Abstract
This study explored men's views of workplace-based HIV self-testing and the barriers and facilitators of linkage to posttest services. Six focus group discussions and individual in-depth interviews were held with employers and employees in private security companies in Uganda (N = 70). Using content analysis, five categories emerged. The first category was the mitigation of potential harm, including reduction of stigma and discrimination, and the need for posttest support. The second category was a perceived need for on-site services where the men proposed on-site prevention services and HIV treatment and care. In the third category, which was strengthening linkage mechanisms, participants proposed expanded clinic hours, improved health facility efficiency, and provision of referral documentation. The fourth and fifth categories were organizational support and social support, respectively. There is need for employers and employees to work together for the success of workplace-based HIV initiatives.
Key words: Africa, HIV self-testing, linkage to care, male, qualitative research, workplace HIV testing
In 2018, there were approximately 38 million people living with HIV globally, with an estimated 54% of them in East and Southern Africa (Joint United Nations Programme on HIV/AIDS [UNAIDS], 2019). In Uganda, the national prevalence of HIV among persons ages 15 to 64 years was 6.2%; it was higher in women (7.6%) than in men (4.7%), as was the proportion of viral load suppression 62.9% and 53.6%, respectively (Ugandan Ministry of Health [MoH], 2017). However, in 2018, AIDS-related mortality was higher in men than in women (UNAIDS, 2019). According to the Ugandan Ministry of Health (MoH), there are fewer men than women who have ever taken an HIV test in Uganda (MoH, 2016). Additionally, 79% of adult women living with HIV are on treatment as compared with 63% of men living with HIV (UNAIDS, 2019). As a consequence, men are more likely to start antiretroviral therapy (ART) at later stages of HIV infection and experience higher morbidity and mortality after starting ART (MoH, 2016). This low uptake undermines the success of proven HIV prevention strategies, for instance, the undetectable equals untransmittable (U = U) approach, where individuals who achieve and steadily sustain an undetectable viral load for at least 6 months cannot transmit HIV (Eisinger et al., 2019). A study among male fisher folk in Uganda reported that a diagnosis of HIV and ART initiation improved their attitude toward involvement in HIV care (Sileo et al., 2019). Globally, there is a dire need for innovative approaches to reach men who do not know their HIV status and improve mechanisms for linking them to treatment if living with HIV or prevention services if identified to be uninfected.
HIV self-testing (HIVST) is one strategy for delivering HIV testing services (HTS; Wong et al., 2019). HIVST has led to an increase in utilization of HTS, especially among men, young people, and first-time testers (Hatzold et al., 2019; Makusha et al., 2015; World Health Organization [WHO], 2016), and an increase in the frequency of testing (Katz et al., 2018). HIVST also helps to address some of the barriers cited for the lack of male engagement in HTS. These include the perception that facilities are designated for women only, long travel distances to access services, waiting in line to access testing or treatment, HIV-associated stigma, and lack of time (d’Elbée et al., 2018; Myers et al., 2017; Okoboi et al., 2019; Volk et al., 2016). Some people expressed fear that HIVST leads to an increase in sexual risk behavior; however, there is no evidence that HIVST leads to an increase in sexual risk-taking behaviors (Katz et al., 2018; Ortblad et al., 2019).
HIVST confers several important immediate benefits. For example, individuals with a reactive HIV self-test can benefit from linkage to care and those with nonreactive ones can benefit from being linked to prevention services. In Kenya, 65% of index partners of female sex workers visited a health facility to confirm their results in 3 months after a self-test, whereas 58% sought HIV treatment and care (Thirumurthy et al., 2016). In a study among men who have sex with men in Canada, the participants with reactive self-tests (0.7%) sought linkages the next day and those with nonreactive self-tests received counseling (Pant Pai et al., 2018). Few published studies report findings on linkage to care (Johnson et al., 2017; Pant Pai, et al., 2013b) and even less on linkage to prevention services following HIVST.
Globally, the prevalence of HIV in the workforce is increasing, and the numbers are estimated to reach 29.9 million with associated loss in earnings projected to surpass 7 billion USD annually by 2020 (International Labour Organization [ILO], 2018). Workers in certain industries may face particularly high risk of HIV, especially when they remain away from home and/or partner for long periods. Such industries include the military, mining, construction, security, petroleum/energy, agriculture, fishing, factory production, and long-distance hauling (WHO, 2018). These are industries typically dominated by men (Camlin et al., 2016; WHO, 2018). HIVST may also increase the uptake of testing if offered as part of workplace-based programs (WHO, 2018). “Workplace programmes refer to a range of company-based interventions including the institution of an HIV/AIDS policy, voluntary counselling and testing, and ART provision” (Mahajan et al., 2007, p. S32). The aim of this study was to explore employers' and employees' perspectives of engagement in workplace-based HIVST, and barriers and facilitators to linkage to care or prevention services. The findings from this study were used to inform the implementation of a workplace-based cluster randomized trial on HIVST (ClinicalTrials.gov: NCT04164433).
Methods
Design, Setting, and Eligibility
This exploratory qualitative description study was conducted in June and July 2019, in two districts in the central and western regions of Uganda. The team identified private security companies in the study area, employing more than 500 males, for inclusion in the study. Potential participants included employers, company executives, and employees. The rationale for the inclusion of these groups was to provide a holistic picture of HIVST at the workplace through participant triangulation. If such a service were to be introduced, the management would have to take into consideration the employees' concerns (barriers) while also enhancing the facilitators. In addition, the employees would need to understand why management may not respond positively to some of their requests. We conducted focus group discussions (FGD) with employees and then individual interviews with company employers and executives to get more depth and detail on the topics that appeared in the group discussions. The FGD for employees were possible because the number of men at the same position was large enough within the same company to recruit an adequate sample size. However, the private security company employers and executives were of small number and could not interact in a focus group comprising their business competition; hence, individual interviews for this group were used. Enrollment into the study stopped when saturation and redundancy (no new information) was obtained from the discussions and interviews. All FGD and individual interviews were audio recorded with permission from the participants.
Focus Group Discussions
Recruitment and enrollment
Select members of the study team met with the managing directors of the companies to explain the study and seek permission to meet with the employees. After permission was granted, the employers convened a general employee meeting. The study team met the employees in a group at the company premises and explained the purpose of the study. Eligible and willing employees then selected an appropriate date and time for an interaction. The inclusion criteria were males, ages 18–64 years, who were employed for longer than 3 months at the same company. The participants were purposively selected to ensure participation of employees from different positions, including security guards, field supervisors, and administrators.
Data collection
Focus group discussions were conducted by three research team members (P.A.M. and two research assistants) in a private room at the companies' premises, with one moderating and another taking notes. The moderator (P.A.M.) introduced the study team and explained the aims of the study. The moderator and research team members were consistent across all focus groups. The discussion guide contained open-ended and probe questions to elicit employees' responses in the broad categories: men's perceptions of HIV testing at the workplace, strategies to increase uptake of HIVST services, and linkage to care. Additional sample questions that were asked of the focus groups are presented in Table 1. Each focus group discussion lasted approximately 90 minutes and started with a short teaching on HIVST. For homogeneity, the focus groups were categorized by employee position or job title. This allowed the employees to express themselves more freely when placed in groups with their work peers, without any inhibitions that might arise from a supervisory or administrative presence. Data from the focus group discussion and probes were collected about the men's perceptions and preferences of access to confirmatory testing, ART initiation and prevention services, and what to do after taking an HIV self-test. The focus groups were audiorecorded, and the recordings were transcribed verbatim. No repeat FGD were indicated. Verbatim transcripts were returned to a sample from each focus group for comments, corrections, and confirmation of the narrative. This participant sample was selected by simple random sampling. Two men were randomly selected from each of the six focus groups and given the opportunity to review the transcripts for completeness and accuracy of the transcribed content.
Table 1.
Focus Group Discussion and In-Depth Interview Guide
| Men's perception of HIV testing at the workplace | 1. What current options for HIV testing are you aware of? Briefly discuss the advantages and disadvantages of each option. 2. Why do you think people go for HIV testing? 3. Why do you think some people do not go for HIV testing? (may be answered above) 4. Why do you think your colleagues (security personnel) go/do not go for testing? Different from above? 5. What have you ever heard about HIV self-testing? (Probe and explain) 6. If this method was made available at your workplace, would you be willing to take an HIV self-test? Why or why not? 7. How much would you be willing to pay for this HIV self-test kit? 8. What are some of the strategies that may be used to promote HIV testing at the workplace? |
| Strategies to increase uptake of HIV self-testing services and linkage to care | 1. The results of an HIV self-test need to be confirmed, what are the challenges people might face in getting a confirmatory test at the health facility? 2. What do you propose as a strategy to help people confirm their test if they received a positive result and link to care and services? 3. Where would you go? 4. How else do you propose for people in workplaces to get encouraged to access confirmatory test services? 5. What safety concerns would you have with self-testing at your workplace? 6. What are some of the strategies that may be used to promote linkage to prevention services after a nonreactive self-test? 7. What form of support do you think you would need for access to care or prevention? |
| Additional questions for employers and company executives | 1. Can employees who take the HIV self-test receive paid time off to go and take confirmatory tests, get treatment or prevention services? If so, how would this work? If no, what can the organization do for them? 2. How can scheduling of duties be done to allow employees to go and seek care? 3. How can we introduce HIV initiatives at the workplace? How can we include the family in workplace-based initiatives? |
In-Depth Interviews
Recruitment and enrollment
The research team (P.A.M. and two research assistants) met the key senior personnel composed of employers and company executives. The company executives were purposively selected according to their position or title. The executives were eligible to participate if they held the position of chief executive officer, chief operating officer, chief financial officer, or executive director for at least 2 years. The team explained the purpose of the study and made an appointment for a later date to interview those who were willing to take part.
Data collection
The principal researcher (P.A.M.) conducted the individual in-depth interviews (IDI) using a guide, and each interview lasted about 45 minutes. Sample interview questions are presented in Table 1. The employers and company executives were enrolled and interviewed individually in their private company offices. The company management was asked additional questions about paying time off, scheduling tasks to allow employees time to go and seek care, and the possibility of introducing workplace-based HIV programs.
Ethical Considerations
Ethical approval for the study was obtained from the Makerere University School of Health Sciences Research Ethics Committee (REC- No: 2018-054). Written informed consent was sought from each participant prior to enrollment into the study. No employee responses or information were shared with the employers. Data were collected in English because the employees and employers were comfortable in expressing themselves in that language. Each participant received Uganda shillings 30,000 “equivalent to $7.80 USD” as compensation for their transport and time.
Data Analysis
At the end of each FGD and IDI, the note taker typed up verbatim transcripts of the recordings and field notes. Data from both FGDs and IDIs were analyzed manually using qualitative content analysis guided by the methodology proposed by Elo and Kyngas (2008). This involved three phases of preparation, organizing, and reporting.
During preparation, three research team members (E.N., P.A.M., C.P.O.) immersed themselves in the data to obtain a sense of it. For the organizing phase, the three members (E.N., P.A.M., C.P.O.) independently analyzed and coded the transcribed data. The coders then met together to agree on the individually assigned codes. Any disagreements between the codes were resolved by consensus. The final codes were then grouped into clusters based on the underlying similarities and assigned to subcategories. For the reporting phase, the subcategories were further merged into meaningful categories. Table 2 shows the data coding tree. Following this individual analysis, the data generated from both the management and the employees were analyzed using dyadic analysis for overlaps, contrasts, and complementarities at text, subtext, descriptive, and interpretive levels (Eisikovits & Koren, 2010).
Table 2.
Coding Tree for Strategies to Optimize Linkage to Care and Prevention After Workplace-Based HIV Self-testing
| Category | Subcategory | Codes | No. of Responsesa | |
| Employees | Executives | |||
| Mitigation of potential harm | Systems to prevent potential harm | Counseling for suicide | 17/58 | 11/12 |
| Counseling for depression | ||||
| Prevention of harm | ||||
| Stigma or discrimination reduction | Employers join in the testing | 6/58 | 4/12 | |
| Open a small clinic | ||||
| Stigma for HIV uninfected | ||||
| Post–self-test support | Phone contact counselor | 38/58 | 5/12 | |
| Someone to talk to | ||||
| Posttest number | ||||
| Perceived need for on-site services | Provision of on-site confirmatory testing | Testing at workplace | 40/58 | 0/12 |
| Open a small clinic | ||||
| Provision of worksite treatment and care | Treatment in community | 12/58 | 8/12 | |
| Pick drugs near home | ||||
| Centralized place to pick condoms | ||||
| Strengthening linkage mechanisms | Expanded clinic hours | Health facilities open longer | 6/58 | 0/12 |
| HIV services 24 hours | ||||
| Improved health facility efficiency | Specific health facilities | 39/58 | 5/12 | |
| Facilities prepared | ||||
| Specific counsellor | ||||
| Clinic days for working men | ||||
| Referral and linkage documentation | Referral letter | 43/58 | 8/12 | |
| Official letter to employers | ||||
| Communication to hospital | ||||
| Organizational support | Job security | No one should lose their job | 43/58 | 3/12 |
| No one should be fired, retain job | ||||
| Employer commitment | Permission for treatment | 36/58 | 1/12 | |
| Paid leave for treatment | ||||
| Mandatory HIV testing | ||||
| Company HIV initiatives | ||||
| Need for confidentiality | Protect information | 15/58 | 0/12 | |
| Professionalism in handling information | ||||
| Not spreading information | ||||
| Flexible employee working hours | Flexible schedule hourly wages | 4/58 | 0/12 | |
| Social support | Couple and partner HIVST | Couple testing | 25/58 | 2/12 |
| Testing with partner | ||||
| Accountability | ||||
| Wife reminder for treatment | ||||
| Peer support | Peer health education | 13/58 | 9/12 | |
| Escorts to facility | ||||
| Peer counseling | ||||
| Health education and sensitization | Health talks | 19/58 | 12/12 | |
| Information to stay safe | ||||
| Share new information | ||||
Note. HIVST = HIV self-testing.
Some participants gave multiple responses in one category.
The study was guided by the four trustworthiness criteria to support the quality of the findings (Lincoln & Guba, 1986). To ensure credibility, the study employed a triangulation of methods using both focus groups and interviews to collect data. Furthermore, the research team spent prolonged time at the men's workplaces prior to data collection to gain insight into the study context and build rapport. For dependability, a sample of employers and employees checked the resulting categories after data analysis to validate the groupings and descriptors identified. They also reviewed the recommendations of the study to confirm that they were supported by the data. To facilitate transferability, the study employed purposive sampling. Additionally, this article provides a detailed description of the methods for researchers to use in conducting future studies on workplace-based HIVST. Confirmability was established by documenting field notes and the researchers' personal reflections in relation to the study. All participant excerpts were deidentified.
Results
Participant Characteristics
Fifty-eight employees participated in six focus groups, and 12 employers and company executives were interviewed. The ages of the participants for the FGD ranged from 18 to 45 years, whereas the participants in the IDI were ages 46–64 years. Of the 38 (54%) employers and employees who had ever tested for HIV, 14 (37%) were tested at an antenatal clinic during a partner's pregnancy. (A summary of participant characteristics can be found in Table 3.)
Table 3.
Demographics of Study Participants
| Participant Characteristics (N = 70) | Frequency (n) | Percentage (%) |
| Age range, years | ||
| 18–25 | 12 | 17.1 |
| 26–35 | 27 | 38.6 |
| 36–45 | 19 | 27.1 |
| 46–64 | 12 | 17.1 |
| Relationship status | ||
| Long-term relationship | 34 | 48.6 |
| Unmarried | 29 | 41.4 |
| Divorced/separated | 7 | 10.0 |
| HIV status (self-reported) | ||
| Known | 38 | 54.3 |
| Unknown | 32 | 45.6 |
| Employment position/Job title | ||
| Security guards | 40 | 57.1 |
| Field supervisors | 10 | 14.3 |
| Administrators | 8 | 11.4 |
| Company executives | 12 | 17.1 |
| Place of HIV test (n = 38) | ||
| Antenatal clinic | 14 | 36.8 |
| Health facility | 7 | 18.4 |
| Community HIV testing event | 11 | 28.9 |
| Voluntary male medical circumcision clinic | 6 | 15.8 |
Strategies to Optimize Linkage to HIV Care or Prevention Following Workplace-Based HIVST
The main strategies to optimize linkage to prevention, care, or treatment are presented under five categories” (a) mitigation of potential harm, (b) perceived need for worksite services, (c) strengthening linkage mechanisms, (d) organizational support, and (e) social support. Participant quotations are presented to illustrate the categories. Figure 1 shows a graphical representation of the categories and subcategories.
Figure 1.
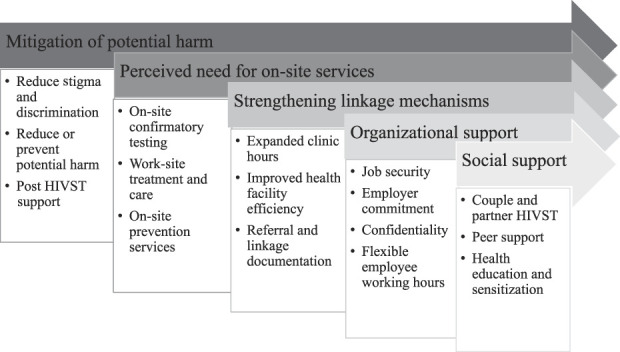
Categories for strategies to optimize linkage to prevention, care, and treatment.
Mitigation of Potential Harm
Post–self-test support
Both groups raised concerns about the lack of face-to-face posttest interaction. They verbalized willingness to link to care if they had someone to talk to or if there were some form of follow-up.
If there is a way we can contact someone after the test, I think it will be very good and will encourage me to take the next steps when I know that I am not alone. (FGD 6 with field officers)
They proposed that detailed information should be provided as part of the pretest interaction. This information might include the health facilities where they can go for confirmatory testing and phone numbers to call in case of any questions or for corroboration of their results.
I feel that after this test, leaves you so alone since you do it at home when there is no counsellor and you may not want to share your worries with your partner at that moment. Is it possible to provide a number for a counsellor? Someone who will not tell other people because I can assure you, receiving this information before the test is one thing but remembering what to do when you are alone and you have your results is another thing. (IDI with company executive)
Reduce/prevent potential harm
A few employees raised concerns about the potential for harm including potential for committing suicide, partner violence, and/or reduced productivity at work following a reactive self-test. They felt that if the worksite was prepared for this, it would help them cope and seek further services.
Some people here have a very bad temper and you can't tell what they can do after finding out their results. When they are making such programs at work, they should plan for such occurrences. For example, by doing more teaching after people take the test and counsel them that it is ok and also help them to know what to do next, teach them about taking drugs and how they help. (FGD 1 with employees)
Stigma or discrimination reduction
Both the employers and employees were willing to link to HIV care in the absence of stigma or discrimination. The employees proposed a small clinic at the workplace that offers several other health services to reduce the stigma and make it easy for them to access HIV treatment or prevention interventions.
In fact, since we are many here, why can't they open a small clinic that caters for our families and us? It does not have to provide all the services, but if people go there for measles, syphilis, pressure [hypertension], when I go for HIV services no one will know what I am getting. (FGD 1 with employees)
The employees also suggested that the company's top management officials should use the same services for acceptability.
The employers should also use these same services so it doesn't look like it is only employees who are sick. There is too much stigma and fear here. (FGD 1 with employees)
The issue of discrimination and stigma was also expressed by some of the company executives as a potential barrier to both testing and linkage to services.
… fellow staff will still discriminate against them and make them uncomfortable because they will just assume that one is HIV positive. There should be a way in which one can comfortably go for treatment or pick condoms without any negative consequences from colleagues. (IDI with company executive)
Perceived Need for On-Site Services
Provision of on-site confirmatory testing
The research team informed all the study participants that people who receive reactive self-tests need to go to a facility for further confirmatory testing. The employees had reservations about having to seek confirmatory testing at the health facility but expressed willingness to take it at their worksite.
I understand that if the kit [HIV self-testing kit] shows that I am negative, I can go to the health facility for testing again but I don't have to do it immediately, while if the kit shows HIV positive, I need to go to a health facility to confirm and possibly start on treatment. My problem is that I still do not have time to go and line up at the hospital given my work schedule. Is it possible for us to receive the kit then go home and do the test then we come back and see the counselor in case we are sick [reactive self-test] and get the test done from here and treatment? This is what they usually do when they come to test us in the community. (FGD 6 with field officers)
Some employers proposed a model of testing to offer each person several testing options at the workplace.
I propose that you give us information about the self-test and the regular test and then offer all testing options so that one can choose the one with which they feel comfortable. That way, no one will say they were forced and if they must get a confirmatory test, they will have chosen that option for themselves. (IDI with company owner)
Provision of on-site prevention services
Several employees were particularly interested in the provision of prevention services such as condoms distributed at the workplace.
For those who are negative, we can access some methods at the workplace. For example, if we give condoms to a responsible officer, people can go and pick from there. (FGD3 with supervisors)
Others proposed conducting mobile voluntary male medical circumcision (VMMC) a few times a year at the workplace.
Personally, I am interested in circumcision, can they get a day and we organize ourselves either to come to the health facility or for them to come and set up and we access the services from here? I have seen people doing that operation outside hospitals [mobile VMMC]. (FGD 1 with employees)
A participant mentioned the provision of pre-exposure prophylaxis (PrEP) at worksites as a method of prevention.
I recently heard of some medicines that you take to prevent getting HIV [PrEP], maybe they can bring those ones here to the clinic and workers can go and pick them from there, sometimes you feel condoms may not be enough. (FGD 1 with employees)
The employees also proposed regular education on the different HIV prevention methods available. They proposed provision of simple material they could take home with them or regularly organized talks at their workplace.
With my busy schedule, I only hear about these things when my wife goes to the antenatal clinic or from TV. They should provide some information at the workplace about HIV prevention. This can be in form of small materials we can take and read from home. Alternatively, they can call people here regularly to teach us. It is very important. (FGD 6 with field officers)
Provision of worksite treatment and care
Both groups of participants reported that the best way to get people to access HIV care was to bring the services to their worksites or a centralized location in the community.
Is it possible for us to receive the kit then go home and do the test then we come back and see the counsellor in case we are sick [diagnosed HIV positive] and get the test done from here and treatment? Or even if they can find one place near where we stay so we can pick the drugs and condoms …. (FGD 6 with field officers)
Some executives strongly supported the provision HIV services at the company premises and expressed their willingness to invest in such initiatives only if the employees were willing to use them.
I think it would be good to have HIV prevention, testing and treatment education at the workplace if the employees make use of them. Sometimes you spend money to design initiatives for the team and they do not utilize them. (IDI with company executive)
Some of the employees proposed the inclusion of HIV testing in the policy to make it mandatory. They suggested that this should happen during recruitment and that new employees could not start working until they showed evidence of linking to care and treatment. The team provided information that although this was a good idea, it goes against some of the five guiding principles of HIV testing: consent, confidentiality, counseling, correct test results and connections to care, and treatment and prevention services (WHO, 2015).
Make HIV testing compulsory for example when new recruits report to work, they should present evidence of having done an HIV test for the records. If they have not done the test, they can immediately receive counselling and test kits, they will only be allowed to start working if they access either prevention or treatment. That way, people will take a test and access treatment. (FGD 5 with field supervisors)
Strengthening Linkage Mechanisms
Expanded clinic hours
Some employees proposed that the employers and policy makers should make an overarching regulation that either reduces the number of hours worked by private security officers or increases the working hours for health facilities. It should be noted that the policies on time off varied between the companies. Therefore, although some employees were entitled to paid time off, others who received hourly pay did not have a similar entitlement. The quote below illustrates this:
The government should help and regulate the private security companies to allow some paid time off since payment is per hour or per day; one is reluctant to even spend any time away from the job. This will mean challenges with consistent use of HIV treatment. Therefore, if health centers could be open a little longer or have HIV testing and treatment facilities available 24 hours a day, which would be much better. (FGD 1 with employees)
Improvement of health facility efficiency
The men expressed frustration with the long lines at the health facility and the discomfort they experienced when they used these facilities. They proposed the creation of customized services for men, including a dedicated counselor at the facility, or “men's day.”
The counsellors can identify some facilities and then receive us or take us there so that it is easier to get into the system. We usually go and look lost at the health center but if we know exactly where we are going and what time, it will make it so much easier to plan and go there. (FGD 5 with supervisors)
The employers recommended that the employees get an organized schedule of clinic visits for proper planning. This is emphasized in the quote below:
Employees should work with the health facility to place their clinic days on a specific day for example the first Friday of the month, this helps the employer plan and allow an employee time off. There should also be a way to follow up and make sure that people are taking their medication and going to the clinic when they say that they are. (IDI with company owner)
Referral and linkage documentation
Many employees expressed the need for some official documentation to give them priority at the health facility.
… provide something in the kit which will reduce the time spent at the health facility, I should just go straight for the confirmatory test and if positive I just receive my results and get connected for treatment. (FGD 4 with managers)
The employees also proposed the documentation to make it easy to get permission from work to access further linkage options.
The health workers should give us something written, which one can use at the workplace to get permission to go and pick medication. (FGD 5 with field supervisors)
Organizational Support
Job security
The employees were willing to access posttest services if they received an assurance of keeping their job without termination.
Management should state it clearly that in case one is found to be positive for any of the tests carried out, no one will lose their job and they will receive support to get treatment, e.g., Sexually transmitted infections and Hepatitis. (FGD 2 with employees)
Employer commitment
The men expressed a need for confirmation from their employers for paid time off to go for confirmatory testing and treatment.
The other time my daughter had malaria and I really struggled to get a off day to go and take care of her. Now, if I must go and get medication and further testing maybe every month, how will that work? If they say they have brought HIV testing here, then they should give us permission to go and access everything that follows a positive test. (FGD 1 with employees)
On the other hand, the company management felt that it was the employee's duty to organize their treatment schedule and request for time off in advance as part of their paid leave allowance. They suggested that the employees needed to find a way to get an organized schedule at the clinic for proper planning of their duties at the workplace.
It is very complicated to start planning for each employee to go for treatment, besides which you have told me that you will not give us their HIV results and we do not want to ask them to give us their results, it is not a requirement for the job. What they can do, is make sure they get a clear schedule from the clinic on when they will need to pick their medicine or get whatever treatment they need, and then they come and apply for sick-leave days. (IDI with company executive)
If our employers allow us to help the officers who need to go to the hospital, we advise them to go for the confirmatory testing as they are leaving the shift and also maybe to seek treatment over the weekend from places that open on their days off. It is hard to give someone a whole shift off in a private company but it will depend on the owners of the company. (FGD 3 with field supervisors)
Flexible employee working hours
The men expressed concern about their work schedules and proposed longer opening hours at health facilities for access of HIV services.
To be honest the working hours here are really hectic. Even when we take a test from the workplace, it is good because we shall know our status. But it might be sometime before one gets time to access other services and treatment. Imagine you test positive and you cannot get time to go to the clinic for 3 more months. That is torture. It would be good if the company can make our hours flexible so we can get a chance to go to the hospital. (FGD 6 with field officers)
Confidentiality
The employees were willing to link to care or prevention if they had an assurance that the employers or health workers would not divulge any information.
Sometimes a member of staff goes to explain their issue to one of the managers and before you know it, information has spread among the other operatives. This information about HIV is very sensitive. What if I go to ask for permission to go for treatment and my colleagues find out? I think the company should first promise that this information will remain confidential. (FGD 2 with employees)
Social Support
Couple and partner HIV self-testing
Men in long-term marital relationships reported that they would more likely seek posttest services if tested with their partner.
If I test with my wife, we can console each other and decide together how we shall move forward. I know my wife, in case we are both positive, she will keep pushing me to make sure I get treatment and take it. (FGD 2 with employees)
Other participants requested each partner to receive their kits and test separately; however, they preferred to receive the pretest information as a couple.
If they give me two kits [HIV self-testing kits], I can use one and give my wife one. Although, I think it would be better for us to receive the counselling and the kits together. I get very forgetful but at least if both of us get the information, then she can remind me when we are taking the test. (FGD 3 with field supervisors)
Peer support
Both groups of participants reported that it would be beneficial if their work colleagues living with HIV volunteered to provide peer support to fellow staff. The support could be in the form of peer counseling or to escort peers to the health facility. Alternatively, they could talk to colleagues who self-test or help them navigate any challenges at the workplace.
If our workmates who are already getting treatment do not mind, they can give us some health education talks even before we take the test. After receiving our results, they can go with us to the health facility and allow us to talk to them when we feel overwhelmed especially with this hectic job. Sometimes knowing that you are not alone is very helpful. (FGD 2 with employees)
Some members of the top management team supported this:
If some of the employees are comfortable and open, they would be very helpful in supporting their other colleagues who test positive and this will reduce stigma. Of course, you need to find someone you trust. (IDI with company executive)
Health education and sensitization
Both management and employees observed that provision of consistent education and information would reinforce the information they received during the pretest counseling. They felt that this would further encourage them to seek care or prevention services.
One thing I have observed with all these health programs is that if you provide regular information, eventually people will remember and act on this information when they must make a choice. I propose that we have regular health talks at the workplace, and information regarding where to go for services placed all over like at the canteen or in the restrooms. (FGD 4 with managers)
We usually organize monthly talks for our staff, but they are mainly about work-related issues. I think if health workers came on some of those days and gave us information on how we should proceed after an HIV test, it would also help. During those same meetings, they can come with things like condoms and distribute to the staff who need them. Sometimes education can save one's life. (IDI with company executive)
Discussion
This study explored male employers' and male employees' views regarding engagement in workplace-based HIVST and linkage to posttest services. The main finding is that there is a perceived need for on-site services to improve access to post-HIVST services. Employees expressed their willingness to link to services if these were brought closer to them at the workplace. This could reduce the proportion of people who take an HIV self-test but do not go to a health facility for confirmatory testing and may also increase the proportion who are initiated on ART. A literature review focusing on the experiences of using and organizing HIVST reported that HIVST supplemented existing resources in the community and clinic to improve HIV care, including confirmatory testing and retesting, mental health counseling, and starting or re-entering ART (Qin et al., 2018). Regarding prevention at the work site, both groups in this study proposed specific health promotion days where mobile voluntary male medical circumcision (VMMC), health education, PrEP, and other prevention services would be offered at worksites. However, programs and workplaces that implement such initiatives should be cautious about unintended disclosure of employees' HIV status.
The employees expressed fear that they may attempt personal harm or hurt others following a reactive HIVST. They expressed this as a potential barrier to seeking services following HIVST at the worksite. However, it should also be noted that there is little, if any, evidence from the literature of the three types of harm (psychological, medical, or social) following HIVST (Brown et al., 2014). In this study, both the employers and employees proposed face-to-face posttest counseling, which could serve to mitigate the potential of harm and provide further information that may improve linkage to services. This is supported by findings where the participants reported the need to have someone to talk to following HIVST to counter their concern of potential for harm if they received the results by themselves (Makusha et al., 2015). This strategy has also shown success in increasing linkage to posttest services after an HIV test (d’Elbée et al., 2018), although sometimes when participants with reactive self-tests were called following referral, the calls went direct to voicemail or went unanswered (Deville & Tempelman, 2019). The findings suggest that any program on workplace-based HIVST should put in place measures to prevent any harm resulting from a reactive HIVST. This may include the presence of an on-site counselor, education, availability of a toll-free telephone line, and the assurance from the employers that employees' jobs will not be affected and that they will be supported to access further services.
Both the employers and employees felt that the linkage to posttest services may be improved by strengthening the existing linkage systems between the point of testing and the health facility. One of the suggestions included customizing the services for the employees. This agrees with findings that people who receive reactive self-test results will more likely seek to access a health facility if the process is stress free and services are offered in a customized manner (Pant Pai et al., 2013a). The Ugandan Ministry of Health (MoH) introduced several strategies over time to improve men's access to HIV services, including expanded clinic hours and special clinics for most-at-risk populations. Additionally, there are referral forms, which should help the men access HIV services faster following nonfacility HIV testing (MoH, 2016). There is need to sensitize the employees and employers about the different options available to address their beliefs about difficulties in accessing care at health facilities. Participants in this study expressed the need for official documentation to ease linkage to care. A study where a “self-referral card” allowed participants to access two health facilities estimated that 56% of people with reactive self-tests were linked to care (Choko et al., 2015). A study in Tanzania reported that most people linked to care with a referral letter, although these forms lacked the requisite information to make it easy for clients to transition into care at the health facilities (Kayabu et al., 2018). Although participants reported concerns with the health facility linkage systems, the challenges with linkage could also arise from procedural errors by the user. Some of the common procedural errors reported with HIVST included users' inability to understand and follow the instructions for use (Simwinga et al., 2019) and errors in specimen collection, and inaccurate reading time (Peck et al., 2014). Errors also frequently arose from removing the kit from the buffer too early, drinking or spilling the buffer fluid, and placing the swab in the buffer before swab collection (Choko et al., 2011; Tun et al., 2018). For example, if participants made an error and read the self-test result as nonreactive instead of reactive, they may not go to the hospital for confirmatory testing and further linkage to care (Choko et al., 2011). This suggests that to strengthen linkage to care or prevention services, health workers could provide detailed information during the pretest counseling sessions.
Organizational support emerged as a key strategy to encouraging linkage to posttest services following workplace-based HIVST. The employees specifically requested some form of commitment from their employers to allow them access to services following HIVST without any repercussions. To them, this meant permission to go for confirmatory testing and to access treatment and any other HIV-related services. Employer commitment is one of the keys to the success of any workplace-based HIV initiative, and the participation by people at all levels in the organization is important for successful implementation of initiatives (Chatora et al., 2018). For instance, in one successful workplace-based HIV initiative, the organization arranged for regional coordinators to accompany employees for treatment (Du Mortier et al., 2016). Trust was also identified as a concern; both that the on-site health providers might share information with management and that management might then retaliate against those with reactive self-tests. They feared that the retaliation might take the form of discrimination, denying time off work to seek posttest services, or allocating fewer work assignments, leading to a reduction in their wages. Participants in a multicounty study consistently identified having an ongoing and trusting patient–provider relationship as one of the most important contributors to the health of people living with HIV. This relationship was essential, right from the initial diagnosis, to linkage and remaining in care (Dawson-Rose et al., 2016). Another way the organizations might support employees is by being cognizant of employees' health status while assigning work tasks to allow them to access care and treatment or preventive services like VMMC or PrEP. This only applies to employees who have willingly disclosed their status to their employers. The employees will more likely disclose their status if they receive an assurance that they will not be penalized for their HIV diagnosis. Workers' HIV test results must be kept confidential and it is an employee's right not to disclose whether they used the self-test kit that they received (WHO, 2018).
The final proposed strategy to improving linkage to services after testing at work sites is social support. The men in long-term relationships expressed that they were more likely to link to posttest services if they received a test kit both for themselves and their partner. The men hoped that this would hold them accountable to consistent condom use or in adherence to treatment and additionally offer the much-needed posttest support. However, a study in Kenya found that although sexually transmitted infection consultations increased among men who tested for HIV with their partners, the intervention was not sufficient to overcome the barriers involved in linkage to HIV care and VMMC (Mark et al., 2019).
Strengths and Limitations
The strength of this study lies in directly engaging both employers and employees to identify their preferences prior to the implementation of programs meant to improve their involvement in workplace-based HIV services. Additionally, we focus on the linkage to both care and prevention services following HIVST. One limitation of this study may have arisen because one group participated only in the FGD and not in the individual IDI and vice versa. There is a possibility that the participants may have expressed socially acceptable views since the study was conducted at their work premises. To minimize this possible effect, the study team categorized the groups according to employee position or job title. Furthermore, the participants were assured that while the general findings would be shared with the employers and company executives, all employees' information would be deidentified.
Conclusions
This study presents potential strategies to optimize linkage to services following workplace-based HIVST. Organizations that seek to conduct workplace-based HIV testing initiatives should assure job security and paid time off to access care at the health facilities. From a research perspective, our findings suggest a need for more extensive implementation research to test the proposed strategies and assess whether they increase linkage to posttest services after workplace-based HIVST. From a policy perspective, the findings from this study may inform the development or review of workplace HIV policies for large male-dominated companies. Participants strongly supported the use of referral letters; however, we recommend that the letters provide the information like that collected during HIV testing at a health facility for seamless transition of care. This may include information regarding whether counseling was done; the type of counseling (individual, couple, or group); and the point of entry for HIV counseling and testing. Additionally, information regarding whether this was provider or client initiated is important, as is clients' demographic information.
Disclosures
The authors report no real or perceived vested interests related to this article that could be construed as a conflict of interest.
Key Considerations
HIV testing remains low among people at risk. HIV self-testing via workplace distribution is a novel approach to increase availability and access to testing among men. However, both access and linkage to posttest services remains a challenge.
It is important to identify and mitigate the numerous barriers to men's engagement in HIV testing services to enhance access and linkage to treatment or preventive services.
Employers and employees need to work together to find solutions to certain issues that may prevent access to testing and linkage to services after HIV self-testing at work sites.
Acknowledgments
This project was made possible by a NURTURE fellowship award funded under Grant Number D43TW010132 (PI: Nelson Sewankambo) from the National Institutes of Health. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the supporting institutions. The authors acknowledge Dorothy Muitta Luwaga and Racheal Nabunya for their assistance in data collection. The authors are grateful to the study participants and to the private security companies for their involvement in this study.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
References
- Brown A. N. Djimeu E. W., & Cameron D. B. (2014). A review of the evidence of harm from self-tests. AIDS and Behaviour, 18(Suppl. 4), S445–S449. 10.1007/s10461-014-0831-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camlin C. S. Ssemmondo E. Chamie G. El Ayadi A. M. Kwarisiima D. Sang N. Kabami J. Charlebois E. Petersen M., & Clark T. D. (2016). Men “missing” from population-based HIV testing: insights from qualitative research. AIDS Care, 28(Suppl. 3), 67–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatora B. Chibanda H. Kampata L., & Wilbroad M. (2018). HIV/AIDS workplace policy addressing epidemic drivers through workplace programs. BMC Public Health, 18, 180. 10.1186/s12889-018-5072-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choko A. T. Desmond N. Webb E. L. Chavula K. Napierala-Mavedzenge S. Gaydos C. A. Makombe S. D. Chunda T. Squire S. B. French N. Mwapasa V., & Corbett E. L. (2011). The uptake and accuracy of oral kits for HIV self-testing in high HIV prevalence setting: A cross-sectional feasibility study in Blantyre, Malawi. PLoS Medicine, 8(10), e1001102. 10.1371/journal.pmed.1001102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choko A. T. MacPherson P. Webb E. L. Willey B. A. Feasy H. Sambakunsi R. Mdolo A. Makombe S. D. Desmond N. Hayes R. Maheswaran H., & Corbett E. L. (2015). Uptake, accuracy, safety, and linkage into care over two years of promoting annual self-testing for HIV in Blantyre, Malawi: A community-based prospective study. PLoS Medicine, 12(9), e1001873. 10.1371/journal.pmed.1001873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson-Rose C. Cuca Y. P. Webel A. R. Solis Baez S. S. Holzemer W. L. Rivero-Mendez M. Sanzero Eller L. Reid P. Johnson M. O. Kemppainen J. Reyes D. Nokes K. Nicholas P. K. Matshediso E. Mogobe K. D. Sabone M. B. Ntsayagae E. I. Shaibu S. Corless I. B. Wantland D., & Lindgren T. (2016). Building trust and relationships between patients and providers: An essential complement to health literacy in HIV care. The Journal of the Association of Nurses in AIDS Care, 27(5), 574–584. 10.1016/j.jana.2016.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deville W., & Tempelman H. (2019). Feasibility and robustness of an oral HIV self-test in a rural community in South-Africa: An observational diagnostic study. PLoS One, 14(4), e0215353. 10.1371/journal.pone.0215353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du Mortier S. Mukangu S. Sagna C. Nyffenegger L., & Aebischer Perone S. (2016). A decade of an HIV workplace programme in armed conflict zones: A social responsibility response of the International Committee of the Red Cross. Journal of Occupational Medicine and Toxicology, 11, 28. 10.1186/s12995-016-0119-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- d'Elbée M. Indravudh P. P. Mwenge L. Kumwenda M. M. Simwinga M. Choko A. T. Hensen B. Neuman M. Ong J. J. Sibanda E. L. Johnson C. C. Hatzold K. Cowan F. M. Ayles H. Corbett E. L., & Terris-Prestholt F. (2018). Preferences for linkage to HIV care services following a reactive self-test: Discrete choice experiments in Malawi and Zambia. AIDS, 32(14), 2043–2049. 10.1097/qad.0000000000001918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisikovits Z., & Koren C. (2010). Approaches to and outcomes of dyadic interview analysis. Qualitative Health Research, 20(12), 1642–1655. [DOI] [PubMed] [Google Scholar]
- Eisinger R. W. Dieffenbach C. W., & Fauci A. S. (2019). HIV viral load and transmissibility of HIV infection: Undetectable equals untransmittable. Journal of the American Medical Association, 321(5), 451–452. 10.1001/jama.2018.21167 [DOI] [PubMed] [Google Scholar]
- Elo S., & Kyngas H. (2008). The qualitative content analysis process. Journal of Advanced Nursing, 62(1), 107–115. 10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- Hatzold K. Gudukeya S. Mutseta M. N. Chilongosi R. Nalubamba M. Nkhoma C. Munkombwe H. Munjoma M. Mkandawire P. Mabhunu V. Smith G. Madidi N. Ahmed H. Kambeu T. Stankard P. Johnson C. C., & Corbett E. L. (2019). HIV self-testing: breaking the barriers to uptake of testing among men and adolescents in sub-Saharan Africa, experiences from STAR demonstration projects in Malawi, Zambia and Zimbabwe. Journal of the International AIDS Society, 22(Suppl. 1), e25244. 10.1002/jia2.25244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Interantional Labour Organization. (2018). The impact of HIV and AIDS on the world of work: Global estimates. https://www.ilo.org/wcmsp5/groups/public/---dgreports/---dcomm/---publ/documents/publication/wcms_630166.pdf [Google Scholar]
- Johnson C. C. Kennedy C. Fonner V. Siegfried N. Figueroa C. Dalal S. Sands A., & Baggaley R. (2017). Examining the effects of HIV self-testing compared to standard HIV testing services: A systematic review and meta-analysis. Journal of the International AIDS Society, 20(1), 21594. 10.7448/ias.20.1.21594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV/AIDS. (2019). AIDSinfo. http://aidsinfo.unaids.org/ [PubMed] [Google Scholar]
- Katz D. A. Golden M. R. Hughes J. P. Farquhar C., & Stekler J. D. (2018). HIV self-testing increases HIV testing frequency in high-risk men who have sex with men: A randomized controlled trial. Journal of Acquired Immune Deficiency Syndrommes, 78(5), 505–512. 10.1097/qai.0000000000001709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kayabu D. E. Ngocho J. S., & Mmbaga B. T. (2018). Effective linkage from point of HIV testing to care and treatment in Tanga region, Tanzania. PLoS One, 13(8), e0201644. 10.1371/journal.pone.0201644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lincoln Y. S., & Guba E. G. (1986). But is it rigorous? Trustworthiness and authenticity in naturalistic evaluation. New Directions for Program Evaluation, 1986(30), 73–84. 10.1002/ev.1427 [DOI] [Google Scholar]
- Mahajan A. P. Colvin M. Rudatsikira J. B., & Ettl D. (2007). An overview of HIV/AIDS workplace policies and programmes in southern Africa. AIDS, 21(Suppl. 3), S31–S39. 10.1097/01.aids.0000279692.54029.a1 [DOI] [PubMed] [Google Scholar]
- Makusha T. Knight L. Taegtmeyer M. Tulloch O. Davids A. Lim J. Peck R., & van Rooyen H. (2015). HIV self-testing could “revolutionize testing in South Africa, but it has got to be done properly”: perceptions of key stakeholders. PLoS One, 10(3), e0122783. 10.1371/journal.pone.0122783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mark J. Kinuthia J. Osoti A. O. Gone M. A. Asila V. Krakowiak D. Sharma M. Parikh S. Ton Q. T. Richardson B. A. Farquhar C., & Roxby A. C. (2019). Male partner linkage to clinic-based services for sexually transmitted infections and human immunodeficiency virus services following couple home-based education and testing. Sexually Transmitted Diseases, 46(11), 716–721. 10.1097/olq.0000000000001057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers J. El-Sadr Davis O. Weinstein E. Remch M. Edelstein A. Khawja A., & Schillinger J. (2017). Availability, accessibility, and price of rapid HIV self-tests, New York City pharmacies, Summer 2013. AIDS and Behaviour, 21(2), 515–524. 10.1007/s10461-016-1594-4 [DOI] [PubMed] [Google Scholar]
- Okoboi S. Twimukye A. Lazarus O. Castelnuovo B. Agaba C. Immaculate M. Nanfuka M. Kambugu A., & King R. (2019). Acceptability, perceived reliability and challenges associated with distributing HIV self-test kits to young MSM in Uganda: A qualitative study. Journal of the International AIDS Society Electronic Resource, 22(3), e25269. 10.1002/jia2.25269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortblad K. F. Kibuuka Musoke D. Ngabirano T. Nakitende A. Harling G. Haberer J. E. McConnell M. Salomon J. A. Oldenburg C. E., & Barnighausen T. (2019). The effect of HIV self-testing delivery models on female sex workers' sexual behaviors: A randomized controlled trial in Urban Uganda. AIDS and Behaviour, 23(5), 1225–1239. 10.1007/s10461-019-02393-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pant Pai N. Behlim T. Abrahams L. Vadnais C. Shivkumar S. Pillay S. Binder A. Deli-Houssein R. Engel N. Joseph L., & Dheda K. (2013a). Will an unsupervised self-testing strategy for HIV work in health care workers of South Africa? A cross sectional pilot feasibility study. PLoS One, 8(11), e79772. 10.1371/journal.pone.0079772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pant Pai N. Sharma J. Shivkumar S. Pillay S. Vadnais C. Joseph L. Dheda K., & Peeling R. W. (2013b). Supervised and unsupervised self-testing for HIV in high- and low-risk populations: A systematic review. PLoS Medicine, 10(4), e1001414. 10.1371/journal.pmed.1001414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pant Pai N. Smallwood M. Desjardins L. Goyette A. Birkas K. G. Vassal A. F. Joseph L., & Thomas R. (2018). An unsupervised smart app-optimized HIV self-testing program in Montreal, Canada: Cross-sectional study. Journal of Medical Internet Research, 20(11), e10258. 10.2196/10258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peck R. B. Lim J. M. van Rooyen H. Mukoma W. Chepuka L. Bansil P. Knight L. C. Muturi N. Chirwa E., & Lee A. M. (2014). What should the ideal HIV self-test look like? A usability study of test prototypes in unsupervised HIV self-testing in Kenya, Malawi, and South Africa. AIDS and Behaviour, 18(4), 422–432. [DOI] [PubMed] [Google Scholar]
- Qin Y. Han L. Babbitt A. Walker J. S. Liu F. Thirumurthy H. Tang W., & Tucker J. D. (2018). Experiences using and organizing HIV self-testing. AIDS, 32(3), 371–381. 10.1097/qad.0000000000001705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sileo K. M. Reed E. Kizito W. Wagman J. A. Stockman J. K. Wanyenze R. K. Chemusto H. Musoke W. Mukasa B., & Kiene S. M. (2019). Masculinity and engagement in HIV care among male fisherfolk on HIV treatment in Uganda. Culture, Health and Sexuality, 21(7), 774–788. 10.1080/13691058.2018.1516299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simwinga M. Kumwenda M. K. Dacombe R. J. Kayira L. Muzumara A. Johnson C. C. Indravudh P. Sibanda E. L. Nyirenda L., & Hatzold K. (2019). Ability to understand and correctly follow HIV self-test kit instructions for use: applying the cognitive interview technique in Malawi and Zambia. Journal of the International AIDS Society, 22, e25253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thirumurthy H. Masters S. H. Mavedzenge S. N. Maman S. Omanga E., & Agot K. (2016). Promoting male partner HIV testing and safer sexual decision making through secondary distribution of self-tests by HIV-negative female sex workers and women receiving antenatal and post-partum care in Kenya: a cohort study. Lancet HIV, 3(6), e266–e274. 10.1016/s2352-3018(16)00041-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tun W. Vu L. Dirisu O. Sekoni A. Shoyemi E. Njab J. Ogunsola S., & Adebajo S. (2018). Uptake of HIV self-testing and linkage to treatment among men who have sex with men (MSM) in Nigeria: A pilot programme using key opinion leaders to reach MSM. Journal of the International AIDS Society, 21(Suppl. 5), e25124. 10.1002/jia2.25124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ugandan Ministry of Health. (2016). National HIV Testing Services Policy and Implementation Guidelines. Ministry of Health. http://154.72.196.19/publications/hivaids/national-hiv-testing-services-policy-and-implementation-guidelines-uganda [Google Scholar]
- Ugandan Ministry of Health. (2017). Uganda population-based HIV impact assessment (UPHIA) 2016-2017. Government of Uganda. http://uac.go.ug/content/uganda-population-based-hiv-impact-assessment-uphia-2016-2017-0 [Google Scholar]
- Volk J. E. Lippman S. A. Grinsztejn B. Lama J. R. Fernandes N. M. Gonzales P. Hessol N. A., & Buchbinder S. (2016). Acceptability and feasibility of HIV self-testing among men who have sex with men in Peru and Brazil. International Journal of STD and AIDS, 27(7), 531–536. 10.1177/0956462415586676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong V. Jenkins E. Ford N., & Ingold H. (2019). To thine own test be true: HIV self-testing and the global reach for the undiagnosed. Journal of the International AIDS Society, 22(Suppl. 1), e25256. 10.1002/jia2.25256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2015). Consolidated guidelines on HIV testing services. https://www.who.int/hiv/pub/guidelines/hiv-testing-services/en/ [Google Scholar]
- World Health Organization. (2016). Guidelines on HIV self-testing and partner notification: supplement to consolidated guidelines on HIV testing services (9789241549868 9241549866). https://apps.who.int/iris/bitstream/handle/10665/251655/9789241549868-eng.pdf [PubMed] [Google Scholar]
- World Health Organization. (2018). HIV Selt-testing at the workplace. https://apps.who.int/iris/bitstream/handle/10665/276170/WHO-CDS-HIV-18.48-eng.pdf [Google Scholar]


