Abstract
The resulting pandemic from the novel severe acute respiratory coronavirus 2, SARS-CoV-2 (COVID-19), continues to exert a strain on worldwide health services due to the incidence of hospitalization and mortality associated with infection. The aim of clinical services throughout the period of the pandemic and likely beyond to endemic infections as the situation stabilizes is to enhance safety aspects to mitigate transmission of COVID-19 while providing a high quality of service to all patients (COVID-19 positive and negative) while still upholding excellent medical standards. In order to achieve this, new strategies of clinical service operation are essential. Researchers have published peer-reviewed reference materials such as guidelines, experiences and advice to manage the resulting issues from the unpredictable challenges presented by the pandemic. There is a range of international guidance also from professional medical organizations, including best practice and advice in order to help imaging facilities adjust their standard operating procedures and workflows in line with infection control principles. This work provides a broad review of the main sources of advice and guidelines for radiology and nuclear medicine facilities during the pandemic, and also of rapidly emerging advice and local/national experiences as facilities begin to resume previously canceled non-urgent services as well as effects on imaging research.
Introduction
Since its emergence in December 2019, SARS-CoV-2, (COVID-19) has had a profound effect on healthcare systems across the world, 1 and no aspect of medical practice has gone unaffected. COVID-19 is a highly transmittable and pathogenic viral infection, with primary transmission being via respiratory droplets and fomites during close unprotected contact between an infector and an infectee. 2 Due to human-to-human transmission and a potentially high volume of asymptomatic carriers, radiology departments are required to implement appropriate infection prevention for the safety of all patients and staff. 3 This process has greatly impacted the way healthcare facilities operate in order to minimize risks associated with infection transmission.
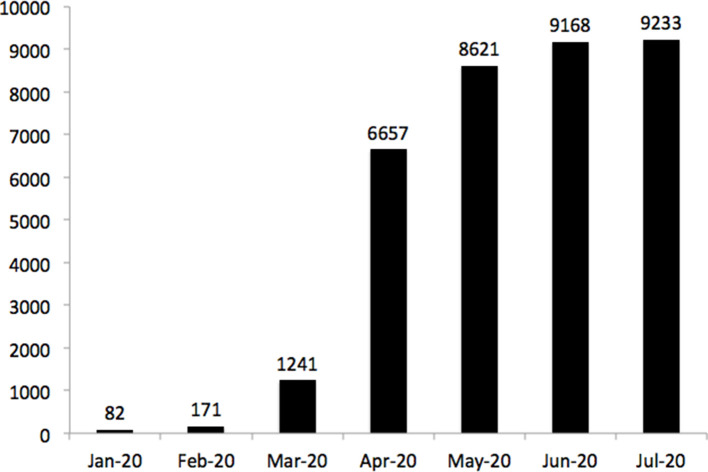
With the rapid publication of articles on the subject since the formal beginning of the pandemic in February (Figure 1), it is thus difficult to digest the rise in research related to administrative practice. This article aims to summarize current standings in international guidance for radiology and nuclear medicine services, as well as review the rapidly growing body of evidence of related peer-reviewed experience and evidence. We also present some emerging initiatives such as the use of artificial intelligence (AI) in COVID-19 stratification and diagnosis, and the effect of the pandemic on imaging research. Although some of the details in this work are time-sensitive due to the nature of the acute global emergency, we believe there is sufficient information to provide some key information and emerging concepts. Table 1 details the most relevant primary guidelines issued to help guide facilities in their local policies and responses to the pandemic.
Figure 1.
The rise in pre-print or accepted publications over all research areas on COVID-19. PubMED search terms Jan 1 2020–Feb 11 2020 “coronavirus” and Feb 11 2020–July 31 2020 “covid-19” or “covid19” in the title or abstract (to reflect the naming convention implemented by the World Health Organization on February 11 2020). Only articles in English were included.
Table 1.
Primary sources of general and modality-specific guidelines
| General facility guidelines | |
|---|---|
| Infection prevention and control and preparedness for COVID-19 in healthcare settings - third update 4 | European Center for Disease Prevention and Control |
| Health and medical surveillance during the coronavirus outbreak 5 | UK Health and Safety Executive |
| Rapid Review of the literature: Assessing the infection prevention and control measures for the prevention and management of COVID-19 in healthcare settings 6 | Health Protection Scotland |
| Coronavirus Disease 2019 (COVID-19) Treatment Guidelines 7 | National Institutes of Health |
| Information for Healthcare Professionals about Coronavirus (COVID-19) 8 | Centers for Disease Control and Prevention |
| Interventional Radiology | |
| BSIR Advice regarding COVID 19 pandemic 9 | British Society of Interventional Radiology |
| SIR COVID-19 toolkit 10 | Society of Interventional Radiology |
| Guidelines for vascular and interventional radiology units during the COVID-19 outbreak: A consensus statement from the Spanish Society of Vascular and Interventional Radiology (SERVEI) 11 | Spanish Society of Vascular and Interventional Radiology |
| Magnetic Resonance Imaging | |
| ACR Guidance on COVID-19 and MR Use 12 | American College of Radiology |
| SCMR’s COVID-19 Prepardness Toolkit 13 | Society of Cardiovascular Magnetic Resonance |
| Nuclear Medicine/PET services | |
| COVID-19 pandemic: Guidance for Nuclear Medicine Departments 14 | International Atomic Energy Association |
| COVID-19: guidance for infection prevention and control in nuclear medicine 15 | British Nuclear Medicine Society |
| BNMS Guidance for Covid-19 Recovery phases 16 | British Nuclear Medicine Society |
| Guidance and Best Practices for Nuclear Cardiology Laboratories during the Coronavirus Disease 2019 (COVID-19) Pandemic: An Information Statement from ASNC and SNMMI 17 | Society of Nuclear Medicine and Molecular Medicine/American Society of Nuclear Cardiology |
| Ultrasound services | |
| World Federation for Ultrasound in Medicine and Biology Position Statement: How to Perform a Safe Ultrasound Examination and Clean Equipment in the Context of COVID-19 18 | World Federation for Ultrasound in Medicine and Biology |
| COVID‐19: Infection prevention and control guidance for all ultrasound practitioners 19 | Australasian Society for Ultrasound in Medicine |
Facility &workforce guidance
Radiology facilities across the world rapidly implemented major changes to their services to mitigate the risk to staff and patients of COVID-19. The Centers for Disease Control and Prevention (CDC) in the USA has produced wide-ranging guidelines covering facility aspects such as planning and optimization of PPE, tools to estimate the surge in demand for imaging services, teleradiology, revenue concerns and mitigating staff shortages. 8 Facilities have been implementing a local infection control policy for their examination rooms and equipment from guidance such as those provided by local government and adapt their care to patients and staff accordingly. 4,20 Advice from UK health institutions have been provided on the effective use and implementation of personal protective equipment (PPE), 21 with further on-the-ground practical modifications such as a risk assessment of each and every patient, as suggested by the Society of Radiographers. 22 With potential staff absence due to illness, quarantine or family care, NHS England has requested health professionals to work beyond their usual scope of practice (along with employer retraining and supervision) as they likely have transferable skills in need throughout a hospital. 23
Examples of institutional practical experiences aimed at enhancing infection control and social distancing procedures specific to radiology can be found from countries initially impacted greatly by the pandemic such as the USA, 24 Netherlands, 25 China 26 and Italy. 27 Multi-centre comparisons of preparedness and ability to respond have also been performed in the USA by a scientific expert panel. 28 Facilities in countries such as Singapore, with previous experience of mitigation of SARS in 2003 and H1N1 in 2009, were quick to implement well-developed contingency plans and have documented their own experiences. 29,30
Safety measures for radiology staff to manage patients with known or suspected COVID-19 infection suggest implementation of a robust plan in radiology departments to prevent further transmission of the virus to patients and staff. 24 Manufacturers of equipment have also produced guidance on specific tools such as recommendations on CT imaging protocols for COVID-19 diagnostic scanning, reconfiguration of fluoroscopy systems for chest radiographs, remote workstation support flexibility and important equipment decontamination protocols. 31–33
As the pandemic evolves and further outbreaks become a possibility, organizations have adjusted their requirements of their imaging facilities and staff. For example, the European Association of Cardiovascular Imaging has produced recommendations on the suitability of cardiac imaging in patients with and without known COVID-19 infection and known or acute cardiac disease, the use of trans-esophageal echocardiography and fetal echocardiography as well as strategies to reduce cross-infection from patients and staff with a focus specifically on cardiac imaging examinations. 34
Telemedicine has become an integral part of patient management due to work at home notices. Investment into IT systems has facilitated remote working and robust platforms for virtual MDT meetings. This initiative is supported by many organizations such as the RCR and CDC, who have produced guidance around the IT requirements for working from home for radiologists such as attending MDTs and remote reporting of images with a relaxation of display guidance with home-based general display quality control of test patterns. 8
Regulatory guidance
With rapid changing of radiology services, legal enforcing agencies have responded with temporary measures on sites adapting to change. Examples include UK Ionizing Radiation (Medical Exposure) Regulations (IR(ME)R) inspectorates offering flexibility within the legislative and regulatory requirements, training due to transfer of staff, equipment quality control schedules, inspections and transfer of services. 35 For Nuclear Medicine facilities as backlogs grow due to the cancellation of non-urgent procedures, the UK Environment Agency has temporarily relaxed certain permit-specific reporting conditions for environmental release or monitoring of radioactive by-products. 36 The Association of Radioactive Substances Advisory Committee (ARSAC) has produced a temporary license to aid in the rapid transfer of existing radionuclide diagnostic services. 37 Under the Control of Substances Hazardous to Health regulations, occupational health technicians/responsible persons can administer an appropriate health questionnaire remotely and full assessments can be deferred for up to 6 months 5
General guidance on patient management
As sites react to the pandemic, clinical management of patients in radiology facilities has undergone rapid changes based on infection control needs. For example, modifications of imaging patients under general anesthesia have suggested that definitive COVID-19 diagnosis should be established before these studies should proceed, 38 and further research has investigated cross-infection rates following adjustments to anesthesia management protocols. 39
The UK Royal College of Radiologists (RCR) has produced guidance documents on the changing operations of clinical radiology and clinical oncology imaging, dealing with topics such as procedure-specific PPE, the role of CT in suspected COVID-19 positive patients, and the role of CT in cancer imaging during the pandemic. 40 As there remains a marked lack of availability of diagnostic services that form key parts of cancer management pathways, work continues to develop “COVID-19-protected” cancer hubs across the UK with robust isolation and testing protocols for the safe delivery of diagnostic services.
Although outside the scope of this review work of operational guidance, there are many papers describing clinical presentation and radiology features of COVID-19 on CT, 41 MRI, 42 ultrasound 43 and PET-CT. 44 Of note is that radiological chest imaging has been noted as “not useful” as a first-line diagnostic test for COVID-19 and should be reserved for hospitalized symptomatic patients with specific clinical indications. 45 Advice and guidelines have been issued by a wide range of organizations as to the proper use of CT and X-ray during the pandemic, such as by the American College of Radiology (ACR) 46 and a consensus statement by the Radiological Society of North America (RSNA). 47 Decision tools have been developed on how best to utilize imaging services in the workup of COVID-19 patients. 48 Further details of clinical presentation data can be found in radiology journals that have dedicated special focus websites with peer-reviewed articles on the topic of COVID-19, such as RSNA [https://pubs.rsna.org/2019-nCoV], The Lancet [https://www.thelancet.com/coronavirus/archive] and the American Journal of Roentgenology [https://www.ajronline.org/topic/cov19]. Decision-making tools and imaging recommendations have also been produced to aid low-to-middle income countries (LMIC) with screening and triage of hospitalized patients as they may not have the same imaging resources of wealthier nations. 49
Interventional radiology
Interventional radiology (IR) provides advanced image-guided treatments of a range of patient conditions, from the well to the vulnerable and from elective outpatients to critically ill intensive care unit patients. Advisory research from Singapore has published detailed preparedness techniques for IR services such as the set up of teams for outpatient and inpatient cases and on-call services, as well as specifying pathways and techniques to be taken with COVID-19 positive cases, PPE concerns and workload optimization. 29 Further Singaporean work has demonstrated the implementation and operation of isolation rooms and suggested staff movement pathways. 50 Other research has demonstrated practical considerations on how the IR theaters site design can be temporarily modified to minimize contagion (i.e., negative pressure theater for COVID-19 positive patients), and how patient workflow and standard operating procedures (SOPs) can be adjusted. 51 A 15-point guideline document from the British Society of Interventional Radiology have been produced with recommendations in a UK framework context including how to optimize caseload, risk stratification of staff and ensuring adequate provision of consumable supplies. 9 A recent consensus statement offers specific strategies in preventive measures and regulations, step by step for donning and doffing personal protective equipment, specific IR procedures which can not be delayed, and advice with high-risk aerosol-generating procedures in IR with COVID-19 positive patients. 11
MRI
A majority of MR procedures are elective outpatient procedures and therefore the current consensus is to minimize the use of MRI unless absolutely necessary. The ACR has produced general guidelines on the use of MRI covering a range of topics from room sanitization and room air exchanges for infection control, use of PPE and adhering to MR compliance of facemasks when entering Zone IV (inside the scanner room). 12 Staff accompanying infectious patients may be wearing respirators when they arrive at the MRI room, and MRI staff may be wearing a respirator as part of their PPE when dealing with these patients. Recent research has examined the MR safety of a range of respirators and facemasks for the presence of ferromagnetic properties. 52 Work has also investigated the MR safety of respiratory hoods and FFP3 facemasks provided by the UK Society of Radiographers. 22 These tests were not performed to American Society for Testing and Materials (ASTM) standards but serve as aids for sites considering their use.
Of concern for COVID-19 are the known cardiovascular complications of respiratory viral infections. 53 The Society for Cardiovascular Magnetic Resonance (SCMR) has published guidance on the approach to CMR requests, updated roles and staffing of CMR technologists, as well as practical implications of scanning ventilated COVID-positive patients. 13
Nuclear medicine
Nuclear medicine facilities come with added logistical considerations due to many producing their own radiopharmaceuticals in house, whether with generators ([99mTc] or [68Ga]) or a cyclotron. Sites may also import many radiopharmaceuticals for diagnostic and therapy uses and thus are heavily reliant on a complex supply chain of materials from a range of distributors likely to themselves be affected during the ongoing crisis. The International Atomic Energy Agency (IAEA) has published a series of webinars related to the pandemic, including on the challenges and guidance for nuclear medicine departments as well as potential issues on the global supply of radiopharmaceuticals. 14
The most recent updates from Nuclear Medicine Europe (NMEu) 54 state that the situation is gradually improving and there are no problems with medical isotope production facilities inside and outside of Europe. However there may still be short-term logistical issues with delivery due to port/airport closures related to remaining government imposed movement restrictions.
The European Association of Nuclear Medicine (EANM) guidance offers aid in adjustment and adaptation to the COVID-19 pandemic by presenting general recommendations for nuclear medicine departments to follow, based on a typical patient’s “journey” through the department. 55 National nuclear medicine organizations are publishing their own practice-based advice and guidelines based on local laws, practice and international guidance such as the British Nuclear Medicine Society (BNMS) 56,57 covering aspects such as postponement of certain examinations via a traffic light system, delivery of radiopharmaceuticals, legal considerations and extra reporting of lung CT scans if acquired as part of a SPECT-CT or PET-CT procedure.
The Society of Nuclear Medicine and Molecular Imaging (SNMMI) and American Society of Nuclear Cardiology (ASNC) published a statement related to the specific adaptations required of nuclear cardiology studies to mitigate transmission of COVID-19, such as single day imaging protocols, eliminating physical cardiac stress testing and social distancing during uptake phases of imaging. 17 A recent article from a number of leaders of nuclear medicine facilities worldwide details the practical precautions and on the ground experiences faced when implementing such rapid and radical changes as those promoted in guidelines. 58
A specific issue of concern in nuclear medicine involves ventilation/perfusion (VQ) pulmonary embolism scanning, which requires the use of aerosolized [99mTc]-DTPA leading to potentially aerosolized secretions, and is regarded as a high-risk procedure of cross-infection. A further complication is that the population of patients suspected of having pulmonary embolism have overlapping symptoms with individuals who are infected with COVID-19. Research has proposed, using perfusion-only scintigraphy, 59 CT pulmonary angiograms and performing VQ imaging together with precautions (i.e., technologists equipped with N95 masks, full PPE, decontamination procedures) only as a last resort. 60 For patients with contraindications for iodine contrast, a perfusion-only SPECT scan has been proposed as an alternative. 61
In regards to radionuclide therapy, BNMS guidelines also detail likely suspension of non-urgent cases of radionuclide, and a review of each patient on an individual basis for potential impact of therapy on the immune system (i.e., lutetium and radium therapies). Some imaging centers have also continued day-case radioiodine hyperthyroid treatments. 15
Ultrasound
The World Federation for Ultrasound in Medicine and Biology (WFUMB) and International Society of Ultrasound in Obstetrics & Gynecology (ISUOG) have produced comprehensive guidance on performing safe ultrasound examinations and cleaning of equipment in the context of the COVID-19 pandemic. 18,62 Of particular concern is ultrasound gel and transducers as transmission vectors and thus the recommendation is to use single-use gel packets for external ultrasound with a comprehensive cleaning regime. As viral RNA has been found in stool samples from COVID-19 infected patients, 63 considerations should also be made for transrectal ultrasound procedures.
Ultrasound has also been investigated as a replacement to a standard stethoscope in urgent care to reduce cross-infection. 64 Lung ultrasound has also been promoted in a diagnostic setting for suspected COVID-19 65 and also in pregnant patients. 66 Work has also suggested standardization techniques in COVID-19 positive patients for improvement of quantitation and reproducibility across sites. 67
As detailed above, a range of papers deals with the clinical identification and presentation of COVID-19 on lung ultrasound images. 43,68 In Italy, success has been obtained in designing a single-day training program to train gynecologists and obstetricians (with no lung imaging experience) in the recognition of the main lung ultrasound patterns of COVID-19. 69 Point-of-care ultrasound (POCUS) technology has recently been adapted to aid in front-line care, which utilize small hand-held ultrasound probes that connect to a smart phone. Such systems allow the triage of patients in tents or other areas outside the hospital facilities where imaging modalities are not available. In the USA, rules have been relaxed to aid patients or other non-medically trained persons to be guided using a standardized protocol under the remote supervision of a practitioner to acquire images for monitoring progress of COVID-19. 70 These systems are an important diagnostic tool, especially in low-to-middle income countries (LMIC) with fewer resources for traditional imaging facilities. POCUS also offers easier ability to disinfect equipment and also removes the need to spend time in proximity to the patient (identified as high-risk procedures). The importance of telemedicine has also been acknowledged as a potential solution of a reported lack of ultrasound training in LMIC, which was identified as being a primary barrier with the wider take up of POCUS. 71
Restarting of routine services
As the pandemic transitions from peak infections to mitigation of lower levels of endemic infection, the major challenge is to create a balance between the elevating demand of regular imaging services with a substantial backlog and mitigation of the spread of COVID-19, which instigated scaling back of services in the first instance. Recent US survey data have demonstrated over 90% of facilities have experienced a dramatic drop of examinations during the course of the pandemic, up to 70% in mammography, and a 47% drop in general nuclear medicine, MRI and fluoroscopic exams. 72 Expert opinions have been published as to how imaging facilities can enable transitions to a “new normal” of service. 73 An interesting change to work practices in the USA recently saw radiologists making house-calls, performing certain image-guided procedures in patients’ homes which lead to a reduction of emergency visits by 77%. 74
An important consideration in restarting suspended services is that of breast imaging such as screening and routine diagnostic mammograms and ultrasound, given the close contact and time required between sonographers and patients. UK numbers estimate a current screening backlog of 2.1 million scans, with 7000 referrals and 380 cancers being missed per week. 75 Recent Canadian breast imaging guidelines have reviewed best practice recommendations for maximal protection of staff and patients, such as pre-screening for COVID-19 symptoms at scheduling and at imaging times (with rescheduling for 2 weeks for symptomatic patients), staggered appointment times, PPE during examination, virtual reporting and consultation, and physical barriers during ultrasound imaging. 76 They also detail a series of four priority category definitions (emergent, urgent, semi-urgent, non-urgent) with corresponding imaging-specific indications and maximal time interval targets that can be adapted by imaging facilities for their own use. Further work from a USA breast cancer consortium outlined three priority categories A, B and C that reflect the urgency categories for clinical indications of surgical and medical breast oncology, as well as associated COVID-19 imaging considerations for these groups. 77 Recent research has also noted that patients experiencing delayed imaging and treatment of breast cancer, so far, are unaffected by worse survival rates. 78
A significant issue within the hospital setting involves staffing, with the testing of healthcare workers being highly promoted in order to reduce unnecessary quarantine, protect the workforce and reduce spread of atypical or asymptomatic cases. 79 Recent work examining infection rates of asymptomatic healthcare workers at a major London hospital demonstrated the importance of multi-timepoint surveillance by testing 400 workers weekly over 16 weeks, and crucially noting that asymptomatic infection among HCWs is low, and unlikely to be a major source of transmission. 80 Related work investigating asymptomatic rates in 554 HCWs in another London hospital demonstrated significantly higher antibody responses in symptomatic over asymptomatic HCWs, and that housekeeping staff accounted for 33% of asymptomatic HCW cases. This may be useful data that may inform future occupational healthcare practices. 81 An investigation of 37 asymptomatic people demonstrated that this group are significantly more contagious than symptomatic people, with a weaker antibody level, which may present implications for immunity strategies and serological surveys of HCWs. 82
ACR guidelines also provide details on the practical aspects of rescheduling and resumption of non-urgent screening programmes such as mammography screening, lung cancer screening, which are also slowly being restarted in the UK, albeit with significantly longer waiting lists. Recent suggestions in the USA have promoted moving these studies to facilities in areas with low incidence of COVID-19 as well as providing general considerations on coordinating facilities and workforce as non-urgent work gradually returns. 83 UK guidance by the RCR details working patterns on how to resume non-urgent elective workoutlining a priority scale of scan/procedure urgency, and a plan to maintain precautionary measures including a dedicated scanner for COVID-19 positive patients if possible. 84
Guidance issued by the BNMS on how to enact a recovery phase have cautioned careful planning and demonstrated a “traffic-light” system to assist with the decision-making process based on the urgency of the appointment. They also guide on the restarting of radionuclide therapies, radionuclide supplies and staffing concerns. 16 Together with the regulatory changes detailed above, sites will have more flexibility in scheduling procedures according this system. 36
Recent work has used a series of variables to plan a recovery of lost imaging volumes during the pandemic such as (1) severity of disease in the local region, including potential subsequent “waves” of infection; (2) lifting of government social distancing restrictions; (3) patient concerns; (4) management of demand for delayed imaging and capacity; (5) economics of health insurance and ability to pay for imaging; and (6) radiology practice profile (emergency, inpatient, outpatient mix and subspecialty types). 85 Related work has produced guidance for the resumption of work with a tiered priority system for patients whom imaging could be delayed with minimal clinical impact. 86 The ACR has produced follow-up recommendations to the resumption of services, with an overall principle of whether the risk of illness or death to a health care worker or patient from health care–acquired COVID-19 is greater than the risk of illness or death from delaying radiology care. The guidance provides a checklist to assess the potential risks to proceeding or postponing an examination that will be of great use to facilities with similar concerns 87
A theme in many countries restarting hospital services centers around the use of face coverings. Clear guidance from the RCR states that “face coverings should be worn by everyone in crowded areas where social distancing is not possible.” 88 PHE advises all patients (and visitors) to wear face covering when attending appointments. 20 UK institutes have used this guidance to develop their own local policies, leading to potential conflicts between facilities. In some countries such as Singapore, wearing a face cover for hospital appointments is less difficult to implement, as it is legal requirement during the pandemic.
Beyond the current pandemic, facilities are being urged to learn and adopt leadership techniques that can lead to greater success for the management of any future pandemics, i.e. further COVID-19 outbreaks in the form of a “second wave” or techniques that can be applied to other large-scale viral infections. Investigators have outlined take-away messages that can bolster the response a facility has to the COVID-19 outbreak 89 such as advocating for clear, concise communication of necessary information, gratitude for front-line staff, and maintaining an attitude of compassion for personnel who made unintended errors during such a stressful time.
Effects of the pandemic on imaging research
Owing to the nature of the rapid shutdown of non-urgent imaging services in response to the pandemic, clinical imaging research programs are likely to have lost valuable imaging data, suffered protocol deviations and be generally affected negatively in the near future. Major considerations will have to be made in order to complete ongoing studies from a logistical perspective, as well as ensuring patient safety and progression of grant applications. Examples of issues for future research include shifting priorities of funding bodies in response to COVID-19, cancellation (or moving online) of scientific meetings, suspension of near-future funding cycles, staff hiring freezes, release of academic clinical experts back to full-time clinical care and general lack of governmental funding available for imaging studies. 73 Charities that sponsor research projects have begun to scale back research plans due to mandatory cancellation of events, closure of charity outlets and a large drop in donations, with some charities projected to lose up to half of their annual fundraising income. 90 An international expert group of academic research program managers has highlighted their acute responses to research programs and reflections on the future of imaging, with an estimate of 1–2 years loss of research productivity. 91
Although this may seem like a bleak picture, new imaging research opportunities may present themselves within the context of infectious diseases, 92 for example the effects of “cytokine storm” due to COVID-19 in the brain. 42 Preliminary uses of artificial intelligence in the context of COVID-19 have recently begun emerging with the large amount of CT datasets acquired. A large study in China demonstrated that deep learning applied to almost 4500 chest CT scans has demonstrated an ability to discriminate COVID-19 from community acquired pneumonia and other non-pneumonic lung diseases with a sensitivity of 87%. 93 Strategies of how AI may be further leveraged have also been explored in a recent review paper. 94 Examples include the stratification of patients into those that may require ventilation, 95 AI-assisted diagnosis for classification of COVID-19 from other pneumonia, 96 and severity assessment of COVID-19. Other studies have investigated automated AI segmentation, 97 quantification of disease progression 98 and a multi-center study also investigated predictions of hospital stay based on classified disease severity, 99 as well as reducing staffing burden in triage situations by first radiological read by AI rather than double-read by humans. In order to aid with AI training, the RSNA has developed a freely available COVID-19 imaging repository. 100 The aim of the datasets is to allow investigation of epidemiological trends and to generate new AI algorithms to assist with COVID-19 disease detection, differentiation from other pneumonias and quantification of lung involvement on CT for prognosis or therapy planning.
Conclusion
There are numerous professional guidelines and advice for imaging facilities to turn to during the course of the current COVID-19 pandemic. National regulators have demonstrated flexibility with registrants regarding certain key aspects of legal implications. Peer-reviewed experience and observations will be a key factor in how professional organizations issue advise and guidelines to their members, and in turn how imaging sites can implement these guidelines safely and in consideration for the best possible outcomes for their patients and staff. As the course of the pandemic evolves from emergency response to restarting non-urgent services, it is imperative that this is done with a clear aim to suppress any further transmission of COVID-19.
Contributor Information
Jim O' Doherty, Email: jim.odoherty@nus.edu.sg.
Sophie O' Doherty, Email: sophie.odoherty@nus.edu.sg.
Carla Abreu, Email: carla.abreu@icr.ac.uk.
Ana Aguiar, Email: anamariaasguiar@gmail.com.
Anthonin Reilhac, Email: areilhac@nus.edu.sg.
Edward Robins, Email: edward_robins@sbic.a-star.edu.sg.
REFERENCES
- 1. Tanne JH, Hayasaki E, Zastrow M, Pulla P, Smith P, Rada AG. Covid-19: how doctors and healthcare systems are tackling coronavirus worldwide. BMJ 2020; 368: m1090. doi: 10.1136/bmj.m1090 [DOI] [PubMed] [Google Scholar]
- 2. Guo Y-R, Cao Q-D, Hong Z-S, Tan Y-Y, Chen S-D, Jin H-J, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil Med Res 2020; 7: 11. doi: 10.1186/s40779-020-00240-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nishiura H, Kobayashi T, Miyama T, Suzuki A, Jung S-M, Hayashi K, et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19. Int J Infect Dis 2020; 94: 154–5. doi: 10.1016/j.ijid.2020.03.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. European Centre for Disease Prevention and Control Infection prevention and control and preparedness for COVID-19 in healthcare settings - third update.. ; 2020. Available from: https://www.ecdc.europa.eu/en/publications-data/infection-prevention-and-control-and-preparedness-covid-19-healthcare-settings [cited 23 June 2020].
- 5. Health and Safety Executive Health and medical surveillance during the coronavirus outbreak.. Available from: https://www.hse.gov.uk/coronavirus/health-surveillance.htm [cited 03 May 2020].
- 6. Health Protection Scotland Rapid review of the literature: assessing the infection prevention and control measures for the prevention and management of COVID-19 in healthcare settings. Public Health Scotland; 2020;. cited 25th June 2020. [Google Scholar]
- 7. COVID-19 Treatment Guidelines Panel Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health;.. Available from: https://www.covid19treatmentguidelines.nih.gov/ [cited 23 June 2020]. [PubMed]
- 8. Centers for Disease Control and Prevention Information for Healthcare Professionals about Coronavirus (COVID-19).. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/index.html [cited 23 June 2020].
- 9. British Society of interventional radiology. BSIR advice regarding Covid 19 pandemic. BSIR; [. cited 03 May 2020. [Google Scholar]
- 10. Society of Interventional Radiology COVID-19 Toolkit. 2020. Available from: https://www.sirweb.org/practice-resources/toolkits/covid-19-toolkit/ [cited 03 May 2020].
- 11. De Gregorio MA, Guirola JA, Magallanes M, Palmero J, Pulido JM, Blazquez J, et al. COVID-19 outbreak: infection control and management protocol for vascular and interventional radiology Departments—Consensus document. Cardiovasc Intervent Radiol 2020; 43: 1208–15. doi: 10.1007/s00270-020-02493-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. American College of Radiology ACR Guidance on COVID-19 and MR Use.. Available from: https://www.acr.org/Clinical-Resources/Radiology-Safety/MR-Safety/COVID-19-and-MR-Use [cited 30th April 2020].
- 13. Society for Cardiovascular Magnetic Resonance SCMR's COVID-19 prepardness toolkit.. ; 2020. Available from: https://scmr.org/page/COVID19 [cited 28th April 2020].
- 14. International Atomic Energy Agency COVID-19 pandemic: guidance for nuclear medicine departments. IAEA 2020;. cited 28th April 2020. [Google Scholar]
- 15. British Nuclear Medicine Society COVID-19: Guidance for infection prevention and control in nuclear medicine.. Available from: https://cdn.ymaws.com/www.bnms.org.uk/resource/resmgr/news_&_press_office/news/new_060420_nuclear_medicine_.pdf [cited 28th April 2020]. [DOI] [PubMed]
- 16. British Nuclear Medicine Society BNMS guidance for Covid-19 recovery phases.. London, UK: British Nuclear Medicine Society. cited 02 May 2020. [Google Scholar]
- 17. Skail H, Murthy VL, Al-Mallah MH, Bateman TM, Beanland R, Better N, et al. Guidance and best practices for nuclear cardiology laboratories during the coronavirus disease 2019 (COVID-19) pandemic: an information statement from ASNC and SNMMI. J Nucl Cardiol 2020;Preprint. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. World Federation for ultrasound in M, biology safety C, Abramowicz JS, Basseal JM. world Federation for ultrasound in medicine and biology position statement: how to perform a safe ultrasound examination and clean equipment in the context of COVID-19. Ultrasound Med Biol 2020; 46: 1821–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Basseal JM, Westerway SC, McAuley T. COVID‐19: infection prevention and control guidance for all ultrasound practitioners. Australas J Ultrasound Med 2020; 23: 90–5. doi: 10.1002/ajum.12210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. England PH. COVID-19: infection prevention and control (IPC. Public Health England 2020;. cited 24 June 2020. [Google Scholar]
- 21. Public Health England COVID-19: infection prevention and control (IPC. 2020;. ; . cited 02 May 2020.
- 22. Society of Radiographers Sor Covid-19 information and resources. Society of RadiographersAvailable from. cited 02 May 2020. [Google Scholar]
- 23. England NHS. Letter: Supporting allied health professionals and allied health professional support workers during the COVID-19 epidemic in the UK.NHS England Letter]. Available from. Available from: https://www.england.nhs.uk/coronavirus/publication/letter-supporting-allied-health-professionals-and-allied-health-professional-support-workers-during-the-covid-19-epidemic-in-the-uk/ [cited 05 May 2020].
- 24. Kooraki S, Hosseiny M, Myers L, Gholamrezanezhad A, Coronavirus GA. Coronavirus (COVID-19) outbreak: what the Department of radiology should know. Journal of the American College of Radiology 2020; 17: 447–51. doi: 10.1016/j.jacr.2020.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kwee TC, Pennings JP, Dierckx RAJO, Yakar D. The crisis after the crisis: the time is now to prepare your radiology department. Journal of the American College of Radiology 2020; 17: 749–51. doi: 10.1016/j.jacr.2020.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Huang Z, Zhao S, Li Z, Chen W, Zhao L, Deng L, et al. The battle against coronavirus disease 2019 (COVID-19): emergency management and infection control in a radiology department. Journal of the American College of Radiology 2020; 17: 710–6. doi: 10.1016/j.jacr.2020.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Laghi A, Grassi R. Italian Radiology’s Response to the COVID-19 Outbreak. Journal of the American College of Radiology 2020; 17: 699–700. doi: 10.1016/j.jacr.2020.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mossa-Basha M, Meltzer CC, Kim DC, Tuite MJ, Kolli KP, Tan BS. Radiology Department Preparedness for COVID-19: Radiology Scientific Expert Review Panel. Radiology 2020; 296: E106–12. doi: 10.1148/radiol.2020200988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gogna A, Punamiya S, Gopinathan A, Irani F, Toh LHW, Wen Cheong LH, et al. Preparing IR for COVID-19: the Singapore experience. Journal of Vascular and Interventional Radiology 2020; 31: 869–75. doi: 10.1016/j.jvir.2020.03.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Goh Y, Chua W, Lee JKT, Ang BWL, Liang CR, Tan CA, et al. Operational Strategies to Prevent Coronavirus Disease 2019 (COVID-19) Spread in Radiology: Experience From a Singapore Radiology Department After Severe Acute Respiratory Syndrome. Journal of the American College of Radiology 2020; 17: 717–23. doi: 10.1016/j.jacr.2020.03.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Healthcare GE. Cleaner and Disinfectant Material Compatibility.. Available from: https://cleaning.gehealthcare.com [cited 02 May 2020].
- 32. Healthineers S. The role of Siemens Healthineers in the COVID-19 pandemic. Siemens Healthineers.. Available from: https://www.siemens-healthineers.com/en-uk/press-room/press-features/pf-covid-19.html [cited 02 May 2020].
- 33. Healthcare P. Support for the Imaging community battling COVID-19.. Available from: https://www.philips.com.sg/healthcare/medical-specialties/covid-19/precision-diagnostics-addressing-covid - education_and_resources [cited 02 May 2020].
- 34. Skulstad H, Cosyns B, Popescu BA, Galderisi M, Salvo GD, Donal E, et al. COVID-19 pandemic and cardiac imaging: EACVI recommendations on precautions, indications, prioritization, and protection for patients and healthcare personnel. Eur Heart J Cardiovasc Imaging 2020; 21: 592–8. doi: 10.1093/ehjci/jeaa072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Care Quality Commission Coronavirus (COVID-19): Changes to IR(ME)R procedures.. Available from: https://www.cqc.org.uk/sites/default/files/20200401_Covid-19_IRMER_national_response_updatedv2.pdf [cited 04 May 2020].
- 36. UK Environment Agency COVID-19 and exceeding permit limits for medical use of radioactive substances: Rps C15. United Kingdom: UK environment agency. 2020;. cited 01 May 2020.
- 37. Administration of radioactive substances Advisory Committee. COVID-19: temporary employer Licence application form. Uk: Arsac; [. cited 03 May 2020. [Google Scholar]
- 38. Mossa-Basha M, Medverd J, Linnau K, Lynch JB, Wener MH, Kicska G, et al. Policies and guidelines for COVID-19 preparedness: experiences from the University of Washington. Radiology 2020; 201326. [DOI] [PubMed] [Google Scholar]
- 39. Zhao S, Ling K, Yan H, Zhong L, Peng X, Yao S, et al. Anesthetic management of patients with COVID 19 infections during emergency procedures. J Cardiothorac Vasc Anesth 2020; 34: 1125–31. doi: 10.1053/j.jvca.2020.02.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Royal College of radiologists. coronavirus (COVID-19): clinical information. London, UK2020 [28th 2020;Available from. [Google Scholar]
- 41. Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis 2020; 20: 425–34. doi: 10.1016/S1473-3099(20)30086-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Poyiadji N, Shahin G, Noujaim D, Stone M, Patel S, Griffith B. COVID-19–associated acute hemorrhagic necrotizing encephalopathy: imaging features. Radiology 2020; 296: E119–20. doi: 10.1148/radiol.2020201187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Buonsenso D, Piano A, Raffaelli F, Bonadia N, de Gaetano Donati K, Franceschi F. Point-Of-Care lung ultrasound findings in novel coronavirus disease-19 pnemoniae: a case report and potential applications during COVID-19 outbreak. Eur Rev Med Pharmacol Sci 2020; 24: 2776–80. [DOI] [PubMed] [Google Scholar]
- 44. Qin C, Liu F, Yen T-C, Lan X. 18F-Fdg PET/CT findings of COVID-19: a series of four highly suspected cases. Eur J Nucl Med Mol Imaging 2020; 47: 1281–6. doi: 10.1007/s00259-020-04734-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Shen K-L, Yang Y-H, Jiang R-M, Wang T-Y, Zhao D-C, Jiang Y, et al. Updated diagnosis, treatment and prevention of COVID-19 in children: experts’ consensus statement (condensed version of the second edition. World J Pediatr 2020; 16: 232–9. doi: 10.1007/s12519-020-00362-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. American College of Radiology ACR Recommendations for the use of Chest Radiography and Computed Tomography (CT) for Suspected COVID-19 Infection.. Available from: https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection [cited 30th April 2020].
- 47. Simpson S, Kay FU, Abbara S, Bhalla S, Chung JH, Chung M, et al. Radiological Society of North America Expert Consensus Statement on Reporting Chest CT Findings Related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA - Secondary Publication. J Thorac Imaging 2020; 35: 219–27. doi: 10.1097/RTI.0000000000000524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. British Society of thoracic imaging. radiology decision tool for suspected COVID-19. British Society of Thoracic Imaging; [Available from. cited 29 April 2020. [Google Scholar]
- 49. Mendel J, Lee J, Rosman D. Current concepts imaging in COVID-19 and the challenges for low and middle income countries. Journal of Global Radiology 2020; 6: 1106. doi: 10.7191/jgr.2020.1106 [DOI] [Google Scholar]
- 50. Too CW, Wen DW, Patel A, Abdul Syafiq AR, Liu J, Leong S, et al. Interventional radiology procedures for COVID-19 patients: how we do it. Cardiovasc Intervent Radiol 2020; 43: 827–36. doi: 10.1007/s00270-020-02483-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Zhu H-D, Zeng C-H, Lu J, Teng G-J. COVID-19: what should interventional radiologists know and what can they do? Journal of Vascular and Interventional Radiology 2020; 31: 876–81. doi: 10.1016/j.jvir.2020.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Murray OM, Bisset JM, Gilligan PJ, Hannan MM, Murray JG. Respirators and surgical facemasks for COVID-19: implications for MRI. Clin Radiol 2020; 75: 405–7. doi: 10.1016/j.crad.2020.03.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Xiong T-Y, Redwood S, Prendergast B, Chen M. Coronaviruses and the cardiovascular system: acute and long-term implications. Eur Heart J 2020; 41: 1798–800. doi: 10.1093/eurheartj/ehaa231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Nuclear medicine Europe (NMEu) emergency response team. updates from the emergency response team. NMEu; 2020 [29th 2020;Available from. [Google Scholar]
- 55. Paez D, Gnanasegaran G, Fanti S, Bomanji J, Hacker M, Sathekge M, et al. COVID-19 pandemic: guidance for nuclear medicine departments. Eur J Nucl Med Mol Imaging 2020; 47: 1615–9. doi: 10.1007/s00259-020-04825-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Buscombe JR, Notghi A, Croasdale J, Pandit M, O'Brien J, Graham R, et al. COVID-19: guidance for infection prevention and control in nuclear medicine. Nucl Med Commun 2020; 41: 499–504. [DOI] [PubMed] [Google Scholar]
- 57. Huang HL, Allie R, Gnanasegaran G, Bomanji J. COVID19 -nuclear medicine departments. be prepared! Nucl Med Commun 2020; 41: 297–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Czernin J, Fanti S, Meyer PT, Allen-Auerbach M, Hacker M, Sathekge M, et al. Nuclear medicine operations in the times of COVID-19: strategies, precautions, and experiences. J Nucl Med 2020; 61: 626–9. doi: 10.2967/jnumed.120.245738 [DOI] [PubMed] [Google Scholar]
- 59. Zuckier LS, Moadel RM, Haramati LB, Freeman LM. Diagnostic evaluation of pulmonary embolism during the COVID-19 pandemic. J Nucl Med 2020; 61: 630–1. doi: 10.2967/jnumed.120.245571 [DOI] [PubMed] [Google Scholar]
- 60. Zuckier LS, Gordon SR. COVID-19 in the nuclear medicine department. be prepared for ventilation scans as well! Nucl Med Commun 2020; 41: 494–5. [DOI] [PubMed] [Google Scholar]
- 61. Burger IA, Niemann T, Patriki D, Fontana F, Beer J-H. Is there a role for lung perfusion [99mTc]-MAA SPECT/CT to rule out pulmonary embolism in COVID-19 patients with contraindications for iodine contrast? Eur J Nucl Med Mol Imaging 2020; 47: 2062–3. doi: 10.1007/s00259-020-04837-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Poon LC, Abramowicz JS, Dall'Asta A, Sande R, Haar G, Maršal K, et al. ISUOG Safety Committee Position Statement on safe performance of obstetric and gynecological scans and equipment cleaning in context of COVID‐19. Ultrasound Obstet Gynecol 2020; 55: 709–12. doi: 10.1002/uog.22027 [DOI] [PubMed] [Google Scholar]
- 63. Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med 2020; 382: 929–36. doi: 10.1056/NEJMoa2001191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Buonsenso D, Pata D, Chiaretti A. COVID-19 outbreak: less stethoscope, more ultrasound. The Lancet Respiratory Medicine 2020; 8: e27: e27. doi: 10.1016/S2213-2600(20)30120-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Soldati G, Smargiassi A, Inchingolo R, Buonsenso D, Perrone T, Briganti DF, et al. Is There a Role for Lung Ultrasound During the COVID ‐19 Pandemic? J Ultrasound Med 2020; 39: 1459–62. doi: 10.1002/jum.15284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Buonsenso D, Raffaelli F, Tamburrini E, Biasucci DG, Salvi S, Smargiassi A, et al. Clinical role of lung ultrasound for diagnosis and monitoring of COVID‐19 pneumonia in pregnant women. Ultrasound Obstet Gynecol 2020; 56: 106–9. doi: 10.1002/uog.22055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Soldati G, Smargiassi A, Inchingolo R, Buonsenso D, Perrone T, Briganti DF, et al. Proposal for international standardization of the use of lung ultrasound for patients with COVID-19: a simple, quantitative, reproducible method. J Ultrasound Med 2020; 39: 1413–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Volpicelli G, Gargani L. Sonographic signs and patterns of COVID-19 pneumonia. Ultrasound J 2020; 12: 22. doi: 10.1186/s13089-020-00171-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Buonsenso D, Moro F, Inchingolo R, Smargiassi A, Demi L, Soldati G, et al. Effectiveness of rapid lung ultrasound training program for gynecologists and obstetricians managing pregnant women with suspected COVID‐19. Ultrasound Obstet Gynecol 2020; 56: 110–1. doi: 10.1002/uog.22066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Huang G, Vengerovsky A, Morris A, Town J, Carlbom D, Kwon Y. Development of a COVID-19 point-of-care ultrasound protocol. Journal of the American Society of Echocardiography 2020; 33: 903–5. doi: 10.1016/j.echo.2020.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Shah S, Bellows BA, Adedipe AA, Totten JE, Backlund BH, Sajed D. Perceived barriers in the use of ultrasound in developing countries. Crit Ultrasound J 2015; 7: 28. doi: 10.1186/s13089-015-0028-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Pablos T. Pandemic paralysis: COVID-19 has major impact on imaging. Aunt Minne. cited 05 May 2020. [Google Scholar]
- 73. Luker GD, Boettcher AN. Transitioning to a New Normal after COVID-19: Preparing to Get Back on Track for Cancer Imaging. Radiology: Imaging Cancer; 2020. 2(3):e204011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Golewale N. Sinha S. a novel health care delivery Model-House call docs. Society of Interventional Radiology 2020 Virtual; 13/6/2020; Virtual. Indiana, United States 2020;. [PubMed] [Google Scholar]
- 75. Cancer Research UK Over 2 million people waiting for cancer screening, tests and treatment. Cancer Research UK. 2020. Available from: https://scienceblog.cancerresearchuk.org/2020/06/01/impact-of-coronavirus-on-cancer-services-revealed-over-2-million-people-waiting-for-screening-tests-and-treatments/. [cited 6th Aug 2020].
- 76. Seely JM, Scaranelo AM, Yong-Hing C, Appavoo S, Flegg C, Kulkarni S, et al. COVID-19: safe guidelines for breast imaging during the pandemic. Can Assoc Radiol J 2020; 846537120928864. [DOI] [PubMed] [Google Scholar]
- 77. Dietz JR, Moran MS, Isakoff SJ, Kurtzman SH, Willey SC, Burstein HJ, et al. Recommendations for prioritization, treatment, and triage of breast cancer patients during the COVID-19 pandemic. The COVID-19 pandemic breast cancer Consortium. Breast Cancer Res Treat 2020; 181: 487–97. doi: 10.1007/s10549-020-05644-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Minami CA, Kantor O, Weiss A, Nakhlis F, King TA, Mittendorf EA.;In Press Association between time to operation and pathological stage in ductal carcinoma in situ and early-stage hormone receptor-positive breast cancer. Journal of the Americal College of surgeons. 2020.. [DOI] [PMC free article] [PubMed]
- 79. Black JRM, Bailey C, Przewrocka J, Dijkstra KK, Swanton C. COVID-19: the case for health-care worker screening to prevent Hospital transmission. The Lancet 2020; 395: 1418–20. doi: 10.1016/S0140-6736(20)30917-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Treibel TA, Manisty C, Burton M, McKnight Áine, Lambourne J, Augusto JB, et al. COVID-19: PCR screening of asymptomatic health-care workers at London Hospital. The Lancet 2020; 395: 1608–10. doi: 10.1016/S0140-6736(20)31100-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Shields AM, Faustini SE, Perez-Toledo M, Jossi S, Aldera EL, Allen JD, et al. SARS-CoV-2 seroconversion in health care workers. medRxiv 2020;:. 20105197 2020.05.18. [Google Scholar]
- 82. Long QX, Tang XJ, Shi QL, Li Q, Deng HJ, Yuan J, et al. Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nat Med 2020;. [DOI] [PubMed] [Google Scholar]
- 83. US Centres for Medicare and Medicaid. Centers for Medicare & Medicaid Services (CMS) Recommendations Re-opening Facilities to Provide Non-emergent Non-COVID-19 Healthcare: Phase I. CMS; [Available from. cited 03 May 2020. [Google Scholar]
- 84. Royal College of radiologists. COVID-19 interim guidance on restarting elective work. London, UK2020 [02nd Mayl 2020;Available from. [Google Scholar]
- 85. Madhuripan N, Cheung HMC, Alicia Cheong LH, Jawahar A, Willis MH, Larson DB. Variables influencing radiology volume recovery during the next phase of the coronavirus disease 2019 (COVID-19) pandemic. Journal of the American College of Radiology 2020; 17: 855–64. doi: 10.1016/j.jacr.2020.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Vagal A, Mahoney M, Allen B, Kapur S, Udstuen G, Wang L, et al. Rescheduling Nonurgent care in radiology: implementation during the coronavirus disease 2019 (COVID-19) pandemic. Journal of the American College of Radiology 2020; 17: 882–9. doi: 10.1016/j.jacr.2020.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Davenport MS, Bruno MA, Iyer RS, Johnson AM, Herrera R, Nicola GN, et al. ACR Statement on Safe Resumption of Routine Radiology Care During the Coronavirus Disease 2019 (COVID-19) Pandemic. Journal of the American College of Radiology 2020; 17: 839–44. doi: 10.1016/j.jacr.2020.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Society of Radiographers/Royal College of Radiologists Guidance for Imaging and Radiotherapy services during the Covid-19 pandemic: Use of face coverings for patients, clients and carers.. Available from: https://www.sor.org/sites/default/files/document-versions/guidance_for_imaging_and_radiotherapy_services_during_the_covid-19_pandemic-_use_of_face_coverings_for_patients_clients_and_carers.pdf [cited 23 June 2020].
- 89. Georgiades C. Leadership lessons from prior pandemics: turning the coronavirus disease 2019 (COVID-19) pandemic into an opportunity. Journal of the American College of Radiology 2020; 17: 906–8. doi: 10.1016/j.jacr.2020.04.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Cancer Research UK £150 million per year could be cut from cancer research, warns charity. Cancer Research UK. 2020. Available from: https://www.cancerresearchuk.org/about-us/cancer-news/press-release/2020-06-24-ps150-million-per-year-could-be-cut-from-cancer-research-warns-charity [cited 24th June 2020].
- 91. Vagal A, Reeder SB, Sodickson DK, Goh V, Bhujwalla ZM, Krupinski EA. The impact of the COVID-19 pandemic on the radiology research enterprise: radiology scientific expert panel. Radiology 2020;;: 201393 Ahead of Print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Eng J, Bluemke DA. Imaging publications in the COVID-19 pandemic: applying new research results to clinical practice. Radiology 2020; 201724: 201724. doi: 10.1148/radiol.2020201724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Li L, Qin L, Xu Z, Yin Y, Wang X, Kong B, et al. Using artificial intelligence to detect COVID-19 and community-acquired pneumonia based on pulmonary CT: evaluation of the diagnostic accuracy. Radiology 2020; 296: E65–71. doi: 10.1148/radiol.2020200905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Shi F, Wang J, Shi J, Wu Z, Wang Q, Tang Z, et al. Review of artificial intelligence techniques in imaging data acquisition, segmentation and diagnosis for COVID-19. IEEE Rev Biomed Eng 2020;: 1 Ahead of Print. doi: 10.1109/RBME.2020.2987975 [DOI] [PubMed] [Google Scholar]
- 95. Shen C, Yu N, Cai S, Zhou J, Sheng J, Liu K, et al. Quantitative computed tomography analysis for stratifying the severity of coronavirus disease 2019. J Pharm Anal 2020;Ahead of Print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Gozes O, Frid-Adar M, Greenspan H, Browning PD, Zhang H, Ji W, et al. Rapid AI Development Cycle for the Coronavirus (COVID-19) Pandemic: Initial Results for Automated Detection & Patient Monitoring using Deep Learning CT Image Analysis Radiology: Artificial Intelligence. 2020; 05037. Ahead of Print. arXiv. [Google Scholar]
- 97. Fan D, Zhou T, G-P J, Zhou Y, Chen G, Fu H, et al. Inf-Net: automatic COVID-19 lung infection segmentation from CT scans. medXriv 2020;. [DOI] [PubMed] [Google Scholar]
- 98. Cao Y, Xu Z, Feng J, Jin C, Han X, Wu H et al.Longitudinal Assessment of COVID-19 Using a Deep Learning–based Quantitative CT Pipeline: Illustration of Two Cases. Radiology: Cardiothoracic Imaging; 2020. 2(2):e200082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Qi X, Jiang Z, Yu Q, Shao C, Zhang H, Yue H, et al. Machine learning-based CT radiomics model for predicting hospital stay in patients with pneumonia associated with SARS-CoV-2 infection: a multicenter study. medRxiv 2020;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Radiological Society of North America. RSNA international COVID-19 open radiology database (RICORD. RSNA; [Available from. cited 02 May 2020. [Google Scholar]