Abstract
Integrin beta 7 (β7), a subunit of the integrin receptor, is expressed on the surface of immune cells and mediates cell–cell adhesions and interactions, e.g., antitumor or autoimmune reactions. Here, we analyzed, whether the stimulation of immune cells by dendritic cells (of leukemic derivation in AML patients or of monocyte derivation in healthy donors) leads to increased/leukemia-specific β7 expression in immune cells after T-cell-enriched mixed lymphocyte culture—finally leading to improved antileukemic cytotoxicity. Healthy, as well as AML and MDS patients’ whole blood (WB) was treated with Kit-M (granulocyte–macrophage colony-stimulating factor (GM-CSF) + prostaglandin E1 (PGE1)) or Kit-I (GM-CSF + Picibanil) in order to generate DCs (DCleu or monocyte-derived DC), which were then used as stimulator cells in MLC. To quantify antigen/leukemia-specific/antileukemic functionality, a degranulation assay (DEG), an intracellular cytokine assay (INTCYT) and a cytotoxicity fluorolysis assay (CTX) were used. (Leukemia-specific) cell subtypes were quantified via flow cytometry. The Kit treatment of WB (compared to the control) resulted in the generation of DC/DCleu, which induced increased activation of innate and adaptive cells after MLC. Kit-pretreated WB (vs. the control) led to significantly increased frequencies of β7-expressing T-cells, degranulating and intracellular cytokine-producing β7-expressing immune cells and, in patients’ samples, increased blast lysis. Positive correlations were found between the Kit-M-mediated improvement of blast lysis (vs. the control) and frequencies of β7-expressing T-cells. Our findings indicate that DC-based immune therapies might be able to specifically activate the immune system against blasts going along with increased frequencies of (leukemia-specific) β7-expressing immune cells. Furthermore, β7 might qualify as a predictor for the efficiency and the success of AML and/or MDS therapies.
Keywords: integrin beta 7, leukemia-derived dendritic cells, immune therapy, AML, MDS
1. Introduction
1.1. Acute Myeloid Leukemia (AML) and Myelodysplastic Syndrome (MDS)
AML and MDS are clonal stem cell disorders of hematopoiesis that lead to the uncontrolled proliferation of progenitor cells and the suppression of healthy, functional cells [1,2], going along with infections, bleeding, thrombosis and anemia [3]. Their prognosis depends on chromosomal aberrations, blast counts and patients’ ages. Standard treatment for AML/high-grade MDS is based on high-dose chemotherapy, hypomethylating agents and stem cell transplantation (SCT), leading to high rates of remission (66–90% of AML cases after 1–2 therapy cycles), however high rates of relapse have also been noted in up to 80% of cases in the following two years [4,5,6].
1.2. DC-Based Immunotherapeutic Approaches
DCs mediate immune responses via major-histocompatibility-complex (MHC)-associated antigen-presentation [7]. In vivo DCs derive from hematopoietic stem cells and monocytes and undergo an activation and maturation process in conjunction with the upregulation of cell adhesion receptors, chemokine receptors (e.g., CCR7), MHC antigens and other co-stimulatory factors [8,9,10].
DCs can be generated ex vivo from healthy monocytes or from myeloid blasts in patients with myeloid leukemia (DCleu, leukemia-derived DC-expressing individual patients’ leukemic antigens). DC/DCleu and their subtypes, e.g., DCleu, mature DC (DCmat) and mature leukemia-derived DC (DCleu-mat) (Table 1), can be generated from whole blood (WB) using selected combinations of response modifiers (e.g., GM-CSF (granulocyte macrophage colony-stimulating factor) + PGE1 (prostaglandin E1) (Kit-M) or GM-CSF+Picibanil (Kit-I)) without the induction of blast proliferation (as detected by blasts’ co-expression of transferrin receptor CD71 (Blaprol-CD71) or intracellular proliferation marker IPO38 (Blaprol-IPO38); see Table 1) [10,11,12,13].
Table 1.
Cell subpopulations.
| Group | Subgroup | Acronym | Markers | Abbrev. (Referred to Cell Fraction) | Reference |
|---|---|---|---|---|---|
| T-cells | T-cells | T | CD3+ | CD3+cells | [14] |
| Transferrin-R-positive late-proliferating T-cells | Tprol-late | CD3+CD71+ | Tprol-late/CD3+ | [14] | |
| Type II C- type lectin-positive early-proliferating T-cells | Tprol-early | CD3+CD69+ | Tprol-early/CD3+ | [14] | |
| CD4-positive T-cells | TCD4+ | CD4+CD3+ | TCD4+/CD3+ | [14] | |
| CD4-negative T-cells | TCD4− | CD4−CD3+ | TCD4−/CD3+ | [14] | |
| Non-naive T-cells | Tnon-naive | CD3+CD45RO+ | Tnon-naive/CD3+ | [15] | |
| Naive T-cells | Tnaive | CD3+CD45RO− | Tnaive/CD3+ | [15] | |
| Central memory T-cells | Tcm | CD3+CD45RO+CCR7+ | Tcm/CD3+ | [15] | |
| CD4-positive non-naive T-cells | Tnon-naiveCD4+ | CD3+CD4+CD45RO+ | Tnon-naiveCD4+/TCD4+ | [10] | |
| CD4-negative non-naive T-cells | Tnon-naiveCD4− | CD3+CD4−CD45RO+ | Tnon-naiveCD4−/TCD4− | [10] | |
| blasts | Blasts | Bla | e.g: CD15, CD34, CD65, CD117, | Bla/cells | [16] |
| Proliferating blasts | Blaprol-CD71 | CD71+Bla+DC− | Blaprol-CDl71/Bla | [17] | |
| Proliferating blasts | Blaprol−IPO38 | IPO38+Bla+DC− | Blaprol-IPO38/Bla | [17] | |
| dendritic cells | Dendritic cells | DC | CD80, CD206, CD209, CD83 | DC/cells | [12] |
| Mature DC | DCmat | DC+CCR7+ | DCmat/cells DCmat/DC |
[13] | |
| Leukemia-derived DC | DCleu | Bla+DC+ | DCleu/cells DCleu/DC DCleu/Bla |
[12] | |
| Mature leukemia-derived DC | DCleu-mat | Bla+DC+CCR7+ | DCleu-mat/cells DCleu-mat/DCleu DCleu-mat/DCmat |
[17] | |
| others | Cytokine-induced killer cells | CIK | CD3+CD56+ | CIK/cells | [10] |
| Natural killer cells | NK | CD3−CD56+ | NK/cells | [10] | |
| Monocytes | Mon | CD14+ | Mon/cells | [10] | |
| Proliferating monocytes | Monprol-CD71 | CD71+CD14+DC− | Monprol-CD71/Mon | ||
| B-cells | B | CD19+ | CD19+/cells | [10] | |
| Integrin beta 7 (β7) | β7-positive T-cells | Tβ7+ | β7+CD3+ | Tβ7+/CD3+ | [15] |
| β7-positive CIK-cells | CIKβ7+ | β7+CD3+CD56+ | CIKβ7+/CIK | ||
| β7-positive NK-cells | NKβ7+ | β7+CD3−CD56+ | NKβ7+/NK | [18] | |
| β7-positive non naive T-cells | Tnon-naiveβ7+ | β7+CD3+CD45RO− | Tnon-naiveβ7+/Tnon-naive | [15] | |
| β7-positive naive T-cells | Tnaiveβ7+ | β7+CD3+CD45RO+ | Tnaiveβ7+/Tnaive | [15] | |
| β7-positive central memory T-cells | Tcmβ7+ | β7+CCR7+CD3+CD45RO+ | Tcmβ7+/Tcm | [15] | |
| DEG | CD107a-positive β7-positive T-cells | Tβ7+107a+ | CD107a+β7+CD3+ | Tβ7+107a+/T β7+ | [19] |
| CD107a-positive β7-positive CIK-cells | CIKβ7+107a+ | CD107a+β7+CD3+CD56+ | CIKβ7+107a+/CIKβ7+ | [19] | |
| CD 107a-positive β7-positive NK-cells |
NKβ7+107a+ | CD107a+β7+CD3−CD56+ | NKβ7+107a+/NKβ7+ | [19] | |
| INTCYT | TNF alpha-positive β7-positive T-cells | Tβ7+TNFα+ | TNFa+β7+CD3+ | Tβ7+TNFα+/Tβ7+ | [20] |
| IFN gamma-positive β7-positive T-cells | Tβ7+IFNγ+ | IFNg+β7+CD3+ | Tβ7+IFNγ+/Tβ7+ | [21] |
Abbrev. cell subpopulations; marker combinations (measured by FACS) defining the different cell subpopulations.
1.3. Key Players of Immune Defense and Their Detection
Immune defense is mediated by humoral and cellular mechanisms of the innate and adaptive immune system [22,23]. The key players of the (fast-acting) innate immune system are monocytes (CD14+), macrophages (CD15+), DCs (e.g., CD206+, CD80+, etc.) as well as NK-cells (CD56+CD3−) and CIK-cells (CD56+CD3+) [13,24,25,26]. The key players of the (antigen-specific/long-lasting) adaptive immune system are B-cells (CD19+), T-cells (CD3+) and their subsets: naive or non-naive T-cells (Tnaive, CD3+CD45RO−; Tnon-naive, CD3+CD45RO+; Tnon-naiveCD4+, CD4+CD3+CD45RO+; and Tnon-naiveCD4−, CD4−CD3+CD45RO+), which give rise to central memory cells (Tcm, CD3+CD45RO+CCR7+), enabling faster reactivation of the immune system against reoccurring targets (see Table 1) [10,27,28]. These cells can be detected via flow cytometry.
Leukemia-specific/antileukemic cells can be quantified using functional analyses. The degranulation assay (DEG) detects the CD107a molecule left on the cell surface after the release of granzymes and perforins [29,30]. The intracellular cytokine assay (INTCYT) allows the intracellular quantification of cytokines (interferon gamma (IFNγ) and tumor necrosis factor alpha (TNFα)), which are considered specific triggers of the immune responses and mediators of cell apoptosis [21,30,31]. Antileukemic blast lytic effects can be detected, e.g., using a non-radioactive fluorolysis assay [13,32,33].
1.4. Integrin Beta 7 (β7)
The β7 subunit, expressed on adaptive and innate immune cells, plays an important role in cell–cell-adhesion [15,34,35] (e.g., β7-expressing T-cells (Tβ7+), Tnon-naive (Tnon-naiveβ7+), Tnaive (Tnaiveβ7+), Tcm (Tcmβ7+), NK-cells (NKβ7+)- and CIK-cells (CIKβ7+); see Table 1). β7 expressed in hematopoietic stem cells (HSC) plays a role in HSC homing [36]. β7 is primarily known for its function in T-cell-trafficking to the gut via interaction with mucosal-addressin-cell-adhesion-molecule-1 (MAdCAM-1) [35,37]. Higher β7 expression on T-cells seems to correlate with cytotoxic effects towards intestinal cells in inflammatory bowel diseases [38] and in NK-cells with higher cytotoxicity in immunodeficiency-virus-infected macaques [39]. β7 has been associated with the intraepithelial differentiation of cytotoxic as well as regulatory T-cells, and therefore, with pro- and anti-inflammatory functions [40]. In the past, higher β7 expression in T-cells could be correlated with higher antileukemic, blastolytic potential in AML samples [15].
1.5. Aim of This Study
The aim of this study was to further explore the role of β7 expression in immune cell subpopulations in uncultured peripheral WB or after mixed lymphocyte culture (MLC) of patients’ or healthy donors’ T-cell-enriched cells with Kit-pretreated WB as stimulator cells.
In detail, we explored:
DC subpopulations using (Kit-treated vs. untreated) WB from leukemia patients (or healthy individuals);
(β7-expressing) innate and adaptive immune cells before and after MLC with Kit-pretreated vs. untreated WB from leukemia patients (or healthy individuals);
The antileukemic activity of cells using the cytotoxicity fluorolysis assay (CTX) after MLC of patients’ T-cells with Kit-pretreated vs. untreated WB as stimulator cells;
Leukemia-specific cells using DEG and INCYT assays in uncultivated WB from leukemia patients (vs. comparable cells for healthy individuals) and after MLC with Kit-pretreated vs. untreated WB;
The correlations between antileukemic functionality, leukemia-specific activity and (β7-expressing) immune cells;
The correlations between patients’ clinical outcomes/prognostic risk assessment and (β7-expressing) immune cells.
2. Results
We further explored the role of β7-expressing (leukemia-specific) immune-reactive cell populations as prognostic markers to predict the clinical outcome, as well as to mediate antileukemic functionality after stimulation. Therefore, we studied the expression of β7 on uncultured immune-reactive cells from AML patients and healthy blood donors (as a control), generated DC/DCleu from healthy and leukemic samples and studied their potential to activate (β7-expressing) immune-reactive cells after T-cell-enriched MLC.
2.1. Generation of DC (Subtypes) from WB
2.1.1. Significantly Higher Frequencies of DCs and Their Subtypes in Patients’ and Healthy WB Samples after Kit Treatment Compared to Control (without Added Kits)
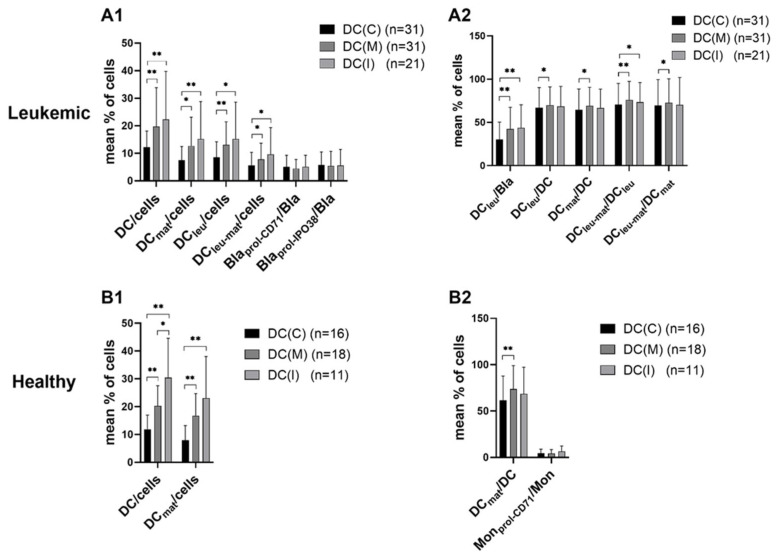
We found significantly higher frequencies of DC/DCleu subtypes under the influence of Kit-M (DC(M)) or Kit-I (DC(I) compared to the control (DC(C) in healthy or AML patients’ samples (e.g., %DC/cells, Figure 1A1,B1). Moreover, in AML samples, frequencies of (mature) DCleu were significantly increased compared to the control (Figure 1A1,A2).
Figure 1.
Generation of DC/DCleu from (A1) leukemic and (B1) healthy WB with and without Kits. WB samples were cultured for 7 days with Kit-M or Kit-I or without added Kits as control. Results with Kit-M (DC(M)) or Kit-I (DC(I)) or without added Kits as control (DC(C)) are given. Mean frequencies ± standard deviation of DC subtypes in (A2) leukemic (AML/MDS) and (B2) healthy samples are given; n—number of cases. Differences were considered as significant (*) when p ≤ 0.05 and as highly significant (**) when p ≤ 0.005. Abbreviations of cell subpopulations are given in Table 1.
2.1.2. No Influence of Kit Treatment on Proliferation of Blasts or Monocytes
The frequencies of proliferating blasts (Blaprol-CD71, Blaprol-IPO38; Figure 1A1) were comparable in Kit-treated patients’ WB and that of the control. Moreover, the frequencies of proliferating monocytes (Monprol-CD71; Figure 1B2) were comparable in Kit-treated healthy donors’ WB and that of the control.
In summary, we found higher frequencies of DCs and their subtypes (DCleu, DCmat and DCleu-mat) in Kit-treated WB when compared to the control. The (DC-independent) proliferation of blasts and monocytes was not induced.
2.1.3. Profiles of Immune-Reactive (and Especially β7-Expressing) Cells in Uncultured WB from AML vs. Healthy Blood Donors
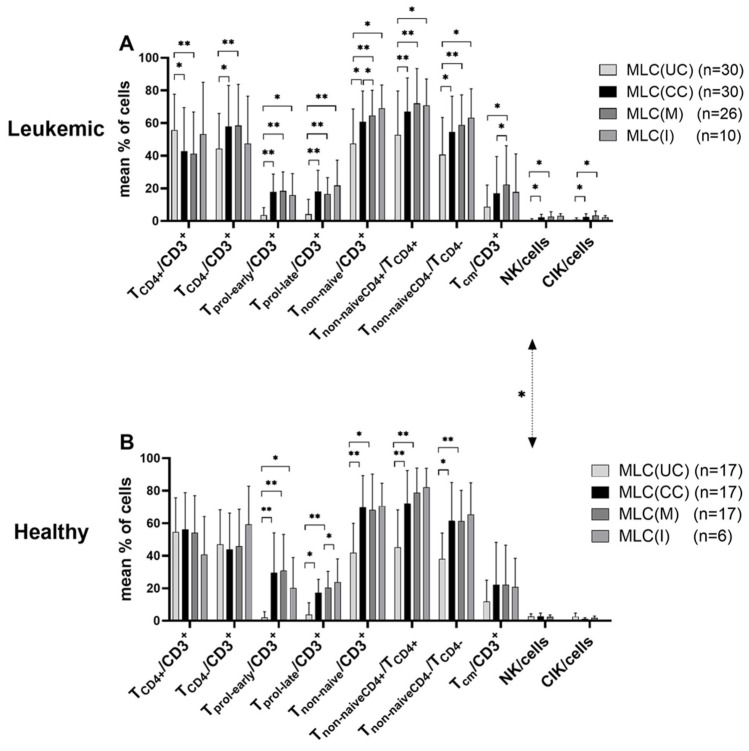
Low frequencies of proliferating T-cells (Tprol-early/CD3+, Tprol-late/CD3+), Tcm/CD3+ and innate immune cells were found in uncultured AML as well as in healthy samples. Significantly higher frequencies of NK-cells were found in (uncultured) healthy vs. AML WB samples (Figure 2, MLC(UC)).
Figure 2.
Composition of immune-reactive cells before and after T-cell-enriched MLC using (A) leukemic and (B) healthy WB with or without Kit pretreatment. Cells were analyzed via flow cytometry before and after 7 days of (T-cell-enriched) MLC with Kit-pretreated or untreated WB and IL-2. Cells before MLC from WB without added Kits as control (MLC(UC)), and cells after MLC, from WB pretreated with Kit-M (MLC(M)), Kit-I (MLC(I)) or without added Kits as control (MLC(CC)), are given. Mean frequencies ± standard deviation of immune-reactive cell subpopulations in (A) leukemic (AML/MDS) and (B) healthy samples are given; n—number of cases. Differences were considered as significant (*) when p ≤ 0.05 and as highly significant (**) when p ≤ 0.005. Double-sided arrows give (significant) differences between defined healthy and leukemic immune-reactive cell subtypes. Abbreviations of cell subpopulations are given in Table 1.
Between 18 and 22% of T-cell (subtypes, e.g., Tnaive/Tnonnaive/Tcm) and even higher frequencies of innate cells co-expressed β7. The differences in β7 expression were significantly lower in uncultured leukemic vs. healthy T-cells (Figure 2A vs. Figure 2B, MLC(UC)).
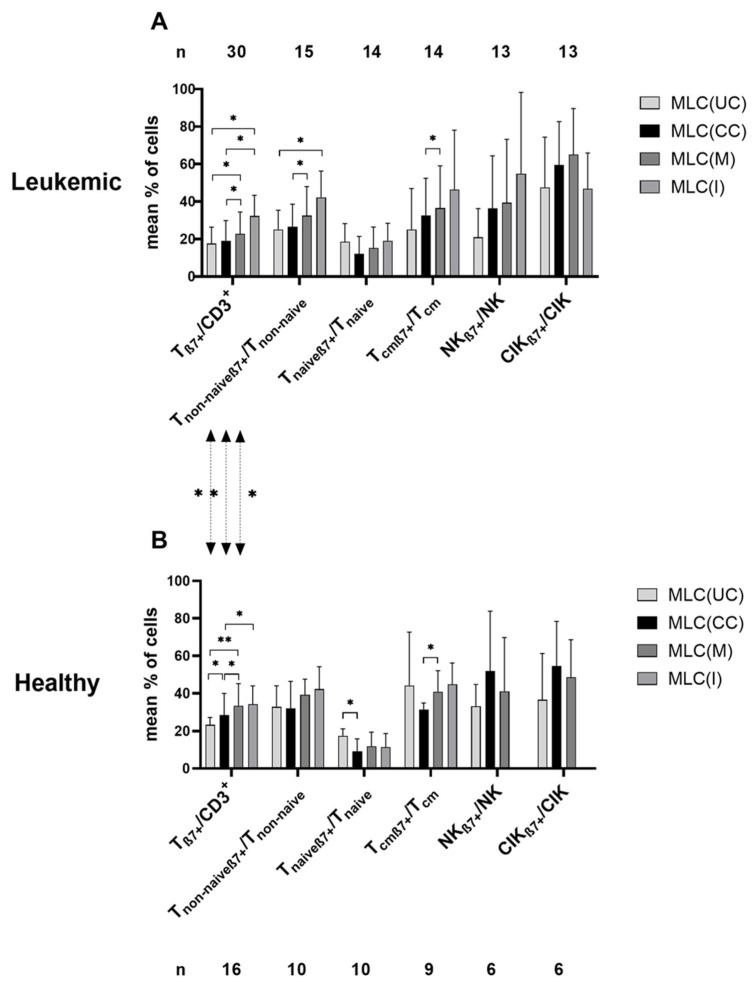
Comparing the expression profiles before vs. after T-cell-enriched MLC (using Kit pretreated (or untreated) patients’ or healthy donors’ WB as stimulator cells), we found higher frequencies of activated/proliferating/CD4− T-cells (e.g., Tnon-naive/CD3+ (and TnonnaiveCD4+/TCD4+ and Tnon-naiveCD4−/TCD4−) and TCD4−/CD3+) within patients’ and healthy samples, as well as higher frequencies of CIK/cells and NK/cells (within patients’ samples) after MLC compared to before (Figure 2). Higher frequencies of β7-expressing immune-reactive cell subpopulations (except for Tnaiveβ7+) were found after MLC compared to before (Figure 3).
Figure 3.
Composition of β7-expressing immune-reactive cells before and after T-cell-enriched MLC using (A) leukemic and (B) healthy WB with and without Kit pretreatment as stimulator cells. Cells were analyzed via flow cytometry before and after 7 days of (T-cell-enriched) MLC with Kit-pretreated or untreated WB and IL-2. Cells before MLC from WB without added Kits as control (MLC(UC)), and cells after MLC, from WB pretreated with Kit-M (MLC(M)), Kit-I (MLC(I)) or without added Kits as control (MLC(CC)), are given. Mean frequencies ± standard deviation of immune-reactive cell subpopulations in (A) leukemic (AML/MDS) and (B) healthy samples are given; n—number of cases. Differences were considered as significant (*) when p ≤ 0.05 and as highly significant (**) when p ≤ 0.005. Double-sided arrows give (significant) differences between defined healthy and leukemic immune-reactive cell subtypes. Abbreviations of cell subpopulations are given in Table 1.
2.2. T-Cell-Enriched Mixed Lymphocyte Culture with Patients’ or Healthy Donors’ Kit-Pretreated (vs. Untreated) WB
2.2.1. Significant Activation and Provision of T-Cells after MLC of Patients’ WB, but Not in Healthy Samples with Kit-Pretreated (vs. Untreated) WB
Comparing the influence of Kit treatment (vs. without) on the composition of immune-reactive cells in patients’ samples, we found significantly higher frequencies of Tnon-naive and Tcm after MLC(M) compared to MLC(CC) (e.g., %Tnon-naive/CD3+: MLC(M) vs. MLC(CC), p ≤ 0.05; and %Tcm/CD3+: MLC(M) vs. MLC(CC), p ≤ 0.05), whereas the frequencies of innate cells were not significantly different (Figure 2A).
No significantly different frequencies of T- or innate cells were found after MLC(M) or MLC(I) vs. the control (MLC(CC) in healthy samples) (Figure 2B).
2.2.2. Significantly Increased Provision of β7-Expressing Immune-Reactive Cells after MLC with Kit-Pretreated Patients’ or Healthy WB Compared to Control (MLC(CC))
After MLC of Kit-treated (vs. untreated) patients’ WB, we found higher frequencies of β7-expressing T-cell subpopulations after MLC(M), e.g., β7-expressing Tcm in the Tcm fraction (% Tcmβ7+/Tcm: MLC(M): 36.58 ± 22.57, p ≤ 0.05; MLC(CC): 32.74 ± 19.72)). The frequencies of β7-expressing T-cell subpopulations were comparable after MLC(M) and MLC(I). No differences between MLC(M), MLC(I) and MLC(CC) were found in β7-expressing innate immune-reactive cells (Figure 3A).
After MLC of Kit-treated (vs. untreated) healthy donors’ WB, we found significantly higher frequencies of Tβ7+ and Tcmβ7+ after MLC(M) and MLC(I) and significantly increased frequencies of Tβ7+/CD3+ compared to MLC(CC) (e.g., %Tβ7+/CD3+: MLC(M): 33.56 ± 11.62, p ≤ 0.05; MLC(CC): 28.54 ± 11.41). The frequencies of β7-expressing cells after MLC(M) and MLC(I) were comparable. No differences could be found in β7-expressing innate immune cells (Figure 3B).
In healthy (compared to patients’) samples, we found significantly higher frequencies of Tβ7+ cells with MLC(UC), MLC(CC) and MLC(M) (p ≤ 0.05, Figure 3).
In summary, Kit-treated (vs. untreated) patients’ WB led to higher frequencies of β7-expressing T-cell subtypes, with an induction of non-naive and memory β7-expressing T-cells after MLC. Higher frequencies of β7-expressing T-cell subtypes were found in healthy donors’ (vs. patients’) samples.
2.2.3. Detection of Antigen-Specific (Degranulating or Intracellularly IFNγ-Producing) β7+ Immune-Reactive Cells in Uncultured WB from AML and Healthy WB Donors or in Immune-Reactive Cells after T-Cell-Enriched MLC
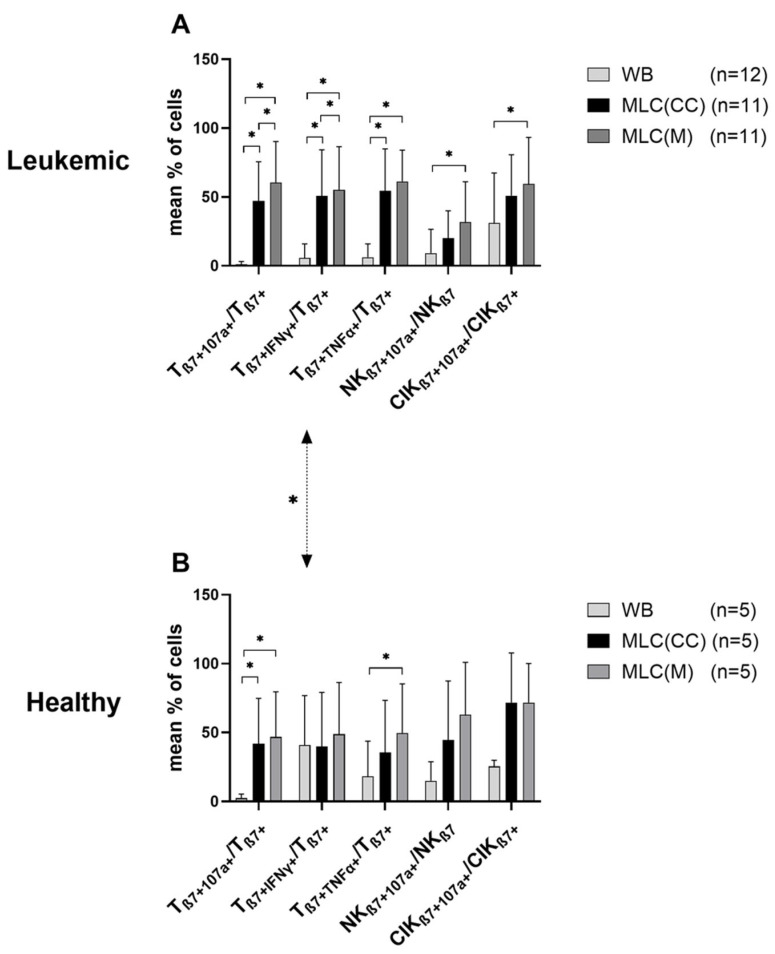
We found low frequencies of antigen-specific degranulating or intracellularly IFNγ-producing immune-reactive cells in uncultured WB from AML and healthy WB donors. Significantly higher frequencies of Tβ7 +IFNγ+/Tβ7+ were found in uncultured healthy WB samples compared to AML WB samples (Figure 4). (Non-significantly) higher frequencies of these antigen-specific cells were found after stimulation with LAA (in AML samples) and with SEB (in healthy samples). Here, we present data without antigen stimulation.
Figure 4.
Composition of β7-expressing degranulating or intracellular cytokine-producing immune-reactive cells in uncultivated WB and after T-cell-enriched MLC using (A) leukemic and (B) healthy WB with or without Kit pretreatment as stimulator cells. Degranulation and intracellular cytokine production were quantified via flow cytometry in untreated and uncultivated WB as well as after 7 days of (T-cell-enriched) MLC with Kit-pretreated or untreated WB and IL-2. Results without LAA or SEB stimulation are given. Uncultivated cells in WB and cultivated cells after MLC from WB pretreated with Kit-M (MLC(M)) or without added Kits as control (MLC(CC)) are given. Mean frequencies ± standard deviation of immune-reactive cell subpopulations in (A) leukemic (AML/MDS) and (B) healthy samples; n—number of cases. Differences were considered as significant (*) when p ≤ 0.05. Double-sided arrows give (significant) differences between defined healthy and leukemic immune-reactive cell subtypes. Abbreviations of cell subpopulations are given in Table 1.
We found significantly increased frequencies in most of antigen-specific (TNFα- or IFNγ-producing or degranulating) T-cell or innate β7-expressing cell types before vs. after MLC (using Kit pretreated (vs. untreated) patients’ or healthy donors’ WB as stimulator cells (e.g., Tβ7 +IFNγ+/Tβ7+ in WB vs. MLC(CC) or WB vs. MLC(M)). This effect was especially evident within patients’ samples, but was also found in healthy samples.
We found significantly higher frequencies of Tβ7+107a+ and Tβ7+IFNγ+ after MLC(M) compared to MLC(CC) in patients’ samples without LAA stimulation (%Tβ7+107a+/Tβ7+: MLC(M): 60.62 ± 29.62, p ≤ 0.05; MLC(CC): 47.15 ± 28.39; Tβ7 +IFNγ+/Tβ7+: MLC(M): 55.24 ± 31.35, p ≤ 0.05; MLC(CC): 50.83 ± 33.50). The frequencies of Tβ7+TNFα+ and of NKβ7+107a+ and CIKβ7+107a+ were comparable after MLC(M) and MLC(CC) (Figure 4A). In patients’ samples with additional LAA stimulation, the degranulation and intracellular cytokine production after MLC(M) and MLC(CC) were comparable (data not shown).
We were able to find (non-significantly) higher frequencies of Tβ7+107a+ and NKβ7+107a+ after MLC(M) compared to MLC(CC) in healthy samples without SEB stimulation (Figure 4B). In healthy samples with additional SEB stimulation, the degranulation and intracellular cytokine production of cells after MLC were comparable (data not shown).
We found comparable frequencies of degranulating or cytokine-producing β7+ immune cells in healthy compared to patients’ samples (Figure 4A vs. Figure 4B).
In summary, we found an induction of degranulating and intracellular cytokine-producing β7+ T-, NK and CIK-cells after MLC using Kit-pretreated WB compared to the control. We also found more degranulation and intracellular cytokine production in healthy donors’ (vs. patients’) samples.
2.2.4. Improved Antileukemic and Blastolytic Functionality of Immune Cells after T-Cell-Enriched MLC with Kit-M-Pretreated (vs. Untreated) WB
We compared the achieved blast lysis (‘lysis’) of MLC(CC), MLC(I) and MLC(M) using the cytotoxicity fluorolysis assay after the co-cultivation of effector (T-cell-enriched MLC stimulated with Kit-pretreated or untreated WB) and target (blast-containing MNC) cells. We quantified the frequencies of viable blasts after 3 and 24 h of incubation time and selected the superior antileukemic effectivity after either 3 or 24 h incubation time as a ‘best of’ value.
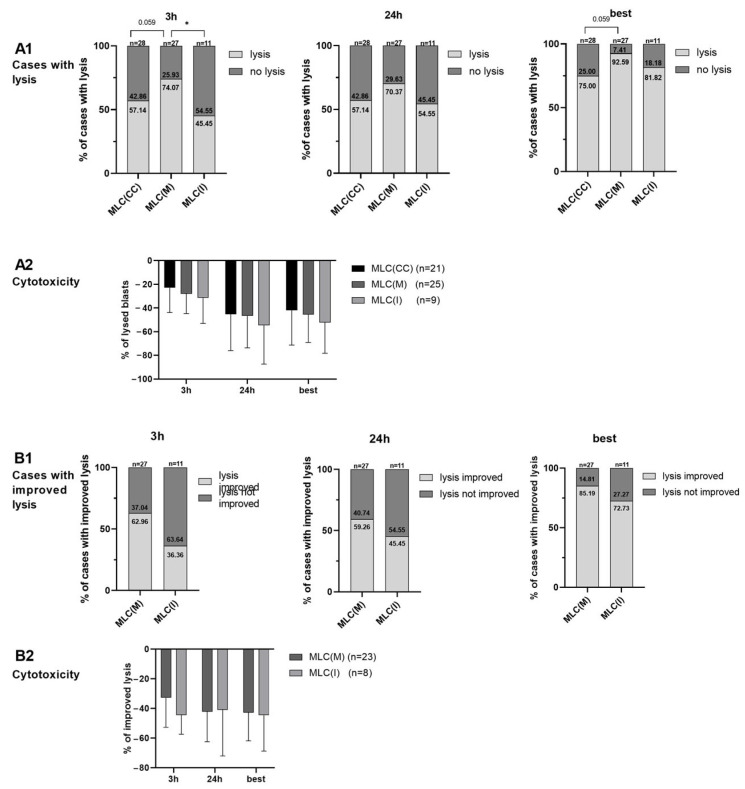
After 3 (24) h of incubation of effector with target cells, blast lysis was found in 74.07 (70.37)% of cases after MLC(M) compared to 57.14 (57.14)% after MLC(CC) and 45.45 (54.55)% after MLC(I) (Figure 5A1), with comparable frequencies of blast lysis after MLC(M), MLC(I) and MLC(CC) in cases with achieved lysis (Figure 5A2). After 3 h of incubation of effector with target cells, we found nearly significantly more cases with lysis after MLC(M) compared to MLC(CC) ((p = 0.059). Figure 5A1). Improved lysis (compared to MLC(CC)) was found in 62.96 (59.26) % of cases after MLC(M) vs. in 36.36 (45.45) % after MLC(I) (Figure 5B1), going along with comparable frequencies after MLC(M) and MLC(I) (compared to MLC(CC)) in cases with improved lysis (Figure 5B2).
Figure 5.
Blastolytic potential of immune-reactive cells after T-cell-enriched MLC using leukemic WB with and without Kit pretreatment as stimulator cells. For the cytotoxicity assay, target and effector cells were coincubated for a total of 24 h. Results after 3 h and 24 h and the ‘best of’ values after coincubation are given. Results after MLC from WB pretreated with Kit-M (MLC(M)) or Kit-I (MLC(I)) or without added Kits as control (MLC(CC)) are given. Percentages of cases (A1) with achieved (vs. non-achieved) blast lysis and (B1) with improved (vs. non-improved) blast lysis are given. Mean frequencies ± standard deviation of (A2) lysed blasts (in cases with lysis) and (B2) lysis improvement (in cases with improved lysis) are given; n—number of cases. Differences were considered as significant (*) when p ≤ 0.05. Abbreviations of cell subpopulations are given in Table 1.
Selecting the best achieved lysis after 3 and 24 h of incubation of effector with target cells (best), we found nearly significantly more cases with lysis after MLC(M) compared to MLC(CC) ((p = 0.059). Figure 5A1). Frequencies of lysed blasts after MLC(M), MLC(I) and MLC(CC) in cases with achieved lysis were not significantly different (Figure 5A2). After MLC(M) vs. MLC(I) (compared to MLC(CC)), blast lysis could be improved in 85.19% of cases after MLC(M) and in 72.73% of cases after MLC(I) (Figure 5B1), going along with the comparable frequencies of lysis improvement after MLC(M) and MLC(I) (compared to MLC(CC)) in cases with improved lysis (Figure 5B2).
In summary, Kit-M treatment indicates clearly (although not significantly) improved blast lysis after MLC when compared to the control in our patient cohort.
2.3. Correlation of (Antigen-Specific) β7 Expression with Patients’ Allocation to Risk Groups, Response to Induction Chemotherapy and Achieved Antileukemic (Ex Vivo) Functionality
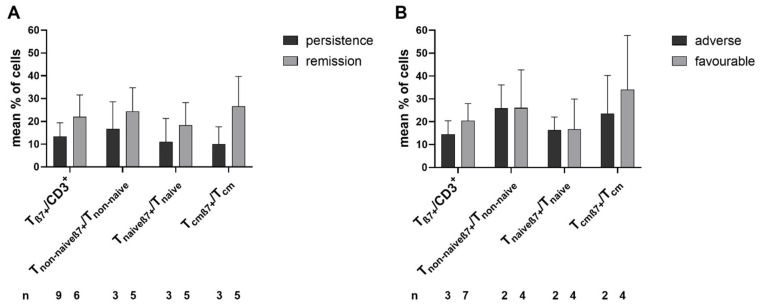
We compared the β7 expression in T-cells and their subtypes in uncultured immune cells in the samples from AML patients at first diagnosis with allocation to the ELN risk groups and response to induction chemotherapy. Patients who achieved (n = 6, vs. those who did not achieve (n = 9)) remission were characterized by clear, although non-significantly higher frequencies of Tβ7+ cells. In patients with favorable (n = 7) vs. adverse ELN risk stratification (n = 3), clear, although non-significantly higher frequencies of Tcmβ7+/Tcm were found (Figure 6A,B).
Figure 6.
Composition of uncultivated β7-expressing immune-reactive cells in AML patients’ samples with patients subdivided into different groups at first diagnosis. Uncultured cells (MLC(UC)) were analyzed via flow cytometry. Mean frequencies ± standard deviation of β7-expressing immune-reactive cell subpopulations in patients with AML at first diagnosis with respect to patients’ (A) responses to chemotherapy and (B) allocation to cytogenetic ELN risk groups are given; n—number of cases. Abbreviations of cell subpopulations are given in Table 1.
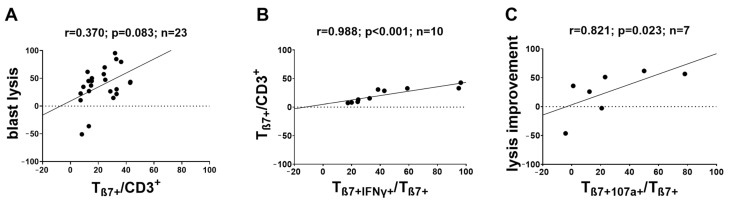
We correlated the degranulation and intracellular cytokine production (frequencies of (leukemia-specific) β7-expressing immune-reactive cells) with (improved) antileukemic functionality after MLC. We found a clear (although not significant) positive correlation between Tβ7+/CD3+ after Kit-M pretreatment and improved blast lysis in MLC(M) (but not in MLC(I)) (compared to MLC(CC)) (r = 0.370; p = 0.083) (Figure 7A). We found significant, positive correlations between the frequencies of β7-expressing cells and the frequencies of intracellular cytokine-producing β7-expressing cells (Tβ7+IFNγ+: r = 0.988, p < 0.001; Tβ7+TNFα+: r = 0.952, p < 0.001) in MLC(M) (Figure 7B). We also found a positive correlation between increased frequencies of Tβ7+107a+ and lysis improvement (r = 0.821; p = 0.023) (Figure 7C) with the blastolytic functionality and frequencies of β7-expressing cells.
Figure 7.
Correlations of antileukemic functionality with frequencies of (leukemia-specific) β7-expressing immune-reactive cells before and after T-cell-enriched MLC using Kit-M-pretreated (vs. untreated as control) leukemic WB as stimulator cells. Cells were analyzed via flow cytometry before and after 7 days of (T-cell-enriched) MLC with Kit-pretreated or untreated WB and IL-2. Results of uncultured cells before MLC (MLC(UC)), and cells after MLC, from WB pretreated with Kit-M (MLC(M)) or without added Kits as control (MLC(CC)), are given. Lysis (improvement) is given as the best of value after MLC(M) (compared to MLC(CC)). (A) Clear positive correlation of frequencies of Tβ7+/CD3+ with best blast lysis after MLC (with Kit-M-pretreated leukemic WB). (B) Significant positive correlation of frequencies of Tβ7+/CD3+) with Tβ7+IFNγ+/Tβ7+ after MLC (with Kit-M-pretreated leukemic WB. (C) Significant positive correlation of frequencies of Tβ7+107a+/Tβ7 with improved blast lysis after MLC (with Kit-M-pretreated leukemic WB). r—correlation coefficient, p—significance, n—number of cases. Differences were considered as significant when p ≤ 0.05 and as highly significant when p ≤ 0.005. Abbreviations of cell subpopulations are given in Table 1.
In summary, Kit treatment of WB led to the increased generation of DC subtypes (DC, DCleu, DCmat and DCleu-mat), to activated immune cells and to increased frequencies of β7-expressing cells compared to the control. Additionally, Kit treatment led to increased frequencies of degranulating and intracellular cytokine-producing β7-expressing immune cell (subtypes). Finally, (partly significant) we saw positive correlations of β7-expressing immune cell (subtypes) with the provision of leukemia-specific/antileukemic cells after T-cell-enriched MLC, with patients’ responses to chemotherapy or with their allocations to risk types in our small patient cohort.
3. Discussion
Expressions of several leukemia-associated antigens (e.g., CD318 and CD11b) have been studied via flow cytometry to determine their value in classifying the disease and to monitor (residual) leukemic cells [41,42]. The evaluation of (leukemia-specific) immunoreactive cells has been shown to further contribute to evaluating therapy efficiency, to quantifying antileukemic reactions and to improving therapy options and prognoses [43,44].
3.1. DC-Based Therapies as Promising Therapy Options
Due to their ability to mediate innate and the adaptive immune response, DCs’ and DCleus’ therapeutic potential has been widely recognized [5,6,7,9]; DC vaccinations with monocyte-derived DCs, as well as DCleu converted from patients’ myeloid blasts, have shown immunological effects in vivo [9,10,45,46].
3.2. Improved Activation of the Adaptive and Innate Immune System with Kit-Treated WB
3.2.1. Ex Vivo DC Generation and (Antileukemic) Immune Cell Activation
DC (subtypes) from healthy as well as patients’ WB samples can be generated in the presence of Kits (compared to controls) [10,27,47,48] (Figure 1). Combinations of GM-CSF and PGE1 (Kit-M) or GM-CSF and Picibanil (Kit I), added to healthy/leukemic whole blood, use the soluble microenvironment in WB (containing, e.g., cytokines and chemokines) as an additional source for response modifiers to generate DC/DCleu. Both Kits provide danger signaling combined with maturation signaling, which guide cells’ differentiation towards DC or DCleu, respectively, as published before [10,48]. The detailed functional pathways of (PGE1-/Picibanil-containing) DC-generating methods are not known. The induction of monocyte or blast proliferation was not seen, thereby indicating that Kits do not induce blast or monocyte proliferation; however, they give rise to significantly increased frequencies of leukemia- or monocyte-derived, mature DC, as already shown [10,11] (Figure 1). According to our findings (also confirmed here), we can deduce that Kit-M might trigger, with higher efficacy, improved/mediated antileukemic reactions compared to Kit I. Moreover, we show that the achieved antileukemic activities (achieved using patients’ samples at first diagnosis) are independent of patients’ sex, cytogenetic risk and blast counts (patients with leukemia in remission might profit from these Kit-mediated effects; (residual) blasts are converted to DCleu and trigger the immune system specifically against blasts). This has to be proven in a clinical trial [17,21].
Furthermore, we confirm that adaptive and innate immune cells from healthy and patients’ samples pretreated (vs. not pretreated) with Kits were regularly (significantly) activated after MLC, giving rise to (significantly) increased frequencies of activated cells of the innate and adaptive immune system in AML samples, pointing to Kit-mediated activation of immune cells and the generation of memory cells (Figure 2), as shown before [9,10,11,21,27,30,48]. We also found higher frequencies of activated immune-reactive cells in healthy (compared to patients’) samples, as already shown [27], possibly pointing to immunological activation against various bacterial, viral or mycotic targets [49,50] (Figure 2). Compared to uncultured cells, activation of immune cell subtypes after MLC was seen, due to the influence of IL-2, as expected [51] (Figure 2 and Figure 3).
3.2.2. Higher β7 Expression in Immune Cells after MLC with Kit-I and Kit-M Treatment of Healthy and Patients’ WB Samples
β7 expression in uncultured T-cells has already been shown to correlate with cell cytotoxicity against leukemic (blasts) and other (intestinal/intraepithelial cells) targets [15,38,39,40]. We found that healthy donors’ samples showed significantly higher frequencies of β7 in T-cells compared to patients’ samples before cultivation, as well as in cells after culture (control, Kit-M) (Figure 3); this confirms the findings of Vogt et al. obtained before/after MLC with blast-containing MNC pretreated using DC-generating methods (MCM-Mimic, Picibanil and Ca-Ionophore) as stimulator cells [15]. These increased frequencies of β7 expression in healthy cells compared to those of patients might indicate a detrimental effect of leukemic immunosuppression on β7 expression in immune cells [49]. Moreover, our data show (significantly) increased frequencies of β7-expressing CD3+, Tnon-naive and Tcm in healthy and patients’ samples after MLC with Kit-M- and Kit-I-pretreated (vs. control) WB (Figure 3). These data might indicate the involvement of β7-expressing immune cells in immune functionality in healthy as well as patients’ samples (Figure 3).
Comparing the DC-generating potential of Kit-I and Kit-M, we found higher frequencies of DC after Kit-I treatment in healthy samples and lower frequencies of DCleu in patients’ samples. This might point to lower efficiency of Kit-I in generating functional DC (Figure 1). These results confirm the unpublished data of Ugur et al. [17], who also showed lower functionality compared to Kit-M.
3.2.3. Increased Production of (Antigen-Specific) Degranulating or Intracellular Cytokine-Producing Immune Cells after MLC of Kit-M-Pretreated Healthy and Patients’ WB Samples
According to their biological function, DCs can help to overcome the anergy of immune-reactive cells and prime effector cells against their targets. Efficacy can (and has to) be demonstrated by induced/increased immune-reactive cells and decreased blast counts. (Functional) specific effects, mediated by DC/DCleu have to be quantified (compared to controls). In the case of DC (loaded with tumor antigens) or DCleu, their capability to activate the immune system specifically against leukemic cells has to be evaluated after (T-cell-enriched) mixed lymphocyte culture (MLC) using DC/DCleu as stimulator cells. The assays to detect leukemia-specific activations are cytokine secretion assays, degranulation assays, intracellular cytokine assays, ELISPOT, TETRAMER, etc. [52]. Adding leukemia-associated antigens (e.g., WT1 and PRAME) to cultures with/without the cultivation of cells can help to detect/enrich low frequencies of specific cells [21,30,53].
DEG und INTCYT assays are useful for demonstrating the antigen-specific activation of immunoreactive cells by measuring cell degranulation and intracellular cytokine production (with and without stimulation with LAA) [21,30]. We already showed significant activation of antigen-specific degranulating or intracellularly cytokine-producing innate and adaptive immune cells after MLC with Kit-M-pretreated (vs. untreated) WB (and low frequencies in uncultured cells) [21,30]. Studying β7-expressing immune cells, we observed higher frequencies of degranulating β7-expressing T- and NK-cells, CIK-cells and intracellularly cytokine-producing T-cells (in healthy and/or patients’ samples) after MLC(M) (compared to the control) (Figure 4A,B), with higher frequencies in healthy compared to patients’ samples (Figure 4A,B). Together with the findings after the Kit-M-mediated MLC of increased β7 expression, this might indicate (specific) involvement of these cells in immune reactivation, in healthy as well as in AML patients.
While the addition of LAA (to patients’ samples) or SEB (to healthy samples) antigen stimulation [21,29] led to higher frequencies of antigen-specific cells, especially in uncultured cell samples, it did not significantly enhance the Kit-M-mediated effects after MLC with respect to induced antigen-specific cells compared to the control (data not shown). This confirms the previous data, which show that Kit-M pretreatment of WB (going along with the generation of DC) stimulates and activates immune-reactive cells and compensates for LAA- or SEB-triggered activating effects [21].
In principle, the induction of leukemia-specific cells can be also detected in vivo by applying the methods given above [54]. Several groups have shown that AML patients treated with DC/DCleu showed significant induction of (leukemia-specific) cellular and humoral immunity, going along with reduced blasts and prolonged overall survival (e.g., [54,55,56,57,58,59], all cited in [52]). Depending on the methods used, significant induction of the leukemia-specific immune response was defined as a 25 (50)% increase in the frequency of leukemia-specific cells compared to the initial count, or significantly higher frequencies of induced specific cells compared to untreated controls (e.g., [55,60,61]).
3.2.4. Increased Blastolytic Functionality of Immune-Reactive Cells in Kit-Pretreated Samples after MLC
The hardest proof of induced or improved antileukemic activity (compared to controls) is the detection of improved blast lysis compared to the controls (e.g., after MLC). This can be achieved via chrome release, fluorolysis or other assays [62]. The Kit pretreatment of blasts in WB has already been shown to improve the antileukemic activation of immunoreactive cells after MLC, going along with significantly increased blast lysis compared to the controls [11,17,21,30,48].
Here, we found (nearly significantly) more cases with a superior blastolytic effect of immune-reactive cells after MLC(M) compared to the control (p = 0.056). Kit-I pretreatment was less effective compared to Kit-M pretreatment in giving rise to improved blastolytic functionality of the immune-reactive cells (Figure 5).
Blast lysis was, for some cases, superior after 3 h of incubation of target with effector cells, and for other cases, after 24 h. These effects could be attributed to different, independent blastolytic mechanisms, namely the faster perforin/granzyme pathways (leading to blast lysis predominantly after 3 h of coincubation of target with effector cells) and the slower Fas/FasL pathways (leading to blast lysis predominantly after 24 h of coincubation of target with effector cells) [17,21,63].
Summarizing the blastolytic effects achieved (after 3 h or 24 h of coincubation of effector with target cells), our data support previous data, which show that the Kit-M pretreatment of WB improves the blastolytic activity of immunoreactive cells in cell cultures [17,21].
3.3. Potential of β7 Monitoring
3.3.1. β7 Expression in Immune-Reactive Cells as a Clue to Higher Susceptibility to Chemotherapy and Kit Treatment
Compared to patients with AML/MDS, the frequencies of β7-expressing cells were higher in healthy donors with a healthy immune system, unaffected by the immunosuppressive effect of neoplastic cells [50,64]. Generally, although the differences were not significant due to low case numbers, AML patients at first diagnosis who achieved (vs. those who did not achieve) leukemia remission after induction chemotherapy presented with higher frequencies of β7-expressing immune cell subtypes in uncultured WB samples; moreover, patients’ assignment to the favorable vs. adverse cytogenetic risk group went along with higher frequencies of β7+ Tcm in uncultured patients’ WB (Figure 6). This could point to an influence of β7-expressing cells in contributing to a healthy functional immune system [15,38,40].
3.3.2. β7 Expression as a Marker for Improved Blast Cytotoxicity
We were able to find positive correlations of achieved blast lysis with frequencies of β7-expressing cells after MLC(M). These results confirm previous findings that showed higher blastolytic cytotoxicity in samples with higher frequencies of β7 expression using different (Kit-independent) DC-generating methods, and could also point to involvement of β7 expression in the mediation of superior blastolytic functionality in immune cells [15]. In addition, the improved blast lysis correlated positively with the increased degranulation activity (Figure 7C), which further demonstrates the antileukemic potential of these Kit-induced β7-expressing immune cells and the enhancing effect of Kit-M pretreatment on antileukemic functionality. Similar correlations could also be found for cells after MLC (Ugur [17] and personal communication; publication in preparation).
Possible correlations of β7 expression with cytotoxicity have been discussed in the context of autoimmune processes [38,40]. In the case of malignant diseases such as AML, it was hypothesized that a correlation between β7 expression and cell toxicity might have potential as a marker indicating the antileukemic functionality of immune cells [15]. This hypothesis could be further supported by our finding that β7 expression also correlated with more pronounced antileukemic intracellular cytokine production of β7-expressing cells after MLC(M) (Figure 7B) (which also correlated with higher antileukemic functionality, as shown before [21]).
We can state that the Kit-M-induced activation of immune cells after T-cell-enriched MLC goes along with increased β7 expression in (leukemia-specific) immune cells and correlates with improved antileukemic activity.
4. Materials and Methods
4.1. Patients and Healthy Sample Acquisition
Heparinized peripheral WB samples (provided by the university hospitals of LMU in Munich, Augsburg, Oldenburg and Tuebingen, as well as the Rotkreuzklinikum in Munich) were taken from patients diagnosed with acute myeloid leukemia (AML) or myelodysplastic syndrome (MDS) and healthy volunteers. Patients’ consent was given according to Helsinki guidelines and the vote of the Ethics Committee of LMU in Munich (vote number: 33905).
We included 31 patients with AML or MDS in acute stages of disease and 18 healthy volunteers (as given in Table 2). Patient age at sample acquisition was, on average, 60.8 (29–98) years, and the age of healthy probands was 31.3 (20–56) years. The male:female ratio of patients was 1:0.8, and 1:1.25 in healthy individuals. The average peripheral blood (PB) blast count of patients was 33 (10–94) %Bla/cells. AML cases were classified according to the FAB classification system [65], and MDS cases according to the WHO classification system [66]. Assessments for AML patients were further risk-classified according to the ELN classification [67] in favorable, intermediate and adverse subgroups, and for MDS patients according to the IPSS-R classification system [5,68] (Table 2).
Table 2.
Characteristics of patients and healthy individuals.
| Diagn. | No. | Age | Sex | Subtype | Stage | Ic bla | Blast Phenotype [cd] | Risk Class. | Response | Exp. |
|---|---|---|---|---|---|---|---|---|---|---|
| AML | 1444 | 35 | f | p/M1 | dgn. | 41 | 33, 65, 15, 34, 117 | favorable | yes | DC; MLC; CTX |
| AML | 1540 | 83 | f | p/M1 | dgn. | 32 | 13, 34, 33, 15, 117, 56 | favorable | no | DC; MLC; CTX; D/I |
| AML | 1427 | 52 | m | p/M2 | dgn. | 94 | 13, 33, 34, 117 | favorable | no | DC; MLC; CTX |
| AML | 1541 | 82 | f | p/M2 | dgn. | 15 | 15, 34, 117 | interm. | no | DC; MLC; CTX; D/I |
| AML | 1442 | 73 | f | p/M4 | dgn. | 15 | 33, 13, 34, 117, 15 | interm. | yes | DC; MLC; CTX |
| AML | 1459 | 54 | m | p/M4 | dgn. | 51 | 33, 64, 15, 4, 56, 14 | favorable | yes | DC; MLC; CTX |
| AML | 1430 | 79 | m | p/M5 | dgn. | 62 | 13, 33, 34, 117 | favorable | nd | DC; MLC; CTX |
| AML | 1432 | 34 | m | p/M5 | dgn. | 57 | 34, 13, 33, 64, 4 | interm. | yes | DC; MLC; CTX |
| AML | 1466 | 47 | f | p/M5 | dgn. | 11 | 33, 15, 13, 117, 34 | adverse | yes | DC; MLC; CTX |
| AML | 1575 | 62 | f | p/M5a | dgn. | 75 | 14, 56, 64, 65, 4 | interm. | yes | DC; MLC; CTX; D/I |
| AML | 1452 | 44 | m | p/nd | dgn. | 11 | 34, 117, 33, 13 | interm. | no | DC; MLC; CTX |
| AML | 1568 | 29 | m | p/nd | dgn. | 69 | 34, 117, 33, 13, 19, 20, 65 | interm. | no | DC; MLC; CTX; D/I |
| AML | 1570 | 36 | f | p/nd | dgn. | 11 | 34, 117, 65, 13, 33 | favorable | no | DC; MLC; CTX; D/I |
| AML | 1492 | 52 | f | s/M2 | dgn. | 38 | 117, 34, 13, 33, 7, 15 | nd | no | DC; MLC; CTX |
| AML | 1542 | 58 | f | s/M4 | dgn. | 52 | 13, 33, 34, 117, 15, 65, 64, 2, 56, 14 | adverse | no | DC; MLC; CTX; D/I |
| AML | 1426 | 61 | f | s/M5 | dgn. | 34 | 13, 33, 34, 64, 117, 14 | adverse | yes | DC; MLC; CTX |
| AML | 1464 | 72 | m | s/nd | dgn. | 38 | 34, 117, 13 | nd | nd | DC; MLC; CTX |
| AML | 1555 | 46 | f | s/nd | dgn. | 20 | 33, 14, 15, 117, 13 | favorable | nd | DC; MLC; D/I |
| AML | 1574 | 56 | m | s/nd | dgn. | 41 | 34, 117, 15, 19 | nd | no | DC; MLC; CTX; D/I |
| AML | 1571 | 61 | m | p/M2 | rel. | 18 | 117, 33, 13, 7 | nd | yes | DC; MLC; CTX; D/I |
| AML | 1424 | 37 | f | p/M4 | rel. | 13 | 13, 14, 33, 117 | nd | nd | DC; MLC; CTX |
| AML | 1548 | 87 | m | p/M5a | rel. | 12 | 33, 15, 117, 34, 56 | nd | no | DC; MLC; CTX; D/I |
| AML | 1449 | 78 | m | s/nd | rel. | 32 | 65, 14, 15, 33, 56, 34 | nd | nd | DC; MLC; CTX |
| AML | 1482 | 75 | m | s/nd | rel. | 12 | 117, 13, 64, 15, 117, 33 | nd | nd | DC; MLC; CTX |
| AML | 1546 | 80 | m | p/nd | pers. | 22 | 33, 34, 13, 117, 14, 65 | nd | no | DC; MLC; |
| AML | 1470 | 67 | m | p/nd | PR a. SCT | 38 | 33, 117, 34, 56, 65 | nd | no | DC; MLC |
| AML | 1457 | 63 | m | s/nd | rel. a. SCT | 37 | 34, 117, 13, 65, 15 | nd | no | DC; MLC; CTX |
| AML | 1543 | 61 | m | p/nd | rel. a. SCT. | 38 | 13, 33, 117, 56, 34 | nd | no | DC; MLC; CTX |
| MDS | 1567 | 98 | f | MDS | dgn. | 14 | 34, 117, 15, 65, 56, 14 | very high | nd | DC; MLC; CTX; D/I |
| MDS | 1573 | 61 | m | MDS | dgn. | 12 | 34, 117, 65, 13, 61 | high | no | DC; MLC; CTX; D/I |
| MDS | 1572 | 63 | f | MDS-EB2 | dgn. | 10 | 34, 117, 65, 33, 13 | very high | no | DC; MLC; CTX; D/I |
| healthy | 1417 | 34 | f | DC; MLC | ||||||
| healthy | 1418 | 22 | m | DC; MLC | ||||||
| healthy | 1421 | 27 | f | DC; MLC | ||||||
| healthy | 1422 | 20 | f | DC; MLC | ||||||
| healthy | 1425 | 27 | m | DC; MLC | ||||||
| healthy | 1428 | 56 | f | DC; MLC | ||||||
| healthy | 1429 | 22 | f | DC; MLC | ||||||
| healthy | 1431 | 22 | m | DC; MLC | ||||||
| healthy | 1436 | 25 | m | DC; MLC | ||||||
| healthy | 1440 | 20 | f | DC; MLC | ||||||
| healthy | 1448 | 27 | f | DC; MLC | ||||||
| healthy | 1458 | 21 | f | DC; MLC | ||||||
| healthy | 1544 | 22 | m | DC; MLC; D/I | ||||||
| healthy | 1545 | 32 | m | DC; MLC; D/I | ||||||
| healthy | 1547 | 46 | f | DC; MLC; D/I | ||||||
| healthy | 1566 | 54 | f | DC; MLC; D/I | ||||||
| healthy | 1576 | 55 | m | DC; MLC; D/I | ||||||
| healthy | 1578 | 32 | m | DC; MLC |
Diagn.—diagnosis; No.—sample number; m—male; f—female. Subtypes: p—primary AML; s—secondary AML. AML (FAB classification); MDS (WHO classification); rel. a. SCT—relapse after stem cell transplantation; rel.—relapse; dgn.—first diagnosis; pers.—persisting disease; PR—partial remission; nd—no data; Ic Bla—immunocytologically determined blasts; Risk Class: cytogenetic (AML ELN) and multifactorial (MDS IPSS-R) risk classification; Response—response to (induction) chemotherapy; Exp.—conducted experiments; MLC—mixed lymphocyte culture; DC—dendritic cell generation; CTX—cytotoxic fluorolysis assay; D/I—degranulation and intracellular cytokine assay.
4.2. Initial Sample Preparation
Mononuclear cells (MNCs) [10,69] were isolated from WB according to standard-preparations. T-cells were prepared using MACS microbead technology (Miltenyi Biotec, Bergisch Gladbach, Germany) [70]. MNC and T-cells were frozen for later experiments, as described [10,69,70].
4.3. Cultivation of Dendritic Cells (DC) and Leukemia-Derived Dendritic Cells (DCleu)
DC and DCleu were cultured with (vs. without) combinations of response modifiers (Kit-M and Kit-I), as described [10].
Kit-M consisted of GM-CSF (final concentration (fc): 800 U/mL, granulocyte macrophage colony stimulating factor, Sanofi-Aventis, Frankfurt, Germany) and PGE1 (fc: 1 µg/mL, prostaglandin E1, Santa Cruz Biotechnology, Dallas, Texas, USA), and Kit-I consisted of GM-CSF (fc: 800 U/mL) and Picibanil (fc: 10 µg/mL, Chugai Pharmaceutical Co., Kajiwara, Japan). Response modifiers were added on Day 0 and on Day 2–3 [27]. After 6–8 days, the cells were harvested, evaluated via flow cytometry and used for further experiments [10]. Cells will be referred to as DC(M) for Kit-M-treated WB, DC(I) for Kit-I-treated WB and DC(C) for the control with untreated WB.
4.4. Cultivation of Cells in Mixed Lymphocyte Cultures (MLC)
After seven days of DC generation (Kit-treated or untreated WB) the cultivation of MLC was started with previously frozen/thawed T-cells in the presence of 50 U/mL IL-2, as described [21,30].
After 6–8 days, cells were harvested, immune cell subtypes were quantified, and degranulation (DEG), intracellular cytokine (INTCYT) and cytotoxicity fluorolysis assays (CTX) were performed, as described [10,27]. Cells before MLC will be referred to as MLC(UC) and those after MLC as MLC(CC) for the control with untreated WB. MLC(M) will refer to MLC with Kit-M-pretreated WB, and MLC(I) to MLC with Kit-I-pretreated WB.
4.5. Degranulation Assay (DEG) and Intracellular Cytokine Assay (INTCYT)
Cells (uncultured WB or T-cell-enriched MLCs, stimulated with or without Kit-treated WB after MLC) were mixed and incubated in parallel with those without leukemia-associated antigens (LAA) (PepTivator WT1 (fc: 0.6 nmol/mL, Miltenyi Biotec, Bergisch Gladbach, Germany) and PepTivator PRAME (fc: 0.6 nmol/mL, Miltenyi Biotec, Bergisch Gladbach, Germany)) for patients’ samples and with staphylococcal enterotoxin B (SEB, fc: 10 µg/mL, Sigma-Aldrich, St. Louis, Missouri, USA), as described [21,30,71].
An FITC-conjugated antibody against CD107a (BioLegend, San Diego, CA, USA) was used to detect cell degranulation as a marker for cell cytotoxicity, as described [19,72]. Finally, cells were harvested and analyzed via flow cytometry [30].
To quantify intracellular cytokine production, antibodies against tumor necrosis factor alpha (TNFα) [20] and interferon gamma (IFNγ) [21] were used: PE/Cy 7-TNFα antibodies (BioLegend, San Diego, CA, USA) and PE-IFNγ antibodies (BioLegend, San Diego, CA, USA)). To stop the cellular cytokine secretion, after one hour of incubation time, Brefeldin A solution (fc: 5 µg/mL, BioLegend, San Diego, CA, USA) was added according to the manufacturer’s instructions. Finally, cells were harvested and analyzed via flow cytometry [21].
4.6. Cytotoxicity Fluorolysis Assay (CTX)
CTX was performed to test the ability of effector cells (T-cell-enriched cells, stimulated with Kit-M-treated or untreated WB) to lyse blast target cells.
Kit-M-treated (vs. untreated as a control) patients’ WB (as ‘stimulator cells‘) and patients’ T-cells (frozen at the start of the experiments) were used as the main ‘effector cells‘ to be activated by MLC. AFTER MLC functionality was measured: cells in MLC (after stimulation with Kit-M-treated (vs. untreated) WB cells) were ‘effector cells‘. Blast-containing MNC (frozen at the start of the experiments) were added as ‘target cells‘. Blasts were stained using patient-related blast markers and were quantified via flowcytometry. Finally, the frequencies of viable (7AAD-negative) blast cells after the incubation of ‘target cells’ (blast-containing MNC) with ‘effector cells’ (T-cell-enriched MLC stimulated (vs. not stimulated) with Kit-M before were quantified, and blast lysis calculated according to previous publications, e.g., [21].
Finally, the difference in viable blast-cells in the main and the control samples was defined as ‘blast lysis’. The ‘lysis improvement’ was determined by comparing the achieved ‘blast lysis’ after MLC with, compared to without, Kit-pretreated WB [10,17,32].
4.7. Quantification of Cells Using Flow Cytometry
Before or after culture, cells were stained using fluorochrome-labeled monoclonal antibodies and quantified using a FACSCalibur four-channel flow cytometer as described [12,16]. The antibodies were conjugated with FITC (fluorescein-isothiocyanate), PE (phycoerythrin), PE/Cy 7 (phycoerythrin/cyanine 7) and APC (allophycocyanin). The FITC-labeled antibodies were: IgG*, CD34*, CD65*, CD33*, CD117***, CD15*, CD56***, CD3**, CD71*, ipo38****, CD19*, CD107a***, CD4**, CD45RO* and CD14*. The PE-labeled antibodies were: IgG*, CD 117*, CD80*, CD83*, CD56*, CD206*, CD3*, IFNγ*** and CD4**. The PE/Cy 7-labeled antibodies were: IgG*, CD15**, CD117*, CD19*, CD34*, CD197**, CD56*, CD4*, TNFα***, CD3* and CD14**. The APC-labeled antibodies were: IgG*, CD206**, CD80***, CD209**, CD83**, CD34*, CD117*, CD14*, CD56*, CD69**, β7**, CD45RO***, CD4**, CD3* and CD19*. The antibodies were supplied by Beckman Coulter (*, Brea, CA, US), BD Biosciences (**, San Jose, CA, US), BioLegend (***, San Diego, CA, US) and Santa Cruz Biotechnology (****, Dallas, TX, US). For the detection of viable cells, 7AAD** was used.
For every patient, highly expressed blast markers (e.g., CD34, CD117, CD65, CD56 or CD15) and DC markers with low/no expression of blasts (e.g., CD80, CD83, CD206 or CD209) were selected to quantify DC or DCleu subpopulations after culture [12,16].
For the detection of intracellular markers (ipo38 and INTCYT), the FIX & PERM Cell Fixation and Cell Permeabilization Kit (Thermo Fisher Scientific, Darmstadt, Germany) was used. Isotype samples served as controls [10,73].
4.8. Statistical Analysis
The analysis of flow cytometric data was conducted using BD CellQuest Pro software (Becton Dickinson, Heidelberg, Germany). Statistical analyses, including the calculation of means, standard deviations and significance, were conducted using Excel 2010 (Microsoft, Redmond, Washington, USA) and SPSS Statistics 26 (IBM, Armonk, New York, NY, USA). Differences and correlations between groups were analyzed using the paired-t-test and the Wilcoxon–Mann–Whitney U test. Correlation analyses were conducted using Pearson correlation and Spearman correlation. Highly significant differences were defined in cases with p-values ≤ 0.005 and significantly different cases with p-values between 0.05 and 0.0051.
5. Conclusions
β7, as a subunit of the integrin receptor, is expressed in several subtypes of healthy and patients’ cells in the adaptive and innate immune system. Pretreatment of AML/MDS patients’ WB samples with blast-modulating Kits (vs. no Kits) increased the frequencies of DC/DCleu, which ultimately increased the frequencies of (leukemia-specific degranulating or cytokine-producing) β7-expressing T- or NK/CIK-cell subtypes after T-cell-enriched MLC. The frequencies of the generated/activated β7-expressing cells correlated ex vivo with the provision of leukemia-specific/antileukemic cells after (T-cell-enriched) MLC with Kit-pretreated (vs. untreated) WB, and in vivo with achieved (vs. not achieved) remission after induction chemotherapy, and with patients’ allocations to favorable (vs. unfavorable) risk types. (Due to the low case numbers available, not all results showed significant results; however, there were always clear differences between groups.)
Acknowledgments
The authors thank the patients, nurses and physicians for their work and support with the sample material and diagnostic reports. The results presented in this article are part of the doctoral thesis of Elias Rackl at the Ludwig Maximilian University of Munich.
Author Contributions
E.R. performed a great portion of the experiments and analyzed all flow cytometric and statistical data. L.L., L.K.K., S.U., E.P., C.G., M.W., F.D.-G., C.P. and D.C.A. contributed data to the DC, MLC, CTX and DEG/INTCYT experiments, which were evaluated by E.R., C.S. and N.R. helped with manuscript preparation. P.B., D.K., J.S., A.R. and C.S. provided the patients’ samples and reports. H.M.S. was responsible for the study design. E.R. and H.M.S. contributed to drafting. C.L.S. contributed to critical revision and discussion and helped with submission. N.R., C.L.S., C.S., E.R. and H.M.S. contributed to editing the manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Samples were collected and patients’ informed consent gathered according to the Helsinki guidelines and with the vote of the Ethics Committee of LMU in Munich (vote number: 33905).
Conflicts of Interest
H.M.S. is involved with Modiblast Pharma GmbH (Oberhaching, Germany), which holds the European Patent 15 801 987.7-1118 and US Patent 15-517627, “Use of immunomodulatory effective compositions for the immunotherapeutic treatment of patients suffering from myeloid leukemias”.
Funding Statement
The project was supported by intramural funding from the working group of HS. Lin Li was funded by grants from the China Scholarship Council (CSC) (File No. 201808210307). Fatemeh Doraneh-Gard was funded by grants from the DAAD (ID 21520154 and scholarship 2016–2017 of the Ludwig Maximilian University of Munich). The funders did not influence the study design, data collection or analysis; the publishing decision; or the manuscript preparation.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Herold G. Innere Medizin 2020. Walter de Gruyter GmbH & Co KG; Berlin, Germany: 2020. [Google Scholar]
- 2.Arber D.A., Orazi A., Hasserjian R., Thiele J., Borowitz M.J., Le Beau M.M., Bloomfield C.D., Cazzola M., Vardiman J.W. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127:2391–2405. doi: 10.1182/blood-2016-03-643544. [DOI] [PubMed] [Google Scholar]
- 3.Lowenberg B., Downing J.R., Burnett A. Acute Myeloid Leukemia. New Engl. J. Med. 1999;341:1051–1062. doi: 10.1056/NEJM199909303411407. [DOI] [PubMed] [Google Scholar]
- 4.Röllig C., Beelen D.W., Braess J., Greil R., Niederwieser D., Passweg J., Reinhardt D., Schlenk R.F. Leitlinie Akute Myeloische Leukämie, Onkopedia, Deutsche Gesellschaft für Hämatologie und Onkologie. [(accessed on 17 November 2020)]. Available online: https://www.onkopedia.com/de/onkopedia/guidelines/akute-myeloische-leukaemie-aml/@@guideline/html/index.html.
- 5.Garcia-Manero G., Chien K.S., Montalban-Bravo G. Myelodysplastic syndromes: 2021 update on diagnosis, risk stratification and management. Am. J. Hematol. 2020;95:1399–1420. doi: 10.1002/ajh.25950. [DOI] [PubMed] [Google Scholar]
- 6.Estey E.H. Acute myeloid leukemia: 2021 update on risk-stratification and management. Am. J. Hematol. 2020;95:1368–1398. doi: 10.1002/ajh.25975. [DOI] [PubMed] [Google Scholar]
- 7.Behrends J., Bischofberger J., Deutzmann R., Ehmke H., Frings S. Duale Reihe Physiologie. Thieme; Stuttgart, Germany: 2016. [Google Scholar]
- 8.Sabado R.L., Balan S., Bhardwaj N. Dendritic cell-based immunotherapy. Cell Res. 2016;27:74–95. doi: 10.1038/cr.2016.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Amberger D.C., Schmetzer H.M. Dendritic Cells of Leukemic Origin: Specialized Antigen-Presenting Cells as Potential Treatment Tools for Patients with Myeloid Leukemia. Transfus. Med. Hemother. 2020;47:432–443. doi: 10.1159/000512452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Amberger D.C., Doraneh-Gard F., Gunsilius C., Weinmann M., Möbius S., Kugler C., Rogers N., Böck C., Ködel U., Werner J.-O., et al. PGE1-Containing Protocols Generate Mature (Leukemia-Derived) Dendritic Cells Directly from Leukemic Whole Blood. Int. J. Mol. Sci. 2019;20:4590. doi: 10.3390/ijms20184590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Plett C., Klauer L.K., Amberger D.C., Ugur S., Rabe A., Fischer Z., Deen D., Hirn-Lopez A., Gunsilius C., Werner J.-O., et al. Immunomodulatory Kits do not induce AML-blasts’ proliferation ex vivo: IPO-38 is an appropriate and reliable marker to detect and quantify proliferating blasts. Clin. Immunol. 2022;242:109083. doi: 10.1016/j.clim.2022.109083. [DOI] [PubMed] [Google Scholar]
- 12.Schmetzer H.M., Kremser A., Loibl J., Kroell T., Kolb H.-J. Quantification of ex vivo generated dendritic cells (DC) and leukemia-derived DC contributes to estimate the quality of DC, to detect optimal DC-generating methods or to optimize DC-mediated T-cell-activation-procedures ex vivo or in vivo. Leukemia. 2007;21:1338–1341. doi: 10.1038/sj.leu.2404639. [DOI] [PubMed] [Google Scholar]
- 13.Grabrucker C., Liepert A., Dreyig J., Kremser A., Kroell T., Freudenreich M., Schmid C., Schweiger C., Tischer J., Kolb H.-J., et al. The Quality and Quantity of Leukemia-derived Dendritic Cells From Patients With Acute Myeloid Leukemia and Myelodysplastic Syndrome Are a Predictive Factor for the Lytic Potential of Dendritic Cells-primed Leukemia-Specific T Cells. J. Immunother. 2010;33:523–537. doi: 10.1097/CJI.0b013e3181d87ffd. [DOI] [PubMed] [Google Scholar]
- 14.Schick J., Vogt V., Zerwes M., Kroell T., Kraemer D., Köhne C.-H., Hausmann A., Buhmann R., Tischer J., Schmetzer H. Antileukemic T-cell Responses Can Be Predicted by the Composition of Specific Regulatory T-cell Subpopulations. J. Immunother. 2013;36:223–237. doi: 10.1097/CJI.0b013e31829180e7. [DOI] [PubMed] [Google Scholar]
- 15.Vogt V., Schick J., Ansprenger C., Braeu M., Kroell T., Kraemer D., Köhne C.-H., Hausmann A., Buhmann R., Tischer J., et al. Profiles of Activation, Differentiation–Markers, or β-Integrins on T Cells Contribute to Predict T Cells’ Antileukemic Responses After Stimulation With Leukemia-derived Dendritic Cells. J. Immunother. 2014;37:331–347. doi: 10.1097/CJI.0000000000000037. [DOI] [PubMed] [Google Scholar]
- 16.Campana D., Behm F.G. Immunophenotyping of leukemia. J. Immunol. Methods. 2000;243:59–75. doi: 10.1016/S0022-1759(00)00228-3. [DOI] [PubMed] [Google Scholar]
- 17.Ugur S., Klauer L.K., Blasi C., Doraneh-Gard F., Plett C., Gunsilius C., Amberger D.C., Weinmann M., Schutti O., Fischer Z., et al. ‘Kit’-mediated blastmodulation to leukemia-derived DC significantly improves antileukemic activities in whole blood independent of AML-patients’ subtypes. Submitted 2022.
- 18.Pérez-Villar J.J., Zapata J.M., Melero I., Postigo A., Sánchez-Madrid F., López-Botet M. Expression and function of α 4/β 7 integrin on human natural killer cells. Immunology. 1996;89:96–104. doi: 10.1046/j.1365-2567.1996.d01-706.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aktas E., Kucuksezer U.C., Bilgic S., Erten G., Deniz G. Relationship between CD107a expression and cytotoxic activity. Cell. Immunol. 2009;254:149–154. doi: 10.1016/j.cellimm.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 20.Rodríguez-Caballero A., García-Montero A.C., Bueno C., Almeida J., Varro R., Chen R., Pandiella A., Orfao A. A new simple whole blood flow cytometry-based method for simultaneous identification of activated cells and quantitative evaluation of cytokines released during activation. Lab. Investig. 2004;84:1387–1398. doi: 10.1038/labinvest.3700162. [DOI] [PubMed] [Google Scholar]
- 21.Klauer L.K., Schutti O., Ugur S., Doraneh-Gard F., Amberger D.C., Rogers N., Krämer D., Rank A., Schmid C., Eiz-Vesper B., et al. Interferon Gamma Secretion of Adaptive and Innate Immune Cells as a Parameter to Describe Leukaemia-Derived Dendritic-Cell-Mediated Immune Responses in Acute Myeloid Leukaemia in vitro. Transfus. Med. Hemother. 2021;49:44–61. doi: 10.1159/000516886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Parkin J., Cohen B. An overview of the immune system. Lancet. 2001;357:1777–1789. doi: 10.1016/S0140-6736(00)04904-7. [DOI] [PubMed] [Google Scholar]
- 23.Dunn G.P., Bruce A.T., Ikeda H., Old L.J., Schreiber R.D. Cancer immunoediting: From immunosurveillance to tumor escape. Nat. Immunol. 2002;3:991–998. doi: 10.1038/ni1102-991. [DOI] [PubMed] [Google Scholar]
- 24.Beutler B. Innate immunity: An overview. Mol. Immunol. 2004;40:845–859. doi: 10.1016/j.molimm.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 25.Schmeel L.C., Schmeel F., Coch C., Schmidt-Wolf I.G.H. Cytokine-induced killer (CIK) cells in cancer immunotherapy: Report of the international registry on CIK cells (IRCC) J. Cancer Res. Clin. Oncol. 2014;141:839–849. doi: 10.1007/s00432-014-1864-3. [DOI] [PubMed] [Google Scholar]
- 26.Franks S., Wolfson B., Hodge J. Natural Born Killers: NK Cells in Cancer Therapy. Cancers. 2020;12:2131. doi: 10.3390/cancers12082131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Boeck C.L., Amberger D.C., Doraneh-Gard F., Sutanto W., Guenther T., Schmohl J., Schuster F., Salih H., Babor F., Borkhardt A., et al. Significance of Frequencies, Compositions, and/or Antileukemic Activity of (DC-stimulated) Invariant NKT, NK and CIK Cells on the Outcome of Patients With AML, ALL and CLL. J. Immunother. 2017;40:224–248. doi: 10.1097/CJI.0000000000000171. [DOI] [PubMed] [Google Scholar]
- 28.Bonilla F.A., Oettgen H.C. Adaptive immunity. J. Allergy Clin. Immunol. 2010;125:S33–S40. doi: 10.1016/j.jaci.2009.09.017. [DOI] [PubMed] [Google Scholar]
- 29.Betts M.R., Brenchley J.M., Price D.A., De Rosa S.C., Douek D.C., Roederer M., Koup R.A. Sensitive and viable identification of antigen-specific CD8+ T cells by a flow cytometric assay for degranulation. J. Immunol. Methods. 2003;281:65–78. doi: 10.1016/S0022-1759(03)00265-5. [DOI] [PubMed] [Google Scholar]
- 30.Pepeldjiyska E., Li L., Gao J., Seidel C.L., Blasi C., Özkaya E., Schmohl J., Kraemer D., Schmid C., Rank A., et al. Leukemia derived dendritic cell (DCleu) mediated immune response goes along with reduced (leukemia-specific) regulatory T-cells. Immunobiology. 2022;227:152237. doi: 10.1016/j.imbio.2022.152237. [DOI] [PubMed] [Google Scholar]
- 31.Letsch A., Scheibenbogen C. Quantification and characterization of specific T-cells by antigen-specific cytokine production using ELISPOT assay or intracellular cytokine staining. Methods. 2003;31:143–149. doi: 10.1016/S1046-2023(03)00124-5. [DOI] [PubMed] [Google Scholar]
- 32.Kienzle N., Olver S., Buttigieg K., Kelso A. The fluorolysis assay, a highly sensitive method for measuring the cytolytic activity of T cells at very low numbers. J. Immunol. Methods. 2002;267:99–108. doi: 10.1016/S0022-1759(02)00150-3. [DOI] [PubMed] [Google Scholar]
- 33.Kumar P., Nagarajan A., Uchil P. Analysis of Cell Viability by the Lactate Dehydrogenase Assay. Cold Spring Harb. Protoc. 2018;2018 doi: 10.1101/pdb.prot095497. [DOI] [PubMed] [Google Scholar]
- 34.Hynes R.O. Integrins: Bidirectional, Allosteric Signaling Machines. Cell. 2002;110:673–687. doi: 10.1016/S0092-8674(02)00971-6. [DOI] [PubMed] [Google Scholar]
- 35.Rivera-Nieves J., Ley K. Role of β7 Integrins in Intestinal Lymphocyte Homing and Retention. Curr. Mol. Med. 2009;9:836–850. doi: 10.2174/156652409789105525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Murakami J.L., Xu B., Franco C.B., Hu X., Galli S.J., Weissman I.L., Chen C.-C. Evidence that β7 Integrin Regulates Hematopoietic Stem Cell Homing and Engraftment Through Interaction with MAdCAM-1. Stem Cells Dev. 2016;25:18–26. doi: 10.1089/scd.2014.0551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Erle D.J., Briskin M.J., Butcher E.C., Garcia-Pardo A., Lazarovits A.I., Tidswell M. Expression and function of the MAdCAM-1 receptor, integrin alpha 4 beta 7, on human leukocytes. J. Immunol. 1994;153:517–528. doi: 10.4049/jimmunol.153.2.517. [DOI] [PubMed] [Google Scholar]
- 38.Tang M.T., Keir M.E., Erickson R., Stefanich E.G., Fuh F.K., Ramirez-Montagut T., McBride J.M., Danilenko D.M. Review article: Nonclinical and clinical pharmacology, pharmacokinetics and pharmacodynamics of etrolizumab, an anti-β7 integrin therapy for inflammatory bowel disease. Aliment. Pharmacol. Ther. 2018;47:1440–1452. doi: 10.1111/apt.14631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reeves R.K., Evans T.I., Gillis J., Johnson R.P. Simian Immunodeficiency Virus Infection Induces Expansion of α4β7 + and Cytotoxic CD56 + NK Cells. J. Virol. 2010;84:8959–8963. doi: 10.1128/JVI.01126-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hardenberg J.-H.B., Braun A., Schön M.P. A Yin and Yang in Epithelial Immunology: The Roles of the αE(CD103)β7 Integrin in T Cells. J. Investig. Dermatol. 2018;138:23–31. doi: 10.1016/j.jid.2017.05.026. [DOI] [PubMed] [Google Scholar]
- 41.Heitmann J.S., Hagelstein I., Hinterleitner C., Roerden M., Jung G., Salih H.R., Märklin M., Kauer J. Identification of CD318 (CDCP1) as novel prognostic marker in AML. Ann. Hematol. 2020;99:477–486. doi: 10.1007/s00277-020-03907-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Graf M., Reif S., Kröll T., Hecht K., Nuessler V., Schmetzer H. Expression of MAC-1 (CD11b) in acute myeloid leukemia (AML) is associated with an unfavorable prognosis. Am. J. Hematol. 2006;81:227–235. doi: 10.1002/ajh.20526. [DOI] [PubMed] [Google Scholar]
- 43.Cheng J., Ma H.-Z., Zhang H. Detection and Analysis of T Lymphocyte Subsets and B Lymphocytes in Patients with Acute Leukemia. Zhongguo Shi Yan Xue Ye Xue Za Zhi. 2019;27:327–330. doi: 10.19746/j.cnki.issn.1009-2137.2019.02.003. [DOI] [PubMed] [Google Scholar]
- 44.Yang W., Xu Y. Clinical significance of Treg cell frequency in acute myeloid leukemia. Int. J. Hematol. 2013;98:558–562. doi: 10.1007/s12185-013-1436-3. [DOI] [PubMed] [Google Scholar]
- 45.Van Tendeloo V.F., Van de Velde A., Van Driessche A., Cools N., Anguille S., Ladell K., Gostick E., Vermeulen K., Pieters K., Nijs G., et al. Induction of complete and molecular remissions in acute myeloid leukemia by Wilms’ tumor 1 antigen-targeted dendritic cell vaccination. Proc. Natl. Acad. Sci. USA. 2010;107:13824–13829. doi: 10.1073/pnas.1008051107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cao H., Vergé V., Baron C., Martinache C., Leon A., Scholl S., Gorin N.-C., Salamero J., Assari S., Bernard J., et al. Cutting Edge Communication: In Vitro Generation of Dendritic Cells from Human Blood Monocytes in Experimental Conditions Compatible for In Vivo Cell Therapy. J. Hematother. 2000;9:183–194. doi: 10.1089/152581600319397. [DOI] [PubMed] [Google Scholar]
- 47.Lopez A.H., Deen D., Fischer Z., Rabe A., Ansprenger C., Stein K., Vogt V., Schick J., Kroell T., Kraemer D., et al. Role of Interferon (IFN)α in “Cocktails” for the Generation of (Leukemia-derived) Dendritic Cells (DCleu) From Blasts in Blood From Patients (pts) With Acute Myeloid Leukemia (AML) and the Induction of Antileukemic Reactions. J. Immunother. 2019;42:143–161. doi: 10.1097/CJI.0000000000000266. [DOI] [PubMed] [Google Scholar]
- 48.Schwepcke C., Klauer L.K., Deen D., Amberger D.C., Fischer Z., Doraneh-Gard F., Gunsilius C., Hirn-Lopez A., Kroell T., Tischer J., et al. Generation of Leukaemia-Derived Dendritic Cells (DCleu) to Improve Anti-Leukaemic Activity in AML: Selection of the Most Efficient Response Modifier Combinations. Int. J. Mol. Sci. 2022;23:8333. doi: 10.3390/ijms23158333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Logan C., Koura D., Taplitz R. Updates in infection risk and management in acute leukemia. Hematology. 2020;2020:135–139. doi: 10.1182/hematology.2020000098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Teague R.M., Kline J. Immune evasion in acute myeloid leukemia: Current concepts and future directions. J. Immunother. Cancer. 2013;1:13. doi: 10.1186/2051-1426-1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schorle H., Holtschke T., Hünig T., Schimpl A., Horak I. Development and function of T cells in mice rendered interleukin-2 deficient by gene targeting. Nature. 1991;352:621–624. doi: 10.1038/352621a0. [DOI] [PubMed] [Google Scholar]
- 52.Yu J., Sun H., Cao W., Song Y., Jiang Z. Research progress on dendritic cell vaccines in cancer immunotherapy. Exp. Hematol. Oncol. 2022;11:3. doi: 10.1186/s40164-022-00257-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Steger B., Milosevic S., Doessinger G., Reuther S., Liepert A., Braeu M., Schick J., Vogt V., Schuster F., Kroell T., et al. CD4+ and CD8+T-cell reactions against leukemia-associated- or minor-histocompatibility-antigens in AML-patients after allogeneic SCT. Immunobiol. 2013;219:247–260. doi: 10.1016/j.imbio.2013.10.008. [DOI] [PubMed] [Google Scholar]
- 54.Bordon Y. Sorting, sorted! Nat. Rev. Immunol. 2016;16:657. doi: 10.1038/nri.2016.115. [DOI] [PubMed] [Google Scholar]
- 55.Li L., Giannopoulos K., Reinhardt P., Tabarkiewicz J., Schmitt A., Greiner J., Rolinski J.M., Hus I., Dmoszynska A., Wiesneth M., et al. Immunotherapy for patients with acute myeloid leukemia using autologous dendritic cells generated from leukemic blasts. Int. J. Oncol. 2006;28:855–861. doi: 10.3892/ijo.28.4.855. [DOI] [PubMed] [Google Scholar]
- 56.Van De Loosdrecht A.A., Van Wetering S., Santegoets S.J.A.M., Singh S.K., Eeltink C.M., den Hartog Y., Koppes M., Kaspers J., Ossenkoppele G.J., Kruisbeek A.M., et al. A novel allogeneic off-the-shelf dendritic cell vaccine for post-remission treatment of elderly patients with acute myeloid leukemia. Cancer Immunol. Immunother. 2018;67:1505–1518. doi: 10.1007/s00262-018-2198-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dong M., Liang D., Li Y., Kong D., Kang P., Li K., Ping C., Zhang Y., Zhou X., Hong L. Autologous Dendritic Cells Combined with Cytokine-Induced Killer Cells Synergize Low-Dose Chemotherapy in Elderly Patients with Acute Myeloid Leukaemia. J. Int. Med Res. 2012;40:1265–1274. doi: 10.1177/147323001204000405. [DOI] [PubMed] [Google Scholar]
- 58.Stroopinsky D., Liegel J., Bhasin M., Cheloni G., Thomas B., Bhasin S., Panchal R., Ghiasuddin H., Rahimian M., Nahas M., et al. Leukemia vaccine overcomes limitations of checkpoint blockade by evoking clonal T cell responses in a murine acute myeloid leukemia model. Haematologica. 2021;106:1330–1342. doi: 10.3324/haematol.2020.259457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Anguille S., Van de Velde A.L., Smits E.L., Van Tendeloo V.F., Juliusson G., Cools N., Nijs G., Stein B., Lion E., Van Driessche A., et al. Dendritic cell vaccination as postremission treatment to prevent or delay relapse in acute myeloid leukemia. Blood. 2017;130:1713–1721. doi: 10.1182/blood-2017-04-780155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Roddie H., Klammer M., Thomas C., Thomson R., Atkinson A., Sproul A., Waterfall M., Samuel K., Yin J., Johnson P., et al. Phase I/II study of vaccination with dendritic-like leukaemia cells for the immunotherapy of acute myeloid leukaemia. Br. J. Haematol. 2006;133:152–157. doi: 10.1111/j.1365-2141.2006.05997.x. [DOI] [PubMed] [Google Scholar]
- 61.Schmitt M., Schmitt A., Rojewski M.T., Chen J., Giannopoulos K., Fei F., Yu Y., Götz M., Heyduk M., Ritter G., et al. RHAMM-R3 peptide vaccination in patients with acute myeloid leukemia, myelodysplastic syndrome, and multiple myeloma elicits immunologic and clinical responses. Blood. 2008;111:1357–1365. doi: 10.1182/blood-2007-07-099366. [DOI] [PubMed] [Google Scholar]
- 62.Adan A., Kiraz Y., Baran Y. Cell Proliferation and Cytotoxicity Assays. Curr. Pharm. Biotechnol. 2016;17:1213–1221. doi: 10.2174/1389201017666160808160513. [DOI] [PubMed] [Google Scholar]
- 63.Lowin B., Hahne M., Mattmann C., Tschopp J. Cytolytic T-cell cytotoxicity is mediated through perforin and Fas lytic pathways. Nature. 1994;370:650–652. doi: 10.1038/370650a0. [DOI] [PubMed] [Google Scholar]
- 64.Rabinovich G.A., Gabrilovich D., Sotomayor E.M. Immunosuppressive Strategies that are Mediated by Tumor Cells. Annu. Rev. Immunol. 2007;25:267–296. doi: 10.1146/annurev.immunol.25.022106.141609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bennett J.M., Catovsky D., Daniel M.-T., Flandrin G., Galton D.A.G., Gralnick H.R., Sultan C. Proposals for the Classification of the Acute Leukaemias French-American-British (FAB) Co-operative Group. Br. J. Haematol. 1976;33:451–458. doi: 10.1111/j.1365-2141.1976.tb03563.x. [DOI] [PubMed] [Google Scholar]
- 66.Swerdlow S.H., Campo E., Harris N.L., Jaffe E.S., Pileri S.A., Stein H., Thiele J. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. 4th ed. International Agency for Research on Cancer; Lyon, France: 2017. [Google Scholar]
- 67.Döhner H., Estey E., Grimwade D., Amadori S., Appelbaum F.R., Büchner T., Dombret H., Ebert B.L., Fenaux P., Larson R.A., et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129:424–447. doi: 10.1182/blood-2016-08-733196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Greenberg P., Cox C., Lebeau M.M., Fenaux P., Morel P., Sanz G., Sanz M., Vallespi T., Hamblin T., Oscier D., et al. International Scoring System for Evaluating Prognosis in Myelodysplastic Syndromes. Blood. 1997;89:2079–2088. doi: 10.1182/blood.V89.6.2079. [DOI] [PubMed] [Google Scholar]
- 69.Böyum A. Separation of leukocytes from blood and bone marrow. Introduction. Scand. J. Clin. Lab. Invest. Suppl. 1968;97:7. [PubMed] [Google Scholar]
- 70.Willasch A., Eing S., Weber G., Kuci S., Schneider G., Soerensen J., Jarisch A., Rettinger E., Koehl U., Klingebiel T., et al. Enrichment of cell subpopulations applying automated MACS technique: Purity, recovery and applicability for PCR-based chimerism analysis. Bone Marrow Transplant. 2009;45:181–189. doi: 10.1038/bmt.2009.89. [DOI] [PubMed] [Google Scholar]
- 71.Whitfield S.J.C., Taylor C., Risdall J.E., Griffiths G.D., Jones J.T.A., Williamson E.D., Rijpkema S., Saraiva L., Vessillier S., Green A.C., et al. Interference of the T Cell and Antigen-Presenting Cell Costimulatory Pathway Using CTLA4-Ig (Abatacept) Prevents Staphylococcal Enterotoxin B Pathology. J. Immunol. 2017;198:3989–3998. doi: 10.4049/jimmunol.1601525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Betts M.R., Koup R.A. Detection of T-Cell Degranulation: CD107a and b. Methods Cell Biol. 2004;75:497–512. doi: 10.1016/s0091-679x(04)75020-7. [DOI] [PubMed] [Google Scholar]
- 73.Kufner S., Zitzelsberger H., Kroell T., Pelka-Fleischer R., Salem A., de Valle F., Schweiger C., Nuessler V., Schmid C., Kolb H.J., et al. Leukemia-Derived Dendritic Cells can be Generated from Blood or Bone Marrow Cells from Patients with Acute Myeloid Leukaemia: A Methodological Approach under Serum-Free Culture Conditions. Scand. J. Immunol. 2005;62:86–98. doi: 10.1111/j.1365-3083.2005.01630.x. [DOI] [PubMed] [Google Scholar]