Abstract
The relationship between endocrine disrupting chemical (EDC) exposure and Precocious Puberty (PP) was investigated in this pilot study, involving girls with signs of PP (P) and pre-pubertal girls (C). Risk factors for PP were assessed through questionnaires, while 17β-oestradiol (E2) levels and oestrogenic activity were quantified on sera. The oestrogenic activity, expressed as E2 equivalent concentration (EEQ), was applied as EDC exposure biomarker. Questionnaires showed a low EDC knowledge, a high EDC exposure, and a potential relationship between some habits at risk for EDC exposure and PP. EEQs were similar between C and P; however, they were significantly higher in girls living in an urban environment than in girls living in a rural environment, suggesting a potential higher EDC exposure in cities. The results of this pilot study highlighted the need to raise awareness on EDCs and can be considered a starting point to clarify the relationship between EDC exposure and PP.
Keywords: early puberty, endocrine disruptors, exposure biomarker, MELN gene reporter assay, oestradiol equivalent concentration, urban environment
1. Introduction
Puberty represents an essential step in the dynamic transition from childhood to adulthood that leads to full reproductive capacity. The mechanisms underlying this process have not been fully understood and include genetic, metabolic, environmental, geographic, and nutritional factors. Indeed, it has been reported that puberty can be influenced by adipose tissue, gastrointestinal function, adrenal androgen production, physical, and psychological stress [1,2,3,4,5].
Precocious Puberty (PP) is an early onset of puberty and is defined as the development of secondary sexual characteristics before the age of eight years in girls and nine years in boys. This development is clinically assessed through Tanner Staging, a rating based on visual estimates using a scale from one (no development) to five (adult maturity) [6,7,8].
Although PP can be related to tumours involving the hypothalamic-pituitary-gonadal axis (HPG axis), genetic factors or rare syndromes, most PP cases are idiopathic, so the risk factors influencing the onset of PP in children have not been fully clarified. Environmental factors may play a role in the timing of pubertal development such as general health status, nutrition, environmental conditions, and socioeconomic status [9,10]. Furthermore, recent studies reported a correlation between the amount of body fat and PP [5,11,12,13]. Not only being overweight and/or obese may influence the onset of PP but also diet, since a high-fat and/or high-glycaemic-index diet may induce a low-grade hypothalamic inflammation and subsequent premature activation of the gonadotropin releasing hormone [5]. A shorter duration of breastfeeding has also been correlated with PP and a relationship between breast milk assumption during the neonatal period and prevention of both overweight and PP has been reported [14]. Recently, the review of Spaziani et al. [8] suggested that early or delayed pubertal development could be related to a group of heterogeneous molecules called endocrine disrupting chemicals (EDCs).
EDCs are exogenous substances or mixtures that alter the function of the endocrine system and consequently cause adverse health effects in an organism or its progeny [15]. They interact with the organism through multiple mechanisms such as direct interaction with the hormonal receptors, interference with the post-receptor pathways, and suppression of hormonal synthesis. Regarding their influence on puberty, their androgenic and oestrogenic effects are crucial, as they could cause an interference with the HPG axis [8]. EDCs can have a natural origin, such as sex steroids, phytoestrogens, and mycotoxins, or a synthetic origin, such as the compounds used in manufacturing (e.g., phthalates, phenols, polychlorinated biphenyls, and polycyclic aromatic hydrocarbons), in the pharmaceutical industry (e.g., 17α- ethinyloestradiol and diethylstilbestrol), or in agriculture (pesticides such as DDT, atrazine, and glyphosate). They are widely spread in the environment, since their presence has been reported in aquatic environments [16,17,18,19], in tap water [20], and in indoor and outdoor air [21,22,23,24]. Finally, at low concentrations, they are present in a multitude of everyday products, such as personal care products and cosmetics [25]. Sources of EDC exposure are numerous and very diverse (e.g., air, water, soil, food, everyday products) and humans are exposed to EDCs not only outdoors, but also in living and working environments. Once entered in the body through ingestion, inhalation, or skin contact, EDCs can reach the bloodstream and can be spread throughout the body [15,26]. Therefore, human EDC exposure greatly varies depending on habits, age, living and working environments.
Due to their behaviour and their peculiar metabolic characteristics, children are particularly exposed to EDCs [15,22] and can have higher concentrations of EDCs in their biological matrices than adults. For example, Rose et al. [27] found that polybrominated diphenyl ether levels were 2 to 10 times higher in children than in adults.
Due to multiple chemicals acting as EDCs, the different routes of exposure and the different factors influencing exposure, the assessment of overall exposure to EDCs is very complex. Using traditional monitoring methods (i.e., chemical analysis), it is only possible to assess a few EDCs in biological matrices and the combined effect of different EDCs cannot be estimated. Therefore, novel methods to assess EDC exposure were proposed by the scientific community. These methods detect the biological effect induced by a mixture of EDCs rather than quantifying the presence of individual EDCs. In particular, oestrogenic activity assays have been proposed to assess EDC exposure in biological samples [28].
The aims of this pilot study were (i) to investigate the possible relationship between signs of PP and potential risk factors (e.g., exposure to EDCs in daily life, occupational EDC exposure of parents, eating habits), (ii) to evaluate the potential application of an in vitro assay (i.e., the gene reporter luciferase assay) as a biomarker of exposure to EDCs. The study involved 40 subjects: girls with clinical signs of PP were classified as cases (P), while age-matched pre-pubertal girls were classified as controls (C). The association between signs of PP and potential risk factors for its occurrence was investigated through questionnaires completed by girls’ parents. Moreover, girls’ serum samples were collected and were analysed with both a chemiluminescence immunoassay to quantify 17β-oestradiol (E2) and a gene reporter luciferase assay to assess the oestrogenic activity. This study was carried out during an exceptional period characterised by the COVID-19 pandemic, that negatively affected the study course (e.g., complications in the recruitment and interruption of research activities) reducing the sample size.
2. Materials and Methods
2.1. Study Design
This pilot study was approved by the Ethical Committee of the A.O.U. Città della Salute e della Scienza di Torino—A.O. Ordine Mauriziano—A.S.L. Città di Torino and involved 40 girls aged between 3 and 8 years. The subjects were recruited from the Regina Margherita Children Hospital of Turin (Piedmont region, Northern Italy). The parents of girls provided written informed consent to participate in the study.
Girls with clinical signs of PP confirmed during their access to the paediatric endocrinology clinic were included in P (n = 30). According to the clinical–hormonal examinations, 13 girls were affected by central PP (characterized by activation of the HPG axis), while 17 were affected by incomplete PP (without activation of the HPG axis). At the time of diagnosis, the stages of breast development according to the female breast development scale of Tanner were the following. Among girls with central PP, 5 girls were classified as stage II, while 8 girls as stage III; among girls with incomplete PP, 12 girls were classified as stage II, while 5 girls as stage III. Regarding Tanner stages of pubic hair development, among girls with central PP, 10 girls were classified as stage I, 2 girls as stage II, and a girl as stage III; among girls with incomplete PP, 10 girls were classified as stage I, 5 girls as stage II, and 2 girls as stage III. One girl with central PP and one with incomplete PP had one episode of blood spotting reported at diagnosis, but not clear menarche. Genetic analyses for PP predisposition were not carried out for this study. At the time of diagnosis and of blood sampling, no P girls had medical treatment for PP, which was subsequently started in 12 out of 13 patients with central PP.
Age-matched pre-pubertal girls were included in C (n = 10). Exclusion criteria were: age ≥8 years, male sex, and presence of endocrine disorders (for C).
In order to collect information on the study population and to evaluate the association between signs of PP and potential risk factors for this condition, questionnaires were distributed to girls’ parents. Moreover, blood samples were collected, and sera were analysed through a chemiluminescence immunoassay to quantify E2 and through a gene reporter luciferase assay to assess the oestrogenic activity as a biomarker of exposure to EDCs.
2.2. Questionnaires
Questionnaires were composed of both open and closed-ended questions and they were organized in the following sections: children personal data (e.g., age, weight, height, residence, clinical data), information about mother and father (e.g., educational level, EDC knowledge), pregnancy (e.g., personal and clinical data during pregnancy), neonatal age (e.g., childbirth type, clinical data during neonatal age, breastfeeding type), type of pubertal development of parents and of any other siblings, possible EDC exposure due to residence, parents’ occupation, lifestyle, and eating habits (see Supplementary Materials 1). Data collected through questionnaires were entered into a database using Microsoft Excel, anonymising the participants to preserve privacy during the study.
Data Processing
Weight and height data were used to calculate the children’s body mass index (BMI) (weight [kg]/height [m] squared) which was used to classify the children as underweight, normal weight, overweight, or obese according to the BMI cut-offs for age proposed by Cole et al. [29,30].
To assess the level of total exposure to EDCs, the sum of residence-related exposure factors (maximum 5 factors) and lifestyle-related exposure factors (maximum 13 factors) was calculated. These two types of factors were chosen as representative of a “current” exposure, while other exposure factors were not considered (e.g., exposure during pregnancy or neonatal period). Therefore, the minimum level of exposure was equal to 0 (no exposure factor), while the maximum level of exposure was equal to 18 (all exposure factors due to residence and lifestyle). The EDC cumulative exposure level of each girl was defined as “low” when exposure factors ranged between 1 and 6 or “high” when exposure factors ranged between 7 and 18. The threshold of 6 was chosen based on the results obtained from the questionnaires: 6 corresponds to half of the maximum number of exposure factors found in this study for a single girl (maximum exposure factors = 11).
2.3. Chemiluminescence Immunoassay (E2 Concentrations)
A chemiluminescence immunoassay was applied in order to quantify E2 concentrations in serum samples using the Elecsys Estradiol III kit (Roche Italia S.p.A., Monza, Italy). The assay was carried out according to manufacturer instructions. The detection limit of the assay was equal to 5 pg/mL.
2.4. Gene Reporter Luciferase Assay (Oestrogenic Activity)
The oestrogenic activity of serum samples was assessed using a gene reporter luciferase assay which measures the expression of a reporter gene regulated by oestrogens [31]. The assay was carried out using the luciferase-transfected MELN cells kindly provided by Dr. P. Balaguer (INSERM, Montpellier, France), which derive from MCF7 breast cancer cells after transfection with the ERE-βGlob-Luc-SVNeo plasmid. The method was applied using the protocol reported by Schilirò et al. [32] modified according to a literature review [28]. MELN cells were grown in 75 cm2 flasks in a 5% CO2/95% air atmosphere under saturating humidity at 37 °C. For cell growth Dulbecco’s Modified Eagle’s Medium Nutrient Mixture F12 Ham (DMEM-F12) medium was used; the medium was supplemented with phenol red and the following supplements: 5% v/v of Foetal Bovine Serum (FBS), 4 mM of L-Glutamine, 100 U/mL–100 μg/mL of Penicillin/Streptomycin, and 1 mg/mL of G418 Geneticin. Since this culture medium can cause oestrogenic activity and impair the results, DMEM-F12 without phenol red and with stripped FBS (i.e., FBS treated with charcoal and dextran in order to remove oestrogens) was used as the experimental medium. The stripped FBS was purchased by Merck (Darmstadt, Germany). Three days before the experiment, the culture medium of 75 cm2 flasks containing cells was replaced with experimental medium to allow cells to adapt. For the experiment, cells of the adapted flasks were trypsnised, counted with hemocytometer (Bürker counting chamber), and seeded in white 96 wells-plates at a density of 40,000 cells/well in 100 μL/well of experimental medium. Cells were then incubated in a 5% CO2/95% air atmosphere under saturating humidity at 37 °C. After 24 h, the experimental medium was removed and replaced with 100 μL of each sample dilution for three replicas. Each human serum sample was diluted at 5% v/v in experimental medium, adding 5% v/v of stripped FBS in order to reach a final concentration of 10% of serum (human serum + stripped FBS). Thereafter, cells were incubated again for 21 h. In each plate, a negative control (C−), which consists of experimental medium supplemented with stripped FBS (10% v/v), and a positive control (C+), which corresponds to E2 in a concentration of 10−8 M in experimental medium supplemented with stripped FBS (10% v/v) were included. Moreover, for each independent experiment, a standard response curve of E2 was set up. The response curve was made up of increasing E2 concentrations in experimental medium with 10% of stripped FBS (final E2 concentrations from 10−12 M to 10−8 M). Each treatment was tested in triplicate in two independent experiments. After 21 h incubation, 100 μL of One-Glo Luciferase Assay System (Promega Italia S.r.l., Milan, Italy), containing fluoroluciferin were added in each well. Plates were shaken for 5 min to allow complete cell lysis. Within 30 min after cell lysis, the luminescence of each well was measured with a luminometer (Infinite Reader M200 Pro, Tecan, Männedorf, Switzerland).
The oestrogenic activity was expressed as relative luciferase activity and was calculated as a percentage of the activity induced by the treatment with respect to the activity induced by the positive control, subtracting the activity of the negative control (relative luciferase activity of C− = 0%, relative luciferase activity of C+ = 100%). The results were elaborated and expressed as E2 equivalent concentration (EEQ). The EEQ is defined as the total concentration of all oestrogenic active compounds in sample normalised to the E2. To express the data as EEQ using statistical analysis software (IBM SPSS Statistics 25, IBM, Armonk, NY, USA), the dose–response curve equation of the reference compound (E2) was estimated. The equation was estimated by entering the logarithm in base ten of the molar concentrations of E2 tested as the independent variable and the relative luciferase activity induced by each concentration as the dependent variable (best fitting = quadratic function; R2 = 0.94, p < 0.001). Next, the relative luciferase activity of the samples tested at 5% was interpolated onto the function and the EEQ value of each sample was thus obtained [33]. Since each sample was tested in two independent experiments, the final EEQ of each sample was expressed as the mean ± standard deviation of the EEQs obtained in the two experiments. The sensitivity of the reporter gene assay on MELN cells is 0.3 pg/mL. However, since the serum samples were diluted to 5% in the experimental culture medium, the sensitivity under the experimental conditions was 6.5 pg/mL.
2.5. Data Analysis and Statistical Analysis
Statistical analyses of data obtained from questionnaires and from laboratory analyses (E2 concentrations and oestrogenic activity) were performed using IBM SPSS Statistics (IBM, Armonk, NY, USA). To summarize general information of the study population, data collected from questionnaires were analysed with descriptive statistics and compared between C and P to investigate a possible association between signs of PP and risks factors (e.g., EDC exposure). Regarding laboratory analyses, as for questionnaires, mean E2 concentrations and mean EEQs were calculated for the whole population and then compared between C and P. Finally, mean E2 concentrations and mean EEQs were compared considering the level of EDC exposure (low or high) and the living environment (urban or rural). For data analysis, E2 concentrations below the detection limit (<5 pg/mL) were considered equal to half the detection limit of the assay (2.5 pg/mL). The Shapiro–Wilk test was performed in order to evaluate data distribution of continuous variables. Since data were not normally distributed, the mean values of these variables were compared among the groups using non-parametric tests (i.e., Mann–Whitney test). Finally, Chi-Square test was performed in order to compare the distribution of categorical variables among the groups. The results were considered statistically significant for p ≤ 0.05.
3. Results and Discussion
3.1. Questionnaire Results
3.1.1. General Characteristics
The study population was composed of 40 female children (three–eight years of age). According to residence, 30.0% of the study population (n = 12) lived in Turin (the main city of Piedmont region), 45.0% (n = 18) in Turin province, and 25.0% (n = 10) in other provinces of the Piedmont region (Northern Italy). The average age was 7.34 ± 1.17 years, while the average BMI was 16.40 ± 3.06 kg/m2.
Based on the specific BMI cut-offs for age proposed by Cole et al. [29,30], 73.0% of girls (n = 27) were normal weight, 13.5% (n = 5) were underweight, and 13.5% (n = 5) were overweight or obese. For three girls it was not possible to calculate BMI due to missing data in the questionnaires. The percentage of overweight/obese girls was lower than the national data reported by the study of Lauria et al. [34]. This study reported the national data on the prevalence of overweight and obese children collected in the national study “OKkio alla SALUTE”, part of the WHO/Europe Childhood Obesity Surveillance Initiative (COSI); it stated that, during year 2016, the prevalence of overweight children (including obese children) among primary school girls was at 30.5% considering the population residing in the whole of Italy, while it was 25.7% considering the population residing in Northern Italy [34].
Regarding parents’ educational level, 28.2% of the mothers and 29.7% of the fathers had an eighth grade or professional diploma, 41.0% and 56.8% had a high school diploma, and 30.8% and 13.5% had a degree.
Concerning EDC knowledge, only 28.2% of the parents declared to know them, while the remaining proportion stated that they had never heard of them (71.8%). EDC knowledge was mainly due to information acquired by TV, internet, books and articles, medical doctors, or work colleagues. This result suggested that it would be extremely important to raise awareness about EDCs and their possible impact on human health. Information campaigns would be especially useful among parents-to-be, since prenatal and early childhood exposure to EDCs may greatly affect the proper development of the child [35,36].
3.1.2. General Characteristics: Comparison between C and P
Mean age was 6.30 ± 1.34 years for C (min 3.90 years, max 7.70 years) and 7.49 ± 0.70 years for P (min 4.90 years, max 7.90 years). A statistically significant difference was found between the two groups (Mann–Whitney test, p < 0.001).
Mean BMI was 15.83 ± 4.99 kg/m2 for C (min 10.42 kg/m2, max 27.78 kg/m2) and 16.58 ± 2.22 kg/m2 for P (min 13.66 kg/m2, max 24.49 kg/m2). Although mean BMI was not statistically different between C and P (Mann–Whitney test, p > 0.05), the percentages of normal weight, underweight, and overweight/obese girls were statistically different (Chi-Square test, p = 0.003); in particular, the percentage of overweight/obese girls was higher in C than in P. This result was unexpected as being overweight/obese has been positively associated with the onset of PP [12,14,37]. Possible interpretations of this result could be the awareness of parents that eating habits can affect the onset and development of this condition (e.g., information received from the general practitioner) and/or the little case series of the present study.
Mothers’ and fathers’ pubertal development and familiarity for PP were not statistically different between C and P. On the contrary, a statistically significant difference was found between C and P in the percentage of siblings with signs of PP. Indeed, the girls in C had no siblings with signs of PP, whereas 75.0% of the girls in P had at least one sibling affected by the same condition (Chi-Square test, p = 0.005). This result is interesting as it confirmed a genetic predisposition to PP, already reported in literature [38,39,40], but could also suggest the importance of lifestyle habits adopted by families (i.e., due to lifestyle habits, all the children of a single family could be highly exposed to EDCs, thus may be more at risk for PP).
Considering the living environment (urban or rural), the percentage of girls living in an urban environment was higher, although not statistically significant, in P than in C (40.0% and 20.0%, respectively).
3.1.3. EDC Exposure
The results showed that a high percentage of parents (especially fathers) were potentially exposed to EDCs in their workplace. Indeed, 42.1% of fathers and 15.4% of mothers worked in the agriculture sector, rubber industries, plastic industries, petrochemical plants, metallurgical plants, electronic industries, beauty sectors, dye industries, and incinerators, which can be considered sources of exposure to EDCs [15]. Moreover, 67.5% of families lived near one or more potential sources of EDCs (i.e., near an industrial plant, mechanical workshop, landfills, cultivated field, chemical warehouse) [15].
Possible exposure to EDCs due to lifestyle was also assessed considering 13 habits that can cause exposure to EDCs. For example, the use of plastic bottles, plastic containers, and clingfilm were considered habits at risk. Indeed, EDCs are contained in these products (e.g., phenols and phthalates) and can be transferred especially to warm foods [41,42]. Consumption of packaged meat/vegetables was also considered a habit at risk as it can be a source of exposure to phthalates and bisphenols [43,44]. In addition, the use of personal care products, which may contain phthalates and parabens [45], was evaluated as a habit that can increase EDC exposure [15].
Overall, girls seem to be potentially exposed to EDCs as 100% of families adopt at least one lifestyle habit that could increase EDC exposure. In particular, the most adopted habits were the use of care creams, the use of clingfilm, the use of spray cosmetics, and the consumption of packaged meat/vegetables.
Through questionnaires, the possible exposure to EDCs through eating habits was also evaluated. Several studies seem to suggest a correlation between eating habits, such as the consumption of canned or highly processed food, and the intake of EDCs. These products may contain several EDCs (e.g., bisphenol A) that can be transferred into food [46,47,48,49]. Consumption of water in plastic bottles has also been associated with exposure to EDCs (e.g., phenols, phthalate) [20,41,42,50]. Moreover, some cooking techniques, due to high temperatures, could lead to food carbonization with the consequent formation of polycyclic aromatic hydrocarbons [15,47,48,51,52]. Finally, consumption of soy products in childhood has also been considered to cause a possible increase in EDC exposure (i.e., phytoestrogens) and was associated with PP in girls [53].
The study population also appears to be potentially exposed due to eating habits. Indeed, a high percentage of families declared a weekly consumption of water in plastic bottles (87.2%), of grilled food (42.5%), and of canned food (34.2%).
3.1.4. EDC Exposure: Comparison between C and P
Regarding EDC exposure due to lifestyle, 4 out of 13 habits were found to be significantly different between C and P. As reported in Table 1, the use of disposable plastic containers, the storage of warm foods in plastic containers, the consumption of packaged meat/vegetables, and the use of candles/incense/air fresheners were significantly higher in C than in P. Considering that the adoption of these habits may lead to a greater exposure to EDCs [43], overall, the results suggested that girls in P were less exposed to EDCs than girls in C. This unexpected result could be related to the awareness of the parents that eating habits can affect the onset and development of this condition and/or the little case series of the current study, so it should be further investigated.
Table 1.
Lifestyle habits for which a statistically significant difference was found between pre-pubertal girls (C) and girls with signs of PP (P). Data are expressed as percentages of families that adopt each habit.
| C (%) | P (%) | Chi-Square Test (p) | |
|---|---|---|---|
| Use of disposable plastic containers | 40.0 | 6.7 | 0.011 |
| Storage of warm foods in plastic containers | 90.0 | 33.3 | 0.002 |
| Consumption of packaged meat/vegetables | 80.0 | 43.3 | 0.044 |
| Use of candles/incense/air fresheners | 80.0 | 16.7 | <0.001 |
Since exposure by ingestion represents one of the main routes of EDC exposure for humans, the potential association between eating habits and the development of signs of PP was investigated comparing C and P. A total of 8 out of 18 eating habits were found to be significantly different between C and P (Table 2).
Table 2.
Eating habits for which a statistically significant difference was found between C and P. Data are expressed as percentages and are divided according to consumption frequency.
| Frequency | C (%) | P (%) | Chi-Square Test (p) | |
|---|---|---|---|---|
| Consumption of sheep meat | Never | 0.0 | 23.3 | 0.047 |
| Annually | 0.0 | 20.0 | ||
| Monthly | 12.5 | 23.3 | ||
| Weekly | 87.5 | 33.4 | ||
| Consumption of pork meat | Never | 0.0 | 13.3 | 0.022 |
| Annually | 0.0 | 0.0 | ||
| Monthly | 10.0 | 46.7 | ||
| Weekly | 90.0 | 40.0 | ||
| Consumption of other meat * | Never | 0.0 | 60.7 | <0.001 |
| Annually | 0.0 | 7.2 | ||
| Monthly | 0.0 | 21.4 | ||
| Weekly | 100.0 | 10.7 | ||
| Consumption of canned foods | Never | 50.0 | 13.3 | 0.017 |
| Annually | 12.5 | 0.0 | ||
| Monthly | 12.5 | 50.0 | ||
| Weekly | 25.0 | 36.7 | ||
| Consumption of water in glass bottles | Never | 25.0 | 70.0 | 0.041 |
| Annually | 0.0 | 0.0 | ||
| Monthly | 0.0 | 3.3 | ||
| Weekly | 75.0 | 26.7 | ||
| Consumption of water from public water sources | Never | 14.3 | 82.8 | 0.002 |
| Annually | 14.3 | 3.4 | ||
| Monthly | 0.0 | 0.0 | ||
| Weekly | 71.4 | 13.8 | ||
| Consumption of fried food | Never | 0.0 | 3.3 | 0.011 |
| Annually | 0.0 | 23.3 | ||
| Monthly | 10.0 | 43.4 | ||
| Weekly | 90.0 | 30.0 | ||
| Consumption of grilled food | Never | 0.0 | 3.3 | 0.006 |
| Annually | 0.0 | 23.3 | ||
| Monthly | 10.0 | 46.7 | ||
| Weekly | 90.0 | 26.7 |
* meat other than bovine, sheep, pork, poultry.
In particular, a higher consumption (in terms of frequency) of water in glass bottles and of water from public sources was found in C with respect to P. These results are interesting, because they can suggest a potential relationship between EDC exposure and signs of PP. Indeed, a greater consumption of water in glass bottles leads to a lower consumption of water in plastic which can instead lead to exposure to EDCs such as, for example, phenols and phthalates. Regarding the consumption of water from public sources, although it does not directly lead to a lower exposure to EDCs, this behaviour could be associated with the use of non-disposable glass bottles. In fact, the consumption of water from public sources often takes place using glass bottles while generally those who consume water already bottled buy it in disposable plastic bottles (more easily available on the market and at a lower cost).
The consumption of pork, sheep, and other meat types was more frequent in C than in P. This result is unexpected since it has been reported that the intake frequency of bovine, sheep, and pork meat were inversely associated with the age at menarche [54] and the consumption of poultry, pork, and processed meat was positively associated with the levels of some EDCs in human serum [27]. However, it is important to underline that the relationship between meat intake, EDC exposure, and age at menarche can be affected by numerous factors. For example, it is not easily identifiable which meat type can lead to a higher EDC exposure, representing a potential risk factor for PP. In fact, the presence of EDCs in meat can depend on many factors including the characteristics of the animal (e.g., species, sex, age that can influence the production of endogenous steroid hormones), materials used to process and package meat, the possible use of hormones in the breeding phases (although Europe banned meat from animals treated with steroid growth hormones), and the use of cooking techniques that can favour EDC presence in foods (e.g., grilling). Moreover, beside EDC-related mechanisms, meat intake might induce an earlier age at menarche through, for example, development of adiposity or micronutrient availability [54].
Conversely, questionnaire results showed that the frequency of canned food consumption was higher in P than in C. This result could suggest that EDC exposure through this eating habit could be associated with the occurrence of PP.
Finally, regarding food cooking techniques, a higher frequency of grilling and frying was found in C than in P. This result is unexpected as overcooking food on the grill could lead to EDC exposure [47,51,52] and is also opposite to the study of Chen et al. [55], in which an unhealthy diet pattern, heavy in fried food, was significantly positively associated with PP.
Overall, the percentage of girls with a high EDC exposure was higher, although not significant, in C than in P (70.0% and 40.0%, respectively).
3.2. Results of Laboratory Analyses
3.2.1. E2 Concentrations
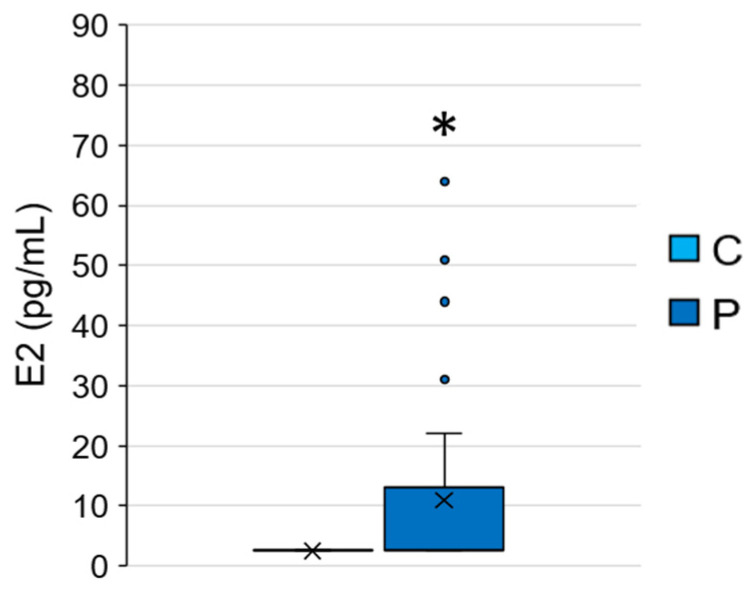
The average E2 concentration of the 40 subjects was 8.85 ± 14.43 pg/mL (min < detection limit, max 64.00 pg/mL), and the comparison between C and P showed that E2 concentrations were significantly higher in P than in C (P = 10.97 ± 16.17 pg/mL, C ≤ detection limit, Mann–Whitney test, p = 0.040) (Figure 1). Moreover, regarding P, the average E2 concentration of girls with central PP was 18.50 ± 21.97 pg/mL, while that of girls with incomplete PP was 5.21 ± 5.50 pg/mL. This result was expected since signs of PP are usually the clinical feature of a premature activation of the HPG axis, which leads to E2 release in females resulting in a high concentration of this hormone in their blood [1,56,57,58], but could also be due to other external factors such as EDC exposure [8,59].
Figure 1.
17β-oestradiol (E2) concentrations measured in C and P. * = p ≤ 0.05, Mann–Whitney test.
The comparison between E2 concentrations found in the present study with the physiological E2 concentrations during the pre-pubertal period showed that the average E2 concentrations in the serum of girls in the present study were within the range of the physiological values (<27 pg/mL, data provided by the Regina Margherita Children hospital, Table S1 in Supplementary Materials 2). As expected, some E2 concentrations measured in P were higher than the upper limit of the pre-pubertal physiological range, confirming that hormone concentrations can be high in these girls.
3.2.2. EEQ Concentrations
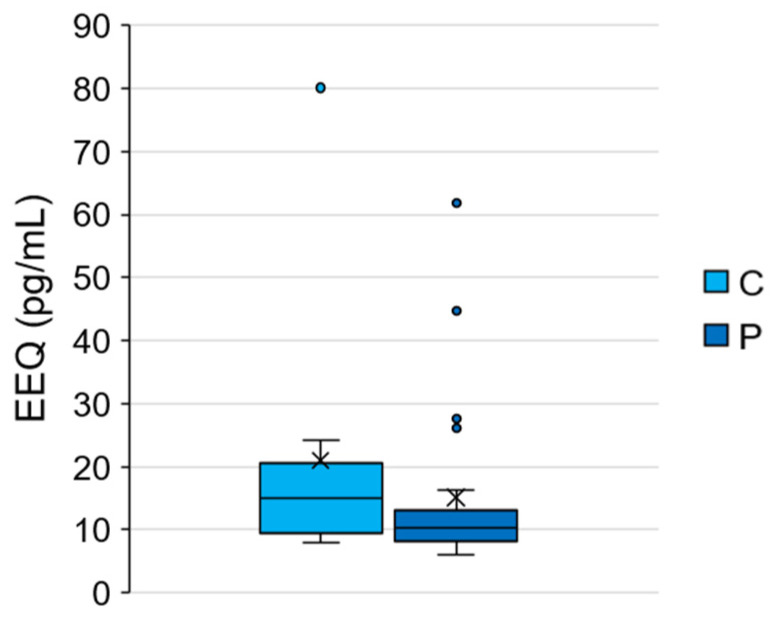
The average EEQ concentration of the 40 subjects was 16.62 ± 15.58 pg/mL (min 6.10 pg/mL, max 80.10 pg/mL). Table 3 shows the mean EEQ concentrations of C and P in comparison with the mean EEQ concentrations of pre-pubertal girls and of PP girls reported in previous studies [60,61,62,63,64,65,66,67,68]. As can be observed, the mean EEQ concentration of C found in the present study (21.03 ± 21.41 pg/mL) was higher than EEQ concentrations found in literature. This finding could suggest that girls in C may have a higher EDC exposure than pre-pubertal girls analysed by other studies. Moreover, EEQ concentration of P found in the present study (15.14 ± 13.24 pg/mL) was similar to or higher than the EEQ concentrations reported by previous studies [61,63,65,69]. It is important to underline that the discrepancy among results could be due to the different methodologies applied in order to estimate EEQ by the different authors [28].
Table 3.
Serum 17β-oestradiol equivalent concentrations (EEQs) found in the present study in comparison with EEQ concentrations reported by previous studies for pre-pubertal girls and for PP girls. Data are presented as mean ± standard deviations (SD).
| Reference | Study Population (n) | EEQ (Mean ± SD, pg/mL) | |
|---|---|---|---|
| Pre-pubertal girls | Present study | 10 | 21.03 ± 21.41 |
| Klein et al., 1994 [62] | 21 | 0.6 ± 0.6 | |
| Klein et al., 1999 [61] | 15 | 0.9 ± 1.0 | |
| Paris et al., 2002 [66] | 18 | 3.5 ± 2.2 | |
| Larmore et al., 2002 [63] | 12 a | 0.3 ± 0.4 | |
| Larmore et al., 2002 [63] | 12 b | 0.6 ± 1.3 | |
| Wilson et al., 2003 [68] | 34 | 3.4 ± 2.9 | |
| Janfaza et al., 2006 [60] | 147 | 1.6 ± 2.6 | |
| Pereira et al., 2015 [67] | 91 | 3.6 ± 2.3 | |
| Mesa Valencia et al., 2019 [64] | 107 | 3.6 ± 2.3 | |
| PP girls | Present study | 30 | 15.14 ± 13.24 |
| Klein et al., 1999 [61] | 20 | 2.3 ± 1.2 | |
| Larmore et al., 2002 [63] | 12 | 2.2 ± 2.7 | |
| Gaspari et al., 2011 [69] | 1 | 13.5 ± 1.0 | |
| Paris et al., 2013 [65] | 15 | 8.4 ± 7.3 |
a = normal weight; b = obese.
Unlike E2 concentrations, no significant differences were found between C and P in EEQ concentrations (Mann–Whitney test, p > 0.05) (Figure 2). Therefore, the present study did not find a strong relationship between EDC exposure and signs of PP. However, some confounding factors could have influenced the results. For example, our control group seems to be highly exposed to EDCs compared to the general population. Indeed, a higher EEQ was found in C with respect to the literature and a higher EDC exposure in C than in P was also confirmed through the questionnaire analysis (e.g., the percentage of highly exposed girls was higher, although not significant, in C than in P: 70.0% and 40.0%, respectively).
Figure 2.
EEQ concentrations measured in C and P. Data were not statistically different (Mann–Whitney test, p > 0.05).
3.2.3. Relationship between EDC Exposure (Low/High) and EEQ
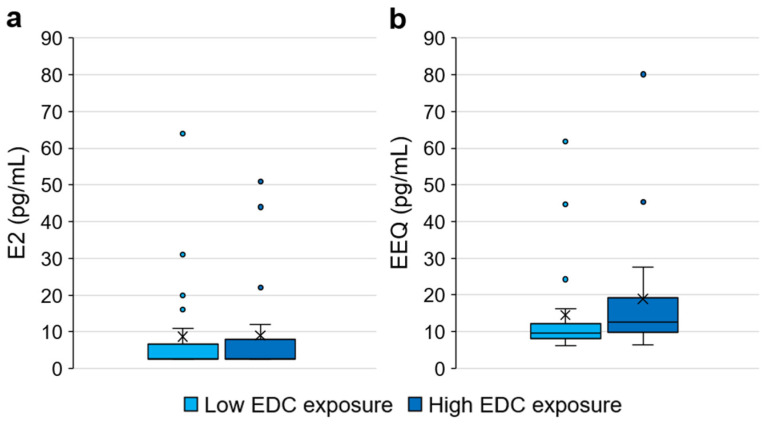
To evaluate the relationship between EDC exposure and oestrogenic activity, the EEQ was compared according to the level of cumulative exposure to EDCs derived from questionnaires. In particular, the oestrogenic activity was compared between girls with a low EDC exposure (n = 21) and girls with a high EDC exposure (n = 19). In order to consider the activity due to endogenous hormones, E2 concentrations were also compared between the two groups.
No statistically significant difference was detected between the two groups (i.e., low/high EDC exposure) for both the considered parameters (i.e., E2 and EEQ) (Mann–Whitney test, p > 0.05) (Figure 3). However, it is interesting to note that while the E2 concentrations seem similar in the two groups (mean E2: low EDC exposure = 8.67 ± 14.76 pg/mL, high EDC exposure = 9.05 ± 14.45 pg/mL), in the low EDC exposure group, a lower EEQ was detected than in the high EDC exposure group (mean EEQ: low EDC exposure = 14.55 ± 13.72 pg/mL, high EDC exposure = 18.89 ± 17.51 pg/mL). This result, despite not significant, could suggest that, with the same endogenous hormone levels (i.e., E2 concentrations) in the high EDC exposure group, a higher concentration of oestrogenic compounds may be present in the serum, resulting in a higher oestrogenic activity. Therefore, this study showed a partial concordance between EDC exposure (estimated using questionnaires) and the results of the gene reporter luciferase assay (applied as a biomarker of EDC exposure). The discrepancy between EDC exposure assessed by questionnaires and EEQ could be explained considering that EDCs are heterogeneous and ubiquitous chemicals whose assessment is difficult to estimate using only questionnaires. Moreover, it should be considered that, through EEQ, only EDCs with oestrogenic activity can be quantified.
Figure 3.
Comparison between girls with low and high endocrine disrupting chemical (EDC) exposure: (a) E2 concentrations; (b) EEQ concentrations. Data were not statistically different (Mann–Whitney test, p > 0.05).
3.2.4. Relationship between Living Environment (Rural/Urban) and EEQ
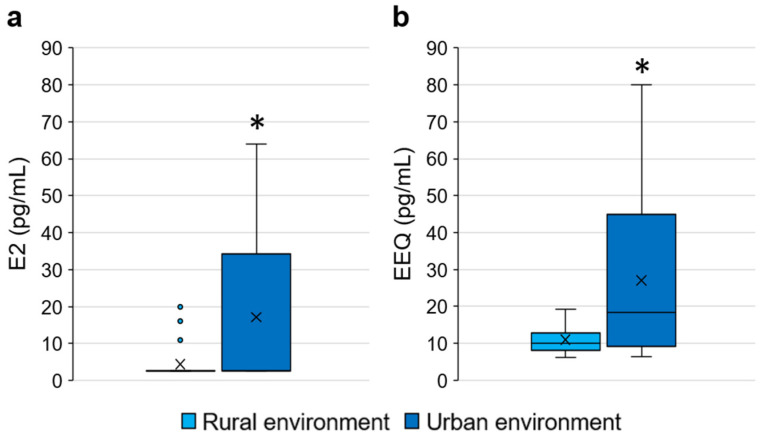
Oestrogenic activity was also compared according to the type of living environment (urban or rural environment). In particular, oestrogenic activity was compared between girls residing in a rural environment (n = 26) and girls residing in an urban environment (n = 14). In order to consider the activity due to endogenous hormones, E2 concentrations were also compared between the two groups.
Th average E2 concentration in the rural environment was 4.38 ± 4.73 pg/mL (min 2.50 pg/mL, max 20.00 pg/mL), while in the urban environment it was 17.14 ± 21.62 pg/mL (min 2.50 pg/mL, max 64.00 pg/mL); average EEQ concentration in the rural environment was 10.98 ± 3.59 pg/mL (min 6.10 pg/mL, max 19.20 pg/mL), while in the urban environment it was 27.08 ± 22.86 pg/mL (min 6.40 pg/mL, max 80.10 pg/mL). Statistically significant differences were found between two groups (i.e., rural vs. urban environment) for both the considered parameters (Mann–Whitney test- E2: p = 0.031; EEQ: p = 0.020) (Figure 4).
Figure 4.
Comparison between girls living in a rural environment and girls living in an urban environment: (a) E2 concentrations; (b) EEQ concentrations. * = p ≤ 0.05 Mann–Whitney test.
This result suggests that living in urban or industrial areas could cause higher oestrogenic activity that is probably due to a higher exposure to EDCs. This hypothesis is supported by several studies which show that people living in urban environments can be exposed to EDCs. The exposure may occur through polluted and heavily anthropized rivers and through the consumption of tap water. Indeed, some studies have shown that the presence of EDCs in anthropized watercourses, due to inadequate urban wastewater management, can lead to pollution of drinking water sources. Since drinking water treatment technology can be ineffective in removing these compounds, consumption of tap water can cause the consequent EDC intake [18,20,70]. Exposure in urban areas may also occur through inhalation of atmospheric EDCs released by human activities (e.g., traffic, industrial processes, waste incineration) [21,71].
In addition to higher oestrogenic activity in girls living in an urban environment than in a rural one, the results of the present study showed that the percentage of girls living in an urban environment was higher, although not statistically significant, in P than in C (40.0% and 20.0%, respectively). This finding suggested that urban environments might influence the age at menarche. In accordance with this hypothesis, several studies reported a significant association between residence in areas with high traffic or high air pollution, such as urban areas, and an earlier age at menarche [72,73,74].
However, although people living in urban environments can be highly exposed to EDCs, an exposure can occur also in rural environments due to agriculture (i.e., use of pesticides in fields) [15] or lifestyle habits; indeed, according to questionnaire results, the percentage of girls living in a rural environment that have a high exposure to EDCs was 57.69%, while the percentage of girls living in a urban environment that have a high exposure to EDCs was only 28.57%.
3.3. Study Limitations
The present study was affected by some limitations. In particular, the applied method (i.e., gene reporter luciferase assay) assessed the overall oestrogenic activity but was not suitable to distinguish between the activity induced by EDCs from that of endogenous hormones. Although this disadvantage was resolved by evaluating the concentration of the main endogenous hormone in the serum (i.e., E2), the interpretation of the results is quite complex. Moreover, despite the estimate of EDC exposure through questionnaires was crucial to integrate the laboratory analysis results, it is important to underline that it was not simple to assess EDC exposure levels through this method. Indeed, EDCs are a group of very heterogeneous molecules that are widely present in numerous everyday products and environmental matrices, so the sources of exposure can be many and estimating the realistic levels of exposure to EDCs is very complex. Therefore, to better estimate EDC exposure, in future studies, it could also be interesting to perform a chemical analysis on serum samples in order to quantify some specific EDCs (e.g., bisphenol A, phthalates, parabens).
This study was carried out during an exceptional period characterised by the COVID-19 pandemic. For more than a year, in hospitals, priority was given to more severe health conditions; therefore, paediatric endocrinology accesses due to suspected PP signs were reduced. The pandemic and the subsequent slow return to normality also caused a lower rate of adhesion in the study by the girls’ families. Therefore, this emergency period has affected the project concerning subject recruitment; furthermore, it has impeded the study course as research and laboratory activities at the university were interrupted due to lockdowns. Consequently, the results of this study may be influenced by sample size, so in order to confirm the results, it would be important to perform other studies on larger populations.
Despite limitations, this study evaluated the possible association between an important clinical condition (i.e., signs of PP), whose incidence is increasing [4,75,76,77], and the exposure to environmental contaminants of emerging concern (i.e., EDCs). The association was studied through the application of an effect-based monitoring tool (i.e., gene reporter luciferase assay) that has the advantage to potentially assess the cumulative exposure to all the substances with an oestrogenic effect, also considering metabolites and substances whose oestrogenic activity has not been studied yet.
4. Conclusions
This pilot study examined the relationship between signs of PP and potential risk factors including EDC exposure. Overall, the questionnaire analysis showed a low EDC knowledge and a high exposure through residence, lifestyle, and eating habits. The results also highlighted quite a high occupational exposure of parents. Since the lack of awareness about EDCs could lead to adoption of habits at risk, it would be important to raise awareness especially among future parents to avoid or decrease prenatal and early childhood exposure allowing the proper development of infants.
As expected, laboratory results confirmed the premature activation of the HPG axis and the consequent E2 release in P (i.e., higher E2 concentration in P than in C).
Despite the comparison between C and P suggesting a potential relationship between some habits at risk for EDC exposure and signs of PP (i.e., to eat canned food and to drink less water in glass bottles and from public sources), a relationship between EDC exposure and signs of PP was not found. Therefore, it was not possible to confirm the interference of EDCs on HPG axis, nor their contribution to the occurrence of PP. This relationship might not be underlined due to potential confounding factors (e.g., the control group seems to be highly exposed to EDCs).
In addition, this study showed only a partial concordance between EDC exposure and the results of the gene reporter luciferase assay. The discrepancy could be explained considering that EDCs are heterogeneous and ubiquitous chemicals whose assessment is difficult to estimate using questionnaires and that EEQ only quantifies EDCs with an oestrogenic activity.
Finally, EEQ concentrations were significantly higher in girls living in an urban environment suggesting that these girls are potentially more exposed to EDCs than girls living in a rural environment.
In conclusion, the results of this study suggested that the joint use of exposure information, quantification techniques, and biological effects-based tools might allow an integrated knowledge of different variables, being useful for the evaluation of a possible relationship between exposure to EDCs and PP. Since pubertal development is a complex process that includes genetic, environmental, and cultural factors, this pilot study can be considered a starting point for broader research aimed at clarifying the still existing doubts about the causes of PP in girls.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph20010014/s1, Questionnaire (Supplementary Materials 1), Table S1: physiological 17β-oestradiol (E2) concentrations (Supplementary Materials 2).
Author Contributions
Conceptualization, L.D.S. and T.S.; methodology, M.G. and A.T.; validation, M.G., A.T. and G.N.B.; formal analysis, M.G. and G.N.B.; investigation, M.G., A.T., G.N.B., R.B. and E.A.; resources, L.D.S. and T.S.; data curation, M.G., A.T., G.N.B., R.B. and E.A.; writing—original draft preparation, G.N.B.; writing—review and editing, M.G., A.T., R.B., E.A., L.D.S. and T.S.; visualization, M.G. and G.N.B.; supervision, L.D.S. and T.S.; project administration, T.S.; funding acquisition, T.S. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethical Committee of the A.O.U. Città della Salute e della Scienza di Torino—A.O. Ordine Mauriziano—A.S.L. Città di Torino (application number: 500.751; identification code: 00587/2020; date of approval: 4 March 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that supports the findings of this study are not publicly available due to privacy and ethical reasons.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was supported by the Fondazione CRT (Cassa di Risparmio di Torino), a private, non-profit Italian organisation with full statutory and management autonomy (CRT funding n° 2018.2300). Fondazione CRT projects and resources target various sectors: from the preservation and promotion of the artistic heritage and cultural activities to scientific research; from education and training to healthcare and assistance for vulnerable social groups; from civil protection and environmental safeguards to innovation in local institutions and support of economic development.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Cheuiche A.V., da Silveira L.G., de Paula L.C.P., Lucena I.R.S., Silveiro S.P. Diagnosis and management of precocious sexual maturation: An updated review. Eur. J. Pediatr. 2021;180:3073–3087. doi: 10.1007/s00431-021-04022-1. [DOI] [PubMed] [Google Scholar]
- 2.Chioma L., Bizzarri C., Verzani M., Fava D., Salerno M., Capalbo D., Guzzetti C., Penta L., Di Luigi L., di Iorgi N., et al. Sedentary lifestyle and precocious puberty in girls during the COVID-19 pandemic: An Italian experience. Endocr. Connect. 2022;11:e210650. doi: 10.1530/EC-21-0650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kiess W., Hoppmann J., Gesing J., Penke M., Körner A., Kratzsch J., Pfaeffle R. Puberty–genes, environment and clinical issues. J. Pediatr. Endocrinol. Metab. 2016;29:1229–1231. doi: 10.1515/jpem-2016-0394. [DOI] [PubMed] [Google Scholar]
- 4.Soriano-Guillén L., Argente J. Central precocious puberty, functional and tumor-related. Best Pract. Res. Clin. Endocrinol. Metab. 2019;33:101262. doi: 10.1016/j.beem.2019.01.003. [DOI] [PubMed] [Google Scholar]
- 5.Valsamakis G., Arapaki A., Balafoutas D., Charmandari E., Vlahos N.F. Diet-induced hypothalamic inflammation, phoenixin, and subsequent precocious puberty. Nutrients. 2021;13:3460. doi: 10.3390/nu13103460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abreu A.P., Kaiser U.B. Pubertal development and regulation. Lancet Diabetes Endocrinol. 2016;4:254–264. doi: 10.1016/S2213-8587(15)00418-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berberoğlu M. Precocious Puberty and Normal Variant Puberty: Definition, etiology, diagnosis and current management-Review. J. Clin. Res. Pediatr. Endocrinol. 2009;1:164–174. doi: 10.4274/jcrpe.v1i4.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Spaziani M., Tarantino C., Tahani N., Gianfrilli D., Sbardella E., Lenzi A., Radicioni A.F. Hypothalamo-Pituitary axis and puberty. Mol. Cell. Endocrinol. 2021;520:111094. doi: 10.1016/j.mce.2020.111094. [DOI] [PubMed] [Google Scholar]
- 9.Buluş A.D., Aşci A., Erkekoglu P., Balci A., Andiran N., Koçer-Gümüşel B. The evaluation of possible role of endocrine disruptors in central and peripheral precocious puberty. Toxicol. Mech. Methods. 2016;26:493–500. doi: 10.3109/15376516.2016.1158894. [DOI] [PubMed] [Google Scholar]
- 10.Latronico A.C., Brito V.N., Carel J.C. Causes, diagnosis, and treatment of central precocious puberty. Lancet Diabetes Endocrinol. 2016;4:265–274. doi: 10.1016/S2213-8587(15)00380-0. [DOI] [PubMed] [Google Scholar]
- 11.Gonc E.N., Kandemir N. Body composition in sexual precocity. Curr. Opin. Endocrinol. Diabetes Obes. 2022;29:78–83. doi: 10.1097/MED.0000000000000687. [DOI] [PubMed] [Google Scholar]
- 12.Liu G., Guo J., Zhang X., Lu Y., Miao J., Xue H. Obesity is a risk factor for central precocious puberty: A case-control study. BMC Pediatr. 2021;21:1–8. doi: 10.1186/s12887-021-02936-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wei Q., Wu M., Li Y.L., Rao R., Li S., Cen Q., Wu H., Lv L., Huang M., Ge Y.P., et al. Physical deviation and precocious puberty among school-aged children in Leshan City: An investigative study. J. Int. Med. Res. 2020;48:300060520939672. doi: 10.1177/0300060520939672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Calcaterra V., Verduci E., Magenes V.C., Pascuzzi M.C., Rossi V., Sangiorgio A., Bosetti A., Zuccotti G., Mameli C. The role of pediatric nutrition as a modifiable risk factor for precocious puberty. Life. 2021;11:1353. doi: 10.3390/life11121353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kabir E.R., Rahman M.S., Rahman I. A review on endocrine disruptors and their possible impacts on human health. Environ. Toxicol. Pharmacol. 2015;40:241–258. doi: 10.1016/j.etap.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 16.Campbell C.G., Borglin S.E., Green F.B., Grayson A., Wozei E., Stringfellow W.T. Biologically directed environmental monitoring, fate, and transport of estrogenic endocrine disrupting compounds in water: A review. Chemosphere. 2006;65:1265–1280. doi: 10.1016/j.chemosphere.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 17.Schilirò T., Pignata C., Rovere R., Fea E., Gilli G. The endocrine disrupting activity of surface waters and of wastewater treatment plant effluents in relation to chlorination. Chemosphere. 2009;75:335–340. doi: 10.1016/j.chemosphere.2008.12.028. [DOI] [PubMed] [Google Scholar]
- 18.Wee S.Y., Aris A.Z., Yusoff F.M., Praveena S.M. Occurrence and risk assessment of multiclass endocrine disrupting compounds in an urban tropical river and a proposed risk management and monitoring framework. Sci. Total Environ. 2019;671:431–442. doi: 10.1016/j.scitotenv.2019.03.243. [DOI] [PubMed] [Google Scholar]
- 19.Zheng R.H., Fang C., Hong F.K., Kuang W.M., Lin C., Jiang Y.L., Chen J.C., Zhang Y.S., Bo J. Developing and applying a classification system for ranking the biological effects of endocrine disrupting chemicals on male rockfish Sebastiscus marmoratus in the Maowei Sea, China. Mar. Pollut. Bull. 2021;163:111931. doi: 10.1016/j.marpolbul.2020.111931. [DOI] [PubMed] [Google Scholar]
- 20.Wee S.Y., Aris A.Z., Yusoff F.M., Praveena S.M. Tap water contamination: Multiclass endocrine disrupting compounds in different housing types in an urban settlement. Chemosphere. 2021;264:128488. doi: 10.1016/j.chemosphere.2020.128488. [DOI] [PubMed] [Google Scholar]
- 21.Darbre P.D. Overview of air pollution and endocrine disorders. Int. J. Gen. Med. 2018;11:191–207. doi: 10.2147/IJGM.S102230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Plunk E.C., Richards S.M. Endocrine-disrupting air pollutants and their effects on the hypothalamus-pituitary-gonadal axis. Int. J. Mol. Sci. 2020;21:9191. doi: 10.3390/ijms21239191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rudel R.A., Perovich L.J. Endocrine disrupting chemicals in indoor and outdoor air. Atmos. Environ. 2009;43:170–181. doi: 10.1016/j.atmosenv.2008.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Teil M.J., Moreau-Guigon E., Blanchard M., Alliot F., Gasperi J., Cladière M., Mandin C., Moukhtar S., Chevreuil M. Endocrine disrupting compounds in gaseous and particulate outdoor air phases according to environmental factors. Chemosphere. 2016;146:94–104. doi: 10.1016/j.chemosphere.2015.12.015. [DOI] [PubMed] [Google Scholar]
- 25.Martín-Pozo L., Gómez-Regalado M.D.C., Moscoso-Ruiz I., Zafra-Gómez A. Analytical methods for the determination of endocrine disrupting chemicals in cosmetics and personal care products: A review. Talanta. 2021;234:122642. doi: 10.1016/j.talanta.2021.122642. [DOI] [PubMed] [Google Scholar]
- 26.Kumar M., Sarma D.K., Shubham S., Kumawat M., Verma V., Prakash A., Tiwari R. Environmental endocrine-disrupting chemical exposure: Role in non-communicable diseases. Front. Public Health. 2020;8:553850. doi: 10.3389/fpubh.2020.553850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rose M., Bennett D.H., Bergman A.K.E., Fängström B., Pessah I.N., Hertz-Picciotto I. PRDEs in 2–5 year-old children from California and associations with diet and indoor environment. Environ. Sci. Technol. 2010;44:2648–2653. doi: 10.1021/es903240g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gea M., Toso A., Schilirò T. Estrogenic activity of biological samples as a biomarker. Sci. Total Environ. 2020;740:140050. doi: 10.1016/j.scitotenv.2020.140050. [DOI] [PubMed] [Google Scholar]
- 29.Cole T.J., Flegal K.M., Nicholls D., Jackson A.A. Body mass index cut offs to define thinness in children and adolescents: International survey. Br. Med. J. 2007;335:194–197. doi: 10.1136/bmj.39238.399444.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cole T.J., Bellizzi M.C., Flegal K.M., Dietz W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. Br. Med. J. 2000;320:1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sonneveld E., Jansen H.J., Riteco J.A.C., Brouwer A., van der Burg B. Development of androgen- and estrogen-responsive bioassays members of a panel of human cell line-based highly selective steroid-responsive bioassays. Toxicol. Sci. 2005;83:136–148. doi: 10.1093/toxsci/kfi005. [DOI] [PubMed] [Google Scholar]
- 32.Schilirò T., Porfido A., Spina F., Varese G.C., Gilli G. Oestrogenic activity of a textile industrial wastewater treatment plant effluent evaluated by the E-screen test and MELN gene-reporter luciferase assay. Sci. Total Environ. 2012;432:389–395. doi: 10.1016/j.scitotenv.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 33.Wagner M., Vermeirssen E.L.M., Buchinger S., Behr M., Magdeburg A., Oehlmann J. Deriving bio-equivalents from in vitro bioassays: Assessment of existing uncertainties and strategies to improve accuracy and reporting. Environ. Toxicol. Chem. 2013;32:1906–1917. doi: 10.1002/etc.2256. [DOI] [PubMed] [Google Scholar]
- 34.Lauria L., Spinelli A., Buoncristiano M., Nardone P. Decline of childhood overweight and obesity in Italy from 2008 to 2016: Results from 5 rounds of the population-based surveillance system. BMC Public Health. 2019;19:618. doi: 10.1186/s12889-019-6946-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Castiello F., Freire C. Exposure to non-persistent pesticides and puberty timing: A systematic review of the epidemiological evidence. Eur. J. Endocrinol. 2021;184:733–749. doi: 10.1530/EJE-20-1038. [DOI] [PubMed] [Google Scholar]
- 36.Lee J.E., Jung H.W., Lee Y.J., Lee Y.A. Early-life exposure to endocrine-disrupting chemicals and pubertal development in girls. Ann. Pediatr. Endocrinol. Metab. 2019;24:78–91. doi: 10.6065/apem.2019.24.2.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li D., Zhang B., Cheng J., Chen D., Wu Y., Luo Q., Zhou L. Obesity-related genetic polymorphisms are associated with the risk of early puberty in Han Chinese girls. Clin. Endocrinol. 2022;96:319–327. doi: 10.1111/cen.14631. [DOI] [PubMed] [Google Scholar]
- 38.Bulcao Macedo D., Nahime Brito V., Latronico A.C. New causes of central precocious puberty: The role of genetic factors. Neuroendocrinology. 2014;100:1–8. doi: 10.1159/000366282. [DOI] [PubMed] [Google Scholar]
- 39.Roberts S.A., Kaiser U.B. Genetics in endocrinology genetic etiologies of central precocious puberty and the role of imprinted genes. Eur. J. Endocrinol. 2020;183:R107–R117. doi: 10.1530/EJE-20-0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Varimo T., Iivonen A.P., Känsäkoski J., Wehkalampi K., Hero M., Vaaralahti K., Miettinen P.J., Niedziela M., Raivio T. Familial central precocious puberty: Two novel MKRN3 mutations. Pediatr. Res. 2021;90:431–435. doi: 10.1038/s41390-020-01270-z. [DOI] [PubMed] [Google Scholar]
- 41.Pamplona-Silva M.T., Mazzeo D.E.C., Bianchi J., Marin-Morales M.A. Estrogenic compounds: Chemical characteristics, detection methods, biological and environmental effects. Water Air Soil Pollut. 2018;229:144. doi: 10.1007/s11270-018-3796-z. [DOI] [Google Scholar]
- 42.Santoro A., Chianese R., Troisi J., Richards S., Nori S.L., Fasano S., Guida M., Plunk E., Viggiano A., Pierantoni R., et al. Neuro-toxic and reproductive effects of BPA. Curr. Neuropharmacol. 2019;17:1109–1132. doi: 10.2174/1570159X17666190726112101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rashid H., Alqahtani S.S., Alshahrani S. Diet: A source of endocrine disruptors. Endocr. Metab. Immune Disord.-Drug Targets. 2020;20:633–645. doi: 10.2174/1871530319666191022100141. [DOI] [PubMed] [Google Scholar]
- 44.Wang Y., Zhu H., Kannan K. A review of biomonitoring of phthalate exposures. Toxics. 2019;7:21. doi: 10.3390/toxics7020021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liu Y.Y., Lin Y.S., Yen C.H., Miaw C.L., Chen T.C., Wu M.C., Hsieh C.Y. Identification, contribution, and estrogenic activity of potential EDCs in a river receiving concentrated livestock effluent in Southern Taiwan. Sci. Total Environ. 2018;636:464–476. doi: 10.1016/j.scitotenv.2018.04.031. [DOI] [PubMed] [Google Scholar]
- 46.Buckley J.P., Kim H., Wong E., Rebholz C.M. Ultra-processed food consumption and exposure to phthalates and bisphenols in the US national health and nutrition examination survey, 2013–2014. Environ. Int. 2019;131:105057. doi: 10.1016/j.envint.2019.105057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lorber M., Schecter A., Paepke O., Shropshire W., Christensen K., Birnbaum L. Exposure assessment of adult intake of bisphenol A (BPA) with emphasis on canned food dietary exposures. Environ. Int. 2015;77:55–62. doi: 10.1016/j.envint.2015.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Melough M.M., Maffini M.V., Otten J.J., Sathyanarayana S. Diet quality and exposure to endocrine-disrupting chemicals among US adults. Environ. Res. 2022;211:113049. doi: 10.1016/j.envres.2022.113049. [DOI] [PubMed] [Google Scholar]
- 49.Steele E.M., Khandpur N., da Costa Louzada M.L., Monteiro C.A. Association between dietary contribution of ultra-processed foods and urinary concentrations of phthalates and bisphenol in a nationally representative sample of the US population aged 6 years and older. PLoS ONE. 2020;15:e0236738. doi: 10.1371/journal.pone.0236738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wagner M., Oehlmann J. Endocrine disruptors in bottled mineral water: Estrogenic activity in the E- Screen. J. Steroid Biochem. Mol. Biol. 2011;127:128–135. doi: 10.1016/j.jsbmb.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 51.Duan X., Shen G., Yang H., Tian J., Wei F., Gong J., Zhang J. Dietary intake of polycyclica aromatic hydrocarbons (PAHs) and associated cancer risk in a cohort of Chinese urban adults: Inter- and intra-individual variability. Chemosphere. 2016;144:2469–2475. doi: 10.1016/j.chemosphere.2015.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yang M., Kim S., Lee E., Cheong H.-K., Chang S.-S., Kang D., Choi Y., Lee S.-M., Jang J.-Y. Sources of polycyclic aromatic hydrocarbon exposure in non-occupationally exposed Koreans. Environ. Mol. Mutagen. 2003;42:250–257. doi: 10.1002/em.10196. [DOI] [PubMed] [Google Scholar]
- 53.Franssen D., Svingen T., Lopez Rodriguez D., Van Duursen M., Boberg J., Parent A.S. A putative adverse outcome pathway network for disrupted female pubertal onset to improve testing and regulation of endocrine disrupting chemicals. Neuroendocrinology. 2022;112:101–114. doi: 10.1159/000515478. [DOI] [PubMed] [Google Scholar]
- 54.Jansen E.C., Marín C., Mora-Plazas M., Villamor E. Higher childhood red meat intake frequency is associated with earlier age at menarche. J. Nutr. 2016;146:792–798. doi: 10.3945/jn.115.226456. [DOI] [PubMed] [Google Scholar]
- 55.Chen C., Chen Y., Zhang Y., Sun W., Jiang Y., Song Y., Zhu Q., Mei H., Wang X., Liu S., et al. Association between dietary patterns and precocious puberty in children: A population-based study. Int. J. Endocrinol. 2018;2018:4528704. doi: 10.1155/2018/4528704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Eugster E.A. Update on precocious puberty in girls. J. Pediatr. Adolesc. Gynecol. 2019;32:455–459. doi: 10.1016/j.jpag.2019.05.011. [DOI] [PubMed] [Google Scholar]
- 57.Kaplowitz P., Bloch C. Evaluation and referral of children with signs of early puberty. Pediatrics. 2016;137:e20153732. doi: 10.1542/peds.2015-3732. [DOI] [PubMed] [Google Scholar]
- 58.Maione L., Bouvattier C., Kaiser U.B. Central precocious puberty: Recent advances in understanding the aetiology and in the clinical approach. Clin. Endocrinol. 2021;95:542–555. doi: 10.1111/cen.14475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhou F., Jin Z., Zhu L., Huang F., Ye A., Hou C. A preliminary study on the relationship between environmental endocrine disruptors and precocious puberty in girls. J. Pediatr. Endocrinol. Metab. 2022;35:989–997. doi: 10.1515/jpem-2021-0691. [DOI] [PubMed] [Google Scholar]
- 60.Janfaza M., Sherman T.I., Larmore K.A., Brown-Dawson J., Klein K.O. Estradiol levels and secretory dynamics in normal girls and boys as determined by an ultrasensitive bioassay: A 10 year experience. J. Pediatr. Endocrinol. Metab. 2006;19:901–909. doi: 10.1515/JPEM.2006.19.7.901. [DOI] [PubMed] [Google Scholar]
- 61.Klein K.O., Mericq V., Brown-Dawson J.M., Larmore K.A., Cabezas P., Cortinez A. Estrogen levels in girls with premature thelarche compared with normal prepubertal girls as determined by an ultrasensitive recombinant cell bioassay. J. Pediatr. 1999;134:190–192. doi: 10.1016/S0022-3476(99)70414-2. [DOI] [PubMed] [Google Scholar]
- 62.Klein K.O., Baron J., Colli M.J., McDonnell D.P., Cutler G.B. Estrogen levels in childhood determined by an ultrasensitive recombinant cell bioassay. J. Clin. Investig. 1994;94:2475–2480. doi: 10.1172/JCI117616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Larmore K.A., O’Connor D., Sherman T.I., Funanage V.L., Hassink S.G., Klein K.O. Leptin and estradiol as related to change in pubertal status and body weight. Med. Sci. Monit. 2002;8:206–211. [PubMed] [Google Scholar]
- 64.Mesa Valencia D.C., Mericq V., Corvalán C., Pereira A. Obesity and related metabolic biomarkers and its association with serum levels of estrogen in pre-pubertal chilean girls. Endocr. Res. 2020;45:102–110. doi: 10.1080/07435800.2019.1681448. [DOI] [PubMed] [Google Scholar]
- 65.Paris F., Gaspari L., Servant N., Philibert P., Sultan C. Increased serum estrogenic bioactivity in girls with premature thelarche: A marker of environmental pollutant exposure? Gynecol. Endocrinol. 2013;29:788–792. doi: 10.3109/09513590.2013.801448. [DOI] [PubMed] [Google Scholar]
- 66.Paris F., Servant N., Térouanne B., Balaguer P., Nicolas J.C., Sultan C. A new recombinant cell bioassay for ultrasensitive determination of serum estrogenic bioactivity in children. J. Clin. Endocrinol. Metab. 2002;87:791–797. doi: 10.1210/jcem.87.2.8269. [DOI] [PubMed] [Google Scholar]
- 67.Pereira A., Corvalán C., Uauy R., Klein K.O., Mericq V. Ultrasensitive estrogen levels at 7 years of age predict earlier thelarche: Evidence from girls of the growth and obesity Chilean cohort. Eur. J. Endocrinol. 2015;173:835–842. doi: 10.1530/EJE-15-0327. [DOI] [PubMed] [Google Scholar]
- 68.Wilson C.A., Heinrichs C., Larmore K.A., Craen M., Brown-Dawson J., Shaywitz S., Ross J., Oeter Klein K. Estradiol levels in girls with Turner’s syndrome compared to normal prepubertal girls as determined by an ultrasensitive assay. J. Pediatr. Endocrinol. Metab. 2003;16:91–96. doi: 10.1515/JPEM.2003.16.1.91. [DOI] [PubMed] [Google Scholar]
- 69.Gaspari L., Paris F., Jeandel C., Sultan C. Peripheral precocious puberty in a 4-month-old girl: Role of pesticides? Gynecol. Endocrinol. 2011;27:721–724. doi: 10.3109/09513590.2010.526666. [DOI] [PubMed] [Google Scholar]
- 70.Maurício R., Dias R., Ribeiro V., Fernandes S., Vicente A.C., Pinto M.I., Noronha J.P., Amaral L., Coelho P., Mano A.P. 17α-Ethinylestradiol and 17β-estradiol removal from a secondary urban wastewater using an RBC treatment system. Environ. Monit. Assess. 2018;190:320. doi: 10.1007/s10661-018-6701-8. [DOI] [PubMed] [Google Scholar]
- 71.Liu B., Xue Z., Zhu X., Jia C. Long-term trends (1990–2014), health risks, and sources of atmospheric polycyclic aromatic hydrocarbons (PAHs) in the U.S. Environ. Pollut. 2017;220:1171–1179. doi: 10.1016/j.envpol.2016.11.018. [DOI] [PubMed] [Google Scholar]
- 72.Jung E.M., Kim H.S., Park H., Ye S., Lee D., Ha E.H. Does exposure to PM10 decrease age at menarche? Environ. Int. 2018;117:16–21. doi: 10.1016/j.envint.2018.04.020. [DOI] [PubMed] [Google Scholar]
- 73.McGuinn L.A., Voss R.W., Laurent C.A., Greenspan L.C., Kushi L.H., Windham G.C. Residential proximity to traffic and female pubertal development. Environ. Int. 2016;94:635–641. doi: 10.1016/j.envint.2016.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wronka I., Kliś K. Effect of air pollution on age at menarche in polish females, born 1993–1998. Sci. Rep. 2022;12:4820. doi: 10.1038/s41598-022-08577-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bräuner E.V., Busch A.S., Eckert-Lind C., Koch T., Hickey M., Juul A. Trends in the incidence of central precocious puberty and normal variant puberty among children in Denmark, 1998 to 2017. JAMA Netw. Open. 2020;3:e2015665. doi: 10.1001/jamanetworkopen.2020.15665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kim Y.J., Kwon A., Jung M.K., Kim K.E., Suh J., Chae H.W., Kim D.H., Ha S., Seo G.H., Kim H.S. Incidence and prevalence of central precocious puberty in Korea: An epidemiologic study based on a national database. J. Pediatr. 2019;208:221–228. doi: 10.1016/j.jpeds.2018.12.022. [DOI] [PubMed] [Google Scholar]
- 77.Stagi S., De Masi S., Bencini E., Losi S., Paci S., Parpagnoli M., Ricci F., Ciofi D., Azzari C. Increased incidence of precocious and accelerated puberty in females during and after the Italian lockdown for the coronavirus 2019 (COVID-19) pandemic. Ital. J. Pediatr. 2020;46:165. doi: 10.1186/s13052-020-00931-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that supports the findings of this study are not publicly available due to privacy and ethical reasons.