Abstract
The identification and management of low parasitemia infections have become increasingly challenging for malaria control and elimination. Submicroscopic Plasmodium infections and G6PD deficiency among febrile patients require more sensitive diagnostic methods to improve detection and careful treatment regime of these infections. In Ethiopia, information on the low density submicroscopic malarial infections and frequency of G6PD deficiency (G6PDd) is scarce. In this study, 297 malaria suspected febrile patient samples were collected from health facilities of Bonga town in southwestern Ethiopia. The positivity rates of Plasmodium infection were determined by microscopy and quantitative PCR. G6PD activity level was determined by careSTART™ G6PD biosensor and the frequency of three common variants: G6PD*A (A376G), G6PD*A− (G202A) and Mediterranean (C563T) were investigated. G6PD gene sequencing was performed to detect mutations in exons 2–11 for both G6PD normal and deficient samples based on the phenotypic assay. More than twice Plasmodium infected samples was detected by qPCR (52/297; 17.4%) than microscopy (21/297; 7.0%). About 31 (10%) of the infections were submicroscopic. Bednet usage and age had a significant association with Plasmodium infection. Of the 271 participants who were tested for G6PD phenotype, 19 (7.0%) had low G6PD level. No mutations were observed in A376G, G202A, and C563T in the G6PDd samples, but three novel non-synonymous mutations in exon 2 including a C to T transition at position ChrX:6504 (Arg to Thr), G to T at ChrX:6369 (Ser to IIe), and G to C at ChrX:6664 (Gln to His) were detected. A high number of submicroscopic Plasmodium infections observed in this study pose a challenge for accurate and timely diagnosis, which could hinder malaria control efforts. G6PD deficiency in malaria patients pose danger when treating patients with primaquine. The three novel mutations detected in exon 2 of the G6PD gene merit further investigation on the hemolytic risk when exposed to oxidative antimalarials, their prevalence, and clinical significance.
Keywords: Submicroscopic Plasmodium infection, Malaria elimination, G6PD deficiency, Southwestern Ethiopia
Background
Malaria is one of the major tropical diseases that poses a threat to public health and adversely affects the economic development of countries in sub-Sahara Africa 1. In Ethiopia, malaria accounts for about 60% of all hospital admission. Much of malaria-related illness and death occur in the most remote, rural areas of the country where there is insufficient health care coverage, poverty, and other socio-economic issues 2,3,4. In 2019, a total of 904,496 malaria cases responsible for 213 deaths were recorded. Ethiopia is one of the few African countries where Plasmodium falciparum and P. vivax coexist 7,8. Plasmodium falciparum accounted for 81% of the total cases, and the remaining cases were attributed to P. vivax 5,6. As malaria prevalence has shown slight decline in the past few years, transmission appears to be heterogeneous across the country, with some areas being relatively free whereas others are still facing a high malaria burden 7, 8, 9.
Malaria control and elimination strategies heavily depend on timely, accurate diagnosis and effective treatment 10,11. Microscopy is a gold standard and common malaria diagnostic test in several African countries because of its high specificity, convenient with a rapid turnaround time, and is inexpensive. However, it has limited sensitivity especially for low parasitemia infections, which require highly competent microscopists complemented by molecular assays. An improved point-of-care detection method is critical because transmission caused by low parasitemia infections hinders the progress and goal of malaria elimination 10. Systematic identification and treatment of individuals with submicroscopic Plasmodium infections as part of the surveillance and intervention strategy would reduce and eliminate the parasite reservoirs that lead to transmission 11,12.
Another factor that impacts the risk of malaria infections is glucose-6-phosphate dehydrogenase deficiency (G6PDd), which is the most common enzymatic disorder of red blood cells, affecting 400 million people worldwide 13. G6PDd is an X-linked disorder with high prevalence particularly in people of African, Asian, and Mediterranean descent. The gene encoding the G6PD protein is polymorphic, with more than 400 variants. In Sub-Saharan Africa, G6PD* B, G6PD*A and G6PD*A- were the most common variants 16. The G6PD variants were relative homogeneous in America, Africa, and western Asia, sharply contrasted with the heterogeneity of variants in China and Southeast Asia. While individuals with G6PD-deficient alleles have selective advantage against severe malaria, they can still be infected with low plasmodium densities and contribute to the transmission reservoirs. The prevalence of G6PDd is high in areas where malaria is endemic 14. In Ethiopia, G6PDd was estimated to be 1–14% 15, but G6PD information is still lacking in most part of southwestern Ethiopia where malaria transmission is high.
The use of single dose primaquine has been recently adopted by the Ethiopian Federal Ministry of Health (FMoH) as a radical treatment regime in 239 districts that are targeted for elimination. However, such treatment regime will be provided without prior G6PD testing. This could pose a high risk to malaria patients who are G6PD deficient and treated with primaquine. Thus, information on the prevalence of submicroscopic infections and G6PD deficiency in malaria patents is necessary for accurate diagnosis and risk-free treatment. This study determined the prevalence and factors associated with submicroscopic malaria infections, the frequency of G6PD deficiency, and the association between G6PD phenotype and genotype among malaria suspected febrile individuals in Southwest part of Ethiopia.
MATERIALS AND METHODS
Ethics approval and consent to participate
The study protocol was reviewed and approved by Institutional Review Board (IRB) of Institute of Health, Jimma University (Ref. No. IHRPGD/711/20) and written informed consent/assent was obtained from all consenting heads of households, parents/guardians, and individuals who were willing to participate in the study. All experimental procedures were performed following the IRB approved protocol.
Study site and sample collection
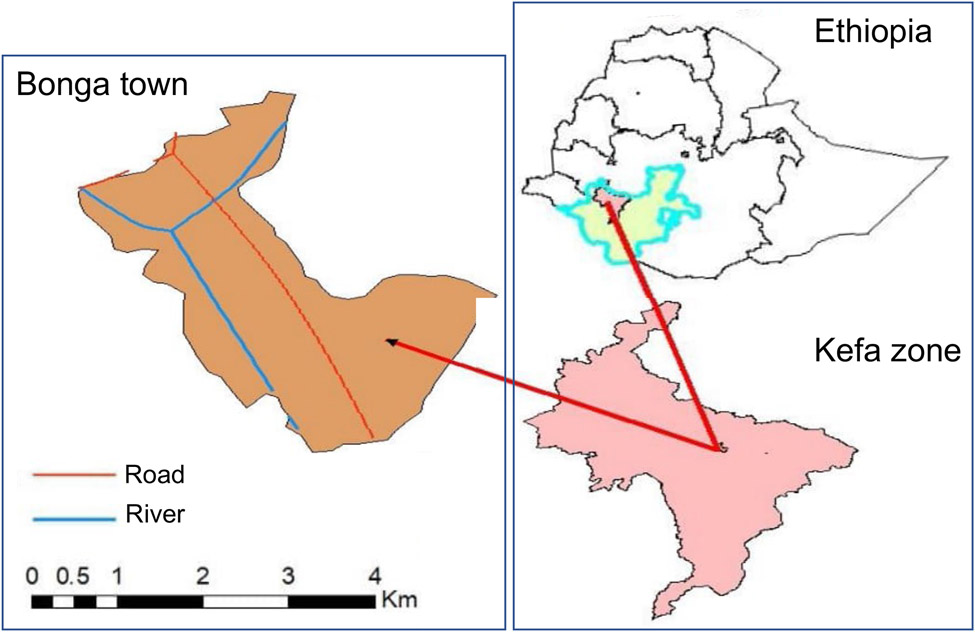
A total of 297 malaria suspected febrile patients were collected at the Bonga Gebretsadiek Shawo general hospital of Bonga town, Southwestern Ethiopia (7°16’N 36°14’E with an average elevation of 1,714 meters; Figure 1) from July to October 2020 based on a cross-sectional study design. Socio-demographic data including gender, age, occupation, records of antimalarial drug treatment, medical history, hemoglobin and G6PD levels (Table 1 & 3) was collected from each study participant. For participants aged below 18 years old, the questionnaire was completed by their guardians or parents. Finger-pricked blood sample of approximately 300μl was collected and preserved in a EDTA tube following standard WHO protocols 17. Thin and thick blood smears were prepared for microscopic examination of malaria parasites 18. A sample was considered as malaria-negative if no parasites were detected after examining 200 fields of the thick smear following standard WHO protocol 19, 20, 21. All slides were read in duplicate by two microscopists at the time of sample collection. For samples that showed discrepancy with qPCR results, we repeated the slide read for verification.
Figure 1.
Map of the study area.
Table 1.
Demographic characteristics of clinical malaria among suspected febrile individuals in Bonga, southwestern Ethiopia. * and ** represent a significant level of 0.05 and 0.01, respectively.
| Parameters | Number of samples |
Total infection |
Odds ratio (95% CI) |
P. vivax | Odds ratio (95% CI) |
P. falciparum | Odds ratio (95% CI) |
Mixed infection |
Odds ratio (95% CI) |
|---|---|---|---|---|---|---|---|---|---|
| Overall | |||||||||
| 297 | 23 (7.7%) | 17 (5.7%) | 12 (4.0%) | ||||||
| Gender | |||||||||
| Female | 176 (59.3%) | 29 | 1 | 14 (7.9%) | 1 | 10 (5.6%) | 1 | 5 (2.8%) | 1 |
| Male | 121 (40.7%) | 23 | 1.19[0.7–2.12] P=0.572 |
9 (7.4%) | 0.93[0.42–2.1] P=0.87 |
7 (5.7%) | 1.02[0.39–2.6] P=0.97 |
7 (5.7%) | 2.03[0.66–6.3] P=0.215 |
| Age | |||||||||
| ≥4 and <15 (%) | 5 (1.6%) | 3 | 1 | 2 (40%) | 1 | 1 (40%) | 1 | 0 | 1 |
| ≥15 and <35 (%) | 215 (72.3%) | 27 | 0.21[0.1–0.5] p=0.0001** |
16 (7.4%) | 0.18[0.057–0.6] P=0.005 |
13 (6.0%) | 0.30[0.1–1.9] P=0.20 |
8 (3.7%) | 0.47[0.03–7.3] P=0.591 |
| ≥35 and <50 (%) | 54 (18.1%) | 7 | 0.1[0.01–0.7] p=0.021* |
3 (5.5%) | 0.14[0.029–0.5] P=0.012 |
2 (3.7%) | 0.19[0.02–1.64] P=0.128 |
2 (3.7%) | 0.55[0.03–10.1] P=0.684 |
| ≥50 (%) | 23 (7.7%) | 5 | 0.2[0.02–1.43] p=0.106 |
2 (8.6%) | 0.22[0.039–1.2] P=0.079 |
1 (4.3%) | 0.22[0.02–2.92] P=0.249 |
2 (8.6%) | 1.25[0.07–22.8] P=0.88 |
| Occupation | |||||||||
| Indoor workera | 185 (62.2) | 32 | 1 | 12 (6.4%) | 1 | 14 (7.5%) | 1 | 6 (3.2%) | 1 |
| Open filed workerb | 112 (37.7) | 20 | 1.03[0.62–1.71] p=0.902 |
11 (9.8) | 1.51[0.69–3.32] P=0.299 |
3 (2.6%) | 0.35[0.104–1.2] P=0.096 |
6 (5.3%) | 1.65[0.55–4.99] P=0.374 |
Office clerks, teachers, shopkeepers, students, pre-school children and housekeeping (Indoor workers)
Farmers, daily laborer, construction workers, guardsman or soldiers, gardener, casual workers, and unemployed (Open filed workers)
Table 3.
Risk factors associated with clinical malaria among febrile individuals in Bonga, southwestern Ethiopia. * and ** represent a significant level of 0.05 and 0.01, respectively.
| Risk factors | Number of samples |
Total infection |
Odds ratio (95% CI) |
P. vivax | Odds ratio (95% CI) |
P. falciparum | Odds ratio (95% CI) |
Mixed infection | Odds ratio (95% CI) |
|---|---|---|---|---|---|---|---|---|---|
| Prior use of antimalarial drugs | |||||||||
| Yes | 81 (82.6%) | 12 | 2.52[0.4–18.1] p=0.358 |
2 (2.4%) | 0.42[0.04–4.4] P=0.467 |
5 (6.1%) | 2.41[0.14–41.74] P=0.544 |
5 (6.1%) | 2.41[0.14–41.7] P=0.544 |
| No | 17 (17.4%) | 1 | 1 | 1 (5.8%) | 1 | 0 | 1 | 0 | 1 |
| Bead nets usage | |||||||||
| Yes | 95(31.9%) | 26 | 1 | 10 (10.5%) | 1 | 6 (6.3%) | 1 | 6 (6.3%) | 1 |
| No | 202(68.0%) | 30 | 0.54[0.34–0.864] p=0.010** |
13 (6.4%) | 0.61[0.3–1.34] P=0.221 |
11 (5.4%) | 0.86[0.33–2.3] P=0.763 |
6 (2.9%) | 0.5[0.16–1.42] P=0.181 |
| Previously infected with malaria | |||||||||
| No | 199 (67%) | 39 | 1 | 20 (10.0%) | 1 | 12 (6.0%) | 1 | 7 (3.5%) | 1 |
| Yes | 98 (33%) | 13 | 0.63[0.32–1.24] p=0.179 |
3 (3.0%) | 0.31[0.1–1.0] P=0.050 |
5 (5.1%) | 0.85[0.31–2.334] P=0.746 |
5 (5.1%) | 1.5[0.5–4.6] P=0.516 |
| G6PD level | |||||||||
| Normal (%) | 214 (78.9%) | 37 | 0.82[0.33–2.1] p=0.674 |
17 (7.9%) | 0.8[0.2–3.023] P=0.691 |
13 (6.1%) | 0.58[0.141–2.4] P=0.446 |
7 (3.2%) | 1.4[0.1–23.6] P=0.817 |
| Intermediate (for female; %) | 38(14.0%) | 4 | 0.5[0.14–1.8] P=0.285 |
2 (5.2%) | 0.5[0.1–3.3] P=0.47 |
1 (2.6%) | 0.25[0.024–2.6] P=0.245 |
3 (7.8%) | 3.6[0.2–66.2] P=0.389 |
| Deficient (%) | 19(7.0%) | 4 | 1 | 2(10.5%) | 1 | 2 (10.5%) | 1 | 0 | 1 |
Parasite DNA extraction and molecular screening
For each sample, parasite DNA was extracted from a dried blood spot (~50 μl) using the Saponin/Chelex method 22. Plasmodium species was examined by quantitative PCR of the 18S rDNA gene using species-specific primers, for P. falciparum and P. vivax, respectively 23, 24. Amplification was performed in a 20 μl reaction mixture containing 2 μl of genomic DNA, 10 μl 2×SYBR Green qPCR Master Mix (Thermo Scientific), and 0.5 μM primer with an initial denaturation at 95°C for 3 min, followed by 45 cycles at 94°C for 30 sec, 55°C for 30 sec, and 68°C for 1 min with a final 95°C for 10 sec. This was followed by a melting curve step of temperature ranging from 65°C to 95°C with 0.5°C increments to determine the melting temperature of each amplified product. Each assay included positive controls of P. falciparum HB-2 767G (MRA-667) and P. vivax E. coli (MRA-178), in addition to negative controls including uninfected samples and nuclease-free water. A standard curve was produced from a 10-fold serial dilution of the control plasmids to determine the efficiency of qPCR. Melting curve analyses were performed for each amplified sample to confirm specific amplifications of the target sequence. Samples yielding threshold cycle (Ct value) higher than 38 (as indicated in the negative controls) were considered negative for Plasmodium species. Parasite density in a sample was quantified with the follow equation: GCN sample = 2 E×(38-Ct sample); where GCN stands for gene copy number, Ct for the threshold cycle of the sample, and E for amplification efficiency 25. The differences in the log-transformed parasite GCN between the microscopic-positive and -negative samples were assessed for significance at the level of P<0.05 by one-tailed t-tests.
Measuring G6PD phenotype
Blood samples from each participant were tested for G6PD enzyme levels by the careSTART™ POCT S1 system (Access Bio Inc.) following the manufacturer’s instructions. Two drops (20–30 μl) of finger-prick whole blood was transferred by micro-pipettes to a strip and inserted into the biosensor at room temperature. The G6PD level was displayed within four minutes and automatically recorded. G6PD normal and deficient individuals were categorized into two classes in male and three classes in female following the WHO classification 26, 27. The adjusted male median (AMM) G6PD activity, defined as the median G6PD activity of all male participants after excluding samples with less than 10% of the overall median activity, was calculated. For male, class I is G6PD deficient with < 30% of the AMM activity and class II is normal with > 30% of the AMM activity. For female, G6PD activity < 30%, 30–80%, and > 80% of the AMM activity are considered as G6PD deficient, intermediate, and normal, respectively 27.
G6PD genotyping
Four PCR assays were conducted using previously published primers to determine mutations in exons 2–11 of the G6PD gene (Supplementary Table 1). For each assay, water was used as a negative control. PCR amplification was conducted in a 20μl reaction mixture containing 2 μl of genomic DNA (~50 ng/μl), 10 μl of 2×Maxima SYBR Green PCR Master Mix (Thermo Fisher) and 0.3uM of each forward and reverse primers. Amplifications were performed with an initial denaturation at 94°C for 3 min, followed by 38 cycles at 94°C for 30 sec, 55°C for 30 sec and 72°C for 60 sec, with a final 6 min extension at 72°C. Amplified PCR products were separated by gel electrophoresis with 1.5% agarose gel at 120 V for 2.00 hours. Amplified PCR products were purified and sequenced on an ABI 3730xl DNA analyzer 28. Sequences were analyzed using ClustalX v2.1 and BioEdit v7.2 29. All sequences were aligned to the NCBI reference sequence (NG_009015.2) to verify the specificity of the PCR products. Samples with poor sequencing quality or showing singleton mutations were re-amplified and sequenced.
Statistical analyses
All data were analyzed using SPSS software package version 21.0. Descriptive statistics was used to summarize the socio-demographic characteristics of the study participants. Bivariate logistic regression was used to determine association of malaria infection with independent variables. Odds ratio and the corresponding 95% CI was calculated to determine the strength of the association. P-value < 0.05 was considered as statistically significant.
Results
Demographic characteristics of study participants
Among all patient samples, 121 (40.7%) were males and 176 (59.3%) were females (Table 1). About 112 (37.2%) participants were engaged in agriculture and open field work (farmers, construction workers, guardsmen and soldiers, gardeners); the remaining 185 (62.2%) were involved in work that is indoors (office clerks, teachers, shopkeepers, students, pre-school children, and housekeepers). The number of Plasmodium infection detected by qPCR (52 out of 297; 17.4%) was more than two-fold higher than that detected by microscopy (21 out of 297; 7.0%). Among the qPCR-positive samples, 23 (7.7%) were identified as P. vivax, 17 (5.7%) as P. falciparum, and 12 (4.0 %) as mixed infection (Table 2). Age group and bednet usage were significantly associated with Plasmodium infection (P<0.05). For those who aged ≥15 - <35 (AOR=0.21, 95% CI: 0.02–0.59, P=0.0001) and ≥35 - <50 (AOR=0.1, 95% CI: 0.01–0.7, P=0.021) were significantly more likely to have malaria infection than those aged below 15 and above 50. Also, those who did not use bednet had significantly higher odds for malaria infection (AOR=0.54, 95% CI: 0.34–0.86, P=0.01) than those who routinely used bednet. All the other variables did not show significant association with Plasmodium infection (P>0.05; Table 3)
Table 2.
Prevalence of submicroscopic infections among 297 malaria suspected febrile individuals in Bonga, southwestern Ethiopia.
| Total number of infections |
Number of P. vivax infections |
Number of P. falciparum infections |
Number of P. vivax and P. falciparum coinfections |
|
|---|---|---|---|---|
| Microscopy | 21 (7.0%) | 5 (1.6%) | 15 (5.0%) | 1 (0.3%) |
| qPCR | 52 (17.4%) | 23 (7.7%) | 17 (5.7%) | 12 (4.0%) |
Frequency of G6PD deficiency based on phenotypic assay
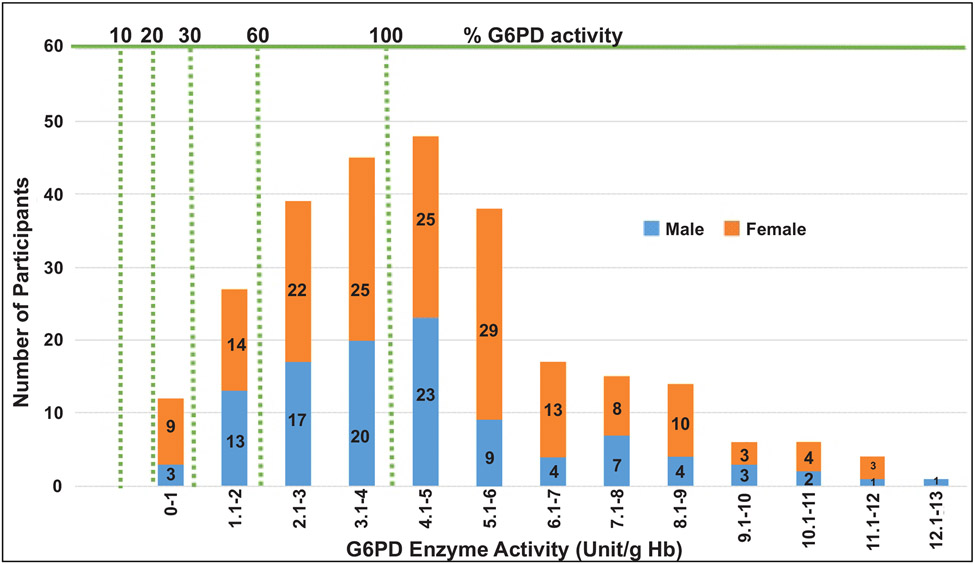
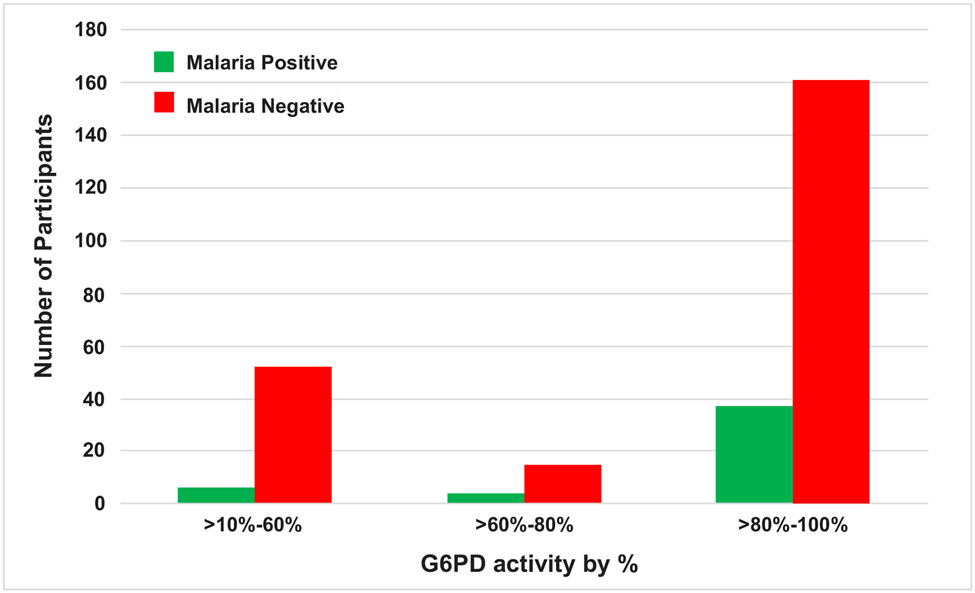
The adjusted median G6PD enzyme activity for male participants was calculated by excluding 26 participants who had enzyme activity less than 10% (i.e., below 0.405 U/g Hb) of the median value obtained for all male participants. The median G6PD activity for all study participants was 4.0 U/g Hb (range: <0.4–13.5 U/g Hb). The adjusted male median enzyme activity (4.05 U/g Hb) was considered 100% enzyme activity (Figure 2). Participants with enzyme activity between 0.4–1.215 U/g Hb (10%−30% of adjusted male median) were considered as deficient. Based on this cut-off value, 19 (6 males and 13 females; 7%) out of 271 participants were identified as deficient for G6PD enzyme activity, 38 (14.0%) had intermediate (for female) and 214 (78.9%) are normal (Table 4). For the six G6PD deficient males, four of them were between 4–35 years old, and two of them were between 35-≤50 years old. For the 13 G6PD deficient females, five of them were between 40–50 years old, and the remaining were younger than 18 years of age. Both P. vivax and P. falciparum infections were observed in G6PD deficient patients (Figure 3). No significant association was observed between G6PD level and Plasmodium infection (P>0.05; Table 3).
Figure 2.
A histogram to show G6PD enzyme activity levels for male and female participants compared to adjusted male median value.
Table 4.
G6PD phenotype distributions among male and female individuals in Bonga, southwestern Ethiopia.
| Sample size | Normal | Intermediate | Deficient | |
|---|---|---|---|---|
| Male | 107 | 101 (94.4%) | - | 6 (5.6%) |
| Female | 164 | 113 (68.9%) | 38 (23.2%) | 13 (7.9%) |
Figure 3.
The frequency of malaria infection by G6PD status.
Association between G6PD phenotype and genotype
No mutations were detected in C563T, G202A, A376G, nor ChrX:154535443 across all samples (Table 5). However, sequence analysis revealed three new mutations in exon 2 namely ChrX:6504 C→T (resulting in the substitution Arg → Thr), ChrX:6369 G→T (resulting in the substitution Ser → IIe), and ChrX:6664 G→C (resulting in the substitution Gln → His). Three of the individuals had normal G6PD activity and the others were G6PD deficient (Table 6).
Table 5.
Distributions of malaria cases by gender and G6PD genotype among malaria suspected febrile individuals in Bonga, southwestern Ethiopia.
| G6PD gene position |
Total | Malaria | Phenotype | Male | Female | ||||
|---|---|---|---|---|---|---|---|---|---|
| Deficient | Normal | Hemizygous | Normal | Heterozygous | Homozygous | Normal | |||
| C563T | 74 | Infected | 6 | 25 | 3 | 8 | 4 | 3 | 9 |
| Not infected | 17 | 41 | 6 | 11 | 1 | 11 | 14 | ||
| ChrX:154535443 | 75 | Infected | 7 | 24 | 3 | 10 | 4 | 4 | 10 |
| Not infected | 16 | 28 | 5 | 14 | 1 | 11 | 13 | ||
| A376G | 78 | Infected | 7 | 21 | 3 | 8 | 3 | 4 | 10 |
| Not infected | 18 | 32 | 6 | 16 | 2 | 12 | 14 | ||
| G202A | 75 | Infected | 7 | 24 | 3 | 10 | 4 | 4 | 10 |
| Not infected | 16 | 28 | 5 | 14 | 1 | 11 | 13 | ||
Table 6.
Distribution of the three new G6PD genotypes where mutations were detected among male and female individuals in Bonga, southwestern Ethiopia.
| Gender | N | G6PD genotype | |||||
|---|---|---|---|---|---|---|---|
| C to T at ChrX:6504 | G to T at ChrX:6369 | G to C at ChrX:6664 | |||||
| Wild type | Mutant | Wild type | Mutant | Wild type | Mutant | ||
| Male | 37 | 34 | 3 (T,T,T) | 33 | 4 (T,T,T,A) | 34 | 3 (T,A,A) |
| Female | 48 | 48 | 0 | 44 | 4 (T,C,A,A) | 46 | 2 (C) |
DISCUSSION
The Ethiopian government aims to eliminate malaria by 2030 30 but submicroscopic infections, relapses of P. vivax, and residual transmission pose major challenges to this goal 31, 32. Submicroscopic malaria infections are hidden parasite reservoirs as infected individuals were not identified and treated with antimalarial drugs. They can serve as the source of infection and contribute to transmission in the community and/or other malaria-free areas 33, 34, 35, thereby hindering malaria control and elimination. The present study showed that submicroscopic infections were high among malaria suspected febrile patients in the southwestern part of Ethiopia. The prevalence of submicroscopic malaria was comparable to previous studies in low-endemic settings such as Malo in southwestern Ethiopia, which reported a prevalence of 9.7% 36, 37; but much lower than that in southwestern Saudi Arabia, Senegal, and Uganda where submicroscopic infection was more than 23% 38, 39, 40. According to a systematic review of P. falciparum prevalence measured by both microscopy and PCR, the prevalence of infection by microscopy was on average 50.8% of that by PCR 30. This substantial discordance highlights the unreliability of microscopic diagnosis particularly in low transmission settings where infections are sparse and parasitemia is low. Among various age groups, individuals aged 15 – 50 were found with significantly higher risk for malaria infection than the others. Such pattern could be related to underlying medical conditions of the study patients, recent travel to high transmission areas, occupation, bednet usage, and/or relapse from previous infections 41.
Across the globe, the prevalence of G6PD deficiency varies by countries, regions, and localities, ranging from 5% to 30% in the Middle East, certain parts of the Mediterranean, and Asia 14, and 0.5 to 4% in Gambella, Oromiya, and Benishangule Gumuz of Ethiopia 42, 45. The frequency of G6PDd among malaria suspected individuals in Bonga areas as well as other parts of southwestern Ethiopia 42 was relatively low compared to other parts of Africa (as high as 35%) 43, 44. There are several reasons for such differences. In Ethiopia, multiple ethnic groups coexist and G6PDd varies by ethnic groups, ranging from 1.4 to 14.3% in the Nuer and Anuak (southwest Ethiopia) and Aregobas (northeast Ethiopia) regions 42, 45. In southern European countries, such as Greece and Italy, G6PDd prevalence ranged from 1–30% and 0–3% 46, respectively, much lower than that reported in Cameroon, Yemen, and Saudi Arabia (7.9–9%) 38, 17, 18. Based on our findings, the frequency of G6PDd was higher in females (7.9%) than in males (5.6%), similar to another study in southeast Iran that showed G6PDd in 18.9% of females and 10.8% of males 47. There could be several reasons for such a difference, such as the fact that X-chromosome inactivation tends to be more prevalent in elderly women than in young women. Our data indicated that nearly half of the G6PDd females were between 40–50 years old, and the remaining were 18 years old or younger. The higher frequency of X-chromosome inactivation in females may associate with an increase in malaria risk 48. Several G6PD variants have been previously identified, and the severity of the disorder varies from variant to variant. There are two major types of G6PD variants: the Mediterranean variant that occurs throughout Europe, Asia, and northern India, and is considered as the most severe form 49. The other type is the African variant, which is prevalent among Africans and is a mild form 50. Though it is yet unclear which of these G6PD variants is particularly associated with hemolytic anemia, our analyses did not indicate any association between G6PD mutations and hemolytic anemia in the Ethiopian P. vivax samples. There is a number of factors that determine the level of hemolysis, including the age of the RBC (with lower G6PD activity in older cells), the total dose of primaquine, and the type of G6PD variants 51. Previous studies have been shown that individuals with a non-severe variant of the G6PD gene are more likely to experience reduced hemoglobin level when the old RBCs with low G6PD activity are lysed upon exposure to primaquine 52. As a result, erythropoiesis increases and the lysed red blood cells are replaced by younger ones with higher levels of G6PD activity, which help stabilize and reverse anemia, as well as avoid further drop of hemoglobin after additional doses of PQ 52. By contrast, RBCs affected by a severe G6PD variant will display hemolysis regardless of whether RBCs are young or old; sustained exposure to an oxidizing agent will result in hemolysis. Continuous uptake of PQ by these patients will result in severe anemia and can be fatal if not treated promptly.
Among G6PD deficient individuals, the number of Plasmodium infection was comparable to G6PD normal individuals. Variation in G6PD level had no effect on the number of clinical cases of malaria. Previous study suggested that low level G6PD may increase sensitivity of P. vivax to oxidative stress 43. P. vivax parasites preferred to invade younger erythrocytes that possess high levels of G6PD enzyme 53, 54. Though enzyme levels are diminished in older erythrocytes, these erythrocytes are less preferable for P. vivax parasite invasion. Thus, there could be a protective effect of G6PD deficiency against parasite invasion 55, 56. The African form of G6PD deficiency has been recently shown to decrease malaria cases by 46% to 58% in endemic regions 57. Ninokata et al. (2006) 58 investigated 345 healthy adults and found that 10% of them were G6PD deficient but none had malaria infection 59. It has been shown that some G6PD variants could have no effect on the number of clinical cases of malaria but on P. vivax parasitemia 60. The mechanism by which this protection is conferred is still unclear. In this study, we found three novel non-synonymous mutations in exon 2 of the G6PD gene in both G6PD normal and deficient individuals. Future study should investigate the prevalence and impact of these mutations on malarial infections.
Conclusion
This study shows a higher prevalence of submicroscopic infections among individuals who did not use ITN and a significantly higher risk of malaria infections in adults. Submicroscopic malaria infections are hurdles against ongoing malaria control programs as they influence transmission dynamics and impose negative health and economic impacts. Sensitive diagnostic methods are needed to improve detection and treatment of these infections in health facilities especially in rural areas of Ethiopia. The use of a single low dose of primaquine to reduce malaria transmission and relapse has been recently adopted by the Ethiopian Federal Ministry of Health as a radical treatment regime for P. vivax in 239 districts that are targeted for elimination. This treatment regime requires wide-scale G6PD assessment given that Bonga, one of the targeted areas, showed a high prevalence of G6PD deficiency but no G6PD testing is available. This could pose a high hemolytic risk to malaria patients who are G6PD deficient and administered with primaquine. It is imperative to re-evaluate the implementation of this treatment regime and provide resources for G6PD assessment broadly across the country to mitigate the potential risk. The prevalence and clinical significance of novel mutations identified in exon 2 of the G6PD gene among G6PD deficient individuals merit further investigations.
Supplementary Material
Supplementary Table 1: PCR primer sequences and amplicon size of G6PD gene, Primer position can be referred to NCBI accession no. NG_009015.2.
Acknowledgements
We are greatly indebted to technicians and the staffs from Bonga Hospital for sample collection, the communities and Kefa zone health office for their support and willingness to participate in this research.
Funding
This research was funded by National Institutes of Health, grant number R01 AI162947.
List of abbreviations
- G6PD
Glucose-6-phosphate dehydrogenase
- PQ
Primaquine
- CQ
Chloroquine
- AMM
Adjusted Male Median
Footnotes
Competing interests
The authors declare no competing interests.
References
- 1.Legesse Y, Tegegn A, Belachew T, Tushune K. 2007. Knowledge, Attitude and Practice about Malaria Transmission and Its Preventive Measures among Households in Urban Areas of Assosa Zone, Western Ethiopia. Ethiop J Heal Dev. Vol. 21 (2): pp. 157–165 DOI: 10.4314/ejhd.v21i2.10044 [DOI] [Google Scholar]
- 2.Howard CT, McKakpo US, Quakyi IA, Bosompem KM, Addison EA, Sun K, Sullivan D, Semba RD., 2007. Relationship of hepcidin with parasitemia and anemia among patients with uncomplicated Plasmodium falciparum malaria in Ghana. Am J Trop Med Hyg;77(4):623–6. [PubMed] [Google Scholar]
- 3.Ghebreyesus TA, Haile M, Witten KH, Getachew A, Yohannes M, Lindsay SW, Byass P., 2000. Household risk factors for malaria among children in the Ethiopian highlands. Trans R Soc Trop Med Hyg. Jan-Feb;94(1):17–21. doi: 10.1016/s0035-9203(00)90424-3. [DOI] [PubMed] [Google Scholar]
- 4.Peterson I, Borrell LN, El-Sadr W, Teklehaimanot A., 2009. Individual and household level factors associated with malaria incidence in a highland region of Ethiopia: a multilevel analysis. Am J Trop Med Hyg. Jan;80(1):103–11. [PubMed] [Google Scholar]
- 5.World Malaria Report 2018. Geneva: World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- 6.Murray CJL., 2015. Choosing indicators for the health-related SDG targets. Lancet. Oct 3;386(10001):1314–1317. doi: 10.1016/S0140-6736(15)00382-7. [DOI] [PubMed] [Google Scholar]
- 7.Negash K, Kebede A, Medhin A, Argaw D, Babaniyi O, Guintran JO, Delacollette C., 2005. Malaria epidemics in the highlands of Ethiopia. East Afr Med J. Apr;82(4):186–92. doi: 10.4314/eamj.v82i4.9279. [DOI] [PubMed] [Google Scholar]
- 8.Guthmann JP, Bonnet M, Ahoua L, Dantoine F, Balkan S, van Herp M, Tamrat A, Legros D, Brown V, & Checchi F (2007). Death rates from malaria epidemics, Burundi and Ethiopia. Emerging infectious diseases, 13(1), 140–143. 10.3201/eid1301.060546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abraha MW, Nigatu TH, 2009. Modeling trends of health and health related indicators in Ethiopia (1995–2008): a time-series study. Health Res Policy Sys 7, 29 . 10.1186/1478-4505-7-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World malaria report 2017. Geneva: World Health Organization; 2017. Licence: CC BY-NC-SA 3.0 IGO [Google Scholar]
- 11.Nayyar GM, Breman JG, Newton PN, Herrington J., 2012. Poor-quality antimalarial drugs in southeast Asia and sub-Saharan Africa. Lancet Infect Dis. Jun;12(6):488–96. doi: 10.1016/S1473-3099(12)70064-6. Erratum in: Lancet Infect Dis. 2012 Jul;12(7):506. [DOI] [PubMed] [Google Scholar]
- 12.Lin JT, Saunders DL, Meshnick SR., 2014. The role of submicroscopic parasitemia in malaria transmission: what is the evidence? Trends Parasitol. Apr;30(4):183–90. doi: 10.1016/j.pt.2014.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nkhoma ET, Poole C, Vannappagari V, Hall SA, Beutler E., 2009. The global prevalence of glucose-6-phosphate dehydrogenase deficiency: a systematic review and meta-analysis. Blood Cells Mol Dis. May-Jun;42(3):267–78. doi: 10.1016/j.bcmd.2008.12.005. Epub 2009 Feb 23. [DOI] [PubMed] [Google Scholar]
- 14.Howes RE, Battle KE, Satyagraha AW, Baird JK, Hay SI., 2013. G6PD deficiency: global distribution, genetic variants and primaquine therapy. Adv Parasitol. ;81:133–201. doi: 10.1016/B978-0-12-407826-0.00004-7. [DOI] [PubMed] [Google Scholar]
- 15.WHO policy brief on single-dose primaquine as gametocytocide in Plasmodium falciparum malaria-2015. January
- 16.Olusanya BO, Osibanjo FB, Slusher TM., 2015. Risk factors for severe neonatal hyperbilirubinemia in low and middle-income countries: a systematic review and meta-analysis. PLoS One. Feb 12;10(2):e0117229. doi: 10.1371/journal.pone.0117229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al-Nood HA, Bazara FA, Al-Absi R, Al-Habori M., 2012. Glucose-6-Phosphate Dehydrogenase Deficiency among Male Blood Donors inSana’a City, Yemen. Oman Med J Jan; 27(1):46–49. Available from http://www.omjournal.org/fultext_PDF.aspx?DetailsID=194&type=fultext [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lauden SM, Chongwain S, Achidi A et al. 2019. Prevalence of glucose-6-phosphate dehydrogenase deficiency in Cameroonian blood donors. BMC Res Notes 12, 195. 10.1186/s13104-019-4226-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cheesbrough M (2006) District Laboratory Practice in Tropical Countries—Part 2. 2nd Edition, Cambridge University Press, New York. 10.1017/CBO9780511543470 [DOI] [Google Scholar]
- 20.Gillespie SH, Pearson RD. 2001. Principles and Practice of Clinical Parasitology Principles and Practice of Clinical Parasitology. Sciences-New York. ISBN 0–471-97729–2 (cased) QR251. P775, 616.9’ 6—dc21 00–047755 [Google Scholar]
- 21.Ogbodo SO, Nwagha UI, Okaka AN, Ogenyi SC, Okoko RO, Nwagha TU., 2009. Malaria parasitaemia among pregnant women in a rural community of eastern Nigeria; need for combined measures. Niger J Physiol Sci. Dec;24(2):95–100. doi: 10.4314/njps.v24i2.52923. [DOI] [PubMed] [Google Scholar]
- 22.Walsh PS, Metzger DA, Higuchi R., 1991. Chelex 100 as a medium for simple extraction of DNA for PCR-based typing from forensic material. Biotechniques. Apr;10(4):506–13. [PubMed] [Google Scholar]
- 23.Snounou G, Viriyakosol S, Zhu XP, Jarra W, Pinheiro L, do Rosario VE, Thaithong S, Brown KN., 1993. High sensitivity of detection of human malaria parasites by the use of nested polymerase chain reaction. Mol Biochem Parasitol. Oct;61(2):315–20. doi: 10.1016/0166-6851(93)90077-b. [DOI] [PubMed] [Google Scholar]
- 24.Johnston SP, Pieniazek NJ, Xayavong MV, Slemenda SB, Wilkins PP, da Silva AJ., 2006. PCR as a confirmatory technique for laboratory diagnosis of malaria. J Clin Microbiol. Mar;44(3):1087–9. doi: 10.1128/JCM.44.3.1087-1089.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lo E, Yewhalaw D, Zhong D, Zemene E, Degefa T, Tushune K, Ha M, Lee MC, James AA, Yan G., 2015. Molecular epidemiology of Plasmodium vivax and Plasmodium falciparum malaria among Duffy-positive and Duffy-negative populations in Ethiopia. Malar J. Feb 19;14:84. doi: 10.1186/s12936-015-0596-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organization. (2016). Testing for G6PD deficiency for safe use of primaquine in radical cure of P. vivax and P. ovale: Policy brief. World Health Organization. https://apps.who.int/iris/handle/10665/250297 [Google Scholar]
- 27.World Health Organization. (2016). In vitro diagnostics medical devices to identify Glucose-6-phosphate dehydrogenase (G6PD) activity. World Health Organization. https://apps.who.int/iris/handle/10665/252628. License: CC BY-NC-SA 3.0 IGO [Google Scholar]
- 28.Lo E, Zhong D, Raya B et al. , (2019). Prevalence and distribution of G6PD deficiency: implication for the use of primaquine in malaria treatment in Ethiopia. Malar J 18, 340 . 10.1186/s12936-019-2981-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clustal X2.1 is a windows interface for the multiple sequence alignment program https://clustalx.software.informer.com/2.1/ and BioEdit is a biological sequence alignment editor https://bioedit.software.informer.com/7.2/
- 30.Okell LC, Ghani AC, Lyons E, Drakeley CJ., 2009. Submicroscopic infection in Plasmodium falciparum-endemic populations: a systematic review and meta-analysis. J Infect Dis. Nov 15;200(10):1509–17. doi: 10.1086/644781. [DOI] [PubMed] [Google Scholar]
- 31.Graves PM, Richards FO, Ngondi J, Emerson PM, Shargie EB, Endeshaw T, Ceccato P, Ejigsemahu Y, Mosher AW, Hailemariam A, et al. , 2009. Individual, household and environmental risk factors for malaria infection in Amhara, Oromia and SNNP regions of Ethiopia. Trans R Soc Trop Med Hyg. Dec;103(12):1211–20. doi: 10.1016/j.trstmh.2008.11.016. Epub 2009 Jan 13. [DOI] [PubMed] [Google Scholar]
- 32.Minucci A, Gentile L, Zuppi C, Giardina B, Capoluongo E., 2012. Rapid and simple identification of the commonest glucose-6-phosphate dehydrogenase (G6PD) Italian mutations: from DNA extraction to genotyping. Clin Chim Acta. Jun 14;413(11–12):1018–9. doi: 10.1016/j.cca.2012.01.032. Epub 2012 Feb 4. [DOI] [PubMed] [Google Scholar]
- 33.Idris Z, Chan C, Kongere J et al. 2016. High and Heterogeneous Prevalence of Asymptomatic and Sub-microscopic Malaria Infections on Islands in Lake Victoria, Kenya. Sci Rep 6, 36958. 10.1038/srep36958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kaura T, Kaur J, Sharma A, Dhiman A, Pangotra M, Upadhyay AK, Grover GS, Sharma SK., 2019. Prevalence of submicroscopic malaria in low transmission state of Punjab: A potential threat to malaria elimination. J Vector Borne Dis.Jan-Mar;56(1):78–84. doi: 10.4103/0972-9062.257780. [DOI] [PubMed] [Google Scholar]
- 35.Arwati H, Yotopranoto S, Rohmah EA et al. 2018. Submicroscopic malaria cases play role in local transmission in Trenggalek district, East Java Province, Indonesia. Malar J 17, 2 . 10.1186/s12936-017-2147-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tadesse FG, van den Hoogen L, Lanke K, Schildkraut J, Tetteh K, Aseffa A, Mamo H, Sauerwein R, Felger I, Drakeley C, et al. , 2017. The shape of the iceberg: quantification of submicroscopic Plasmodium falciparum and Plasmodium vivax parasitaemia and gametocytaemia in five low endemic settings in Ethiopia. Malar J. Mar 3;16(1):99. doi: 10.1186/s12936-017-1749-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baum E, Sattabongkot J, Sirichaisinthop J et al. 2016. Common asymptomatic and submicroscopic malaria infections in Western Thailand revealed in longitudinal molecular and serological studies: a challenge to malaria elimination. Malar J 15, 333 . 10.1186/s12936-016-1393-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hawash Y, Ismail K, Alsharif K, & Alsanie W (2019). Malaria Prevalence in a Low Transmission Area, Jazan District of Southwestern Saudi Arabia. The Korean journal of parasitology, 57(3), 233–242. 10.3347/kjp.2019.57.3.233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vallejo AF, Chaparro PE, Benavides Y et al. 2015. High prevalence of sub-microscopic infections in Colombia. Malar J 14, 201. 10.1186/s12936-015-0711-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Katrak S, Nayebare P, Rek J, Arinaitwe E, Nankabirwa JI, Kamya M, Dorsey G, Rosenthal PJ, Greenhouse B., 2018. Clinical consequences of submicroscopic malaria parasitaemia in Uganda. Malar J. Feb 5;17(1):67. doi: 10.1186/s12936-018-2221-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schwartz Eli, Sadetzki Siegal, Murad Havi, Raveh David, 2001. Age as a Risk Factor for Severe Plasmodium falciparum Malaria in Nonimmune Patients, Clinical Infectious Diseases, Volume 33, Issue 10, 15 November, Pages 1774–1777, 10.1086/322522 [DOI] [PubMed] [Google Scholar]
- 42.Tsegaye A, Golassa L, Mamo H, Erko B., 2014. Glucose-6-phosphate dehydrogenase deficiency among malaria suspects attending Gambella hospital, southwest Ethiopia. Malar J. Nov 18;13:438. doi: 10.1186/1475-2875-13-438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Glucose-6-phosphate dehydrogenase deficiency. WHO Working Group. (1989). Bulletin of the World Health Organization, 67(6), 601–611. [PMC free article] [PubMed] [Google Scholar]
- 44.Sathupak S, Leecharoenkiat K & Kampuansai J, 2021. Prevalence and molecular characterization of glucose-6-phosphate dehydrogenase deficiency in the Lue ethnic group of northern Thailand. Sci Rep 11, 2956 . 10.1038/s41598-021-82477-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Assefa A, Ali A, Deressa W et al. 2018. Glucose-6-phosphate dehydrogenase (G6PD) deficiency in Ethiopia: absence of common African and Mediterranean allelic variants in a nationwide study. Malar J 17, 388 . 10.1186/s12936-018-2538-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Missiou-Tsagaraki S, 1991. Screening for glucose-6-phosphate dehydrogenase deficiency as a preventive measure: prevalence among 1,286,000 Greek newborn infants. J Pediatr. Aug;119(2):293–9. doi: 10.1016/s0022-3476(05)80747-4. [DOI] [PubMed] [Google Scholar]
- 47.McDonagh EM, Thorn CF, Bautista JM, Youngster I, Altman RB, & Klein TE 2012. PharmGKB summary: very important pharmacogene information for G6PD. Pharmacogenetics and genomics, 22(3), 219–228. 10.1097/FPC.0b013e32834eb313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Au WY, Lam V, Pang A, Lee WM, Chan JL, Song YQ, Ma ES, Kwong YL. 2006. Glucose-6-phosphate dehydrogenase deficiency in female octogenarians, nanogenarians, and centenarians. J Gerontol A Biol Sci Med Sci. Oct;61(10):1086–9. doi: 10.1093/gerona/61.10.1086. [DOI] [PubMed] [Google Scholar]
- 49.Beutler E. G6PD: population genetics and clinical manifestations. Blood Rev. 1996. Mar;10(1):45–52. doi: 10.1016/s0268-960x(96)90019-3. [DOI] [PubMed] [Google Scholar]
- 50.Ashley EA, Recht J, White NJ. Primaquine: the risks and the benefits. Malar J. 2014. Nov 3;13:418. doi: 10.1186/1475-2875-13-418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.John GK, Douglas NM, von Seidlein L, Nosten F, Baird JK, White NJ, Price RN. Primaquine radical cure of Plasmodium vivax: a critical review of the literature. Malar J. 2012. Aug 17;11:280. doi: 10.1186/1475-2875-11-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ashley EA, Recht J, White NJ. Primaquine: the risks and the benefits. Malar J. 2014. Nov 3;13:418. doi: 10.1186/1475-2875-13-418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Guindo A, Fairhurst RM, Doumbo OK, Wellems TE, Diallo DA. 2007. X-linked G6PD deficiency protects hemizygous males but not heterozygous females against severe malaria. PLoS Med. Mar;4(3):e66. doi: 10.1371/journal.pmed.0040066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brown M. (2009). Manson’s tropical diseases. The Lancet. Infectious Diseases, 9(7), 407–408. 10.1016/S1473-3099(09)70170-7 [DOI] [Google Scholar]
- 55.Garnham PCC (1966). Malaria parasites and other haemosporidia. Oxford: Blackwell. [Google Scholar]
- 56.ALLISON AC, & CLYDE DF (1961). Malaria in African children with deficient erythrocyte glucose-6-phosphate dehydrogenase. British medical journal, 1(5236), 1346–1349. 10.1136/bmj.1.5236.1346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mbanefo EC, Ahmed AM, Titouna A, Elmaraezy A, Trang NT, Phuoc Long N, Hoang Anh N, Diem Nghi T, The Hung B, Van Hieu M, Ky Anh N, Huy NT, & Hirayama K (2017). Association of glucose-6-phosphate dehydrogenase deficiency and malaria: a systematic review and meta-analysis. Scientific reports, 7, 45963. 10.1038/srep45963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ninokata A, Kimura R, Samakkarn U, Settheetham-Ishida W, & Ishida T (2006). Coexistence of five G6PD variants indicates ethnic complexity of Phuket islanders, Southern Thailand. Journal of human genetics, 51(5), 424–428. [DOI] [PubMed] [Google Scholar]
- 59.Ruwende C, Khoo SC, Snow RW, Yates SN, Kwiatkowski D, Gupta S, Warn P, Allsopp CE, Gilbert SC, Peschu N, et al. 1995. Natural selection of hemi- and heterozygotes for G6PD deficiency in Africa by resistance to severe malaria. Nature. Jul 20;376(6537):246–9. doi: 10.1038/376246a0. [DOI] [PubMed] [Google Scholar]
- 60.Louicharoen C, Patin E, et al. 2009. Positively selected G6PD-Mahidol mutation reduces Plasmodium vivax density in Southeast Asians. Science. Dec 11;326(5959):1546–9. doi: 10.1126/science.1178849. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1: PCR primer sequences and amplicon size of G6PD gene, Primer position can be referred to NCBI accession no. NG_009015.2.