Cascades of emotion: The emergence of borderline personality disorder from emotional and behavioral dysregulation. Review of General Psychology, 13(3), 219–229. 10.1037/a0015687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simor P, & Horváth K (2013). Altered sleep in borderline personality disorder in relation to the core dimensions of psychopathology. Scandinavian Journal of Psychology, 54(4), 300–312. 10.1111/sjop.12048 [DOI] [PubMed] [Google Scholar]
- Sjöström N, Hetta J, & Waern M (2009). Persistent nightmares are associated with repeat suicide attempt: A prospective study. Psychiatry Research, 170(2–3), 208–211. 10.1016/j.psychres.2008.09.006 [DOI] [PubMed] [Google Scholar]
- Soloff PH, & Chiappetta L (2017). Suicidal behavior and psychosocial outcome in borderline personality disorder at 8-year follow-up. Journal of Personality Disorders, 31(6), 774–789. 10.1521/pedi_2017_31_280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tkachenko O, Olson EA, Weber M, Preer LA, Gogel H, & Killgore WD (2014). Sleep difficulties are associated with increased symptoms of psychopathology. Experimental Brain Research, 232(5), 1567–1574. 10.1007/s00221-014-3827-y [DOI] [PubMed] [Google Scholar]
- Vallières A, Ivers H, Bastien CH, Beaulieu-Bonneau S, & Morin CM (2005). Variability and predictability in sleep patterns of chronic insomniacs. Journal of Sleep Research, 14(4), 447–453. 10.1111/j.1365-2869.2005.00480.x [DOI] [PubMed] [Google Scholar]
- Wall K, Vanwoerden S, Penner F, Patriquin M, Alfano CA, & Sharp C (2020). Adolescent sleep disturbance, emotion regulation and borderline features in an inpatient setting. Journal of Clinical Child and Adolescent Psychology. Advance online publication. 10.1080/15374416.2020.1772081 [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. [DOI] [PubMed] [Google Scholar]
- Wechsler D (2001). Wechsler Test of Adult Reading (WTAR). The Psychological Corporation. [Google Scholar]
- Winsper C, & Tang NK (2014). Linkages between insomnia and suicidality: Prospective associations, high-risk subgroups and possible psychological mechanisms. International Review of Psychiatry, 26(2), 189–204. 10.3109/09540261.2014.881330 [DOI] [PubMed] [Google Scholar]
- Winsper C, Tang NK, Marwaha S, Lereya ST, Gibbs M, Thompson A, & Singh SP (2017). The sleep phenotype of borderline personality disorder: A systematic review and meta-analysis. Neuroscience and Biobehavioral Reviews, 73, 48–67. 10.1016/j.neubiorev.2016.12.008 [DOI] [PubMed] [Google Scholar]
- Wojnar M, Ilgen MA, Wojnar J, McCammon RJ, Valenstein M, & Brower KJ (2009). Sleep problems and suicidality in the National Comorbidity Survey Replication. Journal of Psychiatric Research, 43(5), 526–531. 10.1016/j.jpsychires.2008.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Reich DB, & Fitzmaurice GM (2016). Fluidity of the subsyndromal phenomenology of borderline personality disorder over 16 years of prospective follow-up. The American Journal of Psychiatry, 173(7), 688–694. 10.1176/appi.ajp.2015.15081045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuromski KL, Cero I, & Witte TK (2017). Insomnia symptoms drive changes in suicide ideation: A latent difference score model of community adults over a brief interval. Journal of Abnormal Psychology, 126(6), 739–749. 10.1037/abn0000282 [DOI] [PubMed] [Google Scholar]