Visual Abstract
Abstract
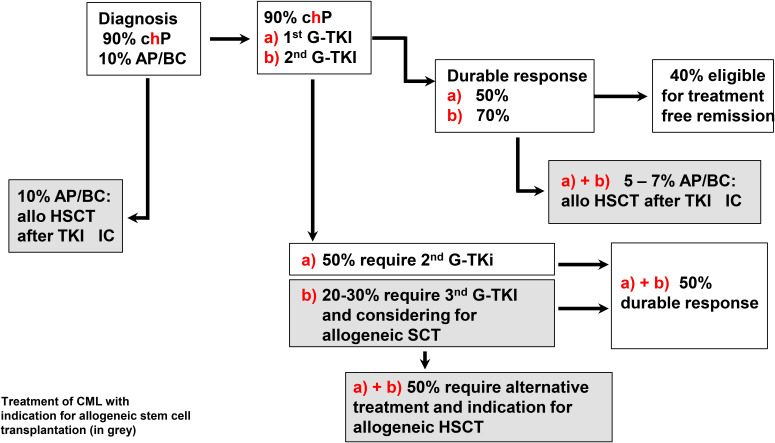
Molecular therapy with tyrosine kinase inhibitors (TKIs) has significantly reduced the indication for allogeneic hematopoietic stem cell transplantation (allo-HSCT) in chronic myeloid leukemia (CML). Treatment-free remission can be obtained in about 50% of patients with an optimal response. However, cure rates up to 90% are restricted to patients receiving HSCT. Timing is essential since HSCT in the early stages of the disease has the best outcome. Patients in a more advanced phase (AdP) than chronic-phase (chP) CML undergo HSCT with suboptimal outcomes, and the gap between chP and AdP disease is widening. First-line therapy should start with first- or second-generation (G) TKIs. Patients failing treatment (BCR-ABL1 transcripts of greater than 10% at 3 and 6 months and greater than 1% at 12 months) should be switched to second-line TKIs, and HSCT should be considered. Patients not responding to 2G-TKI therapy as well as patients in an accelerated phase (AP) or blast crisis (BC) are candidates for HSCT. Therapy resistant BCR-ABL1 mutations, high-risk additional cytogenetic abnormalities, and molecular signs of leukemia progression should trigger the indication for HSCT. Patients who, despite dose adjustments, do not tolerate or develop severe adverse events, including vascular events, to multiple TKIs are also candidates for HSCT. In AdP CML, TKIs do not show long-lasting results, and the outcome of HSCT is less optimal without pretransplant therapy. In these patients the induction of chP2 with TKIs, either alone (AP) or in combination with intensive chemotherapy (BC), followed by HSCT should be pursued.
Learning Objectives
Understand the criteria for considering allogeneic stem cell transplantation for CML patients
Define the risk factors for outcomes after allogeneic stem cell transplantation for CML patients
Acquire the knowledge of how to use TKIs before and after transplantation in CML patients
Introduction
Chronic myeloid leukemia (CML), a disease of predominantly older adult (age >60 years) and male patients, is in many aspects a model for malignant diseases. Described by Virchow and Bennett in 1845 as leucocythemia, it was the first malignancy with a common chromosomal alteration.1,2 After molecular identification of the breakpoints, the main molecular pathomechanisms were unraveled.3,4
Hematopoietic stem cell transplantation (HSCT) was shown to be the only curative option.5 Almost at the same time, treatment with interferon alfa was shown to induce cytogenetic remissions (CyR) in a small proportion of patients.6 The use of BCR-ABL1 transcripts for disease monitoring and donor lymphocyte infusion (DLI) to treat relapse after HSCT were the next hallmarks in the treatment of this disease.7,8 Finally, in 2001 a specific inhibitor of BCR-ABL tyrosine kinase revolutionized the treatment of CML.9 In 2010, the discontinuation of TKIs in patients with optimal response was described and the term “operational cure” used.10
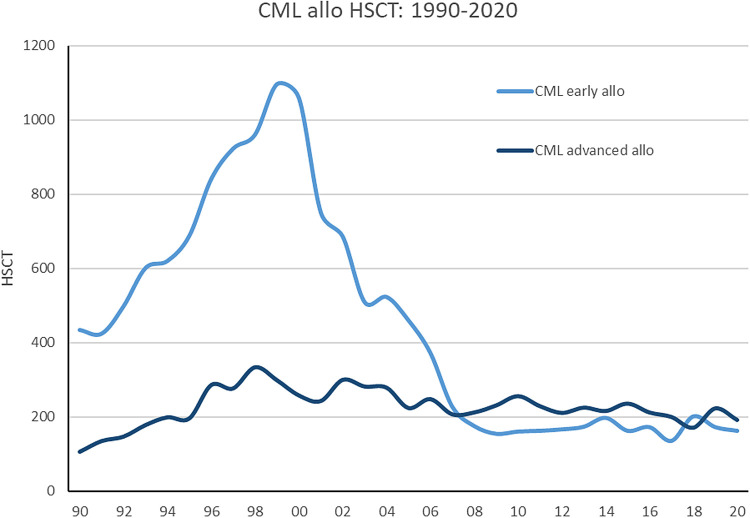
After decades of development, HSCT was increasingly used worldwide, and more than 1.5 million transplants (now 90 000 annually) were reported up to 2019.11 Patients with early chronic-phase (chP) CML were considered an ideal indication for HSCT.12 Interval-diagnosis HSCT (<12 months and >12 months), disease stage (chP, accelerated phase [AP], and blast crisis [BC]), donor (related and unrelated), and gender differences were recognized as major prognostic factors influencing transplant-related mortality (TRM; nonrelapse mortality caused by graft-versus-host disease [GVHD], infections, or toxicities), and relapse incidence (European Society for Blood and Marrow Transplantation [EBMT] risk score).12 Alternative donors became available in 1989 using cord blood and haploidentical donors by ex vivo or in vivo T-cell depletion.13,14 In 1998 reduced- intensity preparative regimens for older adults and patients with comorbidities were developed.15 Today, TRM of 5% to 10% in chP CML and 20% to 25% in advanced phase (AdP) CML remain, and GVHD represents a major complication after HSCT. After the availability of TKIs, HSCT activity in the EBMT registry continuously decreased for chP but remained stable for AP/BC (Figure 1). Nowadays, more patients in non-chP than in chP are transplanted worldwide,11 which underlines the importance of optimizing outcome by improving the timing of HSCT.
Figure 1.
Development of allogeneic stem cell transplantation for CML in Europe from 1990 to 2020 (EBMT registry) showing chP and AdP CML (AP and BC).
Oral TKI therapy in patients with chP CML resulted in an overall survival (OS) of 80% at 10 years, but only approximately 50% remained on first-generation (1G) treatment.9,16 After first, second, and third G-TKIs became available, major molecular remissions (MMR) and even treatment-free remissions were observed.17 Despite this success, a significant proportion of patients become refractory or progress, become intolerant, or develop cytopenia. Approximately 31% of patients switch from first-line to second-line therapy after 11 months.18 Reasons for switching include failure in 32%, intolerance in 57%, and other issues in 12% of patients. Recently, asciminib has demonstrated a higher MMR rate in combination with a more favorable safety profile as bosutinib.19 Despite being well tolerated overall, side effects on TKIs, especially in higher G-TKIs, occur (eg, vasculopathy up to 53% of patients on nilotinib, vascular events in 37% on ponatinib, and pleural effusion in approximately 20% on dasatinib).20,21 Other studies showed an intolerance of 16% or 7% on treatment with dasatinib (5 years) and/or imatinib (5 and 10 years).16,22
Despite HSCT being the only curative treatment, timing assumes an essential role in this process. Decisions should not be taken too early and incur unnecessary risks or too late, which could jeopardize the outcome after HSCT. Results in AdP CML (especially in BC) are poor with single TKI therapy and single HSCT (see below). Recommendations from experts in the field and published results are of fundamental importance in this process.
CLINICAL CASE 1
A 38-year-old construction worker presented with sudden fatigue, nosebleeds, and pneumonia. He had leukocytosis (112 × 109/L), thrombocytopenia (15 × 109/L), and anemia (hemoglobin level of 8.4 g/dL). Initially, an acute myeloid leukemia (AML) was suspected after the bone marrow aspiration revealed 97% blasts with a myeloid phenotype. In addition, a Philadelphia chromosome (Ph) in 20 out of 20 metaphases and a complex aberrant karyotype (including monosomy 7) were detected. A T315I mutation was described in the molecular analyses and a blast crisis (BC) of CML diagnosed.
CLINICAL CASE 2
At a routine checkup, a 60-year-old woman had 30 × 109/L leukocytes, 400 × 109/L platelets, and a hemoglobin level within a normal range. She currently experienced shortness of breath but otherwise felt healthy. After referral to a hematologist, a left shift was found in the differential but no enlargement of the lymph nodes or spleen. Since the Ph chromosome was detected in all metaphases upon bone marrow aspiration, chP CML and a low-risk EUTOS long-term-survival-score was diagnosed.
Who should undergo transplantation
Outcomes of HSCT have improved substantially during the last decades. In a real-world analysis, the Swedish registry reported an OS of 96% at 5 years in chP1 in patients with a median age of 43 years using matched donors.23 In another prospective study, the German CML study group reported 3-year OS rates of 88% and 94% after elective HSCT in high-risk chP (but a 0-1 EBMT score) and in imatinib-failure chP CML patients, respectively. TRM of only 8% was described in this multicenter study, which compares favorably to TRM of 26% in an earlier randomized study after IFN-based treatment in chP CML.24 TKI therapy with only imatinib led approximately 96% OS at 3 years in the same study.24 The European LeukemiaNet (ELN) criteria and the US National Comprehensive Cancer Network (NCCN) guidelines are updated on a regular basis and guide the treatment not only in chP CML. The difference between the 2 involves the definition of response to therapy. Transcripts higher than 10% at 3 months define patients with possible TKI-resistant disease and after 3 months with definite TKI-resistant disease (NCCN guidelines). In the ELN guidelines, transcripts higher than 10% are defined as a warning at 3 months and if confirmed within the next 3 months as failure. Failure means changing to another TKI if therapy started with 1G-TKI but to assessment for HSCT only if therapy started with 2G-TKI. In NCCN guidelines, possible TKI resistance automatically leads to evaluation for HSCT.25,26 On the other hand, the ELN recommendations specify resistance to 2G-TKI as an indication for HSCT.
HSCT results in patients with AP CML are clearly inferior to those in chP1. Before the TKI era, outcomes of HSCT in AP CML were 35% at 2 years and in the imatinib era, 59% at 2 years (compared to 88% and 94% in early chP CML).27,28 In a prospective study, Jiang et al demonstrated an advantage for HSCT over TKI in AP CML (6-year OS, 83.3% vs 51.4%).29 Similar results of 50% to 60% OS at 5 years after imatinib, nilotinib, and dasatinib (60%-70% OS and 10% MMR at 2 years) and bosutinib (60% OS and 11% MMR at 4 years) were reported with TKI monotherapy.30 Ponatinib had slightly higher response rates (84% OS and 34% MMR at 1 year), but randomized comparisons are lacking. Patients with de novo AP CML treated with nilotinib or dasatinib (70% MMR and 90% OS at 3 years, respectively) have been reported to have superior results than AP CML that develops while on therapy.30 Patients with AP CML under treatment should immediately be considered for HSCT, while de novo AP CML might become eligible for HSCT if the response to TKIs is not optimal.
Recommendations according to the ELN and to the NCCN regarding allogeneic stem cell transplantation are outlined in Table 1.
Table 1.
Recommendations for allogeneic stem cell transplantation in CML according to the ELN and the NCCN
| Chronic phase (chP) | Accelerated phase (AP) | Blast phase (BC) |
|---|---|---|
|
ELN 202025 - Disease resistant or intolerant (suboptimal response to 2 or more TKIs) - For the very rare patient with inadequate recovery of normal hematopoiesis - Resistance to 2G-TKIs (first or second line) ponatinib or experimental agent - Failure to respond to ponatinib after 3 months' treatment - Emergence of high-risk cytogenetics: observe closely, consider intensification of treatment (ponatinib, early allo-SCT) |
ELN 202025 - A patient presenting in AP should be treated as a high-risk patient, becoming eligible for HSCT if the response is not optimal - A patient progressing to AP during treatment should immediately be considered for HSCT |
ELN 202025 - Attempt at return to chP2 - Addition of chemotherapy based on AML regimens for myeloid BP (such as dasatinib or ponatinib + FLAG-IDA) or ALL regimens for lymphoid BP (such as imatinib or dasatinib + hyperfractionated CVAD) recommended - After CP2 is achieved proceed to allo-SCT without delay - Transplantation in active BP is not recommended |
|
NCCN guidelines26 - If TKI-resistant disease BCR-ABL1 (IS) >10% at >3 months, switch to alternate TKI and evaluate for HSCT |
NCCN guidelines26 - Disease progression to AP while on TKI therapy should be considered for HSCT - Patients who present with AP at diagnosis should be treated with a TKI, followed by evaluation for allogeneic HSCT based on response to therapy after 3, 6, or 12 months |
NCCN guidelines26 - Recommendation does not depend on response - After therapy with morphology-based induction chemotherapy + TKI in lymphoid and myeloid blast crisis or TKI plus steroids in lymphoid blast crisis and sole TKI in myeloid blast crisis |
CVAD, chemotherapy combination used to treat some types of acute lymphoblastic leukemia (ALL) and non-Hodgkin lymphoma (NHL). Hyper-CVAD includes the drugs cyclophosphamide, vincristine sulfate, doxorubicin hydrochloride (Adriamycin), and dexamethasone; FLAG-IDA, fludarabine, high-dose cytosine arabinoside (AraC), idarubicin, and granulocyte colony-stimulating factor (G-CSF); IS, international scale.
Although AdP CML occurs in a minority of patients (de novo 10%; 5% on dasatinib and 7% on imatinib develop AdP after 5 years), outcomes are inferior to chP CML after HSCT and TKIs alone. Outcomes of BC HSCT in the pre-imatinib era were reported to be only 21% OS at 2 years.28 1G-TKIs in patients with BC resulted in a median OS of 7 to 10 months, while treatment with 2G-TKIs (nilotinib or dasatinib) resulted in an OS of 32% and 30% at 2 years, respectively. In a retrospective study with 104 patients, 1-3G-TKIs plus intensive chemotherapy (IC) and TKIs plus hypomethylating agents led to a higher rate of CRi (57.5% vs 33%), a higher complete CyR rate (45% vs 10.7%), and more patients proceeding to HSCT (32.5% vs 10.7%) than TKIs or IC alone. Long-term results were similar in the combinations and clearly inferior to TKIs or IC alone (OS, 30%-28% vs 13%-0% at 5 years).31 HSCT resulted in long-term OS in patients with advanced CML (34% CI, 23-46, at 15 years). OS was improved in non-BC patients at HSCT with donors 36 years of age or younger and with a higher CD34+ cell dose in the graft.32 The ELN and NCCN provide information on induction chemotherapy according to AML-based morphology and acute lymphocytic leukemia treatment. The ELN emphasizes the need to attempt to return to chP CML with subsequent HSCT without delay and that patients with untreated BC should not undergo HSCT. A study found that in patients in remission for BC, conventional risk factors such as advanced age, poor performance status, a longer interval from diagnosis to HSCT, myeloablative conditioning (MAC), and unrelated donors remained the major determinants of outcome, whereas in those with active BC at transplant, unrelated donor transplantation was associated with prolonged leukemia-free survival (LFS).33 Similar results for advanced CML in the AP or BC or pretreated with TKIs beyond frontline therapy have been reported by other investigators and are listed in Table 2.34-41 The emergence of high-risk additional chromosomal aberrations (ACAs; high-risk ACAs include +8, a second Ph chromosome, i(17q), +19, −7/7q-, 11q23, 3q26.2, and complex aberrant karyotypes) predict a poorer response to TKIs and a higher risk of progression. According to ELN criteria, patients with high-risk ACAs are considered high-risk patients,25 and they should be observed and considered for intensification of treatment, including early HSCT. Gene mutations (RUNX1, ASXL1, IKZF1, WT1, TET2, IDH1/2, CBFB/MYH11, TP53) are found in CML and might be associated with progression to BC.42,43 Such mutations may lead to a genetically based risk classification in the future with the potential for combination with non–BCR-ABL1 targeted therapy. The molecular landscape of mutations, especially concerning epigenetics, has been featured in recent publications.44
Table 2.
Selection of CML studies using HSCT including patients beyond frontline therapy
| Authors | Number of patients | HSCT y | Disease stage (patient %) | TKI used before HSCT (patient %) | TRM % | DFS/LFS/PFS/RI % | OS % | Study type |
|---|---|---|---|---|---|---|---|---|
| chP | ||||||||
| Chaudhury et al34 | 449 177 (<18 y) 272 (18-29 y) |
2001-2010 | chP1 (100) | TKI (60) <18 y TKI (48) 18-29 y |
13 (at 1 y), 18 (at 3 y), 20 (at 5 y) | LFS 59% 57 (<18 y) 60 (18-29 y) n.s. |
75% OS (at 5 y) 76% (<18 y) 74% (18-29 y) n.s. |
Retrospective, multicenter, children and young adults (CIBMTR) |
| Yassine et al35 | 199 (adults) 97 (children/adults) |
Meta- analysis | chP (100) | Meta-analysis | 20 (adults) 28 (children/adults) |
Adult DFS 66%, adults/children DFS 47%/PFS 82% |
Adults 84%, children 91%, adults/children 76% |
Meta-analysis resistant/intolerant chP to >1 TKI |
| AP and BC | ||||||||
| Jiang et al29 | 132 | 2001-2008 | AP (100) | Imatinib (66%) Imatinib + HSCT (34) |
11 | Low risk: imatinib 85% HSCT 95% (PFS at 6 y) High risk: imatinib 19% HSCT 100% (PFS at 5 y) |
Low risk: imatinib 100% HSCT 81% (OS at 6 y) High risk: imatinib 18% HSCT 100% (OS at 5 y) |
Prospective single-center study (imatinib vs HSCT) |
| Khoury et al57 | 449 | 1999-2004 | chP2 (41), AP (41), BC (18) | Imatinib (50) | chP2 33, AP 34, BC 46 (at 1 y) | chP2 27%, AP 37%, BC 10% (LFS at 3 y) |
chP2 36%, AP 43%, BC 14% (OS at 3 y) |
Retrospective multicenter study (CIBMTR) |
| Zheng et al36 | 32 | 2002-2011 | AP (59), BC (41) | Imatinib (53) | Cord 38, sib 12 (at 0.5 y) |
Cord 50% sib 40% (LFS at 5 y) |
Cord 62%, Sib 49% (OS at 5 y) |
Retrospective single-center study (cord vs sib) |
| Radujkovic et al33 | 170 | 2004-2016 | BC in 2 chP (56) BC active (44) |
1G-TKI (59), 2G-TKI (33), 3G-TKI (8) | 19.7 (at 1 y) 23.3 (at 3 y) Active BC: 27.1% 3 y BC in remission: 20.2% 3 y |
LFS 34.6, RI 45.7 (at 1 y). LFS 26.1, RI 50.7 (at 3 y) LFS: active BC: 11.6% 3 y BC in remission 33.8% 3 y RI: active BC: 56.4.6% 3 y BC in remission 45.9% 3 y |
57.5%(at 1 y) 38.5 (at 3 y) Active BC: 23.8% (3 y) BC in remission 51% (3 y) |
Retrospective EBMT study HSCT in treated vs untreated BC |
| Yang et al41 | 278 | 2002-2021 | de novo AP (100) | Imatinib (67) or 2G-TKI (33; nilotinib 24, dasatanib 7, flumatinib 1) | Censored at HSCT | TFS 89% (at 6 y) Low risk 95 (5 y) Interm 76 (5 y) High-risk 19 (5 y) No significance between 1G-TKI versus 2G for TFS |
OS 90% (at 6 y) Low risk 54 (5 y) Interm. 36 (5 y) High-risk 10 (5 y) No significance between 1G-TKI vs 2G for OS |
Comparison between imatinib and 2G-TKI before HSCT |
| Different disease phase | ||||||||
| Saussele et al24 | 84 | 2003-2008 | chP1 (TKI) (23), chP1 (TKI failure) (44), AP (4), BC (30) | Imatinib | 8 in chP (at 3 y) 18 in AdP (at 3 y) |
CMR at last PCR 88% | chP1 (elective) 88%, chP1 (imatinib failure) 94%, AP 59% (OS at 3 y) |
Prospective multicenter study (CML IV study) |
| Jabbour et al55 | 47 | 2004-2007 | chP1 (34), chP2 (21), AP (25), BC (19) | Imatinib failure (100) + 2G-TKI (62) |
13% (at 2 y) | 49% (EFS at 2 y) (mutation 36% vs no mutation 58%) | 63% (OS at 2y) (mutation 44% vs no mutation 76%) | Retrospective single-center study |
| Topcuoglu et al37 | 84 | 1989-2007 | chP1 (79), chP2 (6), AP (15) | NA | 7% RIC 14% MAC |
48% (LFS at 5 y) No difference RIC vs MAC | 56% (OS at 5 y) No difference RIC vs MAC | Retrospective single-center study (RIC vs MAC) |
| Oyekunle et al38 | 68 | 2002 – 2009 | chP1 (40), >chP1 (60) | Pre-HSCT TKI (71), post-HSCT TKI (29) |
NA | 54% (LFS at 2 y) | 63% (OS at 2 y) | Single institute HSCT in TKI era |
| Milojkovic et al51 | 5732 | 2000-2011 | Prior TKI: chP (51), chP >1 2(59), AP (14), BC (10), no-TKI: NR |
Prior TKI (22), no TKI (78) |
NA | Non-TKI 46% Prior TKI 42% (PFS at 5 y) |
Non-TKI 61% Prior TKI 59% (OS at 5 y) |
Retrospective multicenter study (EBMT) |
| Piekarska et al39 | 25 | 2008-2013 | chP1 (50), chP2/AP (29), BC (21) | Dasatinib (53), nilotinib (18), or both (29) | 7.1 (chP1), 12.5 (chP2/AP); 50 (BC) | RI: 29.6% RI: chP1 21.4% RI: chP2/AP 12.5% RI: BP 50% |
chP1 92.9%, chP2/AP 85.7% BP 0% (at 1 or 3 y) |
Prospective |
| Lubking et al23 | 118 | 2002-2017 | chP1 (47.5), chP >1 (40.7), AP/BC (11.9) | Imatinib (39.8), imatinib +2G-TKI (33.1), imatinib +2G-TKI +3G-TKI (5.1), 2G-TKI (13.6), 2G-TKI +3G-TKI (5.1), no TKI (3.4) | 11.6 in chP ≥1 (at 5 y) 23.1 in AP/BC (at 5 y) |
chP: 66% molec relapse (at 2 y) AP/BC: 71.4% progress to AP/BC 50% to AdP in chP >1 |
chP 96,3% 70.1% > chP1/AP 36.9% BP AP/BP to chP 70.1% chP TKI resist. 96.8% (all at 5 y) |
Swedish registry study |
| Hu et al40 | 1223 | 2001-2013 | chP1 (60), chP2 (21), AP (12), BC (7), progression to AP/BC (19) | TKI 1 (median, range 0–3) | 10–20 (at 1 y) | NA | chP 1 HSCT (vs non-HSCT inferior OS, HR 2.4) No difference chP2 and AP; BC trend favoring HSCT |
Life expectancy calculation in comparison to no HSCT (CIBMTR) |
| Niederwieser et al27 | 147 | 1990-2018 | Non-BC (75) BC (25) |
Prior TKI: 1G (27.2); 1G + 2G (13.6); 1G + 3G (0.7); 2G ± 3G (38.1); 3G (0.7) |
28 (at 15 y) 24 in BC (at 5 y) 24 non-BC (at 5 y) |
30% at 10 y and 26% at 15 y BP 24% 5 y Non-BP 31% 5 y |
OS 15 y 34% BP 30% 10 y; 30% 5 y non-BP 41% 10 y; 44% 5 y |
Bicentric retrospective study Long-term follow-up |
| Masouridi-Levrat et al50 | 383 | 2009-2013 | chP1 (38) AP > chP1 (45) BC (16) |
Prior TKI: dasatinib (40) or nilotinib (17) or sequential ± bosutinib/ponatinib (43) |
18 (at 1 y) 24% (at 5 y) No difference between 2G-TKIs |
RFS 40% (at 5 y) RI 29% (at 2 y) RI 36% (at 5 y) |
65% (at 2 y) 56% (at 5 y) chP1 67% AP/chP >1 57% BC 37% |
EBMT study, retrospective study |
CMR, complete molecular response; cord, cord blood; NA, not available; n.s., not significantly different; PCR, polymerase chain reaction; PFS, progression-free survival; RI, relapse incidence; sib, sibling; TFS, transformation-free survival.
Optimal preconditions for HSCT are a low CI Sorror score and good performance status, in addition to the requirement for a suitable donor, preferably a human leukocyte antigen (HLA)–compatible sibling followed by an unrelated donor (10 out of 10 matches).45 If no matched donor is available, alternative donors, such as haploidentical HSCT with post cyclophosphamide or mismatched donors or cord blood, should be taken into consideration.46-49
In addition, HSCT is feasible in patients previously treated with 2G-TKIs with a posttransplant complication rate comparable to that of TKI-naive or imatinib-treated patients.50
CLINICAL CASE 1 (Continued)
The patient was treated with an AML-like induction chemotherapy in combination with ponatinib, a 3G-TKI to overcome the resistance to the T315I mutation. After reaching chP, the patient was referred to an HSCT program.
CLINICAL CASE 2 (Continued)
After therapy with hydroxyurea, the patient was started on the 1G-TKI imatinib. Her response according to ELN criteria was optimal after 3 months. After she discussed the possibility of HSCT with her hematologist, it was decided to continue TKI therapy under continuous BCR-ABL1 monitoring.
Timing: when to perform a transplant
It is generally acceptable to start first-line therapy with TKIs (first or second generation) in chP CML without affecting the outcome of HSCT.25 The response and tolerance to the TKI determine further treatment. The response to the TKI depends on the EUTOS long-term survival score and the presence of high-risk cytogenetics and TKI mutations.51 The presence of the T315I mutation, which is responsive to ponatinib, is a trigger for HSCT.
The ELN provides regular recommendations on how to manage TKI treatment according to BCR-ABL1 transcript reduction at defined time points.52 BCR-ABL1 transcripts higher than 10% at 3 and 6 months of treatment and higher than 1% at 12 months are considered treatment failures and should lead to second-line TKI treatment (either 2G- or 3G-TKI or a TKI responsive to the detected mutation). A donor search should be initiated upon resistance to 2G-TKI treatment.25 Approximately 65% respond to second-line treatment with BCR-ABL1 transcripts of less than or equal to 10%. Nonresponding patients (>10% transcripts at 3 months) have durable CyR of only 50% at 4 years.51
HSCT in early chP CML has been shown to have the best outcome, even after first-line TKI resistance.12 In addition, TKI therapy before HSCT has been associated with better posttransplant outcomes.32 A Center for International Blood and marrow Transplant Research (CIBMTR) study confirmed the beneficial effect of pretransplant TKIs in chP CML for posttransplant survival.53 Delaying HSCT to late chP CML incurs the risk of progression to AdP disease, with unfavorable results. Patients not eligible for HSCT (>80 years of age) should continue on 3G-TKIs or new inhibitors in the testing phase. In pediatric patients, lifelong TKI therapy, including side effects, needs to be balanced with an increased HSCT TRM at the beginning and a possible increased morbidity with chronic GVHD.54
The goal in advanced CML is a return to a chP followed by HSCT. The choice of pretransplant TKIs for AdP CML is not well standardized, but dasatinib and nilotinib have at least safely been administered before HSCT without increased TRM.50,55 Thus, it is appropriate to use TKIs to reduce the disease burden before HSCT for AP CML. The search for a donor should be initiated at diagnosis and HSCT planned after a response (Table 2). In BC, a downgrade to chP2 should be considered a clinical condition requiring, whenever possible, treatment with a combination of TKIs with IC or TKIs with hypomethylating agents followed by HSCT.31 The combination of TKIs plus IC with HSCT has been shown to result in 54% OS at 2 years in AdP CML.27 HSCT remains a unique therapeutic option for patients in chP CML after the failure of 2 TKIs or in those potentially harboring the T315I mutation (after a trial of ponatinib therapy).56
CLINICAL CASE 1 (Continued)
After weighing the pros and cons, the patient decided to undergo HSCT from the HLA-matched brother at a JACIE-certified transplant center. Three months after diagnosis, he underwent peripheral blood HSCT.
CLINICAL CASE 2 (Continued)
After 2 years of optimal response, the patient showed increased BCR-ABL1 transcripts. Molecular analyses detected V299L resistant to dasatinib and Y253H resistant to nilotinib, but both were sensitive only to ponatinib. Treatment with ponatinib was started. Since her 70-year-old brother, her only sibling, had CLL, an unrelated donor search was initiated. Following intolerance to ponatinib (causing headaches and vomiting) but after achieving BCR-ABL1 negativity and lacking access to asciminib, an HSCT was considered.
How to manage transplant therapies
In a CIBMTR study, the prognostic favorable factors for LFS and OS after HSCT in advanced CML were the time from diagnosis to transplantation, good performance status, and access to an HLA fully matched donor.57
In an EBMT study, risk factors for poorer survival were active BC at transplant, advanced age (>45 years), low performance status, a longer interval from diagnosis to transplant, MAC, and the use of an unrelated donor.33
Other studies reported that a low CD34+ cell count in the graft and a higher donor age were adverse risk factors for OS.27 Although no prospective randomized study exists, reduced intensity conditioning (RIC) seems to be a feasible approach that increases accessibility to the transplant procedure.58 Whether younger patients and patients without comorbidities should be transplanted after RIC instead of MAC is still a matter of debate. Similar OS but lower chronic GVHD rates were observed in RIC when compared to MAC.59 RIC may be a reasonable alternative to MAC in the TKI era, but results should be confirmed in a randomized study. However, due to the high risk of relapse in AdP CML, patients who can tolerate MAC should receive it.
Ex vivo T-cell depletion is associated with a high relapse risk, but it has been observed that using anti–T-lymphocyte globulin within the conditioning regimen reduces the incidence of GVHD without increasing the risk of relapse.60
The detection of BCR-ABL1 transcripts early after HSCT has no adverse prognostic significance. However, BCR-ABL1 transcripts (persistently negative, fluctuating, or persistently positive) 6 months post transplant predict a risk of relapse.61 Several reports suggest that early posttransplant TKIs (including 2G- TKIs) are safe to administer effectively in chP CML but are less effective in AdP CML.62,63 Maintenance therapy with TKIs with or without DLIs appears to be safe and has been associated with a lower incidence of extensive chronic GVHD.27,61 Continued regular long-term monitoring of BCR-ABL1 transcripts is required to anticipate the occasional late relapsing patient; however, both the optimal frequency of monitoring and the threshold of BCR-ABL1 transcripts for preemptive therapy with TKIs or DLIs need to be established in the contexts of conditioning regimen and graft manipulation. Although the use of posttransplant TKI therapy is widespread, prospective studies are needed to explore the best TKI dose, the treatment duration, and possible coadministration with DLIs.
A relapse of CML can occur as late as the second decade after HSCT and involves molecular, cytogenetic, and hematological relapse.5 Relapsed CML has been treated with DLIs, TKIs, chemotherapy, and second HSCTs.27,64-67 Combinations of TKI therapy and DLIs can achieve a 5-year postrelapse survival rate of 62%, and some patients became TKI-free, suggesting a persistent graft-versus-leukemia effect.67 Molecular remission without GVHD can be achieved, especially when DLIs were given beyond 1 year from HSCT for molecular or cytogenetic relapse.68
CLINICAL CASE 1 (Continued)
The patient underwent a transplant, after conditioning with fludarabine and myeloablative busulfan, from an HLA-identical brother and, except for neutropenic fever, had an uneventful posttransplant period. During immunosuppression tapering, he developed mild chronic skin GVHD. However, BCR-ABL1 transcripts were still detected 6 months after HSCT. Because of a high risk of relapse, ponatinib was restarted, and the BCR-ABL1 transcripts became negative in the blood. After consultation with his physician following continuous negative BCR-ABL1 transcripts, the patient opted to terminate TKI treatment 5 years post transplant.
CLINICAL CASE 2 (Continued)
A matched unrelated donor was found, and after RIC with busulfan/fludarabine, HSCT was performed without complications. BCR-ABL1 transcripts remained undetectable post HSCT. No TKI prophylaxis was given, and the patient remained BCR-ABL1-negative at 5 years after HSCT.
Summary
Rapid developments in the treatment of CML require continual adaptation regarding indications for curative stem cell transplantation. Patients with chP CML should be started with 1G- or 2G-TKIs and monitored according to ELN or NCCN guidelines. The emergence of high-risk ACAs predict a poorer response to TKIs and a higher risk of progression and are triggers for HSCT. Patients with resistant disease (NCCN) or failure (ELN) should be regarded as candidates for HSCT. Patients with resistance to G2-TKIs should be considered for HSCT if they are not responding to G3 after 3 months. An HLA-identical related or fully matched unrelated donor should be selected, and the intensity of the conditioning regimen should be adjusted according to age and comorbidities. Patients in AP and BC CML should be started on IC with the possible addition of TKIs and are candidates for HSCT. Posttransplant monitoring with quantitative polymerase chain reaction testing is indicated to guide prophylactic or preemptive TKI treatment with or without DLIs.
Contributor Information
Christian Niederwieser, Department of Stem Cell Transplantation, University Medical Center Hamburg-Eppendorf, Germany.
Nicolaus Kröger, Department of Stem Cell Transplantation, University Medical Center Hamburg-Eppendorf, Germany.
Conflict-of-interest disclosure
Christian Niederwieser: no competing financial interests to declare.
Nicolaus Kröger: research funding: Bristol Myers Squibb, Jazz, Neovii, Novartis, Riemser; honoraria: Bristol Myers Squibb, Gilead, Jazz, Neovii, Novartis, Riemser, Sanofi.
Off-label drug use
Christian Niederwieser: nothing to disclose.
Nicolaus Kröger: nothing to disclose.
References
- 1.Nowell P, Hungerford D. A minute chromosome in human chronic granulocytic leukemia. Blut. 1962;8(April):65-66. doi: 10.1007/BF01630378. [DOI] [PubMed] [Google Scholar]
- 2.Rowley JD. Letter: a new consistent chromosomal abnormality in chronic myelogenous leukaemia identified by quinacrine fluorescence and Giemsa staining. Nature. 1973;243(5405):290-293. doi: 10.1038/243290a0. [DOI] [PubMed] [Google Scholar]
- 3.Groffen J, Stephenson J, Heisterkamp N, Deklein A, Bartram C, Grosveld G. Philadelphia chromosomal breakpoints are clustered within a limited region, bcr, on chromosome 22. Cell. 1984;36(1):93-99. doi: 10.1016/0092-8674(84)90077-1. [DOI] [PubMed] [Google Scholar]
- 4.Shtivelman E, Lifshitz B, Gale RP, Canaani E. Fused transcript of abl and bcr genes in chronic myelogenous leukaemia. Nature. 1985;315(6020):550-554. doi: 10.1038/315550a0. [DOI] [PubMed] [Google Scholar]
- 5.Goldman JM, Majhail NS, Klein JP, et al.. Relapse and late mortality in 5-year survivors of myeloablative allogeneic hematopoietic cell transplantation for chronic myeloid leukemia in first chronic phase. J Clin Oncol. 2010;28(11):1888-1895. doi: 10.1200/JCO.2009.26.7757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Talpaz M, Kantarjian HM, McCredie K, Trujillo JM, Keating MJ, Gutterman JU. Hematologic remission and cytogenetic improvement induced by recombinant human interferon alpha A in chronic myelogenous leukemia. N Engl J Med. 1986;314(17):1065-1069. doi: 10.1056/NEJM198604243141701. [DOI] [PubMed] [Google Scholar]
- 7.Lee MS, Chang KS, Freireich EJ, et al.. Detection of minimal residual bcr/abl transcripts by a modified polymerase chain reaction. Blood. 1988;72(3):893-897. [PubMed] [Google Scholar]
- 8.Kolb HJ, Mittermüller J, Clemm C, et al.. Donor leukocyte transfusions for treatment of recurrent chronic myelogenous leukemia in marrow transplant patients. Blood. 1990;76(12):2462-2465. doi: 10.1182/blood.V76.12.2462.bloodjournal76122462 [DOI] [PubMed] [Google Scholar]
- 9.Druker BJ, Talpaz M, Resta DJ, et al.. Efficacy and safety of a specific inhibitor of the BCR-ABL tyrosine kinase in chronic myeloid leukemia. N Engl J Med. 2001;344(14):1031-1037. doi: 10.1056/NEJM200104053441401. [DOI] [PubMed] [Google Scholar]
- 10.Mahon FX, Réa D, Guilhot J, et al; Intergroupe Français des Leucémies Myéloïdes Chroniques. Discontinuation of imatinib in patients with chronic myeloid leukaemia who have maintained complete molecular remission for at least 2 years: the prospective, multicentre Stop Imatinib (STIM) trial. Lancet Oncol. 2010;11(11):1029-1035. doi: 10.1016/S1470-2045(10)70233-3. [DOI] [PubMed] [Google Scholar]
- 11.Niederwieser D, Baldomero H, Bazuaye N, et al.. One and a half million hematopoietic stem cell transplants: continuous and differential improvement in worldwide access with the use of non-identical family donors. Haematologica. 2022;107(5):1045-1053. doi: 10.3324/haematol.2021.279189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gratwohl A, Hermans J, Goldman JM, et al.. Risk assessment for patients with chronic myeloid leukaemia before allogeneic blood or marrow transplantation. Chronic Leukemia Working Party of the European Group for Blood and Marrow Transplantation. Lancet. 1998;352(9134):1087-1092. doi: 10.1016/s0140-6736(98)03030-x. [DOI] [PubMed] [Google Scholar]
- 13.Gluckman E, Broxmeyer HA, Auerbach AD, et al.. Hematopoietic reconstitution in a patient with Fanconi's anemia by means of umbilical-cord blood from an HLA-identical sibling. N Engl J Med. 1989;321(17):1174-1178. doi: 10.1056/NEJM198910263211707. [DOI] [PubMed] [Google Scholar]
- 14.Luznik L, O'Donnell PV, Fuchs EJ. Post-transplantation cyclophosphamide for tolerance induction in HLA-haploidentical bone marrow transplantation. Semin Oncol. 2012;39(6):683-693. doi: 10.1053/j.seminoncol.2012.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Slavin S, Nagler A, Naparstek E, et al.. Nonmyeloablative stem cell transplantation and cell therapy as an alternative to conventional bone marrow transplantation with lethal cytoreduction for the treatment of malignant and nonmalignant hematologic diseases. Blood. 1998;91(3):756-763. 10.1182/blood.V91.3.756 [DOI] [PubMed] [Google Scholar]
- 16.Hochhaus A, Larson RA, Guilhot F, et al; IRIS Investigators. Long-term outcomes of imatinib treatment for chronic myeloid leukemia. N Engl J Med. 2017;376(10):917-927. doi: 10.1056/NEJMoa1609324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mahon FX, Delbrel X, Cony-Makhoul P, et al.. Follow-up of complete cytogenetic remission in patients with chronic myeloid leukemia after cessation of interferon alfa. J Clin Oncol. 2002;20(1):214-220. doi: 10.1200/JCO.2002.20.1.214. [DOI] [PubMed] [Google Scholar]
- 18.Kohlbrenner K, Fabarius A, Reiser M, et al. Therapy in patients with chronic myeloid leukemia outside of clinical trials: results of the German CML- registry (CML-VI). Paper presented at: European Society of Hypertension 31st European Meeting; 17-20 June 2022; Athens, Greece.
- 19.Réa D, Mauro MJ, Boquimpani C, et al.. A phase 3, open-label, randomized study of asciminib, a STAMP inhibitor, vs bosutinib in CML after 2 or more prior TKIs. Blood. 2021;138(21):2031-2041. doi: 10.1182/blood.2020009984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pasvolsky O, Leader A, Iakobishvili Z, Wasserstrum Y, Kornowski R, Raanani P. Tyrosine kinase inhibitor associated vascular toxicity in chronic myeloid leukemia. Cardiooncology. 2015;1(1):5. doi: 10.1186/s40959-015-0008-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brixey AG, Light RW. Pleural effusions due to dasatinib. Curr Opin Pulm Med. 2010;16(4):351-356. doi: 10.1097/MCP.0b013e328338c486. [DOI] [PubMed] [Google Scholar]
- 22.Cortes JE, Saglio G, Kantarjian HM, et al.. Final 5-year study results of DASISION: the Dasatinib versus Imatinib Study in Treatment-Naïve Chronic Myeloid Leukemia Patients trial. J Clin Oncol. 2016;34(20):2333-2340. doi: 10.1200/JCO.2015.64.8899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lübking A, Dreimane A, Sandin F, et al.. Allogeneic stem cell transplantation for chronic myeloid leukemia in the TKI era: population-based data from the Swedish CML registry. Bone Marrow Transplant. 2019;54(11):1764-1774. doi: 10.1038/s41409-019-0513-5. [DOI] [PubMed] [Google Scholar]
- 24.Saussele S, Lauseker M, Gratwohl A, et al; German CML Study Group. Allogeneic hematopoietic stem cell transplantation (allo SCT) for chronic myeloid leukemia in the imatinib era: evaluation of its impact within a subgroup of the randomized German CML Study IV. Blood. 2010;115(10):1880-1885. doi: 10.1182/blood-2009-08-237115. [DOI] [PubMed] [Google Scholar]
- 25.Hochhaus A, Baccarani M, Silver RT, et al.. European LeukemiaNet 2020 recommendations for treating chronic myeloid leukemia. Leukemia. 2020;34(4):966-984. doi: 10.1038/s41375-020-0776-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Deininger MW, Shah NP, Altman JK, et al.. Chronic myeloid leukemia, version 2.2021, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2020;18(10):1385-1415. doi: 10.6004/jnccn.2020.0047. [DOI] [PubMed] [Google Scholar]
- 27.Niederwieser C, Morozova E, Zubarovskaya L, et al.. Risk factors for outcome after allogeneic stem cell transplantation in patients with advanced phase CML. Bone Marrow Transplant. 2021;56(11):2834-2841. doi: 10.1038/s41409-021-01410-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gratwohl A, Brand R, Apperley J, et al; Chronic Leukemia Working Party of the European Group for Blood and Marrow Transplantation. Allogeneic hematopoietic stem cell transplantation for chronic myeloid leukemia in Europe 2006: transplant activity, long-term data and current results. An analysis by the Chronic Leukemia Working Party of the European Group for Blood and Marrow Transplantation (EBMT). Haematologica. 2006;91(4):513-521. [PubMed] [Google Scholar]
- 29.Jiang Q, Xu LP, Liu DH, et al.. Imatinib mesylate versus allogeneic hematopoietic stem cell transplantation for patients with chronic myelogenous leukemia in the accelerated phase. Blood. 2011;117(11):3032-3040. doi: 10.1182/blood-2010-09-308510. [DOI] [PubMed] [Google Scholar]
- 30.How J, Venkataraman V, Soriano Hobbs G. Blast and accelerated phase CML: room for improvement. ASH Educational Program. 2021;2021(1):122-128. doi: 10.1182/hematology.2021000240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Saxena K, Jabbour E, Issa G, et al.. Impact of frontline treatment approach on outcomes of myeloid blast phase CML. J Hematol Oncol. 2021;14(1): 94. doi: 10.1186/s13045-021-01106-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oehler VG, Gooley T, Snyder DS, et al.. The effects of imatinib mesylate treatment before allogeneic transplantation for chronic myeloid leukemia. Blood. 2007;109(4):1782-1789. doi: 10.1182/blood-2006-06-031682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Radujkovic A, Dietrich S, Blok HJ, et al.. Allogeneic stem cell transplantation for blast crisis chronic myeloid leukemia in the era of tyrosine kinase inhibitors: a retrospective study by the EBMT Chronic Malignancies Working Party. Biol Blood Marrow Transplant. 2019;25(10):2008-2016. doi: 10.1016/j.bbmt.2019.06.028. [DOI] [PubMed] [Google Scholar]
- 34.Chaudhury S, Sparapani R, Hu ZH, et al.. Outcomes of allogeneic hematopoietic cell transplantation in children and young adults with chronic myeloid leukemia: a CIBMTR cohort analysis. Biol Blood Marrow Transplant. 2016;22(6):1056-1064. doi: 10.1016/j.bbmt.2016.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yassine F, Reljic T, Moustafa MA, et al.. Efficacy of allogeneic hematopoietic cell transplantation in patients with chronic phase CML resistant or intolerant to tyrosine kinase inhibitors [published online ahead of print 11 March 2022]. Hematol Oncol Stem Cell Ther. doi: 10.1016/j.hemonc.2021.02.003. [DOI] [PubMed] [Google Scholar]
- 36.Zheng C, Tang B, Yao W, et al.. Comparison of unrelated cord blood transplantation and HLA-matched sibling hematopoietic stem cell transplantation for patients with chronic myeloid leukemia in advanced stage. Biol Blood Marrow Transplant. 2013;19(12):1708-1712. doi: 10.1016/j.bbmt.2013.09.008. [DOI] [PubMed] [Google Scholar]
- 37.Topcuoglu P, Arat M, Ozcan M, et al.. Case-matched comparison with standard versus reduced intensity conditioning regimen in chronic myeloid leukemia patients. Ann Hematol. 2012;91(4):577-586. doi: 10.1007/s00277-011-1349-2. [DOI] [PubMed] [Google Scholar]
- 38.Oyekunle A, Zander AR, Binder M, et al.. Outcome of allogeneic SCT in patients with chronic myeloid leukemia in the era of tyrosine kinase inhibitor therapy. Ann Hematol. 2013;92(4):487-496. doi: 10.1007/s00277-012-1650-8. [DOI] [PubMed] [Google Scholar]
- 39.Piekarska A, Gil L, Prejzner W, et al.. Pretransplantation use of the second-generation tyrosine kinase inhibitors has no negative impact on the HCT outcome. Ann Hematol. 2015;94(11):1891-1897. doi: 10.1007/s00277-015-2457-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hu B, Lin X, Lee HC, et al.. Timing of allogeneic hematopoietic cell transplantation (alloHCT) for chronic myeloid leukemia (CML) patients. Leuk Lymphoma. 2020;61(12):2811-2820. doi: 10.1080/10428194.2020.1783444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yang S, Zhang XS, Gale RP, et al.. Co-variates associated with outcomes of tyrosine kinase-inhibitor therapy in persons with chronic myeloid leukaemia initially presenting in accelerated phase. Leukemia. 2022;36(7):1818-1824. doi: 10.1038/s41375-022-01583-4 [DOI] [PubMed] [Google Scholar]
- 42.Hehlmann R. The new ELN recommendations for treating CML. J Clin Med. 2020;9(11):3671. doi: 10.3390/jcm9113671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McKenney AS, Levine RL. Isocitrate dehydrogenase mutations in leukemia. J Clin Invest. 2013;123(9):3672-3677. doi: 10.1172/JCI67266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Adnan-Awad S, Kankainen M, Mustjoki S. Mutational landscape of chronic myeloid leukemia: more than a single oncogene leukemia. Leuk Lymphoma. 2021;62(9):2064-2078. doi: 10.1080/10428194.2021.1894652. [DOI] [PubMed] [Google Scholar]
- 45.Sorror ML, Maris MB, Storer B, et al.. Comparing morbidity and mortality of HLA-matched unrelated donor hematopoietic cell transplantation after nonmyeloablative and myeloablative conditioning: influence of pretransplantation comorbidities. Blood. 2004;104(4):961-968. doi: 10.1182/blood-2004-02-0545. [DOI] [PubMed] [Google Scholar]
- 46.Mielcarek M, Furlong T, O'Donnell PV, et al.. Posttransplantation cyclophosphamide for prevention of graft-versus-host disease after HLA-matched mobilized blood cell transplantation. Blood. 2016;127(11):1502-1508. doi: 10.1182/blood-2015-10-672071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen H, Si Y, He X, et al.. HLA-mismatched hematopoietic stem cell transplantation for treatment of chronic myelogenous leukemia. Blood. 2008;112(11):1113-1113. doi: 10.1182/blood.V112.11.1113.1113. [DOI] [Google Scholar]
- 48.Xiao-Jun H, Lan-Ping X, Kai-Yan L, et al.. HLA-mismatched/haploidentical hematopoietic stem cell transplantation without in vitro T cell depletion for chronic myeloid leukemia: improved outcomes in patients in accelerated phase and blast crisis phase. Ann Med. 2008;40(6):444-455. doi: 10.1080/07853890801908903. [DOI] [PubMed] [Google Scholar]
- 49.Sanz J, Sanz GF. Umbilical cord blood transplantation from unrelated donors in adult patients with chronic myeloid leukaemia. Best Pract Res Clin Haematol. 2010;23(2):217-222. doi: 10.1016/j.beha.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 50.Masouridi-Levrat S, Olavarria E, Iacobelli S, et al.. Outcomes and toxicity of allogeneic hematopoietic cell transplantation in chronic myeloid leukemia patients previously treated with second-generation tyrosine kinase inhibitors: a prospective non-interventional study from the Chronic Malignancy Working Party of the EBMT. Bone Marrow Transplant. 2022;57(1):23-30. doi: 10.1038/s41409-021-01472-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Milojkovic D, Apperley JF, Gerrard G, et al.. Responses to second-line tyrosine kinase inhibitors are durable: an intention-to-treat analysis in chronic myeloid leukemia patients. Blood. 2012;119(8):1838-1843. doi: 10.1182/blood-2011-10-383000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Baccarani M, Castagnetti F, Gugliotta G, Rosti G. A review of the European LeukemiaNet recommendations for the management of CML. Ann Hematol. 2015;94(suppl 2):S141-S147. doi: 10.1007/s00277-015-2322-2. [DOI] [PubMed] [Google Scholar]
- 53.Lee SJ, Kukreja M, Wang T, et al.. Impact of prior imatinib mesylate on the outcome of hematopoietic cell transplantation for chronic myeloid leukemia. Blood. 2008;112(8):3500-3507. doi: 10.1182/blood-2008-02-141689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hafez HA, Abdallah A, Hammad M, et al.. Outcomes of allogenic hematopoietic cell transplantation for childhood chronic myeloid leukemia: single-center experience. Pediatr Transplant. 2020;24(4):e13664. doi: 10.1111/petr.13664. [DOI] [PubMed] [Google Scholar]
- 55.Jabbour E, Cortes J, Santos FP, et al.. Results of allogeneic hematopoietic stem cell transplantation for chronic myelogenous leukemia patients who failed tyrosine kinase inhibitors after developing BCR-ABL1 kinase domain mutations. Blood. 2011;117(13):3641-3647. doi: 10.1182/blood-2010-08-302679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nicolini FE, Basak GW, Kim DW, et al.. Overall survival with ponatinib versus allogeneic stem cell transplantation in Philadelphia chromosome-positive leukemias with the T315I mutation. Cancer. 2017;123(15):2875-2880. doi: 10.1002/cncr.30558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Khoury HJ, Kukreja M, Goldman JM, et al.. Prognostic factors for outcomes in allogeneic transplantation for CML in the imatinib era: a CIBMTR analysis. Bone Marrow Transplant. 2012;47(6):810-816. doi: 10.1038/bmt.2011.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Crawley C, Szydlo R, Lalancette M, et al; Chronic Leukemia Working Party of the EBMT. Outcomes of reduced-intensity transplantation for chronic myeloid leukemia: an analysis of prognostic factors from the Chronic Leukemia Working Party of the EBMT. Blood. 2005;106(9):2969-2976. doi: 10.1182/blood-2004-09-3544. [DOI] [PubMed] [Google Scholar]
- 59.Chhabra S, Ahn KW, Hu ZH, et al.. Myeloablative vs reduced-intensity conditioning allogeneic hematopoietic cell transplantation for chronic myeloid leukemia. Blood Adv. 2018;2(21):2922-2936. doi: 10.1182/bloodadvances.2018024844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zander AR, Kröger N, Schleuning M, et al.. ATG as part of the conditioning regimen reduces transplant-related mortality (TRM) and improves overall survival after unrelated stem cell transplantation in patients with chronic myelogenous leukemia (CML). Bone Marrow Transplant. 2003;32(4):355-361. doi: 10.1038/sj.bmt.1704157. [DOI] [PubMed] [Google Scholar]
- 61.Kaeda J, O'Shea D, Szydlo RM, et al.. Serial measurement of BCR-ABL transcripts in the peripheral blood after allogeneic stem cell transplantation for chronic myeloid leukemia: an attempt to define patients who may not require further therapy. Blood. 2006;107(10):4171-4176. doi: 10.1182/blood-2005-08-3320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Carpenter PA, Snyder DS, Flowers ME, et al.. Prophylactic administration of imatinib after hematopoietic cell transplantation for high-risk Philadelphia chromosome-positive leukemia. Blood. 2007;109(7):2791-2793. doi: 10.1182/blood-2006-04-019836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nakasone H, Kanda Y, Takasaki H, et al; Kanto Study Group for Cell Therapy. Prophylactic impact of imatinib administration after allogeneic stem cell transplantation on the incidence and severity of chronic graft versus host disease in patients with Philadelphia chromosome-positive leukemia. Leukemia. 2010;24(6):1236-1239. doi: 10.1038/leu.2010.83. [DOI] [PubMed] [Google Scholar]
- 64.Goldman JM, Melo JV. Chronic myeloid leukemia—advances in biology and new approaches to treatment. N Engl J Med. 2003;349(15):1451-1464. doi: 10.1056/NEJMra020777. [DOI] [PubMed] [Google Scholar]
- 65.Kim YJ, Kim DW, Lee S, et al.. Cytogenetic clonal evolution alone in CML relapse post-transplantation does not adversely affect response to imatinib mesylate treatment. Bone Marrow Transplant. 2004;33(2):237-242. doi: 10.1038/sj.bmt.1704332. [DOI] [PubMed] [Google Scholar]
- 66.DeAngelo DJ, Hochberg EP, Alyea EP, et al.. Extended follow-up of patients treated with imatinib mesylate (Gleevec) for chronic myelogenous leukemia relapse after allogeneic transplantation: durable cytogenetic remission and conversion to complete donor chimerism without graft-versus-host disease. Clin Cancer Res. 2004;10(15):5065-5071. doi: 10.1158/1078-0432.CCR-03-0580. [DOI] [PubMed] [Google Scholar]
- 67.Savani BN, Montero A, Kurlander R, Childs R, Hensel N, Barrett AJ. Imatinib synergizes with donor lymphocyte infusions to achieve rapid molecular remission of CML relapsing after allogeneic stem cell transplantation. Bone Marrow Transplant. 2005;36(11):1009-1015. doi: 10.1038/sj.bmt.1705167. [DOI] [PubMed] [Google Scholar]
- 68.Radujkovic A, Guglielmi C, Bergantini S, et al; Chronic Malignancies Working Party of the European Society for Blood and Marrow Transplantation. Donor lymphocyte infusions for chronic myeloid leukemia relapsing after allogeneic stem cell transplantation: may we predict graft-versus- leukemia without graft-versus-host disease? Biol Blood Marrow Transplant. 2015;21(7):1230-1236. doi: 10.1016/j.bbmt.2015.03.012. [DOI] [PubMed] [Google Scholar]