Abstract
Background
Hemorrhoids are a common benign disorder that can require surgery for treatment. Aluminum potassium sulfate and tannic acid (ALTA) have been used as a sclerotherapy agent that induces noninvasive sclerosis and regression of hemorrhoids without surgery. However, there is no objective index for determining its effectiveness. In this study, we prospectively investigated the usefulness of our method as an objective indicator of the effectiveness of ALTA sclerotherapy.
Methods
From April 2015 to April 2019, 241 patients underwent ALTA sclerotherapy. We standardized a simple evaluation method using the lumen of the lower rectum as observed through a clear plastic proctoscope. Patients’ hemorrhoids were evaluated preoperatively and their subjective satisfaction with treatment by our new method was evaluated on postoperative day 7.
Results
Our method showed that among patients who lost the rectal lumen before treatment, the lumen was reacquired after ALTA sclerotherapy in 96.1% (224/233). McNemar test showed the effect of ALTA sclerotherapy to be significantly associated with lumen gain [κ value, 0.0027; 95% confidence interval (CI): 0.0001–0.0052], P<0.001]. Patients’ subjective satisfaction with the treatment was significantly higher in the group reacquiring the lumen (Fisher’s exact test, P=0.0186). Among those patients needing re-treatment, 59.4% (19/32) had lost their lumen during follow-up [mean difference, 0.578; standard deviation (SD): 0.502, P<0.001].
Conclusions
Our simple method using a clear plastic proctoscope could objectively indicate the effect of ALTA sclerotherapy and patients who needed re-treatment on losing their lumen during follow-up. We believe this method is highly advantageous for patients, can advocate the concept of the hemorrhoid shrinking sign, and will contribute to the development of new indication criteria for ALTA sclerotherapy.
Keywords: Hemorrhoids, sclerotherapy, aluminum potassium sulfate and tannic acid (ALTA), hemorrhoid shrinking sign (HSS)
Introduction
Internal hemorrhoids with irreducible prolapse, which are internal hemorrhoids of grades III to IV by Goligher’s classification (1), generally require surgical treatment (2,3). Surgery is superior to other treatments including oral medication, rubber band ligation, and sclerotherapy in terms of effectiveness, but it requires a longer hospital stay and more time for postoperative treatment and incurs additional anxiety, pain, and complications including hemorrhage and disabled anal function (2-4). Sclerotherapy for hemorrhoid treatment has a long history, and its main indications have typically been for internal hemorrhoids of grades I or II, with limited indications for grade III hemorrhoids including prolapse (3,5). An injection of 5% phenol in almond oil as sclerotherapy had conventionally been in wide use, but its efficiency was limited as a randomized controlled trial showed no advantage of this form of sclerotherapy over laxative use (6).
Sclerotherapy using aluminum potassium sulfate and tannic acid (ALTA; development code name: OC108) according to a four-step injection method has been applied for internal hemorrhoids of more than grade III (7). ALTA was pharmaceutically modified in Japan from the additives of Xiaozhiling, which is a Chinese agent for the treatment of internal hemorrhoids (8). ALTA injected into hemorrhoids induces a strong local inflammatory reaction, resulting in persistent fibrosis and the adhesion and fixation of hemorrhoidal tissue to the muscular layer that lead to noninvasive sclerosis and regression of the hemorrhoids (7,9). After a clinical trial using ALTA for hemorrhoids begun in 1998 showed similar efficacy to that of surgery but with less serious complications and a low possibility of adverse events, the Japanese government approved its commercial use for hemorrhoids in 2005 (9). Since then, ALTA sclerotherapy has been popularly performed in Japan and Korea as a safe and less invasive alternative hemorrhoid treatment (7,10-12). The clinical results of ALTA sclerotherapy are quite good, and more than 50,000 cases of ALTA sclerotherapy are performed annually in Japan according to the National Database of Health Insurance Claims and Specific Health Checkups of Japan (NBD) in 2021 (13).
However, the recurrence rate with ALTA is higher than that with surgery for large internal hemorrhoids such as those of higher Goligher’s classification (9,12,14), and evaluation of the effectiveness of ALTA sclerotherapy is often left to the surgeon. Except for the disappearance of subjective symptoms or a cumbersome method using transanal ultrasound (15), no objective criteria for judging treatment efficacy have been established.
We thought the criteria and methods should be simple, clear, and easy to follow. On the basis of these ideas, we standardized our evaluation method for hemorrhoids in this study. Thus, we conducted a prospective observational study in which we assessed the validity of proctoscopy findings as a measure of effective hemorrhoid treatment after ALTA sclerotherapy to prove its clinical usefulness and establish objective indications for ALTA sclerotherapy. We present the following article in accordance with the STROBE reporting checklist (available at https://qims.amegroups.com/article/view/10.21037/qims-22-471/rc).
Methods
Patients
In this prospective cohort study, we investigated the relationship between the lumen at the lower rectum, the patients’ subjective satisfaction with the treatment, and re-treatment in 241 outpatients who underwent ALTA injection monotherapy for internal hemorrhoids from April 2015 to April 2019 at Miyazaki Sorano Clinic and were followed up for more than 6 months. Preoperatively, patients’ defecation was evaluated using the Kirwan classification system (16,17), and no patient had bowel dysfunction of more than 2. We assigned what we refer to as a Kirwan Score as follows: 1 for perfect continence, 2 for flatus incontinence, 3 for occasional minor soiling, 4 for frequent major soiling, and 5 if colostomy is required. In this study, no patients had severe organ failure, severe drug hypersensitivity, or were of American Society of Anesthesiologists (ASA) physical status class IV–VI (18). Patients’ clinical characteristics and results of clinical examinations including Goligher’s classification (1) were recorded in a prospective database. All patients provided informed consent for their anonymized data to be used for study purposes. This study was approved by the Human Research Ethics Committee of the Japan Society of Coloproctology (Ethics approval number: 30-JSCP·IRB-2) and conducted in accordance with the Declaration of Helsinki (as revised in 2013).
ALTA sclerotherapy and evaluation of hemorrhoids
ALTA sclerotherapy for hemorrhoids was performed according to a four-stage injection method previously described (7). The dose of ALTA was reduced by 1 to 2 mL in all four stages in the anterior wall in this study because ulceration was more common in the anterior wall. All treatments were performed as day surgery. The patient was positioned in the Sims position, and ALTA sclerotherapy was performed without anesthesia other than the analgesics contained in the ALTA solution.
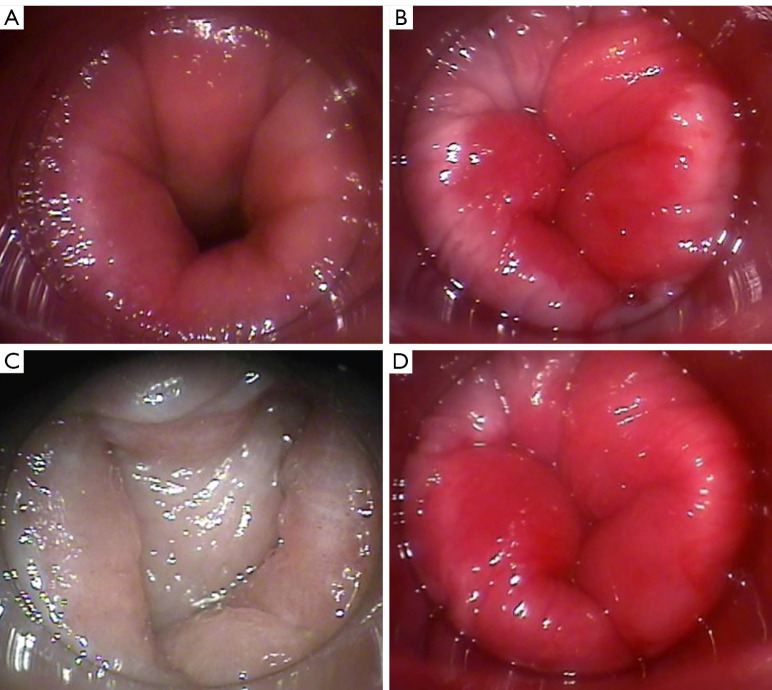
To assess the severity of the patients’ hemorrhoids preoperatively and on postoperative day 7, we used a clear plastic proctoscope to observe the “lumen” of the lower rectum where hemorrhoids protrude into the lower rectum and divided them into two groups: those with and without the lumen as follows. A commercially available clear plastic tube proctoscope (AT-PT001, medium size, outer diameter: 17 mm, working length: 75 mm; ARAKAWA SEISAKUSHO Co., Ltd., Tokyo, Japan) (Figure 1) was connected to a TV monitor system (R-TV2000S; Yufu Itonaga Co., Ltd., Tokyo, Japan) and deeply inserted into the rectum, and the frontal view of the rectal lumen was obtained (Figure 2A). The proctoscope was pulled back to the dentate line so that the Herrmann line could be seen (Figure 2B), and after fecal juice was removed using gauze, the hemorrhoid region was pushed a few millimeters into the rectum to determine whether a space was present. We then determined whether the mucosal surfaces did not touch each other, that is, whether a lumen existed (lumen positive) (Figure 2C) or not (lumen negative) (Figure 2D). In the evaluation, the angle of the proctoscope should be adjusted such that it is always in the center of the anal canal, and the presence or absence of a lumen should be checked when the patient applies strain. The lumen was checked on postoperative day 7 and at the time re-treatment when required. Findings were double-checked by two proctologists who were familiar with and trained in the methods described in this section.
Figure 1.

The commercially available clear plastic tube proctoscope (AT-PT001, ARAKAWA SEISAKUSHO Co., Ltd., Tokyo, Japan) used for this study.
Figure 2.
Images showing the assessment method and morphology of the mucosa at the lower margin of the rectum using the clear plastic proctoscope. (A) Frontal view of rectal lumen when the proctoscope is deeply inserted. (B) Herrmann line when the proctoscope was pulled back to the dentate line. (C,D) Evaluation of the lumen at the end of the rectum: (C) lumen positive; (D) lumen negative.
The hemorrhoid shrinking sign (HSS) (19) and the patients’ subjective satisfaction of effectiveness after ALTA sclerotherapy were also evaluated on postoperative day 7 as the effects of the therapy. HSS is defined as a change in the presence of the lumen from lumen negative preoperatively to lumen positive postoperatively. Patients were given a questionnaire asking whether the most bothersome preoperative symptoms had improved with surgery to determine subjective effectiveness as classified into three groups: C-1, complete disappearance of subjective symptoms; C-3, unchanged compared with preoperative symptoms; and C-2, between C-1 and C-3.
Data analysis
Data are shown as the number (percentage) of patients or as the average (range), unless otherwise indicated. The McNemar test was used to identify the relationship between ALTA sclerotherapy and the change in the lumen. The κ value and 95% confidence interval (CI) were calculated. The correlation between the lumen and subjective satisfaction as the effect of ALTA sclerotherapy on postoperative day 7 and that between re-treatment and the lumen or subjective satisfaction were examined by Fisher’s exact test. The association between the need for re-treatment and change in the lumen and subjective satisfaction was explored using the Wilcoxon signed-rank test, a non-parametric statistical hypothesis test. The mean differences, standard deviation, and P values were calculated, and a P value of <0.05 was considered to indicate statistical significance.
Results
Included in the study were 241 patients [113 men, 128 women; average age: 58.9 (range, 23–90) years]. ALTA sclerotherapy was performed for internal hemorrhoids of Goligher’s grade II (116 patients), grade III (90 patients), and grade IV (35 patients). There were no missing data in this study. The mean number of hemorrhoids treated was 3.0 (range, 1–5), and the mean volume of ALTA injected was 15.0 (range, 5.0–38.8) mL. We found an improvement in subjective symptoms after ALTA sclerotherapy of C-1 and C-2 subjective effectiveness in 99.6% (240/241) of the patients on postoperative day 7.
Our method using a clear plastic proctoscope showed that 96.7% (233/241) of the patients were lumen negative preoperatively, but after ALTA sclerotherapy, only 3.7% (9/241) were still lumen negative. This indicates that 224 of the 233 (96.1%) patients who were lumen negative before treatment became lumen positive with ALTA sclerotherapy, which was associated with significant lumen gain (κ value, 0.0027; 95% CI: 0.0001–0.0052, P<0.001) by McNemar test (Table 1).
Table 1. McNemar test of the paired existence of the lumen in the lower rectum before and after aluminum potassium sulfate and tannic acid sclerotherapy.
| Variable | On postoperative day 7 | κ value (95% CI) | P value | ||
|---|---|---|---|---|---|
| Lumen negative | Lumen positive | Total | |||
| Preoperatively, lumen negative | 9 | 224 | 233 | 0.0027 (0.0001–0.0052) | <0.001 |
| Preoperatively, lumen positive | 0 | 8 | 8 | ||
| Total | 9 | 232 | 241 | ||
CI, confidence interval.
Among the 232 lumen-positive patients on postoperative day 7, subjective satisfaction of effectiveness was C-1, i.e., complete disappearance of symptoms, in 73.3% and C-2 in 26.7%, whereas that in the lumen-negative group was C-1 in 55.6%, C-2 in 33.3%, and C-3 in 11.1% of the patients. Fisher’s exact test showed that patients’ subjective satisfaction of effectiveness with ALTA sclerotherapy was significantly higher in the lumen-positive versus lumen-negative group (P=0.0186) (Table 2).
Table 2. Existence of a lumen in the lower rectum and patients’ subjective satisfaction of effectiveness by aluminum potassium sulfate and tannic acid sclerotherapy on postoperative day 7.
| Subjective satisfaction | On postoperative day 7 | P value | |
|---|---|---|---|
| Lumen negative (n=9) | Lumen positive (n=232) | ||
| C-1 | 5 (55.6) | 170 (73.3) | 0.0186 |
| C-2 | 3 (33.3) | 62 (26.7) | |
| C-3 | 1 (11.1) | 0 (0.0) | |
Data are presented as No. (%). C-1, complete disappearance of subjective symptoms; C-3, unchanged compared with preoperative symptoms; C-2, between C-1 and C-3.
Re-treatment for hemorrhoids was required in 33 (13.7%) of the 241 patients. The median time to re-treatment was 5.8 (range, 1.0–48.0) months. In the lumen-positive group on postoperative day 7, 32 cases of re-treatment were observed for a re-treatment rate of 13.8%, whereas only one re-treatment was observed in the lumen-negative group for a re-treatment rate of 11.1%, which was not statistically different between the two groups by Fisher’s exact test. In terms of the patients’ subjective satisfaction of effectiveness on postoperative day 7, the re-treatment rate in those with C-1 satisfaction was 9.4%, whereas the rates in those with C-2 and C-3 satisfaction were 25.8% and 100%, respectively. Fisher’s exact test showed the re-treatment rates in patients with C-2 and C-3 satisfaction to be significantly higher than that in those with C-1 satisfaction (P=0.001).
When the lumen was checked again at re-treatment, 13 patients (39.4%) were lumen positive and 20 (60.6%) lumen negative (Table 3). As 32 patients with re-treatment were lumen positive on postoperative day 7, 19 patients (59.4%) had converted to lumen negative (i.e., had lost the lumen) at the time re-treatment was required (Table 3). Furthermore, subjective satisfaction had also worsened at re-treatment. The results of the Wilcoxon signed-rank test showed a significant association between loss of the lumen and deterioration of subjective satisfaction (P=0.001).
Table 3. Characteristics of 33 patients who required re-treatment after aluminum potassium sulfate and tannic acid sclerotherapy.
| Variables | 33 patients who underwent re-treatment | Mean difference | Standard deviation | P value | |
|---|---|---|---|---|---|
| On postoperative day 7 | At time of re-treatment | ||||
| Lumen of the lower rectum | 0.578 | 0.502 | <0.001 | ||
| Positive | 32 (97.0) | 13 (39.4) | |||
| Negative | 1 (3.0) | 20 (60.6) | |||
| Subjective satisfaction | 0.758 | 0.663 | <0.001 | ||
| C-1 | 16 (48.5) | 0 (0.0) | |||
| C-2 | 16 (48.5) | 23 (70.0) | |||
| C-3 | 1 (3.0) | 10 (30.0) | |||
Data are presented as No. (%). C-1, complete disappearance of subjective symptoms; C-3, unchanged compared with preoperative symptoms; C-2, between C-1 and C-3.
Re-treatments were performed using surgical treatment (ligation and excision) in 14 patients and re-administration of ALTA in 19 patients, for which additional surgical treatment was performed in 4 patients. The reason for re-treatment in the 13 lumen-positive patients was due to external hemorrhoids. We found no recurrences of internal hemorrhoids.
Discussion
In this study, we found that a simple indicator, the lumen of the lower rectum as visualized with a clear plastic proctoscope, reflects the extent of hemorrhoids and that this indicator can be improved with ALTA sclerotherapy. Although 96.7% (233/241) of the patients had no lumen at the lower rectum preoperatively, 96.1% (224/233) of these patients acquired the lumen after ALTA sclerotherapy, indicating that the lumen may be a useful indicator in determining the effectiveness of hemorrhoid treatment. Because no concrete method to judge effectiveness after ALTA sclerotherapy has been presented so far, we tried to objectively evaluate hemorrhoids and the effect of ALTA sclerotherapy by using the lumen at the lower rectum, which refers to the space in the lower rectum. When a symptomatic hemorrhoid protrudes into the inferior margin of the rectum, the lumen of the lower rectum becomes narrow.
The direct evaluation of hemorrhoids is often difficult due to individual differences in the length and angle of the anal canal. The instruments used for examination also differ between institutions. In setting up an indicator, we wanted the evaluation method to be simple because anal surgery and subsequent follow-up are generally performed in busy outpatient clinics. Therefore, the method of confirming the lumen in this study was clearly standardized and described in detail from the instruments used to the evaluation technique performed to increase reproducibility and objectivity. Our method focused not only on the region of the treated hemorrhoids but also on the lower rectum. We hypothesized that focusing on the lower rectum would allow us to explore the correlation between the patients’ subjective satisfaction and objective assessment. In fact, our objective method using the lumen significantly correlated with their subjective degree of satisfaction (P=0.0186) (Table 2).
We recently defined and advocated the “hemorrhoid shrinking sign (HSS)” as a change in the presence of the lumen at the lower rectum from lumen negative preoperatively to lumen positive postoperatively with ALTA sclerotherapy, and it does not include patients who were lumen positive preoperatively (Video 1) (19). A positive HSS (patients with change from lumen negative to lumen positive) is considered to be an indicator of a favorable effect of treatment as this was seen in many of the patients (96.1%) in our study in which ALTA was effective.
Video 1.

Confirmation of the “lumen” of the lower rectum using a clear plastic tube proctoscope. After being deeply inserted into the rectum, the proctoscope is pulled back to the dentate line to identify the Herrmann line. Then, the hemorrhoid region is pushed a few millimeters into the rectum to determine whether a space is present and that the mucosal surfaces do not touch each other. This video shows the “lumen negative” state before ALTA sclerotherapy, in which the lumen does not exist due to the hemorrhoid, and the “lumen positive” state after treatment. ALTA, aluminum potassium sulfate and tannic acid.
In the present study, although the situation of the lumen at day 7 could not predict recurrence, we showed that in many patients who required re-treatment, the lumen that was present in the anal canal on day 7 had disappeared (Table 3). It was clear that the risk of re-treatment was high during the follow-up period once the lumen became negative and that careful and intensive follow-up was required after the lumen changed to lumen negative. The usefulness of the HSS will be analyzed in our next study after accumulating additional cases, and the relationship between HSS and re-treatment, for which the patients’ subjective satisfaction classifications of C-2 and C-3 showed significantly higher re-treatments rates in this study, and patients’ characteristics such as Goligher’s classification will be examined.
Our study is limited by its execution as a single-arm observational study of ALTA sclerotherapy. However, the patients’ rate of subjective satisfaction at day 7 and that of objective effectiveness are high. The retreatment rate was 13.7% (33/241 patients), and 8.3% (20/241 patients) of these patients were considered to have recurrent internal hemorrhoids (Table 3). The results of this study are similar to the previously reported results of ALTA: Miyamoto et al. reported that the cumulative success rates of Grades II and III were 95.9% and 93.1%, respectively (12); Takano et al. reported a 1-year recurrence rate of 16% (7); and Abe et al. reported a 3-year recurrence rate of 7.4% (20). The results are also comparable to treatments other than ALTA such as non-surgical treatments including rubber band ligation and infrared coagulation: the review by Cocorullo et al. reported respective recurrence rates of 10–18% and 13% (21). It was impossible to track the progress of hemorrhoids in all patients because almost all were cured after a few postoperative follow-up visits, and the patients stopped returning to the clinic. Prognostic studies using patient contact by telephone and mail are being considered in the future.
Hemorrhoids are a very common benign disease, but surgery for hemorrhoids can be a huge burden on the patient. ALTA sclerotherapy can be as effective as surgery while being minimally invasive (20). However, recurrence was also more common with ALTA compared to surgery, and especially, it is less suitable than surgery for advanced cases (12,14). For this reason, criteria for properly selecting patients to receive ALTA sclerotherapy is necessary, but first, it is important to objectively evaluate the effectiveness of ALTA sclerotherapy. Our method incorporating a clear plastic proctoscope in the present study allowed us to simply and precisely evaluate the effect of ALTA sclerotherapy and to extract patients who required re-treatment by checking for the loss of lumen during follow-up. By accumulating data in the future using this method, we hope to extract factors that indicate the necessity of re-treatment and contribute to the development of therapeutic indications for ALTA sclerotherapy.
Supplementary
The article’s supplementary files as
Acknowledgments
We would like to thank Prof. Tina Tajima, St. Marianna University School of Medicine, for assistance in reviewing the manuscript to ensure proper English expression.
Funding: None.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Human Research Ethics Committee of the Japan Society of Coloproctology (No. 30-JSCP·IRB-2), and informed consent was obtained from all the patients. This work complied with the current laws in Japan.
Footnotes
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://qims.amegroups.com/article/view/10.21037/qims-22-471/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-471/coif). The authors have no conflicts of interest to declare.
References
- 1.Goligher JC. Haemorrhoids or piles. In: Goligher JC, Duthie HL, Nixon HH. editors. Surgery of the anus, rectum and colon. 4th edition. London: Baillière Tindall; 1984:96. [Google Scholar]
- 2.MacRae HM, McLeod RS. Comparison of hemorrhoidal treatments: a meta-analysis. Can J Surg 1997;40:14-7. [PMC free article] [PubMed] [Google Scholar]
- 3.Ganz RA. The evaluation and treatment of hemorrhoids: a guide for the gastroenterologist. Clin Gastroenterol Hepatol 2013;11:593-603. 10.1016/j.cgh.2012.12.020 [DOI] [PubMed] [Google Scholar]
- 4.Dekker L, Han-Geurts IJM, Rørvik HD, van Dieren S, Bemelman WA. Rubber band ligation versus haemorrhoidectomy for the treatment of grade II-III haemorrhoids: a systematic review and meta-analysis of randomised controlled trials. Tech Coloproctol 2021;25:663-74. 10.1007/s10151-021-02430-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khoury GA, Lake SP, Lewis MC, Lewis AA. A randomized trial to compare single with multiple phenol injection treatment for haemorrhoids. Br J Surg 1985;72:741-2. 10.1002/bjs.1800720924 [DOI] [PubMed] [Google Scholar]
- 6.Senapati A, Nicholls RJ. A randomised trial to compare the results of injection sclerotherapy with a bulk laxative alone in the treatment of bleeding haemorrhoids. Int J Colorectal Dis 1988;3:124-6. 10.1007/BF01645317 [DOI] [PubMed] [Google Scholar]
- 7.Takano M, Iwadare J, Ohba H, Takamura H, Masuda Y, Matsuo K, Kanai T, Ieda H, Hattori Y, Kurata S, Koganezawa S, Hamano K, Tsuchiya S. Sclerosing therapy of internal hemorrhoids with a novel sclerosing agent. Comparison with ligation and excision. Int J Colorectal Dis 2006;21:44-51. 10.1007/s00384-005-0771-0 [DOI] [PubMed] [Google Scholar]
- 8.Shi Z, Zhou J, He X. On Treatment of Third Degree Internal Hemorrhoids with "Xiaozhiling" Injection. J Trad Chin Med 1981;1:115-20. [Google Scholar]
- 9.Yamana T. Japanese Practice Guidelines for Anal Disorders I. Hemorrhoids. J Anus Rectum Colon 2018;1:89-99. 10.23922/jarc.2017-018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tokunaga Y, Sasaki H, Saito T. Evaluation of sclerotherapy with a new sclerosing agent and stapled hemorrhoidopexy for prolapsing internal hemorrhoids: retrospective comparison with hemorrhoidectomy. Dig Surg 2010;27:469-72. 10.1159/000320321 [DOI] [PubMed] [Google Scholar]
- 11.Hachiro Y, Kunimoto M, Abe T, Kitada M, Ebisawa Y. Aluminum potassium sulfate and tannic acid (ALTA) injection as the mainstay of treatment for internal hemorrhoids. Surg Today 2011;41:806-9. 10.1007/s00595-010-4386-x [DOI] [PubMed] [Google Scholar]
- 12.Miyamoto H, Hada T, Ishiyama G, Ono Y, Watanabe H. Aluminum potassium sulfate and tannic acid sclerotherapy for Goligher Grades II and III hemorrhoids: Results from a multicenter study. World J Hepatol 2016;8:844-9. 10.4254/wjh.v8.i20.844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Database of Health Insurance Claims and Specific Health Checkups of Japan [internet]. Ministry of Health, Labour and Welfare [cited 2022 May 5]. Available online: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000177221_00010.html. In Japanese.
- 14.Yano T, Asano M, Tanaka S, Oda N, Matsuda Y. Prospective study comparing the new sclerotherapy and hemorrhoidectomy in terms of therapeutic outcomes at 4 years after the treatment. Surg Today 2014;44:449-53. 10.1007/s00595-013-0564-y [DOI] [PubMed] [Google Scholar]
- 15.Miyamoto H, Asanoma M, Miyamoto H, Takasu C, Shimada M. Three-dimensional power Doppler transanal ultrasonography, to monitor haemorrhoidal blood flow after Doppler-guided ALTA sclerosing therapy. Colorectal Dis 2013;15:e84-8. 10.1111/codi.12024 [DOI] [PubMed] [Google Scholar]
- 16.Kirwan WO, Turnbull RB, Jr, Fazio VW, Weakley FL. Pullthrough operation with delayed anastomosis for rectal cancer. Br J Surg 1978;65:695-8. 10.1002/bjs.1800651008 [DOI] [PubMed] [Google Scholar]
- 17.Sato S, Shiozawa M, Uchiyama M, Sugano N, Rino Y, Masuda M. Correlation between endoscopic features of the anastomosis after low anterior resection and postsurgical anorectal function. J Gastrointest Oncol 2019;10:188-93. 10.21037/jgo.2018.11.09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Daabiss M. American Society of Anaesthesiologists physical status classification. Indian J Anaesth 2011;55:111-5. 10.4103/0019-5049.79879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oga J. The evaluation of curability in ALTA monotherapy. J Jpn Soc Colorectal Anal Dis 2018;72:1-7. [Google Scholar]
- 20.Abe T, Kunimoto M, Hachiro Y, Ohara K, Inagaki M. Long-term Outcomes of Aluminum Potassium Sulfate and Tannic Acid Sclerotherapy for Prolapsed Hemorrhoids: A Single-Center, Observational Study. Dis Colon Rectum 2022;65:271-5. 10.1097/DCR.0000000000002284 [DOI] [PubMed] [Google Scholar]
- 21.Cocorullo G, Tutino R, Falco N, Licari L, Orlando G, Fontana T, Raspanti C, Salamone G, Scerrino G, Gallo G, Trompetto M, Gulotta G. The non-surgical management for hemorrhoidal disease. A systematic review. G Chir 2017;38:5-14. 10.11138/gchir/2017.38.1.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as