Abstract
Background
To compare the sensory change and recovery of infraorbital area associated with zygomaticomaxillary and orbital floor fractures and their recoveries and investigate the factors that affect them.
Methods
We retrospectively reviewed 652 patients diagnosed with zygomaticomaxillary (n=430) or orbital floor (n=222) fractures in a single center between January 2016 and January 2021. Patient data, including age, sex, medical history, injury mechanism, Knight and North classification (in zygomaticomaxillary fracture cases), injury indication for surgery (in orbital floor cases), combined injury, sensory change, and recovery period, were reviewed. The chi-square test was used for statistical analysis.
Results
Orbital floor fractures occurred more frequently in younger patients than zygomaticomaxillary fractures (p<0.001). High-energy injuries were more likely to be associated with zygomaticomaxillary fractures (p<0.001), whereas low-energy injuries were more likely to be associated with orbital floor fractures (p<0.001). The sensory changes associated with orbital floor and zygomaticomaxillary fractures were not significantly different (p=0.773). Sensory recovery was more rapid and better after orbital floor than after zygomaticomaxillary fractures; however, the difference was not significantly different. Additionally, the low-energy group showed a higher incidence of sensory changes than the high-energy group, but the difference was not statistically significant (p=0.512). Permanent sensory changes were more frequent in the high-energy group, the difference was statistically significant (p=0.043).
Conclusion
The study found no significant difference in the incidence of sensory changes associated with orbital floor and zygomaticomaxillary fractures. In case of orbital floor fractures and high-energy injuries, the risk of permanent sensory impairment should be considered.
Keywords: Maxillary fractures, Orbital fractures, Zygoma, Zygomatic fractures
INTRODUCTION
Facial bone fracture patients suffer various symptoms. Symptoms such as pain, tenderness, and mouth-opening limitations improve soon after open reduction. However, facial sensory changes in areas innervated by the infraorbital nerve have prolonged recovery; these sensory changes include hypoesthesia, dysesthesia, paresthesia, and anesthesia of the upper lip, cheek, lower eyelid, and ala of the nose. The incidences of these symptoms are 30% to 80% of all zygomatic fractures and 31% to 50% of orbital floor fractures [1–9]. Infraorbital nerve originates from the maxillary nerve, a branch of the trigeminal nerve, that runs along the inferior orbital fissure to reach the orbital cavity, and then passes through the infraorbital canal to come out of the infraorbital foramen and reaches the face [10]. Clinically, sensory changes after a mid-facial fracture are frequent; unlike bone union ending in 3 to 4 weeks, sensory changes last for up to a year, causing inconvenience to patients [11]. There are several studies on infraorbital nerve disturbances associated with zygomaticomaxillary and orbital floor fractures. However, only a few of them compare the incidence of sensory changes between zygomaticomaxillary and orbital floor fractures. In this study, we compared the differences in sensory changes related to basic patient characteristics such as age, sex, and injury mechanism. In addition, we compared the sensory change and recovery of infraorbital area associated with zygomaticomaxillary and orbital floor fractures.
METHODS
We reviewed the computed tomography (CT) image data of patients diagnosed of zygomaticomaxillary or orbital floor fractures in a single center between January 2016 and January 2021. The patients diagnosed of zygomaticomaxillary or orbital floor fractures who did not present for follow-up in Wonju Severance Christian Hospital, patients younger than 18 years, patients whose sensory changes could not be evaluated (e.g., loss of consciousness), and patients with open fractures with mechanical infraorbital nerve transection were excluded from this study. Zygomaticomaxillary fractures of Knight and North classification type 2 are pure zygomatic arch fractures, and they were excluded from this study because they did present with sensory changes. A total of 652 patients with 430 zygomaticomaxillary fractures and 222 orbital floor fractures were evaluated retrospectively.
The evaluated variables were as follows: age, sex, hypertension, diabetes mellitus, injury mechanism, Knight and North classification (in zygomaticomaxillary fracture cases), injury indicated for surgery (in orbital floor cases), combined injury, sensory changes, and recovery period. The injury mechanisms were categorized as follows: traffic accidents, falls, motorcycle accidents, slips, assault, sports injuries, syncope, and others. The injury mechanisms were generally classified into the high-energy (traffic accident, fall-down injury, and motorcycle accident) and low-energy (slip-down injury, assault, sports injury, syncope, and others) groups [12]. For orbital floor fractures, the indications for surgery were as follows: (1) limitation of eye movement with muscle incarceration; (2) fracture area of >1 cm2 or >50% of the orbital floor; and (3) >2 mm of enophthalmos [13]. All surgery was performed within 2 weeks of injury when the better outcomes and fewer postoperative complications were expected [14].
The sensory changes were evaluated as two-point subjective infraorbital sensory changes and divided into hyperesthesia and hypoesthesia. Sensory change evaluation was conducted every 6 months until 24 months. A permanent sensory change, by definition, did not recover within 24 months. The 24 months follow-up permitted time for neural regeneration that may exceed 6 months postinjury [15].
The chi-square test was used to compare the groups, and p-values of <0.05 denoted statistical significance. All data were analyzed with SPSS version 23.0 (IBM Corp., Armonk, NY, USA).
RESULTS
Baseline characteristics of patients with orbital floor and zygomaticomaxillary fractures
Orbital floor fractures occurred more frequently in younger patients than zygomaticomaxillary fractures (41.6±16.8 vs. 49.9±18.4, p<0.001). In addition, the fracture type may depend on the injury mechanism: high- versus low-energy injuries. High-energy injuries were more likely to be associated with zygomaticomaxillary fractures (27.0% vs. 44.0%, p<0.001), while low-energy injuries were more likely to be associated with orbital floor fractures (73.0% vs. 56.0%, p<0.001). Regarding co-injuries, zygomaticomaxillary fractures were more likely to be accompanied by musculoskeletal injuries (11.3% vs. 17.9%, p<0.027) (Table 1).
Table 1.
Patient characteristics
| Variable | Total (n=652) | Orbital floor (n=222) | Zygomaticomaxillary (n=430) | p-valuea) |
|---|---|---|---|---|
| Age | 41.0±18.3 | 41.6±16.8 | 49.9±18.4 | <0.001 |
|
| ||||
| Female sex | 151 (23.2) | 51 (23.0) | 100 (23.3) | 0.935 |
|
| ||||
| Hypertension | 92 (14.1) | 26 (11.7) | 66 (15.3) | 0.206 |
|
| ||||
| Diabetes mellitus | 40 (6.1) | 14 (6.3) | 26 (6.0) | 0.896 |
|
| ||||
| Mechanism | <0.001 | |||
| Traffic accident | 132 (20.2) | 37 (16.7) | 95 (22.1) | |
| Fall-down injury | 78 (12.0) | 16 (7.2) | 62 (14.4) | |
| Motorcycle accident | 40 (6.1) | 7 (3.2) | 33 (7.7) | |
| Slip-down injury | 122 (18.7) | 42 (18.9) | 80 (18.6) | |
| Assault | 115 (17.6) | 71 (32.0) | 44 (10.2) | |
| Sports injury | 71 (10.9) | 29 (13.1) | 42 (9.8) | |
| Syncope | 49 (7.5) | 7 (3.2) | 42 (9.8) | |
| Others | 45 (6.9) | 13 (5.9) | 32 (7.4) | |
|
| ||||
| Energy of injury | <0.001 | |||
| Low energy | 403 (61.8) | 162 (73.0) | 241 (56.0) | |
| High energy | 249 (38.2) | 60 (27.0) | 189 (44.0) | |
|
| ||||
| Co-injury | 272 (41.7) | 74 (33.3) | 198 (46.1) | |
| Musculoskeletal | 102 (15.7) | 25 (11.3) | 77 (17.9) | 0.027 |
| Internal organ | 15 (2.3) | 2 (0.9) | 13 (3.0) | 0.087 |
| Others | 155 (23.8) | 47 (21.2) | 108 (25.2) | 0.262 |
Values are presented as the mean±SD or number (%).
Chi-square test.
Sensory changes and their recoveries in the two fracture groups
The prevalence of sensory changes associated with orbital floor and zygomaticomaxillary fractures were not significantly different (16.2% vs. 15.2%, p=0.773). Zygomaticomaxillary fractures were associated with a higher incidence of hypoesthesia than orbital floor fractures, but the difference was not statistically significant (13.3% vs. 11.7%, p=0.575) (Table 2).
Table 2.
Infraorbital nerve disturbance associated with orbital and zygomaticomaxillary fractures
| Variable | Orbital floor (n=222) | Zygomaticomaxillary (n=430) | p-valuea) |
|---|---|---|---|
| Sensory change | 36 (16.2) | 66 (15.2) | 0.773 |
| Hyperesthesia | 10 (4.5) | 9 (2.1) | 0.083 |
| Hypoesthesia | 26 (11.7) | 57 (13.3) | 0.575 |
|
| |||
| Permanent sensory change | 3 (1.4) | 13 (3.0) | 0.191 |
Values are presented as the number (%).
Chi-square test.
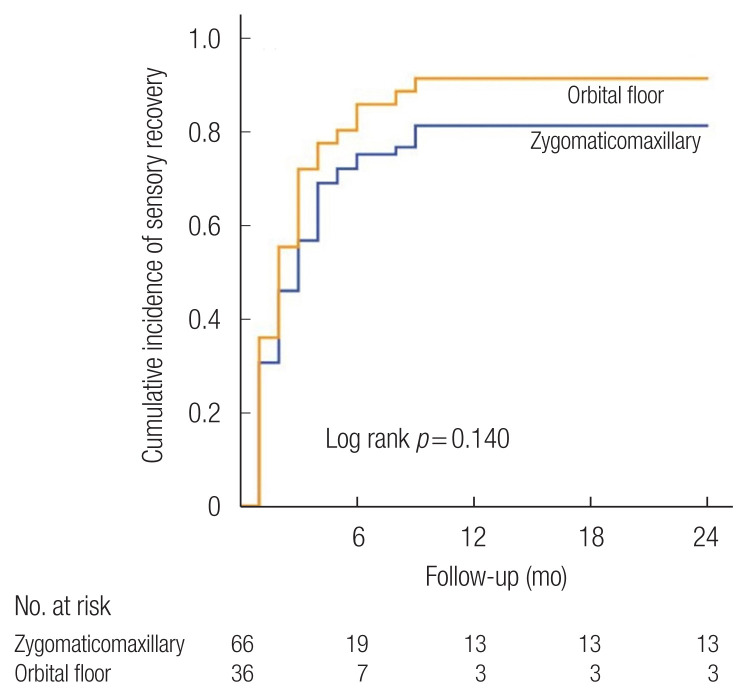
Sensory recovery was more rapid, and the overall sensory recovery was better, in the orbital floor than in the zygomaticomaxillary fracture group. However, the difference was not statistically significant (6 months recovery rate 80.6% vs. 71.2%, 12 months recovery rate 91.7% vs. 80.3%, p=0.140) (Fig. 1). Of the total of 652 patients, 16 did not have sensory recovery as of 24 months. Of the patients with sensory recovery, none recovered after 12 months.
Fig. 1.
Cumulative incidence of sensory recovery after zygomaticomaxillary and orbital floor fractures.
Sensory changes and recovery stratified by injury mechanism
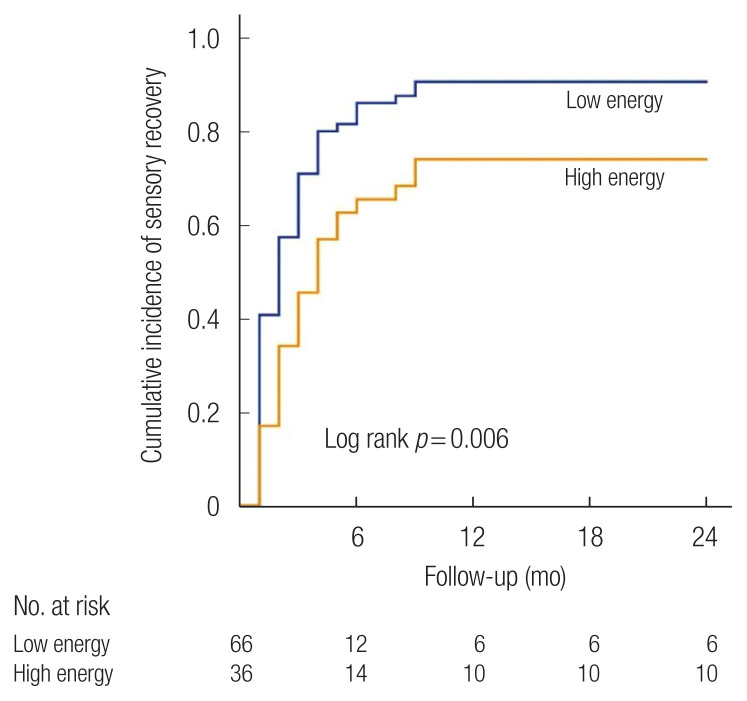
The low-energy group had a higher incidence of sensory changes than the high-energy group, but the difference was not statistically significant (16.4% vs. 14.5%, p=0.512). However, permanent sensory changes were more incident in the high-energy group than in the low-energy group, and the difference was statistically significant (1.5% vs. 4.0%, p=0.043) (Table 3).
Table 3.
Infraorbital nerve disturbance associated with low/high energy injuries
| Variable | Low energy (n=403) | High energy (n=249) | p-valuea) |
|---|---|---|---|
| Sensory change | 66 (16.4) | 36 (14.5) | 0.512 |
| Hyperesthesia | 12 (3.0) | 7 (2.8) | 0.902 |
| Hypoesthesia | 54 (13.4) | 29 (11.6) | 0.514 |
|
| |||
| Permanent sensory change | 6 (1.5) | 10 (4.0) | 0.043 |
Values are presented as the number (%).
Chi-square test.
Sensory recovery was more rapid, and better overall in the low-energy than in the high-energy group; the difference was statistically significant (6 months recovery rate 81.8% vs. 61.1%, 12 months recovery rate 90.9% vs. 72.2%, p=0.006) (Fig. 2).
Fig. 2.
Cumulative incidence of sensory recovery after low- and high-energy injuries.
Sensory changes and recovery stratified by the fracture subgroups
For zygomaticomaxillary fractures, the incidence of sensory changes and permanent sensory changes were evaluated using the Knight and North classification. The sensory changes and permanent sensory changes were not significantly different across the Knight and North classification (Table 4). For orbital floor fractures, the incidence of sensory changes and permanent sensory changes were evaluated based on their association with injuries indicated for surgery.
Table 4.
Infraorbital nerve dysfunction associated with zygomaticomaxillary fractures of the Knight and North classification
| Variable | Type of fracture | p-valueb) | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| 1 (n=176) | 2a) | 3 (n=104) | 4 (n=50) | 5 (n=29) | 6 (n=71) | ||
| Sensory change | 25 (14.2) | 12 (11.5) | 11 (22.0) | 8 (27.6) | 10 (14.1) | 0.167 | |
| Hyperesthesia | 4 (2.3) | 2 (1.9) | 1 (2.0) | 0 | 2 (2.8) | 0.932 | |
| Hypoesthesia | 21 (11.9) | 10 (9.6) | 10 (20.0) | 8 (27.6) | 8 (11.3) | 0.064 | |
|
| |||||||
| Permanent sensory change | 3 (1.7) | 3 (2.9) | 2 (4.0) | 2 (6.9) | 3 (4.2) | 0.550 | |
Values are presented as the number (%).
Type 2 fractures were excluded in this study;
Chi-square test.
Sensory changes were more prevalent in the group with injuries with indications for surgery than in the group with injuries without indications for surgery, with the difference being statistically significant (27.3% vs. 5.4%, p<0.001). Hypoesthesia was also significantly more prevalent in the injury group with than without indications for surgery (20.9% vs. 2.7%, p<0.001) (Table 5). Permanent sensory changes were only observed in the injury group with indications for surgery (2.7%).
Table 5.
Infraorbital nerve dysfunction associated with orbital floor fracture after injuries with indications for surgery
| Variable | Surgical indication (n=110) | Non-indication (n=112) | p-valuea) |
|---|---|---|---|
| Sensory change | 30 (27.3) | 6 (5.4) | <0.001 |
| Hyperesthesia | 7 (6.4) | 3 (2.7) | 0.186 |
| Hypoesthesia | 23 (20.9) | 3 (2.7) | <0.001 |
|
| |||
| Permanent sensory change | 3 (2.7) | 0 | 0.078 |
Values are presented as the number (%).
Chi-square test.
DISCUSSION
Sensory changes are frequent sequelae of zygomaticomaxillary and orbital floor fractures, which may affect the infraorbital nerve. The infraorbital nerve is often involved in trauma at the site of the infraorbital fissure, canal, or foramen, such as zygomaticomaxillary and orbital floor fractures, and can be damaged by blunt trauma or bony compression at the fracture site. Sensory changes are more frequently associated with displaced than non-displaced fractures [16], and the duration of recovery depend on several factors, including injury mechanism and method of treatment [17,18]. Therefore, physical examination at the time of injury and explaining the prognosis and course to the patient is important for the treatment of zygomaticomaxillary or orbital floor fractures. The authors investigated the prevalence and recovery of sensory changes associated with zygomaticomaxillary and orbital floor fractures and differences in the frequency and severity of sensory damage associated with pure orbital floor fractures, which have relatively minor damage, compared with zygomaticomaxillary fractures.
In this study, we reviewed the CT image data of patients diagnosed with zygomaticomaxillary or orbital floor fractures. CT is considered gold standard for evaluating fracture status and postoperative outcomes [19]. There were differences between the baseline characteristics of the orbital floor and zygomaticomaxillary fracture groups. First, orbital floor fractures occurred at younger ages than zygomaticomaxillary fractures. Second, the mechanisms underlying the injuries associated with the two categories of fractures differed. The zygomaticomaxillary fracture group had more high-energy injuries (traffic accident, fall-down injury, motorcycle accident), and the orbital floor group had more low-energy injuries (slip, assault, sports injury, and syncope). Considering these two results, the average age of occurrence for orbital floor fractures (mean 41.6 years) was significantly lower than that for the zygomaticomaxillary fractures (mean 49.9 years). Orbital floor fractures are also more frequently associated with low-energy trauma (73%), such as assault and sports injury, which are assumed to be related to physical activity. Zygomaticomaxillary fractures are more frequently associated with high-energy injuries (44%), such as traffic accidents, motorcycle accidents, and falls, than orbital floor fractures (27%). Zygomaticomaxillary fractures are also more frequently accompanied by musculoskeletal injuries (17.9%) than orbital floor fractures (11.3%). Based on these results, we could conclude that zygomaticomaxillary fractures are more frequently high-energy fractures than orbital floor fractures. These findings are similar to those of a previous study, which reported that 1,142 patients with motor vehicle accidents, work-related injuries, fall-related injuries, and maxillofacial bone fractures have a higher prevalence of combined injuries [20].
Montovani et al. [21] reported in their study that zygomaticomaxillary fractures (76.8%) are more frequent in men than orbital floor fractures (23.2%). They attributed this to the predominance of males in driving, drinking alcohol, and sports, which are more associated with zygomaticomaxillary fracture-related injuries. However, our study showed no gender-related differences between the two types of fractures. We supposed that facial bone fractures were more frequent during the active ages and more active males.
A comparison of the sensory changes in the two groups showed no statistically significant difference in incidence. In planning this study, we expected the zygomaticomaxillary fracture group to have a higher incidence of sensory changes and a longer duration of recovery. However, the incidence of sensory changes was not significantly different in the orbital floor and zygomaticomaxillary fracture groups (16.2% vs. 15.2%, p= 0.773). Zygomaticomaxillary fractures were associated with a higher incidence of hypoesthesia than orbital floor fractures, but the difference was not statistically significant (13.3% vs. 11.7%, p=0.575). Sensory recovery was more rapid and better in the orbital floor fracture group than in the zygomaticomaxillary fracture group, but the difference was not statistically significant. Oh et al. [22] revealed that sensory recovery associated with orbital floor fractures was more rapid than that associated with zygomaticomaxillary fractures in their study of 63 patients. Homer evaluated sensory recovery after orbital floor and zygomaticomaxillary fractures in 42 patients, and they also reported that infraorbital nerve dysfunction associated with zygomaticomaxillary fractures was associated with longer sensory recovery than that associated with orbital floor fractures [5]. However, in this study of 652 patients, we could not find significant differences in the incidence and recovery of sensory changes after orbital floor and zygomaticomaxillary fractures. From this result, we concluded that the fracture type did not have a significant impact on the incidence and recovery of sensory changes.
Hilaire et al. [23] evaluated the distributions of bone fractures associated with high-energy and low-energy injuries across the upper, middle, and lower faces of 113 patients, and they found that mid-facial fractures were most prevalent. Other types of fractures such as LeFort and multiple facial fractures, were also found to be similar. In our study, the incidence of sensory changes was not significantly different in the low- and high-energy injury groups. However, permanent sensory changes were more incident in the high-energy injury group and the difference was significant (1.5% vs. 4.0%, p=0.043).
As a result, this study indicated that there was no significant difference in the incidence of sensory changes and subsequent permanent sensory change in the patients with zygomaticomaxillary and orbital floor fractures. When the injury mechanism was considered, the prevalence of permanent sensory change increased in the high-energy injury group, which means that the intensity of damage can predict permanent sensory damage rather than the location of damage to the infraorbital nerve. Based on these results, we concluded that the mechanism of injury was associated with the incidence and prognosis of sensory changes than the classification of fractures, such as zygomaticomaxillary and orbital floor fractures. In addition, the risk of permanent sensory changes should be assessed based on the mechanisms of the fractures.
We evaluated the sensory changes based on the Knight and North classification in the zygomaticomaxillary fracture group because the classification is based on the rotation of the zygoma body. We supposed that nerve injury could change in the direction of rotation of the zygoma body with distraction or compression injury. However, this study showed no differences between sensory disturbance and recovery related to the classification. Oh et al. [22] assumed in their study that the Knight and North classification was only based on the direction of rotation, it was not an indicator of the severity of a fracture, and it could not affect the sensory change incidence and recovery. We expected differences in the sensory disturbance depending on the direction of the rotation of the zygoma; however, based on our study results, we concluded that this classification had no significant effect on the incidence and recovery of infraorbital nerve disturbance.
For orbital floor fractures, injuries with indications for surgery were associated with a higher incidence of sensory changes and permanent sensory changes than those without indications of surgery. This is probably because more extensive fractures were associated with worse damage to the nerve. For patients with injuries with indications for surgery, it is necessary to assess for sensory changes before surgery and educate patients on prognosis.
In this study, the incidence of permanent sensory changes was similar to that reported in a previous study [24]. Of the 652 patients in this study, 16 (2.45%) had sensory changes 24 months after the injury. All the patients who did not have sensory recovery until 12 months after trauma showed sensory disturbance within 24 months after injury. Based on this, we cautiously concluded that the patients who did not have recovery of the sensory changes until 12 months after trauma could not be expected to recover.
This study has several limitations. The study was retrospective in nature. In addition, evaluation of sensory change was subjective.
The strengths of this study are as follows. It was a comparative study with a larger sample than previous studies. In addition, the study compared the sensory changes based on age, sex, injury mechanism, and the type of fractures.
There was no significant difference in the incidence of sensory changes in patients with zygomaticomaxillary and orbital floor fractures. The orbital floor group demonstrated a shorter sensory recovery period and a lower incidence of permanent sensory changes than the zygomaticomaxillary fracture group, but there was no statistically significant difference. Therefore, in case of orbital floor fracture the risk of permanent sensory impairment should be considered, especially for cases with indications for surgery. Furthermore, since the mechanism of a fracture, rather than the type (orbital floor fracture and zygomaticomaxillary fracture), affects sensory changes and their prognosis, clinicians should pay attention to the risk of permanent sensory impairment associated with high-energy injuries.
Abbreviation
- CT
computed tomography
Footnotes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Institutional Review Board of Wonju Severance Christian Hospital (IRB No. CR321064) and performed in accordance with the principles of the Declaration of Helsinki. The informed consent was waived because this study design is a retrospective chart review.
Author contributions
Conceptualization: Jiye Kim. Data curation: Sung Hwa Kim, Dae Ryong Kang. Formal analysis: Jiye Kim. Methodology: Sung Hwa Kim, Dae Ryong Kang, Jiye Kim. Project administration: Sug Won Kim. Writing - original draft: Sug Won Kim, Jeong Ho Kim, Jiye Kim. Writing - review & editing: Jeong Ho Kim, Sug Won Kim, Jiye Kim. Investigation: Sang Woo Han. Supervision: Sug Won Kim, Jiye Kim.
REFERENCES
- 1.Kearney AM, Shah N, Zins J, Gosain AK. Fifteen-year review of the American Board of Plastic Surgery maintenance of certification tracer data: clinical practice patterns and evidence-based medicine in zygomatico-orbital fractures. Plast Reconstr Surg. 2021;147:967e–975e. doi: 10.1097/PRS.0000000000007955. [DOI] [PubMed] [Google Scholar]
- 2.Sargent LA, Fernandez JG. Incidence and management of zygomatic fractures at a level I trauma center. Ann Plast Surg. 2012;68:472–6. doi: 10.1097/SAP.0b013e31823d2c6b. [DOI] [PubMed] [Google Scholar]
- 3.Nordgaard JO. Persistent sensory disturbances and diplopia following fractures of the zygoma. Arch Otolaryngol. 1976;102:80–2. doi: 10.1001/archotol.1976.00780070058004. [DOI] [PubMed] [Google Scholar]
- 4.Hollier LH, Thornton J, Pazmino P, Stal S. The management of orbitozygomatic fractures. Plast Reconstr Surg. 2003;111:2386–92. doi: 10.1097/01.PRS.0000061010.42215.23. [DOI] [PubMed] [Google Scholar]
- 5.Homer N, Glass LR, Lee NG, Lefebvre DR, Sutula FC, Freitag SK, et al. Assessment of infraorbital hypesthesia following orbital floor and zygomaticomaxillary complex fractures using a novel sensory grading system. Ophthalmic Plast Reconstr Surg. 2019;35:53–5. doi: 10.1097/IOP.0000000000001162. [DOI] [PubMed] [Google Scholar]
- 6.Bartoli D, Fadda MT, Battisti A, Cassoni A, Pagnoni M, Riccardi E, et al. Retrospective analysis of 301 patients with orbital floor fracture. J Craniomaxillofac Surg. 2015;43:244–7. doi: 10.1016/j.jcms.2014.11.015. [DOI] [PubMed] [Google Scholar]
- 7.Gas C, Sidjilani BM, Dodart L, Boutault F. Isolated fractures of the orbital floor: conclusions of a retrospective study of 85 cases. Rev Stomatol Chir Maxillofac. 1999;100:27–33. [PubMed] [Google Scholar]
- 8.Westermark A, Jensen J, Sindet-Pedersen S. Zygomatic fractures and infraorbital nerve disturbances. Miniplate osteosynthesis vs. other treatment modalities. Oral Surg Oral Diagn. 1992;3:27–30. [PubMed] [Google Scholar]
- 9.Peltomaa J, Rihkanen H. Infraorbital nerve recovery after minimally dislocated facial fractures. Eur Arch Otorhinolaryngol. 2000;257:449–52. doi: 10.1007/s004050000264. [DOI] [PubMed] [Google Scholar]
- 10.Nam Y, Bahk S, Eo S. Anatomical study of the infraorbital nerve and surrounding structures for the surgery of orbital floor fractures. J Craniofac Surg. 2017;28:1099–104. doi: 10.1097/SCS.0000000000003416. [DOI] [PubMed] [Google Scholar]
- 11.Lee SY, Kim SH, Hwang JH, Kim KS. Sensory recovery after infraorbital nerve avulsion injury. Arch Craniofac Surg. 2020;21:244–8. doi: 10.7181/acfs.2020.00290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Christensen J, Sawatari Y, Peleg M. High-energy traumatic maxillofacial injury. J Craniofac Surg. 2015;26:1487–91. doi: 10.1097/SCS.0000000000001789. [DOI] [PubMed] [Google Scholar]
- 13.Boyette JR, Pemberton JD, Bonilla-Velez J. Management of orbital fractures: challenges and solutions. Clin Ophthalmol. 2015;9:2127–37. doi: 10.2147/OPTH.S80463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee YJ. Orbital floor fracture repair with implants: a retrospective study. Arch Craniofac Surg. 2021;22:177–82. doi: 10.7181/acfs.2020.00640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Das AK, Bandopadhyay M, Chattopadhyay A, Biswas S, Saha A, Balkrishna UM, et al. Clinical evaluation of neurosensory changes in the infraorbital nerve following surgical management of zygomatico-maxillary complex fractures. J Clin Diagn Res. 2015;9:ZC54–8. doi: 10.7860/JCDR/2015/16511.7008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ellis E. Fractures of the zygomatic complex and arch. In: Fonseca RJ, Walker RV, Betts NJ, Barber HD, editors. Oral and maxillofacial trauma. 2nd ed. Philadelphia: W.B. Saunders; 1997. pp. 571–632. [Google Scholar]
- 17.De Man K, Bax WA. The influence of the mode of treatment of zygomatic bone fractures on the healing process of the infraorbital nerve. Br J Oral Maxillofac Surg. 1988;26:419–25. doi: 10.1016/0266-4356(88)90095-2. [DOI] [PubMed] [Google Scholar]
- 18.Kristensen S, Tveteras K. Zygomatic fractures: classification and complications. Clin Otolaryngol Allied Sci. 1986;11:123–9. doi: 10.1111/j.1365-2273.1986.tb00117.x. [DOI] [PubMed] [Google Scholar]
- 19.Moon SJ, Lee WJ, Roh TS, Baek W. Sex-related and racial variations in orbital floor anatomy. Arch Craniofac Surg. 2020;21:219–24. doi: 10.7181/acfs.2020.00143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kostakis G, Stathopoulos P, Dais P, Gkinis G, Igoumenakis D, Mezitis M, et al. An epidemiologic analysis of 1,142 maxillofacial fractures and concomitant injuries. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114(5 Suppl):S69–73. doi: 10.1016/j.tripleo.2011.08.029. [DOI] [PubMed] [Google Scholar]
- 21.Montovani JC, de Campos LM, Gomes MA, de Moraes VR, Ferreira FD, Nogueira EA. Etiology and incidence facial fractures in children and adults. Braz J Otorhinolaryngol. 2006;72:235–41. doi: 10.1016/S1808-8694(15)30061-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oh D, Yun T, Kim J, Choi J, Jeong W, Chu H, et al. The measurement of the sensory recovery period in Zygoma and blow-out fractures with neurometer current perception threshold. Arch Plast Surg. 2016;43:411–7. doi: 10.5999/aps.2016.43.5.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hilaire CS, Johnson A, Loseth C, Alipour H, Faunce N, Kaminski S, et al. Facial fractures and associated injuries in high- versus low-energy trauma: all are not created equal. Maxillofac Plast Reconstr Surg. 2020;42:22. doi: 10.1186/s40902-020-00264-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cai EZ, Koh YP, Hing EC, Low JR, Shen JY, Wong HC, et al. Computer-assisted navigational surgery improves outcomes in orbital reconstructive surgery. J Craniofac Surg. 2012;23:1567–73. doi: 10.1097/SCS.0b013e318260ef33. [DOI] [PubMed] [Google Scholar]