Abstract
Background
With advancements in technology and ablation techniques, catheter ablation for the treatment of atrial fibrillation (AF) has become safer with time. In the past, standard-of-care recommended overnight stay for outpatient procedures. As safety has improved and procedure times have shortened, some centers have allowed for same-day discharge. We report the results of a multi-center, randomized clinical trial investigating the safety of same-day discharge post-cryoballoon ablation.
Methods
Patients with paroxysmal atrial fibrillation underwent pulmonary vein isolation (PVI) with the Medtronic Arctic Advance cryoballoon at 3 US centers. Six hours after the procedure, patients were randomized to either stay overnight or be discharged same day.
Results
A total of 49 patients were enrolled. Two patients were withdrawn prior to randomization. One patient chose to withdraw after randomization. Of the 22 patients randomized to same-day discharge and the 23 patients randomized the overnight stay, no significant adverse outcomes were reported in either group. Occurrence of adverse events did not differ significantly between the two groups. Procedure time and fluoroscopy time did not significantly differ between groups.
Conclusions
This is the first randomized trial examining the safety of same-day discharge post-cryoballoon ablation. Based on our results, same-day discharge following cryoballoon ablation for paroxysmal AF is a safe option following uncomplicated ablation for PVI. Operators should use their discretion in selecting patients for same-day discharge.
Keywords: Atrial fibrillation, Cryoballoon ablation, Same-day discharge, Catheter ablation
Introduction
Catheter ablation of atrial fibrillation (AF) has significantly grown in volume due to improvements in safety and efficacy. For patients undergoing an elective AF ablation, same-day discharge has been closely examined as a cost-saving measure for hospital systems; however, the value of medical economics must be balanced against the priority of patient safety. As AF ablation practice and outcomes continue to evolve and rates of post-procedural complications continue to decline, multiple studies have demonstrated the safety of same-day discharge (SDD). Late complications usually occur more than 24 h post-AF ablation and are, therefore, not impacted by routine overnight stay (ONS) [1]. Previous studies have shown that there were no statistically significant differences between SDD and ONS groups in terms of acute complication, emergency room visits, major adverse cardiovascular events, mortality, and 30-day readmission. However, most research related to the feasibility of same-day discharge in patients undergoing AF ablation has been retrospective or observational in nature. Among twelve major studies, a review by Rashedi et al. included 18,065 ablations, of which 7320 (40.52%) patients were discharged on the same day as their procedure. Major complications remained low 0.7–1.1% and readmission or emergency room visits were also about 3%, without statistically significant differences between SDD and overnight stay (ONS) groups [2]. A similar review by Prasitlumkum et al. analyzing ten of the same studies did not find a significant difference in rate of complications [3]. Additional studies include the SODA study, which showed no statistically significant difference between SDD and ONS patient groups in terms of mortality, major adverse cardiovascular events, all-cause readmission, or AF readmission [4]. Another study by Sahashi et al. provided a 1:3 propensity-matched study including 1751 matched pairs. Their analyses did not show a significant difference between 30-day readmission (12.7% for SDD group versus 9.7% for ONS group) [5].
Of note, the majority of patients in the aforementioned studies received radiofrequency (RF) ablation, with the exception of the study by Creta et al. (79.2% cryoballoon) and the study by Kowalski et al. Although the cryoballoon system is generally more expensive, cryoballoon ablation is associated with a reduction in costs driven by fewer hospitalizations and reduction in the need for repeat ablation, compared to radiofrequency (RF) ablation [6]. Same-day discharge following cryoballoon ablation could further reduce costs and healthcare utilization. The data consistently demonstrates same-day discharge is safe and feasible, but this data is not conclusive primarily due to its retrospective nature. We report the results of the first multi-center, randomized clinical trial investigating the safety of same-day discharge post-cryoballoon ablation.
Methods
This study protocol was approved by each center’s Institutional Review Board. Study patients provided informed consent prior to study participation.
Study population
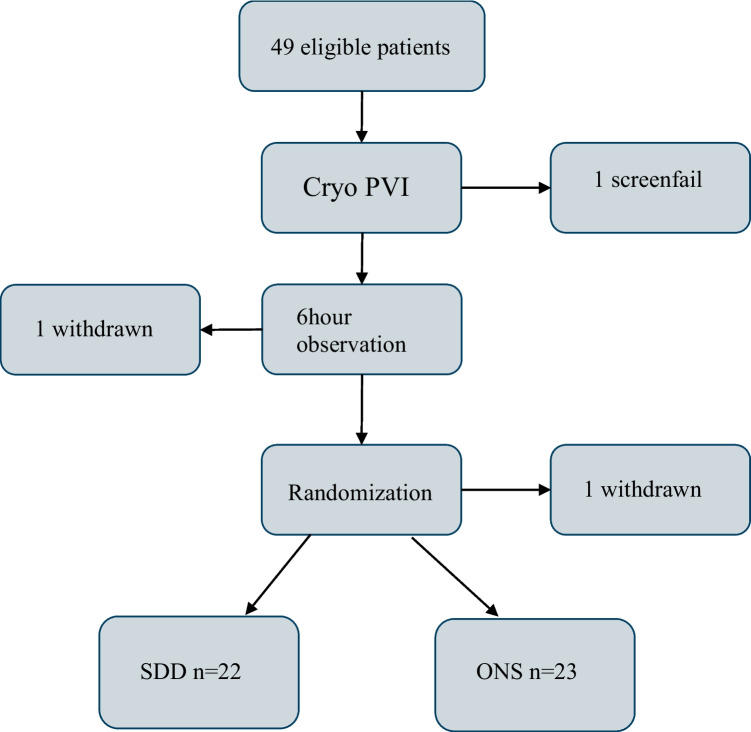
Patients with paroxysmal atrial fibrillation that underwent pulmonary vein isolation (PVI) using cryoballoon (Medtronic Arctic Advance™) at 3 US centers were screened and enrolled. To participate, subjects were required to be ≥ 18 years old, have a left ventricular ejection fraction (LVEF) > 40%, a creatinine clearance > 50, and CHA2DS2-VASc ≤ 3. Ablation procedure was performed under general anesthesia. If a patient had an uncomplicated procedure with < 4 h of general anesthesia, they were monitored for 6 h post-procedure, during which time complete hemostasis at the access site(s) was achieved. Provided a patient experienced no complications or incidence of early AF during this observation period, the patient was then randomized to same-day discharge (SDD group) or overnight stay (ONS group). This decision-making process is summarized in Fig. 1.
Fig. 1.
Decision-making tree
Ablation procedure and periprocedural management
All cryoballoon ablations were performed at one of three participating hospitals with the 28 mm Arctic Advance™ cryoballoon (Medtronic, Minneapolis). Details on PVI procedure with cryoballoon have been described elsewhere, previously [7]. The cryoballoon was advanced to the left atrium (LA) though the 12F FlexCath™ sheath (Medtronic, Minneapolis) following successful transseptal puncture. Choice of 3D electroanatomic mapping system was up to provider discretion with or without PV venogram. Pulmonary vein isolation was achieved with the cryoballoon by freezing–thawing cycle(s) at the antrum of each PV upon satisfying occlusion of PV and time-to-isolation. In the present study, no extra-PV ablation with the exception of a cavo-tricuspid isthmus line performed with RF as necessary. An activated clotting time (ACT) was maintained > 350 s throughout the procedure by using heparin which was reversed at the end of procedure.
At the end of the procedure, after all catheters and sheaths were removed, a Figure-8 suture was placed over the puncture site at the groin(s) with or without a venous closure device. Patients were transferred to the recovery room for routine post-procedural monitoring. Patients were monitored for 6 h post-procedure. Due to the need for 6 h of monitoring, many of the study procedures were performed prior to noon. Time to ambulation was based on institutional standard of care, 3 to 4 h. Complete hemostasis was defined as no pain, active bleeding, or expanding hematoma at the access site(s) after ambulating. If patients maintained normal sinus rhythm and did not experience vascular complication during this observation period, they were then randomized to same-day discharge or overnight stay. The randomization was balanced within each site using a dynamic blocked randomization scheme. There was no stratification beyond the study site. Patients then returned to outpatient clinics for follow-up at 2 weeks and 1 month.
Study endpoints
The primary endpoint was acute and short-term safety within 30 days of procedure. Serious adverse events were defined as complications requiring medical-surgical intervention, inpatient stay or prolonged hospitalization (> 24 h), permanent injury or impairment, or death. The secondary endpoint was healthcare utilization, defined as hospital readmission, emergency department visits, and unscheduled office visits.
Statistical analysis
Sample size calculation was performed prior to patient enrollment. Enrollment target was 260 subjects, with 130 randomized to each of the two randomized arms. With an expected loss to follow-up rate of 5%, we expected 123 subjects in each arm who had completed 30-day follow-up. This sample size would provide high power of at least 81% for the Farrington and Manning non-inferiority score test (at the 0.05 significance level) to conclude that the major adverse event rate in the same day discharge arm is no more than 10% higher than that of the next day discharge arm, given both groups having exactly the same major adverse event rate ranging from 0 to 10%.
Baseline characteristics including age, gender, race, ethnicity, and procedural parameters including procedure time, fluoroscopy times, contrast use, and procedural complications were summarized in each arm using the median and interquartile range for continuous variables and proportion for categorical variables, and data were compared between the two arms using unpaired t-test for continuous variables and Fisher’s exact for categorical variables. The proportion of patients with hospital readmission, emergency department visits, and unscheduled office visits was summarized for each arm using proportion and compared between the two arms using Fisher’s exact test.
Results
Enrollment
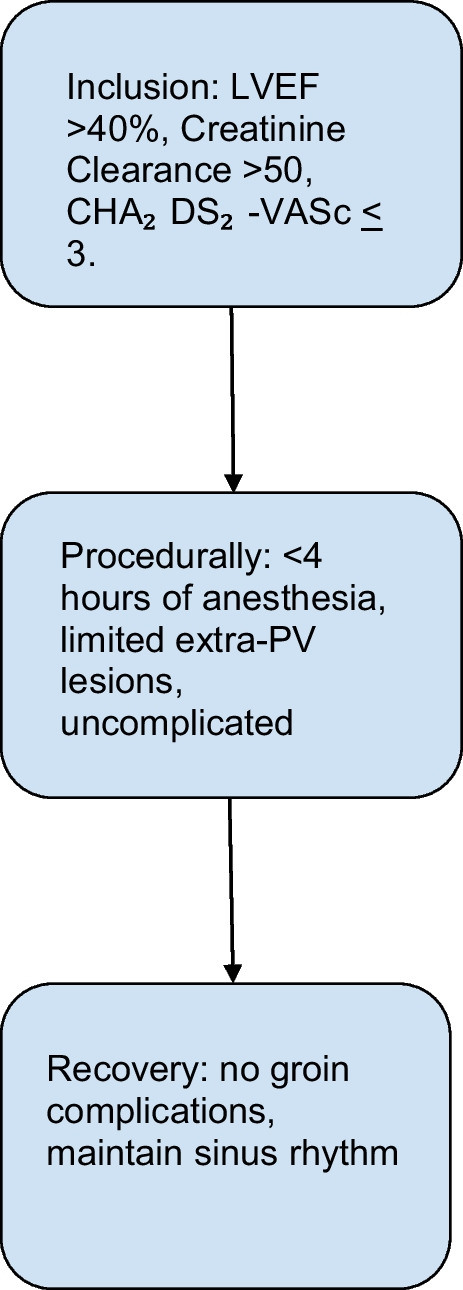
Enrollment began in November 2018 and ended in October 2020. A total of 49 patients signed the informed consent and were enrolled. One patient was determined to be a screen failure following additional complex ablation. One patient was withdrawn due to concern for post-operative complications prior to randomization. This was the only patient not considered eligible for same-day discharge. Thus, 46 patients completed randomization; however, one patient chose to withdraw following randomization to SDD. The remaining 45 patients completed study randomization and follow-up (Fig. 2). There was no crossover between groups.
Fig. 2.
Enrollment
Demographics
Clinical characteristics at baseline were balanced between the two groups (Table 1). There were no statistically significant differences between baseline characteristics, comorbidities, or medication use. During data analysis, one patient in ONS was found to have an incorrectly calculated CHA2S2VASc score. However, as this patient completed randomization and study follow-up, their data was still included in this analysis.
Table 1.
Patient demographics
| Same-day discharge (n = 22) | Overnight stay (n = 23) | |
|---|---|---|
| Male sex | 15 (68%) | 17 (74%) |
| Age | 58.5 ± 12.0 | 61.96 ± 7.84 |
| Body mass index | 31.3 ± 5.42 | 29.6 ± 4.06 |
| New York Heart Association class I | 1 (4.5%) | 0 (0%) |
| New York Heart Association class III | 1 (4.5%) | 1 (4.3%) |
| New York Heart Association class unknown | 3 (13.6%) | 0 (0%) |
| 1st degree atrioventricular block | 3 (13.6%) | 1 (4.3%) |
| Unknown atrioventricular block | 0 (0%) | 1 (4.3%) |
| Right bundle branch block | 0 (0%) | 1 (4.3%) |
| Diabetes | 2 (9.0%) | 0 (0%) |
| Hyperlipidemia | 9 (41%) | 12 (52%) |
| Chronic kidney disease | 0 (0%) | 1 (4.3%) |
| Coronary artery disease | 1 (4.5%) | 3 (13%) |
| Myocardial infarction | 1 (4.5%) | 1 (4.3%) |
| Percutaneous coronary intervention | 1 (4.5%) | 1 (4.3%) |
| Hypertension | 12 (54.5%) | 11 (47.8%) |
| Transient ischemic attack | 0 (0%) | 1 (4.3%) |
| Stroke | 1 (4.5%) | 0 (0%) |
| Anticoagulation use | 17 (77.2%) | 20 (87%) |
| Antiarrhythmic drug use | 14 (63.6%) | 9 (39.1%) |
| ACE-inhibitor use | 2 (9.0%) | 2 (8.7%) |
| Beta blocker use | 10 (45.5%) | 15 (65.2%) |
Primary endpoints
Procedure time for the SDD group was 85.6 ± 18.7 and 81.1 ± 19.6 min for the ONS group, which was not statistically significant. Intraoperative fluoroscopy time was significantly different between groups by unpaired t-test, 15.2 ± 7.5 min for the SDD group and 11.3 ± 5.1 min for the ONS group (p = 0.0447). Eight patients had additional RFA touch (1 AT, 1 SVT, 5 RA Flutter and 1 LA flutter).
All patients completed 30-day follow-up per study protocol. No significant adverse outcomes were reported in either group. There were no instances of phrenic nerve palsy, pulmonary vein stenosis, ventricular tachyarrhythmia, pericardial tamponade, hemoptysis, stroke or transient ischemic attack, myocardial infarction, pacemaker implant, atrioesophageal fistula, neurological deficit, or deaths in either group. Nearly all patients received a Figure-8 Stitch to achieve hemostasis at the end of procedure (SDD: 20/22; ONS 19/23). One patient in the SDD group and three patients in the ONS group also received an adjunctive vascular closure device. Manual compression alone was applied in one patient from each group.
Arrhythmia recurrence
Three patients from the SDD group had recurrence of symptomatic palpitations or documented atrial tachyarrhythmia by 30-day follow-up. New medications were started in two of the three patients. Two patients were scheduled for direct current cardioversion (DCCV), but they did not require the procedure due to spontaneous conversion to normal sinus rhythm (NSR). One patient in the ONS group had new-onset atrial flutter during overnight stay and underwent DCCV the morning after the procedure. All other patients, including the one from the ONS group who received cardioversion during overnight stay, maintained sinus rhythm at the end of this study. No repeat ablations were performed during the follow-up period.
Secondary endpoint
There was one emergency room visit per group. One patient in the SDD group presented 2 days post-ablation due to new-onset cough. The examination workup was negative and the patient completed the study without further complaints or adverse events. One patient in the ONS group presented to the emergency department (ED) approximately 2 weeks postoperatively for shortness of breath. The patient was diagnosed with pneumonia unrelated to the procedure and completed treatment. No patients were hospitalized.
Discussion
To our knowledge, this is the first prospective randomized trial examining the safety and feasibility of same-day discharge post-cryoballoon ablation. Overnight stay and patient observation have been the standard practice at most centers for patients undergoing AF ablation. Traditionally, this was to ensure that patients had no acute complications within 24 h post-procedure. With experience gained and novel technologies, AF ablation has become a routine procedure in any EP lab and can be completed on an outpatient basis, making SDD possible and an option for both physicians and patients. We found that in selected low-risk patients, SDD is feasible and, as compared with ONS, is not associated with more acute and short-term serious adverse events occurred within 30 days after discharge. This is consistent with previously published findings in retrospective, observational studies.
The primary consideration for SDD should be patient safety. A number of techniques may be utilized to reduce the most common complications, including but not limited to anesthetic complication, access complication, cardiac tamponade, and heart failure [8]. Ultrasound guidance for femoral venous access in electrophysiology procedures reduces major and minor vascular complications, inadvertent artery puncture, post-procedural groin pain, and puncture time [9]. Insertion of coronary sinus catheter from the femoral vein eliminates the possibility of pneumothorax. Use of intracardiac echocardiography allows the operator to monitor the pericardium in real-time throughout the procedure and confirm the absence of pericardial effusion after all catheters are removed. Even if a patient developed tamponade after the procedure, symptoms would usually present within the next few hours. Chances of delayed tamponade exist but extremely low if a patient remained asymptomatic and hemodynamically stable by the time that figure of 8 suture was removed (i.e., 4 h after procedure). Given the long period of observation, echocardiogram was not performed prior to same-day discharge. It is unclear that by keeping how many patients for an ONS can one adverse event due to delayed tamponade be prevented.
The selection of ablation modality itself may also be a consideration for determining SDD. Cryoablation of AF is different from RF ablation in multiple aspects which affect the type of discharge and safety considerations. For example, no extra fluid is needed during a cryoablation procedure, preventing fluid overload/congestive heart failure exacerbation, especially in patients with pre-existing structural heart disease. Although cryoablation does not create steam pop, cryoballoon ablation also carries additional considerations. The 12 Fr sheath is required for cryoballoon and is therefore potentially associated with higher risk of complications at the access site. Our practice suggested that a Figure-8 suture is a reliable method to achieve hemostasis for venous puncture, even in cases when a large sheath is used. There was no major groin complication in either group of our study. Venous closure devices are a potential option to reduce bed rest time, hospital stay, and groin complications pending more evidence from clinical trials. However, the use of vascular closure devices for every patient may drive up costs and offset the cost-effective benefits of SDD. Phrenic nerve injury is more commonly seen in a cryoablation procedure, but should not delay SDD, as most patients are asymptomatic or have minor symptoms and will generally recover in the next few days to weeks [10].Considering these factors, cryoablation of AF is theoretically associated with a lower risk of acute/short-term serious adverse events compared to RF ablation procedure, but no head-to-head comparison has ever been made in an SDD trial, to date.
The authors acknowledge that complications are not always entirely avoidable; therefore, patient selection is also a key factor in SDD. Evaluation criteria should include age, comorbidities, patient preference, caregiving support, and level of ablation complexity, among others, as was implemented in our study and others. We consider participants of the present study “low risk” because they generally only received PVI during the procedure, completely recovered from general anesthesia, and had no symptoms and signs of tamponade, or major access complications before randomization. In fact, these patients represented the majority of AF ablation cases in the EP lab and recovery room. There was one case of ED visit in each group, but neither was SDD-related. Interestingly, in the study performed by Deyell MW et al., the most common cause of ED visit after SDD was AF/arrhythmia [11]. Although recurrent atrial tachyarrhythmia is common, especially during the first 90 days after AF ablation, there is unlikely a causal relationship between recurrence and SDD; and recurrent atrial tachyarrhythmia should not be a concern of SDD.
In addition, although cost information was not systematically collected from all participating centers, our study further supports same-day discharge as cost-effective for hospitals. Catheter ablation is a costly procedure, primarily due to the tools for the procedure and the need for overnight hospitalization [12]. Based on the cost estimates provided by Banner University Medical Center Phoenix, SDD could result in a savings of $2286 to $4502 per patient depending on how patients are monitored overnight. For comparable analysis to previous studies, assuming a caseload of 250 patients annually, that would be a cost savings for the hospital between $571,500 and $1,125,500. This cumulative savings would depend on the proportion of patients discharged the same day as their procedure. The calculation is assuming all 250 patients were discharged same day and includes the staffing for monitoring and the cost associated with patient care per bed. Cost information was not collected during our study; therefore, this is merely an estimation that is higher than the Kowalski et al. experience ($45,825–$83,813 in annual savings) [13] and estimates by Creta et al. (£83, 927) [14]. Further study is needed to apply these data beyond the inpatient setting, perhaps to outpatient surgery centers. Such expansion may provide an additional setting to enhance ablation access and further compound savings.
These cost estimates do not include the use of vascular closure devices, as the study did not require their use prior to SDD, and the cost estimate is beyond the scope of this report. Data examining the safety and feasibility of SDD with the use of vascular closure devices has been reported as a method of mitigating one of the most common complications associated with catheter ablation—vascular complications [15]—however, the use of vascular closure devices for every patient may drive up costs for SDD depending on the device and hospital system. Yet, the usage of closure devices may allow for same-day discharge for patients who are considered “higher risk,” such as those with elevated venous pressure. Current trials such as the AMBULATE trial [16] exclude these patients; therefore, future trials should consider studying this population.
Study limitations
This study is limited primarily by the sample size. The study was conducted during the COVID-19 pandemic, which greatly impacted recruitment. Many patients were unwilling to participate in the study due to the possibility of an overnight stay. Furthermore, several institutions halted elective procedures and clinical research studies for prolonged periods throughout the pandemic, further limiting enrollment. The results of this study, despite its small sample size, are consistent with larger non-randomized studies. It is prudent to consider further randomized trials with a larger sample size.
The inclusion criteria may also represent a type of selection bias. Although selection bias of distribution between groups was mitigated by randomization, the patients selected for consideration of same-day discharge in this trial are among the healthiest possible due to limited comorbidities. Further study is needed for consideration of same-day discharge in patient populations with greater risk.
Conclusion
This is the first randomized trial examining the safety of same-day discharge after cryoballoon ablation for AF. Our results are consistent with prior retrospective data, further supporting same-day discharge following cryoballoon ablation for paroxysmal AF as a safe option. Operators should use their discretion in selecting patients for same-day discharge.
Funding
This study was funded by a research grant from Medtronic, Inc. (Minnesota, USA).
Data Availability
The data that support the findings of this study are available from the corresponding author, ETC, upon reasonable request.
Declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of each institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Institutional Review Board for all centers.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
Dr. John Harding has consulted for and received research support from Medtronic. Dr. Wilber Su has received research grants and consulted for Medtronic. The remaining authors have no relevant financial or non-financial interests to disclose.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Paul Nordin A, Drca N, Insulander P, Bastani H, Bourke T, Braunschweig F, Kennebäck G, von Olshausen G, Sadigh B, Saluveer O, Tapanainen J, Schwieler J, Åkerström F, Jensen-Urstad M. Low incidence of major complications after the first six hours post atrial fibrillation ablation: is same-day discharge safe and feasible in most patients? J Cardiovasc Electrophysiol. 2021;32(11):2953–2960. doi: 10.1111/jce.15243. [DOI] [PubMed] [Google Scholar]
- 2.Rashedi S, Tavolinejad H, Kazemian S, Mardani M, Masoudi M, Masoudkabir F, Haghjoo M. Efficacy and safety of same-day discharge after atrial fibrillation ablation: a systematic review and meta-analysis. Clin Cardiol. 2022;45(2):162–172. doi: 10.1002/clc.23778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prasitlumkum N, Cheungpasitporn W, Chokesuwattanaskul R, Kewcharoen J, Tokavanich N, Navaravong L, Jongnarangsin K. Comparison between same-day discharge and overnight stay after atrial fibrillation ablation: systematic review and meta-analysis. Pacing Clin Electrophysiol. 2021;44(12):2054–2066. doi: 10.1111/pace.14380. [DOI] [PubMed] [Google Scholar]
- 4.Bailey SA, Subramanian K, Sanchez J, P Horton R, Natale A, Thambidorai S. Same day versus overnight discharge in patients undergoing ablation for atrial fibrillation (SODA) study. J Atr Fibrillation. 2021;14(2):20200499. 10.4022/jafib.20200499. [DOI] [PMC free article] [PubMed]
- 5.Sahashi Y, Kuno T, Tanaka Y, Passman R, Briasoulis A, Malik AH. The 30-day readmission rate of same-day discharge protocol following catheter ablation for atrial fibrillation: a propensity score-matched analysis from National Readmission Database. Europace. 2022;24(5):755–761. doi: 10.1093/europace/euab296. [DOI] [PubMed] [Google Scholar]
- 6.Chun KRJ, Brugada J, Elvan A, Gellér L, Busch M, Barrera A, Schilling RJ, Reynolds MR, Hokanson RB, Holbrook R, Brown B, Schlüter M, Kuck KH; FIRE AND ICE Investigators. The impact of cryoballoon versus radiofrequency ablation for paroxysmal atrial fibrillation on healthcare utilization and costs: an economic analysis from the fire and ice trial. J Am Heart Assoc. 2017;6(8):e006043. 10.1161/JAHA.117.006043. Erratum in: J Am Heart Assoc. 2017 Sep 15;6(9). [DOI] [PMC free article] [PubMed]
- 7.Su W, Kowal R, Kowalski M, Metzner A, Svinarich JT, Wheelan K, Wang P. Best practice guide for cryoballoon ablation in atrial fibrillation: the compilation experience of more than 3000 procedures. Heart Rhythm. 2015;12(7):1658–1666. doi: 10.1016/j.hrthm.2015.03.021. [DOI] [PubMed] [Google Scholar]
- 8.Cappato R, Calkins H, Chen SA, Davies W, Iesaka Y, Kalman J, Kim YH, Klein G, Natale A, Packer D, Skanes A, Ambrogi F, Biganzoli E. Updated worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circ Arrhythm Electrophysiol. 2010;3(1):32–38. doi: 10.1161/CIRCEP.109.859116. [DOI] [PubMed] [Google Scholar]
- 9.Kupó P, Pap R, Sághy L, Tényi D, Bálint A, Debreceni D, Basu-Ray I, Komócsi A. Ultrasound guidance for femoral venous access in electrophysiology procedures-systematic review and meta-analysis. J Interv Card Electrophysiol. 2020;59(2):407–414. doi: 10.1007/s10840-019-00683-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chu E, Zhang C, Musikantow DR, Turagam MK, Langan N, Sofi A, Choudry S, Syros G, Miller MA, Koruth JS, Whang W, Dukkipati SR, Reddy VY. Barriers and financial impact of same-day discharge after atrial fibrillation ablation. Pacing Clin Electrophysiol. 2021;44(4):711–719. doi: 10.1111/pace.14217. [DOI] [PubMed] [Google Scholar]
- 11.Deyell MW, Leather RA, Macle L, Forman J, Khairy P, Zhang R, Ding L, Chakrabarti S, Yeung-Lai-Wah JA, Lane C, Novak PG, Sterns LD, Bennett MT, Laksman ZW, Sikkel MB, Andrade JG. Efficacy and safety of same-day discharge for atrial fibrillation ablation. JACC Clin Electrophysiol. 2020;6(6):609–619. doi: 10.1016/j.jacep.2020.02.009. [DOI] [PubMed] [Google Scholar]
- 12.Deshmukh A, Patel NJ, Pant S, Shah N, Chothani A, Mehta K, Grover P, Singh V, Vallurupalli S, Savani GT, Badheka A, Tuliani T, Dabhadkar K, Dibu G, Reddy YM, Sewani A, Kowalski M, Mitrani R, Paydak H, Viles-Gonzalez JF. In-hospital complications associated with catheter ablation of atrial fibrillation in the United States between 2000 and 2010: analysis of 93 801 procedures. Circulation. 2013;128(19):2104–2112. doi: 10.1161/CIRCULATIONAHA.113.003862. [DOI] [PubMed] [Google Scholar]
- 13.Kowalski M, Parikh V, Salcido JR, Chalfoun N, Albano A, O'Neill PG, Bowers MR, Gauri A, Braegelmann KM, Lim HW, Akhrass P, Shah R, Bekheit S, Epstein LM, Aryana A. Same-day discharge after cryoballoon ablation of atrial fibrillation: a multicenter experience. J Cardiovasc Electrophysiol. 2021;32(2):183–190. doi: 10.1111/jce.14843. [DOI] [PubMed] [Google Scholar]
- 14.Creta A, Ventrella N, Providência R, Earley MJ, Sporton S, Dhillon G, Papageorgiou N, Chow A, Lambiase PD, Lowe M, Schilling RJ, Finlay M, Hunter RJ. Same-day discharge following catheter ablation of atrial fibrillation: a safe and cost-effective approach. J Cardiovasc Electrophysiol. 2020;31(12):3097–3103. doi: 10.1111/jce.14789. [DOI] [PubMed] [Google Scholar]
- 15.Portoles-Hernandez A, Toquero-Ramos J, Garcia-Gomez S, Castro-Urda V, Garcia-Izquierdo E, Jimenez-Sanchez D, Segura-Dominguez M, Aguilera-Agudo C, Veloza-Urrea D, Fernandez-Lozano I. Same-day discharge for atrial fibrillation ablation: use of suture-mediated vascular closure device. EP Europace. 2021;23(Supplement_3):euab116.291,
- 16.Natale A, Mohanty S, Liu PY, Mittal S, Al-Ahmad A, De Lurgio DB, Horton R, Spear W, Bailey S, Bunch J, Musat D, O'Neill P, Compton S, Turakhia MP; AMBULATE Trial Investigators. Venous vascular closure system versus manual compression following multiple access electrophysiology procedures: the ambulate trial. JACC Clin Electrophysiol. 2020;6(1):111–124. 10.1016/j.jacep.2019.08.013. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, ETC, upon reasonable request.