Abstract
Introduction
Obesity and type 2 diabetes (T2D) are two closely related pandemic conditions. Novel technologies represent promising tools for their management, the use of which has been greatly encouraged during the COVID-19 pandemic. The aim of the present study is to compare a web-based nutritional intervention versus a traditional one, before and during the Italian ‘lockdown’ period due to the COVID-19 outbreak, in overweight and obese subjects affected by T2D or impaired glucose regulation (IGR).
Methods
For the study, 36 subjects were randomly allocated into two arms: a traditional arm, providing face-to-face individual and group-based intervention; and a web arm, deploying the in-presence traditional approach with intervention provided through web technologies. The outcomes were the data resulting from the comparison between the subjects’ anthropometric and clinical parameters as well as PREDIMED scores at baseline with those at 3 months (T3), 6 months (T6) and at lockdown.
Results
In the web arm we detected a progressive reduction in weight and body mass index (BMI) from baseline to T6 and a minimal increase of both parameters during the lockdown. Improvement of these parameters compared with baseline was observed in controls during the lockdown. The PREDIMED score improved at T6 compared with baseline in both arms. Significant variations were observed considering weight (p < 0.001), BMI (p = 0.001) and PREDIMED scores (p = 0.023) over time.
Discussion
The study showed the effectiveness and feasibility of a short-term nutritional web-based intervention in patients affected by T2D or IGR before and during the COVID 19 pandemic.
Clinical Trial registration number: NCT04386200, ClinicalTrials.gov.
Keywords: Web-based intervention, nutrition, type 2 diabetes, obesity, COVID-19, pandemic, telehealth
Introduction
Obesity and type 2 diabetes (T2D) are two closely related pandemic conditions: most people with T2D are overweight or obese.1 Evidence shows that obesity management, through strategies including lifestyle intervention, can slow the progression of impaired glucose regulation (IGR) to T2D and may enhance T2D treatment.2 As is well known, a small weight loss in overweight or obese T2D subjects allows for glycaemic control improvement and a reduced need for glucose-lowering medications.2
Telemedicine is a tool that can support traditional clinical practice, and promote involvement and decision making and new methodologies to support educational interventions.3,4 Telehealth uses telecom-munications and virtual technology to support and favour healthcare access (particularly for chronic diseases), as well as to reduce the crowding of facilities, thus resulting in cost-effectiveness.5 Mobile Health (mHealth), through mobile wireless technologies, is a resource that can improve access to health information and promote changes in health-related behaviours.6 The use of information technologies requires that both patients and healthcare providers are capable of accessing and utilizing the technology.
In recent years, there has been an increase in the number of technologies which can facilitate long-distance clinical care, education, and health administration, including live video teleconferencing, remote patient monitoring, the use of mobile health applications, texting and emailing.7 Although there is no doubt regarding the potential of these tools, especially in reducing physical co-presence, it must be emphasized that achieving behavioural changes is a very complex process.8 In this regard, a key challenge is to make essential information available to users, to help and involve the subjects in the decision-making process, and to develop and implement services that can be agreed and appreciated by the user.9 Information and communication technologies (ICT) can be a promising resource to promote and support an individual’s active and meaningful participation in health management.9 Moreover, ICT could be used to foster healthy lifestyles and achieve well-being through an individual’s empowerment, engagement and self-management.9
Patients’ empowerment could be favoured by health education through a patient-centred approach or by promoting an active role for the patient; for example, by encouraging patients to look for online information or join group sessions with other patients.8,10 It has been observed that group-based lifestyle intervention versus standard care fostered modest weight loss at 6 and 12 months of treatment in adults with T2D.11 Group dynamics and peer identification are likely to promote greater self-esteem, self-perception and well-being while reducing anxiety related to diabetes.12
In recent years, research has focused on mobile wireless technologies and wearable devices (mHealth) as promising and cost-effective tools for the promotion of health and behavioural changes among patients with chronic diseases. These are fostered by feedback, social support and easier interactions with healthcare providers, other patients, and family members.13
On 11 March 2020, the World Health Organization announced the outbreak of a Coronavirus Disease-2019 (COVID-19) pandemic;14 at the time, Italy was considered the epicentre of the disease in Europe.15 At that time, the Italian government announced a ‘lockdown’ state. This restrictive measure consisted of the limitation of freedom of movement, activities and social interactions, although guaranteeing all essential services.15
During the lockdown period, most people had to change their exercise and nutritional habits, which impacted on their body weight.16 Obese individuals with and without diabetes should pursue lifestyle changes, while complying with the measures of social distancing and isolation of positive cases.17 In people with diabetes, changes in lifestyle habits, in addition to the restricted access to routine visits, might contribute to uncontrolled metabolic states or to worsening comorbidities.18 In this context, telemedicine can represent a useful tool for the management of diabetes, and other chronic diseases.18,19
The COVID-19 pandemic has in fact greatly encouraged the delivery of telemedicine and telehealth, although their routine use by the health system would be required for high performance in an emergency state.20 This circumstance offers the opportunity to verify their effectiveness in contexts of diabetes management never previously experienced.21
In this complex and constantly evolving scenario, the aim of the present study is to compare a web-based intervention versus a traditional nutritional one, with a focus on anthropometric and clinical parameters and adherence to a Mediterranean Diet (MedDiet), before and during the Italian ‘lockdown’ period, in overweight or obese people affected by T2D or IGR and involved in a nutritional and healthy lifestyle programme.
Methods
From February to September 2019, 50 overweight or obese individuals were recruited in a 12-month randomized control trial at the Diabetes, Nutrition and Metabolism Unit at the Hospital of University “Gabriele d’Annunzio” in Chieti, Italy. The study aimed at testing web-based strategies to promote adherence to a healthy lifestyle and medical nutritional therapy (MNT) over time.
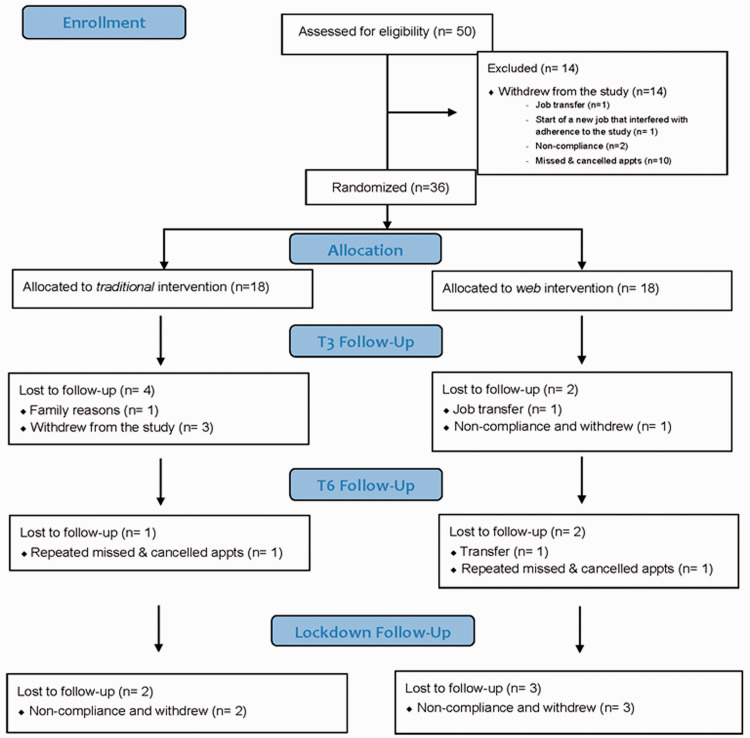
Among these patients, 14 subjects withdrew from the study. The dropouts were due to work reasons that interfered with adherence to the study, non-compliance or failure to show up to scheduled appointments. In total, 36 individuals were randomly allocated either to a web arm (n = 18) or a traditional arm (n = 18) as reported in the participants’ flow chart (Figure 1).
Figure 1.
Participants’ flow chart.
Study protocols were registered in the National Clinical Trials Registry (NCT04386200) and approved by the Ethics Committee of the Province di Chieti e Pescara (approval number 1913). In accordance with the Declaration of Helsinki, all participants gave their written informed consent prior to their inclusion in the study.
Inclusion and exclusion criteria
The inclusion criteria were overweight or obese (body mass index (BMI) ≥25 kg/m2) subjects (male or female), ≥18 years of age, affected by T2D or IGR (impaired fasting glucose (IFG) or impaired glucose tolerance (IGT)), with basic skills in the use of web-based technologies and Internet functions (e.g. the ability to browse the web, use email, download and/or upload multimedia files, access and consult a website), and with access to the Internet. These abilities had been communicated via an interview with medical staff. In accordance with current guidelines, the criteria for diagnosing T2D was a random plasma glucose ≥200 mg/dl, in a subject with classic symptoms of the disease (polyuria, polydipsia, weight loss). In the absence of classic symptoms, the diagnostic criteria, confirmed by at least two repeat testings, were fasting plasma glucose (FPG) ≥126 mg/dl (fasting defined as no caloric intake for at least 8 h) or 2-hour plasma glucose ≥200 mg/dl during the 75 g oral glucose tolerance test (OGTT) or HbA1c ≥48 mmol/mol (6.5%) using a standardized and IFFC-aligned method.22,23 IGR (also known as “Dysglycemia”) refers to ‘a metabolic state between normal glucose homeostasis and diabetes’.24,25 IGR includes both IFG, characterized by FPG levels between 100 and 125 mg/dl, and/or IGT as 2-h plasma glucose during 75 g OGTT levels between 140 and 199 mg/dl or HbA1c 42–48 mmol/mol (IFCC aligned).22,23 The exclusion criteria were: subjects affected by type 1 diabetes, subjects affected by eating behaviour disorders, presence of conditions that could interfere with the development and completion of the project or failing adherence to the protocol.
Interventions and outcome assessment
At baseline, each subject underwent an individual interview focusing on MNT and healthy lifestyle with a physician and a dietician from the diabetes team. Demographic characteristics, and clinical and anthropometric parameters were collected. Body weight and height, BMI, waist and hip circumferences (WC and HC, respectively), waist-to-hip ratio (WHR), capillary fasting blood glucose, venous HbA1c, and blood pressure were included.
In detail, participants’ body weight and height were measured using mechanical scales with a stadiometer, while participants wore light clothing and no shoes; BMI was calculated by applying the formula kg/m2. WC and HC were registered using a flexible centimetre tape measure, and WHR was calculated using the formula WC/HC. Blood pressure was measured by the physician, and clinical biomarkers results were collected.
Moreover, adherence to the MedDiet was assessed using a validated 14-item questionnaire (PREDIMED) which generates a range of possible scores: no adherence (score ≤5), medium adherence (6≤ score ≤9), and maximum adherence (score ≥10).26
Participants allocated in the traditional arm were actively involved in face-to-face individual and group-based intervention through a theoretical and practical course. Those allocated in the web arm integrated both the above-mentioned traditional approach with intervention provided through web technologies.
The first face-to-face individual intervention was a clinical check-up and the recording of the individual’s clinical history. Also, during this first encounter, participants were instructed on how to keep a journal on dietary self-monitoring, based on the scientific literature.27 The journal entries were discussed by the participant and the physician at the next meeting.
To ensure the active involvement of patients in the change process, educational group sessions intervention was considered essential to improve the lifestyle of obese and/or T2D subjects.10 For both arms, the group-based intervention was organized in sessions performed with small groups of up to 10 people in the presence of a trained facilitator, every 3 months. The programme, which included content on healthy nutrition and lifestyle and the promotion of physical activity, was conducted using a group session educational approach, in accordance with the best clinical practices described in the current scientific literature.12,28,29 In detail, each group session was structured in different stages: an opening stage with the reception of the participants and an introduction to the topic of the meeting; a second stage with a discussion and activities involving the participants, such as problem-solving exercises and real-life simulations; and a final stage in which instructions for the next meeting were shared and clarified.
In the group meetings of the traditional arm, participants were provided with useful information on healthy nutritional behaviour as well as learning material and hand-outs with exercises, which were collected and discussed in the next meeting.
In the web arm, the same contents were made available only through a web-based platform used to create a classroom-like environment to enable interaction with healthcare providers and fellow patients. Personal credentials were provided to access the platform, where repeatable exercises with immediate feedback were also placed to assess patients’ awareness. Furthermore, a one-to-one chat application was deployed whenever the web-based platform was not deemed user-friendly.
After 3 months (T3) and 6 months (T6) from baseline, BMI data, as well as WHR, capillary fasting blood glucose, venous HbA1c, blood pressure and PREDIMED scores were collected in both groups. In particular, at each face-to-face outpatient visit, the subjects’ anthropometric and clinical parameters were detected and recorded as described for the baseline. The original protocol would have included the assessment of these parameters up to 12 months of treatment. Unfortunately, the outbreak of the COVID-19 pandemic caused mobility restrictions, which halted in-presence group meetings and routine outpatient visits. In this new and unpredictable condition, it became necessary to identify new strategies to provide support to patients while reducing travel.
As for the web arm, multimedia content on healthy nutrition and active lifestyle to be adopted during the lockdown was shared using a web-based platform or a chat application; the same content was communicated by phone to subjects allocated to the traditional group. Subsequently, after about 40 days of lockdown, all patients involved in the project, regardless of the treatment group previously assigned, were engaged online using the PREDIMED questionnaire administered via the web.
Participants from both arms were therefore invited to record their weight and circumferences data at home and report them to their care providers using communication technologies. The participants had been previously instructed on how to collect reference points measurements using a flexible tape measure.
Due to the unexpected critical situation, the endpoint of this study became the comparison between the data of the two arms, and more specifically, the participants’ anthropometric and clinical parameters as well as their PREDIMED scores, at baseline, T3, T6 and at lockdown.
Statistical analysis
This study was designed to show the effect of remote therapeutic reinforcement through web-based strategies compared with a traditional approach. The main outcome was the difference in weight between the web arm and the traditional one. Assuming a difference of at least 3% with a standard deviation of 4.5% between two groups, 18 patients in each group were required for an 80% power and 5% significance.30 Patients were randomly assigned to two groups (web or traditional) with 1:1 ratio.
Departures from normal distribution were evaluated for each variable using a Shapiro–Wilk’s test; as quantitative variables do not show a normal distribution they were reported as median and interquartile range (IQR). Categorical data were summarized as frequency and percentage. The primary and secondary quantitative outcomes such as BMI, WC, HC, WHR, fasting glucose, blood pressure and PREDIMED score were analysed using different linear mixed models. Linear mixed model is a powerful method for analysing data from longitudinal studies in which there are multiple measurements on each subject. This approach allows explicit modelling of the within-person and between-person variation in the outcome, while taking into account the correlation between repeated measurements on the same individual. Linear mixed model for repeated measurements was applied to regress baseline, T3, T6 and ‘lockdown’ measures on the fixed-effect factors assuming unstructured covariance matrix.
The false discovery rate correction (FDR) was used to control the family-wise type I error rate and an FDR adjusted p-value less than 0.05 was determined to be statistically significant. All the statistical analyses were performed using R software environment for statistical computing and graphics version 3.5.2.31
Results
The baseline characteristics of the 36 participants allocated to the web arm (n = 18, 9 males and 9 females) and the traditional arm (n = 18, 7 males and 11 females) have been summarized in Table 1.
Table 1.
Baseline characteristics of the 36 subjects randomized to web group or traditional group.
| Characteristic | Traditional group (n=18) | Web group (n=18) |
|---|---|---|
| Age (year)† | 63.5 (53.0, 65.8) | 56.5 (55.0, 63.0) |
| Weight (kg)† | 95.5 (82.5, 104.0) | 102.5 (90.1, 110.6) |
| BMI (kg/m2)† | 33.7 (29.4, 37.1) | 35.2 (30.1, 39.8) |
| Waist circumference (cm)† | 111.5 (102.2, 118.2) | 112.5 (105.2, 119.9) |
| Hip circumference (cm)† | 112.5 (105.5, 118.0) | 119.8 (108.2, 126.8) |
| WHR † | 1.0 (0.9, 1.0) | 1.0 (0.9, 1.0) |
| Fasting Blood Glucose (mg/dl)† | 118.0 (109.0, 127.0) | 109.5 (97.5, 118.5) |
| HbA1c (%)† | 6.5 (6.0, 7.4) | 6.4 (5.9, 6.6) |
| HbA1c (mmol/mol)† | 48 (42, 57) | 46 (41, 49) |
| Systolic blood pressure (mmHg)† | 145.0 (130.0, 150.0) | 127.5 (115.0, 140.0) |
| Diastolic blood pressure (mmHg)† | 80.0 (80.0, 88.8) | 80.0 (75.0, 90.0) |
| Diagnosis‡ | ||
| T2D | 14 (77.8%) | 13 (72.2%) |
| IFG | 4 (22.2%) | 3 (16.7%) |
| IGT | 0 (0.0%) | 2 (11.1%) |
| PREDIMED (score)† | 7.5 (7.0, 9.0) | 8.0 (8.0, 9.5) |
BMI: Body Mass Index; WHR: waist-to-hip ratio; T2D: Type 2 Diabetes; IFG: Impaired Fasting Glucose; IGT: Impaired Glucose Tolerance; PREDIMED: PREvención con DIeta MEDiterránea.
†Data are presented as median and interquartile range (IQR).
‡Data are presented as frequency and percentage (%).
The comparison of anthropometric and clinical parameters, plus PREDIMED scores at baseline with those at T3, T6 and at ‘lockdown’, for both groups, are presented in Table 2.
Table 2.
Median and interquartile range (IQR) of evaluated parameters at different control of follow-up; p-values derived from linear mixed model between arms.
| Variable |
Baseline |
T3 |
T6 |
Lockdown period |
p-value |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Traditional arm | Web arm | Traditional arm | Web arm | Traditional arm | Web arm | Traditional arm | Web arm | Time* | Group** | Interaction*** | |
| Weight (kg) | 95.5 | 102.5 | 94.5 | 97.0 | 96.5 | 92.0 | 91.2 | 93.0 | <0.001 | 0.075 | 0.516 |
| (82.5, 104.0) | (90.1, 110.6) | (76.8, 97.4) | (85.1, 106.6) | (78.8, 100.5) | (83.5, 105.0) | (72.8, 95.8) | (90.0, 105.0) | ||||
| BMI (kg/m2) | 33.7 | 35.2 | 34.2 | 34.7 | 34.1 | 33.4 | 32.1 | 33.7 | 0.001 | 0.338 | 0.380 |
| (29.4, 37.1) | (30.1, 39.8) | (29.0, 36.6) | (28.7, 37.9) | (31.7, 36.9) | (29.7, 37.0) | (26.8, 35.3) | (30.0, 37.3) | ||||
| Waist circumference (cm) | 111.5 | 112.5 | 111.5 | 107.0 | 108.0 | 106.0 | 112.0 | 110.5 | 0.171 | 0.633 | 0.761 |
| (102.2, 118.2) | (105.2, 119.9) | (100.2, 115.8) | (97.0, 115.5) | (102.0, 116.5) | (98.5, 109.4) | (95.2, 119.8) | (104.0, 115.5) | ||||
| Hip circumference (cm) | 112.5 | 119.8 | 113.8 | 116.5 | 115.0 | 114.0 | 112.0 | 112.0 | 0.129 | 0.475 | 0.273 |
| (105.5, 118.0) | (108.2, 126.8) | (106.0, 118.2) | (108.8, 123.0) | (106.5, 120.5) | (109.2, 123.8) | (102.0, 113.0) | (109.5, 114.5) | ||||
| WHR | 1.0 | 1.0 | 1.0 | 0.9 | 1.1 | 1.1 | 1.1 | 0.9 | 0.044 | 0.295 | 0.097 |
| (0.9, 1.0) | (0.9, 1.0) | (0.9, 1.0) | (0.8, 1.0) | (1.0, 1.1) | (1.0, 1.2) | (1.0, 1.1) | (0.9, 0.9) | ||||
| Systolic blood pressure (mmHg) | 145.0 | 127.5 | 130.0 | 120.0 | 140.0 | 130.0 | 132.0 | 127.5 | 0.962 | 0.054 | 0.913 |
| (130.0, 150.0) | (115.0, 140.0) | (117.5, 142.5) | (112.5, 130.0) | 127.5, 142.5) | (115.0, 130.0) | (125.0, 139.2) | (121.2, 131.2) | ||||
| Diastolic blood pressure (mmHg) | 80.0 | 80.0 | 75.0 | 80.0 | 80.0 | 80.0 | 79.5 | 85.0 | 0.110 | 0.929 | 0.078 |
| (80.0, 88.8) | (75.0, 90.0) | (72.5, 85.0) | (77.5, 85.0) | (77.5, 80.0) | (70.0, 85.0) | (76.8, 80.0) | (82.5, 85.5) | ||||
| Fasting Blood Glucose (mg/dl) | 111.0 | 119.0 | 105.0 | 109.0 | 103.5 | 105.0 | 109.0 | 134.0 | 0.839 | 0.652 | 0.294 |
| (102.0, 149.5) | (114.0, 125.0) | (94.0, 121.0) | (103.5, 128.0) | (97.0, 107.0) | (104.0, 113.5) | (104.0, 119.0) | (119.8, 146.5) | ||||
| PREDIMED | 8.0 | 8.0 | 8.0 | 8.0 | 9.0 | 10.0 | 7.5 | 8.0 | 0.023 | 0.877 | 0.941 |
| (7.0, 8.8) | (7.0, 9.0) | (6.0, 10.0) | (7.0, 10.0) | (8.5, 10.0) | (9.0, 11.0) | (7.0, 9.0) | (8.0, 9.5) | ||||
BMI: Body Mass Index; WHR: waist-to-hip ratio; PREDIMED: PREvención con DIeta MEDiterránea.
Bolded p-values are significant after FDR correction.
*Effect of time, for each variable; the differences have been tested between the means of the two arms at different follow-up control.
**Effect of group for each variable; the differences have been tested between the means of web arm in four times (baseline, T3, T6 and lockdown) and the means of the traditional arm at the same four times.
***Probability that the effect of time is greater in one distinct arm (interaction time*arm).
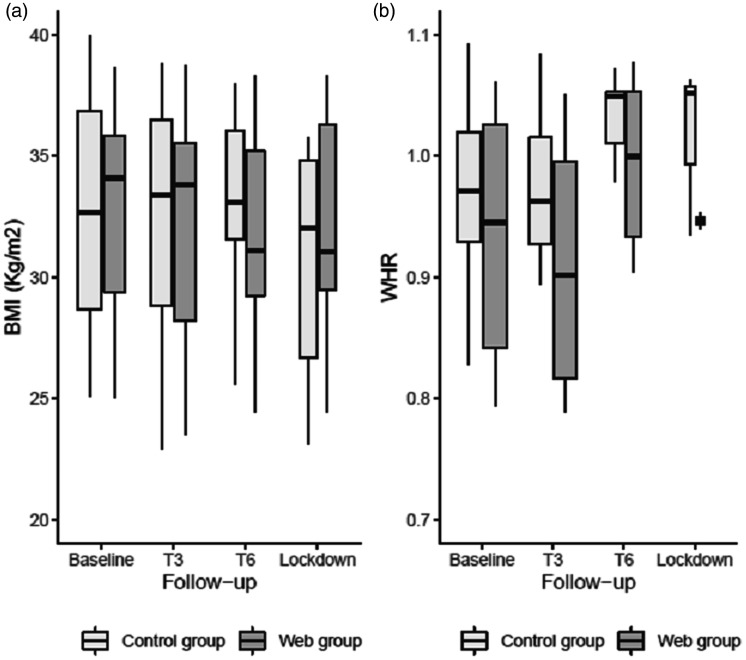
The web arm results showed a progressive weight loss and an improvement of BMI from baseline (weight = 102.5 IQR: 90.1–110.6 and BMI = 35.2 IQR: 30.1–39.8) to T6 (weight = 92.0 IQR: 83.5–105.0 and BMI = 33.4 IQR: 29.7–37.0). In this group, an increase in both parameters was observed between T6 and the lockdown period (weight = 93.0 IQR: 90.0–105.0 and BMI = 33.7 IQR: 30.0–37.3). In the traditional arm, however, weight and BMI values increased between baseline (weight = 95.5 IQR: 82.5–104.0 and BMI = 33.7 IQR: 29.4–37.1) and T6 (weight = 96.5 IQR: 78.8–100.5 and BMI = 34.1 IQR: 31.7–36.9), and decreased during lockdown (weight = 91.2 IQR: 72.8–95.8 and BMI = 32.1 IQR: 26.8–35.3). The comparison of these parameters between arms was not significant during the entire follow-up period; contrariwise, for both arms we observed a statistically significant variation when considering weight and BMI values over time (p < 0.001 and p = 0.001, respectively) (Table 2 and Figure 2). No statistically significant interaction was found between intervention arm and follow-up (p = 0.516 and 0.380, respectively).
Figure 2.
The within- and between-patient variation of Body Mass Index (BMI) (Panel a) and waist-to-hip ratio (WHR) (Panel b) over time (at baseline, after 3 months (T3), after 6 months (T6), at lockdown).
In the web arm, the median WHR decreased between baseline and T3, and between T6 and the lockdown period. In the traditional arm, an increase at T6 and a subsequent stabilization of parameter was shown (Table 2 and Figure 2). The model shows, however, that the variation during the follow-up of WHR is not significant for either arm (Table 2).
No other significant differences were detected for the waist and hip circumference, blood pressure, and fasting blood glucose values.
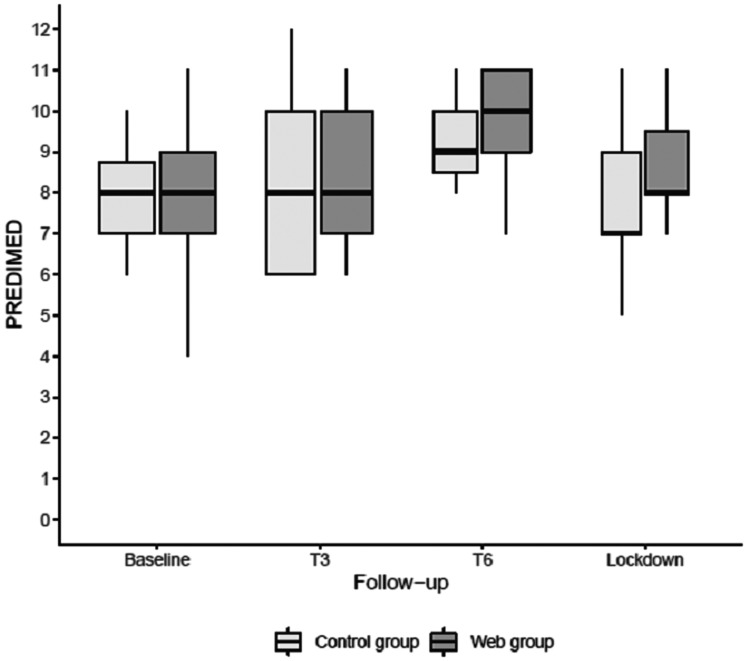
Finally, variation of PREDIMED scores was significant during the entire follow-up period (p = 0.023); this effect is the same in both arms (interaction effect p = 0.941) (Table 2 and Figure 3).
Figure 3.
The within- and between-patient variation of PREDIMED scores over time (at baseline, after 3 months (T3), after 6 months (T6), at lockdown).
In detail, the PREDIMED questionnaire registered an improved median score at T6 compared with baseline in both arms (web 2.5 IQR: 0.2–3.2 vs. traditional 1.0 IQR: 0.2–2.5). Interestingly, in the web arm, the median score of PREDIMED increased from medium (8.0 IQR: 7.0–9.0) to maximum adherence at T6 (10.0 IQR: 9.0–11.0). In the traditional arm PREDIMED improved from baseline to T6, while remaining in the range of medium adherence (8.0 IQR: 7.0–8.8 vs. 9.0 IQR: 8.5–10.0, respectively). These results, however, were not maintained during lockdown in either group (web 8.0 IQR: 8.0–9.5 vs. traditional 7.5 IQR: 7.0–9.0).
Discussion
The incidence of diabetes and obesity is growing rapidly worldwide, and this is due to unhealthy lifestyles and nutritional habits as well as a genetic vulnerability.32 Hence there is a need to promote lifestyle interventions that may favour obesity management and weight loss in overweight or obese T2D people.2
Novel technologies represent promising tools for diabetes management.4 Telemedicine intervention has proven effective in improving BMI in overweight and obese people and in patients with chronic diseases, including diabetes, especially for treatments over 6 months.33 Moreover, a recent review reported an improvement in clinical outcomes in patients with diabetes (especially in recently diagnosed diabetic subjects, age < 55 years, high baseline HbA1c) assisted by telemedicine interventions.34 However, research highlighted the need take into account some aspects required by this approach, such as the need for a patient’s adequate technological/digital literacy, the empowerment process triggered by health education, and the behavioural changes supported by easier interactions with care providers, other patients, and family members.8,13
The pandemic outbreak of COVID-19 has made it necessary, in many countries including Italy, to introduce government policies aimed at social distancing and limiting activities and freedom of movement. It follows that the lockdown period may have impacted negatively on both lifestyle and psychological well-being.35,36
In this scenario, the use of web and new communication technologies has become essential to overcome distance and physical co-presence in most aspects of life, including health.18 The current pandemic has accelerated, in fact, the regular use of telemedicine in clinical practice, without forgetting that routine use by the health system would be desirable.20 Patients affected by conditions such as obesity and diabetes mellitus are at high risk for serious infections and sequelae. Providing them with strategies to foster a healthy lifestyle can be critical.37 To that aim, the Regional Government of Abruzzo approved a document on the implementation of telemedicine in diabetes management during the COVID-19 pandemic.38
In light of these scientific elements, the present study aims to verify the effects of a traditional nutritional intervention versus a web-based one, with a focus on anthropometric and clinical parameters and adherence to the MedDiet, in overweight or obese individuals affected by T2D or IGR before and during the Italian lockdown period in 2020. All participants had already been involved in a nutritional and healthy lifestyle programme before the lockdown.
A free-of-charge web platform was used to integrate face-to-face learning with an online environment. The study was facilitated by our previous research on a possible combination of new technologies with behavioural change theories (i.e. transtheoretical model of change, social cognitive theory, self-determination theory).39–41 Our research showed how the process of change of a single participant, as part of a community, can be favoured by the dynamics of mutual group support and by the reinforcement, even at a distance, of care providers.
Results detected that participants allocated to the web arm achieved a progressive weight loss and an improvement of median BMI until T6 and a minimal increase of weight and BMI between T6 and lockdown. Similarly, a clear improvement of median weight and BMI values compared with baseline was observed during lockdown in the control group, where a traditional approach would have been used.
These data regarding the intervention adopted during the lockdown are even more interesting in light of the results of a recent survey which reported 48.6% perceived weight gain but only 13.9% perceived weight reduction in the Italian population during the COVID-19 pandemic.42 Another Italian study detected a 1.51 kg self-reported weight gain and a 0.58 kg/m2 BMI increase in a sample of outpatients with obesity, after the first month of lockdown.43 Our results observed a significant variation when considering weight and BMI values over time for both arms.
These data are consistent with a recent study that showed a significant weight loss at 6 and 12 months of intervention in patients with T2D involved in a digital lifestyle change programme.44 Its authors concluded that a digital approach could provide a strategy to help people access nutritional advice and weight management support.44 In our study, the improvement of BMI detected in the traditional arm during lockdown is in accordance with a recent study in patients with T2D, which combined tele-monitoring with individual phone coaching for structured lifestyle intervention.45 Results showed, after 3 months, a significant BMI improvement in tele-assisted participants compared with usual care ones, thus confirming the promising potential of this approach in support of patients with T2D.45
BMI is the obesity index that, more than others, is related to the estimated risks for coronary heart disease and stroke in the T2D population based on specific cardiovascular risk calculators, such as the Framingham Risk Score, the UKPDS version 2.0 and the ADVANCE risk engines.46 Interestingly, we observed an improvement in BMI or a stabilization of the parameters when participants were engaged with web-based intervention, thus confirming the potential of this approach.
Regarding the median WHR, we detected a fluctuating trend with a decrease between baseline and T3, an increase between T3 and T6, and a subsequent improvement between T6 and the lockdown period, in the web arm. Contrariwise, an increase at T6 and a subsequent stabilization of the median WHR was found in the traditional arm. Although they are not statistically significant, the positive WHR results of our study seem promising. A recent work has, in fact, demonstrated that overall (BMI) and central (WHR) obesity can represent risk factors for COVID-19 hospitalization.47
Finally, another interesting result concerned the PREDIMED questionnaire. We detected an improvement of scores at T6 versus baseline in both arms; in particular, the web group score rose from a medium to a maximum range of adherence to the MedDiet at T6. During the lockdown period we found a slight worsening of previous scores, albeit more evidently in the web arm. Both groups reached medium adherence scores; the median value was, however, better in the web group participants than in controls. Despite showing a slight deterioration during lockdown, these results are in accordance with the above-mentioned Italian survey which observed that about 60% of the Italian population ranked in the medium adherence score to the MedDiet (7 IQR: 6–9) during the COVID-19 pandemic.42 It is also worth noticing that the survey found a lower score in Central Italy, where our research was conducted, compared with Northern and Southern Italy and the Islands, as well as an inverse correlation between PREDIMED score and BMI. Overweight and obese individuals had, in fact, a lower level of adherence to the MedDiet in comparison to those with normal weight.42 In light of these findings and the emergency scenario described, we hypothesize that the provided web-based intervention enabled participants to keep in touch and stay engaged, thus contributing to avoiding radical and unhealthy lifestyle changes during the lockdown. Self-care and therapeutic compliance could be improved by an individual’s perception of having a healthcare team always available via telemedicine.8
Furthermore, this study showed that internal and external obstacles intervened during the procedure, resulting in non-compliance and withdrawal of some participants from both arms. The lack of motivation or of willpower, busyness, as well as social and family environment and logistic problems were described as possible crucial internal and external hurdles to lifestyle change.48,49 Both internal factors, such as the user’s behaviour and motivation, and external ones, including lack of organizational support and home obstructions, can hinder the realization of healthcare e-consultation services.50
The present study has some limitations, the first being the number of dropouts that occurred during the study. We believe that some of the obstacles encountered by patients, such as difficultly in accessing face-to-face intervention, might be overcome by an entirely web-based approach. Other limitations are the possible inaccuracy of self-measurement of participants’ circumferences during lockdown and the lack of data for some factors such as the patients’ socioeconomic status, social support, and adherence to medical therapy, which impacted on our results.
The unexpected deviation from the original protocol due to the pandemic outbreak might also be considered as a limitation; we believe, however, that it represented a strength and an opportunity. In fact, it allowed for the promotion of technological tools for the remote management of subjects with diabetes. Furthermore, the tools and the multimedia material devised for the project are free and re-usable, with a proven sustainability for the healthcare system; also, the methodological approach adopted offers potential implementation in other types of clinical practice. Finally, by imputing trajectories for the anthropometric variables to assess the effect of missing data on the stability of the results, we observed similar results in the median values compared with those considered for the main analysis.
In conclusion, the study showed the effectiveness and feasibility of a short-term nutritional web-based intervention in patients affected by T2D or IGR before and during the COVID-19 pandemic. The lockdown was an emergency scenario which impacted on the socioeconomic, professional, behavioural, and psychological state of the participants; it also had implications in various aspects of their lives, including lifestyle, nutritional habits, and anthropometric parameters. In this context, found that the provided web-based intervention allowed us to keep in touch with participants and helped them maintain some of the positive results they had previously obtained, which might have otherwise been lost. Although the results of the present study are encouraging, more extensive research with larger sample sizes needs to be conducted to further explore the effectiveness of a nutritional web-based intervention, so as to optimize the provision of outpatient visits.
Acknowledgements
The authors wish to thank Fondazione AMD Onlus for the research support, as well as the patients who participated in the study.
Author contributions
The study was designed by EV and FF. EV contributed to the recruitment of patients, clinical evaluation and data acquisition. FF performed the nutritional intervention and contributed to data acquisition and interpretation. EV and FF enrolled participants, MDN assigned participants to different arms. The manuscript was drafted by EV and FF. MDN was the biostatistician that performed and supervised the statistical analyses and helped in the drafting and editing of the article. All authors were involved in critical revision and approved the final version of the manuscript before submission. EV and MDN are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Declaration of conflicting interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr Fraticelli reports grant from Fondazione Associazione Medici Diabetologi (AMD) Onlus, during the conduct of the study.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by a research grant, given to Federica Fraticelli, from Fondazione Associazione Medici Diabetologi (AMD) Onlus, Italy.
ORCID iDs
Federica Fraticelli https://orcid.org/0000-0002-8169-1864
Ester Vitacolonna https://orcid.org/0000-0003-1756-661X
Supplemental material
Supplemental material for this article is available online.
References
- 1.Chawla R, Jaggi S.Medical management of diabesity. J Assoc Physicians India 2019; 67(12): 52–56. [PubMed] [Google Scholar]
- 2.American Diabetes Association. 8. Obesity management for the treatment of type 2 diabetes: Standards of medical care in diabetes-2020. Diabetes Care 2020; 43(Suppl 1): S89–S97. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO). Telemedicine, Telehealth, and Health Information Technology, https://www.who.int/goe/policies/countries/usa_support_tele.pdf (2006, accessed 13 July 2020).
- 4.Maurizi AR, Piemonte V, Pozzilli P.Diabetes on demand and novel technologies. Diabetes Metab Res Rev 2018; 34(2). [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization (WHO). Telehealth, https://www.who.int/gho/goe/telehealth/en/ (2016, accessed 13 July 2020).
- 6.World Health Organization (WHO). eHealth at WHO, https://www.who.int/ehealth/about/en/ (2018, accessed 13 July 2020).
- 7.Lurie N, Carr BG.The role of telehealth in the medical response to disasters. JAMA Intern Med 2018; 178(6): 745–746. [DOI] [PubMed] [Google Scholar]
- 8.Fantinelli S, Marchetti D, Verrocchio MC, et al. Assessment of psychological dimensions in telemedicine care for gestational diabetes mellitus: A systematic review of qualitative and quantitative studies. Front Psychol 2019; 10: 153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spanakis EG, Santana S, Tsiknakis M, et al. Technology-based innovations to foster personalized healthy lifestyles and well-being: A targeted review. J Med Internet Res 2016; 18(6): e128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Feo P, Fatone C, Burani P, et al. An innovative model for changing the lifestyles of persons with obesity and/or Type 2 diabetes mellitus. J Endocrinol Invest 2011; 34(10): e349–e354. [DOI] [PubMed] [Google Scholar]
- 11.Liss DT, Finch EA, Cooper A, et al. One-year effects of a group-based lifestyle intervention in adults with type 2 diabetes: A randomized encouragement trial. Diabetes Res Clin Pract 2018; 140: 36–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Trento M, Passera P, Borgo E, et al. A 5-year randomized controlled study of learning, problem solving ability, and quality of life modifications in people with type 2 diabetes managed by group care. Diabetes Care 2004; 27(3): 670–675. [DOI] [PubMed] [Google Scholar]
- 13.Wang Y, Xue H, Huang Y, et al. A systematic review of application and effectiveness of mHealth interventions for obesity and diabetes treatment and self-management. Adv Nutr 2017; 8(3): 449–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization (WHO). WHO announces COVID-19 outbreak a pandemic, http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic (2020, accessed 13 July 2020).
- 15.Paterlini M. Lockdown in Italy: Personal stories of doing science during the COVID-19 quarantine. Nature. Online ahead of print 2 April 2020. DOI:10.1038/d41586-020-01001-8. [DOI] [PubMed]
- 16.Lippi G, Henry BM, Bovo C, et al. Health risks and potential remedies during prolonged lockdowns for coronavirus disease 2019 (COVID-19). Diagnosis (Berl )2020; 7(2): 85–90. [DOI] [PubMed] [Google Scholar]
- 17.Luzi L, Radaelli MG.Influenza and obesity: Its odd relationship and the lessons for COVID-19 pandemic. Acta Diabetol 2020; 57(6): 759–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ghosh A, Gupta R, Misra A.Telemedicine for diabetes care in India during COVID19 pandemic and national lockdown period: Guidelines for physicians. Diabetes Metab Syndr 2020; 14(4): 273–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Perrone G, Zerbo S, Bilotta C, et al. Telemedicine during Covid-19 pandemic: Advantage or critical issue? Med Leg J 2020; 88(2): 76–77. [DOI] [PubMed] [Google Scholar]
- 20.Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare 2020; 26(5): 309–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Garg SK, Rodbard D, Hirsch IB, et al. Managing new-onset type 1 diabetes during the COVID-19 pandemic: Challenges and opportunities. Diabetes Technol Ther 2020; 22(6): 431–439. [DOI] [PubMed] [Google Scholar]
- 22.American Diabetes Association. 2. Classification and diagnosis of diabetes: Standards of medical care in diabetes-2020. Diabetes Care 2020. Jan; 43(Suppl 1): S14–S31. [DOI] [PubMed] [Google Scholar]
- 23.Associazione Medici Diabetologi (AMD) - Società Italiana di Diabetologia (SID). Standard Italiani per la cura del diabete mellito 2018, http://www.siditalia.it/pdf/Standard%20di%20Cura%20AMD%20-%20SID%202018_protetto2.pdf (2018, accessed 27 August 2020).
- 24.Nichols GA, Hillier TA, Brown JB.Progression from newly acquired impaired fasting glucose to type 2 diabetes. Diabetes Care 2007; 30(2): 228–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Engberg S, Vistisen D, Lau C, et al. Progression to impaired glucose regulation and diabetes in the population-based Inter99 study. Diabetes Care 2009; 32(4): 606–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martínez-González MA, García-Arellano A, Toledo E, et al. A 14-item Mediterranean diet assessment tool and obesity indexes among high risk subjects: The PREDIMED trial. PLoS One 2012; 7(8): e43134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yu Z, Sealey-Potts C, Rodriguez J.Dietary self-monitoring in weight management: Current evidence on efficacy and adherence. J Acad Nutr Diet 2015; 115(12): 1931–1938. [DOI] [PubMed] [Google Scholar]
- 28.Trento M, Passera P, Tomalino M, et al. Group visits improve metabolic control in type 2 diabetes: A 2-year follow-up. Diabetes Care 2001; 24(6): 995–1000. [DOI] [PubMed] [Google Scholar]
- 29.Trento M, Passera P, Bajardi M, et al. Lifestyle intervention by group care prevents deterioration of type ii diabetes: A 4-year randomized controlled clinical trial. Diabetologia 2002; 45(9): 1231–1239. [DOI] [PubMed] [Google Scholar]
- 30.Rock CL, Flatt SW, Pakiz B, et al. Weight loss, glycemic control, and cardiovascular disease risk factors in response to differential diet composition in a weight loss program in type 2 diabetes: A randomized controlled trial. Diabetes Care 2014; 37(6): 1573–1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/, (accessed 13 July 2020).
- 32.Kumar N, Puri N, Marotta F, et al. Diabesity: An epidemic with its causes, prevention and control with special focus on dietary regime. Funct Foods Health Dis 2017; 7(1): 1–16. [Google Scholar]
- 33.Huang JW, Lin YY, Wu NY.The effectiveness of telemedicine on body mass index: A systematic review and meta-analysis. J Telemed Telecare 2019; 25(7): 389–401. [DOI] [PubMed] [Google Scholar]
- 34.Timpel P, Oswald S, Schwarz PEH, et al. Mapping the evidence on the effectiveness of telemedicine interventions in diabetes, dyslipidemia, and hypertension: An umbrella review of systematic reviews and meta-analyses. J Med Internet Res 2020; 22(3): e16791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Balanzá-Martínez V, Atienza-Carbonell B, Kapczinski F, et al. Lifestyle behaviours during the COVID-19 – time to connect. Acta Psychiatr Scand 2020; 141(5): 399–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roy D, Tripathy S, Kar SK, et al. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J Psychiatr 2020; 51: 102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yang YC, Chou CL, Kao CL. Exercise, nutrition, and medication considerations in the light of the COVID pandemic, with specific focus on geriatric population: A literature review. J Chin Med Assoc. 2020; Aug 17. DOI:10.1097/JCMA.0000000000000393. [DOI] [PMC free article] [PubMed]
- 38.Regione Abruzzo. O.P.G.R. n. 34 del 10.04.2020. Misure urgenti regionali durante l'emergenza COVID-19. Telemedicina applicata al diabete, http://www.regione.abruzzo.it/content/opgr-n-34-del-10042020 (2020, accessed 13 July 2020).
- 39.Marchetti D, Fraticelli F, Polcini F, et al. Preventing adolescents’ diabesity: Design, development, and first evaluation of “Gustavo in Gnam’s Planet”. Games Health J 2015; 4(5): 344–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fraticelli F, Marchetti D, Polcini F, et al. Technology-based intervention for healthy lifestyle promotion in Italian adolescents. Ann Ist Super Sanita 2016; 52(1): 123–127. [DOI] [PubMed] [Google Scholar]
- 41.Marchetti D, Fraticelli F, Polcini F, et al. A school educational intervention based on a serious game to promote a healthy lifestyle. MJCP 2018; 6(3): 1–16. [Google Scholar]
- 42.Di Renzo L, Gualtieri P, Pivari F, et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J Transl Med 2020; 18(1): 229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pellegrini M, Ponzo V, Rosato R, et al. Changes in weight and nutritional habits in adults with obesity during the “lockdown” period caused by the COVID-19 virus emergency. Nutrients 2020; 12(7): 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Idris I, Hampton J, Moncrieff F, et al. Effectiveness of a digital lifestyle change program in obese and type 2 diabetes populations: Service evaluation of real-world data. JMIR Diabetes 2020; 5(1): e15189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.von Storch K, Graaf E, Wunderlich M, et al. Telemedicine-assisted self-management program for type 2 diabetes patients. Diabetes Technol Ther 2019; 21(9): 514–521. [DOI] [PubMed] [Google Scholar]
- 46.Markova A, Boyanov M, Bakalov D, et al. Body composition indices and cardiovascular risk in type 2 diabetes. CV biomarkers are not related to body composition. Open Med (Wars) 2020; 15: 309–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hamer M, Gale CR, Kivimäki M, et al. Overweight, obesity, and risk of hospitalization for COVID-19: A community-based cohort study of adults in the United Kingdom. Proc Natl Acad Sci USA 2020; 117(35): 21011–21013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Stone NJ, Saxon D.Approach to treatment of the patient with metabolic syndrome: Lifestyle therapy. Am J Cardiol 2005; 96(4A): 15E–21E. [DOI] [PubMed] [Google Scholar]
- 49.Ziebland S, Thorogood M, Yudkin P, et al. Lack of willpower or lack of wherewithal? “Internal” and “external” barriers to changing diet and exercise in a three year follow-up of participants in a health check. Soc Sci Med 1998; 46(4–5): 461–465. [DOI] [PubMed] [Google Scholar]
- 50.Almathami HKY, Win KT, Vlahu-Gjorgievska E.Barriers and facilitators that influence telemedicine-based, real-time, online consultation at patients' homes: Systematic literature review. J Med Internet Res 2020; 22(2): e16407. [DOI] [PMC free article] [PubMed] [Google Scholar]