To the editor,
I read the state-of-the-art review of interstitial cystitis/bladder pain syndrome (IC/BPS) by Ueda et al. [1] with great interest. An erudite, scholarly paper, it states there is a crisis as regards IC—namely, there has been no progress for 25 years. The authors concluded [1], “Thus, there can be no bright future for IC/BPS without these 3 steps: (1) understanding the symptoms, (2) detecting abnormal findings in or outside the bladder, and (3) verifying that the abnormality is the cause of the symptoms” [1]. This commentary aims to address their statements, first by introducing an important discovery to International Neurourology Journal readers, Dr. Scheffler’s histologically validated cure of IC/BPS with Hunner ulcer (nonulcerating) [2], and then by discussing its implications relevant to those 3 statements [1].
Scheffler set out to manage a 73-year-old woman with classical posterior fornix syndrome (PFS) symptoms—predictably co-occurring chronic pelvic pain (CPP), urge, abnormal emptying/retention, nocturia, and frequency—caused by laxity of the uterosacral ligaments (USLs) and cured by repair thereof [3], not IC, by repair of cardinal ligaments and USLs, which is the standard cure for PFS [3].
To test whether any relationship exists between PFS and IC [2], we revisited previous data from 46 women with CPP and 171 bladder symptoms, treated for PFS with tissue fixation system (TFS) mini-sling surgery, who fit the International Continence Society (ICS) definition of IC [4]. Their workup [5], included the validated Integral Theory System Questionnaire, preoperative and postoperative urodynamics evaluations, and speculum testing (Fig. 1). The cure rates [5] were 76% for CPP, 74% for urge incontinence, 80% for abnormal emptying/retention, 75% for nocturia 75%, and 50% for frequency. Two women had glomerulations. None had Hunner ulcers. In another study by Wagenlehner et al. [6], among 1,420 women with prolapse and PFS symptoms treated by 2 different posterior sling operations, 599 had CPP, 1,179 had bladder symptoms, and 162 had fecal incontinence. A TFS study by Liedl et al. [7], found that 194 women had CPP, with 881 bladder symptoms that were variously cured. Other data showed small pain/urge symptom deterioration at 5 years [8]. The cure of CPP and bladder symptoms [6-8] was in accordance with the ICS definition of IC. All studies [6-8] fit the IC definition [4], but no Hunner ulcers were reported in any study.
Fig. 1.
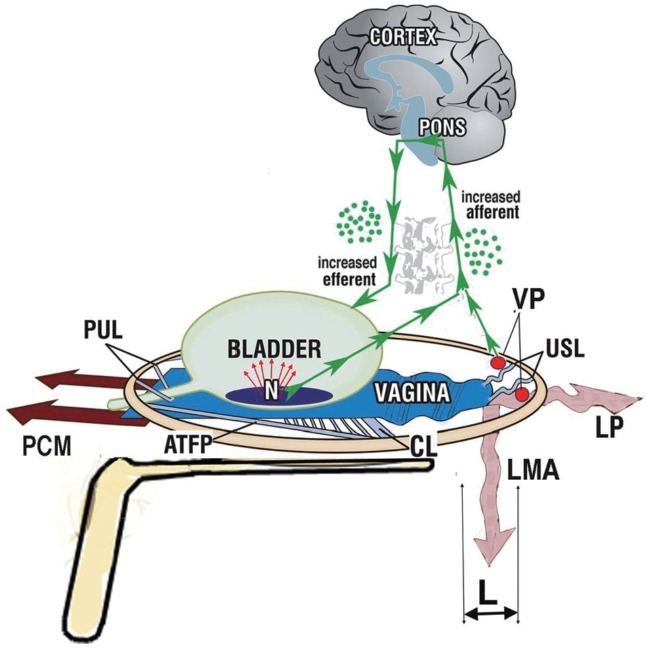
The speculum test reduces urge by mechanically supporting the stretch receptors (N). It reduces pain by mechanically supporting the uterosacral ligaments (USL), which are the natural support of the visceral plexuses (VP). Withdrawal of the supporting speculum is followed by immediate return of the pain and, if present, urinary urgency. Large arrows represent the reflex striated muscle forces of the PCM, LP, and LMA. The green arrows represent the afferent nerve impulses from N and efferent impulses from the pons. “L” and the wavy form of the muscles represent ligament laxity and weak contractile force, respectively. PUL, pubourethral ligaments; CL, cardinal ligaments; PCM, pubococcygeus muscle; LP, levator plate muscle; LMA, longitudinal muscle of the anus; ATFP, arcus tendineus fasciae pelvis.
How is it that PFS studies [2,5-8] following the integral theory paradigm [9] have reported pain/urge cure by USL repair, while scholarly reviews have stated that the pathogenesis of IC is unknown and there is no cure [1]?
The answer may be found in Thomas Kuhn’s famous book, The Structure of Scientific Revolutions [10]. Kuhn [10] states that solutions to chronic problems in science do not arrive gradually. Instead, they arrive in leaps. They are usually disruptive and only become “normal science” when there is a crisis. The leap in the science behind the IC cure, was the integral theory of female urinary incontinence, which was first published in 1990 [9]. It stated that stress urinary incontinence (SUI) and urge urinary incontinence both had the same origin, laxity in the vagina or its supporting ligaments, a consequence of damaged collagen/elastin from childbearing or age. The prototype midurethral sling for SUI cure [9] quickly became the gold-standard operation for SUI (tension-free vaginal tape). The urge, pain and emptying part of the theory [11] is the subject of this commentary.
With reference to (1) understanding the symptoms (i.e., elucidating the pathogenesis of OAB and bladder pain, “related to the nervous, endocrine, and immune systems”) [1], the hypothesis of lax USLs causing CPP was described in the German literature in 1938 by Martius [12] and independently in the English literature by Petros [13] in 1996.
Fig. 2 describes afferent and efferent visceral nerves that travel to the visceral plexus (VP), which is best regarded as a type of nerve junction. If USLs are loose, the force of gravity may stimulate unsupported VP afferent axons from specific end organs, usually several at a time, which explains the co-occurrence of CPP at several different sites. VPs send afferent impulses to the brain, which (falsely) interprets them as an injury (pain) coming from a particular end organ(s). The brain reacts to the perceived injury by sending visceral efferent signals to the end organ, to activate resident “sleeper cells” (Fig. 2). These may produce T cells, mast cells, and other inflammatory cells. In this context, an ulcerated Hunner ulcer could be viewed as an extreme manifestation of this inflammatory reaction. With reference to (2) “detecting abnormal findings in or outside the bladder” [1], the speculum test (Fig. 1) works by mechanically supporting USLs. This support temporarily restores the structural integrity of the USLs to decrease pain afferents and urge afferents by supporting the urothelial receptors. With reference to (3) “verifying that the abnormality is the cause of the symptoms“ [1], reports of PFS (or IC) cure by surgically reinforcing USLs [2,5-8] verify the hypothesis of weak USLs as causative of IC.
Fig. 2.
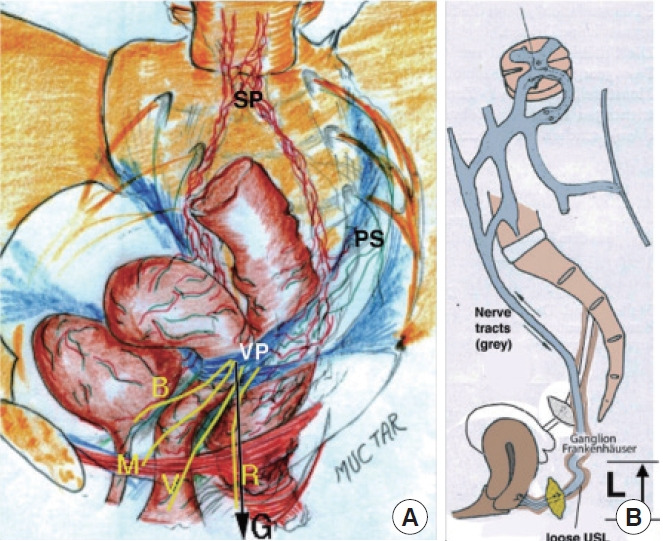
Pathogenesis of chronic pelvic pain from unsupported visceral plexuses. (A) The visceral plexus (VP) with the SP (sympathetic T11–L2) and PS (parasympathetic S2–4) components. End organ afferent nerves from muscles (M), bladder (B), vagina (V), rectum (R)—travel to the VP, which serves as a type of relay junction. G signifies the force of gravity acting on these nerves in the upright position. (B) A Frankenhauser ganglion (sympathetic) supported by uterosacral ligaments (USL). Laxity (L) in USLs means they no longer can support the VPs, so they can be stimulated by “G.” Upward arrows indicate afferent impulses from the VP to the brain, and downward arrows indicate impulses from the brain to the end organ. Panel A by permission, Muctar S. Reproduced by permission of Pelviperineology.
In conclusion, if non-Hunner IC is proven to be the same or similar to PFS, it answers the dilemma of Ueda et al. [1], “Collectively assuming that HLD and non-Hunner IC/BPS is one disease entity has become a major impediment.” It also opens the door for future research to further investigate the hypotheses presented here for the cascade of pain and end-organ inflammatory reactions caused by the inability of loose USLs to support the VPs at T11–L2 and S2–4.
Footnotes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Ueda T, Hanno PM, Saito R, Meijlink JM, Yoshimura N. Current understanding and future perspectives of interstitial cystitis/bladder pain syndrome. Int Neurourol J. 2021;25:99–110. doi: 10.5213/inj.2142084.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scheffler KU, Oliver W, Hakenberg OW, Petros PE. Cure of interstitial cystitis and non-ulcerating Hunner’s Ulcer by cardinal/uterosacral ligament repair. Urol Int. 2021;105:920–3. doi: 10.1159/000515647. [DOI] [PubMed] [Google Scholar]
- 3.Petros PE, Ulmsten U. The posterior fornix syndrome: a multiple symptom complex of pelvic pain and abnormal urinary symptoms deriving from laxity in the posterior fornix. Scand J Urol Nephrol. 1993;27(153 Suppl):89–93. [Google Scholar]
- 4.Doggweiler R, Whitmore KE, Meijlink JM, Drake MJ, Frawley H, Nordling J, et al. A standard for terminology in chronic pelvic pain syndromes: a report from the chronic pelvic pain working group of the international continence society. Neurourol Urodyn. 2017;36:984–1008. doi: 10.1002/nau.23072. [DOI] [PubMed] [Google Scholar]
- 5.Petros PE, Richardson PA. Interstitial cystitis symptoms as defined are indistinguishable from posterior fornix syndrome symptoms cured by uterosacral ligament repair. Pelviperineology. 2021;40:145–53. [Google Scholar]
- 6.Wagenlehner F, Muller-Funogea I, Perletti G, Abendstein B, Goeschen K, Inoue H, et al. Vaginal apical prolapse repair using two different sling techniques improves chronic pelvic pain, urgency and nocturia: a multicentre study of 1420 patients. Pelviperineology. 2016;35:99–104. [Google Scholar]
- 7.Liedl B, Inoue H, Sekiguchi Y, Haverfield M, Richardson P, Yassourides A, et al. Is overactive bladder in the female surgically curable by ligament repair Cent. European J Urol. 2017;70:53–9. doi: 10.5173/ceju.2017.938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Inoue H, Kohata Y, Fukuda T, Monma M, Uzawa Y, Kubo Y, et al. Repair of damaged ligaments with tissue fixation system minisling is sufficient to cure major prolapse in all three compartments: 5-year data. J Obstet Gynaecol Res. 2017;43:1570–7. doi: 10.1111/jog.13413. [DOI] [PubMed] [Google Scholar]
- 9.Petros PE, Ulmsten UI. An integral theory of female urinary incontinence. Experimental and clinical considerations. Acta Obstet Gynecol Scand Suppl. 1990;153:7–31. doi: 10.1111/j.1600-0412.1990.tb08027.x. [DOI] [PubMed] [Google Scholar]
- 10.Kuhn T. The structure of scientific revolutions. 3rd ed. Chicago (IL): University of Chicago Press; 1996. [Google Scholar]
- 11.Petros PE, Ulmsten UI. An integral theory and its method for the diagnosis and management of female urinary incontinence. Scand J Urol Nephrol Suppl. 1993;153:1–93. [PubMed] [Google Scholar]
- 12.Martius H. Über einen häufigen gynäkologischen, Symptomkomplex. Arch Gynecol Obstet. 1938;166:332–5. [Google Scholar]
- 13.Petros PE. Severe chronic pelvic pain in women may be caused by ligamentous laxity in the posterior fornix of the vagina. Aust NZ J Obstet Gynaecol. 1996;36:351–4. doi: 10.1111/j.1479-828x.1996.tb02727.x. [DOI] [PubMed] [Google Scholar]
- 14.Liedl B, Inoue H, Sekiguchi Y, Gold D, Wagenlehner F, Haverfield M, et al. Update of the Integral Theory and system for management of pelvic floor dysfunction in females. Eur Urol Suppl. 2018;17:100–8. [Google Scholar]


