Abstract
Background
eHealth tools such as patient portals and personal health records, also known as patient-centered digital health records, can engage and empower individuals with chronic health conditions. Patients who are highly engaged in their care have improved disease knowledge, self-management skills, and clinical outcomes.
Objective
We aimed to systematically review the effects of patient-centered digital health records on clinical and patient-reported outcomes, health care utilization, and satisfaction among patients with chronic conditions and to assess the feasibility and acceptability of their use.
Methods
We searched MEDLINE, Cochrane, CINAHL, Embase, and PsycINFO databases between January 2000 and December 2021. PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines were followed. Eligible studies were those evaluating digital health records intended for nonhospitalized adult or pediatric patients with a chronic condition. Patients with a high disease burden were a subgroup of interest. Primary outcomes included clinical and patient-reported health outcomes and health care utilization. Secondary outcomes included satisfaction, feasibility, and acceptability. Joanna Briggs Institute critical appraisal tools were used for quality assessment. Two reviewers screened titles, abstracts, and full texts. Associations between health record use and outcomes were categorized as beneficial, neutral or clinically nonrelevant, or undesired.
Results
Of the 7716 unique publications examined, 81 (1%) met the eligibility criteria, with a total of 1,639,556 participants across all studies. The most commonly studied diseases included diabetes mellitus (37/81, 46%), cardiopulmonary conditions (21/81, 26%), and hematology-oncology conditions (14/81, 17%). One-third (24/81, 30%) of the studies were randomized controlled trials. Of the 81 studies that met the eligibility criteria, 16 (20%) were of high methodological quality. Reported outcomes varied across studies. The benefits of patient-centered digital health records were most frequently reported in the category health care utilization on the “use of recommended care services” (10/13, 77%), on the patient-reported outcomes “disease knowledge” (7/10, 70%), “patient engagement” (13/28, 56%), “treatment adherence” (10/18, 56%), and “self-management and self-efficacy” (10/19, 53%), and on the clinical outcome “laboratory parameters,” including HbA1c and low-density lipoprotein (LDL; 16/33, 48%). Beneficial effects on “health-related quality of life” were seen in only 27% (4/15) of studies. Patient satisfaction (28/30, 93%), feasibility (15/19, 97%), and acceptability (23/26, 88%) were positively evaluated. More beneficial effects were reported for digital health records that predominantly focus on active features. Beneficial effects were less frequently observed among patients with a high disease burden and among high-quality studies. No unfavorable effects were observed.
Conclusions
The use of patient-centered digital health records in nonhospitalized individuals with chronic health conditions is potentially associated with considerable beneficial effects on health care utilization, treatment adherence, and self-management or self-efficacy. However, for firm conclusions, more studies of high methodological quality are required.
Trial Registration
PROSPERO (International Prospective Register of Systematic Reviews) CRD42020213285; https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=213285
Keywords: telemedicine, health records, personal, electronic health records, outcome assessment, health care
Introduction
Background
The prevalence and disease burden of chronic health conditions is on the rise. The World Health Organization predicts that by 2030, chronic noncommunicable health conditions will account for >50% of the total disease burden [1,2]. In particular, cardiovascular conditions, cancer, respiratory conditions, and diabetes have the highest morbidity and mortality [1]. Currently, 60% of the US population has at least 1 chronic condition and 42% of the population has multiple chronic conditions [3]. This results in a high individual disease burden owing to the large impact on social participation and required patient self-management skills. Self-management refers to a person’s ability to manage the clinical, psychosocial, and societal aspects of their illness and its care [4]. In contrast, self-efficacy is a person’s belief that he or she can successfully execute this behavior [4]. Apart from a high individual disease burden, the prevalence of chronic conditions imposes a high macroeconomic burden [5]. Furthermore, an increasing shortage of health care providers is expected, among others in the United States [6] and Europe [7,8]. In combination with the increased pressure put on health systems by unexpected events such as the COVID-19 pandemic, this shortage threatens the delivery of essential health services [9]. To preserve the access to care for all patients, new technologies are increasingly being developed and adopted, including patient-centered digital health records.
Such patient-centered digital health records can significantly help engage and empower patients with a chronic health condition [10-13]. Patient-centered digital health records enable patients to take on a more active role in their care by allowing them to view parts of their medical records, such as medication lists, laboratory and imaging results, allergies, and correspondence. Other common features include secure messaging, requesting prescription refills, video consultation, paying bills, and managing appointments. Examples of patient-centered digital health records include patient portals and personal health records (PHRs). Patient-centered digital health records differ in the volume and detail of the provided medical data, functionalities, and level of patient control, as shown in Textbox 1. Highly engaged patients are reported to have increased disease knowledge, better self-management, more self-efficacy, and improved clinical outcomes [14-16]. The effects of using patient-centered digital health records may be most substantial for patients with chronic conditions. Many self-management skills are required, and their potential gains are the highest. Not only patients but the entire health care system might benefit from an increased adoption of patient-centered digital health records.
Proposed taxonomy of patient-centered digital health records [10,17-21].
Electronic health record (EHR): a digital version of a health care provider’s paper chart, used by health care professionals alone. Patients cannot access data in an EHR. An EHR might contain data from one health care institution or from multiple institutions. Its scope can range from regional, to national, or international.
Patient portal: the patient-facing interface of an EHR that enables people to view sections of their medical record. This might include access to test results, medication lists, or therapeutic instructions. Health care providers or health care offices determine what health information is accessible for patients. Patient portals often have additional features such as patient-professional messaging, requesting prescription refills, scheduling appointments, or communicating patient-reported outcomes. By definition, patient portals are “tethered,” in which “tethered” refers to a patient portal’s connection to an EHR. Occasionally, a patient portal is referred to as a tethered personal health record (PHR).
PHR: a PHR is similar to a patient portal and can have similar features. However, the main difference is that contents are managed and maintained by individuals, not health care providers. People can access, manage, and share their health information, and that of others for whom they are authorized, such as parents or caretakers. Health information from different health care institutions may reside in a single patient-managed PHR. In general, PHRs are not tethered unless otherwise specified. Few tethered PHRs currently exist but are increasingly being developed [22].
Patient-centered digital health records: an umbrella term referring to patient portals, tethered PHRs, and part of the untethered PHRs. Patient-centered digital health records enable a 2-way exchange of health information between patients and the health care system and provide patients with the ability to view, download, or transmit their health information on the web. This health information is updated at regular intervals. In addition, it enables communication between patients and the health care system, either by adding or editing health information, exchanging patient-reported outcomes, or by using communication tools such as messaging. Additional functionalities are often present.
“Electronic medical record” is an outdated term [21]. It can be considered a professional-centered EHR with limited functionalities.
Currently, huge investments of time and resources are made in patient-centered digital health records. However, limited insight exists in how the use of patient-centered digital health records by patients with a broad range of chronic conditions affects clinical and patient-reported outcomes and health care utilization. Moreover, we lack an overview of their effects on patient satisfaction, and the feasibility and acceptability of their use by people with chronic conditions. Previous systematic reviews focused on one health condition [23], focused on one type of digital health record [24-27], investigated a select set of health outcomes [24,26,28], or are now obsolete in this rapidly changing technological landscape [23,25,27].
Objectives
Therefore, in this systematic review, we summarized the available evidence on patient-centered digital health records. Our primary objective was to assess how patient-centered digital health records for nonhospitalized patients with chronic conditions affect clinical and patient-reported health outcomes and health care utilization. Our secondary objective was to evaluate patient satisfaction with and feasibility and acceptability of using patient-centered digital health records. Results of this systematic review may help guide future development and implementation.
Methods
The protocol for this study was registered in the International PROSPERO (International Prospective Register of Systematic Reviews) Register of Systematic Reviews (CRD42020213285) [29]. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines were followed [30].
Literature Search
A medical librarian (MB) conducted the original literature search using the following databases: MEDLINE, Cochrane Library, CINAHL, Embase, and PsycINFO. All original studies published between January 1, 2000, and December 1, 2020, were assessed. A search update in MEDLINE was performed for all studies published between December 1, 2020, and December 31, 2021. Multimedia Appendix 1 presents the full search strategy. Articles published before 2000 were excluded because of the rapidly changing field of digital health technology [30].
Eligibility Criteria
Patient-centered digital health records were defined as mobile health (mHealth) or eHealth technologies that enable a 2-way exchange of health information between patients and the health care system, such as patient portals, PHRs, or mHealth apps with a health record functionality. A patient-centered digital health record provides patients with the ability to view, download, or transmit their health information on the web. This health information was updated at regular intervals. In addition, a patient-centered digital health record allows for communication between patients and the health care system, either by adding or editing health information, exchanging patient-reported outcomes, or by using communication tools such as messaging. Several other functionalities are common, but were not considered essential; for example, appointment scheduling, requesting prescription refill, viewing educational material, using decision support tools, and using connected wearables. Exclusion criteria were nondigital health records, digital health records intended for hospitalized patients, and digital health records that are not accessible to patients, such as the clinician-facing components of the electronic health record (EHR).
Studies
Studies investigating patient-centered digital health records intended for nonhospitalized patients with a chronic health condition were included. Only studies published in English were included. Eligible studies included randomized controlled trials (RCTs), quasi-experimental studies, nonexperimental observational studies (including cohort and cross-sectional studies), and pilot or feasibility studies. Of mixed methods studies, only nonqualitative parts were used for data extraction. Studies that only described health care providers’ experiences were excluded.
Participants
Studies on patients with a chronic health condition of all age groups were considered. Chronic conditions included all diseases with a moderate to high disease burden and moderate to high impact on daily life. Consequently, these conditions demand considerable self-management skills from patients to manage the clinical, psychosocial, and societal aspects of chronic condition and its care. The selection of chronic conditions included in our search strategy was based on the Charlson Comorbidity Index, other literature, and clinical expertise [31,32]. Diseases included cancer, arthritis, HIV, AIDS, asthma, chronic obstructive pulmonary disease, chronic heart conditions, hematologic disease, chronic kidney disease, celiac disease, inflammatory bowel disease, cystic fibrosis, diabetes mellitus, and multiple sclerosis (MS).
Outcomes
Studies were required to report at least one primary or secondary outcome. Primary outcomes were clinical outcomes (including disease events and complications, vital parameters, and laboratory parameters), patient-reported outcomes (including self-management and self-efficacy, patient engagement, health-related quality of life (HRQoL), stress and anxiety, and treatment adherence), and health care utilization (including the number of emergency department [ED] visits and hospitalizations, the use of preventive or recommended care services by patients, and regular workload for health care professionals). Secondary outcomes included technology-related outcomes (including patient satisfaction, feasibility, and acceptability). Definitions and examples of these 13 outcomes are presented in Table 1.
Table 1.
Definitions and examples of all health outcomes included in this systematic review.
| Included study outcomes | Definitions and examples | |
| Clinical outcomes | ||
|
|
Disease events and complications |
|
|
|
Vital parameters |
|
|
|
Laboratory parameters |
|
| Patient-reported outcomes | ||
|
|
Self-management and self-efficacy |
|
|
|
Patient engagement |
|
|
|
Health-related quality of life |
|
|
|
Treatment adherence |
|
| Health care utilization: >all types of encounters between patients and health care providers, including EDd visits, hospitalizations, outpatient clinic appointments, and telephone calls | ||
|
|
ED visits and hospitalizations |
|
|
|
Recommended care services |
|
|
|
Regular workload |
|
| Technology-related outcomes | ||
|
|
Patient satisfaction |
|
|
|
Feasibility |
|
|
|
Acceptability |
|
aHbA1c: glycated hemoglobin.
bLDL: low-density lipoprotein.
ceGFR: estimated glomerular filtration rate.
dED: emergency department.
Data Extraction
Two independent reviewers (MB and SB) assessed titles, abstracts, and full texts for eligibility. Disagreements were resolved by discussion, if necessary, with a third reviewer (SG).
A modified, electronic version of the standardized Cochrane data extraction form [39] was used to extract the following data items: first author’s name; publication year; study design; disease or diseases studied; study aim; country and setting; participants’ age and sex; sample size; inclusion and exclusion criteria; follow-up duration; description, features, and purpose of the patient-centered digital health record and (if applicable) of the comparator; size and description of the control group (if applicable); device used; description of health outcomes and results; and main study findings.
Quality Appraisal
For quality appraisal, Joanna Briggs Institute (JBI) critical appraisal tools for RCTs, cross-sectional studies, cohort studies, and quasi-experimental studies were used [40]. JBI tools were modified to better suit the assessment of digital health record studies. Several items were added, including adequate patient-centered digital health record descriptions and selection bias measures, as presented in Multimedia Appendix 2. As the JBI tools differed in the number of items, all scores were converted to a 15-point scale. Articles with a score of ³12 were considered of “high quality,” between 8.5 and 11.9 of “medium quality,” and <8.5 of “low quality.”
Data Synthesis
Associations between patient-centered digital health record use and health outcomes were categorized in 3 groups: “beneficial,” “neutral or clinically nonrelevant,” or “undesired.” Categorizations were determined by our interpretation of study findings, based on meaningful clinical effects and statistical significance (P<.05), and could therefore differ from the authors’ conclusions. Statistical significance was considered relevant only if the effect size were clinically significant. If available, minimal clinically important differences were used to assess effect sizes. The summarization of effects was based on the vote-counting method, as no meta-analysis could be performed. The findings were summarized for all conditions, grouped by disease category (diabetes mellitus, cardiopulmonary diseases, hematology-oncology diseases, and other diseases), and grouped according to outcome type (clinical outcomes, patient-reported outcomes, health care utilization, and technology-related outcomes).
Subgroup Analyses
Several subgroup analyses were performed. The first subgroup included conditions with a high disease burden. These included conditions with either impaired social participation or that require a high level of self-management skills. Impaired social participation was defined as being unable to participate in work or school or engage with friends and family as desired because of the condition or its treatment. High self-management skills are defined as recurrent actions demanded from patients to prevent or treat the disease or its consequences, including high disease-related knowledge needed to actively engage in decision-making. This subgroup was determined based on clinical expertise of the study team. Second, we assessed 2 subgroups: patient-centered digital health records that predominantly offered passive features and those that predominantly offered active features. Passive features are those through which the patient receives information but does not actively add information. Active features are those in which the patient performs an action and actively engages with the digital health record. The third subgroup of interest included studies with high methodological quality. A sensitivity analysis was performed to investigate whether our results were influenced by poor quality studies. Finally, the subgroups of interest were studies that included older participants (mean age >55 years), a high number of female participants (>45%), or a racially diverse population (<50% White participants).
Results
Overview
The search yielded 7716 unique publications. After screening the titles and abstracts, 320 full-text articles were retrieved. A total of 81 articles met the inclusion criteria. No non-English articles that met the inclusion criteria were identified. Figure 1 shows the study PRISMA flowchart. In total, 1,639,556 participants were included in the studies of this systematic review. Most (74/81, 91%) studies included only adult participants. Of the total 1,369,913 participants, 99% (n=1,629,660) were adults. Nine studies included children or their parents, with a total number of 9297 children and 599 parents. Sample sizes of studies varied from 10 to 267,208 participants. Furthermore, 46% (747,370/1,639,556) of the participants were female. Of the 81 included studies, health literacy was reported by 7 (9%) studies and insurance status by 15 (20%) studies. Race distribution was reported by 74% (60/81) of studies, of which 47 (78%) studies included a population of which more than half were White and 26 (43%) studies of which >75% were White.
Figure 1.
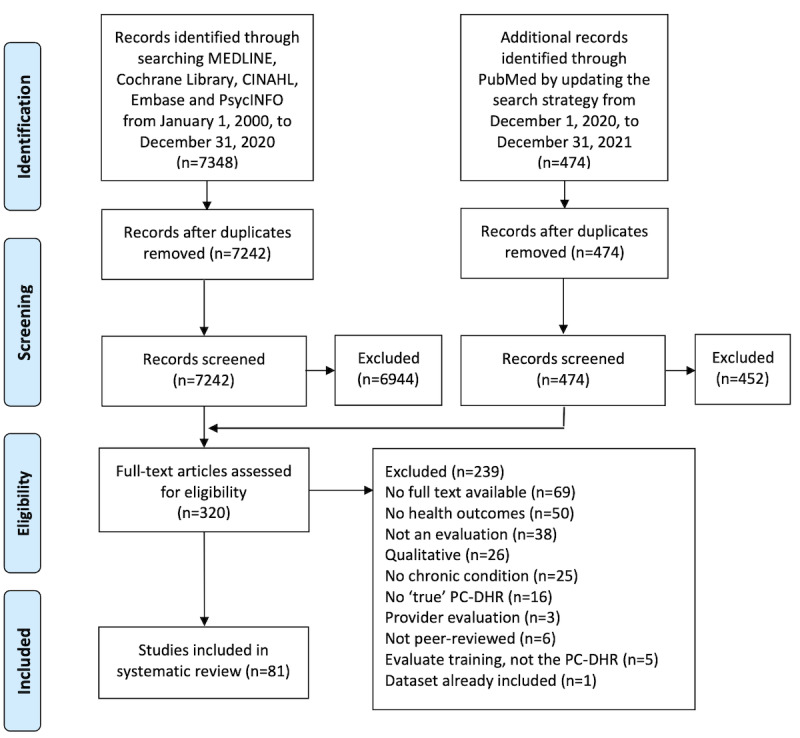
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram. PC-DHR: patient-centered digital health record.
Study Characteristics
Study characteristics are presented in Tables 2-5 (36 studies are listed in Table 2; 11 studies are listed in Table 3, 14 studies are listed in Table 4, and 20 studies are listed in Table 5). Most investigated conditions were type 1 or 2 diabetes mellitus (37/81, 46%), cardiovascular conditions (14/81, 17%), and malignancies (11/81, 14%). Studies were mostly conducted in the following countries: United States (58/81, 72%), the Netherlands (7/81, 9%), Canada (5/81, 6%), and United Kingdom (3/81, 4%). In addition, 30% (24/81) of the studies were RCTs, 27% (22/81) were cross-sectional studies, 20% (16/81) were retrospective observational cohort studies, and 23% (18/81) were quasi-experimental studies, including pretest-posttest and feasibility studies. One study was a secondary data analysis of the intervention group in an RCT. Of the 55 studies that reported follow-up durations, 6 (7%) studies had a follow-up of less than a month, 25 (31%) studies between 1 and 6 months, 14 (17%) studied between 7 and 12 months, and 10 (12%) studies of >12 months.
Table 2.
Study characteristics of studies investigating diabetes mellitus (of 37 studies investigating diabetes mellitus, 36 are listed in Table 2).a
| Author, year | Country, setting | Study population, disease, controlled? | Burdenb | Study design | Sample size | Age (years)c, mean (SD) | Genderc (female), n (%) | Racec (White), n (%) |
| Bailey et al [41], 2019 | United States, 2 academic hospitals | Adults with DMd, on high-risk medication | − | Pilot or feasibility | 100 | 56 (11) | 57 (57) | 48 (48) |
| Boogerd et al [42], 2017 | Netherlands, 7 medical centers | Parents of children <13 years with DM type 1 | + | Pilot or feasibility | Ie=54, Cf=51 | 9.1 (2.7): Children | 30 (56) | NRg |
| Byczkowski et al [43], 2014 | United States, 1 academic hospital | Parents of children with DM (or CFh or JIAi) | ± | Cross-sectional | I=126, C=89 | 11 (NR) | 69 (54.8) | 115 (91.3) |
| Chung et al [44], 2017 | United States, outpatient care organization | Adults with DM | − | Cohort | I=12,485, C=2831 | 56 (12) | 5493 (44) | 5119 (41) |
| Conway et al [45], 2019 | United Kingdom, Scotland’s health system | Patients with DM | − | Cross-sectional | 1095 | 58 (12) | 405 (36.99) | 873 (78.73) |
| Devkota et al [46], 2016 | United States, 6 PCPsj | Patients with DM type 2 | − | Cohort | I=409, C=1101 | 58 (12)k | 235 (57.5) | 250 (61.1) |
| Dixon et al [47], 2016 | United States, 3 community centers | Adults with DM type 2 | − | Pilot or feasibility | 96 | 53 (11) | 56 (58) | 47 (49) |
| Graetz et al [48], 2018 | United States, integrated health system | Adults with DM | − | Cross-sectional | 267,208 | NR | 127,458 (47.7) | 116,770 (43.7) |
| Graetz et al [49], 2020 | United States, integrated health system | Adults with DM with at least 1 oral drug | − | Cross-sectional | 111,463 | 64 (13) | 51,545 (46.24) | 45,205 (40.56) |
| Grant et al [50], 2008 | United States, 11 PCPs | Adults with DM using medication | − | RCTl | I=126, C=118 | 59 (10) | 54 (42.9) | 117 (92.9) |
| Lau et al [51], 2014 | Canada, 1 academic hospital | Adults with DM | − | Cohort | I=50, C=107 | 55 (14) | 22 (44) | NR |
| Lyles et al [52], 2016 | United States, integrated health system | Adults with DM type 2 using statins | − | Cohort | I=8705, C=9055 | 61 (11)k | 4013 (46.1) | 3134 (36)k |
| Martinez et al [53], 2021 | United States, 4 medical centers | Adults with DM type 2 using medication | − | Pilot or feasibility | 60 | 58 (13) | 33 (55) | 41 (68) |
| McCarrier et al [54], 2009 | United States, 1 diabetes clinic | Adults <50 years with uncontrolled DM type 1 | + | RCT | I=41, C=36 | 57 (8) | 15 (37) | 39 (95) |
| Osborn et al [55], 2013 | United States, 1 academic hospital | Adults with DM type 2 using medication | − | Cross-sectional | I=62, C=13 | 57 (8) | 39 (63) | 46 (74) |
| Price-Haywood and Luo [56], 2017 | United States, integrated health system | Adults with DM or HTm | − | Cohort | I=10,497, C=90,522 | NR | 6205 (59.11) | 8055 (76.74) |
| Price-Haywood et al [57], 2018 | United States, integrated health system | Adults with DM or HT | − | Cohort | I=11,138, C=89,880 | 58 (13) | 6,204 (55.7) | NR |
| Quinn et al [58], 2018 | United States, 26 PCPs | Adults <65 years with DM type 2 | − | RCT | I=82, C=25 | 54 (8) | 39 (48) | 51 (62) |
| Reed et al [59], 2015 | United States, integrated health system | Adults with DM, HT, CADn, asthma, or CHFo | ± | Cross-sectional | 1041 | NR | 587 (56.4) | 618 (59.4) |
| Reed et al [60], 2019 | United States, integrated health system | Adults with DM+HT, CAD, asthma, or CHF | ± | Cross-sectional | 165,477 | NR | 79,594 (48.1) | NR (60.9) |
| Reed et al [61], 2019 | United States, integrated health system | Adults with DM, asthma, HT, CAD, CHF or CV event risk | ± | Cross-sectional | I=1392, C=407 | NR | 719 (51.7) | 816 (58.6) |
| Riippa et al [62], 2014 | Finland, 10 PCPs | Adults with DM, HT or HCp | − | RCT | I=80, C=57 | 61 (9) | 45 (56) | NR |
| Riippa et al [63], 2015 | Finland, 10 PCPs | Adults with DM, HT or HC | − | RCT | I=80, C=57 | 61 (9) | 45 (56) | NR |
| Robinson et al [64], 2020 | United States, 1 veteran hospital | Veterans with uncontrolled DM type 2 | − | Cross-sectional | I=446, C=754 | 66 (8) | 28 (6.3) | 384 (86.1) |
| Ronda et al [65], 2014 | Netherlands, 62 PCPs+1 hospital | Adults with DM | − | Cross-sectional | I=413, C=758 | 64 (12) | 154 (37.3) | 383 (93.6) |
| Ronda et al [66], 2015 | Netherlands, 62 PCPs+1 hospital | Adults with DM | − | Cross-sectional | I=413, C=219 | 59 (13) | 154 (37.3) | 383 (93.6) |
| Sabo et al [67], 2021 | United States, 21 practices | Adults with DM type 2 | − | Cohort | I=189, C=148 | 61 (13) | 75 (40.9) | 113 (72.9) |
| Sarkar et al [68], 2014 | United States, integrated health system | Adults with DM | − | Cohort | I=8705, C=9055 | 61 (11)k | 4013 (46.1) | 5072 (58.27) |
| Seo et al [69], 2020 | South Korea, 1 academic hospital | Patients with DM | − | Cohort | I=133, C=7320 | 54 (10) | 23 (17.3) | NR |
| Sharit et al [70], 2018 | United States, 1 veterans center | Overweight veterans with prediabetes | − | Pilot or feasibility | 38 | 58 (8) | 9 (24) | 8 (21)k |
| Shimada et al [71], 2016 | United States, Veteran registry | Veterans with uncontrolled DM, HT or LDLq | − | Cohort | I=50,482, C=61,204 | 61 (10) | 2060 (4.08) | 35,761 (70.84) |
| Tenforde et al [72], 2012 | United States, 1 community hospital | Adults <75 years with DM | − | Cohort | I=4036, C=6710 | 59 (10) | 1857 (46)k | 3,390 (84)k |
| van Vugt et al [73], 2016 | Netherlands, 52 PCPs | Patients with DM type 2 | − | RCT | I=66, C=66 | 68 (10) | 54 (41) | 91 (69) |
| Vo et al [74], 2019 | United States, integrated health system | Adults <80 years with DM type 2 | − | RCT | I=673, C=603 | 61 (10) | 296 (44) | 394 (58.5) |
| Wald et al [75], 2009 | United States, 230 PCPs | Patients with DM type 2 | − | RCT | 126 | 59 (NR) | 53 (42.1) | 117 (92.9) |
| Zocchi et al [76], 2021 | United States, nationwide | Patients with DM type 2, partly uncontrolled | − | Cohort | 95,043 | 63 (10) | 4,339 (4.57) | 68,954 (72.55) |
aAll studies are listed in Tables 2-5 and are reported in the disease category of the condition that is most prominently investigated. The study by Druss et al [77] is therefore listed in Table 5.
bIf conditions are considered to have a high disease burden or demand high self-management skills, a positive sign is shown. Otherwise, a sign is indicated. A ± sign indicates that multiple diseases have been studied, and only some of the diseases were considered to have a high disease burden.
cIf available, age (years), gender, and race were reported by digital health record users (“the intervention group”).
dDM: diabetes mellitus.
eI: intervention.
fC: control.
gNR: not reported.
hCF: cystic fibrosis.
iJIA: juvenile idiopathic arthritis.
jPCP: primary care practice.
kPresented numbers were estimated based on the data provided in the original articles.
lRCT: randomized controlled trial.
mHT: hypertension.
nCAD: coronary artery disease.
oCHF: congestive heart failure.
pHC: hypercholesterolemia.
qLDL: low-density lipoprotein.
Table 5.
Study characteristics of studies investigating other diseases (of 21 studies investigating other diseases, 20 are listed in Table 5). Diseases include kidney disease (n=3, 15%), mental health disorders (n=3, 15%), multiple sclerosis (n=2, 10%), inflammatory bowel disease (n=2, 10%), rheumatologic conditions (n=2, 10%), and others (n=8, 40%).a
| Author, year | Country, setting | Study population, disease, controlled? | Burdenb | Study design | Sample size | Age (years)c, mean (SD) | Genderc (female), n (%) | Racec (White), n (%) |
| Anand et al [103], 2017 | Thailand, HIV clinic | MSMd and transgender women with HIV, partly uncontrolled | + | RCTe | 186 | 30 (10)f | 7 (4) | 0 (0) |
| Bidmead and Marshall [104], 2016 | United Kingdom, 1 community hospital | Patients with IBDg | + | Cross-sectional | 60 | NRh | NR | NR |
| Crouch et al [105], 2015 | United States, 1 HIV clinic | Veterans with HIV, partly uncontrolled | + | Cross-sectional | Ii=20, Cj=20 | 43 (11) | 1 (5) | 19 (95) |
| Druss et al [106], 2014 | United States, 1 mental health center | Patients with a mental disorder+chronic condition | + | RCT | I=85, C=85 | 49 (7) | 42 (49) | 13 (15) |
| Druss et al [77], 2020 | United States, 2 mental health centers | Patients with a mental disorder+DMk, HTl, or HCm | + | RCT | I=156, C=155 | 51 (6.5) | 95 (61) | 29 (19) |
| Jhamb et al [107], 2015 | United States, 4 nephrology clinics | Adults visiting nephrology clinics, partly uncontrolled | + | Cross-sectional | 1098 | 58 (16) | 549 (50) | 952 (86.7) |
| Kahn et al [108], 2010 | United States, HIV clinic | Patients with HIV or AIDS | + | Pilot or feasibility | 136 | NR | 15 (11)f | 106 (78)f |
| Keith McInnes et al [109], 2013 | United States, 8 Veteran hospitals | Veterans with HIV, partly uncontrolled | + | Cross-sectional | 1871 | NR | 51 (2.73) | 342 (18.28) |
| Keith McInnes et al [110], 2017 | United States, Veterans care system | Veterans with HIV+detectable viral load, partly uncontrolled | + | Cohort | 3374 | NR | 128 (3.79) | 1130 (33.49) |
| Kiberd et al [111], 2018 | Canada, dialysis clinic | Adult with home dialysis | + | Pilot or feasibility | 41 | 57 (2) | 13 (48) | NR |
| Lee et al [112], 2017 | South Korea, 1 surgery department | Patients with cleft lip or cleft palate surgery | − | Pilot or feasibility | 50 | 36 (NR) | 33 (66) | NR |
| Miller et al [113], 2011 | United States, MSn clinic | Patients with MS | + | RCT | I=104, C=102 | 48 (9) | 73 (71.6) | 80 (78.4) |
| Navaneethanet al [114], 2017 | United States, multiple health centers | Adults with chronic kidney disease, partly uncontrolled | + | RCT | I=152, C=57 | 68 (NR)f | 79 (52) | 117 (77) |
| Plimpton [115], 2020 | United States, HIV clinic | Women with HIV, partly uncontrolled | + | Pilot or feasibility | 22 | 41 (11) | 22 (100) | 7 (32) |
| Reich et al [116], 2019 | United States, 1 community hospital | Adults with IBDo | + | RCT | I=64, C=63 | 42 (16) | 28 (46) | 48 (77) |
| Scott Nielsen et al [117], 2012 | United States, 1 academic center | Adults with MS | + | Cross-sectional | I=120, C=120 | 45 (11) | 90 (75) | 115 (95.8) |
| Son and Nahm [118], 2019 | United States, online senior community | Patients >49 years with 1 or more chronic conditions | ± | Secondary data analysis | 272 | 70 (9) | 191 (70.2) | 213 (78.3) |
| Tom et al [119], 2012 | United States, integrated health system | Parents of children age <6 years with 1 or more chronic conditions | ± | Cross-sectional | I=166, C=90 | 3 (1) | 66 (39.8) | 113 (68.1) |
| van den Heuvel et al [120], 2018 | Netherlands, 3 hospitals | Adults with bipolar disorder | + | Cross-sectional | 39 | 45 (11) | 44 (67) | NR |
| van der Vaart et al [121], 2014 | Netherlands, 1 hospital | Patients with rheumatoid arthritis | + | Cross-sectional | 214 | 62 (13) | 140 (65.4) | NR |
aAll studies are listed in Tables 2-5 and are reported in the disease category of the condition that is most prominently investigated. The study by Byczkowski et al [43] is therefore listed in Table 2.
bIf conditions are considered to have a high disease burden or demand high self-management skills, a positive sign is shown. Otherwise, a sign is indicated. A ± sign indicates that multiple diseases have been studied, and only some of the diseases were considered to have a high disease burden.
cIf available, age (years), gender, and race were reported by digital health record users (“the intervention group”).
dMSM: men who have sex with men.
eRCT: randomized controlled trial.
fPresented numbers were estimated based on the data provided in the original articles.
gIBD: inflammatory bowel disease.
hNR: not reported.
iI: intervention.
jC: control.
kDM: diabetes mellitus.
lHT: hypertension.
mHC: hypercholesterolemia.
nMS: multiple sclerosis.
oIBD: inflammatory bowel disease.
Table 3.
Study characteristics of studies investigating cardiopulmonary diseases (of 21 studies investigating cardiopulmonary diseases, 11 are listed in Table 3).a
| Author, year | Country, setting | Study population, disease, controlled? | Burdenb | Study design | Sample size | Age (years)c, mean (SD) | Genderc (female), n (%) | Racec (White), n (%) |
| Aberger et al [78], 2014 | United States, renal transplant clinic | Postrenal transplant patients with HTd | + | Pilot or feasibility | 66 | 54 (NRe) | 34 (52)f | 48 (72)f |
| Ahmed et al [79], 2016 | Canada, 2 academic hospitals | Adults with asthma using medication | + | RCTg | Ih=49, Ci=51 | NR | 32 (68) | NR |
| Apter et al [80], 2019 | United States, multicenter hospitals | Adults with asthma using prednisone | + | RCT | I=151, C=150 | 49 (13) | 270 (89.7) | 4 (1.3) |
| Fiks et al [81], 2015 | United States, 3 PCPsj | Children aged 6-12 years with asthma, partly uncontrolled | + | RCT | I=30, C=30 | 8.3 (1.9) | 26 (87) among parents | 13 (43) |
| Fiks et al [82], 2016 | United States, 20 PCPs | Children aged 6-12 years with asthma, partly uncontrolled | + | Pilot or feasibility | I=237, C=8896 | NR | 101 (42.8) | 144 (61.5) |
| Kogut et al [83], 2014 | United States, 1 community hospital | Adults aged >49 years with cardiopulmonary disorders | ± | Pilot or feasibility | 30 | NR | 14 (47) | NR |
| Kim et al [84], 2019 | South Korea, 1 academic hospital | Patients with obstructive sleep apnea | − | RCT | I=30, C=13 | 43 (10)f | NR (15) | NR |
| Lau et al [85], 2015 | Australia, nationwide | Adults with asthma | + | RCT | I=154, C=176 | 40 (14) | 124 (80.5) | NR |
| Manard et al [86], 2016 | United States, PCP registry | Adults with uncontrolled HT | − | Cohort | I=400, C=1171 | 61 (12) | 262 (65.5) | 72 |
| Toscos et al [87], 2020 | United States, 1 community hospital | Patients with nonvalvular AFk with OACl | + | RCT | I=76, C=77 | 71 (9) | 60 (37.5) | 153 (99.4) |
| Wagner et al [88], 2012 | United States, 24 PCPs | Patients with hypertension, partly uncontrolled | − | RCT | I=193, C=250 | 55 (12) | 145 (75.1) | 96 (50.5) |
aAll studies are listed in Tables 2-5 and are reported in the disease category of the condition that is most prominently investigated. The studies by Price-Haywood and Luo [56], Price-Haywood et al [57], Reed et al [59], Reed et al [60], Reed et al [61], Riippa et al [62], Riippa et al [63], Shimada et al [71] are listed in Table 2. The study by Martinez Nicolás et al [89] is listed in Table 4. The study by Druss et al [77] is therefore listed in Table 5.
bIf conditions are considered to have a high disease burden or demand high self-management skills, a positive sign is shown. Otherwise, a sign is indicated. A ± sign indicates that multiple diseases have been studied, and only some of the diseases were considered to have a high disease burden.
cIf available, age (years), gender, and race were reported by digital health record users (“the intervention group”).
dHT: hypertension.
eNR: not reported.
fPresented numbers were estimated based on the data provided in the original articles.
gRCT: randomized controlled trial.
hI: intervention.
iC: control.
jPCP: primary care practice.
kAF: atrial fibrillation.
lOAC: oral anticoagulant drug.
Table 4.
Study characteristics of studies investigating hematological and oncological diseases (n=14).
| Author, year | Country, setting | Study population, disease, controlled? | Burdena | Study design | Sample size | Age (years)b, mean (SD) | Genderb (female), n (%) | Racec (White), n (%) |
| Cahill et al [90], 2014 | United States, cancer center | Adults with glioma | + | Cross-sectional | 186 | 44 (13) | 87 (46.8) | 149 (86.1) |
| Chiche et al [91], 2012 | France, 1 community hospital | Adults with ITPc | ± | RCTd | Ie=28, Cf=15 | 48 (15)g | 21 (75) | NRh |
| Collins et al [92], 2003 | United Kingdom, hemophilia centers | Patients with hemophilia >11 years | + | Pilot or feasibility | 10 | NR | NR | NR |
| Coquet et al [93], 2020 | United States, cancer center | Patients with cancer+chemotherapy | + | Cohort | I=3223, C=3223 | 59 (15) | 1,554 (49.78) | 1,804 (49.68) |
| Groen et al [94], 2017 | Netherlands, cancer center | Patients with lung cancer | + | Pilot or feasibility | 37 | 60 (8) | 16 (47) | 37 (100) |
| Hall et al [95],2014 | United States, Cancer Center | Patients with resection for CRCi or ECj | + | Pilot or feasibility | 49 | 59 (12)g | 37 (76) | 48 (98) |
| Hong et al [96], 2016 | United States, academic pediatric hospital | Children aged 13-17 years with cancer or a blood disorder+parents | + | Cross-sectional | 46 | 15 (1.2)g | 10 (63) among children | NR |
| Kidwell et al [97], 2019 | United States, multicenter hospitals | Patients aged 13-24 years with sickle cell disease | + | Pilot or feasibility | 44 | 19 (NR) | 24 (55) | 0 (0) |
| Martinez Nicolás et al [89], 2019 | Spain, 4 community hospitals | Patients with COPDk, CHFl, or hematologic malignancy | + | Pilot or feasibility | 577,121 | 42 (23) | 319,725g (55) | NR |
| O’Hea et al [98], 2021 | United States, cancer centers | Adult women with nonmetastatic breast cancer ending treatment | + | RCT | I=100, C=100 | 61 (11) | 100 (100) | 85 (85) |
| Pai et al [99], 2013 | Canada, cancer center | Adult men with prostate cancer | + | Cross-sectional | 17 | 64 (7)g | 0 (0) | 16 (95) |
| Tarver et al [100], 2019 | United States, academic hospital | Patients with colorectal cancer | + | Cross-sectional | 22 | 58 (10) | 10 (45) | NR |
| Wiljer et al [101], 2010 | Canada, breast cancer registry | Patients with breast cancer | + | Pilot or feasibility | 311 | NR | 303 (99.7) | NR |
| Williamson et al [102], 2017 | United States, pediatric cancer center | Pediatric cancer survivors | + | Cohort | 56 | NR | 27 (48) | 49 (88) |
aIf conditions are considered to have a high disease burden or demand high self-management skills, a positive sign is shown. Otherwise, a sign is indicated. A ± sign indicates that multiple diseases have been studied, and only some of the diseases were considered to have a high disease burden.
bIf available, age (years), gender, and race were reported by digital health record users (“the intervention group”).
cITP: idiopathic thrombocytopenic purpura.
dRCT: randomized controlled trial.
eI: intervention.
fC: control.
gPresented numbers were estimated based on the data provided in the original articles.
hNR: not reported.
iCRC: colorectal cancer.
jEC: endometrial cancer.
kCOPD: chronic obstructive pulmonary disease.
lCHF: congestive heart failure.
Explanations of the patient-centered digital health records investigated in each study are presented in Tables 6-9. Patient-centered digital health records range from a pilot patient portal enabling patients to view a limited set of their medical data to comprehensive PHRs, offering extensive data access and enabling appointment scheduling and prescription refill requests. A minority (12/81, 15%) of studies specifically evaluated ≥1 digital health record features such as secure messaging or a medication adherence module. In addition, 15% (12/81) of studies used a hybrid approach to assess a combination of a digital health record with a connected device, or with training, coaching, or face-to-face visits.
Table 6.
Patient-centered digital health record descriptions for disease category diabetes mellitus (of 37 studies investigating diabetes mellitus, 36 are listed in Table 6).a
| Author, year | Name | Type | What is evaluated?b | Passive features | Active features | Focusc | ||||||
| Bailey et al [41], 2019 | Electronic Medication Complete Communication | PPd | Adherence module alone | View health information (medical summary), read after-visit summary, read educational material | Report medication concerns, monitor medication use | Active | ||||||
| Boogerd et al [42], 2017 | Sugarspace | PP | PP | View treatment goals, read educational material | Parent-professional communication, peer support | Active | ||||||
| Byczkowski et al [43], 2014 | In-house developed | PP | PP | View health information (including laboratory results, medication), view appointments, read disease-specific information | Messaging, upload documents, receive reminders | Passive | ||||||
| Chung et al [44], 2017 | Not reported | PP | Messaging | View health information | Messaging | Active | ||||||
| Conway et al [45], 2019 | My Diabetes My Way | Tethered PHRe | PHR | View health information from primary and secondary care (including clinical parameters, medication, and correspondence), read educational material | Report self-measurements | Passive | ||||||
| Devkota et al [46], 2016 | MyChart | PP | PP | View health information (including laboratory results, diagnoses, medication, vital signs), read educational material | Messaging, request prescription refills, schedule appointments, pay bills | Passive | ||||||
| Dixon et al [47], 2016 | CareWeb | PP | Medication module alone | View health information (including measurements, medication) | Report barriers to medication adherence | Passive | ||||||
| Graetz et al [48], 2018 and Graetz et al [49], 2020 | “Kaiser Permanente portal” | PP | PP | View health information (including laboratory results) | Messaging, schedule appointments, request prescription refills, pay bills | Active | ||||||
| Grant et al [50], 2008 | Not reported | PP | PP | View health information (including medication, laboratory results) | Edit medication lists, messaging, report adherence barriers or adverse effects | Active | ||||||
| Lau et al [121], 2014 | BCDiabetes | PP | PP | View health information (including laboratory results), view care plan, read educational material | Messaging, use a journal | Passive | ||||||
| Lyles et al [52], 2016 | “Kaiser Permanente portal” | PP | Medication module alone | View health information (including medical history, laboratory results, and visit summaries) | Messaging, schedule appointments, request prescription refills | Active | ||||||
| Martinez et al [53], 2021 | My Diabetes Care, part of My Health at Vanderbilt | PP | Diabetes module | View health information (including laboratory results and vaccinations), visualize information, read educational material | Messaging, peer support, decision support tools | Active | ||||||
| McCarrier et al [54], 2009 | Living with Diabetes Intervention | PP | PP+case manager | View health information (including correspondence, action plans, and laboratory results), read diabetes-related information | Upload blood glucose readings, use a journal | Active | ||||||
| Osborn et al [55], 2013 | My Health At Vanderbilt | PP | PP | View health information (including vital signs, laboratory results, and medication), read educational information | Messaging, manage appointments, use health screening tools, pay bills | Passive | ||||||
| Price-Haywood and Luo [56], 2017 and Price-Haywood et al [57], 2018 | MyOchsner | PP | PP | View health information (including an after-visit summary, allergies, and laboratory results) | Messaging, request prescription refills, schedule appointments | Passive | ||||||
| Quinn et al [58], 2018 | Not reported | PP | PP | View self-reported health information (including medication and measurements), read educational material | Messaging, report self-measurements and medication changes, receive automated feedback | Active | ||||||
| Reed et al [59], 2015 | “Kaiser Permanente portal” | PP | Messaging alone | View health information (including laboratory results and correspondence) | Messaging, request prescription refills, schedule appointments | Active | ||||||
| Reed et al [60], 2019 (1) and Reed et al [61], 2019 | “Kaiser Permanente portal” | PP | PP | View health information from primary care and secondary care (including laboratory results and visit summaries) | Messaging, request prescription refills, schedule visits | Passive | ||||||
| Riippa et al [62], 2014 and Riippa et al [63], 2015 | Not reported | PP | PP | View health information (including diagnoses, laboratory results, vaccinations, and medication), view care plan, read educational material | Messaging | Passive | ||||||
| Robinson et al [64], 2020 | My HealtheVet | PP | Messaging alone | View health information (including medication and correspondence), view appointments | Messaging, request prescription refills, receive reminders, upload notes and measurements, use a journal | Passive | ||||||
| Ronda et al [65], 2014 and Ronda et al [66], 2015 | Digitaal logboek | PP | PP | View diabetes-specific health information (including laboratory results, diagnoses, and medication), view treatment goals, view appointments | Messaging, upload self-measurements | Passive | ||||||
| Sabo et al [67], 2021 | Diabetes Engagement and Activation Platform | PP | PP | View health information (including medication and self-reported glucose measurements) | Report diet, physical activity, blood glucose measurements, complications, mental health and goals, receive alerts | Active | ||||||
| Sarkar et al [68], 2014 | “Kaiser Permanente portal” | PP | PP | View health information (including medical history, laboratory results, and visit summaries), view appointments | Messaging, request prescription refills | Passive | ||||||
| Seo et al [69], 2020 | My Chart in My Hand | Tethered PHR | PHR+sugar function | View health information (including laboratory results, medication, allergies, diagnoses) | Edit information, schedule appointment; sugar function: log treatment, food intake, and exercise | Active | ||||||
| Sharit et al [70], 2018 | My HealtheVet | PP | Track Health module+wearable | View health information (including medication and correspondence), view appointments | Messaging, request prescription refills, receive reminders; track Health module: record diet and activity, upload data from connected accelerometer | Active | ||||||
| Shimada et al [71], 2016 | My HealtheVet | PP | Messaging, prescription refills | View health information (including medication and correspondence), view appointments | Messaging, request prescription refills, receive reminders, upload notes and self-measurements, use a journal | Active | ||||||
| Tenforde et al [72], 2012 | MyChart | PP | PP | View health information (including diagnoses and laboratory results), read diabetes educational material | Messaging, view glucometer readings, receive reminders | Passive | ||||||
| van Vugt et al [73], 2016 | e-Vita | Tethered PHR | PHR+personal coach | View health information (measurements), read diabetes education | Messaging, self-management support program for personal goal setting and evaluation | Active | ||||||
| Vo et al [74], 2019 | “Kaiser Permanente portal” | PP | PP+PreVisit Prioritization messaging | View health information (including medical history, laboratory results, and visit summaries), view appointments | PreVisit Prioritization messaging to report priorities before a clinic visit, request prescription refills | Active | ||||||
| Wald et al [75], 2009 | Patient Gateway | Tethered PHR | PHR | View health information (including medication, allergies, and laboratory results) | Suggest corrections, report care concerns, ask for referrals, create care plans before visits | Active | ||||||
| Zocchi et al [76], 2021 | My HealtheVet | PP | PP | View health information (including medication, laboratory results, imaging, and correspondence) | Messaging, requesting prescription refills, download health information | Active | ||||||
aAll studies are listed once in Tables 2-5 and are reported in the disease category of the condition that is most prominently investigated. We have included only the functionalities that the authors have reported in their articles. We have applied the taxonomy as presented in Textbox 1 on the information provided by the authors. Therefore, our classification of patient-centered digital health records might not correspond with the term used by the authors.
bIn this column, we indicated whether authors evaluated the complete patient-centered digital health record, or only part of it.
cBy definition, patient-centered digital health records have both passive and active features. In this column, we indicate whether patient-centered digital health records predominantly offer passive or active features. In passive features, patients receive information but do not actively add it. In terms of active features, patients perform an action and actively engage with the portal.
dPP: patient portal.
ePHR: personal health record.
Table 9.
Patient-centered digital health record descriptions for disease category other diseases (of 21 studies investigating other diseases, 20 are listed in Table 9).a
| Author, year | Name | Type | What is evaluated?b | Passive features | Active features | Focusc | ||||||
| Anand et al [103], 2017 | Adam’s Love | PPd | PP | View health information (HIV test results), receive appointment reminders | Schedule HIV test appointments, use e-counseling, receive appointment reminders | Active | ||||||
| Bidmead et al [104], 2016 | Patients Know Best | Tethered PHRe | PHR | View health information (including medication, laboratory results, and correspondence), read educational material | Communication with health care providers, upload and share health information | Active | ||||||
| Crouch et al [105], 2015 | My HealtheVet | PP | PP | View health information (including laboratory results and correspondence) | Messaging, request prescription refills | Passive | ||||||
| Druss et al [106], 2014 | MyHealthRecord | PP | PP+training | View health information (including diagnoses, measurements, laboratory results, medication, and allergies), view treatment goals | Prompts remind patients of routine preventive service | Passive | ||||||
| Druss et al [77], 2020 | Not reported | PP | PP+training | View health information (including medication, allergies, measurements, and laboratory results) | Formulate long-term goals, that are translated into action plans with progress tracking | Active | ||||||
| Jhamb et al [107], 2015 | Not reported | PP | PP | View health information (including diagnoses, allergies, immunizations, and laboratory results) | Messaging, schedule appointments, request prescription refills | Passive | ||||||
| Kahn et al [108], 2010 | MyHERO | PP | PP | View health information (including diagnoses, medication, laboratory results, and allergies), view appointments, read information on interpreting test results | Upload notes and self-measurements | Passive | ||||||
| Keith McInnes et al [109], 2013 and Keith McInnes et al [110], 2017 | My HealtheVet | PP | PP | View health information (including medication and correspondence), view appointments | Messaging, request prescription refills, receive reminders, upload notes and self-measurements, use a journal | Passive | ||||||
| Kiberd et al [111], 2018 | RelayHealth | PP | PP | View health information (including test results and medication) | Messaging | Active | ||||||
| Lee et al [112], 2017 | CoPHR | PP | PP | View health information (including diagnoses, laboratory results, medication, allergies, vital signs, and correspondence), view appointments, view treatment plan, read educational information | Manage and edit appointments and health information | Passive | ||||||
| Miller et al [113], 2011 | Mellen Center Care Online | Untethered PHR | PHR | Review previously entered symptoms and HRQoLf | Messaging, report symptoms and HRQoL and evaluate changes, preparation for appointments | Active | ||||||
| Navaneethan et al [114], 2017 | MyChart | PP | PP+part of users received training | View health information (including medication and laboratory results), read educational material | Messaging, schedule appointments, request prescription refills | Passive | ||||||
| Plimpton [115] 2020 | Not reported | PP | PP | View health information | Messaging | Passive | ||||||
| Reich et al [116], 2019 | MyChart | PP | PP | View health information (including laboratory results, diagnoses, medication, and vital signs) | Messaging | Passive | ||||||
| Scott Nielsen et al [117], 2012 | PatientSite10 | PP | PP | View health information (including laboratory results, and imaging), read educational material | Messaging, schedule appointments, request prescription refills, upload self-measurements, pay bills | Active | ||||||
| Son and Nahm [118], 2019 | MyChart | PP | PP+training | View health information (including medication and laboratory results), read educational material | Messaging, schedule appointments, request prescription refills | Passive | ||||||
| Tom et al [119], 2012 | MyGroupHealth | PP | PP | View health information (including diagnoses, medication, and test results), read after-visit summaries, proxy access | Messaging, schedule appointments | Passive | ||||||
| van den Heuvel et al [120], 2018 | “PHR-BD” | Tethered PHR | Tethered PHR+mood chart | View health information (including diagnoses, laboratory results, medication, and correspondence), read educational material | Messaging, report symptoms in a mood chart, view personal crisis plan | Active | ||||||
| van der Vaart et al [121], 2014 | Not reported | PP | PP | View health information (including diagnoses, medication, and laboratory results), read educational material | Report and monitor HRQoL outcomes | Active | ||||||
aAll studies are listed once in Tables 2-5 and are reported in the disease category of the condition that is most prominently investigated. We have included only the functionalities that the authors have reported in their articles. We have applied the taxonomy as presented in Textbox 1 on the information provided by the authors. Therefore, our classification of patient-centered digital health records might not correspond with the term used by the authors.
bIn this column, we indicated whether authors evaluated the complete patient-centered digital health record, or only part of it.
cBy definition, patient-centered digital health records have both passive and active features. In this column, we indicate whether patient-centered digital health records predominantly offer passive or active features. In passive features, patients receive information but do not actively add it. In terms of active features, patients perform an action and actively engage with the portal.
dPP: patient portal.
ePHR: personal health record.
fHRQoL: health-related quality of life.
Table 7.
Patient-centered digital health record descriptions for disease category cardiopulmonary diseases (of 21 studies investigating cardiopulmonary diseases, 11 are listed in Table 7).a
| Author, year | Name | Type | What is evaluated?b | Passive features | Active features | Focusc | ||||||
| Aberger et al [78], 2014 | Good Health Gateway | PPd | PP+BPe cuff | View BP measurements, view treatment goals | Communicate self-reported adherence, receive automated and tailored feedback | Active | ||||||
| Ahmed et al [79], 2016 | My Asthma Portal | PP | PP | View health information (including medication and diagnoses), read general and tailored asthma information | Monitor and receive feedback on self-management practices | Passive | ||||||
| Apter et al [80], 2019 | MyChart | PP | PP | View health information (including laboratory results, vaccinations, and medication), view appointments | Messaging, request prescription refills, schedule appointments | Passive | ||||||
| Fiks et al [81], 2015 and Fiks et al [82], 2016 | MyAsthma | PP | PP | View care plan, read educational material | Report symptoms, treatment adherence, concerns and side effects | Active | ||||||
| Kim et al [84], 2019 | MyHealthKeeper | Tethered PHRf | PHR+activity tracker | View previously uploaded self-reported data | Upload self-reported data (eg, diet, sleep, weight, BP, step count), connect with wearables, receive feedback from health care providers | Active | ||||||
| Kogut et al [83], 2014 | ER-Card | Untethered PHR | PHR+home visits by pharmacists | View patient-reported medication list | Pharmacists view and review patient-reported medication lists, and discuss potential concerns in home visits | Active | ||||||
| Lau et al [85], 2015 | Healthy.me | Untethered PHR | PP+extra feature | View Asthma Action Plan, read educational content | Schedule appointments, peer support, self-report medication, use a journal | Passive | ||||||
| Manard et al [86], 2016 | Not reported | PP | PP+BP cuff | View health information (including laboratory results, vital signs, and diagnoses) | Messaging, request prescription refills, upload measurements from connected BP cuff | Passive | ||||||
| Toscos et al [87], 2020 | MyChart | PP | PP+smart pill bottle | View health information (including laboratory results, vaccinations, and medication), view appointments | Messaging, request prescription refills, schedule appointments Smart Pill Bottle: a device that sends notifications when a user opens or fails to open the lid, based on the dose schedule | Active | ||||||
| Wagner et al, 2012 [88] | MyHealthLink | Tethered PHR | PHR | View health information (including diagnoses, medication, and allergies), read educational material | Messaging, goal setting, upload self-measurements (including BP) | Active | ||||||
aAll studies are listed once in Tables 2-5 and are reported in the disease category of the condition that is most prominently investigated. We have included only the functionalities that the authors have reported in their articles. We have applied the taxonomy as presented in Textbox 1 on the information provided by the authors. Therefore, our classification of patient-centered digital health records might not correspond with the term used by the authors.
bIn this column, we indicated whether authors evaluated the complete patient-centered digital health record, or only part of it.
cBy definition, patient-centered digital health records have both passive and active features. In this column, we indicate whether patient-centered digital health records predominantly offer passive or active features. In passive features, patients receive information but do not actively add it. In terms of active features, patients perform an action and actively engage with the portal.
dPP: patient portal.
eBP: blood pressure.
fPHR: personal health record.
Table 8.
Patient-centered digital health record descriptions for disease category hematological and oncological diseases (n=14).a
| Author, year | Name | Type | What is evaluated?b | Passive features | Active features | Focusc | ||||||
| Cahill et al [90], 2014 | MyMDAnderson | Tethered PHRd | PHR | View health information (including correspondence, operative reports, laboratory results, and imaging), read education material | Messaging, request prescription refills, schedule appointments | Passive | ||||||
| Chiche et al [91], 2012 | Sanoia | PPe | PP+ITPf features | View health information (including allergies, vaccinations, medication, and test results), ITP-specific educational material, read emergency protocols | Messaging | Passive | ||||||
| Collins et al [92], 2003 | Advoy | PP | PP | View health information (treatment regimen), read educational material | Registration of symptoms and medication use, automated alerts are sent to professionals | Active | ||||||
| Coquet et al [93], 2020 | MyHealth portal | PP | Email use | View health information (including laboratory results) | Messaging, schedule appointments, request prescription refills, pay bills | Active | ||||||
| Groen et al [94], 2017 | MyAVL | PP | PP | View health information (including laboratory results, lung function, and correspondence), view appointments, read personalized information | Upload patient-reported outcomes, receive tailored physical activity advice | Active | ||||||
| Hall et al [95], 2014 | MyFoxChase | PP | Genetic screening | View health information (including laboratory results), view appointments, read educational material | Messaging, receive alerts if genetic screening results are available | Passive | ||||||
| Hong et al [96], 2016 | MyChart | PP | PP | View health information (including laboratory results, medication, allergies) | Messaging, schedule appointments, request prescription refills, use a journal | Passive | ||||||
| Kidwell et al [97], 2019 | MyChart | PP | PP | View health information (including laboratory results, medication, diagnoses, and allergies), view appointments, read information about sickle cell disease | Messaging | Passive | ||||||
| Martinez Nicolás et al [89], 2019 | Not reported | PP | PP | View health information (including laboratory results, imaging, and medication) | Messaging, teleconsulting, schedule appointments, upload glucose measurements | Active | ||||||
| O’Hea et al [98], 2021 | Polaris Oncology Survivorship Transition | PP | PP | View health information (including diagnoses, operative reports, and medication), view appointments, read educational material | Request a referral | Passive | ||||||
| Pai et al [99], 2013 | PROVIDER | Tethered PHR | PHR | View health information (including laboratory results, medication, pathology, imaging, and correspondence), read educational material | Messaging, use decision support tools, fill in questionnaires | Passive | ||||||
| Tarver et al [100], 2019 | OpenMRS | Tethered PHR | PHR+extra feature | View health information (including treatment history, diagnoses, and care plan), view a treatment summary, read educational material | Messaging, peer support | Passive | ||||||
| Wiljer et al [101], 2010 | InfoWell | Tethered PHR | PHR | View health information (including medication, laboratory results, imaging, and pathology), view appointments | Patients can organize and upload care information | Passive | ||||||
| Williamson et al [102], 2017 | SurvivorLink | Untethered PHR | PHR | Read educational material | Upload health documents and share these with professionals | Active | ||||||
aAll studies are listed once in Tables 2-5 and are reported in the disease category of the condition that is most prominently investigated. We have included only the functionalities that the authors have reported in their articles. We have applied the taxonomy as presented in Textbox 1 on the information provided by the authors. Therefore, our classification of patient-centered digital health records might not correspond with the term used by the authors.
bIn this column, we indicated whether authors evaluated the complete patient-centered digital health record, or only part of it.
cBy definition, patient-centered digital health records have both passive and active features. In this column, we indicate whether patient-centered digital health records predominantly offer passive or active features. In passive features, patients receive information but do not actively add it. In terms of active features, patients perform an action and actively engage with the portal.
dPHR: personal health record.
ePP: patient portal.
fITP: idiopathic thrombocytopenic purpura.
Outcomes
An overview of reported associations for each health outcome is shown in Figure 2. The proportions of beneficial effects reported per health outcome are presented in Multimedia Appendices 3 and 4. For high-quality studies, proportions are presented in Multimedia Appendix 3. An overview of study conclusions and associated outcomes is presented in Tables 10-13. Studies were grouped according to disease group.
Figure 2.
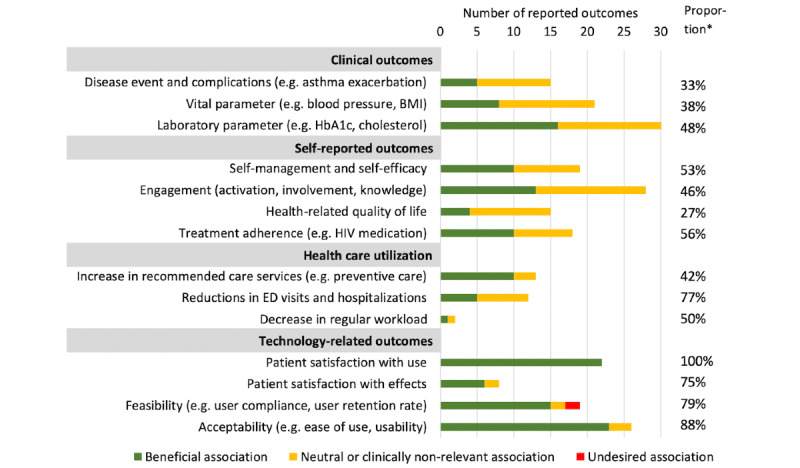
Health outcomes associated with patient-centered digital health record use. Associations refer to meaningful clinical effects or statistical significance. If studies report multiple health outcome within 1 category, each health outcome is included separately. *The proportion of health outcomes for which beneficial effects were reported. ED: emergency department.
Table 10.
Conclusions and health outcomes: all studies investigating diabetes (n=37), of which 8 (22%) are of high methodological quality.a
| Author, year | Participants | Comparison | Main conclusion | Study design | Clinical | Patient reported | Care utilization | Technology | Qualityb |
| Boogerd et al [42], 2017 | Parents of children with DMc type 1 | PPd users versus PP nonusers | Patient portal use is not associated with less parental stress. The more stress, the more parents use the portal. | QEe |

|

|
—f |

|

|
| Lau et al [51], 2014 | Patients with DM | Pretest PP nonuse versus posttest PP use | Patient portal use is associated with improved glycemic control. | Cohort |

|
— | — | — |

|
| Lyles et al [52], 2016 | Adults with DM type 2 using statins, registered for PP | Prescription refill use versus no refill use | Requesting prescription refills is associated with improved statin adherence. | Cohort | — |

|
— | — |

|
| McCarrier et al [54], 2009 | Adults aged <50 years with uncontrolled DM type 1 | Nurse-aided PP users versus PP nonusers | Patient portal use results in improved self-efficacy, but not in improved glycemic control. | RCTg |

|

|
— |

|

|
| Price-Haywood and Luo [56], 2017 | Adults with DM (or HTh) | PP users versus PP nonusers | Patient portal use is associated with more primary care visits and telephone encounters, but not with less hospitalizations or EDi visits. | Cohort |

|
— |

|
— |

|
| Sarkar et al [68], 2014 | Adults with DM, registered for PP | Recurrent prescription refill use versus occasional refill use versus no refill use | Recurrent use of prescription refills is associated with improvements in adherence and lipid control. | Cohort |

|
— | — | — |

|
| Shimada et al [71], 2016 | Veterans with uncontrolled DM, registered for PP | Messaging and prescription refills users versus PP users who use neither | Messaging or requesting prescription refills is associated with improved glycemic control. | Cohort |

|
— | — | — |

|
| van Vugt et al [73], 2016 | Patients with DM type 2, registered for PHRj | PHR+personal coach versus PHR use alone | PHR use does not result in improved glycemic control, self-care, distress, nor well-being, regardless of personal coaching. | RCT |

|

|
— |

|

|
| Dixon et al [47], 2016 | Adults with DM type 2 | Pretest PP nonusers versus posttest PP users | Patient portal use is associated with improved adherence, but not with changes in clinical outcomes nor care utilization. | QE |

|

|

|
— |

|
| Druss et al [77], 2020 | Patients with a mental disorder+DM, HT or HCk | PP users versus PP nonusers | Patient portal use does not result in clinically relevant improvements in perceived quality of care, patient activation nor HRQoLl. | RCT |

|

|

|
— |

|
| Graetz et al [49], 2020 | Adults with DM with at least 1 oral drug | PP users versus PP nonusers | Patient portal use is associated with small, likely irrelevant improvements in glycemic control and medication adherence. | Cross |

|

|
— | — |

|
| Grant et al [50], 2008 | Adults with DM using medication | Tethered PP use versus untethered PP use | Using a tethered patient portal results in increased patient participation, but not improved glycemic control. | RCT |

|

|
— | — |

|
| Reed et al [60], 2019 | Adults with DM+HT, asthma, CADm, or CHFn | PP users versus PP nonusers | Patient portal use is associated with more outpatient office visits, and with reduced ED visits and preventable hospitalizations. | Cross |

|
— |

|
— |

|
| Riippa et al [62], 2014 | Adults with DM, HT, or HC | PP users versus PP nonusers | Patient portal use does not result in clinically relevant improvements in patient activation, except among adults with low baseline activation. | RCT | — |

|
— | — |

|
| Riippa et al [63], 2015 | Adults with DM, HT, or HC | PP users versus PP nonusers | Patient portal use does not result in clinically relevant improvement in patient activation nor HRQoL. | RCT | — |

|

|

|

|
| Robinsonet al [64], 2020 | Veterans with uncontrolled DM type 2, registered for PP | Responders on team-initiated messages versus nonresponders | Responding on messages is associated with improved self-management and self-efficacy. | Cross | — |

|
— | — |

|
| Ronda et al [65], 2014 | Adults with DM | Recurrent PP users versus PP nonusers | Recurrent patient portal use is associated with better self-efficacy and knowledge. | Cross | — |

|
— |

|

|
| Ronda et al [66], 2015 | Adults with DM, registered for PP | Persistent users versus early quitters | Recurrent users believe the patient portal increases disease knowledge, and they find it useful. | Cross | — |

|
— |

|

|
| Sabo et al [67], 2021 | Adults with DM type 2, registered for PP | PP users versus PP nonusers | Patient portal use has minor, clinically irrelevant effects on BMI, and no effects on glycemic control nor blood pressure. | RCT |

|
— | — | — |

|
| Seo et al [69], 2020 | Patients with DM, registered for PHR | Continuous users versus noncontinuous users | Continuous use of a tethered PHR is associated with slightly improved glycemic control. Clinical implications are doubtful. | Cohort |

|
— | — | — |

|
| Sharit et al [70], 2018 | Overweight veterans with prediabetes | Pretest PP nonuse versus posttest PP use | Using an accelerometer-connected patient portal is associated with improvements in physical activity and blood pressure. | QE |

|

|
— |

|

|
| Tenforde et al [72], 2012 | Adults aged <75 years with DM | PP users versus PP nonusers | Patient portal use is associated with slightly improved diabetes control, lipid profile, and blood pressure. Clinical implications are doubtful. | Cohort |

|
— |

|
— |

|
| Vo et al [74], 2019 | Adults aged <80 years with DM type 2, registered for PP | Previsit message use versus no previsit message use | Sending previsit prioritization messages does not result in improved glycemic control, but does result in improved perceived shared-decision-making. | RCT |

|

|
— | — |

|
| Zocchi et al [76], 2021 | Patients with DM type 2, registered for PP | PP users | Among existing patient portal users with uncontrolled DM or high LDLo, increased use is associated with improved control. | Cohort |

|
— | — | — |

|
| Bailey et al [41], 2019 | Adults with DM, on high-risk medication | PP users | Patients are satisfied with the patient portal. | QE | — | — | — |

|

|
| Byczkowski et al [43], 2014 | Parents of children with DM (or CFp or JIAq) | PP users | Patients consider the patient portal to be useful in managing and understand their child’s disease. | Cross | — |

|
— |

|

|
| Chung et al [44], 2017 | Adults with DM, registered for PP | Message users versus message nonusers | Using secure messaging is associated with better glycemic control. | Cohort |

|

|

|
— |

|
| Conway et al [45], 2019 | Patients with DM, registered for PP | PP users | Patients believe the tethered diabetes PHR might improve their diabetes self-care. | Cross | — |

|
— |

|

|
| Devkota et al [46], 2016 | Patients with DM type 2 | PP users who read and write emails versus PP nonusers | Reading and writing emails is associated with improved glycemic control. | Cohort |

|

|
— | — |

|
| Graetz et al [48], 2018 | Adults with DM | PP users versus PP nonusers | Patient portal use is associated with improved adherence to medication and preventive care utilization. | Cross | — |

|

|
— |

|
| Martinez et al [53], 2021 | Adults with DM type 2 using medication, registered for PP | Pretest PP nonuse versus posttest PP use | Patient portal use results in clinically not relevant improvements in patient activation and self-efficacy. This is related to the very short follow-up period of the study. | QE | — |

|
— |

|

|
| Osborn et al [55], 2013 | Adults with DM type 2 using medication | PP users versus PP nonusers | Patient portal use is not associated with improved glycemic control, as compared with nonusers. However, among users, more frequent use is associated with improved glycemic control. | Cross |

|
— | — | — |

|
| Price-Haywood et al [57], 2018 | Adults with DM (or HT) | PP users versus PP nonusers | Messaging is associated with improved glycemic control. | Cohort |

|
— | — | — |

|
| Quinn et al [58], 2018 | Adults aged <65 years with DM type 2 | PP+extra module users versus PP users | Messaging is associated with better glycemic control. Note: glycemic parameters were predicted and not represent measurements. | RCT |

|

|
|||
| Reed et al [59], 2015 | Adults with DM, HT, asthma, CAD, or CHF, registered for PP | PP users | One-third of patients report that messaging in a patient portal results in less health care visits and improved overall health. | Cross | — |

|

|
— |

|
| Reed et al [61], 2019 | Adults with DM, asthma, HT, CAD, CHF, or CVr event risk | PP users versus PP nonusers | One-third of patients report that using the patient portal improves overall health. | Cross | — |

|
— |

|

|
| Wald et al [75], 2009 | Patients with DM type 2 | PHR users who created a previsit plan | Users who create a previsit care plan feel better prepared for visits. | RCT | — |

|
— |

|

|
aStudies are listed multiple times in Tables 10-13. Per disease category, the relevant subconclusion and health outcomes are described. Associations with health outcomes are color-coded as green for beneficial, yellow for neutral or clinically nonrelevant, or red for undesired. The half green and half yellow symbol implies that one study investigated multiple outcomes in one category and reported beneficial associations for some outcomes and neutral associations for others.
bQuality appraisal—green: high quality; yellow: medium quality; red: low quality.
cDM: diabetes mellitus.
dPP: patient portal.
eQE: quasi-experimental, including pretest-posttest studies and feasibility studies.
fThe study did not assess any health outcome in a certain category.
gRCT: randomized controlled trial.
hHT: hypertension.
iED: emergency department.
jPHR: personal health record.
kHC: hypercholesteremia.
lHRQoL: health-related quality of life.
mCAD: coronary artery disease.
nCHF: congestive heart failure.
oLDL: low-density lipoprotein.
pCF: cystic fibrosis.
qJIA: juvenile idiopathic arthritis.
rCV: cardiovascular.
Table 13.
Conclusions and health outcomes: studies investigating other diseases (n=21), of which 2 (10%) are of high methodological quality.a
| Author, year | Participants | Comparison | Conclusion | Study design | Clinical | Patient reported | Care utilization | Technology | Qualityb |
| Miller et al [113], 2011 | Patients with multiple sclerosis | PHRc use versus PHR that only enables messaging | Using an untethered PHR results in slightly improved HRQoLd, but not in improved self-efficacy, disease control nor health care utilization. | RCTe | — |

|

|
—f |

|
| Navaneethan et al [114], 2017 | Adults with chronic kidney disease | PPg users+coach versus PP users versus PP nonusers | Patient portal use, regardless of added training, does not result in improved kidney function, nor altered health care utilization. | RCT |

|
— |

|
— |

|
| Anand et al [103], 2017 | MSMh and transgender women with HIV | PP users | The patient portal is feasible and acceptable. | RCT | — | — | — |

|

|
| Druss et al [106], 2014 | Patients with a mental disorder+chronic condition | PP users versus PP nonusers | Patient portal use results in increased use of preventive health services and medical visits, but not in improved HRQoL. | RCT |

|

|

|
— |

|
| Druss et al [77], 2020 | Patients with a mental disorder+DMi, HTj, or HCk | PP users versus PP nonusers | Patient portal use does not result in clinically relevant improvements in perceived quality of care, patient activation, nor HRQoL. | RCT |

|

|

|
— |

|
| Jhamb et al [107], 2015 | Adults visiting nephrology clinics | PP users versus PP nonusers | Patient portal use might be associated with improved blood pressure control, although its clinical relevance is unclear. | Cross-sectional |

|
— | — |

|

|
| Keith McInnes et al [109], 2013 | Veterans with HIV | PP users versus PP nonusers | Patient portal use is associated with improved adherence to HIV medication. | Cross-sectional | — |

|
— |

|

|
| Keith McInnes et al [110], 2017 | Veterans with HIV+detectable viral load, registered for PP | Messaging or prescription refill users versus nonusers | Requesting prescription refills is associated with improved HIV control, but messaging is not. | Cohort |

|
— | — | — |

|
| Kiberd et al [111], 2018 | Adult with home dialysis | Pretest PP nonuse versus posttest PP use | Patient portal use is not associated with improvements in HRQoL nor perceived quality of care. Both were already high at baseline. | QEl | — |

|
— |

|

|
| Lee et al [112], 2017 | Patients with cleft lip or cleft palate surgery | PP users versus PP tailored for lip or cleft palate surgery | Using a tailored, disease-specific patient portal is associated with increased disease knowledge. | QE | — |

|
— |

|

|
| Reich et al [116], 2019 | Patients with inflammatory bowel disease | PP users versus PP nonusers | Patient portal use does not result in improved HRQoL, but results in a higher vaccination rate. Patient satisfaction is high. | RCT | — |

|

|

|

|
| Scott Nielsen et al [117], 2012 | Patients with multiple sclerosis | PP users versus PP nonusers | Messaging in a patient portal is associated with more clinic visits, but not with less EDm visits nor hospitalizations. | Cross-sectional | — | — |

|

|

|
| Tom et al [119], 2012 | Parents of children age <6 years with 1 ore more chronic condition(s) | PP users versus PP nonusers | Patient portal use is not associated with improved access to care, nor perceived quality of care. It is considered feasible. | Cross-sectional | — |

|
— |

|

|
| van den Heuvel et al [120], 2018 | Adults with bipolar disorder | Pretest PHR nonusers versus posttest PHR users | PHR use is not associated with improved HRQoL, patient empowerment, symptom reduction, nor disease burden. | Cross-sectional | — |

|
— |

|

|
| van der Vaart et al [121], 2014 | Patients with rheumatoid arthritis | Pretest PP nonusers versus posttest PP users | Patient portal use is not associated with improved patient empowerment. It is considered useful and understandable. | Cross-sectional | — |

|
— |

|

|
| Bidmead et al [104], 2016 | Patients with inflammatory bowel disease | PHR users | PHR use is not associated with improved self-management. | Cross-sectional |

|

|

|

|

|
| Byczkowski et al [43], 2014 | Parents of children with CFo or JIAp (or DM) | PP users | Patients consider the patient portal to be useful in managing and understand their child’s disease. | Cross | — |

|
— |

|

|
| Crouch et al [105], 2015 | Veterans with HIV | PP users versus PP nonusers | Patient portal use is associated with improved patient activation, disease knowledge, HIV load, but not with improved CD4-count nor treatment adherence | Cross-sectional | — |

|
— |

|

|
| Kahn et al [108], 2010 | Patients with HIV or aids | PP users | Patients are satisfied with the patient portal and consider it to be helpful in managing their problems. | QE | — |

|
— |

|

|
| Plimpton [115], 2020 | Women with HIV | Pretest PP nonuse versus posttest PP use | Patient portal use is associated with an increase in planned visits, but not with a decrease in missed visits. A trend toward improved viral load is seen. | QE |

|
— |

|
— |

|
| Son et al [118], 2019 | Patients aged >49 years with 1 or more chronic condition(s) | PP users | Patients consider a patient portal to be helpful in increasing self-management. | Cohort | — |

|
— |

|

|
aStudies are listed multiple times in Tables 10-13. Per disease category, the relevant subconclusion and health outcomes are described.
bFor color coding of quality appraisal and health outcomes, see Table 10.
cPHR: personal health record.
dHRQoL: health-related quality of life.
eRCT: randomized controlled trial.
fThe study did not assess any health outcome in a certain category.
gPP: patient portal.
hMSM: men who have sex with men.
iDM: diabetes mellitus.
jHT: hypertension.
kHC: hypercholesteremia.
lQE: quasi-experimental, including pilot or feasibility studies.
mED: emergency department.
oCF: cystic fibrosis.
pJIA: juvenile idiopathic arthritis.
Table 11.
Conclusions and health outcomes: studies investigating cardiopulmonary diseases (n=21), of which 6 (29%) are of high methodological quality.a
| Author, year | Participants | Comparison | Conclusion | Study design | Clinical | Patient reported | Care utilization | Technology | Qualityb |
| Ahmed et al [79], 2016 | Adults with asthma using medication | PPc users versus PP nonusers | Patient portal use does not result in durable improvements in HRQoLd nor asthma control. | RCTe |

|

|

|

|

|
| Fiks et al [81], 2015 | Children aged 6-12 years with asthma | PP users versus PP nonusers | Patient portal use results in improved asthma control. | RCT |

|

|

|

|

|
| Lau et al [85], 2015 | Adults with asthma | PHRf users versus PHR nonusers | PHR use does not increase the use of asthma action plans, and does not affect asthma control, health care utilization nor work or school participation. | RCT |

|

|

|
—g |

|
| Manard et al [86], 2016 | Adults with uncontrolled HTh | PP users versus PP nonusers | Using a patient portal linked with a blood pressure cuff is not associated with improved blood pressure control. | Cohort |

|
— | — | — |

|
| Price-Haywood and Luo [56], 2017 | Adults with HT (or DMi) | PP users versus PP nonusers | Patient portal use is associated with more primary care visits and telephone encounters, but not hospitalizations or EDj visits. Effects on blood pressure control are not clinically relevant. | Cohort |

|
— |

|
— |

|
| Shimada et al [71], 2016 | Veterans with uncontrolled HCk or HT, registered for PP | Users of both messaging and prescription refills versus nonusers | Messaging or requesting prescription refills are both associated with improved lipid control. Requesting prescription refills is associated with improved blood pressure control. | Cohort |

|
— | — | — |

|
| Apter et al [80], 2019 | Adults with asthma using prednisone | PP use+training versus PP use+assistance via home visits | Patient portal use results in minor improvements in asthma control and HRQoL. Conducting home visits results in more improvements in these outcomes. | RCT |

|

|

|
— |

|
| Druss et al [77], 2020 | Patients with a mental disorder+DMi, HTj, or HCk | PP users versus PP nonusers | Patient portal use does not result in clinically relevant improvements in perceived quality of care, patient activation, nor HRQoL. | RCT |

|

|

|
— |

|
| Fiks et al [82], 2016 | Children aged 6-12 years with asthma | PP users versus PP nonusers | Patient portal use is associated with improved treatment adherence. Among patients with uncontrolled asthma, its use is associated with more care visits. Adoption is low. | QEl | — |

|

|

|

|
| Martinez Nicolás et al [89], 2019 | Patients with COPDm or CHFn | Pretest PP nonuse versus posttest PP use | Patient portal use is associated with less hospitalizations, readmissions, and ED visits among patients with CHF and COPD. | QE |

|
— |

|
— |

|
| Reed et al [60], 2019 | Adults with DM+HT, asthma, CADm, or CHFn | PP users versus PP nonusers | Patient portal use is associated with more outpatient office visits, and with reduced ED visits and preventable hospitalizations. | Cross |

|
— |

|
— |

|
| Riippa et al [62], 2014 | Adults with DM, HT, or HC | PP users versus PP nonusers | Patient portal use does not result in clinically relevant improvements in patient activation, except for patients with low baseline activation. | RCT | — |

|
— | — |

|
| Riippa et al [63], 2015 | Adults with DM, HT, or HC | Patient portal versus usual care | Patient portal use does not result in clinically relevant improvement in patient activation nor HRQoL. | RCT | — |

|
— |

|

|
| Toscos et al [87], 2020 | Patients with nonvalvular AFo with an oral anticoagulant drug | PP users versus PP nonusers | Using a patient portal connected to a Smart Pill Bottle does not result in improved drug adherence. | RCT | — |

|
— | — |

|
| Wagner et al [88], 2012 | Patients with HT | PHR users versus PHR nonusers | Using a tethered PHR does not result in clinically relevant improvements in blood pressure control, patient activation nor health care utilization. Adoption is low. | RCT |

|

|

|

|

|
| Aberger et al [78], 2014 | Postrenal transplant patients with HT | PP users | Using a patient portal–linked blood pressure monitoring system is associated with improved blood pressure control. | QE |

|
— | — | — |

|
| Kim et al [84], 2019 | Patients with obstructive sleep apnea | PHR+activity tracker versus PHR alone versus nonusers | Using a tethered PHR results in more weight loss, regardless of its connection to an activity tracker. No sleep-related outcome improvements are seen. | RCT |

|
— | — |

|

|
| Kogut et al [83], 2014 | Adults aged >49 years with cardiopulmonary disorders | PHR users versus PHR nonusers | Pharmacists reviewing patient-reported medication lists in a PHR might identify more medication-related problems. | QE |

|
— | — | — |

|
| Price-Haywood et al [57], 2018 | Adults with HT or DM | PP users versus PP nonusers | Messaging is not associated with improved blood pressure control. | Cohort |

|
— | — | — |

|
| Reed et al [59], 2015 | Adults with DM, HT, asthma, CADp, or CHF, registered for PP | PP users | One-third of patients report that messaging in a patient portal results in less health care visits and improved overall health. | Cross-sectional | — |

|

|
— |

|
| Reed et al [61], 2019 | Adults with DM, asthma, HT, CAD, CHF, or CVq event risk | PP users versus PP nonusers | A third of patients reports that using the patient portal improves overall health. | Cross-sectional | — |

|
— |

|

|
aStudies are listed multiple times in Tables 10-13. Per disease category, the relevant subconclusion and health outcomes are described.
bFor color coding of quality appraisal and health outcomes, see Table 10.
cPP: patient portal.
dHRQoL: health-related quality of life.
eRCT: randomized controlled trial.
fPHR: personal health record.
gThe study did not assess any health outcome in a certain category.
hHT: hypertension.
iDM: diabetes mellitus.
jED: emergency department.
kHC: hypercholesteremia.
lQE: quasi-experimental, including pilot or feasibility studies.
mCOPD: chronic obstructive pulmonary disease.
nCHF: Congestive heart failure.
oAF: atrial fibrillation.
pCAD: coronary artery disease.
qCV: cardiovascular.
Table 12.
Conclusions and health outcomes: studies investigating hematological and oncological diseases (n=14), of which 2 are of high methodological quality (14%).a
| Author, year | Participants | Comparison | Conclusion | Study design | Clinical | Patient reported | Care utilization | Technology | Qualityb |
| Cahill et al [90], 2014 | Adults with a brain tumor | PHRc users versus PHR nonusers | Using a tethered PHR is associated with improvements in patient uncertainty. | Cross-sectional | — |

|
—d | — |

|
| Coquet et al [93], 2020 | Patients with cancer+chemotherapy, registered for PPe | Email users versus email nonusers | Sending emails is associated with improved 2-year survival, less missed appointments, and less hospitalizations. | Cohort |

|
— |

|
— |

|
| Chiche et al [91], 2012 | Adults with ITPf | PP users versus PP nonusers | Patient portal use does not result in improved HRQoLg. The portal is acceptable and feasible. | RCTh | — |

|
— |

|

|
| Groen et al [94], 2017 | Patients with lung cancer | PP users | Patient portal use does not affect HRQoL nor patient engagement. It is feasible and acceptable. | QEi | — |

|
— |

|

|
| Hall et al [95], 2014 | Patients with cancer resection | PP users | Disclosing results of genetic cancer screening in a patient portal might be feasible and acceptable, and is not associated with more anxiety. Yet, few abnormal results were observed. | QE | — |

|
— |

|

|
| Kidwell et al [97], 2019 | Patients aged 13-24 years with sickle cell disease | PP users | Patient portal use is not associated with improved medical decision-making by patients. It is acceptable and easy to use. | QE | — |

|
— |

|

|
| Martinez Nicolás et al [89], 2019 | Patients with hematologic malignancy | Pretest PP nonuse versus posttest PP use | Patient portal use is not associated with less hospitalizations, readmissions, nor EDj department visits. | QE |

|
— |

|
— |

|
| Williamson et al [102], 2017 | Pediatric cancer survivors | PHR users versus PHR registrants | Patient portal use is not associated with less missed appointments. | Cohort | — | — |

|

|

|
| Collins et al [92], 2003 | Patients with hemophilia >11 years | Users | An electronic treatment log is considered feasible and easy to use. | QE | — | — | — |

|

|
| Hong et al [96], 2016 | Children aged 13-17 years with cancer or a blood disorder+parents | PP users | A small cohort considers a patient portal to be feasible and useful. | Cross-sectional | — |

|
— |

|

|
| O’Hea et al [98], 2021 | Women with breast cancer | PP users versus PP nonusers | Patient portal use does not result in improved HRQoL nor disease knowledge. | RCT | — |

|
— | — |

|
| Pai et al [99], 2013 | Men with prostate cancer | PHR users | Patients are satisfied with a tethered PHR and find it increases disease knowledge. | Cross-sectional | — |

|
— |

|

|
| Tarver et al [100], 2019 | Patients with colorectal cancer | Tethered PHR users | Patients are satisfied with an integrated care plan and find it useful. | Cohort | — | — | — |

|

|
| Wiljer et al [101], 2010 | Patients with breast cancer | Pretest PHR nonusers versus posttest PHR users | PHR use is not associated with improved self-efficacy, nor with a clinically relevant decrease in anxiety. Satisfaction is high. | QE | — |

|
— |

|

|
aStudies are listed multiple times in Tables 10-13. Per disease category, the relevant subconclusion and health outcomes are described.
bFor color coding of quality appraisal# and health outcomes, see Table 10.
cPHR: personal health record.
dThe study did not assess any health outcome in a certain category.
ePP: patient portal.
fITP: idiopathic thrombocytopenic purpura.
gHRQoL: health-related quality of life.
hRCT: randomized controlled trial.
iQE: quasi-experimental, including pilot or feasibility studies.
jED: emergency department.
Clinical Outcomes
In 44 studies investigating a total of 69 clinical outcomes, a beneficial association with digital health record use was reported for 42% (29/69) of the outcomes. Hospitalizations and exacerbations were the most frequently studied disease events and complications, with beneficial effects reported in half of the studies (2/4 and 2/4, respectively). Blood pressure was the most frequently studied vital parameter, with beneficial effects reported in 36% (5/14) of the studies. HbA1c and cholesterol levels were the most frequently studied laboratory parameters, with beneficial effects reported in 53% (10/19) and 57% (4/7) of the studies, respectively. No clinical outcomes were unfavorably affected by patient-centered digital health record use. In comparison with the total population, higher proportions of beneficial effects were reported for diabetes mellitus and cardiopulmonary diseases. When focusing on 14 high-quality studies, beneficial effects were observed less frequently, in only 30% (7/23) of the clinical outcomes.
Studies that assessed vital parameters generally reported few other health outcomes. However, among the studies that assessed disease events and complications, and laboratory parameters, beneficial effects were often associated with improved treatment adherence [52,68,71,81]. We hypothesize that this might be related to the removal of logistical barriers for patients in obtaining web-based prescription refills, as opposed to having to call health care providers or send them an email. Of the 6 high-quality studies that investigated treatment adherence, 2 studies assessed patient-centered digital health records that enabled patients to request prescription refills and found beneficial effects on adherence [52,68].
Patient-Reported Outcomes
Overall, in 53 studies investigating a total of 86 patient-reported outcomes, a beneficial association with digital health record use was reported for 45% (39/86) of the outcomes. Of the 18 studies investigating 19 self-management or self-efficacy outcomes, beneficial effects were reported in 53% (9/19). Of these 9 studies, 56% (5/9) used validated questionnaires. For patient engagement outcomes, large differences in the proportions of beneficial effects were observed: from 11% (1/9) for patient activation, to 56% (5/9) for patient involvement, and 70% (7/10) for disease knowledge. However, only in measuring patient activation, validated questionnaires were principally used (8/9, 88% of studies). For HRQoL, beneficial effects were reported in 27% (4/15) of the studies, of which half used validated HRQoL questionnaires. No patient-reported outcomes were unfavorably affected by patient-centered digital health record use. In comparison to the total population, higher proportions of beneficial effects were reported for diabetes mellitus, especially for patient engagement and treatment adherence. Lowest proportions were reported for cardiopulmonary diseases, especially for patient engagement. When focusing on 10 high-quality studies, a lower proportion (7/19, 37%) of beneficial effects was observed.
We observed that improvements in patient engagement were especially facilitated by strengthening patient-professional communication; for example, through secure messaging [71,81,93]. In addition, both self-efficacy and HRQoL primarily seemed to be reinforced through the use of 2 functionalities: patient-professional communication [54,90,113] and information on disease progression [90,113].
Health Care Utilization
For 24 studies investigating a total of 27 health care utilization outcomes, a beneficial association with digital health record use was observed for 59% (16/27) of the outcomes. The highest proportion (10/13, 77%) of beneficial effects was reported for an increased use of recommended care services. Of these 13 studies, 5 (38%) focused on recommended care services for people with uncontrolled disease, 4 (31%) on the use of preventive care services, and 4 (31%) on medical follow-up rates. In 25% (3/12) of the studies that assessed reductions in ED visits and hospitalizations, these were accompanied by an increased use of other care services, including outpatient clinic appointments and secure messaging. Compared with the total population, highest proportions of beneficial effects were reported for diabetes mellitus and hematological and oncological diseases. When focusing on 7 high-quality studies, lower proportions (3/9, 33%) of beneficial effects were observed.
Technology-Related Outcomes
For 39 studies investigating a total of 75 technology-related outcomes, a beneficial association with digital health record use was observed for 88% (66/75) of the outcomes. All (22/22, 100%) studies reported high patient satisfaction with accessing and using digital health records. Furthermore, 75% (6/8) of the studies reported high patient satisfaction with the effects of using digital health records. High feasibility was reported by 79% (15/19) of the studies, and high acceptability by 88% (23/26) of the studies. Highest feasibility was reported for digital health records intended for people with hematological and oncological diseases. Lowest feasibility and acceptability were reported for digital health records intended for people with cardiopulmonary diseases. When focusing on 6 high-quality studies, proportions of studies that found beneficial effects were similar.
High Disease Burden or Self-management
A subgroup of 47 studies that investigated patients with a high disease burden or high self-management was assessed. The following conditions were included: malignancies (11 studies), asthma (9 studies), HIV infection and AIDS (6 studies), hematologic conditions (5 studies), chronic kidney disease (3 studies), chronic heart failure (4 studies), mental disorders (3 studies), multiple sclerosis (2 studies), inflammatory bowel disease (2 studies), rheumatologic conditions (2 studies), insulin-dependent diabetes mellitus (2 studies), atrial fibrillation (1 study), cystic fibrosis (1 study), and posttransplant patients (1 study). In general, the digital health records assessed in this subgroup were more often tailored to specific patient populations through the addition of specialized functionalities or connected wearables.
In comparison with studies investigating patients with no high disease burden, studies investigating patients with a high disease burden reported considerably higher proportions of beneficial effects for vital parameters, patient engagement, reductions in ED visits and hospitalizations, and for all technology-related outcomes. Considerably lower proportions of beneficial effects were reported for laboratory parameters, health-related quality of life, treatment adherence, and increased use of recommended care services. For the 9 high methodological quality studies on high disease burden or self-management, the proportions of studies that found beneficial effects were roughly similar.
Focus on Passive Versus Active Features
Of the 81 studies, 41 (51%) of the studied patient-centered digital health records focused on passive features and 40 (49%) focused on active features. In comparison with digital health records with an active focus, more beneficial effects were observed among digital health records with a passive focus for laboratory parameters (9/16, 56% vs 7/17, 41%), self-management and self-efficacy (7/11, 64% vs 3/8, 38%), patient engagement (9/15, 60% vs 4/13, 31%), and for an increased use of recommended care services (5/6, 83% vs 5/7, 71%). Compared with digital health records with a passive focus, more beneficial effects were observed among digital health records with an active focus on disease events or complications (4/10, 40% vs 1/5, 20%) and reductions in ED visits and hospitalizations (4/6, 67% vs 1/6, 17%). However, when focusing on high-quality studies, higher proportions of beneficial effects were seen for digital health records with an active focus on all clinical outcomes, patient-reported outcomes, reductions in ED visits and hospitalizations, patient satisfaction, and acceptability.
Quality Appraisal
Of the 81 included studies, 27 (33%) studies were graded as low quality, 38 (47%) as medium quality, and 16 (20%) as high quality (Tables 10-13). Studies investigating cardiopulmonary conditions were of the highest quality, with 29% (6/21) of the studies graded as high quality. Of the 24 included RCTs, 7 (29%) were of high quality. Only 38% (9/24) of the RCTs concealed allocation to treatment groups, and 67% (16/24) used intention-to-treat analyses. Of the 57 studies with other designs, 9 (16%) were graded as high quality. Overall, 15% (12/81) of studies reported power calculations.
Among the 65 studies that were graded as medium or low quality, only 35% (23/65) used reliable or validated tools for the measurement of all their outcomes and 48% (31/65) for part of their outcomes. Of these 65 studies, 10 (15%) studies took adequate measures to limit selection bias and 17 (26%) studies used a control group or randomized participants.
When focusing on the 16 high-quality studies, 3 functionalities appeared to be the most effective: secure messaging to lower barriers in patient-professional interaction, prescription refill functions to improve medication adherence, and information provision on disease progression. In addition, in 16 high-quality studies, the proportions of beneficial effects were similar for a subgroup of studies that included older participants (mean age >55 years), which included a high number of female participants (>45%), or included a racially diverse population (<50% White participants), as compared with the total population.
Discussion
Principal Findings
In this systematic review, we evaluated evidence on the effects of the use of patient-centered digital health records in nonhospitalized patients with chronic health conditions on clinical and patient-reported outcomes, health care utilization, and technology-related outcomes. Beneficial effects were most frequently reported for the use of recommended care services (10/13, 77%) and for 4 patient-reported outcomes: disease knowledge (7/10, 70%), patient involvement (5/9, 56%), treatment adherence (10/18, 56%), and self-management and self-efficacy (10/19, 53%). Regarding clinical outcomes, beneficial effects were reported in 42% (29/69) of the studies. Beneficial effects were least frequently reported for disease events and complications (5/15, 33%) and health-related quality of life (4/15, 27%). For digital health records that predominantly focused on active features, higher proportions of beneficial effects on nearly all health outcomes were observed among the high-quality studies.
In this study, we observed that patient-centered digital health record use may be associated with an increased use of recommended care services. Beneficial effects on ED visits and hospitalizations were mainly observed when accompanied by an increased rate of follow-up appointments or secure messaging [60,89,93]. This might imply that reducing ED visits and hospitalizations is primarily achieved by facilitating patient-professional communication.
Beneficial effects were most often reported for patients with diabetes or cardiopulmonary disorders. We suggest 2 explanations. First, the focus of digital health records has been directed toward patients with diabetes and asthma for some time because of the sheer number of people with these conditions. This could have resulted in higher-quality patient-centered digital health records and patients who were more accustomed to their use. Second, the relative improvements in health outcomes might be smaller among patients with a condition with a high disease burden because of a higher baseline level of self-management skills and disease knowledge.
The proportions of beneficial effects varied considerably between health outcomes, which may be explained by 2 reasons. First, outcomes with a higher proportion of beneficial effects were more often the primary study outcomes than the secondary outcomes. Digital health records were more frequently tailored for these outcomes, yielding higher beneficial effects. Second, outcome assessment was generally less robust for outcomes with a higher proportion of beneficial effects, such as self-management and patient engagement, which might have resulted in more false-positive effects.
Comparison With Earlier Evidence
Our results are more positive than those of the previous systematic reviews. This might be because of the increasing acceptance of digital health records, their improving quality, the increasing body of literature, or variations in digital health record definitions used. Two previous reviews found mixed effects on the use of portals on health outcomes and health care utilization [27] and reported positive effects on qualitatively assessed self-management in only one-third of the studies [25]. A recent systematic review that focused on portals intended for hospitalized patients found mixed results for patient engagement [26]. A systematic review that included only qualitative studies found that portal use was associated with positive effects on self-efficacy, treatment adherence, and disease knowledge [28]. In a review on eHealth interventions that aim to promote medication use, a weak association between digital health record use and health-related quality of life was observed [10]. This implies that digital health record engagement is not yet sufficient to affect patients’ overall health-related quality of life.
Strengths and Limitations
This systematic review has several strengths. Our search strategy was comprehensive, to account for the lack of consensus in digital health record terminology. In addition, a wide variety of health outcomes were considered relevant to determine the impact of digital health record use. However, several limitations of this study must be considered. First, comparisons between studies were difficult because of the variety in evaluated functionalities. A similar diversity was observed among the reported follow-up durations, participants’ ages, study sample sizes, and outcomes. Second, because it was not possible to perform a meta-analysis owing to the heterogeneity in reported (disease-specific) outcome measurements and effects, we used the vote-counting method. Therefore, we could not report the effect estimates and indicated directions of effects [122]. Third, owing to a lack of agreement on feasibility and acceptability thresholds, much is left to the authors’ discretion. Fourth, JBI critical appraisal tools rank every item equally despite being not equally important. Finally, publication bias could have resulted in overestimation of the positive effects of patient-centered digital health records. More studies with positive results have been published. In addition, many of the included studies assessed more “mature” patient-centered digital health records, which could have overestimated the effects.
We observed that high patient satisfaction rates did not fully reflect in other health outcomes. This can be partly attributed to acquiescence bias and satisficing [123]. Moreover, satisfaction was often reduced to a narrow ease-of-use questionnaire, instead of satisfaction with the contribution to overall disease management. Finally, several studies only included recurrent users in their analyses, which could falsely increase feasibility. Moreover, these recurrent users likely experienced positive effects of using digital health records, which would have resulted in an overestimation of effects in randomized studies with no intention-to-treat analysis and in all nonrandomized studies.
The voluntary adoption of patient-centered digital health records by patients might reflect an intrinsic, preexisting motivation for self-management and care engagement bias, which may overestimate their effects. Patient-centered digital health record use could even be considered a surrogate measure for engagement [109,124,125]. Thus, it might be best to consider digital health records as vehicles for empowerment, strengthening existing self-management capabilities [126,127].
The effects of using patient-centered digital health records on health outcomes are not always direct but often depend on intermediate steps. For example, requesting prescription refills might depend on the actions performed by (slow-responding) physicians, nurses, or pharmacies. Thus, if using a digital health record would have no observable effects on health outcomes, this could also be a result of these intermediate steps or unforeseen processes and may not be attributable to the use of the patient-centered digital health record.
The proportion of beneficial effects reported in high-quality studies was lower as compared with all included studies for clinical outcomes (30% vs 42%), patient-reported outcomes (37% vs 45%), and health care utilization (33% vs 59%). Nevertheless, the proportions are clinically relevant and promising considering this newly emerging field. The observed differences might be related to 4 factors. First, the selection of motivated, well-educated, digitally minded participants might have overestimated the results in most low- and moderate-quality studies. Second, most studies did not measure ongoing user activity, and assumed that registered users became recurrent users. Third, nearly all low- and moderate-quality studies reported high dropout rates, which could overestimate acceptance rates. Finally, the lack of consensus on digital health record terminology hindered the interpretation of findings. We would advocate the use of uniform definitions, such as those presented in Textbox 1 [10,17-20].
Future Research
Future studies should adopt additional measures to adhere to a uniform taxonomy, use log data, and limit selection bias. The exclusion of less-engaged people could further expand the digital divide between patients who are digitally proficient and those who are not, resulting in an increasingly unequal distribution of care services. We suggest that researchers include a diverse population based on age, gender, disease burden, race, education level, and health literacy [128]. Finally, further research should focus on determining which functionalities are mostly responsible for the effects on the outcomes.
Conclusions
The use of patient-centered digital health records in chronic conditions is potentially associated with beneficial effects on several patient-reported outcomes and recommended care services in a considerable number of studied digital health records. The rates of the effects were approximately similar for different patient groups. Feasibility and acceptability were high. Our findings support further implementation of patient-centered digital health records in clinical practice. Yet, higher-quality research is needed to identify effects per disease category and per health outcome and to learn which patients might benefit from specific functionalities.
Acknowledgments
This project was supported by grants K23HL150232 (principal investigator [PI]: SMB) and K23HL141447 (PI: RMC) from the National Heart, Lung, and Blood Institute of the National Institutes of Health and by grant NWA.1160.18.038 (PI: MH Cnossen, WP leader SCG) of the Netherlands Organization for Scientific Research (NWO) for the SYMPHONY consortium. The content is solely the responsibility of the authors and does not necessarily represent National Institutes of Health or NWO.
Abbreviations
- ED
emergency department
- JBI
Joanna Briggs Institute
- PHR
personal health record
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PROSPERO
International Prospective Register of Systematic Reviews
- RCT
randomized controlled trial
The search strategy used, that includes terms related to the search categories: “patient,” “intervention,” and “outcome.”.
The 4 modified Joanna Briggs Institute critical appraisal tools used in this study.
Proportion of beneficial effects reported per health outcome of all studies, presented per disease category.
The proportion of beneficial effects reported per health outcome of 16 high quality studies, presented per disease category.
Footnotes
Authors' Contributions: All authors were involved in the design of the research protocol. MB performed the search strategy. MRB and SMB assessed all titles, abstracts, and full texts for eligibility. SCG helped resolve the discussion if necessary. MRB and SMB performed data extraction and synthesis. All authors provided feedback on the manuscript and approved the final manuscript.
Conflicts of Interest: SCG received an unrestricted medical research grant from Sobi. The authors have no futher interests to declare.
References
- 1.Noncommunicable diseases. World Health Organization. 2021. Sep 16, [2022-12-01]. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases . [PubMed]
- 2.Benziger CP, Roth GA, Moran AE. The global burden of disease study and the preventable burden of NCD. Glob Heart. 2016 Dec;11(4):393–7. doi: 10.1016/j.gheart.2016.10.024. https://globalheartjournal.com/articles/abstract/10.1016/j.gheart.2016.10.024 .S2211-8160(16)30760-8 [DOI] [PubMed] [Google Scholar]
- 3.Buttorff C, Ruder T, Bauman M. Multiple Chronic Conditions in the United States. Santa Monica, CA, USA: RAND Corporation; 2017. [Google Scholar]
- 4.Schulman-Green D, Jaser S, Martin F, Alonzo A, Grey M, McCorkle R, Redeker NS, Reynolds N, Whittemore R. Processes of self-management in chronic illness. J Nurs Scholarsh. 2012 Jun;44(2):136–44. doi: 10.1111/j.1547-5069.2012.01444.x. https://europepmc.org/abstract/MED/22551013 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen S, Kuhn M, Prettner K, Bloom DE. The macroeconomic burden of noncommunicable diseases in the United States: estimates and projections. PLoS One. 2018 Nov 1;13(11):e0206702. doi: 10.1371/journal.pone.0206702. https://dx.plos.org/10.1371/journal.pone.0206702 .PONE-D-18-15898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The Complexities of Physician Supply and Demand: Projections From 2019 to 2034. Association of American Medical Colleges. 2021. Jun, [2022-09-01]. https://tinyurl.com/yfren872 .
- 7.European Commission. Directorate-General for Employment. Social Affairs and Inclusion. McGrath J. Analysis of Shortage and Surplus Occupations 2020. Luxembourg, Luxembourg: Publications Office of the European Union; 2020. [Google Scholar]
- 8.Medical staffing in England: a defining moment for doctors and patients. British Medical Association. 2021. Jul 11, [2022-09-01]. https://www.pslhub.org/learn/improving-patient-safety/workforce-and-resources/safe-staffing-levels/medical-staffing-in-england-a-defining-moment-for-doctors-and-patients-bma-11-july-2021-r4856/
- 9.COVID-19 continues to disrupt essential health services in 90% of countries. World Health Organization. 2021. Apr 23, [2022-09-01]. https://www.who.int/news/item/23-04-2021-covid-19-continues-to-disrupt-essential-health-services-in-90-of-countries#:~:text=The%20second%20round%20of%20 a,since%20the%20first%20survey%20conducted .
- 10.Lancaster K, Abuzour A, Khaira M, Mathers A, Chan A, Bui V, Lok A, Thabane L, Dolovich L. The use and effects of electronic health tools for patient self-monitoring and reporting of outcomes following medication use: systematic review. J Med Internet Res. 2018 Dec 18;20(12):e294. doi: 10.2196/jmir.9284. https://www.jmir.org/2018/12/e294/ v20i12e294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Risling T, Martinez J, Young J, Thorp-Froslie N. Evaluating patient empowerment in association with eHealth technology: scoping review. J Med Internet Res. 2017 Sep 29;19(9):e329. doi: 10.2196/jmir.7809. https://www.jmir.org/2017/9/e329/ v19i9e329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barello S, Triberti S, Graffigna G, Libreri C, Serino S, Hibbard J, Riva G. eHealth for patient engagement: a systematic review. Front Psychol. 2016 Jan 8;6:2013. doi: 10.3389/fpsyg.2015.02013. https://air.unimi.it/handle/2434/696411 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morton K, Dennison L, May C, Murray E, Little P, McManus RJ, Yardley L. Using digital interventions for self-management of chronic physical health conditions: a meta-ethnography review of published studies. Patient Educ Couns. 2017 Apr;100(4):616–35. doi: 10.1016/j.pec.2016.10.019. https://linkinghub.elsevier.com/retrieve/pii/S0738-3991(16)30489-X .S0738-3991(16)30489-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mc Namara KP, Versace VL, Marriott JL, Dunbar JA. Patient engagement strategies used for hypertension and their influence on self-management attributes. Fam Pract. 2014 Aug;31(4):437–44. doi: 10.1093/fampra/cmu026.cmu026 [DOI] [PubMed] [Google Scholar]
- 15.Greene J, Hibbard JH, Sacks R, Overton V, Parrotta CD. When patient activation levels change, health outcomes and costs change, too. Health Aff (Millwood) 2015 Mar;34(3):431–7. doi: 10.1377/hlthaff.2014.0452.34/3/431 [DOI] [PubMed] [Google Scholar]
- 16.Peters AE, Keeley EC. Patient engagement following acute myocardial infarction and its influence on outcomes. Am J Cardiol. 2017 Nov 01;120(9):1467–71. doi: 10.1016/j.amjcard.2017.07.037.S0002-9149(17)31210-9 [DOI] [PubMed] [Google Scholar]
- 17.What are the differences between EHMRs, EHRs and PHRs? HealthIT.gov. 2019. [2022-12-01]. https://www.healthit.gov/faq/what-are-differences-between-electronic-medical-records-electronic-health-records-and-personal .
- 18.A HIMSS Guide to Participating in a Health Information Exchange: HIMSS Healthcare Information Exchange HIE Guide Work Group White Paper. Healthcare Information and Management Systems Society (HIMSS) 2009. Aug, [2022-09-01]. https://assets.hln.com/pdf/HIMSS-HIEGuideWhitePaper.pdf?utm_source=legacy&utm_medium=redirect&utm_campaign=webmig21&utm_term=pdf/HIMSS-HIEGuideWhitePaper.pdf .
- 19.Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006;13(2):121–6. doi: 10.1197/jamia.M2025. https://europepmc.org/abstract/MED/16357345 .M2025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Safran C, Bloomrosen M, Hammond WE, Labkoff S, Markel-Fox S, Tang PC, Detmer DE, Expert Panel Toward a national framework for the secondary use of health data: an American Medical Informatics Association White Paper. J Am Med Inform Assoc. 2007;14(1):1–9. doi: 10.1197/jamia.M2273. https://europepmc.org/abstract/MED/17077452 .M2273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cronin RM, Jimison H, Johnson KB. Personal health informatics. In: Shortliffe EH, Cimino JJ, editors. Biomedical Informatics: Computer Applications in Health Care and Biomedicine. Cham, Switzerland: Springer; 2021. pp. 363–89. [Google Scholar]
- 22.MedMij | Dutch Personal Health Environment. [2022-12-01]. https://medmij.nl/en/home/
- 23.Ammenwerth E, Schnell-Inderst P, Hoerbst A. The impact of electronic patient portals on patient care: a systematic review of controlled trials. J Med Internet Res. 2012 Nov 26;14(6):e162. doi: 10.2196/jmir.2238. https://www.jmir.org/2012/6/e162/ v14i6e162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Andrikopoulou E, Scott P, Herrera H, Good A. What are the important design features of personal health records to improve medication adherence for patients with long-term conditions? A systematic literature review. BMJ Open. 2019 Sep 26;9(9):e028628. doi: 10.1136/bmjopen-2018-028628. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=31558449 .bmjopen-2018-028628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kruse CS, Bolton K, Freriks G. The effect of patient portals on quality outcomes and its implications to meaningful use: a systematic review. J Med Internet Res. 2015 Feb 10;17(2):e44. doi: 10.2196/jmir.3171. https://www.jmir.org/2015/2/e44/ v17i2e44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dendere R, Slade C, Burton-Jones A, Sullivan C, Staib A, Janda M. Patient portals facilitating engagement with inpatient electronic medical records: a systematic review. J Med Internet Res. 2019 Apr 11;21(4):e12779. doi: 10.2196/12779. https://www.jmir.org/2019/4/e12779/ v21i4e12779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goldzweig GL, Orshansky G, Paige NM, Towfigh AA, Haggstrom DA, Miake-Lye I, Beroes JM, Shekelle PG. Electronic patient portals: evidence on health outcomes, satisfaction, efficiency, and attitudes: a systematic review. Ann Intern Med. 2013 Nov 19;159(10):677–87. doi: 10.7326/0003-4819-159-10-201311190-00006.1770672 [DOI] [PubMed] [Google Scholar]
- 28.Han HR, Gleason KT, Sun CA, Miller HN, Kang SJ, Chow S, Anderson R, Nagy P, Bauer T. Using patient portals to improve patient outcomes: systematic review. JMIR Hum Factors. 2019 Dec 19;6(4):e15038. doi: 10.2196/15038. https://humanfactors.jmir.org/2019/4/e15038/ v6i4e15038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brands M, Gouw S, Beestrum M, Fijnvandraat K, Badawy S. Patient-centered digital health interventions and their effects on health outcomes: a systematic review. CRD42020213285. PROSPERO. 2020. [2022-12-01]. https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=213285 . [DOI] [PMC free article] [PubMed]
- 30.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021 Mar 29;372:n71. doi: 10.1136/bmj.n71. http://www.bmj.com/lookup/pmidlookup?view=long&pmid=33782057 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Price M, Bellwood P, Kitson N, Davies I, Weber J, Lau F. Conditions potentially sensitive to a personal health record (PHR) intervention, a systematic review. BMC Med Inform Decis Mak. 2015 Apr 18;15:32. doi: 10.1186/s12911-015-0159-1. https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-015-0159-1 .10.1186/s12911-015-0159-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, Januel J, Sundararajan V. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011 Mar 15;173(6):676–82. doi: 10.1093/aje/kwq433.kwq433 [DOI] [PubMed] [Google Scholar]
- 33.Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004 Aug;39(4 Pt 1):1005–26. doi: 10.1111/j.1475-6773.2004.00269.x. https://europepmc.org/abstract/MED/15230939 .HESR269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vahdat S, Hamzehgardeshi L, Hessam S, Hamzehgardeshi Z. Patient involvement in health care decision making: a review. Iran Red Crescent Med J. 2014 Jan;16(1):e12454. doi: 10.5812/ircmj.12454. https://europepmc.org/abstract/MED/24719703 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fitzgerald JT, Funnell MM, Hess GE, Barr PA, Anderson RM, Hiss RG, Davis WK. The reliability and validity of a brief diabetes knowledge test. Diabetes Care. 1998 May;21(5):706–10. doi: 10.2337/diacare.21.5.706. [DOI] [PubMed] [Google Scholar]
- 36.Shmueli A. The SF-36 profile and health-related quality of life: an interpretative analysis. Qual Life Res. 1998 Apr;7(3):187–95. doi: 10.1023/a:1024959508246. [DOI] [PubMed] [Google Scholar]
- 37.Barroso NE, Hungerford GM, Garcia D, Graziano PA, Bagner DM. Psychometric properties of the Parenting Stress Index-Short Form (PSI-SF) in a high-risk sample of mothers and their infants. Psychol Assess. 2016 Oct;28(10):1331–5. doi: 10.1037/pas0000257. https://europepmc.org/abstract/MED/26595220 .2015-52780-001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Adherence to Long-Term Therapies: Evidence for Action. World Health Organization. 2003. [2022-09-01]. http://apps.who.int/iris/bitstream/handle/10665/42682/9241545992.pdf?sequence=1 .
- 39.Data collection form for intervention reviews for RCTs and non-RCTs - template. Version 3. Cochrane Collaboration. 2014. [2022-09-01]. https://dplp.cochrane.org/sites/dplp.cochrane.org/files/public/uploads/CDPLPG%20data%20collection%20form%20for%20intervention%20reviews%20for%20RCTs%20and%20non-RCTs.doc .
- 40.Critical Appraisal Tools. Joanna Briggs Institute. [2022-09-01]. https://jbi.global/critical-appraisal-tools .
- 41.Bailey SC, Wallia A, Wright S, Wismer GA, Infanzon AC, Curtis LM, Brokenshire SA, Chung AE, Reuland DS, Hahr AJ, Hornbuckle K, Lockwood K, Hall L, Wolf MS. Electronic health record-based strategy to promote medication adherence among patients with diabetes: longitudinal observational study. J Med Internet Res. 2019 Oct 21;21(10):e13499. doi: 10.2196/13499. https://www.jmir.org/2019/10/e13499/ v21i10e13499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Boogerd E, Maas-Van Schaaijk NM, Sas TC, Clement-de Boers A, Smallenbroek M, Nuboer R, Noordam C, Verhaak CM. Sugarsquare, a Web-based patient portal for parents of a child with type 1 diabetes: multicenter randomized controlled feasibility trial. J Med Internet Res. 2017 Aug 22;19(8):e287. doi: 10.2196/jmir.6639. https://www.jmir.org/2017/8/e287/ v19i8e287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Byczkowski TL, Munafo JK, Britto MT. Family perceptions of the usability and value of chronic disease web-based patient portals. Health Informatics J. 2014 Jun;20(2):151–62. doi: 10.1177/1460458213489054. https://journals.sagepub.com/doi/10.1177/1460458213489054?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed .1460458213489054 [DOI] [PubMed] [Google Scholar]
- 44.Chung S, Panattoni L, Chi J, Palaniappan L. Can secure patient-provider messaging improve diabetes care? Diabetes Care. 2017 Oct;40(10):1342–8. doi: 10.2337/dc17-0140.dc17-0140 [DOI] [PubMed] [Google Scholar]
- 45.Conway NT, Allardice B, Wake DJ, Cunningham SG. User experiences of an electronic personal health record for diabetes. J Diabetes Sci Technol. 2019 Jul;13(4):744–50. doi: 10.1177/1932296818818837. https://europepmc.org/abstract/MED/30585085 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Devkota B, Salas J, Sayavong S, Scherrer JF. Use of an online patient portal and glucose control in primary care patients with diabetes. Popul Health Manag. 2016 Apr;19(2):125–31. doi: 10.1089/pop.2015.0034. [DOI] [PubMed] [Google Scholar]
- 47.Dixon BE, Alzeer AH, Phillips EO, Marrero DG. Integration of provider, pharmacy, and patient-reported data to improve medication adherence for type 2 diabetes: a controlled before-after pilot study. JMIR Med Inform. 2016 Feb 08;4(1):e4. doi: 10.2196/medinform.4739. https://medinform.jmir.org/2016/1/e4/ v4i1e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Graetz I, Huang J, Brand RJ, Hsu J, Yamin CK, Reed ME. Bridging the digital divide: mobile access to personal health records among patients with diabetes. Am J Manag Care. 2018 Jan;24(1):43–8. https://www.ajmc.com/pubMed.php?pii=87412 .87412 [PMC free article] [PubMed] [Google Scholar]
- 49.Graetz I, Huang J, Muelly ER, Fireman B, Hsu J, Reed ME. Association of mobile patient portal access with diabetes medication adherence and glycemic levels among adults with diabetes. JAMA Netw Open. 2020 Mar 05;3(2):e1921429. doi: 10.1001/jamanetworkopen.2019.21429. https://europepmc.org/abstract/MED/32074289 .2761257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Grant RW, Wald JS, Schnipper JL, Gandhi TK, Poon EG, Orav EJ, Williams DH, Volk LA, Middleton B. Practice-linked online personal health records for type 2 diabetes mellitus: a randomized controlled trial. Arch Intern Med. 2008 Sep 08;168(16):1776–82. doi: 10.1001/archinte.168.16.1776. https://europepmc.org/abstract/MED/18779465 .168/16/1776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lau M, Campbell H, Tang T, Thompson DJ, Elliott T. Impact of patient use of an online patient portal on diabetes outcomes. Can J Diabetes. 2014 Mar;38(1):17–21. doi: 10.1016/j.jcjd.2013.10.005.S1499-2671(13)01356-7 [DOI] [PubMed] [Google Scholar]
- 52.Lyles CR, Sarkar U, Schillinger D, Ralston JD, Allen JY, Nguyen R, Karter AJ. Refilling medications through an online patient portal: consistent improvements in adherence across racial/ethnic groups. J Am Med Inform Assoc. 2016 Apr;23(e1):e28–33. doi: 10.1093/jamia/ocv126. https://europepmc.org/abstract/MED/26335983 .ocv126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Martinez W, Hackstadt AJ, Hickson GB, Knoerl T, Rosenbloom ST, Wallston KA, Elasy TA. The my diabetes care patient portal intervention: usability and pre-post assessment. Appl Clin Inform. 2021 May;12(3):539–50. doi: 10.1055/s-0041-1730324. http://www.thieme-connect.com/DOI/DOI?10.1055/s-0041-1730324 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.McCarrier KP, Ralston JD, Hirsch IB, Lewis G, Martin DP, Zimmerman FJ, Goldberg HI. Web-based collaborative care for type 1 diabetes: a pilot randomized trial. Diabetes Technol Ther. 2009 Apr;11(4):211–7. doi: 10.1089/dia.2008.0063. https://europepmc.org/abstract/MED/19344195 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Osborn CY, Mayberry LS, Wallston KA, Johnson KB, Elasy TA. Understanding patient portal use: implications for medication management. J Med Internet Res. 2013 Jul 03;15(7):e133. doi: 10.2196/jmir.2589. https://www.jmir.org/2013/7/e133/ v15i7e133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Price-Haywood EG, Luo Q. Primary care practice reengineering and associations with patient portal use, service utilization, and disease control among patients with hypertension and/or diabetes. Ochsner J. 2017;17(1):103–11. https://europepmc.org/abstract/MED/28331456 . [PMC free article] [PubMed] [Google Scholar]
- 57.Price-Haywood EG, Luo Q, Monlezun D. Dose effect of patient-care team communication via secure portal messaging on glucose and blood pressure control. J Am Med Inform Assoc. 2018 Jun 01;25(6):702–8. doi: 10.1093/jamia/ocx161. https://europepmc.org/abstract/MED/29444256 .4849779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Quinn CC, Butler EC, Swasey KK, Shardell MD, Terrin MD, Barr EA, Gruber-Baldini AL. Mobile diabetes intervention study of patient engagement and impact on blood glucose: mixed methods analysis. JMIR Mhealth Uhealth. 2018 Mar 02;6(2):e31. doi: 10.2196/mhealth.9265. https://mhealth.jmir.org/2018/2/e31/ v6i2e31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Reed M, Graetz I, Gordon N, Fung V. Patient-initiated e-mails to providers: associations with out-of-pocket visit costs, and impact on care-seeking and health. Am J Manag Care. 2015 Dec 01;21(12):e632–9. https://www.ajmc.com/pubMed.php?pii=86469 .86469 [PubMed] [Google Scholar]
- 60.Reed ME, Huang J, Brand RJ, Neugebauer R, Graetz I, Hsu J, Ballard DW, Grant R. Patients with complex chronic conditions: health care use and clinical events associated with access to a patient portal. PLoS One. 2019 Jun 19;14(6):e0217636. doi: 10.1371/journal.pone.0217636. https://dx.plos.org/10.1371/journal.pone.0217636 .PONE-D-18-36593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Reed ME, Huang J, Millman A, Graetz I, Hsu J, Brand R, Ballard DW, Grant R. Portal use among patients with chronic conditions: patient-reported care experiences. Med Care. 2019 Oct;57(10):809–14. doi: 10.1097/MLR.0000000000001178. [DOI] [PubMed] [Google Scholar]
- 62.Riippa I, Linna M, Rönkkö I. The effect of a patient portal with electronic messaging on patient activation among chronically ill patients: controlled before-and-after study. J Med Internet Res. 2014 Nov 19;16(11):e257. doi: 10.2196/jmir.3462. https://www.jmir.org/2014/11/e257/ v16i11e257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Riippa I, Linna M, Rönkkö I. A patient portal with electronic messaging: controlled before-and-after study. J Med Internet Res. 2015 Nov 09;17(11):e250. doi: 10.2196/jmir.4487. https://www.jmir.org/2015/11/e250/ v17i11e250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Robinson SA, Zocchi MS, Netherton D, Ash A, Purington CM, Connolly SL, Vimalananda VG, Hogan TP, Shimada SL. Secure messaging, diabetes self-management, and the importance of patient autonomy: a mixed methods study. J Gen Intern Med. 2020 Oct;35(10):2955–62. doi: 10.1007/s11606-020-05834-x. https://europepmc.org/abstract/MED/32440998 .10.1007/s11606-020-05834-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ronda MC, Dijkhorst-Oei LT, Rutten GE. Reasons and barriers for using a patient portal: survey among patients with diabetes mellitus. J Med Internet Res. 2014 Nov 25;16(11):e263. doi: 10.2196/jmir.3457. https://www.jmir.org/2014/11/e263/ v16i11e263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ronda MC, Dijkhorst-Oei LT, Rutten GE. Patients' experiences with and attitudes towards a diabetes patient web portal. PLoS One. 2015 Jun 18;10(6):e0129403. doi: 10.1371/journal.pone.0129403. https://dx.plos.org/10.1371/journal.pone.0129403 .PONE-D-15-00899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sabo R, Robins J, Lutz S, Kashiri P, Day T, Webel B, Krist A. Diabetes engagement and activation platform for implementation and effectiveness of automated virtual type 2 diabetes self-management education: randomized controlled trial. JMIR Diabetes. 2021 Mar 29;6(1):e26621. doi: 10.2196/26621. https://diabetes.jmir.org/2021/1/e26621/ v6i1e26621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sarkar U, Lyles CR, Parker MM, Allen J, Nguyen R, Moffet HH, Schillinger D, Karter AJ. Use of the refill function through an online patient portal is associated with improved adherence to statins in an integrated health system. Med Care. 2014 Mar;52(3):194–201. doi: 10.1097/MLR.0000000000000069. https://europepmc.org/abstract/MED/24374412 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Seo D, Park YR, Lee Y, Kim JY, Park JY, Lee JH. The use of mobile personal health records for hemoglobin A1c regulation in patients with diabetes: retrospective observational study. J Med Internet Res. 2020 Jun 02;22(6):e15372. doi: 10.2196/15372. https://www.jmir.org/2020/6/e15372/ v22i6e15372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sharit J, Idrees T, Andrade AD, Anam R, Karanam C, Valencia W, Florez H, Ruiz JG. Use of an online personal health record's Track Health function to promote positive lifestyle behaviors in Veterans with prediabetes. J Health Psychol. 2018 Apr;23(5):681–90. doi: 10.1177/1359105316681065.1359105316681065 [DOI] [PubMed] [Google Scholar]
- 71.Shimada SL, Allison JJ, Rosen AK, Feng H, Houston TK. Sustained use of patient portal features and improvements in diabetes physiological measures. J Med Internet Res. 2016 Jul 01;18(7):e179. doi: 10.2196/jmir.5663. https://www.jmir.org/2016/7/e179/ v18i7e179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tenforde M, Nowacki A, Jain A, Hickner J. The association between personal health record use and diabetes quality measures. J Gen Intern Med. 2012 Apr;27(4):420–4. doi: 10.1007/s11606-011-1889-0. https://europepmc.org/abstract/MED/22005937 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.van Vugt M, de Wit M, Sieverink F, Roelofsen Y, Hendriks SH, Bilo HJ, Snoek FJ. Uptake and effects of the e-vita personal health record with self-management support and coaching, for type 2 diabetes patients treated in primary care. J Diabetes Res. 2016;2016:5027356. doi: 10.1155/2016/5027356. doi: 10.1155/2016/5027356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Vo MT, Uratsu CS, Estacio KR, Altschuler A, Kim E, Alexeeff SE, Adams AS, Schmittdiel JA, Heisler M, Grant RW. Prompting patients with poorly controlled diabetes to identify visit priorities before primary care visits: a pragmatic cluster randomized trial. J Gen Intern Med. 2019 Jun;34(6):831–8. doi: 10.1007/s11606-018-4756-4. https://europepmc.org/abstract/MED/30746642 .10.1007/s11606-018-4756-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wald JS, Grant RW, Schnipper JL, Gandhi TK, Poon EG, Businger AC, Orav EJ, Williams DH, Volk LA, Middleton B. Survey analysis of patient experience using a practice-linked PHR for type 2 diabetes mellitus. AMIA Annu Symp Proc. 2009 Nov 14;2009:678–82. https://europepmc.org/abstract/MED/20351940 . [PMC free article] [PubMed] [Google Scholar]
- 76.Zocchi MS, Robinson SA, Ash AS, Vimalananda VG, Wolfe HL, Hogan TP, Connolly SL, Stewart MT, Am L, Netherton D, Shimada SL. Patient portal engagement and diabetes management among new portal users in the Veterans Health Administration. J Am Med Inform Assoc. 2021 Sep 18;28(10):2176–83. doi: 10.1093/jamia/ocab115. https://europepmc.org/abstract/MED/34339500 .6335848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Druss BG, Li J, Tapscott S, Lally CA. Randomized trial of a mobile personal health record for behavioral health homes. Psychiatr Serv. 2020 Aug 01;71(8):803–9. doi: 10.1176/appi.ps.201900381. https://europepmc.org/abstract/MED/32362226 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Aberger EW, Migliozzi D, Follick MJ, Malick T, Ahern DK. Enhancing patient engagement and blood pressure management for renal transplant recipients via home electronic monitoring and web-enabled collaborative care. Telemed J E Health. 2014 Sep;20(9):850–4. doi: 10.1089/tmj.2013.0317. https://europepmc.org/abstract/MED/25046403 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ahmed S, Ernst P, Bartlett SJ, Valois MF, Zaihra T, Paré G, Grad R, Eilayyan O, Perreault R, Tamblyn R. The effectiveness of web-based asthma self-management system, my asthma portal (MAP): a pilot randomized controlled trial. J Med Internet Res. 2016 Dec 01;18(12):e313. doi: 10.2196/jmir.5866. https://www.jmir.org/2016/12/e313/ v18i12e313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Apter AJ, Localio AR, Morales KH, Han X, Perez L, Mullen AN, Rogers M, Klusaritz H, Howell JT, Canales MN, Bryant-Stephens T. Home visits for uncontrolled asthma among low-income adults with patient portal access. J Allergy Clin Immunol. 2019 Sep;144(3):846–53.e11. doi: 10.1016/j.jaci.2019.05.030. https://europepmc.org/abstract/MED/31181221 .S0091-6749(19)30752-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Fiks AG, Mayne SL, Karavite DJ, Suh A, O'Hara R, Localio AR, Ross M, Grundmeier RW. Parent-reported outcomes of a shared decision-making portal in asthma: a practice-based RCT. Pediatrics. 2015 Apr;135(4):e965–73. doi: 10.1542/peds.2014-3167. https://europepmc.org/abstract/MED/25755233 .peds.2014-3167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Fiks AG, DuRivage N, Mayne SL, Finch S, Ross ME, Giacomini K, Suh A, McCarn B, Brandt E, Karavite D, Staton EW, Shone LP, McGoldrick V, Noonan K, Miller D, Lehmann CU, Pace WD, Grundmeier RW. Adoption of a portal for the primary care management of pediatric asthma: a mixed-methods implementation study. J Med Internet Res. 2016 Jun 29;18(6):e172. doi: 10.2196/jmir.5610. https://www.jmir.org/2016/6/e172/ v18i6e172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kogut SJ, Goldstein E, Charbonneau C, Jackson A, Patry G. Improving medication management after a hospitalization with pharmacist home visits and electronic personal health records: an observational study. Drug Healthc Patient Saf. 2014 Jan 17;6:1–6. doi: 10.2147/DHPS.S56574. https://europepmc.org/abstract/MED/24465136 .dhps-6-001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kim JW, Ryu B, Cho S, Heo E, Kim Y, Lee J, Jung SY, Yoo S. Impact of personal health records and wearables on health outcomes and patient response: three-arm randomized controlled trial. JMIR Mhealth Uhealth. 2019 Jan 04;7(1):e12070. doi: 10.2196/12070. https://mhealth.jmir.org/2019/1/e12070/ v7i1e12070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lau AY, Arguel A, Dennis S, Liaw ST, Coiera E. "Why didn't it work?" Lessons from a randomized controlled trial of a web-based personally controlled health management system for adults with asthma. J Med Internet Res. 2015 Dec 15;17(12):e283. doi: 10.2196/jmir.4734. https://www.jmir.org/2015/12/e283/ v17i12e283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Manard W, Scherrer JF, Salas J, Schneider FD. Patient portal use and blood pressure control in newly diagnosed hypertension. J Am Board Fam Med. 2016;29(4):452–9. doi: 10.3122/jabfm.2016.04.160008. http://www.jabfm.org/cgi/pmidlookup?view=long&pmid=27390376 .29/4/452 [DOI] [PubMed] [Google Scholar]
- 87.Toscos T, Coupe A, Wagner S, Ahmed R, Roebuck A, Flanagan M, Drouin M, Mirro M. Engaging patients in atrial fibrillation management via digital health technology: the impact of tailored messaging. J Innov Card Rhythm Manag. 2020 Aug;11(8):4209–17. doi: 10.19102/icrm.2020.110802. https://europepmc.org/abstract/MED/32874747 .icrm.2020.110802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wagner PJ, Dias J, Howard S, Kintziger KW, Hudson MF, Seol Y, Sodomka P. Personal health records and hypertension control: a randomized trial. J Am Med Inform Assoc. 2012;19(4):626–34. doi: 10.1136/amiajnl-2011-000349. https://europepmc.org/abstract/MED/22234404 .amiajnl-2011-000349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Martínez Nicolás I, Lê Cook B, Flores M, Del Olmo Rodriguez M, Hernández Rodríguez C, Llamas Sillero P, Baca-Garcia E. The impact of a comprehensive electronic patient portal on the health service use: an interrupted time-series analysis. Eur J Public Health. 2019 Jun 01;29(3):413–8. doi: 10.1093/eurpub/cky257.5240936 [DOI] [PubMed] [Google Scholar]
- 90.Cahill JE, Lin L, LoBiondo-Wood G, Armstrong TS, Acquaye AA, Vera-Bolanos E, Gilbert MR, Padhye NS. Personal health records, symptoms, uncertainty, and mood in brain tumor patients. Neurooncol Pract. 2014 Jun;1(2):64–70. doi: 10.1093/nop/npu005. https://europepmc.org/abstract/MED/26034618 .npu005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chiche L, Brescianini A, Mancini J, Servy H, Durand JM. Evaluation of a prototype electronic personal health record for patients with idiopathic thrombocytopenic purpura. Patient Prefer Adherence. 2012;6:725–34. doi: 10.2147/PPA.S36320. https://europepmc.org/abstract/MED/23077409 .ppa-6-725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Collins PW, Bolton-Maggs P, Stephenson D, Jenkins B, Loran C, Winter M. Pilot study of an Internet-based electronic patient treatment record and communication system for haemophilia, Advoy.com. Haemophilia. 2003 May;9(3):285–91. doi: 10.1046/j.1365-2516.2003.00747.x.747 [DOI] [PubMed] [Google Scholar]
- 93.Coquet J, Blayney DW, Brooks JD, Hernandez-Boussard T. Association between patient-initiated emails and overall 2-year survival in cancer patients undergoing chemotherapy: evidence from the real-world setting. Cancer Med. 2020 Nov;9(22):8552–61. doi: 10.1002/cam4.3483. https://europepmc.org/abstract/MED/32986931 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Groen WG, Kuijpers W, Oldenburg HS, Wouters MW, Aaronson NK, van Harten WH. Supporting lung cancer patients with an interactive patient portal: feasibility study. JMIR Cancer. 2017 Aug 08;3(2):e10. doi: 10.2196/cancer.7443. https://cancer.jmir.org/2017/2/e10/ v3i2e10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hall MJ, Herda MM, Handorf EA, Rybak CC, Keleher CA, Siemon M, Daly MB. Direct-to-patient disclosure of results of mismatch repair screening for Lynch syndrome via electronic personal health record: a feasibility study. Genet Med. 2014 Nov;16(11):854–61. doi: 10.1038/gim.2014.42. https://linkinghub.elsevier.com/retrieve/pii/S1098-3600(21)02659-9 .S1098-3600(21)02659-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hong MK, Wilcox L, Feustel C, Wasileski-Masker K, Olson TA, Simoneaux SF. Adolescent and caregiver use of a tethered personal health record system. AMIA Annu Symp Proc. 2016 Feb 10;2016:628–37. https://europepmc.org/abstract/MED/28269859 . [PMC free article] [PubMed] [Google Scholar]
- 97.Kidwell KM, Peugh J, Westcott E, Nwankwo C, Britto MT, Quinn CT, Crosby LE. Acceptability and feasibility of a disease-specific patient portal in adolescents with sickle cell disease. J Pediatr Hematol Oncol. 2019 Oct;41(7):561–7. doi: 10.1097/MPH.0000000000001341. https://europepmc.org/abstract/MED/30339657 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.O'Hea EL, Creamer S, Flahive JM, Keating BA, Crocker CR, Williamson SR, Edmiston KL, Harralson T, Boudreaux ED. Survivorship care planning, quality of life, and confidence to transition to survivorship: a randomized controlled trial with women ending treatment for breast cancer. J Psychosoc Oncol. 2022;40(5):574–94. doi: 10.1080/07347332.2021.1936336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Pai HH, Lau F, Barnett J, Jones S. Meeting the health information needs of prostate cancer patients using personal health records. Curr Oncol. 2013 Dec;20(6):e561–9. doi: 10.3747/co.20.1584. https://europepmc.org/abstract/MED/24311957 .conc-20-e561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tarver WL, Robb BW, Haggstrom DA. Usefulness and usability of a personal health record and survivorship care plan for colorectal cancer survivors: survey study. JMIR Cancer. 2019 Aug 20;5(2):e10692. doi: 10.2196/10692. https://cancer.jmir.org/2019/2/e10692/ v5i2e10692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wiljer D, Leonard KJ, Urowitz S, Apatu E, Massey C, Quartey NK, Catton P. The anxious wait: assessing the impact of patient accessible EHRs for breast cancer patients. BMC Med Inform Decis Mak. 2010 Sep 01;10:46. doi: 10.1186/1472-6947-10-46. https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/1472-6947-10-46 .1472-6947-10-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Williamson RS, Cherven BO, Gilleland Marchak J, Edwards P, Palgon M, Escoffery C, Meacham LR, Mertens AC. Meaningful use of an electronic personal health record (ePHR) among pediatric cancer survivors. Appl Clin Inform. 2017 Mar 15;8(1):250–64. doi: 10.4338/ACI-2016-11-RA-0189. https://europepmc.org/abstract/MED/28293684 .2016-11-RA-0189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Anand T, Nitpolprasert C, Kerr SJ, Apornpong T, Ananworanich J, Phanuphak P, Phanuphak N. Implementation of an online HIV prevention and treatment cascade in Thai men who have sex with men and transgender women using Adam's Love Electronic Health Record system. J Virus Erad. 2017 Jan 01;3(1):15–23. doi: 10.1016/S2055-6640(20)30293-4. https://europepmc.org/abstract/MED/28275454 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Bidmead E, Marshall A. A case study of stakeholder perceptions of patient held records: the Patients Know Best (PKB) solution. Digit Health. 2016 Sep 21;2:2055207616668431. doi: 10.1177/2055207616668431. https://journals.sagepub.com/doi/10.1177/2055207616668431?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed .10.1177_2055207616668431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Crouch PB, Rose CD, Johnson M, Janson SL. A pilot study to evaluate the magnitude of association of the use of electronic personal health records with patient activation and empowerment in HIV-infected veterans. PeerJ. 2015 Mar 19;3:e852. doi: 10.7717/peerj.852. https://europepmc.org/abstract/MED/25802815 .852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Druss BG, Ji X, Glick G, von Esenwein SA. Randomized trial of an electronic personal health record for patients with serious mental illnesses. Am J Psychiatry. 2014 Mar;171(3):360–8. doi: 10.1176/appi.ajp.2013.13070913.1815010 [DOI] [PubMed] [Google Scholar]
- 107.Jhamb M, Cavanaugh KL, Bian A, Chen G, Ikizler TA, Unruh ML, Abdel-Kader K. Disparities in electronic health record patient portal use in nephrology clinics. Clin J Am Soc Nephrol. 2015 Nov 06;10(11):2013–22. doi: 10.2215/CJN.01640215. https://cjasn.asnjournals.org/cgi/pmidlookup?view=long&pmid=26493242 .CJN.01640215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kahn JS, Hilton JF, Van Nunnery T, Leasure S, Bryant KM, Hare CB, Thom DH. Personal health records in a public hospital: experience at the HIV/AIDS clinic at San Francisco General Hospital. J Am Med Inform Assoc. 2010;17(2):224–8. doi: 10.1136/jamia.2009.000315. https://europepmc.org/abstract/MED/20190069 .17/2/224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Keith McInnes D, Shimada SL, Rao SR, Quill A, Duggal M, Gifford AL, Brandt CA, Houston TK, Ohl ME, Gordon KS, Mattocks KM, Kazis LE, Justice AC. Personal health record use and its association with antiretroviral adherence: survey and medical record data from 1871 US veterans infected with HIV. AIDS Behav. 2013 Nov;17(9):3091–100. doi: 10.1007/s10461-012-0399-3. [DOI] [PubMed] [Google Scholar]
- 110.McInnes DK, Shimada SL, Midboe AM, Nazi KM, Zhao S, Wu J, Garvey CM, Houston TK. Patient use of electronic prescription refill and secure messaging and its association with undetectable HIV viral load: a retrospective cohort study. J Med Internet Res. 2017 Mar 15;19(2):e34. doi: 10.2196/jmir.6932. https://www.jmir.org/2017/2/e34/ v19i2e34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Kiberd J, Khan U, Stockman C, Radhakrishnan A, Phillips M, Kiberd BA, West KA, Soroka S, Chan C, Tennankore KK. Effectiveness of a web-based eHealth portal for delivery of care to home dialysis patients: a single-arm pilot study. Can J Kidney Health Dis. 2018 Sep 7;5:2054358118794415. doi: 10.1177/2054358118794415. https://journals.sagepub.com/doi/10.1177/2054358118794415?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed .10.1177_2054358118794415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Lee J, Kim JG, Jin M, Ahn K, Kim B, Kim S, Kim J. Beneficial effects of two types of personal health record services connected with electronic medical records within the hospital setting. Comput Inform Nurs. 2017 Nov;35(11):574–81. doi: 10.1097/CIN.0000000000000362. [DOI] [PubMed] [Google Scholar]
- 113.Miller DM, Moore SM, Fox RJ, Atreja A, Fu AZ, Lee JC, Saupe W, Stadtler M, Chakraborty S, Harris CM, Rudick RA. Web-based self-management for patients with multiple sclerosis: a practical, randomized trial. Telemed J E Health. 2011;17(1):5–13. doi: 10.1089/tmj.2010.0133. https://europepmc.org/abstract/MED/21214498 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Navaneethan SD, Jolly SE, Schold JD, Arrigain S, Nakhoul G, Konig V, Hyland J, Burrucker YK, Dann PD, Tucky BH, Sharp J, Nally JV. Pragmatic randomized, controlled trial of patient navigators and enhanced personal health records in CKD. Clin J Am Soc Nephrol. 2017 Sep 07;12(9):1418–27. doi: 10.2215/CJN.02100217. https://cjasn.asnjournals.org/cgi/pmidlookup?view=long&pmid=28778854 .CJN.02100217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Plimpton E. A quality improvement project to increase patient portal enrollment and utilization in women living with HIV at risk for disengagement in care. J Assoc Nurses AIDS Care. 2020;31(1):60–5. doi: 10.1097/JNC.0000000000000153. [DOI] [PubMed] [Google Scholar]
- 116.Reich J, Canakis A, Shankar D, Harrington J, Apte M, Weinberg J, Jones E, Noronha A, Wasan SK, Farraye FA. The use of an EHR patient portal (Mychart-Epic) in patients with inflammatory bowel disease. Crohn's Colitis 360. 2019 Oct;1(3):otz039. doi: 10.1093/crocol/otz039. [DOI] [Google Scholar]
- 117.Nielsen AS, Halamka JD, Kinkel RP. Internet portal use in an academic multiple sclerosis center. J Am Med Inform Assoc. 2012;19(1):128–33. doi: 10.1136/amiajnl-2011-000177. https://europepmc.org/abstract/MED/21571744 .amiajnl-2011-000177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Son H, Nahm ES. Older adults' experience using patient portals in communities: challenges and opportunities. Comput Inform Nurs. 2019 Jan;37(1):4–10. doi: 10.1097/CIN.0000000000000476. [DOI] [PubMed] [Google Scholar]
- 119.Tom JO, Mangione-Smith R, Solomon C, Grossman DC. Integrated personal health record use: association with parent-reported care experiences. Pediatrics. 2012 Jul;130(1):e183–90. doi: 10.1542/peds.2011-1786.peds.2011-1786 [DOI] [PubMed] [Google Scholar]
- 120.van den Heuvel SC, Meije D, Regeer EJ, Sinnema H, Riemersma RF, Kupka RW. The user experiences and clinical outcomes of an online personal health record to support self-management of bipolar disorder: a pretest-posttest pilot study. J Affect Disord. 2018 Oct 01;238:261–8. doi: 10.1016/j.jad.2018.05.069.S0165-0327(18)30030-2 [DOI] [PubMed] [Google Scholar]
- 121.van der Vaart R, Drossaert CH, Taal E, Drossaers-Bakker KW, Vonkeman HE, van de Laar MA. Impact of patient-accessible electronic medical records in rheumatology: use, satisfaction and effects on empowerment among patients. BMC Musculoskelet Disord. 2014 Mar 26;15:102. doi: 10.1186/1471-2474-15-102. https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/1471-2474-15-102 .1471-2474-15-102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, Hartmann-Boyce J, Ryan R, Shepperd S, Thomas J, Welch V, Thomson H. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020 Jan 16;368:l6890. doi: 10.1136/bmj.l6890. http://www.bmj.com/lookup/pmidlookup?view=long&pmid=31948937 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Dunsch F, Evans DK, Macis M, Wang Q. Bias in patient satisfaction surveys: a threat to measuring healthcare quality. BMJ Glob Health. 2018 Apr 12;3(2):e000694. doi: 10.1136/bmjgh-2017-000694. https://gh.bmj.com/lookup/pmidlookup?view=long&pmid=29662696 .bmjgh-2017-000694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hanna L, Gill SD, Newstead L, Hawkins M, Osborne RH. Patient perspectives on a personally controlled electronic health record used in regional Australia. Health Inf Manag. 2017 Jan;46(1):42–8. doi: 10.1177/1833358316661063.1833358316661063 [DOI] [PubMed] [Google Scholar]
- 125.Fylan F, Caveney L, Cartwright A, Fylan B. Making it work for me: beliefs about making a personal health record relevant and useable. BMC Health Serv Res. 2018 Jun 14;18(1):445. doi: 10.1186/s12913-018-3254-z. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-018-3254-z .10.1186/s12913-018-3254-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Greenberg AJ, Falisi AL, Finney Rutten LJ, Chou WS, Patel V, Moser RP, Hesse BW. Access to electronic personal health records among patients with multiple chronic conditions: a secondary data analysis. J Med Internet Res. 2017 Jun 02;19(6):e188. doi: 10.2196/jmir.7417. https://www.jmir.org/2017/6/e188/ v19i6e188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Stewart M, Brown JB, Donner A, McWhinney IR, Oates J, Weston WW, Jordan J. The impact of patient-centered care on outcomes. J Fam Pract. 2000 Sep;49(9):796–804. [PubMed] [Google Scholar]
- 128.Antonio MG, Petrovskaya O, Lau F. The state of evidence in patient portals: umbrella review. J Med Internet Res. 2020 Nov 11;22(11):e23851. doi: 10.2196/23851. https://www.jmir.org/2020/11/e23851/ v22i11e23851 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The search strategy used, that includes terms related to the search categories: “patient,” “intervention,” and “outcome.”.
The 4 modified Joanna Briggs Institute critical appraisal tools used in this study.
Proportion of beneficial effects reported per health outcome of all studies, presented per disease category.
The proportion of beneficial effects reported per health outcome of 16 high quality studies, presented per disease category.


