Abstract
Background
High-quality cardiopulmonary resuscitation (HQ-CPR) focuses on improving heart and brain blood perfusion. The evaluation of HQ-CPR included depth, frequency, rate of chest compressions, and the occurrence of chest recoil between two chest compressions. Staff performing CPR may not be performing HQ-CPR since it is influenced by individual stamina, physical strength, and lack of target marker. We aimed to study the impact of 100 times per minute rate vs. 120 times per minute CPR rate on the depth and percentage of depth-on-target done by trained staff on a manikin.
Methods
This was a cross-over randomized control study. The subjects were anesthesiology and intensive care residents in a tertiary teaching hospital in Indonesia, all certified to perform advanced life support. The subject was asked to perform both CPR of 100 and 120 times per minute after a period of one-day rest. The standardized adult manikin was used, and the depth of CPR was measured using a pad-sensor attached to the manikin, and the results were transferred to recording software. Analysis was done using the chi-square analysis, and p < 0.05 was considered statistically significant.
Results
A total of 35 subjects were included. The results showed that the average compression depth at 100 times/minute was more statistically superficial than the 120 times/minute treatment (5.210 ± 0.319 vs. 5.430 ± 0.283, p = 0.007). In contrast, the compression depth-on-target percentage was significantly higher at a speed of 100 times per minute (37.130 ± 10.233 vs. 18.730 ± 7.224, p = 0.0001).
Conclusion
One hundred times per minute CPR resulted in a statistically significant lower compression depth, although not clinically significant, with a statistically significant higher percentage of compression depth-on-target than 120 times per minute CPR.
Keywords: Keywords: chest compression , code blue , compression depth , CPR , resuscitation
Introduction
Both out-of-hospital cardiac arrest (OHCA) and in-hospital cardiac arrest are significant health challenges with an average of 55 OHCAs per 100.000 person-years, and survival remains poor. Studies have shown that the incidence of survival to admission was 22% (95% confidence interval: 20.7%–23.4%). 1 High-quality cardiopulmonary resuscitation (HQ-CPR) remains the standard of care during cardiac arrest and focuses on improving blood perfusion to the heart and brain. The measured quality of HQ-CPR included a depth of 5 cm, a rate of 100–120 times per minute, complete chest wall recoil compressions, and minimum interruption. 2 - 5
Chest compressions target an increase in intrathoracic pressure to generate blood flow, and American Heart Association (AHA) recommends chest compression depth of about 5 cm but no more than 6 cm. Chest compressions that are too fast or too slow will harm blood flow and a rate of 100–120 times per minute is the recommended rate by many guidelines. 2 , 6 - 8 Studies showed that chest compressions at a rate of more than 120 beats/minute result in lower life expectancy because a higher rate of chest compressions causes a shorter time for blood filling to the heart and decreases the percentage of compressions that achieve the target depth with effective chest recoil. 1 - 3
Since CPR is done manually by trained health care workers or compressors in most parts of the world, there are human-related factors to consider to the quality of CPR. Those factors are the compressor’s physical strength, stamina, and training, which contribute to how soon and how far fatigue will be set before CPR quality is reduced. Studies show that the higher the compression rate, the faster the compressor achieves fatigue and decreased compression quality. Compressor fatigue occurs in the first 60 to 90 seconds, characterized by decreased depth and altered compression rate. This decrease in the quality of CPR reduced the patient’s chance of survival. 2 , 5 , 9 , 10 We aimed to study the impact of 100 times per minute rate vs. 120 times per minute CPR rate on the depth and percentage of depth-on-target done by trained staff on a manikin.
Methods
This study was a cross-over randomized control study with recruited anesthesiology residents in a tertiary teaching hospital in Indonesia as study subjects. The study was carried out in January 2021. The hospital’s institutional review board approved the study with document number LB.02.01/X.6.5/17/2021 and written informed consent before the experiment. The writing of this paper partially follows the CONSORT guidelines for experimental studies. Written informed consent was obtained from the subject for their participation in this study, and their personal information was anonymized information to be published in this article.
Anesthesiology residents certified with advanced life support were included in the study. Exclusion criteria were body mass index (BMI) below 18 or over 25 kg/m 2 (previous studies show that this was a confounding variable for depth of compression) 2 , 3 , subjects with hearing impairment that can affect the ability to listen to verbal instructions, history of heart disease, history of severe respiratory disorders, low back pain, history of trauma to extremities, and neuropathies, and the subject who had a 24-hour nightshift the day before the time of the experiment. Drop-out criteria were subjects who could not proceed with the experiment owing to concerns about chest pain, dyspnea, or other symptoms that require the subject to stop the experiment or when the manikin and devices developed technical problems.
The subjects were asked to perform CPR 100 times per minute for 2.5 minutes without interruption and 120 times per minute for 2.5 minutes the day after. The rates were guided by a metronome, and 10 seconds listening period before the experiments were conducted. Subjects’ weight, height, and heart rate were measured before the experiment and after. The procedure was done on a manikin (Laerdal chest compressions manikin; Laerdal Medical Ltd, Orpington, UK) connected to an audio-feedback defibrillator with a recording depth sensor via pads attached to the manikin’s chest (R-series defibrillator; ZOLL Medical Corporation, Chelmsford, MA). The manikin’s depth and percentage of depth information were automatically sent to a measurement software (Rescuenet code reviewer, ZOLL Medical Corporation).
Compression rate was defined as the amount of chest compression performed in 1 minute. Depth was in centimeters, and the percentage of depth-on-target as the depth achieved above 5 cm for 2.5 minutes. All required variables were recorded automatically in the software.
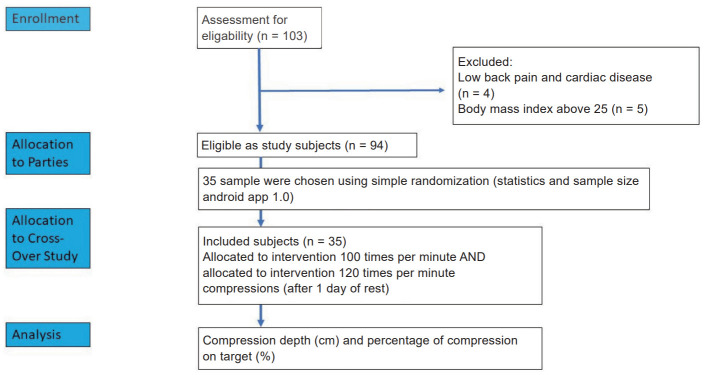
This study’s sample size was calculated using a type one error Alpha (α) of 0.05, type two error Beta (β) of 0.2. Based on a previous study 11 , the significant difference was found at standard deviation estimated at 2, and the difference in the average depth of the two rates studied on this paper was 3 cm. The calculation resulted in a minimum sample size of 13 subjects for each experiment or 26 subjects in total for both groups. Since this was a cross-over study design, 26 were taken for a minimal sample, and the number of samples was added by 10% to a minimum of 29 people. The author decided to use 35 sample subjects that were randomized from 94 eligible subjects by simple randomization (statistics and sample size Android app 1.0) ( Fig. 1 ).
Fig. 1 . CONSORT flow diagram.
The normality test was performed using the Shapiro–Wilk test. For numerical data, we used paired t -test for normally distributed data and Wilcoxon test for data not normally distributed. For categorical data, we used chi-square if the conditions were met or exact-Fisher test and Kolmogorov Smirnov. The result was considered statistically significant if p -value < 0.05.
Results
Thirty-five subjects were randomized using simple randomization technique from 94 residents that matched the inclusion and exclusion criteria ( Fig. 1 ), and all completed the study. There was no significant difference in the demographic profile amongst the subjects’ age, sex, BMI, and heart rate before and after performing CPR. In general, the subjects had an average age of 31.0 ± 2.87 years old, mainly were males (65.7%), had an average BMI of 22.56 ± 1.54 kg/m 2 , average heart rate of 85.00 ± 8.00 times/minute before performing 100 times/minute CPR, and had an average heart rate of 85.00 ± 7.00 times/minute before performing 120 times/minute CPR ( Table 1 ).
Table 1 . General characteristics of subjects .
SD: standard deviation; BMI: body mass index.
|
Variable |
Total (N = 35) |
|
Age, years |
|
|
Mean ± SD |
31.0 ± 2.87 |
|
Median |
31.00 |
|
Range, min–max |
24.00–40.00 |
|
Sex, n (%) |
|
|
Male |
23 (65.7) |
|
Female |
12 (34.3) |
|
BMI (kg/m 2 ) |
|
|
Mean ± SD |
22.56 ± 1.54 |
|
Median |
22.60 |
|
Range, min–max |
18.03–24.84 |
|
Heart rate before compression rate of 100 times/minute, times/minute |
|
|
Mean ± SD |
85.00 ± 8.00 |
|
Median |
86.00 |
|
Range, min–max |
63.00–101.00 |
|
Heart rate before compression rate of 120 times/minute, times/minute |
|
|
Mean ± SD |
85.00 ± 7.00 |
|
Median |
86.00 |
|
Range, min–max |
63.00–101.00 |
In this study, the average compression depth was 5.2 ± 0.3 cm in one cycle of CPR with 100 times/minute rate and 5.4 ± 0.3 cm in one cycle of CPR with 120 times/minute rate. There were significant differences in both groups with a p -value < 0.05. Data collected on subjects with a CPR rate of 100 times/minute showed an average compression depth of 37.1 + 10.2%, while subjects with a CPR rate of 120 times/minute showed an average compression depth of 18.7 ± 7.2%. The difference was statistically significant with p = 0.0001. The comparison between the difference in compressor pulse increase at a rate of 100 was statistically higher in the 120 times/minute group (22.7 ± 9.7 vs. 32.4 ± 8.8 times/minute, p = 0.0001) ( Table 2 ).
Table 2 . Comparison of compression depth, percentage of comparison depth, and subject heart-rate increase .
|
Variable |
Compression rate |
p value |
|
|
100 times/minute group (N = 35) |
120 times/minute group (N = 35) |
||
|
Compression depth, cm |
5.2 ± 0.3 |
5.4 ± 0.3 |
0.007 |
|
Percentage of compression depth, % |
37.1 ± 10.2 |
18.7 ± 7.2 |
0.0001 |
|
The difference in subject heart-rate increase |
22.7 ± 9.7 |
32.4 ± 8.8 |
0.0001 |
An additional analysis was done on the compression rates during the 2.5 minutes and was measured in percentage. The average rate in group 100 times per minute was 100.0 ± 1.5 times per minute and in the 120 times per minute group was 119.0 ± 1.0 times per minute. The “above” target achieved is where the actual compression rate exceeds the metronome rate, “in target” is where the actual compression rate is per the metronome rate, and “below target” is where the actual compression rate is below the metronome rate. The average for achieved target rate “above” and “in target” set-rate was statistically higher in the 100 times/minute group (40.7 ± 15.3% vs. 27.6 ± 8.3%, p = 0.0001; 49.8 ± 12.5% vs. 24.3 ± 15.2%, p = 0.0001). The average “below” target set-rate was statistically lower in the 100 times/minute group (9.3 ± 9.8% vs. 47.9 ± 16.4%, p = 0.0001). The variety of achieved target depth during the 2.5 minutes “above” and “in target” was not statistically significant in both treatments (5.1 ± 13.4% vs. 6.1 ± 9.9%, p = 0.170; 74.9 ± 18.3% vs. 80.8 ± 18.6%, p = 0.213). The average depth comparison “below” target was statistically significant in the 100 times per minute treatment (19.8 ± 18.4% vs. 13.1 ± 18.6%, p = 0.064) ( Table 3 ).
Table 3 . Comparison of achieved ranges of rate and depth during testing .
|
Variable |
Compression rate |
p value |
|
|
100 times/minute group (N = 35) |
120 times/minute group (N = 35) |
||
|
Average rate, times per minute |
100.0 ± 1.5 |
119.0 ± 1.0 |
Not applicable (study protocol) |
|
Achieved target rate |
|||
|
Above, % |
40.7 ± 15.3 |
27.6 ± 8.3 |
0.0001 |
|
In target, % |
49.8 ± 12.5 |
24.3 ± 15.2 |
0.0001 |
|
Below, % |
9.3 ± 9.8 |
47.9 ± 16.4 |
0.0001 |
|
Achieved target depth |
|||
|
Above, % |
5.1 ± 13.4 |
6.1 ± 9.9 |
0.170 |
|
In target, % |
74.9 ± 18.3 |
80.8 ± 18.6 |
0.213 |
|
Below, % |
19.8 ± 18.4 |
13.1 ± 18.6 |
0.064 |
Discussion
The study has several limitations regarding its applicability in a clinical setting. Since the treatment was done to a standardized manikin, this study cannot emulate real-life conditions of resuscitation where the patient’s anatomical variables such as weight and compliance concerning the compressor’s variables are more complex. Another weakness of this study was that the duration of the treatment was short, 2.5 minutes, and a realistic approach would be a more extended treatment period. However, the results of CPR quality and heart rate were already statistically significant, which provides a basis to conclude that even a short period of compression causes a certain amount of fatigue. There is also a potential bias that the subjects subjected to two treatments, although they can erase confounding variables such as general activity capacity, BMI, and skill, may also add a bias in which the subjects may perform a better performance in the second treatment after an experience with the first. This bias could be avoided by randomizing the treatment options on each subject during the two days of trial which was not done in this study. Points of interest for future study are to perform a subgroup analysis to observe the difference between male and female compressors, the effect of BMI on the depth of compression, the effect on chest-recoil, and a trend analysis of time to fatigue in the 2.5 minutes cycle which was not done in our study because of method and equipment limitations.
A study done in male versus female compressors found that female compressors significantly produce lower depth, and both groups produce decrease of compression depth in an earlier period of the 9 minutes experiment. The same study concluded that a rescuer with a higher BMI and in better physical fitness results was able to deliver consistent results with less fatigue. 12 Electromyography studies to measure muscle activity in the spinal and lumbar area on compressors show that fatigue began at the 2-minute mark and from the 5-minute mark, muscle activity was reduced which signals fatigue. This imbalance of muscle force has the potential to cause long-term injury in rescuers. 13
As the study result showed, the 120 times/minute treatment produced statistically significant and better depth than the 100 times/minute although it was not clinically significant because both depths were within the recommended depth (5 cm). Interestingly, achieved depth and more precise rate achievement were statistically better on the 100 times/minute depth which shows that the 100 times/minute group was more consistent in achieving the HQ-CPR target. This consistency could be related to significantly lower heart rate changes in the 100 times/minute group which signals less fatigue in the compressors
This study aims to target AHA recommendations that the appropriate rate and depth of compression must be met for each beat per cycle. This study also supports the AHA recommendation on the use of audiovisual feedback and guidance in HQ-CPR, where increasing the rate of chest compressions without rate control or frequency guidance reduces the incidence of the return of spontaneous circulation owing to a decrease in coronary backflow and a decrease in the accuracy of the compression depth percentage and which compressor fatigue played a role. 5 , 13 - 16
A randomized control trial (CPR CARE study) shows that the quality of CPR was poor in the control using no audiovisual feedback. Intervention improves compliance with the AHA guidelines associated with better outcomes. 17 The same results were also supported by a meta-analysis that in both manikin and human studies, feedback during resuscitation can result in rescuers providing compression parameters closer to recommendations. A practical recommendation from our study is that guided CPR provides a better image of resuscitation quality. As fatigue is a central component of the quality of compression influenced by compression rate, sex, and body mass, a resuscitation leader must consider this when providing high-quality resuscitation. A shorter “compressor” switch might be recommended against the guidelines in some conditions, and the use of an automatic compression device is an alternative for better consistency in resuscitation while protecting healthcare workers against CPR-related injuries.
In conclusion, our result concluded that CPR rate of 100 times/minute achieved a lower depth—but not a clinically significant difference—with a higher percentage of depth-on-target compared to the CPR rate of 120 times/minute.
References
- 1. Yan S, Gan Y, Jiang N, et al. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care . 2020;24:61. doi: 10.1186/s13054-020-2773-2 [DOI] [PMC free article] [PubMed]
- 2. Kramer-Johansen J, Edelson DP, Losert H, Köhler K, Abella BS. Uniform reporting of measured quality of cardiopulmonary resuscitation (CPR). Resuscitation . 2007;74:406-417. doi: 10.1016/j.resuscitation.2007.01.024 [DOI] [PubMed]
- 3. Lee SH, Ryu JH, Min MK, et al. Optimal chest compression rate in cardiopulmonary resuscitation: a prospective, randomized crossover study using a manikin model. Eur J Emerg Med . 2016;23:253-257. doi: 10.1097/MEJ.0000000000000249 [DOI] [PubMed]
- 4. Meaney PA, Bobrow BJ, Mancini ME, et al. Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association [published correction appears in Circulation 2013;128:e120] [published correction appears in Circulation 2013;128:e408]. Circulation . 2013;128:417-435. doi: 10.1161/CIR.0b013e31829d8654 [DOI] [PubMed]
- 5. Nolan JP, Soar J, Zideman DA, et al. European Resuscitation Council Guidelines for Resuscitation 2010 Section 1. Executive summary. Resuscitation . 2010;81:1219-1276. doi: 10.1016/j.resuscitation.2010.08.021 [DOI] [PubMed]
- 6. Nolan JP, Berg RA, Andersen LW, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein resuscitation registry template for in-hospital cardiac arrest: a consensus report from a Task Force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia). Circulation . 2019;140:e746-e757. doi: 10.1161/CIR.0000000000000710 [DOI] [PubMed]
- 7. Atkins DL, de Caen AR, Berger S, et al. 2017 American Heart Association focused update on pediatric basic life support and cardiopulmonary resuscitation quality: an update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation . 2018;137:e1-e6. doi: 10.1161/CIR.0000000000000540 [DOI] [PubMed]
- 8. González-Otero DM, Russell JK, Ruiz JM, et al. Association of chest compression and recoil velocities with depth and rate in manual cardiopulmonary resuscitation. Resuscitation . 2019;142:119-126. doi: 10.1016/j.resuscitation.2019.07.023 [DOI] [PubMed]
- 9. Ćwiertnia M, Kawecki M, Ilczak T, Mikulska M, Dutka M, Bobiński R. Comparison of standard and over-the-head method of chest compressions during cardiopulmonary resuscitation—a simulation study. BMC Emerg Med . 2019;19:73. doi: 10.1186/s12873-019-0292-8 [DOI] [PMC free article] [PubMed]
- 10. Jaafar A, Abdulwahab M, Al-Hashemi E. Influence of rescuers’ gender and body mass index on cardiopulmonary resuscitation according to the American Heart Association 2010 Resuscitation Guidelines. Int Sch Res Notices . 2015;2015:246398. doi: 10.1155/2015/246398 [DOI] [PMC free article] [PubMed]
- 11. Duval S, Pepe PE, Aufderheide TP, et al. Optimal combination of compression rate and depth during cardiopulmonary resuscitation for functionally favorable survival. JAMA Cardiol . 2019;4:900-908. doi: 10.1001/jamacardio.2019.2717 [DOI] [PMC free article] [PubMed]
- 12. Russo SG, Neumann P, Reinhardt S, et al. Impact of physical fitness and biometric data on the quality of external chest compression: a randomised, crossover trial. BMC Emerg Med . 2011;11:20. doi: 10.1186/1471-227X-11-20 [DOI] [PMC free article] [PubMed]
- 13. Cobo-Vázquez C, De Blas G, García-Canas P, Del Carmen Gasco-García M. Electrophysiology of muscle fatigue in cardiopulmonary resuscitation on manikin model. Anesth Prog . 2018;65:30-37. doi: 10.2344/anpr-65-01-06 [DOI] [PMC free article] [PubMed]
- 14. Rössler B, Goschin J, Maleczek M, et al. Providing the best chest compression quality: standard CPR versus chest compressions only in a bystander resuscitation model. PLoS One . 2020;15:e0228702. doi: 10.1371/journal.pone.0228702 [DOI] [PMC free article] [PubMed]
- 15. Heidenreich JW, Berg RA, Higdon TA, Ewy GA, Kern KB, Sanders AB. Rescuer fatigue: standard versus continuous chest-compression cardiopulmonary resuscitation. Acad Emerg Med . 2006;13:1020-1026. doi: 10.1197/j.aem.2006.06.049 [DOI] [PubMed]
- 16. Cheng A, Brown LL, Duff JP, et al. Improving cardiopulmonary resuscitation with a CPR feedback device and refresher simulations (CPR CARES Study): a randomized clinical trial. JAMA Pediatr . 2015;169:137-144. doi: 10.1001/jamapediatrics.2014.2616 [DOI] [PubMed]
- 17. Kirkbright S, Finn J, Tohira H, Bremner A, Jacobs I, Celenza A. Audiovisual feedback device use by health care professionals during CPR: a systematic review and meta-analysis of randomised and non-randomised trials. Resuscitation . 2014;85:460-471. doi: 10.1016/j.resuscitation.2013.12.012 [DOI] [PubMed]