Abstract
Rationale
The adoption of prone positioning for patients with acute respiratory distress syndrome (ARDS) has historically been poor. However, in mechanically ventilated patients with coronavirus disease (COVID-19) ARDS, proning has increased. Understanding the factors influencing this change is important for further expanding and sustaining the use of prone positioning in appropriate clinical settings.
Objectives
To characterize factors influencing the implementation of prone positioning in mechanically ventilated patients with COVID-19 ARDS.
Methods
We conducted a qualitative study using semistructured interviews with 40 intensive care unit (ICU) team members (physicians, nurses, advanced practice providers, respiratory therapists, and physical therapists) working at two academic hospitals. We used the Consolidated Framework for Implementation Research, a widely used implementation science framework outlining important features of implementation, to structure the interview guide and thematic analysis of interviews.
Results
ICU clinicians reported that during the COVID-19 pandemic, proning was viewed as standard early therapy for COVID-19 ARDS rather than salvage therapy for refractory hypoxemia. By caring for large volumes of proned patients, clinicians gained increased comfort with proning and now view proning as a low-risk, high-benefit intervention. Within ICUs, adequate numbers of trained staff members, increased team agreement around proning, and the availability of specific equipment (e.g., to limit pressure injuries) facilitated greater proning use. Hospital-level supports included proning teams, centralized educational resources specific to the management of COVID-19 (including a recommendation for prone positioning), and an electronic medical record proning order. Important implementation processes included informal dissemination of best practices through on-the-job learning and team interactions during routine bedside care.
Conclusions
The implementation of prone positioning for COVID-19 ARDS took place in the context of evolving clinician viewpoints and ICU team cultures. Proning was facilitated by hospital support and buy-in and leadership from bedside clinicians. The successful implementation of prone positioning during the COVID-19 pandemic may serve as a model for the implementation of other evidence-based therapies in critical care.
Keywords: prone positioning, acute respiratory distress syndrome, coronavirus disease, implementation science
Early prone positioning for patients with moderate to severe acute respiratory distress syndrome (ARDS) was shown to reduce mortality in a randomized controlled trial and meta-analyses (1–3). Despite this evidence and a subsequent multisociety ARDS guideline strongly recommending prone positioning (4), adoption has historically been poor. Before the coronavirus disease (COVID-19) pandemic, studies showed that only 16–33% of patients with ARDS received proning (5–9). Potential reasons for low adoption include underrecognition of ARDS by clinicians (5, 10), a perception of proning as salvage therapy for refractory hypoxemia (6, 11), concern that proning is prohibitively labor intensive (12), and a preference for and availability of alternative adjunctive therapies (e.g., neuromuscular blockade, extracorporeal membrane oxygenation) (11, 13).
Proning practice has changed during the COVID-19 pandemic. In studies from multiple countries, 53–70% of mechanically ventilated patients with COVID-19 received prone positioning (14–17). In our own medical system, there was a 50% absolute increase in the use of early proning in COVID-19 versus historic ARDS (18), and in other health systems there are reports of increased hospital-level ability to offer proning (19). However, a multisite study in the United States showed considerable variation in proning use among hospitals (5–80% of patients proned), suggesting a continuing need for improved implementation (20). Although new therapies and advances in medicine may take more than a decade to move from discovery into clinical care (21), prone positioning for COVID-19 ARDS was rapidly adopted (18). This rapid implementation provides a model for understanding how evidence-based critical care practices can be quickly and efficiently adopted (22).
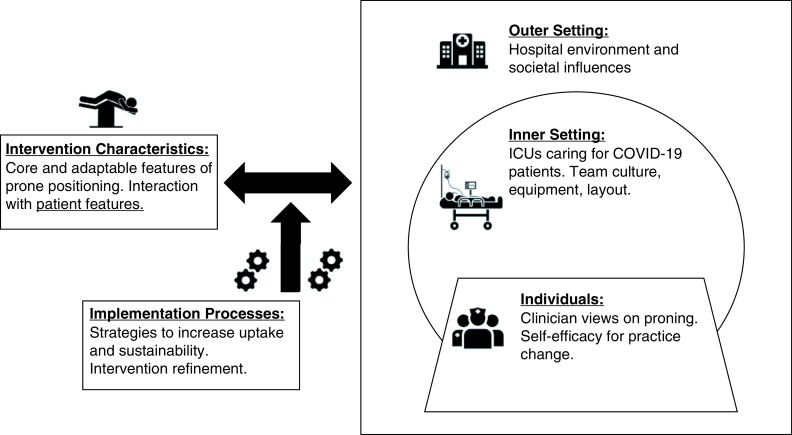
Implementation science uses frameworks, such as the Consolidated Framework for Implementation Research (CFIR), to systematically assess and identify important implementation factors across multiple domains (23). The CFIR, which is a framework recommended by the American Thoracic Society (24), comprises five domains (intervention characteristics, individuals, inner setting, outer setting, and implementation processes) that affect implementation and assists with rigorously conceptualizing implementation investigations (23). In this study we used the CFIR to guide a qualitative investigation of the factors influencing the rapid implementation of prone positioning for COVID-19 ARDS (25). Improved understanding of these factors will inform further expansion and sustainability of prone positioning and could inform the implementation of evidence-based critical care more broadly.
Methods
Study Design, Setting, and Participants
We conducted a qualitative study with intensive care unit (ICU) team members caring for patients with COVID-19 ARDS. Participants were recruited from three medical ICUs at two hospitals, a large quaternary-care academic center and a smaller community–academic hospital, in the Johns Hopkins Health System in Baltimore, Maryland. We recruited attending pulmonary and critical care medicine physicians and fellows, advanced practice providers (APPs), registered nurses (RNs), and respiratory therapists (RTs). After initial interviews, we also recruited physical therapists (PTs) from the “proning team” (a team that assisted ICUs with carrying out proning during COVID-19 surges) (26). We used purposive sampling, consisting of direct outreach to clinicians (medical doctors [MDs], APPs, and PTs) known to be engaged with the use of prone positioning, and convenience sampling (for RNs and RTs) through recruitment e-mails to staff members and presentations at staff meetings. We targeted a minimum sample size of five providers of each type from each hospital. APPs and PTs were recruited only from the larger quaternary-care center, as APPs are not employed in the smaller hospital ICU, and the proning team was available only at the larger academic center. Participants of all types and from both hospitals were recruited and interviewed on a rolling basis. The final sample size was determined by data saturation, which was considered to have occurred when no new themes emerged with additional interviews. Study reporting follows the Consolidated Criteria for Reporting Qualitative Research (see Appendix A in the online supplement) (27).
This study was approved by the Johns Hopkins School of Medicine Institutional Review Board (IRB00259955), and participants provided verbal consent.
Interview and Data Collection
One-on-one semistructured interviews following a written interview guide targeting CFIR domains were conducted using video conferencing software (see Appendices B and C). Study-specific CFIR domain definitions are shown in Figure 1. “Patient characteristics,” which is not a separate domain of the CFIR, was considered a subdomain of “intervention characteristics,” as the patient–intervention interaction was considered an important feature for implementation (28). The interview guide was drafted by author C.H.H. and then revised in discussion with authors with expertise in critical care (D.N.H. and M.P.K.), implementation science (M.N.E. and M.P.K.), and qualitative research (M.N.E. and M.P.K.). The initial interview guide was then pilot tested with one participant (fellow) and underwent minimal revisions. After subsequent interviews, the interview guide was iteratively updated after discussion of interview transcripts between the interviewer (C.H.H.) and senior authors D.N.H. and M.N.E. using the constant comparison method to explore emerging themes from prior interviews. Interview audio was recorded and transcribed verbatim using a medical transcription service.
Figure 1.
Consolidated Framework for Implementation Research (CFIR) domains with study-specific definitions. The CFIR consists of five domains to organize the study of factors that are important for effective implementation. The intervention (intervention domain), in this case, prone positioning, is introduced into a context that consists of individual clinicians (individuals) working in ICUs (inner setting) that exist within the broader hospital and societal context (outer setting). The intervention has core features necessary for efficacy and efficiency but is also adapted and refined by the context in which it is introduced (double arrow to individuals, inner setting, and outer setting). Implementation processes are the strategies that can improve implementation (increased adoption, penetration, and sustainability) of the intervention being implemented. COVID-19 = coronavirus disease; ICU = intensive care unit.
Qualitative Analysis
Interview transcripts were analyzed using NVivo 12.0 software (QSR International Pty Ltd.). We used thematic analysis to identify themes, which we then mapped to CFIR domains. The initial codebook was developed by authors C.H.H., B.S., and M.N.E., who analyzed the first five transcripts. Subsequent transcripts were then coded by C.H.H. by applying codes to selected quotations, and new codes were added as themes emerged (29). Transcripts were then coded in duplicate by an additional team member (B.S. or M.E.C.). Qualitative coders (C.H.H., B.S., and M.E.C.) met frequently to ensure consistency and completeness of coding, with a fourth investigator (M.N.E.) consulted for unresolved discrepancies. Interrater reliability was assessed and demonstrated high percentage agreement (99%) and fair interrater reliability (Cohen’s κ = 0.40).
Results
Interviews with 40 ICU team members were conducted from February to July 2021. Participant characteristics are shown in Table 1. Of the MD, APP, and PT participants contacted, 21 of 24 participated. Of the 20 RNs and RTs who responded to recruitment materials, 19 participated. The median interview length was 24 minutes (range, 12–44 min).
Table 1.
Demographic and occupational characteristics of study participants
| Characteristic | Full Sample (n = 40) |
|---|---|
| Provider type, n (%) | |
| Attending MD | 7 (17.5) |
| Fellow MD | 5 (12.5) |
| APP | 4 (10.0) |
| RN | 12 (30.0) |
| RT | 7 (17.5) |
| PT | 5 (12.5) |
| Hospital, n (%)* | |
| Academic | 28 (70.0) |
| Community–academic | 13 (32.5) |
| Demographics/occupational | |
| Age, y, median (IQR) | 34 (30–39) |
| Female, n (%) | 29 (72.5) |
| Years in health care, median (IQR) | 9.5 (6.0–14.5) |
| Years in ICU, median (IQR) | 7.0 (3.5–10.0) |
| Clinical role exclusively in ICU, n (%) | 24 (60.0) |
Definition of abbreviations: APP = advanced practice provider; ICU = intensive care unit; IQR = interquartile range; MD = medical doctor; PT = physical therapist; RN = registered nurse; RT = respiratory therapist.
One participant reported splitting time equally between both campuses and is counted in both the academic and community–academic categories.
CFIR Intervention Domain: Prone Positioning
Consistent with quantitative work showing increased frequency of proning, earlier proning initiation, and longer proning sessions in patients with COVID-19 ARDS (18), participants noted practice changes:
(APP02) Within the first couple of blood gases if their P/F [partial pressure of arterial oxygen/fraction of inspired oxygen] ratio fell below 150, we were proning them, which was very different than before when we usually would’ve given patients hours and hours . . . maybe even a day or two to try to come around.
Some of these changes were attributed to a higher volume of patients with more homogeneous and severe ARDS:
(MD12) Proning has been more of a focus during this pandemic, in part because we’ve had more patients that qualify as having severe ARDS and would qualify for prone positioning.
In addition, participants noted that proning use expanded to populations in whom there have historically been concerns about proning (e.g., high body mass index, hemodynamic instability):
(RN04) As COVID has progressed . . . we’re not finding exceptions anymore. . . . We’re not really finding unpronable patients. We are finding ways to make it work for just about everybody.
CFIR Individual Domain: ICU Clinicians
Themes involving ICU clinicians are shown with supporting quotations in Table 2. Repeated exposure to proning reinforced provider belief in efficacy. This shifted clinician views on the risk and benefits of proning, yielding a view of proning as a low-risk, high-benefit intervention. However, the increased volumes of proned patients receiving longer proning sessions also made some of the adverse effects of proning more apparent (i.e., severe pressure wounds, musculoskeletal injuries). Although this could deter further proning, some clinicians noted that these risks did not alter their decisions to use proning:
Table 2.
Consolidated Framework for Implementation Research individual domain: intensive care unit clinician factors influencing proning use in coronavirus disease acute respiratory distress syndrome
| Study Theme and Subthemes | (Provider Type and Number) Supporting Quotation |
|---|---|
| Clinician views of proning | |
| Repeated exposure reinforced belief in efficacy | (RT07) Before COVID, it was more of like, “Do we really know if this is going to work . . .?” But I think going through COVID, it’s like we knew this is going to work. So, I think everyone’s viewpoint kind of shifted. |
| Repeated exposure shifted views on risks/benefits | (MD01) I think that I’ve seen enough volume of patients now to see that it’s a potentially high-benefit, low-risk intervention. . . . Whereas before, I think my mind-set might have been like, “Should we prone them,” now, my question might be like, “Is there a reason I should not prone them?” |
| Repeated and prolonged proning revealed newly apparent risks | (MD06) The harms of prolonged proning that I’ve seen during COVID, I just had only rarely seen pre-COVID. And I think it’s just the volume of people proned and the volume of people prone for prolonged periods of time . . . really severe pressure injuries, facial injuries, periorbital edema, shoulder injuries, brachial plexus injuries. |
| Improved familiarity and comfort with proning may influence future practice | (MD02) I would definitely attempt it in other non-COVID ARDS patients. But I wonder what my practice will be like because we are able to manage non-COVID ARDS in the MICU, (flu, and other things) sort of without as much aggressive proning, from my memory. But I certainly would consider doing it and I would feel very comfortable with it. |
Definition of abbreviations: ARDS = acute respiratory distress syndrome; COVID = coronavirus disease; MD = medical doctor; MICU = medical intensive care unit; RT = respiratory therapist.
(MD03) We’re talking about lives being saved, and wounds are not going to kill this person. So, we just got to bite the bullet.
Participants anticipated that they would also increase their use of proning in patients with non–COVID-19 ARDS, though there was uncertainty regarding necessity and efficacy in that setting (Table 2).
CFIR Inner Setting: ICU Characteristics
Major themes related to ICU characteristics involved 1) staffing, 2) team experience with proning, and 3) ICU equipment and layout (Table 3). To carry out proning safely, adequate numbers of trained staff members were needed. Although the number of bedside providers needed to prone a patient was well defined by our participants (three or four ICU team members), an optimal nurse-to-patient ratio for proned patients was debated, specifically, whether a 1:1 nurse-to-patient ratio was required. Although some MDs/APPs favored less intensive staffing ratios, the extra nursing care required for proned patients may be less apparent to these clinicians:
Table 3.
Consolidated Framework for Implementation Research inner setting: intensive care unit factors influencing proning use in coronavirus disease acute respiratory distress syndrome
| Study Theme (Definition) and Subthemes | (Provider Type and Number) Supporting Quotation |
|---|---|
| Staffing (staffing requirements for safe proning and challenges in staffing) | (RN09): You need the physical people to flip people. . . . I [also] need somebody who’s going to know you can’t yank a central line this way. . . . It’s not just [the] physical people, but people who [have] probably done it before, like who can kind of do it safely. |
| Adequate staff with training needed | (RN10) I mean, I think if we could really figure out about the whole making them a one-to-one versus if it was okay to have them paired with another patient . . . I think if there is a way that they can maintain safety and that we can also have it paired with another patient, I think that’s the best because I don’t think that really staffing is ever going to get better. |
| Optimal nurse-to-patient ratio unknown | (APP04) I think we also had this real stigma [that] with staffing, that if a patient was proned, at least from a nursing perspective, that it needed to be a one-on-one nurse to patient ratio. . . . Once COVID hit, you would have two proned patients that you were paired together with. . . . I think it made us realize that the act of proning takes a little bit of work to get them flipped, but once they are proned, you aren’t really doing anything with them. |
| Travel nurses brought different degrees of experience | (RN11) Then the other issue is the number of travelers. . . . We don’t know which ones of them are comfortable with proning, have done it a lot, what their process was, and they’re not that good about knowing our policies. |
| Frequent attending MD/fellow turnover led to variability in practice | (RN08) What became challenging was . . . when a provider would want them supinated like on a Tuesday, and then we would allow that to happen, and then on Wednesday, a new attending would come in and it would be, “Oh, let’s prone them,” and we were like, “Wait a minute. We just did that, they’re doing okay.” |
| Team experience with proning | |
| Team agreement |
(MD10) Probably the single biggest change was just the rapidity in which people got proned and, I think, the acceptance of the team that we were doing this. I mean, it just happened and there is no whingeing* about it. (RN09) What has changed from our end is every time we see a patient start to not do well or have increase in oxygen or PEEP requirements, we almost automatically know that we are going to end up proning them. But I feel like, in that way, everybody ends up being on the same page almost. |
| Repeated proning improved comfort | (APP02) I think it’s a lot more comfort with us doing it too. I don’t really sense near as much anxiety about turning a patient, or they may not be stable enough to turn, which was a comment we would hear frequently [before COVID-19]. I mean, you still hear that, certainly, if a patient is unstable, but nearly everybody was felt to be too unstable to prone previously, and now it’s a rare circumstance that you get that feedback. |
| Decision to prone made by staff members with less training | (MD04) I think proning, especially if you do it with any frequency as we have been doing, it’s a pretty safe thing to do, and therefore the benefit to risk ratio is favorable, and I think interns and residents should have the privilege to [decide to] prone. |
| Preparation for proning became standard | (MD11) Making sure they have the lines in place, and stuff ahead of the fact probably is an intentional process now, whereas I don’t think we always sort of thought ahead for that. |
| ICU equipment and layout | |
| ICUs stocked with basic but important equipment | (PT01) I think using the simple equipment worked. Of course, things like using Mepilex bandages to protect bony prominences, and the Z-Flo pillow to prevent kind of pressure ulcers on the face. Those are important. |
| Wider beds and specialty beds became standard in some units | (RN03) So with these new beds, they’re wider than our regular beds which is helpful. With this supination and proning, we need a little bit more space. They’re also air [mattresses], so they’re better for their pressure injury prevention, and then also the way that the bed tilts in a way that we can still feed the patients because it’s important to feed them. |
| Room size and patient visibility | (RN04) It was definitely more difficult in [repurposed COVID-19 ICU] . . . because [the rooms] are not ICU rooms, so they’re a lot smaller. . . . A majority of their doors are just wooden regular doors and didn’t even have windows on them. To have a patient that sick that you’re proning and not being able to see them was a big challenge. . . . They replaced the doors to have windows, which is better, but still, it’s definitely much easier with the ICU style, having the glass door window. |
Definition of abbreviations: APP = advanced practice provider; COVID = coronavirus disease; ICU = intensive care unit; MD = medical doctor; PEEP = positive end-expiratory pressure; PT = physical therapist; RN = registered nurse.
Colloquial for “whining.”
(RT01) There’s a lot more frustrations for them [RNs] in terms of how much more care is involved for the patient and how it complicates their care. . . . Just bathing the patient becomes much more of an event.
A potential staffing-related barrier to proning was the use of travel nurses, who had variable experience with and perceptions of prone positioning. An additional challenge was the frequent turnover in attending MDs and fellows (part of the COVID-19 staffing model in these hospitals). This revealed variable proning practices (e.g., when to initiate proning, when to supinate) that were frustrating for the ICU teams carrying out proning.
Many participants noted increased team agreement around proning in comparison with team attitudes before COVID-19. This agreement and increased comfort with proning led to more rapid and decisive use of this therapy:
(MD10) We did a lot less of salvage proning, and I think we did a lot less of waffling back and forth, “Should we prone? Should we not?.”
As proning increased, the decision to initiate proning was often made by MDs at earlier stages of training. For example, residents began deciding to initiate proning overnight, whereas previously this decision would have been discussed on the next day’s ICU rounds. Although this may decrease a barrier to proning, there were also concerns regarding this trend:
(MD10) The decision was being made at a progressively lower level as the pandemic went on. . . . That’s both good and bad. . . . There were a couple of times when I think the decision was almost reflexive, and it would have benefited from a little more consideration. Someone who’s got ARDS but also has renal failure clearly is going to need a dialysis catheter; probably should wait to prone them until we have the dialysis catheter in.
Several features of ICU practice, equipment, and layout were important for proning. During the pandemic, ICUs more intentionally prepared patients for potential proning (i.e., potentially needed vascular access and imaging obtained). Regarding equipment, participants noted that proning was accomplished with basic but important equipment that included foam bandages to protect vulnerable pressure points, pressure redistributing pillows (30) to provide protection against pressure injuries around the face, and blanket rolls to support the patient during proning. Having this equipment readily available was important for the teams who performed the proning procedures. No participants reported the use of proning-specific equipment such as specialty proning beds (31). However, in one of the dedicated COVID-19 units, wider specialty beds with air mattresses to reduce pressure wounds became standard for any patient who might be proned, and were viewed by the nursing team as instrumental for efficient and safe proning.
CFIR Outer Setting: Hospital and Societal Context
Several hospital and larger contextual factors influenced proning (Table 4). Early in the pandemic, both study hospitals dedicated resources to support the expansion of prone positioning. This included developing proning educational materials and disseminating them on a centralized online platform shared between both hospitals. At the larger academic center the administration supported the formation of a proning team that assisted with proning in times of high volume. Finally, an electronic medical record order for proning was developed and shared between both hospitals. This was viewed as helpful for creating standardized communication and work flows to support proning.
Table 4.
Consolidated Framework for Implementation Research outer setting: hospital and societal factors influencing proning use in coronavirus disease acute respiratory distress syndrome
| Study Theme (Definition) and Subthemes | (Provider Type and Number) Supporting Quotation |
|---|---|
| Hospital resources | |
| Hospital dedicated resources to proning | (RN02) There was an educational video created and put on the COVID-19 resource portal, and they knew that there were other institutions using this, so there was a video made here at Hopkins describing it. And I know the prone team—that group, because I became a part of it later on. And I know there was a literature search involved and much thought, and then they got the resources to develop it and put it out there for the entire hospital to use. |
| Proning EMR order | (APP01) All of a sudden, this magical Epic [EMR] order appeared [and] it wasn’t a nursing communication anymore. So, it became more standardized for supinating and prone . . . over time and with kind of comfort level, that decision [to prone] became more of just as far as we’re going to add a pressor or vasodilator therapy as something that kind of came a little more fluidly. |
| Dedicated COVID-19 units (hospital created units dedicated wholly to COVID-19 critical care) | |
| Repurposed units presented training challenges | (MD12) And I think there’s excitement, generally, being in the [new COVID-19 ICU]. Those are not all ICU-trained-level nurses, although now they’ve become that. I think, in the beginning, there was certainly a lot of . . . intimidation around, like, “Ugh, how are we going to learn how to do this? How are we going to actually do this?” But now, people have really taken advantage of it and picked it up as time’s gone on. |
| Developed expertise in proning and ARDS management more broadly | (MD02) The advantage that we had on ICU X [the new COVID-19 ICU] is that these nurses were almost like a blank slate . . . And I would say what’s interesting is these nurses are really good at treating hypoxic respiratory failure. . . . So one, it [proning] was part of the training on how to take care of these COVID ICU patients. And then two, it was just kind of a like—with that was just like full team buy-in. |
| Implementation of proning may have been better in these units | (RT02) So in the COVID ICUs, we are going to proning immediately. We’re proning patients a lot faster; we’re leaving them prone longer. Whereas in the non-COVID ICUs, we’re kind of waiting a little bit and saying, “Hey we’ve tried APRV for a while; we’ve tried this for a while.” But rather than leaving the patient prone for 24 h or 48 h, they more so are 12 h, 24 h, let’s supinate this patient. |
| COVID-19 as a novel disease | |
| Lack of other proven therapies refocused care on evidence-based practice | (APP01) I think it came down to that we didn’t really have any targeted treatment for this. And all of the kind of anecdotal data that came out, as far as out of Italy and New York. . . . And fortunately, I think being at Hopkins, the thought was like, “Well, we go evidence-based-wise.” So we’ll continue what we’re doing from the ARDS Network. And it was pretty obvious we were still going to prone. . . . And we have to just go back to our guidelines and our P/Fs of less than 150 and do it early. |
| Interest in “novel” approaches to new disease process | (MD10) And I think the fact that it was a new disease, not a new syndrome, but a new disease . . . [the] suggestion of “we should prone everyone as soon as they hit those criteria,” I think the ground for that was a lot more fertile than if it had just been, “We’re going to start proning every patient with ARDS.” |
| Researcher interest in proning | (MD04) And COVID was a new problem, and a lot of people were paying special attention to it, including more than one person in the pulmonary division who was interested in proning, and when somebody is very focused on an aspect of the problem, clinicians understand that this is something worth considering. So, the fact that there’s a researcher prowling around talking about proning raises consciousness. |
Definition of abbreviations: APP = advanced practice provider; APRV = airway pressure release ventilation; ARDS=acute respiratory distress syndrome; COVID = coronavirus disease; EMR = electronic medical record; ICU = intensive care unit; MD = medical doctor; P/F = partial pressure of arterial oxygen/fraction of inspired oxygen; RN = registered nurse; RT = respiratory therapist.
The creation of dedicated COVID-19 ICUs, which occurred at both hospitals, presented challenges and opportunities for proning. Before COVID-19, some of these ICUs were nonmedical ICUs or intermediate-care units (IMCs). In these units, rapidly training the staff, who often had limited experience caring for patients with ARDS, was a challenge. However, this same lack of experience could be advantageous when introducing new practices, with one participant noting that the team in an IMC repurposed as an ICU was a “blank slate.” Furthermore, the teams in dedicated COVID-19 units rapidly developed syndrome-specific expertise and this facilitated the confidence and expertise to then support proning in less experienced units:
(MD02) A sick patient came [to the cardiovascular surgical ICU (CVSICU)] . . . and they were going to consider cannulation [ECMO], but they wanted to optimize sedation, the vent, and then prone. The [COVID-19 ICU] charge nurse went . . . and helped them [prone]. I think there was a little pride in that, right? . . . This IMC turned renegade ICU . . . going down to the CVSICU to be like, “This is our expertise.”
In a larger contextual frame, COVID-19 as a novel disease influenced teams to adopt new approaches for patients with ARDS. This was stimulated in part by initially limited therapeutic options for COVID-19, reports from other ICUs experiencing early COVID surges, and other COVID-19– related changes to the clinical environment:
(MD03) COVID shows up, and now everything’s different, right? Like, “New walls, new doctors, new equipment, new gear, new hours.” . . . I think just sort of being like, “Actually, this has been the way we should be doing things.”
CFIR: Implementation Processes
Implementation processes that supported prone positioning for COVID-19 ARDS are outlined in Table 5 and comprise 1) staff leadership and training, 2) the use of a proning team, 3) guidelines and proning policies, 4) access to training materials, and 5) dissemination of best practices. Staff training was led by experienced nurses who provided bedside education for more junior nurses and overall championed the expansion of prone positioning. Although this was supplemented by some proning-specific educational initiatives (e.g., lectures, skills day), on-the-job learning was viewed as the most important training aspect.
Table 5.
Consolidated Framework for Implementation Research implementation strategies: implementation processes affecting proning in coronavirus disease acute respiratory distress syndrome
| Study Theme (Definition) and Subthemes | (Provider Type and Number) Supporting Quotation |
|---|---|
| Approach to staff training (processes to train staff on proning effectively) | |
| Leadership and education from experienced nurses | (RN03) We’ve done a lot of surveys with our staff on what they found most helpful and what they didn’t find helpful. So, providing them journal articles, providing them policies to review . . . didn’t learn that way. . . . I think that the best way that they learned, and they were able to absorb the most information, was repeated exposure to the same thing. And we also did one-to-one nursing. . . . I think the best thing that worked for them was treating it like a preceptorship, like when they’re new nurses, so. |
| Proning-specific educational initiatives | (MD03) So a lot of informal—talking about it on rounds. And then for the nursing staff, we did a brief educational, like five minutes at the nurse staff meeting. We created a little document to distribute to the nursing staff that just sort of had the basic parameters of PROSEVA. |
| On-the-job learning | (RN11) The physician can write the order to prone, but they don’t have any experience in any of this. So, there’s really no one to guide us [with carrying out proning]. It’s a learn as you go process. |
| Proning team (team composed of dedicated nurses (initially) and outpatient PTs redeployed to inpatient setting to assist with proning) | |
| Availability of prone team, particularly helpful in high-volume periods | (RT02) It [the prone team] was definitely one of the best things that we could’ve implemented during the period of the pandemic because it’s so difficult when you have an ICU full of 15 intubated patients and maybe 7 or 8 of the 15 are proned. It’s so difficult to coordinate with all of the nurses that you need, the techs that you need, as well as the RT that you need to be able to prone, supinate, do head turns for these patients. So having a dedicated PT, [or] having two dedicated PTs . . . on the prone team [available to help], that eliminated taking away three people . . . [from] their patient that are potentially not doing well. |
| Helped less experienced units learn proning best practices | (PT04) But [in] the units that had no experience, they were looking to us from day one because they didn’t know at all [how to prone]. |
| Innovative positioning to decrease musculoskeletal injury | (PT02) As we went along, brachial plexopathies and pressure injuries, but also shoulder subluxations were kind of the main things to watch out for. And so, I’ve seen enough bodies moving that that kind of comes intuitively to me, which I had noticed for the nurses, it didn’t. They were like, “Can the arm move like that?” And I was like, “Yeah.” Or they’d be super comfortable with the position that the patient was in, and I’d be like, “No. . . . that’s a up to five-year recovery.” . . . So, it’s amazing that the person is alive and be totally worth it, but if we could prevent five years of disability in someone’s arm just by supporting their shoulder while we move it, that would be pretty cool. |
| Guidelines, policies and procedures (the role of these documents in proning implementation) | |
| Specific COVID-19 critical care guidelines were helpful |
(MD10) I think, in the MICU, what drove [the increased use in proning] was that in the ramp up to COVID we tried to come up with some—not knowing very much—we came up with some guidelines saying, look, we’re operating under the assumption that this is ARDS. We should treat it like ARDS [including proning]. (RN02) I think the recommendation of proning in the COVID patients helped sort of stir the work that was probably needed to develop the new method [for proning] . . . stirred the work to kind of look at how to make this intervention easier to implement. |
| Guidance for the mechanical aspects of proning | (RN08) Thankfully, our nurse educator . . . did a whole proning policy, which gave us all the guidance that we needed on how to follow the correct steps to do the actual pronation itself. And that was almost always printed out and reviewed if anybody was ever unsure. |
| Protocols may be too proscribed and did not evolve with changes in proning practice | (RN10) It [proning protocol] was helpful, but I hate to insert it into this conversation, only because I feel like it’s now becoming a nuisance for me, only because it was written for ARDS patients long before COVID was a thing. So, the thing I said about the time frame [of when to prone and supinate patients] with the 16 h and the 4 h, of course, that doesn’t apply. |
| Providing access to training materials | |
| Prone positioning instructional video | (APP04) I felt like a video was also something that was really helpful. So, we made a video on the actual proning procedure, and flipping, and supinating, and all of that. We made a video from the PT perspective on shoulder subluxation and how to prevent that. And then, we made another video from the wound care perspective on how to prevent facial injuries. And I think it just adapted to everybody’s learning style, whether you were somebody who liked to read something, or whether you needed to actually see it be done, whether you needed to hear it, you could just listen to the video. |
| COVID-19 information portal | (RN02) Another tool was the educational video that we received, and then the COVID-19 resource portal that had a ton of information and other literature that just—if a nurse wanted to learn, “Is there recommendations for tube feeding?” etc. |
| Dissemination of best practices (process for distributing information on proning best practices) | |
| Informal dissemination of information | (RN04) I was trying to do a lot of education with skin and wound and preventing pressure ulcers. . . . But there’s no real way to spread that information to everybody. So, it was literally word of mouth, like whenever you happened to go turn somebody, you would say it to those three people. And then you would go turn somebody else and say it to those three people. . . . I mean, we were getting inundated with so many e-mails, and it’s not necessarily applicable to everybody. [In] a couple of units, we would institute pressure ulcer prevention bulletin boards, but I mean, who knows who’s really stopping to look at that and read that when you’re busy with your patients. |
Definition of abbreviations: APP = advanced practice provider; ARDS = acute respiratory distress syndrome; COVID = coronavirus disease; ICU = intensive care unit; MD = medical doctor; MICU = medical intensive care unit; PROSEVA = Proning Severe ARDS Patients; PT = physical therapist; RN = registered nurse; RT = respiratory therapist.
A proning team was created at the larger academic hospital early in the pandemic and was initially composed of senior nurses and subsequently staffed by redeployed outpatient PTs. This team was crucial during COVID-19 surges and early in the pandemic, when they helped teach less experienced units to prone safely. In addition, the PTs on the proning team developed innovative positioning adjustments to decrease risk of musculoskeletal injuries in proned patients (i.e., brachial plexopathies, shoulder subluxations). Using these protective positions may have increased provider comfort, particularly as these risks of proning became apparent:
(RT02) We needed a little bit proper training on how to position the arms because we ended up seeing a lot of patients who had injuries with moving their arms or their shoulders around. And having a PT—that was helpful . . . that’s their bread and butter.
Several implementation processes involved proning policies, guidelines, and the tools needed to disseminate them. Early in the pandemic, Johns Hopkins Medicine created institution-specific guidelines for the care of critically ill patients with COVID-19 (including a recommendation for proning). Participants viewed this locally informed guidance as instrumental for implementing prone positioning. Although existing protocols on the mechanical aspects of proning were helpful, they did not always reflect current proning practice (e.g., longer proning sessions), and this led to some frustration with their use. To disseminate guidelines, protocols, and other proning-specific educational materials, a centralized information portal was created to reach clinicians across both hospitals. In addition, many participants discussed that best practices were also disseminated informally via staff interactions during routine bedside care.
Discussion
Greater use of prone positioning in mechanically ventilated patients with COVID-19 ARDS occurred in the setting of shifting individual and ICU team approaches to proning. This was supported by deliberate ICU and hospital features, including the availability of basic but important equipment, centralized access to institution-specific guidelines and educational materials, and the formation of a dedicated proning team. Leadership and bedside education from experienced nurses were critical for staff training and dissemination of best practices.
Our findings align with important principles from other studies describing the implementation of complex ICU interventions (11, 32–34). In an implementation mapping study of prone positioning conducted just before the COVID-19 pandemic, implementation strategies for increasing proning use were derived from qualitative interviews with ICU clinicians and leaders (11). Several of their implementation recommendations are consistent with processes that were effective in our setting. This includes leadership and staff education from local experts (in this case senior nurses), the availability of locally developed proning guidelines and protocols, and the use of proning teams. In addition, our participants noted that although guidelines and protocols could be helpful, they did not evolve as proning practice changed, highlighting a need for flexibility in local protocols. Our study also indicates the importance of ICU team buy-in for implementing an intervention such as proning, which requires input from multiple disciplines (e.g., MDs/APPs to prescribe, RNs/RTs/PTs to carry out safely) (32, 33). Specifically, participants highlighted the leadership of senior nurses in teaching and championing the use of prone positioning, and these leaders were crucial change agents in implementing prone positioning. Finally, the support of hospital administration for forming proning teams, developing systemwide guidelines, and creating centralized access to guidelines and educational resources were important facilitators and highlight the importance of hospital support for facilitating the use of evidence-based interventions (32). The consistency of these implementation processes across studies reinforces their importance in implementing evidence-based critical care.
Our findings suggest that several previously noted barriers to proning were partially overcome in the setting of COVID-19 ARDS. For one, individuals and team views toward proning evolved to seeing proning as early standard therapy for COVID-19 ARDS, rather than salvage therapy for patients with refractory hypoxemia (7, 11). This evolution was stimulated in part by repeated exposure to proning, which reinforced beliefs in efficacy, and by clinicians seeing that adverse effects could be mitigated in part by innovations in positioning (e.g., PTs’ position techniques to decrease shoulder subluxations) and improved wound care. Second, patient factors such as obesity and relative hemodynamic instability, which have been deterrents to proning use (6, 11), were less of a barrier as teams gained comfort with using proning in these patient populations. Finally, in contrast to concerns about the resource and labor-intensive nature of prone positioning (11, 12), our participants reported that proning could be accomplished without specialized proning-specific equipment and by small teams of appropriately trained staff members.
There are few published reports of interventions designed to increase the use of evidence-based ARDS interventions, highlighting the need for effective implementation strategies (35). The successful expansion of proning in ARDS from COVID-19 can serve as a model for designing such interventions. Our findings suggest several features that could be effective in implementation interventions for proning and other evidence-based interventions. Outside of the pandemic context, and in non–COVID-19 ARDS, there is a need for processes to maintain ICU clinician and team comfort with interventions that may not be as frequently indicated but still appropriate in the right clinical settings. Tools to trigger the use of indicated therapies when the incidence of severe ARDS is lower could include spaced learning (36) and simulation-based practice (37). These strategies may reproduce some of the experience of repetitive exposure to ARDS (as experienced during the COVID-19 pandemic). In relation to other evidence-based ARDS practices, proning is unique in that the initial feedback to providers who prone a patient is often positive, as oxygenation can immediately improve (38). In contrast, the immediate feedback to bedside clinicians who initiate low tidal volume ventilation may be negative (patient discomfort and/or tachypnea), and the benefits may be realized only days/weeks/months after initiation (39). These intervention–patient–provider interactions may influence the tailoring of implementation strategies to increase adoption and penetration of critical care interventions.
Our findings also show the importance of interprofessional staff members in fostering on-the-job training for proning and other multidisciplinary therapies (33). Our participants pointed to different needs and experiences of prescribers (MDs, APPs who may “order” proning) and those who carry the procedure out (e.g., RNs, RTs, PTs). These differences included different perceptions of the workload of caring for proned patients and different educational needs (i.e., guidelines for MDs/APPs and protocols/on-the-job learning for RNs/RTs/PTs). At the same time, team agreement was a key proning facilitator. Therefore, resolving differences of opinions and approaches to a therapy within ICU teams is important for successful implementation of evidence-based therapies.
Strengths and limitations
There are several limitations to this study. First, participants were recruited from three ICUs across two hospitals, and these findings may not transfer to other settings. In addition, these were urban hospitals from a well-resourced university-based health system, and their proning experience may not reflect implementation challenges in other settings (e.g., community or rural sites). Second, member checking, a method of using participant feedback on study results to explore the credibility of findings, was not used. However, our study team included investigators who were clinically active in these ICUs (C.H.H., M.E.C., B.S., and D.N.H.), and their input on thematic analysis adds to the credibility of our findings. Third, although we had multiple ICU stakeholders participate, resident MDs were not included, and as noted, residents do play a role in determining initial therapies for patients with ARDS. However, the time spent by residents in our ICUs varies widely, and our goal was to interview clinicians with significant sustained ICU experience. Finally, our study primarily reflects the approach of individuals and teams to proning in mechanically ventilated patients with COVID-19 ARDS. Whether the same practice and implementation changes occurred in non–COVID-19 ARDS treated during the COVID-19 pandemic is not known.
Conclusions
Greater use of proning in patients with ARDS from COVID-19 was stimulated by changing clinician views and ICU team cultures and was supported by both deliberate and informal processes for training and dissemination of information. Evaluating how these features may be replicated in nonpandemic settings and among patients with non–COVID-19 ARDS could improve the implementation of proning and other evidence-based critical care interventions.
Footnotes
Supported by National Heart, Lung, and Blood Institute grants F32HL160039 (C.H.H.) and T32HL007534 (C.H.H., M.E.C., and B.S.).
Author Contributions: Conception and design: C.H.H., M.P.K., D.N.H., and M.N.E. Acquisition of data: C.H.H. and M.N.E. Analysis and interpretation of data: C.H.H., M.E.C., B.S., M.P.K., D.N.H., and M.N.E. Drafting or revising of the manuscript: C.H.H., M.E.C., B.S., M.P.K., D.N.H., and M.N.E. Final approval of manuscript: C.H.H., M.E.C., B.S., M.P.K., D.N.H., and M.N.E.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Guérin C, Reignier J, Richard J-C, Beuret P, Gacouin A, Boulain T, et al. PROSEVA Study Group Prone positioning in severe acute respiratory distress syndrome. N Engl J Med . 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 2. Munshi L, Del Sorbo L, Adhikari NKJ, Hodgson CL, Wunsch H, Meade MO, et al. Prone position for acute respiratory distress syndrome: a systematic review and meta-analysis. Ann Am Thorac Soc . 2017;14:S280–S288. doi: 10.1513/AnnalsATS.201704-343OT. [DOI] [PubMed] [Google Scholar]
- 3. Sud S, Friedrich JO, Adhikari NKJ, Fan E, Ferguson ND, Guyatt G, et al. Comparative effectiveness of protective ventilation strategies for moderate and severe acute respiratory distress syndrome: a network meta-analysis. Am J Respir Crit Care Med . 2021;203:1366–1377. doi: 10.1164/rccm.202008-3039OC. [DOI] [PubMed] [Google Scholar]
- 4. Fan E, Del Sorbo L, Goligher EC, Hodgson CL, Munshi L, Walkey AJ, et al. American Thoracic Society, European Society of Intensive Care Medicine, and Society of Critical Care Medicine An official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine clinical practice guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am J Respir Crit Care Med . 2017;195:1253–1263. doi: 10.1164/rccm.201703-0548ST. [DOI] [PubMed] [Google Scholar]
- 5. Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. LUNG SAFE Investigators ESICM Trials Group. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA . 2016;315:788–800. doi: 10.1001/jama.2016.0291. [DOI] [PubMed] [Google Scholar]
- 6. Guérin C, Beuret P, Constantin JM, Bellani G, Garcia-Olivares P, Roca O, et al. Investigators of the APRONET Study Group, the REVA Network, the Réseau Recherche de la Société Française d’Anesthésie-Réanimation (SFAR-Recherche) and the ESICM Trials Group A prospective international observational prevalence study on prone positioning of ARDS patients: the APRONET (ARDS Prone Position Network) study. Intensive Care Med . 2018;44:22–37. doi: 10.1007/s00134-017-4996-5. [DOI] [PubMed] [Google Scholar]
- 7. Duggal A, Rezoagli E, Pham T, McNicholas BA, Fan E, Bellani G, et al. LUNG SAFE Investigators and the ESICM Trials Group Patterns of use of adjunctive therapies in patients with early moderate to severe ards: insights from the LUNG SAFE study. Chest . 2020;157:1497–1505. doi: 10.1016/j.chest.2020.01.041. [DOI] [PubMed] [Google Scholar]
- 8. Duan EH, Adhikari NKJ, D’Aragon F, Cook DJ, Mehta S, Alhazzani W, et al. Canadian Critical Care Trials Group Management of acute respiratory distress syndrome and refractory hypoxemia: a multicenter observational study. Ann Am Thorac Soc . 2017;14:1818–1826. doi: 10.1513/AnnalsATS.201612-1042OC. [DOI] [PubMed] [Google Scholar]
- 9. Qadir N, Bartz RR, Cooter ML, Hough CL, Lanspa MJ, Banner-Goodspeed VM, et al. Severe ARDS: Generating Evidence (SAGE) Study Investigators Society of Critical Care Medicine’s Discovery Network. Variation in early management practices in moderate-to-severe ARDS in the United States: the Severe ARDS: Generating Evidence Study. Chest . 2021;160:1304–1315. doi: 10.1016/j.chest.2021.05.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sjoding MW. Translating evidence into practice in acute respiratory distress syndrome: teamwork, clinical decision support, and behavioral economic interventions. Curr Opin Crit Care . 2017;23:406–411. doi: 10.1097/MCC.0000000000000437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Klaiman T, Silvestri JA, Srinivasan T, Szymanski S, Tran T, Oredeko F, et al. Improving prone positioning for severe ARDS during the COVID-19 pandemic: an implementation mapping approach. Ann Am Thorac Soc . 2021;18:300–307. doi: 10.1513/AnnalsATS.202005-571OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Law AC, Forbath N, O’Donoghue S, Stevens JP, Walkey AJ. Hospital-level availability of prone positioning in Massachusetts ICUs. Am J Respir Crit Care Med . 2020;201:1006–1008. doi: 10.1164/rccm.201910-2097LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Li X, Scales DC, Kavanagh BP. Unproven and expensive before proven and cheap: extracorporeal membrane oxygenation versus prone position in acute respiratory distress syndrome. Am J Respir Crit Care Med . 2018;197:991–993. doi: 10.1164/rccm.201711-2216CP. [DOI] [PubMed] [Google Scholar]
- 14. Botta M, Tsonas AM, Pillay J, Boers LS, Algera AG, Bos LDJ, et al. PRoVENT-COVID Collaborative Group Ventilation management and clinical outcomes in invasively ventilated patients with COVID-19 (PRoVENT-COVID): a national, multicentre, observational cohort study. Lancet Respir Med . 2021;9:139–148. doi: 10.1016/S2213-2600(20)30459-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Estenssoro E, Loudet CI, Ríos FG, Kanoore Edul VS, Plotnikow G, Andrian M, et al. SATI-COVID-19 Study Group Clinical characteristics and outcomes of invasively ventilated patients with COVID-19 in Argentina (SATICOVID): a prospective, multicentre cohort study. Lancet Respir Med . 2021;9:989–998. doi: 10.1016/S2213-2600(21)00229-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Johnson SW, Garcia MA, Sisson EKQ, Sheldrick CR, Kumar VK, Boman K, et al. Hospital variation in management and outcomes of acute respiratory distress syndrome due to COVID-19. Crit Care Explor . 2022;10:e0638. doi: 10.1097/CCE.0000000000000638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Le Terrier C, Sigaud F, Lebbah S, Desmedt L, Hajage D, Guérin C, et al. COVID-ICU Group on behalf of the REVA Network and the COVID-ICU Investigators Early prone positioning in acute respiratory distress syndrome related to COVID-19: a propensity score analysis from the multicentric cohort COVID-ICU network-the ProneCOVID study. Crit Care . 2022;26:71. doi: 10.1186/s13054-022-03949-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hochberg CH, Psoter KJ, Sahetya SK, Nolley EP, Hossen S, Checkley W, et al. Comparing prone positioning use in COVID-19 versus historic acute respiratory distress syndrome. Crit Care Explor . 2022;4:e0695. doi: 10.1097/CCE.0000000000000695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Audhya X, Bosch NA, Stevens JP, Walkey AJ, Law AC. Changes to hospital availability of prone positioning after the COVID-19 pandemic. Ann Am Thorac Soc . doi: 10.1513/AnnalsATS.202201-070RL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gupta S, Hayek SS, Wang W, Chan L, Mathews KS, Melamed ML, et al. STOP-COVID Investigators Factors associated with death in critically ill patients with coronavirus disease 2019 in the US. JAMA Intern Med . 2020;180:1436–1447. doi: 10.1001/jamainternmed.2020.3596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Barr J, Paulson SS, Kamdar B, Ervin JN, Lane-Fall M, Liu V, et al. The coming of age of implementation science and research in critical care medicine. Crit Care Med . 2021;49:1254–1275. doi: 10.1097/CCM.0000000000005131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Taylor SP, Kowalkowski MA, Beidas RS. Where is the implementation science? An opportunity to apply principles during the COVID-19 pandemic. Clin Infect Dis . 2020;71:2993–2995. doi: 10.1093/cid/ciaa622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci . 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Weiss CH, Krishnan JA, Au DH, Bender BG, Carson SS, Cattamanchi A, et al. ATS Ad Hoc Committee on Implementation Science An Official American Thoracic Society research statement: implementation science in pulmonary, critical care, and sleep medicine. Am J Respir Crit Care Med . 2016;194:1015–1025. doi: 10.1164/rccm.201608-1690ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sinuff T, Cook DJ, Giacomini M. How qualitative research can contribute to research in the intensive care unit. J Crit Care . 2007;22:104–111. doi: 10.1016/j.jcrc.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 26. Short B, Parekh M, Ryan P, Chiu M, Fine C, Scala P, et al. Rapid implementation of a mobile prone team during the COVID-19 pandemic. J Crit Care . 2020;60:230–234. doi: 10.1016/j.jcrc.2020.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Tong A, Sainsbury P, Craig J. Consolidated Criteria for Reporting Qualitative Research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care . 2007;19:349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 28. Safaeinili N, Brown-Johnson C, Shaw JG, Mahoney M, Winget M. CFIR simplified: pragmatic application of and adaptations to the Consolidated Framework for Implementation Research (CFIR) for evaluation of a patient-centered care transformation within a learning health system. Learn Health Syst . 2019;4:e10201. doi: 10.1002/lrh2.10201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Creswell JW. Qualitative inquiry and research design: choosing among five approaches. London: Sage; 2007. [Google Scholar]
- 30. Brennan MR, Laconti D, Gilchrist R. Using conformational positioning to reduce hospital-acquired pressure ulcers. J Nurs Care Qual . 2014;29:182–187. doi: 10.1097/NCQ.0b013e3182a79ca9. [DOI] [PubMed] [Google Scholar]
- 31. Morata L, Sole ML, Guido-Sanz F, Ogilvie C, Rich R. Manual vs automatic prone positioning and patient outcomes in acute respiratory distress syndrome. Am J Crit Care . 2021;30:104–112. doi: 10.4037/ajcc2021674. [DOI] [PubMed] [Google Scholar]
- 32. Eakin MN, Ugbah L, Arnautovic T, Parker AM, Needham DM. Implementing and sustaining an early rehabilitation program in a medical intensive care unit: a qualitative analysis. J Crit Care . 2015;30:698–704. doi: 10.1016/j.jcrc.2015.03.019. [DOI] [PubMed] [Google Scholar]
- 33. Rak KJ, Kahn JM, Linstrum K, Caplan EA, Argote L, Barnes B, et al. Enhancing implementation of complex critical care interventions through interprofessional education. ATS Sch . 2021;2:370–385. doi: 10.34197/ats-scholar.2020-0169OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Costa DK, White MR, Ginier E, Manojlovich M, Govindan S, Iwashyna TJ, et al. Identifying barriers to delivering the awakening and breathing coordination, delirium, and early exercise/mobility bundle to minimize adverse outcomes for mechanically ventilated patients: a systematic review. Chest . 2017;152:304–311. doi: 10.1016/j.chest.2017.03.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Giovanni SP, Jennerich AL, Steel TL, Lokhandwala S, Alhazzani W, Weiss CH, et al. Promoting evidence-based practice in acute respiratory distress syndrome: a systematic review. Crit Care Explor . 2021;3:e0391. doi: 10.1097/CCE.0000000000000391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Versteeg M, Hendriks RA, Thomas A, Ommering BWC, Steendijk P. Conceptualising spaced learning in health professions education: a scoping review. Med Educ . 2020;54:205–216. doi: 10.1111/medu.14025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Richards JB, Claar D, McCurdy MT, Shah NG, McSparron JI, Seam N. Impact of risk and volume on procedural training of pulmonary and critical care fellows. ATS Sch . 2021;2:212–223. doi: 10.34197/ats-scholar.2020-0110OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Scaramuzzo G, Gamberini L, Tonetti T, Zani G, Ottaviani I, Mazzoli CA, et al. ICU-RER COVID-19 Collaboration Sustained oxygenation improvement after first prone positioning is associated with liberation from mechanical ventilation and mortality in critically ill COVID-19 patients: a cohort study. Ann Intensive Care . 2021;11:63. doi: 10.1186/s13613-021-00853-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rubenfeld GD, Cooper C, Carter G, Thompson BT, Hudson LD. Barriers to providing lung-protective ventilation to patients with acute lung injury. Crit Care Med . 2004;32:1289–1293. doi: 10.1097/01.ccm.0000127266.39560.96. [DOI] [PubMed] [Google Scholar]