Emergency endotracheal intubation is a high-risk procedure commonly performed in hospitalized patients who are suffering from critical illness. Standardized metrics are needed to allow for continuous quality improvement and serve as outcome measures for emergency airway research. Ideally, the core outcome metric used to evaluate emergency endotracheal intubation research and quality improvement would be easily measurable, patient centered, and modifiable by interventions under study. In this Viewpoint, we describe the first-pass success rate, the metric most frequently used for assessing emergency endotracheal intubation, and highlight both the strengths and weaknesses of this outcome. We further identify alternative candidate outcomes for future research and quality improvement initiatives with respect to emergency endotracheal intubation and characterize an important gap in critical care airway research.
The term first-pass success is traditionally defined as successful intubation after the first insertion of the laryngoscope blade into the mouth (1). Given the colloquial nature of the term first-pass success and the lack of distinctions within the term regarding what a “pass” is and what “success” refers to, we will use the alternative term “intubation on first attempt” for the remainder of this manuscript. Whether the airway management community should consider moving away from the term first-pass success and toward a more descriptive term is a subject that warrants further discussion.
The idea of measuring intubation on first attempt was initially described in 1984 by prehospital personnel (2). The sentinel retrospective study that linked intubation on first attempt rates to clinical outcomes for critically ill patients was reported by anesthesia providers intubating patients outside the operating room (1). Since the publication of these data, intubation on first attempt has been used as an outcome measure for controlled laryngoscopy in the operating room and during the emergency airway management of critically ill patients (3–6). The rationale behind the use of intubation on first attempt as an outcome measure has been reinforced over time by the demonstration that complications and mortality escalate with increasing numbers of procedural attempts across a variety of clinical environments (6, 7). Given the robustness of this correlation, intubation on first attempt has been widely used as the primary outcome for studies determining best practice during emergency endotracheal intubations (3, 4, 8–10).
Despite its widespread adoption, intubation on first attempt has several limitations that should be acknowledged. First, the traditionally used definition of intubation on first attempt as provided above does not fully encompass the entirety of the procedure, which includes both laryngoscopy (visualization of glottis) and intubation (successful insertion of the endotracheal tube into the trachea). Despite successful visualization of the glottis, repeated attempts at insertion of an endotracheal tube may increase the risk of complications, including airway trauma and propensity for prolonged intubation with physiologic consequences.
To mitigate this potential shortcoming, several recent trials have defined intubation on first attempt to include both a single attempt at laryngoscopy and a single attempt at insertion of an endotracheal tube (5, 11). This latter definition is especially pertinent given the increasing use of hyperangulated video laryngoscopes, which allow for improved laryngeal visualization despite widely described challenges during endotracheal tube delivery (4, 12). The reporting of both the traditional definition and the augmented definition of first-pass success to include tube delivery on the first attempt may serve to encompass this new perspective prioritizing the documentation of early tube delivery as well as facilitate comparison between emerging and prior data reporting the traditional definition.
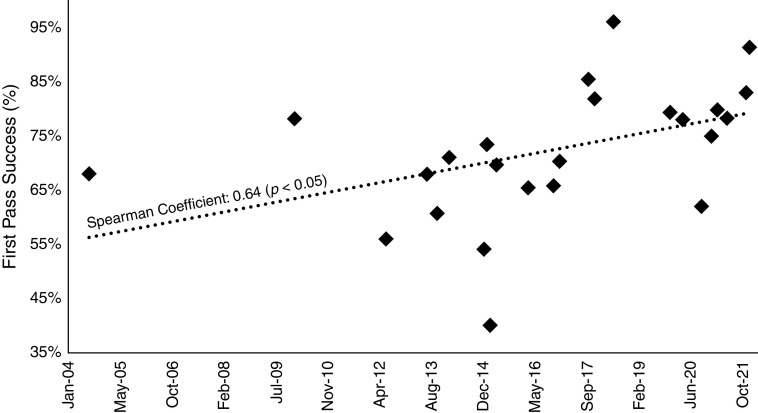
Furthermore, over the past decade the success rate for intubations on first attempt outside of the operating room or emergency department has improved. On examination of the reference groups of retrospective and prospective studies, intubation on first attempt ranged from 54% to 78% in studies before 2015 and then increased to a range of 75–83% afterward (Figure 1). In the two most recent high-impact trials, intubation on first attempt was >80% (10, 13). The explanation for this trend toward higher rates of intubation on first attempt is likely a function of increased use of video laryngoscopy, neuromuscular blockade, and airway adjuncts and the adoption of intubation bundles to standardize the approach toward difficult airways (12, 14). As the baseline for intubation on first attempt increases, the proportion of the outcome potentially modifiable through the implementation of novel interventions will shrink. Thus, investigators studying novel airway interventions or approaches are limited in the degree to which they can realistically improve intubation on first attempt. Greater sample sizes will be needed to detect increasingly small and less clinically significant differences.
Figure 1.
First-pass success (%) over time among control or reference groups of studies on patients in intensive care units or medical wards undergoing emergency endotracheal intubation. Retrospective and prospective cohort studies as well as randomized controlled trials were included. Studies were excluded if the target population was patients with cardiac arrest. Trendline was added to demonstrate increasing first-pass success over time period examined. The Spearman correlation coefficient between first-pass success and month of study publication was 0.64 (P < 0.05) (1, 3–5, 7–10, 12–27).
Finally, intubation on first attempt is a purely mechanical outcome measure that does not capture the full complexity of airway management in critically ill patients. Importantly, this outcome does not reflect the physiologically difficult airway, in which the mechanical approach to intubation is straightforward but the respiratory or hemodynamic status of the patient is in peril. If, for example, video laryngoscopy improves first-pass success over direct laryngoscopy, but the intubation time is longer and patients are at higher risk of clinically significant desaturation, then it would be incorrect to conclude the superiority of video laryngoscopy over direct laryngoscopy based on improved rates of intubation on first attempt alone.
Given the above-described limitations, the identification of novel outcomes is crucial for future emergency endotracheal intubation studies. Alternative measures that can be accurately reported and are clinically significant and generalizable across environments are needed. Such alternative proximal outcomes may include peri-intubation hypotension requiring vasopressor support, hypoxemia, witnessed aspiration of gastric contents into the trachea, or cardiac arrest. Some outcome measures, such as vasopressor use for hemodynamic instability, may be extracted from the medical record and are comparable across various settings. Others, such as hypoxemia or aspiration of gastric contents, may be more difficult to standardize. Given the known limitations of self-reported data and the granularity needed for high-quality studies, independent observers (such as those used in the INTUBE study) or members of the airway team not directly involved with the intubation attempt may be necessary for accurate reporting of certain outcomes (15). This may introduce variable complexity with respect to the reporting of outcomes. For example, the observer may be more likely to accurately report lowest oxygen saturation during or after the procedure, whereas the proceduralist would be most likely to be able to estimate if the patient experiences clinically significant aspiration of gastric contents into the airway.
It is important when selecting proximal outcomes for a study to tailor the outcome to the intervention under investigation. An example would be focusing on cardiovascular instability when studying sedatives or periprocedural hypoxemia when examining the clinical approach to apneic oxygenation. A further important consideration in selecting appropriate proximal outcomes is the need to be cautious with the use of dichotomous variables. Many patients undergoing emergent endotracheal intubation may experience a dichotomous proximal outcome (such as the use of vasopressor support) before they are exposed to the intervention being studied. To mitigate this problem, the use of continuous or ordinal outcomes, such as a change in peripheral oxygen saturation from baseline, may be more elucidating.
A further possibility when using proximal events as outcomes is to combine several into a composite outcome, such as that used in the recently published International Observational Study to Understand the Impact and Best Practices of Airway Management in Critically Ill Patients (INTUBE) (15). This could support trial design by increasing statistical power. However, there are important drawbacks to this approach, including the potential for unequal clinical significance of the different components of the outcome and therefore statistical significance being driven by a less-important clinical driver of the overall study result. For instance, clinicians would agree that a witnessed aspiration that did not lead to clinically relevant chemical pneumonitis or intubation of the esophagus that was recognized without subsequent vital sign instability is not as pertinent to patient outcomes as hemodynamic instability requiring vasopressor support.
Long-term outcomes may focus on patient survival and include metrics such as in-hospital mortality, 28-day mortality, or organ failure–free or ventilator-free days. These events are equally important for clinicians as well as patients and families and warrant consideration during larger randomized studies on emergent endotracheal intubation interventions. However, these outcomes have inherent drawbacks because of the multitude of factors that influence long-term outcomes for critically ill patients. Furthermore, it may be postulated that if a long-term outcome is to be impacted by an intervention during emergency intubation, proximal outcomes such as oxygen desaturation would also be impacted. As interventions, including intubation techniques, become more patient specific, there may be further utility for studying longer-term outcomes in depth.
Improving the outcomes of patients undergoing emergency airway management is an imperative for the critical care, emergency medicine, and anesthesia communities. Examination of published data demonstrates that intubation on first attempt has progressively increased over the last two decades. For this and other reasons described above, novel outcome measures are needed to evaluate emergency airway management. These measures should be tailored to the intervention under investigation.
Footnotes
Supported by the National Heart, Lung, and Blood Institute (NHLBI) of the National Insitutes of Health (NIH) (R61 HL162980 [A.M.]).
Author Contributions: All authors contributed to study conception, design, data acquisition, analysis, and preparation of this manuscript.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Mort TC. Emergency tracheal intubation: complications associated with repeated laryngoscopic attempts. Anesth Analg . 2004;99:607–613. doi: 10.1213/01.ANE.0000122825.04923.15. [DOI] [PubMed] [Google Scholar]
- 2. Stewart RD, Paris PM, Winter PM, Pelton GH, Cannon GM. Field endotracheal intubation by paramedical personnel: success rates and complications. Chest . 1984;85:341–345. doi: 10.1378/chest.85.3.341. [DOI] [PubMed] [Google Scholar]
- 3. Janz DR, Semler MW, Lentz RJ, Matthews DT, Assad TR, Norman BC, et al. Facilitating EndotracheaL intubation by Laryngoscopy technique and apneic Oxygenation Within the ICU Investigators and the Pragmatic Critical Care Research Group Randomized trial of video laryngoscopy for endotracheal intubation of critically ill adults. Crit Care Med . 2016;44:1980–1987. doi: 10.1097/CCM.0000000000001841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lascarrou JB, Boisrame-Helms J, Bailly A, Le Thuaut A, Kamel T, Mercier E, et al. Clinical Research in Intensive Care and Sepsis (CRICS) Group Video laryngoscopy vs direct laryngoscopy on successful first-pass orotracheal intubation among ICU patients: a randomized clinical trial. JAMA . 2017;317:483–493. doi: 10.1001/jama.2016.20603. [DOI] [PubMed] [Google Scholar]
- 5. Driver BE, Prekker ME, Klein LR, Reardon RF, Miner JR, Fagerstrom ET, et al. Effect of use of a bougie vs endotracheal tube and stylet on first-attempt intubation success among patients with difficult airways undergoing emergency intubation: a randomized clinical trial. JAMA . 2018;319:2179–2189. doi: 10.1001/jama.2018.6496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sakles JC, Chiu S, Mosier J, Walker C, Stolz U. The importance of first pass success when performing orotracheal intubation in the emergency department. Acad Emerg Med 20132071–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. De Jong A, Rolle A, Pensier J, Capdevila M, Jaber S. First-attempt success is associated with fewer complications related to intubation in the intensive care unit. Intensive Care Med . 2020;46:1278–1280. doi: 10.1007/s00134-020-06041-2. [DOI] [PubMed] [Google Scholar]
- 8. Guihard B, Chollet-Xémard C, Lakhnati P, Vivien B, Broche C, Savary D, et al. Effect of rocuronium vs succinylcholine on endotracheal intubation success rate among patients undergoing out-of-hospital rapid sequence intubation: a randomized clinical trial. JAMA . 2019;322:2303–2312. doi: 10.1001/jama.2019.18254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jaber S, Rollé A, Godet T, Terzi N, Riu B, Asfar P, et al. STYLETO trial group Effect of the use of an endotracheal tube and stylet versus an endotracheal tube alone on first-attempt intubation success: a multicentre, randomised clinical trial in 999 patients. Intensive Care Med . 2021;47:653–664. doi: 10.1007/s00134-021-06417-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Driver BE, Semler MW, Self WH, Ginde AA, Trent SA, Gandotra S, et al. BOUGIE Investigators and the Pragmatic Critical Care Research Group Effect of use of a bougie vs endotracheal tube with stylet on successful intubation on the first attempt among critically ill patients undergoing tracheal intubation: a randomized clinical trial. JAMA . 2021;326:2488–2497. doi: 10.1001/jama.2021.22002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Russell DW, Casey JD, Gibbs KW, Ghamande S, Dargin JM, Vonderhaar DJ, et al. PREPARE II Investigators and the Pragmatic Critical Care Research Group Effect of fluid bolus administration on cardiovascular collapse among critically ill patients undergoing tracheal intubation: a randomized clinical trial. JAMA . 2022;328:270–279. doi: 10.1001/jama.2022.9792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hypes CD, Stolz U, Sakles JC, Joshi RR, Natt B, Malo J, et al. Video laryngoscopy improves odds of first-attempt success at intubation in the intensive care unit: a propensity-matched analysis. Ann Am Thorac Soc . 2016;13:382–390. doi: 10.1513/AnnalsATS.201508-505OC. [DOI] [PubMed] [Google Scholar]
- 13. Matchett G, Gasanova I, Riccio CA, Nasir D, Sunna MC, Bravenec BJ, et al. EvK Clinical Trial Collaborators Etomidate versus ketamine for emergency endotracheal intubation: a randomized clinical trial. Intensive Care Med . 2022;48:78–91. doi: 10.1007/s00134-021-06577-x. [DOI] [PubMed] [Google Scholar]
- 14. Mosier JM, Sakles JC, Stolz U, Hypes CD, Chopra H, Malo J, et al. Neuromuscular blockade improves first-attempt success for intubation in the intensive care unit: a propensity matched analysis. Ann Am Thorac Soc . 2015;12:734–741. doi: 10.1513/AnnalsATS.201411-517OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Russotto V, Myatra SN, Laffey JG, Tassistro E, Antolini L, Bauer P, et al. INTUBE Study Investigators Intubation practices and adverse peri-intubation events in critically ill patients from 29 countries. JAMA . 2021;325:1164–1172. doi: 10.1001/jama.2021.1727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Amalric M, Larcher R, Brunot V, Garnier F, De Jong A, Rigollet VM, et al. Impact of videolaryngoscopy expertise on first-attempt intubation success in critically Ill patients. Crit Care Med . 2020;48:e889–e896. doi: 10.1097/CCM.0000000000004497. [DOI] [PubMed] [Google Scholar]
- 17. Diaz-Guzman E, Mireles-Cabodevila E, Heresi GA, Bauer SR, Arroliga AC. A comparison of methohexital versus etomidate for endotracheal intubation of critically ill patients. Am J Crit Care . 2010;19:48–54. doi: 10.4037/ajcc2010562. [DOI] [PubMed] [Google Scholar]
- 18. Fein DG, Mastroianni F, Murphy CG, Aboodi M, Malik R, Emami N, et al. Impact of a critical care specialist intervention on first pass success for emergency airway management outside the ICU. J Intensive Care Med . 2021;36:80–88. doi: 10.1177/0885066619886816. [DOI] [PubMed] [Google Scholar]
- 19. Hypes C, Sakles J, Joshi R, Greenberg J, Natt B, Malo J, et al. Failure to achieve first attempt success at intubation using video laryngoscopy is associated with increased complications. Intern Emerg Med . 2017;12:1235–1243. doi: 10.1007/s11739-016-1549-9. [DOI] [PubMed] [Google Scholar]
- 20. Koenig SJ, Lakticova V, Narasimhan M, Doelken P, Mayo PH. Safety of propofol as an induction agent for urgent endotracheal intubation in the medical intensive care unit. J Intensive Care Med . 2015;30:499–504. doi: 10.1177/0885066614523100. [DOI] [PubMed] [Google Scholar]
- 21. Kory P, Guevarra K, Mathew JP, Hegde A, Mayo PH. The impact of video laryngoscopy use during urgent endotracheal intubation in the critically ill. Anesth Analg . 2013;117:144–149. doi: 10.1213/ANE.0b013e3182917f2a. [DOI] [PubMed] [Google Scholar]
- 22. Lakticova V, Koenig SJ, Narasimhan M, Mayo PH. Video laryngoscopy is associated with increased first pass success and decreased rate of esophageal intubations during urgent endotracheal intubation in a medical intensive care unit when compared to direct laryngoscopy. J Intensive Care Med . 2015;30:44–48. doi: 10.1177/0885066613492641. [DOI] [PubMed] [Google Scholar]
- 23. Mosier JM, Whitmore SP, Bloom JW, Snyder LS, Graham LA, Carr GE, et al. Video laryngoscopy improves intubation success and reduces esophageal intubations compared to direct laryngoscopy in the medical intensive care unit. Crit Care . 2013;17:R237. doi: 10.1186/cc13061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nauka PC, Chen JT, Shiloh AL, Eisen LA, Fein DG. Practice, outcomes, and complications of emergent endotracheal intubation by critical care practitioners during the COVID-19 pandemic. Chest . 2021;160:2112–2122. doi: 10.1016/j.chest.2021.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Noppens RR, Geimer S, Eisel N, David M, Piepho T. Endotracheal intubation using the C-MAC® video laryngoscope or the Macintosh laryngoscope: a prospective, comparative study in the ICU. Crit Care . 2012;16:R103. doi: 10.1186/cc11384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Semler MW, Janz DR, Russell DW, Casey JD, Lentz RJ, Zouk AN, et al. A multicenter, randomized trial of ramped position vs sniffing position during endotracheal intubation of critically ill adults. Chest . 2017;152:712–722. doi: 10.1016/j.chest.2017.03.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Silverberg MJ, Li N, Acquah SO, Kory PD. Comparison of video laryngoscopy versus direct laryngoscopy during urgent endotracheal intubation: a randomized controlled trial. Crit Care Med . 2015;43:636–641. doi: 10.1097/CCM.0000000000000751. [DOI] [PubMed] [Google Scholar]