Abstract
Objective
This meta-analysis with statistical power analysis aimed to evaluate the difference between full-endoscopic and microscopic spinal decompression in treating spinal stenosis.
Methods
We searched PubMed, Embase, CENTRAL (Cochrane Central Register of Controlled Trials), and CNKI (China National Knowledge Infrastructure) for relevant randomized controlled trials (RCTs) regarding the comparison of full-endoscopic versus microscopic spinal decompression in treating lumbar spinal stenosis through February 28, 2022. Two independent investigators selected studies, extracted information, and appraised methodological quality. Meta-analysis was conducted using RevMan 5.4 and STATA 14.0, and statistical power analysis was performed using G*Power 3.1.
Results
Six RCTs involving 646 patients met selection criteria. Meta-analysis suggested that, compared with microscopic decompression, full-endoscopic spinal decompression achieved more leg pain improvement (mean difference [MD], -0.20; 95% confidence interval [CI], -0.30 to -0.10; p = 0.001), shortened operative time (MD, -12.71; 95% CI, -18.27 to -7.15; p < 0.001), and decreased the incidence of complications (risk ratio, 0.43; 95% CI, 0.22–0.82; p = 0.01), which was supported by a statistical power of 98.57%, 99.97%, and 81.88%, respectively.
Conclusion
Full-endoscopic spinal decompression is a better treatment for lumbar spinal stenosis, showing more effective leg pain improvement, shorter operative time, and fewer complications than microscopic decompression.
Keywords: Full-endoscopic spinal decompression, Microscopic spinal decompression, Lumbar stenosis, Meta-analysis
INTRODUCTION
Lumbar spinal stenosis is described as pathological spinal canal narrowing [1], which will result in a series of neurological symptoms due to subsequent compression of nerve roots, including back and leg pain, claudication, and walking difficulty [2,3]. As one of the most prevalent degenerative conditions [4-6], lumbar spinal stenosis was associated with an increased social and economic burden because it leads to pain and disability and reduces patients’ quality of life [7].
For patients diagnosed with lumbar spinal stenosis at the initial phase, conservative treatments are always recommended [8], including physical therapy, anti-inflammatory agents, and drugs for relieving pain [9-11]. However, patients will be advised to receive surgical intervention if it was more appropriate according to clinical symptoms, physical disability, and magnetic resonance imaging findings [12-16]. Previous studies have demonstrated that surgical intervention was involved in better clinical outcomes in patients with lumbar spinal stenosis [12,14,17]. Unfortunately, traditional open spinal decompression will result in significant trauma, a longer length of hospitalization, and an increased risk of postoperative complications because this surgery requires extensive dissection and stretching of the fatty muscles of the spine [18-20]. Subsequently, various minimally invasive methods have emerged as an alternative to traditional open spinal decompression preserving the normal vertebral structures, preventing segmental instability, and reducing soft tissue damage [21-23].
Among available minimally invasive methods, microscopic spinal decompression has become one of the most common procedures related to less blood loss, lower risk of postoperative pain, and shorter hospital stays [23]. It’s pointed out that microscopic spinal decompression also faced some disadvantages, such as bleeding in the field of view and postoperative adhesions in the spinal canal [24]. However, with advancements in endoscopic spinal surgery, a full-endoscopic spinal system such as uniportal endoscopic system [25,26] and biportal endoscopic spinal system [27] has been developed and used for the treatment of lumbar spinal stenosis.
Several meta-analyses [28-32] have investigated the therapeutic values of the full-endoscopic spinal system in the treatment of lumbar spinal stenosis compared with microscopic spinal decompression. However, the credibility of results from the published meta-analyses was greatly impaired by some limitations, such as incorrect inclusion of studies with overlapping samples and inappropriate combination of data from randomized controlled trials (RCTs) and retrospective studies [33,34]. Moreover, as one of full-endoscopic surgery, transforaminal endoscopic spine system (TESSYS) was not considered in previous meta-analyses. Therefore, we performed the present meta-analysis to further evaluate the comparative effects and safety of full-endoscopic decompression versus microscopic decompression by only including RCTs.
MATERIALS AND METHODS
1. Study Design
This meta-analysis was designed according to recommendations made by the Cochrane Handbook [35]. Meanwhile, pooled results were reported according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) statement [36]. We did not apply for Institutional Review Board’s approval because the data analysis in this meta-analysis was performed based on published studies.
2. Literature Search
Two independent investigators searched PubMed, Embase, Cochrane Central Register of Controlled Trials (CENTRAL), and China National Knowledge Infrastructure (CNKI) for retrieving relevant RCTs from the establishment date of each database through February 28, 2022. The search strategy was developed using the combination of medical subject heading with the free word with the following terms: “spinal stenosis,” “full endoscopic,” “biportal endoscopic spinal surgery,” “unilateral biportal endoscopic technique,” “two portal endoscopic spinal surgery,” “microscopic decompression surgery,” “micro endoscopic spine surgery,” and “random.” The sensitivity of the search strategy was modified according to the requirements of databases. No language and publication status were restricted the in literature search. We summarized detailed search strategies of target databases in Supplementary Table 1. Moreover, we screened reference lists of eligible studies and previous meta-analyses to find additional studies. A third experienced investigator was invited to solve disagreements between 2 investigators about literature retrieval.
3. Selection Criteria
Studies were eligible for our meta-analysis if (1) they enrolled eligible adult patients with diagnosed lumbar spinal stenosis, (2) they are RCTs with full texts, (3) they compared full-endoscopic spinal decompression with microscopic spinal decompression for treating lumbar spinal stenosis, and (4) they reported at least one outcome from visual analogue scale (VAS) score for leg and back pain, operative time, estimated blood loss, the length of hospital stays, and the overall incidence of complications. Certainly, studies were excluded from our meta-analysis if (1) patients suffering from spinal stenosis resulting from a herniated intervertebral disc, (2) studies were designed as ineligible design, such as literature reviews, case reports, experimental studies, (3) repeated studies with relatively poor methodological quality and insufficient information, and (4) essential data for statistical analysis were not available after contacting the leading authors.
4. Data Extraction
Two independent investigators performed the study selection process according to selection criteria from 3 steps: (1) removal of duplicates, (2) initial eligibility evaluation based on the titles and abstracts, and (3) final eligibility evaluation through checking full texts. Then, essential information was independently extracted by 2 investigators using predesigned standard data extraction sheet from each eligible study: reference information (the first author’s name and publication year), country, sample size randomly assigned into both groups, the proportion of male patients, mean age of patients, types of full-endoscopic spinal decompression, follow-up duration, outcomes of interest, and information for methodological quality. We contacted the leading author to obtain essential information if necessary. A third senior investigator was requested to resolve discrepancies between 2 independent investigators.
5. Outcomes of Interest
We defined the VAS score for leg and back pain at the final follow-up as the primary outcomes in this meta-analysis. Moreover, we regarded operative time, estimated blood loss, the length of hospital stays, and the overall incidence of complications as the secondary outcomes.
6. Risk of Bias Assessment
Two investigators used the Cochrane risk of bias assessment tool to independently assess the methodological quality of the included RCTs [37]. In this assessment tool, the following 6 domains were involved: random sequence generation and allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective outcome reporting (reporting bias), and other issues. Depending on the actual information reported in the included studies, each domain could be labeled with a “low,” “unclear,” or “high” risk of bias.
7. Statistical Analysis
Before performing quantitative synthesis, we used the chi-square test [38] and I2 statistic [39] to evaluate the statistical heterogeneity across eligible studies. A fixed-effects model was selected for data analysis if the absence of statistical heterogeneity (p> 0.1, I2< 50%); otherwise, data analysis was carried out based on a random-effects model (p ≤ 0.1, I2≥ 50%) [39]. For dichotomous data, we used the risk ratio (RR) with a corresponding 95% confidence interval (CI) to express the estimates, and the mean difference (MD) with a corresponding 95% CI was sued to express the estimates [40]. We evaluated publication bias for primary outcomes by utilizing Begg rank correlation test [41] and Egger linear regression test [42]. Statistical analysis was carried out using Review Manager (RevMan) 5.4 (Cochrane Collaboration, Oxford, UK), and publication bias examination was performed by using Stata 14.0 (StataCorp LLC, College Station, TX, USA) [43]. Moreover, we also calculated the statistical power for each outcome using G*Power software version 3.1 to determine the confidence in drawing a definitive conclusion [44,45].
RESULTS
1. Literature Search Results
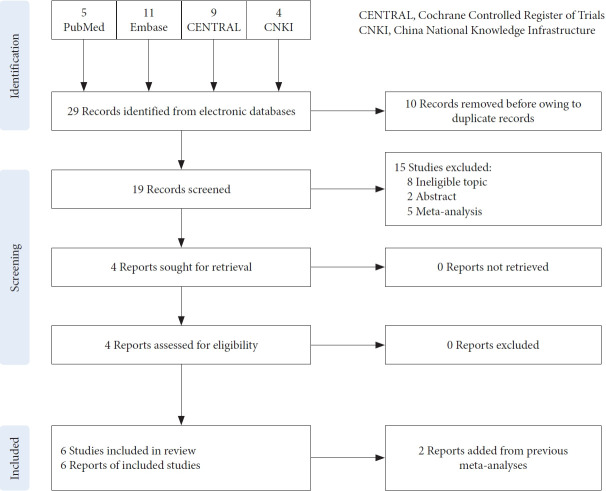
We identified a total of 29 relevant studies from 4 target electronic databases through performing search strategies, including PubMed (n= 5), Embase (n= 11), CENTRAL (n= 9), and CNKI (n= 4). After screening step by step, 4 eligible RCTs were considered to meet our selection criteria. Moreover, 2 additional RCTs were determined from previous meta-analyses. Finally, 6 RCTs [46-51] were included in this meta-analysis. The process of study selection is indicated in Fig. 1.
Fig. 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram for the process of study selection.
2. The Characteristics of Included Studies
The basic information of included studies is summarized in Table 1. Among the 6 eligible RCTs, the sample size of individual study varied from 62 to 161, with 646 patients. All studies were published between 2009 and 2020. Two studies compared biportal technique with microscopic decompression, 3 studies compared uniportal technique with microscopic decompression, and one study compared the TESSYS with microscopic decompression. The follow-up duration of included studies ranged from 6 months to 24 months. Moreover, four [47,49-51] and five [47-51] studies reported VAS scores for leg and back pain, respectively. All studies [46-51] reported single-level operative time, 3 studies [46-48] reported estimated blood loss, 3 studies [47,48,50] reported the length of hospital stays, and 5 studies [47-51] reported the incidence of complications. The outcomes of included studies are summarized in Supplementary Table 2.
Table 1.
Basic information of included studies (n=6)
| Study | Country | Sample size | Male ratio | Mean age (yr) | Full-endoscopic | Follow-up (mo) |
|---|---|---|---|---|---|---|
| Kang et al. [48] 2019 | Korea | 32 vs. 30 | 0.51 | 65.1 vs. 67.2 | Biportal | 6 |
| Park et al. [50] 2020 | Korea | 32 vs. 32 | 0.48 | 66.2 vs. 67.1 | Biportal | 12 |
| Komp et al. [49] 2015 | Germany | 71 vs. 64 | 0.57 | 62 | Uniportal | 24 |
| Hatati et al. 2021 | Saudi Arabia | 77 vs. 77 | 0.61 | 64.6 vs. 65.0 | Uniportal | 24 |
| Ruetten et al. [51] 2009 | Germany | 81 vs. 80 | 0.46 | 64 | Uniportal | 19 |
| Chen et al. [47] 2018 | China | 35 vs. 35 | 0.65 | 55.2 vs. 56.1 | TESSYS | 12 |
3. Quality Assessment
Among 6 included studies, the majority (83.3%) [46-50] were evaluated as low risk in random sequence generation except for one study [51], which only stated random but did not describe the details of generating random sequence. Only 2 studies [49,50] were rated as low risk in allocation concealment, blinding of participants and personnel, and blinding of outcome assessment. All studies were labeled with unclear or low risk in attrition bias domains except for one study [51], which had a high risk in attrition bias. All studies [46-51] were regarded as low risk for reporting bias and other bias. Detailed risk of bias assessment is indicated in Supplementary Fig. 1.
4. Meta-Analysis Results
1) Leg and back pain
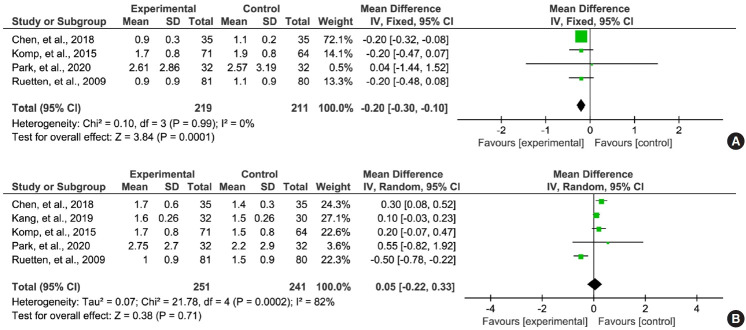
Four studies [47,49-51] reported VAS scores for leg pain at the final follow-up of full-endoscopic spinal decompression in the treatment of lumbar spinal stenosis. We did not detect statistical heterogeneity across studies (I2= 0%, p= 0.99). Therefore, statistical analysis was carried out based on the fixed-effect model. The pooled result indicated that full-endoscopic spinal decompression was associated with more leg pain relief than microscopic decompression (MD, -0.20; 95% CI, -0.30 to -0.10; p= 0.0001) (Fig. 2A).
Fig. 2.
Meta-analysis of visual analogue scale score for leg (A) and back pain (B) between full-endoscopic and microscopic spinal decompression. SD, standard deviation; IV, inverse variance; CI, confidence interval; df, degrees of freedom.
Five studies [47-51] reported VAS scores for back pain at the final follow-up of full-endoscopic spinal decompression in the treatment of lumbar spinal stenosis. Substantial statistical heterogeneity was determined between studies (I2= 82%, p < 0.1). We, therefore, selected the random-effect model to perform statistical analysis, and the result indicated no difference between fullendoscopic and microscopic spinal decompression (MD, 0.05; 95% CI, -0.22 to 0.33; p= 0.71) (Fig. 2B).
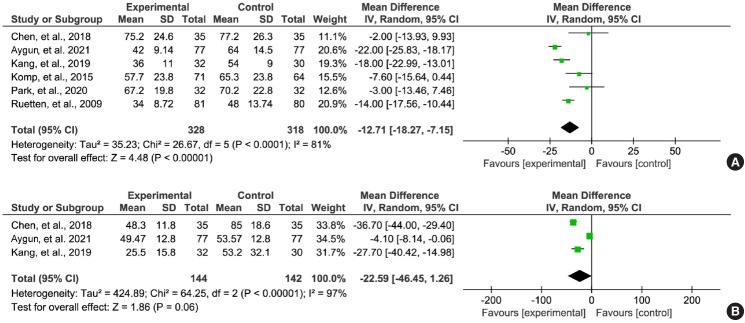
2) Operative time
All studies [46-51] reported single-level operative time between the 2 groups. Substantial statistical heterogeneity was detected between the articles (I2= 81%, p< 0.1), and thus the random-effects model was selected for statistical analysis. Meta-analysis indicated that, compared with microscopic spinal decompression, full-endoscopic spinal decompression was associated with shorter operative time (MD, -12.71; 95% CI, -18.27 to -7.15; p< 0.01) (Fig. 3A).
Fig. 3.
Meta-analysis of operative time (A) and estimated blood (B) loss between full-endoscopic and microscopic spinal decompression. SD, standard deviation; IV, inverse variance; CI, confidence interval; df, degrees of freedom.
3) Estimated blood loss
Among included studies, 3 studies [46-48] estimated the volume of blood loss during treatment. As there was statistical heterogeneity between the studies (I2= 97%, p= 0.06), we, therefore, selected the random-effects model to perform statistical analysis. Pooled results suggested no statistical difference between full-endoscopic and microscopic spinal decompression (MD, -22.59; 95% CI, -46.45 to1.26; p= 0.06) (Fig. 3B).
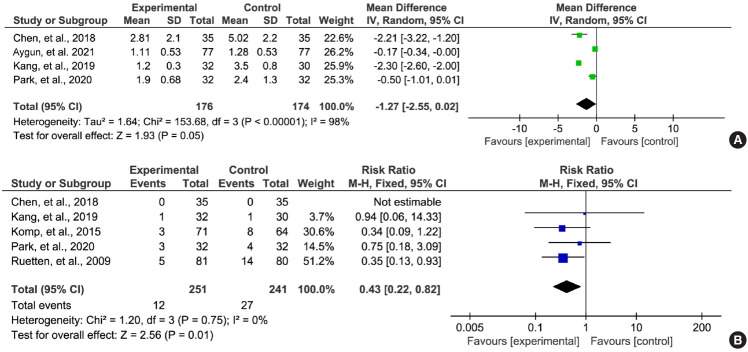
4) The length of hospital stays
Four studies [46-48,50] reported the length of hospital stays after treatment. Substantial statistical heterogeneity was detected between studies (I2= 98%, p = 0.05). We therefore used the random-effect model to perform statistical analysis. The result indicated no statistical difference between full-endoscopic and microscopic spinal decompression in terms of this outcome (MD, -1.27; 95% CI, -2.55 to 0.02; p= 0.05) (Fig. 4A).
Fig. 4.
Meta-analysis of the length of hospital stays (A) and the overall incidence of complications (B) between full-endoscopic and microscopic spinal decompression. SD, standard deviation; IV, inverse variance; CI, confidence interval; df, degrees of freedom.
5) Overall incidence of complications
Five studies [47-51] reported the incidence of complications between full-endoscopic spinal surgery and microscopic decompression. Statistical examination did not detect the presence of substantial statistical heterogeneity between the studies (I2= 0%, p= 0.01). We therefore selected the random-effects model for statistical analysis. Meta-analysis indicated a lower overall incidence of complications in patients receiving full-endoscopic spinal decompression than microscopic spinal decompression (RR, 0.43; 95% CI, 0.22–0.82; p= 0.01) (Fig. 4B).
5. Statistical Power
We calculated the statistical power of all outcomes at the significance level of 0.05. Finally, the statistical power of individual outcomes was 98.57% for leg pain, 10.13% for back pain, 99.97% for operative time, 58.35% for the estimated blood loss, 73.70% for the length of hospital stay, and 81.88% for an overall incidence of complications.
6. Publication Bias
Although the number of eligible studies did not meet the criteria of conducting publication bias, we still sought to evaluate publication bias by performing Egger and Begg tests. As indicated in Supplementary Fig. 2, symmetric Egger and Begg plots were created of VAS score for leg (z= 1.70, p= 0.089; t= 1.85, p= 0.206) and back (z= 0.24, p= 0.806; t= 1.44, p= 0.245) pain, indicating absence of publication bias.
DISCUSSION
Full-endoscopic spinal decompression has several advantages as an emerging minimally technique, including flexibility, a wide and clear field of view, and less soft tissue damage. However, the therapeutic effects and safety of full-endoscopic spinal decompression continue to be debatable in treating lumbar spinal stenosis in clinical practice compared with microscopic spinal decompression. After including 6 eligible RCTs, the present meta-analysis indicated that full-endoscopic spinal surgery effectively relieved leg pain, with shorter operative time and a lower incidence of complications than microscopic spinal decompression. Unfortunately, we did not perform a separate analysis to compare different full-endoscopic spinal decompression with microscopic spinal decompression due to the limited number of eligible studies, which might introduce bias to impair the reliability of our results. Nevertheless, the statistical power of leg pain, operative time, and the overall incidence of complications exceeded the acceptable level of 80.00%, indicating the robustness and reliability of these outcomes. However, the statistical power of back pain, the estimated blood loss, and the length of hospital stay did not get to the acceptable level. Therefore, the pooled results of these 3 outcomes should be interpreted cautiously. Future RCTs with large sample size and high quality are required to determine the difference between the 2 treatments in terms of these 3 outcomes. In addition, more studies should be performed to explore the difference between different full endoscopic spinal decompression techniques.
Several meta-analyses [28-32] have investigated the comparative effects and safety of full-endoscopic spinal decompression with microscopic spinal decompression to treat lumbar spinal stenosis. Unfortunately, the findings from these meta-analyses must be considered in a cautious manner due to several limitations. For example, all meta-analyses included 2 studies [52,53] from the same cohort (a prospective case-control study and a retrospective). Therefore, overlapped samples were included to falsely enhance the statistical power. It must be noted that, certainly, all meta-analyses simultaneously included RCTs and retrospective studies to estimate the comparative effects and safety between full-endoscopic spinal decompression and microscopic decompression. However, according to the methodological framework, it is inappropriate to combine results from RCTs and non-RCTs [35].
Compared with previous meta-analyses, the present meta-analysis generated more robust and reliable findings due to methodological advantages. First, only RCTs were included for the final analysis in this meta-analysis, which significantly enhanced the comparability between studies and the statistical power. Second, all available full-endoscopic spinal decompression systems were considered in the present meta-analysis. However, previous meta-analyses only included biportal or uniportal techniques, which limited the number of eligible studies and did not comprehensively consider the types of full-endoscopic decompression. Third, we either identified relevant studies by searching 4 electronic databases or added additional studies by checking previous meta-analyses, which greatly decreased the risk of missing potentially eligible studies. Finally, we calculated the statistical power of all outcomes to achieve a creditable conclusion, demonstrating the robustness and reliability of positive results in the present meta-analysis.
The present meta-analysis has some limitations, which could not be ignored. First, only 6 eligible RCTs with inadequate sample size were included in the final statistical analysis. Therefore, our findings may be fluctuated due to inadequate statistical power. Second, follow-up duration was different from one to another eligible study. However, we only extracted data at the final follow-up to evaluate the comparative effects and safety, which may introduce bias to impair the robustness of our findings. Third, this meta-analysis identified 3 available full-endoscopic spinal surgeries for lumbar spinal stenosis, including uniportal technique, biportal technique, and TESSYS. However, subgroup analysis was not performed according to the types of full-endoscopic spinal decompression due to inadequate number of eligible studies, which could cause heterogeneous results. Fourth, although on restriction on language and publication status was imposed in this meta-analysis, potential risk of missing relevant studies could not be avoided because only 4 electronic databases were considered. Fifth, we developed the methodological framework for this meta-analysis in strict accordance with the recommendations made by the Cochrane handbook; however, we did not register the formal protocol in any public platform.
CONCLUSION
This meta-analysis evaluated the comparative effect and safety of full-endoscopic spinal decompression with microscopic spinal decompression in treating lumbar spinal stenosis by including 6 RCTs. Our results suggested that full-endoscopic spinal decompression is more effective than microscopic decompression, with more significant leg pain relief, shorter operative time, and lower complications. Due to the extremely insufficient statistical power of back pain, the estimated blood loss, and the length of hospital stay, future studies with a large-scale and high quality are warranted to determine the difference between full-endoscopic spinal decompression and microscopic decompression in treating lumbar spinal stenosis. Moreover, studies are also required to investigate the comparative effects and safety of different full-endoscopic spinal decompression systems.
Footnotes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: ZY, WL, WH; Formal analysis: HW, WH; Methodology: ZY, HW, WL, WH; Writing - original draft: ZY, HW, WL; Writing - review & editing: ZY, HW, WL.
SUPPLEMENTARY MATERIALS
Supplementary Tables 1-2 and Figs. 1-2 can be found via https://doi.org/10.14245/ns.2244600.300.
Search strategy of target databases
Outcomes of included studies (n=6)
Risk of bias assessment.
Egger and Begg plots of visual analogue scale score for leg and back pain between full-endoscopic (a) and microscopic spinal decompression (b). SE, standard error.
REFERENCES
- 1.Liu Z, Zhang S, Li J, et al. Biomechanical comparison of different interspinous process devices in the treatment of lumbar spinal stenosis: a finite element analysis. BMC Musculoskelet Disord. 2022;23:585. doi: 10.1186/s12891-022-05543-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee SY, Kim TH, Oh JK, et al. Lumbar stenosis: a recent update by review of literature. Asian Spine J. 2015;9:818–28. doi: 10.4184/asj.2015.9.5.818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Machado GC, Ferreira PH, Yoo RI, et al. Surgical options for lumbar spinal stenosis. Cochrane Database Syst Rev. 2016;11:CD012421. doi: 10.1002/14651858.CD012421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parker SL, Godil SS, Mendenhall SK, et al. Two-year comprehensive medical management of degenerative lumbar spine disease (lumbar spondylolisthesis, stenosis, or disc herniation): a value analysis of cost, pain, disability, and quality of life: clinical article. J Neurosurg Spine. 2014;21:143–9. doi: 10.3171/2014.3.SPINE1320. [DOI] [PubMed] [Google Scholar]
- 5.Abbas J, Peled N, Hershkovitz I, et al. Facet tropism and orientation: risk factors for degenerative lumbar spinal stenosis. Biomed Res Int. 2020;2020:2453503. doi: 10.1155/2020/2453503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kalff R, Ewald C, Waschke A, et al. Degenerative lumbar spinal stenosis in older people: current treatment options. Dtsch Arztebl Int. 2013;110:613–23. doi: 10.3238/arztebl.2013.0613. quiz 624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deyo RA, Mirza SK, Martin BI, et al. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010;303:1259–65. doi: 10.1001/jama.2010.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koc Z, Ozcakir S, Sivrioglu K, et al. Effectiveness of physical therapy and epidural steroid injections in lumbar spinal stenosis. Spine (Phila Pa 1976) 2009;34:985–9. doi: 10.1097/BRS.0b013e31819c0a6b. [DOI] [PubMed] [Google Scholar]
- 9.Mazanec DJ, Podichetty VK, Hsia A. Lumbar canal stenosis: start with nonsurgical therapy. Cleve Clin J Med. 2002;69:909–17. doi: 10.3949/ccjm.69.11.909. [DOI] [PubMed] [Google Scholar]
- 10.Theodoridis T, Krämer J, Kleinert H. Conservative treatment of lumbar spinal stenosis--a review. Z Orthop Unfall. 2008;146:75–9. doi: 10.1055/s-2007-989394. [DOI] [PubMed] [Google Scholar]
- 11.Siebert E, Prüss H, Klingebiel R, et al. Lumbar spinal stenosis: syndrome, diagnostics and treatment. Nat Rev Neurol. 2009;5:392–403. doi: 10.1038/nrneurol.2009.90. [DOI] [PubMed] [Google Scholar]
- 12.Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med. 2008;358:794–810. doi: 10.1056/NEJMoa0707136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ma XL, Zhao XW, Ma JX, et al. Effectiveness of surgery versus conservative treatment for lumbar spinal stenosis: a system review and meta-analysis of randomized controlled trials. Int J Surg. 2017;44:329–38. doi: 10.1016/j.ijsu.2017.07.032. [DOI] [PubMed] [Google Scholar]
- 14.Amundsen T, Weber H, Nordal HJ, et al. Lumbar spinal stenosis: conservative or surgical management?: a prospective 10-year study. Spine (Phila Pa 1976) 2000;25:1424–35. doi: 10.1097/00007632-200006010-00016. discussion 1435-6. [DOI] [PubMed] [Google Scholar]
- 15.Weber C, Giannadakis C, Rao V, et al. Is there an association between radiological severity of lumbar spinal stenosis and disability, pain, or surgical outcome? A multicenter observational study. Spine (Phila Pa 1976) 2016;41:E78–83. doi: 10.1097/BRS.0000000000001166. [DOI] [PubMed] [Google Scholar]
- 16.Sirvanci M, Bhatia M, Ganiyusufoglu KA, et al. Degenerative lumbar spinal stenosis: correlation with Oswestry Disability Index and MR imaging. Eur Spine J. 2008;17:679–85. doi: 10.1007/s00586-008-0646-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Malmivaara A, Slätis P, Heliövaara M, et al. Surgical or nonoperative treatment for lumbar spinal stenosis? A randomized controlled trial. Spine (Phila Pa 1976) 2007;32:1–8. doi: 10.1097/01.brs.0000251014.81875.6d. [DOI] [PubMed] [Google Scholar]
- 18.Hu ZJ, Fang XQ, Zhou ZJ, et al. Effect and possible mechanism of muscle-splitting approach on multifidus muscle injury and atrophy after posterior lumbar spine surgery. J Bone Joint Surg Am. 2013;95:e192. doi: 10.2106/JBJS.L.01607. [DOI] [PubMed] [Google Scholar]
- 19.Fritsch EW, Heisel J, Rupp S. The failed back surgery syndrome: reasons, intraoperative findings, and long-term results: a report of 182 operative treatments. Spine (Phila Pa 1976) 1996;21:626–33. doi: 10.1097/00007632-199603010-00017. [DOI] [PubMed] [Google Scholar]
- 20.Guha D, Heary RF, Shamji MF. Iatrogenic spondylolisthesis following laminectomy for degenerative lumbar stenosis: systematic review and current concepts. Neurosurg Focus. 2015;39:E9. doi: 10.3171/2015.7.FOCUS15259. [DOI] [PubMed] [Google Scholar]
- 21.Arai Y, Hirai T, Yoshii T, et al. A prospective comparative study of 2 minimally invasive decompression procedures for lumbar spinal canal stenosis: unilateral laminotomy for bilateral decompression (ULBD) versus muscle-preserving interlaminar decompression (MILD) Spine (Phila Pa 1976) 2014;39:332–40. doi: 10.1097/BRS.0000000000000136. [DOI] [PubMed] [Google Scholar]
- 22.Min WK, Kim JE, Choi DJ, et al. Clinical and radiological outcomes between biportal endoscopic decompression and microscopic decompression in lumbar spinal stenosis. J Orthop Sci. 2020;25:371–8. doi: 10.1016/j.jos.2019.05.022. [DOI] [PubMed] [Google Scholar]
- 23.Mobbs RJ, Li J, Sivabalan P, et al. Outcomes after decompressive laminectomy for lumbar spinal stenosis: comparison between minimally invasive unilateral laminectomy for bilateral decompression and open laminectomy: clinical article. J Neurosurg Spine. 2014;21:179–86. doi: 10.3171/2014.4.SPINE13420. [DOI] [PubMed] [Google Scholar]
- 24.Benoist M, Ficat C, Baraf P, et al. Postoperative sciatica from epidural fibrosis and lumbar arachnoiditis. Results of 38 repeat operations. Rev Rhum Mal Osteoartic. 1979;46:593–9. [PubMed] [Google Scholar]
- 25.Polikandriotis JA, Hudak EM, Perry MW. Minimally invasive surgery through endoscopic laminotomy and foraminotomy for the treatment of lumbar spinal stenosis. J Orthop. 2013;10:13–6. doi: 10.1016/j.jor.2013.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thomé C, Zevgaridis D, Leheta O, et al. Outcome after lessinvasive decompression of lumbar spinal stenosis: a randomized comparison of unilateral laminotomy, bilateral laminotomy, and laminectomy. J Neurosurg Spine. 2005;3:129–41. doi: 10.3171/spi.2005.3.2.0129. [DOI] [PubMed] [Google Scholar]
- 27.Soliman HM. Irrigation endoscopic decompressive laminotomy. A new endoscopic approach for spinal stenosis decompression. Spine J. 2015;15:2282–9. doi: 10.1016/j.spinee.2015.07.009. [DOI] [PubMed] [Google Scholar]
- 28.Li C, Ju F, Li W, et al. Efficacy and safety of unilateral biportal endoscopy compared with microscopic decompression in the treatment of lumbar spinal stenosis: a protocol for systematic review and meta-analysis. Medicine (Baltimore) 2021;100:e27970. doi: 10.1097/MD.0000000000027970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liang J, Lian L, Liang S, et al. Efficacy and complications of unilateral biportal endoscopic spinal surgery for lumbar spinal stenosis: a meta-analysis and systematic review. World Neurosurg. 2022;159:e91–102. doi: 10.1016/j.wneu.2021.12.005. [DOI] [PubMed] [Google Scholar]
- 30.Pairuchvej S, Muljadi JA, Ho JC, et al. Full-endoscopic (biportal or uni-portal) versus microscopic lumbar decompression laminectomy in patients with spinal stenosis: systematic review and meta-analysis. Eur J Orthop Surg Traumatol. 2020;30:595–611. doi: 10.1007/s00590-019-02604-2. [DOI] [PubMed] [Google Scholar]
- 31.Perez-Roman RJ, Gaztanaga W, Lu VM, et al. Endoscopic decompression for the treatment of lumbar spinal stenosis: an updated systematic review and meta-analysis. J Neurosurg Spine. 2021;36:549–57. doi: 10.3171/2021.8.SPINE21890. [DOI] [PubMed] [Google Scholar]
- 32.Pranata R, Lim MA, Vania R, et al. Biportal endoscopic spinal surgery versus microscopic decompression for lumbar spinal stenosis: a systematic review and meta-analysis. World Neurosurg. 2020;138:e450–8. doi: 10.1016/j.wneu.2020.02.151. [DOI] [PubMed] [Google Scholar]
- 33.Lin GX, Hu BS, Rui G. Letter to the editor regarding “Full endoscopic (bi portal or uni portal) versus microscopic lumbar decompression laminectomy in patients with spinal stenosis: systematic review and meta analysis”. Eur J Orthop Surg Traumatol. 2022 Jan 15; doi: 10.1007/s00590-021-03177-9. . [Epub] [DOI] [PubMed] [Google Scholar]
- 34.Lin GX, Rui G, Jhang SW, et al. Letter to the editor regarding “biportal endoscopic spinal surgery versus microscopic decompression for lumbar spinal stenosis: a systematic review and meta-analysis”. World Neurosurg. 2022;157:248. doi: 10.1016/j.wneu.2021.09.082. [DOI] [PubMed] [Google Scholar]
- 35.Higgins JPT, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2021) Cochrane; 2021. Available from www.training.cochrane.org/handbook. [Google Scholar]
- 36.Page MJ, Moher D, Bossuyt PM, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160. doi: 10.1136/bmj.n160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 39.Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Doi SA, Furuya-Kanamori L, Xu C, et al. Controversy and debate: questionable utility of the relative risk in clinical research: Paper 1: a call for change to practice. J Clin Epidemiol. 2022;142:271–9. doi: 10.1016/j.jclinepi.2020.08.019. [DOI] [PubMed] [Google Scholar]
- 41.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101. [PubMed] [Google Scholar]
- 42.Egger M, Davey Smith G, Schneider M, et al. Bias in metaanalysis detected by a simple, graphical test. BMJ. 1997;315:629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chaimani A, Mavridis D, Salanti G. A hands-on practical tutorial on performing meta-analysis with Stata. Evid Based Ment Health. 2014;17:111–6. doi: 10.1136/eb-2014-101967. [DOI] [PubMed] [Google Scholar]
- 44.Faul F, Erdfelder E, Lang AG, et al. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–91. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 45.Faul F, Erdfelder E, Buchner A, et al. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41:1149–60. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- 46.Aygun H, Abdulshafi K. Unilateral biportal endoscopy versus tubular microendoscopy in management of single level degenerative lumbar canal stenosis: a prospective study. Clin Spine Surg. 2021;34:E323–8. doi: 10.1097/BSD.0000000000001122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen K, Pan HS, Huang MF, et al. Comparative effect of transforaminal endoscopic spine system versus micro endoscopic discectomy for the treatment of lumbar spinal lateral recess stenosis. Chin J Pain Med. 2018;24:229–34. [Google Scholar]
- 48.Kang T, Park SY, Kang CH, et al. Is biportal technique/endoscopic spinal surgery satisfactory for lumbar spinal stenosis patients? A prospective randomized comparative study. Medicine (Baltimore) 2019;98:e15451. doi: 10.1097/MD.0000000000015451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Komp M, Hahn P, Oezdemir S, et al. Bilateral spinal decompression of lumbar central stenosis with the full-endoscopic interlaminar versus microsurgical laminotomy technique: a prospective, randomized, controlled study. Pain Physician. 2015;18:61–70. [PubMed] [Google Scholar]
- 50.Park SM, Park J, Jang HS, et al. Biportal endoscopic versus microscopic lumbar decompressive laminectomy in patients with spinal stenosis: a randomized controlled trial. Spine J. 2020;20:156–65. doi: 10.1016/j.spinee.2019.09.015. [DOI] [PubMed] [Google Scholar]
- 51.Ruetten S, Komp M, Merk H, et al. Surgical treatment for lumbar lateral recess stenosis with the full-endoscopic interlaminar approach versus conventional microsurgical technique: a prospective, randomized, controlled study. J Neurosurg Spine. 2009;10:476–85. doi: 10.3171/2008.7.17634. [DOI] [PubMed] [Google Scholar]
- 52.Heo DH, Lee DC, Park CK. Comparative analysis of three types of minimally invasive decompressive surgery for lumbar central stenosis: biportal endoscopy, uniportal endoscopy, and microsurgery. Neurosurg Focus. 2019;46:E9. doi: 10.3171/2019.2.FOCUS197. [DOI] [PubMed] [Google Scholar]
- 53.Heo DH, Quillo-Olvera J, Park CK. Can percutaneous biportal endoscopic surgery achieve enough canal decompression for degenerative lumbar stenosis? Prospective casecontrol study. World Neurosurg. 2018;120:e684–9. doi: 10.1016/j.wneu.2018.08.144. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search strategy of target databases
Outcomes of included studies (n=6)
Risk of bias assessment.
Egger and Begg plots of visual analogue scale score for leg and back pain between full-endoscopic (a) and microscopic spinal decompression (b). SE, standard error.