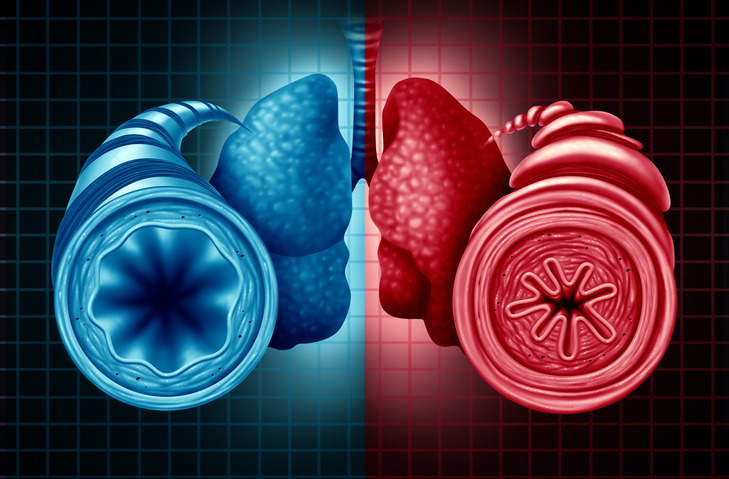
Primary ciliary dyskinesia (PCD) is a multiorgan disease with symptoms related to ineffective or absent beating of motile cilia in different body systems (1). It typically presents early in life with unexplained respiratory distress in the first 24 hours after birth; other cardinal symptoms include chronic productive cough and persistent rhinosinusitis, both usually beginning during infancy (1). Lung disease in people with PCD is characterized by impaired mucociliary clearance, recurrent bacterial infection, and pulmonary exacerbations resulting in progressive obstructive lung disease and bronchiectasis (1, 2).
Neutrophil-dominated inflammation of the airways with elevated levels of neutrophil chemoattractants is well documented in PCD (3–5). Airway epithelial cells respond to inhaled bacteria by producing proinflammatory cytokines to recruit neutrophils and other immune cells to the site of infection (6). The antibacterial response of neutrophils is essential to contain infection and includes phagocytosis, neutrophil extracellular trap formation, and the release of reactive oxygen species and proteases (7). In healthy subjects, the inflammatory response is usually restrained and resolved by antiinflammatory cytokines, but it tends to persist in chronic airway diseases, including PCD and cystic fibrosis (CF) (3). There is also evidence to suggest that abnormal mucus clearance can initiate and potentially maintain airway inflammation independent of infection (8). The link between inflammation and the subsequent course of lung disease has been studied extensively in CF (9, 10), but data are currently lacking for PCD.
In this issue of AnnalsATS, Sagel and colleagues (pp. 67–74) present the findings of the first multicenter observational study on airway inflammation in pediatric patients with PCD (11). Sputum inflammatory markers such as neutrophil elastase (NE), interleukin (IL)-1β, IL-8, and tumor necrosis factor-α concentrations correlated positively with abnormal computed tomography findings and negatively with lung function (11). No significant difference was found between the different groups of ciliary defects, but sputum NE, IL-1β, and tumor necrosis factor-α concentrations were higher in those with positive sputum cultures for common bacterial pathogens.
The finding of persistent neutrophilic inflammation in PCD is consistent with previous single-center studies that evaluated differences in airway inflammation between patients with PCD and patients with CF. Bush and colleagues demonstrated that IL-8 sputum concentrations are higher in PCD than CF, although some of the measurements were performed during pulmonary exacerbations (5). We had previously assessed airway inflammation in a small group of patients with PCD at the time of clinical stability, during pulmonary exacerbations, and after treatment in comparison with patients with CF infected with similar bacterial pathogens (4). Sputum neutrophil counts were elevated in patients with stable PCD, and, at the time of exacerbation, absolute neutrophil counts were significantly higher in PCD than in CF, even though bacterial density was higher in the CF group. Markers of airway inflammation improved with treatment in both groups, but a significant decrease in NE activity after the antibiotic course was only seen in patients with PCD. Therefore, although both diseases are characterized by neutrophilic inflammation, differences exist, especially during pulmonary exacerbation and in the response to antibiotic treatment, which need to be explored further to better understand the specifics of airway inflammation in both diseases.
Higher sputum neutrophil counts in patients have previously been linked to clinical severity, as reflected by increased cough frequency (12), but the study by Sagel and colleagues is the first to demonstrate that measurements of airway inflammation are associated with impaired lung function and structural damage. These findings show a linkage to disease progression and could serve as possible markers for disease trajectories and severity. Although the findings reported by Sagel and colleagues do not necessarily prove causation, such measurements may help to further our understanding of how lung damage occurs in PCD. Longitudinal studies are needed to better delineate the predictive role of biomarkers of airway inflammation for the subsequent course of lung disease.
Genotype–phenotype relationships in PCD have emerged over recent years, linking different genetic variants and ultrastructural defects to disease severity (13). Sagel and colleagues have assessed the airway inflammatory response by comparing two main groups divided on the basis of their ciliary defect: the outer dynein arm defect group and the inner dynein arm defect and microtubular disorganization group. They did not find significant differences between the two groups regarding the inflammatory response. This may be related to the small number of patients in each group and the fact that other genetic mutations with different electron microscopy findings were underrepresented in this cohort, and it does not preclude the possibility that genotype–phenotype correlations exist if assessed in larger patient populations.
Understanding airway inflammation in PCD lung disease is important because it opens the possibility for targeted therapies addressing specific components of the inflammatory response. Defining specific biomarkers of inflammation could thus play a significant role in the development of antiinflammatory therapies for PCD lung disease. So far, only one interventional study has explored this avenue in PCD. The macrolide azithromycin, in addition to its bacteriostatic effects, has known antiinflammatory properties (14), and a recent multicenter, double-blind, randomized, placebo-controlled trial demonstrated that azithromycin decreased the rate of respiratory exacerbations in patients with PCD (15). Although not systematically assessed in that study, the effect of azithromycin on the inflammatory response has previously been documented in CF, where treatment was associated with a significant reduction in serum inflammatory markers (16). Almost one-fourth of the children in the study by Sagel and colleagues were treated with azithromycin as chronic maintenance therapy, raising the question of whether some of the findings were impacted by azithromycin therapy. Although sputum markers of inflammation offer the possibility to directly assess the inflammatory response in the airways, studies using serum biomarkers could also be pursued to assess the effect of therapies on the inflammatory response.
To summarize, Sagel and colleagues have extended our understanding of airway inflammation in PCD and have provided convincing evidence for a correlation between increased inflammatory markers and structural lung damage as well as decreased lung function. Although these measurements are unlikely to be performed in most clinical settings, inflammatory markers could potentially serve as biomarkers in PCD. These markers may help to assess the efficacy of targeted antiinflammatory therapies in clinical trials. The study by Sagel and colleagues is an important step toward a better understanding of the pathophysiology of PCD along the path to specific therapies that can be used in clinical care.
Footnotes
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Shapiro AJ, Zariwala MA, Ferkol T, Davis SD, Sagel SD, Dell SD, et al. Genetic Disorders of Mucociliary Clearance Consortium Diagnosis, monitoring, and treatment of primary ciliary dyskinesia: PCD Foundation consensus recommendations based on state of the art review. Pediatr Pulmonol . 2016;51:115–132. doi: 10.1002/ppul.23304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ratjen F, Bell SC, Rowe SM, Goss CH, Quittner AL, Bush A. Cystic fibrosis. Nat Rev Dis Primers . 2015;1:15010. doi: 10.1038/nrdp.2015.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cockx M, Gouwy M, Van Damme J, Struyf S. Chemoattractants and cytokines in primary ciliary dyskinesia and cystic fibrosis: key players in chronic respiratory diseases. Cell Mol Immunol . 2018;15:312–323. doi: 10.1038/cmi.2017.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ratjen F, Waters V, Klingel M, McDonald N, Dell S, Leahy TR, et al. Changes in airway inflammation during pulmonary exacerbations in patients with cystic fibrosis and primary ciliary dyskinesia. Eur Respir J . 2016;47:829–836. doi: 10.1183/13993003.01390-2015. [DOI] [PubMed] [Google Scholar]
- 5. Bush A, Payne D, Pike S, Jenkins G, Henke MO, Rubin BK. Mucus properties in children with primary ciliary dyskinesia: comparison with cystic fibrosis. Chest . 2006;129:118–123. doi: 10.1378/chest.129.1.118. [DOI] [PubMed] [Google Scholar]
- 6. Whitsett JA, Alenghat T. Respiratory epithelial cells orchestrate pulmonary innate immunity. Nat Immunol . 2015;16:27–35. doi: 10.1038/ni.3045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mantovani A, Cassatella MA, Costantini C, Jaillon S. Neutrophils in the activation and regulation of innate and adaptive immunity. Nat Rev Immunol . 2011;11:519–531. doi: 10.1038/nri3024. [DOI] [PubMed] [Google Scholar]
- 8. Mall M, Grubb BR, Harkema JR, O’Neal WK, Boucher RC. Increased airway epithelial Na+ absorption produces cystic fibrosis-like lung disease in mice. Nat Med . 2004;10:487–493. doi: 10.1038/nm1028. [DOI] [PubMed] [Google Scholar]
- 9. Sagel SD, Wagner BD, Anthony MM, Emmett P, Zemanick ET. Sputum biomarkers of inflammation and lung function decline in children with cystic fibrosis. Am J Respir Crit Care Med . 2012;186:857–865. doi: 10.1164/rccm.201203-0507OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cantin AM, Hartl D, Konstan MW, Chmiel JF. Inflammation in cystic fibrosis lung disease: pathogenesis and therapy. J Cyst Fibros . 2015;14:419–430. doi: 10.1016/j.jcf.2015.03.003. [DOI] [PubMed] [Google Scholar]
- 11. Sagel SD, Kupfer O, Wagner BD, Davis SD, Dell SD, Ferkol TW, et al. Genetic Disorders of Mucociliary Clearance Consortium Airway inflammation in children with primary ciliary dyskinesia. Ann Am Thorac Soc . 2023;20:67–74. doi: 10.1513/AnnalsATS.202204-314OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zihlif N, Paraskakis E, Lex C, Van de Pohl LA, Bush A. Correlation between cough frequency and airway inflammation in children with primary ciliary dyskinesia. Pediatr Pulmonol . 2005;39:551–557. doi: 10.1002/ppul.20202. [DOI] [PubMed] [Google Scholar]
- 13. Brennan SK, Ferkol TW, Davis SD. Emerging genotype-phenotype relationships in primary ciliary dyskinesia. Int J Mol Sci . 2021;22:8272. doi: 10.3390/ijms22158272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pollock J, Chalmers JD. The immunomodulatory effects of macrolide antibiotics in respiratory disease. Pulm Pharmacol Ther . 2021;71:102095. doi: 10.1016/j.pupt.2021.102095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kobbernagel HE, Buchvald FF, Haarman EG, Casaulta C, Collins SA, Hogg C, et al. Efficacy and safety of azithromycin maintenance therapy in primary ciliary dyskinesia (BESTCILIA): a multicentre, double-blind, randomised, placebo-controlled phase 3 trial. Lancet Respir Med . 2020;8:493–505. doi: 10.1016/S2213-2600(20)30058-8. [DOI] [PubMed] [Google Scholar]
- 16. Ratjen F, Saiman L, Mayer-Hamblett N, Lands LC, Kloster M, Thompson V, et al. Effect of azithromycin on systemic markers of inflammation in patients with cystic fibrosis uninfected with Pseudomonas aeruginosa. Chest . 2012;142:1259–1266. doi: 10.1378/chest.12-0628. [DOI] [PMC free article] [PubMed] [Google Scholar]


