Abstract
Purpose
To explore the effect of intravesical electrical stimulation (IVES) on urinary adenosine triphosphate (ATP) and nitric oxide (NO) in rats with detrusor underactivity (DU) induced by bilateral pelvic nerve crush (bPNC), and to determine the underlying peripheral mechanism.
Methods
Twenty-four female Sprague-Dawley rats were equally divided into 3 groups: sham; bPNC; and IVES. Rats in the IVES group began to receive IVES treatment 10 days after bPNC (20 minutes per day for 14 consecutive days). After the 14th IVES, rat urine was collected and cystometry was performed. The serum creatinine, blood urea nitrogen, and urinary ATP and NO levels were measured, and a routine urinalysis was performed.
Results
The maximum cystometric capacity (MCC), maximum changes in bladder pressure during filling (∆FP), and postvoid residual urine (PVR) in the IVES group were significantly lower than the bPNC group, and the maximum changes in bladder pressure during voiding (∆VP) was significantly higher than the bPNC group. Compared with the sham group, the MCC, ∆FP and PVR were significantly increased, and the maximum voiding pressure (MVP) and ∆VP were significantly decreased in the bPNC group. After bPNC, urinary ATP was significantly decreased, and urinary NO was significantly increased. In IVES-treated rats, urinary ATP was significantly higher than the bPNC group, and NO was significantly lower than the bPNC group. In addition, the ATP-to-NO ratio of the rats in the bPNC group was significantly lower than the sham and IVES groups. Correlation analysis showed that the ATP and NO were not correlated with the MCC, ∆FP, MVP, ∆VP, and PVR.
Conclusions
Promoting the release of urothelial ATP and inhibiting the release of urothelial NO may be one of the peripheral mechanisms underlying IVES in the treatment of DU. Specifically, IVES may shift the balance between excitation and inhibition toward excitation.
Keywords: Urinary Bladder, Underactive; Intravesical electrical stimulation; Bilateral pelvic nerve crush; Adenosine triphosphate; Nitric oxide
• HIGHLIGHTS
- Explore the possible mechanism of intravesical electrical stimulation in the treatment of detrusor underactivity.
INTRODUCTION
Detrusor underactivity (DU) is defined by the International Continence Society as “detrusor contraction of inadequate strength and/or duration, resulting in prolonged bladder emptying and/or a failure to achieve complete bladder emptying in the absence of urethral obstruction” [1]. The prevalence of DU is 12%–45% in women and 9%–48% in men [2]. Multiple etiologies have been proposed to explain the mechanisms underlying DU, including aging, bladder outlet obstruction, diabetes, and iatrogenic nerve injury. Among the putative etiologies, iatrogenic causes include iatrogenic nerve injury during pelvic surgery, such as bilateral pelvic nerve injury during radical hysterectomy, thus resulting in damage to the nerve plexus innervating the bladder, and leading to bladder degeneration, denervation, and secondary structural changes [3].
Treatment options for DU are limited. The efficacy and safety of drug therapy, such as M receptor agonists and acetylcholinesterase inhibitors, are controversial [4]. Surgical treatments, such as latissimus dorsi detrusorplasty and transurethral cyst neck incision, are not options due to the associated trauma and complications [5]. Intravesical electrical stimulation (IVES) involves insertion of a urinary catheter with stimulating electrodes into the bladder, and use of normal saline as a medium to stimulate the detrusor via the surviving afferent nerve connection between the detrusor and the center, thus inducing the bladder to produce a feeling of urination and increasing the output of nerve impulses, promoting urination, or improving the ability to control urination [6]. The technique involves a stimulation electrode (cathode) that is inserted into the catheter and into the bladder together through the urethra, with the other end of the electrode connected to the stimulator. Normal saline (0.9%) is used as a conduction medium in the bladder. The anode electrode is attached to an area of the skin that feels reserved, usually on the lower abdomen.
In 1975, Katona and Berényi [7] began to promote the application of IVES in the treatment of neurogenic voiding dysfunction. Several investigators worldwide have demonstrated the effectiveness of IVES in DU patients [6,8,9]; however, the mechanism underlying IVES is not fully understood. Experimental studies have shown that IVES involves direct activation of Aδ afferent fibers from low-threshold bladder mechanoreceptors, which include the sensory system responsible for initiating and maintaining the voiding response. It has also been suggested that the IVES-induced voiding response is due to enhanced excitatory synaptic transmission in the central voiding response pathway [10]. Studies have shown that activation of the bladder afferent pathway is accompanied by the release of sensory neurotransmitters from the urothelium, such as adenosine triphosphate (ATP) or nitric oxide (NO) [11]. In animal studies, urothelial ATP and epithelial NO synthase levels are also altered in under- and overactive bladders (OABs); specifically, the urinary ATP:NO ratio is decreased in underactive bladder (UAB) and increased in overactive bladder (OAB) [12]. The correlation between IVES and urinary ATP and NO levels has not been reported to date. Therefore, we determined the effect of IVES on urinary ATP and NO levels in rats with DU to elucidate the mechanism underlying IVES.
MATERIALS AND METHODS
Animal Model
Twenty-four female Sprague-Dawley (SD) rats (235–275 g, 8 w–10 w), were used according to the experimental protocol approved by the Capital Medical University Animal Care and Use Committee (AEEI-2021-171). Rats were housed in plastic cages with soft bedding and free access to food and water under a 12/12 hours reversed light-dark cycle. Under isoflurane anesthesia, bilateral preganglionic pelvic nerves were exposed by a midline laparotomy. As previously described, bilateral pelvic nerve crush (bPNC) was induced by applying a WA3040 forceps (Jinzhong, Shanghai, China) 1×15s to the nerve [13]. Ampicillin sodium (100 mg/kg) was administered subcutaneously once daily for 5 days after the operation to prevent infection. While the rats were awake, gently press the abdomen manually, and assist the rats to empty the bladder 3 times a day (7:00, 15:00, and 23:00).
The experimental rats were randomly divided into 3 groups: (1) sham (n=8), sham-operated with a lower abdominal incision, bilateral pelvic nerve identification, and no nerve crush; (2) bPNC (n =8); and (3) IVES (n =8): bPNC, followed by IVES treatment.
Intravesical Electrical Stimulation
IVES was started 10 days after the bPNC as previously described [14]. Each rat in the IVES group were stimulated for 20 minutes per day for 14 days. The experimental procedure for IVES refers to the previous experiments [15,16]. In brief, under isoflurane anesthesia, a specially designed PE-50 catheter (0.58 inside diameter [i.d.] and 0.96 mm outside diameter [o.d.]) with a monopolar platinum wire electrode (0.2 mm o.d.) inside that can be used for both IVES and cystometry was inserted into the bladder through the urethra with a length of 2.5–3 cm. The catheter electrode was used as a cathode and a patch electrode under the abdominal skin at the level of the bladder as the anode (Fig. 1A). Before IVES, the bladder was filled with 0.2 mL of saline. IVES was administered with a Power-lab system (AD instruments, Canberra, Australia) giving unipolar square wave pulses of 0.2-msec duration, with a frequency of 20 Hz and an intensity of 7–11 mA [15,16]. At this pulse duration and intensity, only myelinated Aδ afferents were activated by the IVES procedure, and there was no direct motor response from the bladder, suggesting that stimulation was well below the threshold for activation of postmyelinated motor fibers [10]. Under isoflurane anesthesia, rats in the sham and bPNC groups received intravesical catheter and abdominal patch electrodes for 20 minutes per day, but without stimulation, for 14 days. After each session, the probe was washed with sterile soap and water and immersed in a disinfectant container. All rats were placed supine on an electric heating pad that was maintained at a temperature of 37°C.
Fig. 1.
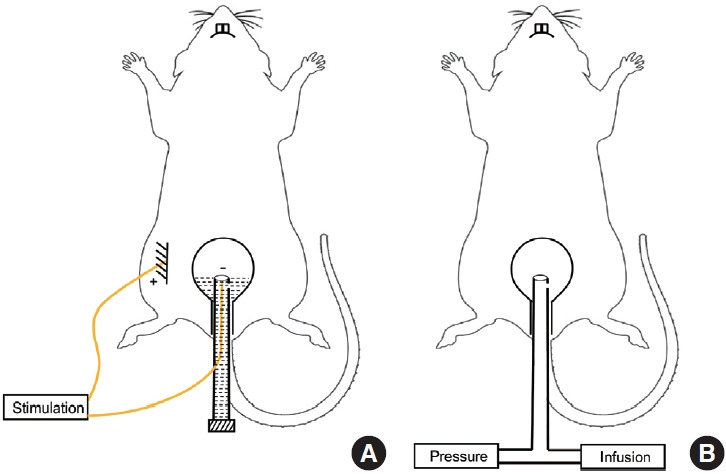
Schematic diagram of IVES (A) and cystometry (B). IVES, intravesical electrical stimulation.
Urine Collection
After the 14th IVES session, a 4-hour urine specimen was collected from each rat in a clean metabolic cage, and 0.5 mL of urine was stored in a -80°C refrigerator for routine urinalysis and urinary ATP and NO assays.
Cystometry
After urine collection, all 24 rats underwent a cystometrogram (CMG) using AcqKnowledge 4.4 software (Biopac Systems, Goleta, CA, USA). Under urethane (1.2 g/kg subcutaneously) anesthesia, the specially designed catheter was inserted into the bladder through the urethra (length=2.5–3 cm; Fig. 1B). The catheter was connected via a 3-way stopcock to a microinfusion pump (Stoelting Co., Wood Dale, IL, USA) for a saline infusion and a pressure transducer (MP150; Biopac Systems Inc., Goleta, CA, USA) to record the bladder pressure. Room temperature saline was infused into bladder at a rate of 0.08 mL/min for the CMG and 3 micturition cycles were recorded.
The following CMG parameters were evaluated: (1) maximum cystometric capacity (MCC), perfusion volume before urination; (2) maximum changes in bladder pressure during filling (∆FP), peak bladder pressure minus basal pressure during filling; (3) bladder compliance (BC), calculated by the volume change ∆V) divided by the change in bladder pressure (∆P, the threshold pressure - basal pressure) during the filling period (∆V/∆P); (4) maximum voiding pressure (MVP), maximum bladder pressure during voiding; (5) maximum changes in bladder pressure during voiding (∆VP), the peak pressure during voiding minus the end-fill pressure; (6) postvoid residual urine (PVR), the amount drained from the catheter after each urination; and (7) voided volume (VV), the value of MCC minus PVR. All parameters were measured 3 times, and the average value was adopted.
Assay of Serum Creatinine and Blood Urea Nitrogen
After CMG, 2 mL of blood was drawn from the heart of each rat, placed in an anticoagulant tube for 2 hours at room temperature, centrifuged at 3,000 r/min for 15 minutes, and 100 μL of serum was obtained and stored at -80°C. Creatinine (Cr) and blood urea nitrogen (BUN) levels were detected using an automatic biochemical analyzer (Leidu, Shenzhen, China).
Routine Urinalysis and Urinary ATP and NO Assays
The following urine measurements were performed using a urine analyzer (Urit, Guangxi, China): white blood cell (WBC) count; blood (BLD); protein (PRO); glucose (GLU); pH; specific gravity (SG); urobilinogen (URO); bilirubin (BIL); ketone bodies (KET).
The urinary ATP level was measured using a standard commercial kit (Jiancheng Bioengineering Institute, Nanjing, China) with a spectrophotometer (Infinite M200PRO; Tecan, Shanghai, China). Luciferase was added to the wells, followed by an equal volume of the sample. The highest luminescence value was recorded for each sample. After stabilizing the lowest luminescence reading, standard additions were made to prevent interference with the assay results due to any urinary compounds.
The NO level was determined using an antioxidant analyzer (Jiancheng Bioengineering Institute, Nanjing, China) and a Unico7200 spectrophotometer (Unico, Shanghai, China). At the beginning of each analysis, a nitrate standard curve was constructed, then 20 mL of the solution was injected into the reaction chamber and the peak areas were compared to the standard curve.
Statistical Analysis
IBM SPSS Statistics ver. 25.0 (IBM Co., Armonk, NY, USA) was used for statistical analysis. GraphPad Prism ver. 9 (GraphPad Software Inc., La Jolla, CA, USA) was used for all the graphics. Experimental data are presented as the mean±standard error of the mean. For statistical analysis we used 1-way analysis of variance, followed by a Bonferroni multiple comparison posttest. We analyzed the correlations between urinary ATP and NO levels and urodynamic parameters using Spearman correlation analysis. P<0.05 was considered a statistically significant difference.
RESULTS
Body Weight
After the 14th IVES session, there was no significant difference in body weight among the sham, bPNC, and IVES groups (250.00±10.00 g, 250.60±12.66 g, and 249.40±13.21 g, respectively, P=0.979) (Fig. 2).
Fig. 2.
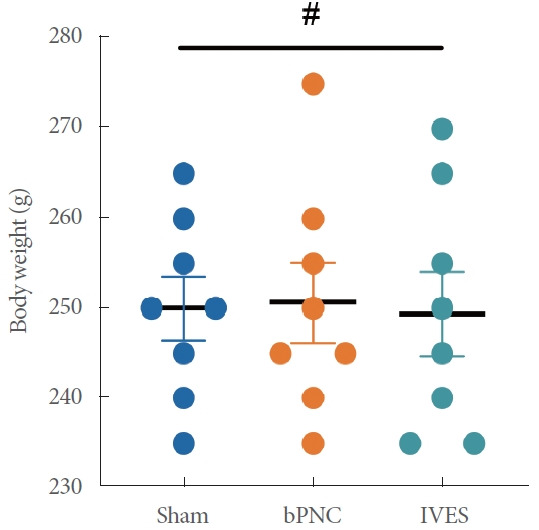
Comparison of body weight among sham, bPNC, and IVES groups. The data are presented as mean±standard error of the mean. IVES, intravesical electrical stimulation. #P>0.05. bPNC, bilateral pelvic nerve crush.
Cystometrograms
Fig. 3A–C show representative traces of CMG in sham, bPNC, and IVES groups. During CMG, bPNC resulted in a significant increase in MCC, ∆FP and PVR, and a significant decrease in MVP and ∆VP compared with the sham group (Table 1; Fig. 3D, E, G–I). However, in IVES-treated rats, MCC, ∆FP, and PVR were significantly decreased, and ∆VP were significantly increased compared with the bPNC group (Table 1; Fig. 3D, E, H, I). MCC was significantly increased in the IVES group compared with the sham group, while MVP and ∆VP were significantly decreased (Table 1; Fig. 3D, G, H). There was no significant difference in BC and VV among the 3 groups of rats (Table 1, Fig. 3F).
Fig. 3.
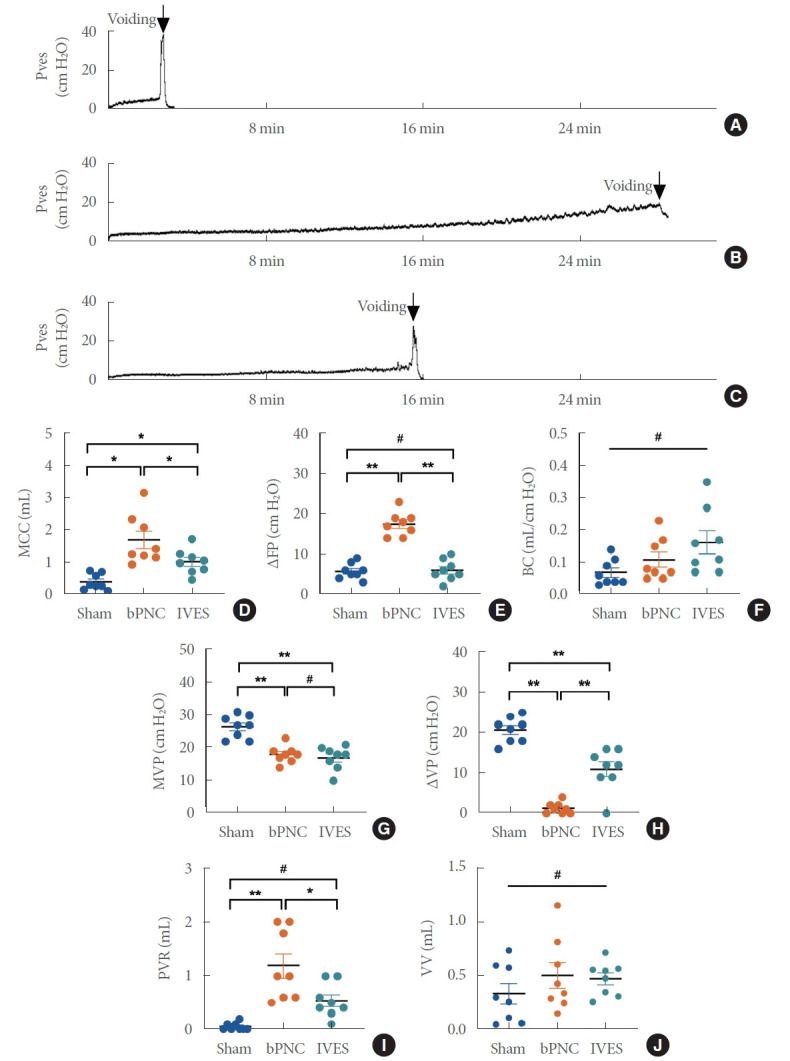
Cystometrograms. Sham group (A), bPNC group (B), IVES group (C), quantitative analysis of cystometric (D-J) parameters. The data are presented as mean±standard error of the mean. Pves, intravesical pressure; MCC, maximum cystometric capacity; ΔFP, maximum changes in bladder pressure during filling; BC, bladder compliance; MVP, maximum voiding pressure; ΔVP, maximum changes in bladder pressure during voiding; PVR, postvoid residual urine; VV, voided volume; bPNC, bilateral pelvic nerve crush; IVES, intravesical electrical stimulation. *P<0.05, **P<0.001, #P>0.05.
Table 1.
Comparison of cystometric parameters among sham, bPNC, and IVES groups
| Parameter | Sham | bPNC | IVES |
|---|---|---|---|
| MCC (mL) | 0.39 ± 0.09 | 1.70 ± 0.27a),* | 1.01 ± 0.14b),c),* |
| ∆FP (cm H2O) | 5.75 ± 0.70 | 17.50 ± 1.05 a),** | 6.00 ± 0.93b),** |
| BC (mL/cm H2O) | 0.07 ± 0.01 | 0.11 ± 0.02 | 0.16 ± 0.03 |
| MVP (cm H2O) | 26.50 ± 1.24 | 18.00 ± 0.93 a),** | 17.00 ± 1.27c),** |
| ∆VP (cm H2O) | 20.75 ± 1.11 | 0.50 ± 0.50 a),** | 11.00 ± 1.84 b),c),** |
| PVR (mL) | 0.05 ± 0.03 | 1.19 ± 0.23 a),** | 0.54 ± 0.11b),* |
| VV (mL) | 0.34 ± 0.10 | 0.51 ± 0.12 | 0.48 ± 0.06 |
Values are presented as mean±standard error of the mean.
bPNC, bilateral pelvic nerve crush; IVES, intravesical electrical stimulation; MCC, maximum cystometric capacity; ΔFP, maximum changes in bladder pressure during filling; BC, bladder compliance; MVP, maximum voiding pressure; ΔVP, maximum changes in bladder pressure during voiding; PVR, postvoid residual urine; VV, voided volume.
P<0.05,
P<0.001.
For bPNC group vs. sham group.
For IVES group vs. bPNC group.
For IVES group vs. sham group.
Serum Cr and BUN Levels
The serum Cr and BUN levels were 32.80±2.99 μmol/L and 21.66±1.39 mg/dL in the sham group, 30.09±3.99 μmol/L and 24.94±2.11 mg/dL in the bPNC group, and 27.57±3.91 μmol/ L and 23.88±0.23 mg/dL in the IVES group. No significant differences in serum Cr and BUN levels were detected among the 3 groups (Fig. 4).
Fig. 4.
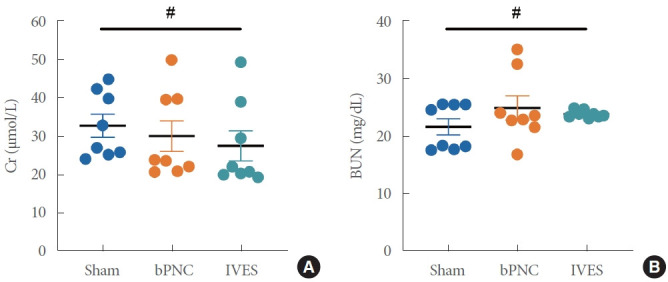
The level of Cr (A) and BUN (B). The data are presented as mean±standard error of the mean. Cr, serum creatinine; BUN, blood urea nitrogen; bPNC, bilateral pelvic nerve crush; IVES, intravesical electrical stimulation. #P>0.05.
Routine Urinalysis
No significant difference existed in the routine urinalyses among the 3 groups of rats (Table 2).
Table 2.
Routine urinalysis results of 3 groups of rats
| Item | Sham | bPNC | IVES | P-value |
|---|---|---|---|---|
| WBC (Cell/μL) | 0 | 0 | 0 | - |
| BLD (Cell/μL) | 0 | 0 | 0 | - |
| PRO (g/L) | 0 | 0 | 0 | - |
| Glu (mmol/L) | 0 | 0 | 0 | - |
| pH | 7.000 ± 0.232 | 6.938 ± 0.175 | 6.938 ± 0.113 | 0.961 |
| SG | 1.022 ± 0.001 | 1.024 ± 0.001 | 1.025 ± 0.001 | 0.259 |
| URO | 0 | 0 | 0 | - |
| BIL (μmol/L) | 0 | 0 | 0 | - |
| KET (mmol/L) | 0 | 0 | 0 | - |
Values are presented as mean±standard error of the mean.
bPNC, bilateral pelvic nerve crush; IVES, intravesical electrical stimulation; WBC, white blood cell; BLD, blood; PRO, protein; Glu, glucose; SG, specific gravity; URO, urbilinogen; BIL, bilirubin; KET, ketonebody.
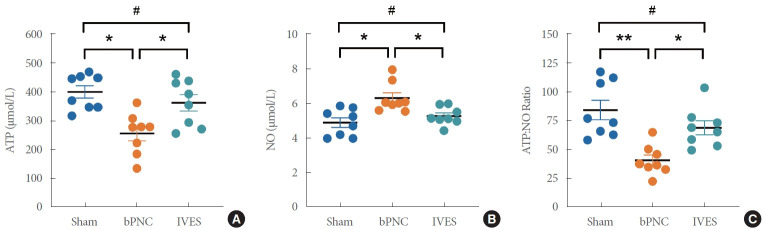
Urinary NO, ATP, and ATP:NO Ratio
Fig. 5 shows the levels of ATP, NO and ATP:NO ratio in the urine of 3 groups of rats. For ATP, bPNC group were significantly lower than sham group (257.40 ±25.45 μmol/L vs. 401.00 ±21.30 μmol/L), while IVES group were significantly higher than bPNC group (363.60±28.42 μmol/L vs. 257.40± 25.45 μmol/L; Fig. 5A). On the contrary, the NO of bPNC group was significantly higher than that of sham group (6.33±0.30 μmol/L vs. 4.91±0.28 μmol/L), while the NO of IVES group was significantly lower than that of bPNC group (5.29±0.18 μmol/L vs. 6.33±0.30 μmol/L; Fig. 5B). We also compared the ratio of ATP:NO, and the bPNC group was significantly lower than the sham group and the IVES group, respectively (41.09±4.56 vs. 84.59±8.48; 41.09±4.56 vs. 69.17±6.03, Fig. 5C). Correlation of Urinary ATP and NO Levels With Urodynamic
Fig. 5.
Comparison of urinary ATP, NO, and ATP:NO ratio levels among sham, bPNC, and IVES groups. The data are presented as mean±standard error of the mean. ATP, adenosine triphosphate; NO, nitric oxide; bPNC, bilateral pelvic nerve crush; IVES, intravesical electrical stimulation. *P<0.05, **P<0.001, #P>0.05.
Parameters
There was no statistically significant correlation between urinary ATP or NO levels with urodynamic parameters such as MCC, ∆FP, MVP, ∆VP, and PVR (Table 3).
Table 3.
Correlation of urinary ATP and NO levels with urodynamic parameters
| Parameter | ATP |
NO |
||
|---|---|---|---|---|
| r | P-value | r | P-value | |
| MCC (mL) | -0.421 | 0.32 | 0.002 | 0.996 |
| ∆FP (cm H2O) | -1.156 | 0.099 | 0.788 | 0.246 |
| MVP (cm H2O) | 0.909 | 0.171 | -0.752 | 0.247 |
| ∆VP (cm H2O) | -1.648 | 0.119 | 0.993 | 0.331 |
| PVR (mL) | -0.344 | 0.428 | 0.6 | 0.169 |
ATP, adenosine triphosphate; NO, nitric oxide; MCC, maximum cystometric capacity; ΔFP, maximum changes in bladder pressure during filling; MVP, maximum voiding pressure; ΔVP, maximum changes in bladder pressure during voiding; PVR, postvoid residual urine.
DISCUSSION
The major findings of this study are as follows: (1) bPNC in rats successfully created a DU model; (2) bPNC-induced rat urothelial ATP release was significantly decreased and urothelial NO release was significantly increased; and (3) IVES treatment had a significant effect on the normalization of the changes in urinary tract epithelial transmitter release induced by bPNC in rats (i.e., NO [decrease] and ATP [increase]).
DU has always been a challenging medical condition because DU has no effective treatment other than intermittent catheterization. However, intermittent catheterization is not a true cure, and noninvasive electrical regulation is undoubtedly a better choice.
We created a DU model of peripheral nerve injury by squeezing the bilateral pelvic nerves. Previous studies have shown that 10 days after bPNC, rats already exhibit DU characteristics [14], and 9 weeks after bPNC, rats still show DU characteristics [17]. In this study the functional characteristics of DU, such as increased MCC and PVR and decreased MVP and ∆VP, were observed 24 days after bPNC. The pelvic nerve transmits afferent and efferent signals between the lower urinary tract and the central nervous system [13]. Therefore, compression of the pelvic nerve can lead to mixed injuries. To investigate the possible mechanism underlying IVES for the treatment of DU, we chose a model of mild crush injury (1 ×15 seconds) of the pelvic nerve and maintained the integrity of the hypogastric and pudendal nerves, thus ensuring the residual neural activity between the lower urinary tract and the central nervous system.
Detrusor contraction is the end result of the interaction of multiple afferent stimuli from the urothelium and suburothelium. In addition to acetylcholine and norepinephrine, many other mediators, such as ATP and NO, also affect detrusor contractile function by affecting afferent signals from the bladder [18,19].
Studies have confirmed that bladder epithelial cells release ATP during bladder filling, and ATP acts on P2X receptors (mainly P2X3) on the submucosal sensory plexus to participate in bladder sensation and the voiding reflex [20,21]. ATP binds to the ionotropic P2X receptor, a non-specific cation channel, which initiates cation influx and membrane depolarization. Subsequent activation of L-type Ca2+ channels increase intracellular Ca2+ and increases Ca2+-induced Ca2+release form intracellular stores to initiate contraction [22]. It has also been suggested that urothelial ATP may induce detrusor contraction by increasing pacemaker activity in lamina propria myofibroblasts [23]. In this study the urinary ATP of rats with DU in the bPNC group was significantly decreased; however, the MCC, ∆FP, and PVR were significantly decreased, the ∆VP were significantly increased, and urinary ATP was also significantly increased in rats treated with IVES compared to rats in the bPNC group. Dewulf et al. [17] reported that the bladder contractile function of rats did not improve 9 weeks after bPNC. Similarly, a study by Payne et al. [24] on pelvic motor and sensory autonomic axon regeneration showed no additional recovery between 4 and 12 weeks after injury. Thus, the recovery of bladder function of rats in the IVES group was mainly due to the intervention with IVES. Kontani and Hayashi [25] recorded bladder function in rats with DU symptoms after bilateral pelvic nerve transection, which resulted in increased bladder pressure by stimulating the hypogastric nerve. The hypogastric nerve of the rats in this experiment remained intact, so the above results suggest that the hypogastric nerve may be involved in IVES-induced bladder contraction. Following nerve injury, neurons switch their gene expression from an excitatory phenotype to a regenerative phenotype, resulting in reduced neurofilament and neurotransmitter production and increased brain-derived neurotrophic factor (BDNF) [26]. Al-Majed et al. [27] reported that nerve electrical stimulation can up-regulate BDNF and its receptor tyrosine kinase B (TrkB) in both sensory and motoneurons, thereby upregulating regeneration-related genes. It has also been reported that nerve electrical stimulation can promote nerve sprouting, nerve regeneration, target organ reinnervation, and functional recovery after nerve injury by enhancing the intrinsic nerve regeneration processes [28]. It can be speculated that IVES can promote the binding of BDNF and TrkB receptors by upregulating BDNF in nerve cells, thereby upregulating regeneration-related proteins, enabling damaged nerves to sprout and regenerate, thereby promoting the reinnervation of pelvic nerves to the detrusor muscle and restoring bladder function. In response to electrical stimulation, ATP-induced activation may involve depolarization and increased Ca2+ influx. IVES may induce upregulation of purinergic receptors to improve bladder function. More precise reasons warrant further research.
NO is an inhibitory neurotransmitter that acts by increasing the intracellular second messenger, cGMP [29]. Aizawa et al. [30] determined the effect of NO on sensory afferent signals by directly recording the electrical activity of afferent nerves in the rat bladder. Aizawa et al. [30] reported that the intravenous administration of L-arginine, a NO substrate, decreased mechanosensitive afferent activity of Aδ and C fibers during saline filling of the bladder, and intravesical instillation of a NO synthase inhibitor (N(ω)nitro-L-arginine methyl ester hydrochloride [L-NAME]) increased fiber-like afferent activity, and intravenous L-arginine inhibited the afferent activity of these 2 fibers, suggesting that the NO-cGMP signaling pathway is involved in the inhibition of bladder mechanosensitivity and hypersensitivity response inhibition. Munoz et al. [12] showed that urinary NO release is significantly enhanced in artificially induced UAB rats. We also found that the urinary NO levels were significantly increased in the bPNC group with DU symptoms compared with the sham group. It has been reported that IVES induces bladder contractions by exciting low-threshold mechanical Aδ afferent fibers in the bladder wall [15]. The above finding indicated that improvement of DU symptoms in rats after IVES treatment may be attributed to IVES counteracting the inhibitory effect of NO on the neural activity of Aδ afferent fibers. Payne et al. [24] found that the regeneration capacity of sensory nerves after splanchnic nerve injury was significantly higher than that of motor nerves, and the promotion of nerve regeneration by nerve electrical stimulation could also accelerate the recovery of bladder sensory nerves [28], thereby indirectly altering NO levels. NO is produced constitutively in tissues by neuronal and endothelial NO synthase (NOS) enzymes (e.g., neuronal NOS and endothelial NOS, respectively), but also by inducible NOS (e.g., inducible NOS) under specific conditions, such as inflammation [31], via non-vesicular mechanisms release [32]. Therefore, the NO level should not be directly affected by IVES treatment; however, IVES can indirectly affect NO levels via effects on NOS activity. In the future, we will investigate whether IVES treatment induces changes in NOS activity that might account for the differences in NO levels observed in this study. In bPNC rats treated with IVES, IVES significantly restored the balance between the levels of excitatory and inhibitory transmitters released from the urothelium. After IVES treatment, the balance between excitation and inhibition is likely to shift toward excitation.
Serum Cr and BUN are 2 important indicators of renal function. Cr is a metabolite of muscle in the body and BUN is a metabolite of protein in the body. There were no significant differences in the serum Cr and BUN levels among the 3 groups of rats in this study. Under certain pathologic conditions, such as bladder infection or inflammation, the bladder urothelium releases more ATP or NO into the bladder, resulting in elevated urinary ATP or NO concentrations [33]. There were no significant differences in the WBC count, BLD, PRO, GLU, pH, SG, URO, BIL, and KET in the routine urinalyses of the 3 groups of rats in this study, and the number of WBCs was 0. The above data show that IVES therapy did not cause upper urinary tract injury and no urinary tract infections, and thus was safe.
Studies have shown that the urinary ATP:NO ratio is representative of the overall sensory transmission in the bladder, and the ATP:NO ratio is higher in OAB and lower in UAB [12]. Therefore, the ratio of ATP:NO can be used as a measure of bladder dysfunction. In this study, we calculated the ratio of ATP:NO in the urine of the 3 groups of rats and found that the ratio of ATP:NO in the bPNC group was significantly lower than the sham and IVES groups. This ratio may be of great clinical significance, as follows: (1) the ratio may help in the diagnosis of UAB with uncertain urodynamic findings; (2) the ratio may be used as an evaluation index of bladder sensation and provide evidence for the changes in bladder sensation in UAB treated with IVES; and (3) based on this study, we provided preliminary evidence for the role of ATP and NO in peripheral neurotransmission in IVES-treated DU.
The release of ATP and NO into the urine suggests that the urothelium is the source of both transmitters, and that bladder urine can be used as a source for monitoring ATP and NO release under physiologic or pathologic conditions. Daneshgari et al. [34] showed that the frequency of bladder contractions was positively correlated with urinary ATP and negatively correlated with urinary NO. Cho et al. [35] have shown that ATP levels from mucosal bladder specimens positively correlated with bladder contractility index and detrusor pressure at maximum flow in patients with UABs. In the present study we did not detect a significant correlation between urinary ATP and NO and urodynamic parameters (MCC, ∆FP, MVP, ∆VP, and PVR). The possible reasons for the inconsistency of this result with those of other studies are differences in urodynamic parameters, and different sources of ATP and NO collection. According to the significant differences in urodynamic parameters between groups of rats in this study, we think that the difference in CMGs (MCC, ∆FP, ∆VP, and PVR) of bPNC rats and IVES rats in IVES is the motor effect. The effect of IVES on bladder sensory transmission still needs our further study to verify.
In this study we used a rat model of pelvic nerve injury that mimics pelvic surgery-induced DU. Because the etiology of DU is often multifactorial, our findings in this simplified animal model may not be applicable in complex clinical settings. We only treated bPNC rats with IVES for 14 days, however, the long-term mechanism of action of IVES remains to be determined. In addition, this study only tentatively explored the peripheral mechanism underlying IVES in the treatment of DU by urinalysis, and because more in-depth peripheral and central mechanisms of action are also very important, we will conduct corollary studies.
In conclusion, promoting the release of urothelial ATP and inhibiting the release of urothelial NO may be one of the potential peripheral mechanisms underlying IVES in the treatment of DU. The effects of IVES on bladder function are associated with changes in the balance between excitatory and inhibitory transmitter levels in peripheral nerve activity.
Footnotes
Funding/Grant Support
This study was supported by the National Key Research and Development Program (No. 2018YFC2002203).
Research Ethics
The animal study was reviewed and approved by the Capital Medical University Animal Care and Use Committee (AEEI- 2021-171).
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTION STATEMENT
·Conceptualization: HD, LL
·Data curation: HD, XW, ZZ
·Formal analysis: HD
·Funding acquisition: HD
·Methodology: HD, LL, XL
·Project administration: HD
·Visualization: HD, QL
·Writing - original draft: HD
·Writing - review & editing: HD, LL
REFERENCES
- 1.Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002;21:167–78. doi: 10.1002/nau.10052. [DOI] [PubMed] [Google Scholar]
- 2.Osman NI, Chapple CR. Contemporary concepts in the aetiopathogenesis of detrusor underactivity. Nat Rev Urol. 2014;11:639–48. doi: 10.1038/nrurol.2014.286. [DOI] [PubMed] [Google Scholar]
- 3.Giannantoni A, Mearini E, Zucchi A, Costantini E, Mearini L, Bini V, et al. Bladder and urethral sphincter function after radical retropubic prostatectomy: a prospective long-term study. Eur Urol. 2008;54:657–64. doi: 10.1016/j.eururo.2007.10.054. [DOI] [PubMed] [Google Scholar]
- 4.Miyazato M, Yoshimura N, Chancellor MB. The other bladder syndrome: underactive bladder. Rev Urol. 2013;15:11–22. [PMC free article] [PubMed] [Google Scholar]
- 5.Moreno-Palacios J, Maldonado-Alcaraz E, Montoya-Martínez G, Serrano-Brambila E. Outcomes and complications of sphincterotomy with bladder neck incision in neurologically healthy male patients with voiding dysfunction. Arch Esp Urol. 2012;65:244–50. [PubMed] [Google Scholar]
- 6.Gladh G, Mattsson S, Lindström S. Intravesical electrical stimulation in the treatment of micturition dysfunction in children. Neurourol Urodyn. 2003;22:233–42. doi: 10.1002/nau.10078. [DOI] [PubMed] [Google Scholar]
- 7.Katona F, Berényi M. Intravesical transurethral electrotherapy in meningomyelocele patients. Acta Paediatr Acad Sci Hung. 1975;16:363–74. [PubMed] [Google Scholar]
- 8.Hagerty JA, Richards I, Kaplan WE. Intravesical electrotherapy for neurogenic bladder dysfunction: a 22-year experience. J Urol. 2007;178(4 Pt 2):1680–3. doi: 10.1016/j.juro.2007.03.188. discussion 1683. [DOI] [PubMed] [Google Scholar]
- 9.Deng H, Liao L, Wu J, Chen G, Li X, Wang Z, et al. Clinical efficacy of intravesical electrical stimulation on detrusor underactivity: 8 Years of experience from a single center. Medicine (Baltimore) 2017;96:e8020. doi: 10.1097/MD.0000000000008020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jiang CH. Modulation of the micturition reflex pathway by intravesical electrical stimulation: an experimental study in the rat. Neurourol Urodyn. 1998;17:543–53. doi: 10.1002/(sici)1520-6777(1998)17:5<543::aid-nau11>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 11.Birder LA. Urinary bladder urothelium: molecular sensors of chemical/thermal/mechanical stimuli. Vascul Pharmacol. 2006;45:221–6. doi: 10.1016/j.vph.2005.08.027. [DOI] [PubMed] [Google Scholar]
- 12.Munoz A, Smith CP, Boone TB, Somogyi GT. Overactive and underactive bladder dysfunction is reflected by alterations in urothelial ATP and NO release. Neurochem Int. 2011;58:295–300. doi: 10.1016/j.neuint.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deruyver Y, Weyne E, Dewulf K, Rietjens R, Pinto S, Van Ranst N, et al. Intravesical activation of the cation channel TRPV4 improves bladder function in a rat model for detrusor underactivity. Eur Urol. 2018;74:336–45. doi: 10.1016/j.eururo.2018.05.020. [DOI] [PubMed] [Google Scholar]
- 14.Takaoka EI, Kurobe M, Okada H, Takai S, Suzuki T, Shimizu N, et al. Effect of TRPV4 activation in a rat model of detrusor underactivity induced by bilateral pelvic nerve crush injury. Neurourol Urodyn. 2018;37:2527–34. doi: 10.1002/nau.23790. [DOI] [PubMed] [Google Scholar]
- 15.Ebner A, Jiang C, Lindström S. Intravesical electrical stimulation--an experimental analysis of the mechanism of action. J Urol. 1992;148:920–4. doi: 10.1016/s0022-5347(17)36778-2. [DOI] [PubMed] [Google Scholar]
- 16.Jiang CH, Lindström S. Intravesical electrical stimulation induces a prolonged decrease in micturition threshold volume in the rat. J Urol. 1996;155:1477–81. [PubMed] [Google Scholar]
- 17.Dewulf K, Weyne E, Gevaert T, Deruyver Y, Voets T, Ridder D, et al. Functional and molecular characterisation of the bilateral pelvic nerve crush injury rat model for neurogenic detrusor underactivity. BJU Int. 2019;123(5A):E86–96. doi: 10.1111/bju.14649. [DOI] [PubMed] [Google Scholar]
- 18.Kumar V, Chapple CC, Chess-Williams R. Characteristics of adenosine triphosphate [corrected] release from porcine and human normal bladder. J Urol. 2004;172:744–7. doi: 10.1097/01.ju.0000131244.67160.f4abstract. [DOI] [PubMed] [Google Scholar]
- 19.Harvey RA, Skennerton DE, Newgreen D, Fry CH. The contractile potency of adenosine triphosphate and ecto-adenosine triphosphatase activity in guinea pig detrusor and detrusor from patients with a stable, unstable or obstructed bladder. J Urol. 2002;168:1235–9. doi: 10.1016/S0022-5347(05)64632-0. [DOI] [PubMed] [Google Scholar]
- 20.Vlaskovska M, Kasakov L, Rong W, Bodin P, Bardini M, Cockayne DA, et al. P2X3 knock-out mice reveal a major sensory role for urothelially released ATP. J Neurosci. 2001;21:5670–7. doi: 10.1523/JNEUROSCI.21-15-05670.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cockayne DA, Dunn PM, Zhong Y, Rong W, Hamilton SG, Knight GE, et al. P2X2 knockout mice and P2X2/P2X3 double knockout mice reveal a role for the P2X2 receptor subunit in mediating multiple sensory effects of ATP. J Physiol. 2005;567(Pt 2):621–39. doi: 10.1113/jphysiol.2005.088435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andersson KE, Arner A. Urinary bladder contraction and relaxation: physiology and pathophysiology. Physiol Rev. 2004;84:935–86. doi: 10.1152/physrev.00038.2003. [DOI] [PubMed] [Google Scholar]
- 23.Ikeda Y, Fry C, Hayashi F, Stolz D, Griffiths D, Kanai A. Role of gap junctions in spontaneous activity of the rat bladder. Am J Physiol Renal Physiol. 2007;293:F1018–25. doi: 10.1152/ajprenal.00183.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Payne SC, Belleville PJ, Keast JR. Regeneration of sensory but not motor axons following visceral nerve injury. Exp Neurol. 2015;266:127–42. doi: 10.1016/j.expneurol.2015.02.026. [DOI] [PubMed] [Google Scholar]
- 25.Kontani H, Hayashi K. Urinary bladder response to hypogastric nerve stimulation after bilateral resection of the pelvic nerve or spinal cord injury in rats. Int J Urol. 1997;4:394–400. doi: 10.1111/j.1442-2042.1997.tb00214.x. [DOI] [PubMed] [Google Scholar]
- 26.Gordon T. In: Nerves & nerve injuries. Tubbs RS, Rizk E, Shoja MM, Loukas M, Barbaro N, Spinner RJ, editors. Amsterdam: Elsevier; 2015. The biology, limits, and promotion of peripheral nerve regeneration in rats and humans; pp. 993–1019. [Google Scholar]
- 27.Al-Majed AA, Tam SL, Gordon T. Electrical stimulation accelerates and enhances expression of regeneration-associated genes in regenerating rat femoral motoneurons. Cell Mol Neurobiol. 2004;24:379–402. doi: 10.1023/B:CEMN.0000022770.66463.f7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Balog BM, Deng K, Labhasetwar V, Jones KJ, Damaser MS. Electrical stimulation for neuroregeneration in urology: a new therapeutic paradigm. Curr Opin Urol. 2019;29:458–65. doi: 10.1097/MOU.0000000000000632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rahnama’i MS, Ückert S, Hohnen R, van Koeveringe GA. The role of phosphodiesterases in bladder pathophysiology. Nat Rev Urol. 2013;10:414–24. doi: 10.1038/nrurol.2013.101. [DOI] [PubMed] [Google Scholar]
- 30.Aizawa N, Igawa Y, Nishizawa O, Wyndaele JJ. Effects of nitric oxide on the primary bladder afferent activities of the rat with and without intravesical acrolein treatment. Eur Urol. 2011;59:264–71. doi: 10.1016/j.eururo.2010.10.035. [DOI] [PubMed] [Google Scholar]
- 31.Förstermann U, Closs EI, Pollock JS, Nakane M, Schwarz P, Gath I, et al. Nitric oxide synthase isozymes. Characterization, purification, molecular cloning, and functions. Hypertension. 1994;23(6 Pt 2):1121–31. doi: 10.1161/01.hyp.23.6.1121. [DOI] [PubMed] [Google Scholar]
- 32.Morris JL, Jobling P, Gibbins IL. Differential inhibition by botulinum neurotoxin A of cotransmitters released from autonomic vasodilator neurons. Am J Physiol Heart Circ Physiol. 2001;281:H2124–32. doi: 10.1152/ajpheart.2001.281.5.H2124. [DOI] [PubMed] [Google Scholar]
- 33.Smith CP, Vemulakonda VM, Kiss S, Boone TB, Somogyi GT. Enhanced ATP release from rat bladder urothelium during chronic bladder inflammation: effect of botulinum toxin A. Neurochem Int. 2005;47:291–7. doi: 10.1016/j.neuint.2005.04.021. [DOI] [PubMed] [Google Scholar]
- 34.Daneshgari F, Liu G, Imrey PB. Time dependent changes in diabetic cystopathy in rats include compensated and decompensated bladder function. J Urol. 2006;176:380–6. doi: 10.1016/S0022-5347(06)00582-9. [DOI] [PubMed] [Google Scholar]
- 35.Cho KJ, Koh JS, Choi J, Kim JC. Changes in adenosine triphosphate and nitric oxide in the urothelium of patients with benign prostatic hyperplasia and detrusor underactivity. J Urol. 2017;198:1392–6. doi: 10.1016/j.juro.2017.06.080. [DOI] [PubMed] [Google Scholar]