Abstract
Major depressive disorder (MDD) is the leading cause of disability worldwide. Treatment with antidepressant drugs (ATD), which target monoamine neurotransmitters including serotonin (5HT), are only modestly effective. Monoamine oxidase (MAO) metabolizes 5HT to 5-hydroxy indoleacetic acid (5HIAA). Genetic variants in the X-chromosome-linked MAO-encoding genes, MAOA and MAOB, have been associated with clinical improvement following ATD treatment in depressed patients. Our aim was to analyze the association of MAOA and MAOB genetic variants with (1) clinical improvement and (2) the plasma 5HIAA/5HT ratio in 6-month ATD-treated depressed individuals. Clinical (n = 378) and metabolite (n = 148) data were obtained at baseline and up to 6 months after beginning ATD treatment (M6) in patients of METADAP. Mixed-effects models were used to assess the association of variants with the Hamilton Depression Rating Scale (HDRS) score, response and remission rates, and the plasma 5HIAA/5HT ratio. Variant × sex interactions and dominance terms were included to control for X-chromosome-linked factors. The MAOA rs979605 and MAOB rs1799836 polymorphisms were analyzed. The sex × rs979605 interaction was significantly associated with the HDRS score (p = 0.012). At M6, A allele-carrying males had a lower HDRS score (n = 24, 10.9 ± 1.61) compared to AA homozygous females (n = 14, 18.1 ± 1.87; p = 0.0067). The rs1799836 polymorphism was significantly associated with the plasma 5HIAA/5HT ratio (p = 0.018). Overall, CC/C females/males had a lower ratio (n = 44, 2.18 ± 0.28) compared to TT/T females/males (n = 60, 2.79 ± 0.27; p = 0.047). The MAOA rs979605 polymorphism, associated with the HDRS score in a sex-dependent manner, could be a useful biomarker for the response to ATD treatment.
Keywords: pharmacogenetics, major depressive disorder, serotonin, MAO, antidepressant drugs
1. Introduction
Major depressive disorder (MDD) is the current leading cause of disability worldwide [1]. Differences between sexes exist, too, as adult females are twice as likely to develop MDD and have a greater risk of experiencing longer and more severe depressive episodes compared to men [2]. Antidepressant drugs (ATD), which modulate monoamine neurotransmitter levels, remain a common treatment option for MDD. However, only about one-third of ATD-treated individuals achieve remission [3]. Identifying biomarkers to predict treatment response is thus an important clinical challenge.
Monoamine oxidase (MAO) metabolizes monoamine neurotransmitters, including serotonin (5HT) [4]. Two MAO proteins have been characterized, namely MAOA and MAOB, encoded by the neighboring X chromosome (Xp11.23) genes, MAOA and MAOB, respectively [4]. MAOA preferentially metabolizes 5HT and noradrenaline, while MAOB preferentially metabolizes phenylethylene and benzylamine [4,5]. MAO expression changes with age [4] and differs between males and females [5]. Smoking also decreases MAO activity [5] although former smokers exhibit increased platelet MAO activity [6]. MAOB is more abundant in the brain, and MAOB expression occurs mainly in serotonergic and histaminergic neurons and astrocytes, while MAOA is expressed in dopaminergic and noradrenergic neurons [4,7]. In the periphery, MAOA is predominantly expressed in fibroblasts, while MAOB is the sole MAO in platelets [4].
MAOA and MAOB density in various brain regions was increased in the context of a medication-free major depressive episode (MDE) compared to healthy controls [8,9]. MAOA density remained elevated in MDD individuals following treatment with a selective serotonin reuptake inhibitor (SSRI), although it was lower in individuals achieving remission compared to recurrent MDE sufferers [10]. Increased levels of plasma 5-hydroxyindoleacetic acid (5HIAA)—the main metabolite of 5HT—were also observed in unmedicated depressed individuals compared to healthy controls, suggesting greater 5HT metabolism in the context of MDD [11]. Since direct evaluation of MAO activity in the human brain is difficult, peripheral 5HT and 5HIAA levels may serve as a viable proxy [12]. Given their role in monoamine metabolism, MAOA and MAOB are interesting targets in neurological disorders [4,13]. As such, factors influencing their expression or function are of similar interest.
Genetic variants within the MAO-encoding genes have been studied in various psychiatric contexts, including depression, bipolar disorder, and schizophrenia [4,14]. Studies examining ATD response in MDD have focused notably on the upstream variable number tandem repeat (uVNTR) within the MAOA promoter. While some report no association with response [15,16,17,18], others report that the short-form uVNTR is associated with improved clinical outcomes [19,20,21]. Regarding MAOA polymorphisms, the rs6323 (NM_000240.4:c.891G>T) synonymous polymorphism has been the most analyzed. In several studies, the rs6323(T) allele was associated with improved treatment response [16,22,23] although in Han Chinese females with depression, it was closely associated with poorer response to venlafaxine [24]. The MAOA rs979605 (NM_000240.4:c.1262+69A>T/G) intronic polymorphism and rs6323 were also associated with reduced MAO enzymatic activity [5,25]. Regarding MAOB, it was observed that female TT homozygotes for the rs1799836 (NM_000898.5:c1348-36A>G) intronic polymorphism responded better to treatment [26]. Lower MAO activity was also observed in Swedish rs1799836(T) allele carriers [27].
Different factors complicate the analysis of X-chromosomal variants. For one, females carry two gene copies (and thus two alleles), while males carry one. However, X-chromosome inactivation (XCI) silences 1 of the gene copies in females. Still, factors such as XCI skewness (i.e., imbalanced allelic expression) and escape from XCI (i.e., expression from both silenced and active chromosomes) [28]—for which conflicting findings for MAOA/MAOB have been reported [29,30,31]—may influence MAOA/MAOB expression. Due to this complexity, X- and Y-linked variants are sometimes omitted from genome-wide association studies of ATD response [32,33]. Those that include them [34,35], however, may not adjust for these factors. As such, associations between X-chromosomal variants and clinical improvement after ATD treatment would benefit from controlling for these factors.
The associations of MAOA/MAOB genetic variants with clinical improvement after ATD treatment and MAO activity, which modulates monoamine concentrations—common targets of ATD therapy—qualify them as potential biomarkers for clinical improvement following ATD treatment in MDD. Given their X-chromosomal location, improved analysis of these genetic factors may help to explain sex differences in the context of MDD and its treatment. We attempted such an analysis by examining the association of MAOA/MAOB genetic variants with (1) clinical improvement following ATD treatment and (2) the plasma 5HIAA/5HT ratio as an estimate of MAO activity in a cohort of 6-month ATD-treated individuals with a current MDE in the context of MDD.
2. Results
2.1. Patient Demographics
Sociodemographic characteristics for the whole clinical and metabolomic cohorts and with respect to sex are shown in Table 1. For males (n = 119) and females (n = 259) of the clinical cohort, respectively, the mean age was 45.9 and 45 years, and 96% and 88% of subjects were Caucasian. Missing at follow-up rates relative to baseline were 4% and 6% after 1 month of ATD treatment (M1), 28% and 33% after 3 months (M3), and 46% and 47% after 6 months (M6).
Table 1.
Sociodemographic characteristics according to males and females.
| Total | Male | Female | ||
|---|---|---|---|---|
| Clinical cohort | ||||
| n = 378 | n = 119 | n = 259 | ||
| Age (in years) (m ± SD) | 45.3 ± 13.3 | 45.9 ± 12.8 | 45 ± 13.6 | |
| Education (n(%)) | Primary | 35(9) | 11(9) | 24(9) |
| High school | 166(44) | 45(38) | 121(47) | |
| University | 176(47) | 62(52) | 114(44) | |
| Ethnicity (n(%)) | Caucasian | 343(91) | 114(96) | 229(88) |
| African | 24(6) | 1(1) | 23(9) | |
| Mixed | 10(3) | 4(3) | 6(2) | |
| Smoking status (n(%)) | Current | 144(38) | 48(40) | 96(37) |
| Former | 48(13) | 22(18) | 26(10) | |
| Non | 186(49) | 49(41) | 137(53) | |
| Pack years (m ± SD) | 14 ± 13.5 | 14.4 ± 12 | 13.8 ± 14.3 | |
| Recurrent MDE (n(%)) | 278(74) | 79(66) | 199(77) | |
| Onset age MDE (in years) (m ± SD) | 35.2 ± 14.4 | 36.6 ± 15.1 | 34.5 ± 14 | |
| Baseline HDRS (m ± SD) | 24.7 ± 4.9 | 24.8 ± 5 | 24.7 ± 4.8 | |
| Therapy (n(%)) | SSRI | 156(41) | 49(41) | 107(41) |
| SNRI | 152(40) | 49(41) | 103(40) | |
| TCA | 24(7) | 6(5) | 18(7) | |
| Other | 34(9) | 9(8) | 25(10) | |
| ECT | 12(3) | 6(5) | 6(2) | |
| Missing at follow-up (n(%)) | M1 | 20(5) | 5(4) | 15(6) |
| M3 | 119(31) | 33(28) | 86(33) | |
| M6 | 176(47) | 55(46) | 121(47) | |
| Metabolomic cohort | ||||
| n = 148 | n = 52 | n = 96 | ||
| Age (in years) (m ± SD) | 46.2 ± 12.2 | 45.6 ± 11.8 | 46.5 ± 12.4 | |
| Education (n(%)) | Primary | 15(10) | 5(10) | 10(10) |
| High school | 58(39) | 15(29) | 43(45) | |
| University | 74(50) | 31(60) | 43(45) | |
| Ethnicity (n(%)) | Caucasian | 139(94) | 49(94) | 90(94) |
| African | 7(5) | 1(2) | 6(6) | |
| Mixed | 2(1) | 2(4) | 0(0) | |
| Smoking status (n(%)) | Current | 53(36) | 22(42) | 31(32) |
| Former | 15(10) | 9(17) | 6(6) | |
| Non | 80(54) | 21(40) | 59(61) | |
| Pack years (m ± SD) | 13.6(11.3) | 14.6(11.9) | 12.8(10.9) | |
| Recurrent MDE (n(%)) | 100(68) | 30(58) | 70(73) | |
| Onset age MDE (in years) (m ± SD) | 36.7 ± 14.4 | 37.5 ± 15.7 | 36.2 ± 13.7 | |
| Baseline HDRS (m ± SD) | 23.4 ± 4.1 | 23.6 ± 4.5 | 23.3 ± 3.9 | |
| ATD-naïve (n(%)) | 59(40) | 22(42) | 37(39) | |
| Therapy (n(%)) | SSRI | 61(41) | 20(38) | 41(43) |
| SNRI | 61(41) | 25(48) | 36(38) | |
| TCA | 12(8) | 3(6) | 9(9) | |
| Other | 12(8) | 4(8) | 8(8) | |
| ECT | 2(1) | 0(0) | 2(2) | |
Sociodemographic characteristics of the whole sample and in males and females of the clinical and metabolomic cohorts. ATD, antidepressant drug; ECT, electroconvulsive therapy; HDRS, 17-item Hamilton Depression Rating Scale; m, mean; M1, after 1 month of treatment; M3, after 3 months of treatment; M6, after 6 months of treatment; MDE, major depressive episode; n, number of individuals; SD, standard deviation; SNRI, serotonin norepinephrine reuptake inhibitor; SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressant.
2.2. Genetic Variant Selection
A total of 29 MAOA (26 single-nucleotide polymorphisms (SNP) and 3 insertion/deletions) and 25 MAOB (25 SNPs) genetic variants were identified. Among these, five MAOA SNPs and one MAOB SNP had a call rate ≥ 95% and a minor allele frequency (MAF) ≥ 5% (see Table 2). None significantly deviated from Hardy–Weinberg equilibrium (HWE). The five MAOA SNPs were in linkage disequilibrium (LD) (see Figure S1). The MAOA rs979605(A > G) genetic polymorphism was selected as a MAOA haplotype proxy for further analysis. The rs979605(G) allele was correlated with the rs6323(T) allele. Allelic frequencies did not significantly differ between males and females.
Table 2.
Genomic and haplotypic information of the 6 selected MAOA and MAOB variants.
| Rs# | Region | Variant Effect |
RefSeq | Major Allele | Minor Allele | HWEF | MAFTotal (%) | MAFF (%) | MAFM (%) | p |
|---|---|---|---|---|---|---|---|---|---|---|
| MAOA | ||||||||||
| rs6323 | Exon 8 | p.Arg297Arg | NM_000240 | T | G | 0.56 | 32.7 | 32.9 | 36.8 | 0.32 |
| rs2235186 | Intronic | G | A | 0.56 | 32.9 | 32.9 | 38.2 | 0.32 | ||
| rs979606 | Intronic | T | C | 0.51 | 32.8 | 32.8 | 37.8 | 0.32 | ||
| rs979605 | Intronic | G | A | 0.78 | 34.8 | 33.6 | 38.2 | 0.62 | ||
| rs1137070 | Exon 14 | p.Asp470Asp | NM_000240 | C | T | 0.63 | 34.0 | 33.8 | 36.8 | 0.59 |
| Haplotype frequency | ||||||||||
| 65.6% | 33.7% | |||||||||
| MAOB | ||||||||||
| rs1799836 | Intronic | T | C | 0.99 | 45.1 | 45.8 | 38.7 | 0.08 | ||
For each variant, we show the rs identifier (rs#), its genomic region, its protein-level effect and the corresponding RefSeq accession, the major and minor alleles, HWE (in females), the total and female- and male-specific MAFs, and the p-value of the χ2 test comparing male and female frequencies. For MAOA variants, we also show the frequency of the major and minor allele haplotypes. F, female; HWE, Hardy–Weinberg equilibrium; M, male; MAF, minor allele frequency; p, p-value.
Sociodemographic characteristics with respect to sex and MAOA rs979605 and MAOB rs1799836 genotypes are shown in Table 3 and Table 4, respectively. Significant differences in the missing at follow-up rate (M1) and in age and the prescribed therapy were observed between female MAOA rs979605 genotypes of the clinical and metabolomic cohorts, respectively (see Table 3). Likewise, significant differences in ethnicity and in smoking status were observed between female MAOB rs1799836 genotypes of the clinical and metabolomic cohorts, respectively (see Table 4).
Table 3.
Sociodemographic characteristics according to MAOA rs979605 genotypes in males and females.
| MAOA rs979605 | ||||||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | |||||||
| G | A | p | GG | GA | AA | p | ||
| Clinical Cohort | ||||||||
| n = 76 | n = 43 | n = 119 | n = 108 | n = 32 | ||||
| Age (in years) (m ± SD) | 46.8 ± 12.8 | 44.4 ± 12.9 | 0.28 | 43.3 ± 14.1 | 45.6 ± 13.5 | 49.3 ± 11 | 0.055 | |
| Education (n(%)) | Primary | 7(9) | 4(9) | 0.90 | 10(8) | 10(9) | 4(12) | 0.24 |
| High school | 27(36) | 18(42) | 48(40) | 58(54) | 15(47) | |||
| University | 41(54) | 21(49) | 61(51) | 40(37) | 13(41) | |||
| Ethnicity (n(%)) | Caucasian | 72(95) | 42(98) | 1.00 | 103(87) | 99(92) | 27(84) | 0.46 |
| African | 1(1) | 0(0) | 12(10) | 8(7) | 3(9) | |||
| Mixed | 3(4) | 1(2) | 3(3) | 1(1) | 2(6) | |||
| Smoking status (n(%)) | Current | 29(38) | 19(44) | 0.77 | 48(40) | 37(34) | 11(34) | 0.52 |
| Former | 14(18) | 8(19) | 14(12) | 8(7) | 4(12) | |||
| Non | 33(43) | 16(37) | 57(48) | 63(58) | 17(53) | |||
| Pack years (m ± SD) | 14.1 ± 12 | 14.9 ± 12.3 | 0.92 | 13.6 ± 16.9 | 13.3 ± 12 | 16.6 ± 9.7 | 0.29 | |
| Recurrent MDE (n(%)) | 54(71) | 25(58) | 0.16 | 88(74) | 87(81) | 24(75) | 0.46 | |
| Onset age MDE (in years) (m ± SD) | 36.9 ± 14.2 | 36.1 ± 16.9 | 0.81 | 34.4 ± 14.8 | 33.9 ± 13 | 36.4 ± 14.4 | 0.70 | |
| Baseline HDRS (m ± SD) | 25.3 ± 5.1 | 23.9 ± 4.8 | 0.13 | 24.5 ± 4.8 | 24.9 ± 5.1 | 24.9 ± 4.3 | 0.77 | |
| Therapy (n(%)) | SSRI | 30(39) | 19(44) | 0.81 | 49(41) | 47(44) | 11(34) | 0.87 |
| SNRI | 30(39) | 19(44) | 46(39) | 43(40) | 14(44) | |||
| TCA | 4(5) | 2(5) | 8(7) | 8(7) | 2(6) | |||
| Other | 7(9) | 2(5) | 13(11) | 7(6) | 5(16) | |||
| ECT | 5(7) | 1(2) | 3(3) | 3(3) | 0(0) | |||
| Missing at follow-up (n(%)) | M1 | 4(5) | 1(2) | 0.65 | 2(2) | 10(9) | 3(9) | 0.017 * |
| M3 | 23(30) | 10(23) | 0.52 | 43(36) | 30(28) | 13(41) | 0.26 | |
| M6 | 36(47) | 19(44) | 0.85 | 59(50) | 44(41) | 18(56) | 0.21 | |
| Metabolomic Cohort | ||||||||
| n = 19 | n = 33 | n = 42 | n = 42 | n = 12 | ||||
| Age (in years) (m ± SD) | 45.3 ± 11 | 45.8 ± 12.5 | 0.91 | 44 ± 12.6 | 46.7 ± 12.4 | 54.2 ± 8.9 | 0.023 * | |
| Education (n(%)) | Primary | 3(16) | 2(6) | 0.26 | 3(7) | 6(14) | 1(8) | 0.69 |
| High school | 3(16) | 12(36) | 17(40) | 20(48) | 6(50) | |||
| University | 13(68) | 18(55) | 22(52) | 16(38) | 5(42) | |||
| Ethnicity (n(%)) | Caucasian | 19(100) | 30(91) | 0.70 | 39(93) | 39(93) | 12(100) | 1.00 |
| African | 0(0) | 1(3) | 3(7) | 3(7) | 0(0) | |||
| Mixed | 0(0) | 2(6) | 0(0) | 0(0) | 0(0) | |||
| Smoking status (n(%)) | Current | 9(47) | 13(39) | 0.93 | 14(33) | 13(31) | 4(33) | 0.97 |
| Former | 3(16) | 6(18) | 3(7) | 2(5) | 1(8) | |||
| Non | 7(37) | 14(42) | 25(60) | 27(64) | 7(58) | |||
| Pack years (m ± SD) | 15.8 ± 13.3 | 13.9 ± 11.4 | 0.70 | 7.5 ± 8.2 | 15.7 ± 11.5 | 19.8 ± 10.3 | 0.51 | |
| Recurrent MDE (n(%)) | 9(47) | 21(64) | 0.38 | 30(71) | 31(74) | 9(75) | 1.00 | |
| Onset age MDE (in years) (m ± SD) | 38.7 ± 16.8 | 36.8 ± 15.3 | 0.60 | 36.6 ± 14 | 35.1 ± 12.9 | 38.9 ± 16.2 | 0.80 | |
| Baseline HDRS (m ± SD) | 22.5 ± 3.5 | 24.2 ± 4.9 | 0.30 | 23.6 ± 4.2 | 23.1 ± 3.8 | 23.4 ± 3.5 | 0.86 | |
| ATD-naïve (n(%)) | 6(32) | 16(48) | 0.46 | 14(33) | 20(48) | 3(25) | 0.28 | |
| Therapy (n(%)) | SSRI | 6(32) | 14(42) | 0.79 | 14(33) | 25(60) | 2(17) | 0.038 * |
| SNRI | 11(58) | 14(42) | 18(43) | 13(31) | 5(42) | |||
| TCA | 1(5) | 2(6) | 5(12) | 2(5) | 2(17) | |||
| Other | 1(5) | 3(9) | 3(7) | 2(5) | 3(25) | |||
| ECT | 0(0) | 0(0) | 2(5) | 0(0) | 0(0) | |||
Sociodemographic characteristics of males and females of the clinical and metabolomic cohorts according to MAOA rs979605 genotypes. Males are hemizygous for either allele G or A. Females are either GG homozygotes, GA heterozygotes, or AA homozygotes. Wilcoxon rank-sum tests were used to compare age, pack years, onset age of MDE, and baseline HDRS (presented as mean ± standard deviation) between males, while Kruskal–Wallis tests were used to compare these variables between females. Fisher’s exact tests were used to compare education status, ethnicity, smoking status at baseline, MDE recurrence, prescribed therapy, missing at follow-up rates over time, and ATD-naïve status (presented as the group number and percentage). * p < 0.05. ATD, antidepressant drug; ECT, electroconvulsive therapy; HDRS, 17-item Hamilton Depression Rating Scale; m, mean; M1, after 1 month of treatment; M3, after 3 months of treatment; M6, after 6 months of treatment; MDE, major depressive episode; n, number of individuals; p, p-value; SD, standard deviation; SNRI, serotonin norepinephrine reuptake inhibitor; SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressant.
Table 4.
Sociodemographic characteristics according to MAOB rs1799836 genotypes in males and females.
| MAOB rs1799836 | ||||||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | |||||||
| T | C | p | TT | TC | CC | p | ||
| Clinical Cohort | ||||||||
| n = 71 | n = 45 | n = 70 | n = 126 | n = 61 | ||||
| Age (in years) (m ± SD) | 45.6 ± 12.7 | 46.8 ± 13.4 | 0.69 | 44.2 ± 13.7 | 45.4 ± 13.4 | 45.6 ± 14 | 0.85 | |
| Education (n(%)) | Primary | 7(10) | 4(9) | 1 | 5(7) | 13(10) | 6(10) | 0.5 |
| High school | 27(38) | 17(38) | 38(54) | 52(41) | 30(49) | |||
| University | 36(51) | 24(53) | 27(39) | 61(48) | 25(41) | |||
| Ethnicity (n(%)) | Caucasian | 68(96) | 43(96) | 0.57 | 66(94) | 114(90) | 47(77) | <0.001 * |
| African | 0(0) | 1(2) | 2(3) | 7(6) | 14(23) | |||
| Mixed | 3(4) | 1(2) | 1(1) | 5(4) | 0(0) | |||
| Smoking status (n(%)) | Current | 26(37) | 21(47) | 0.6 | 26(37) | 43(34) | 25(41) | 0.19 |
| Former | 14(20) | 8(18) | 10(14) | 8(6) | 8(13) | |||
| Non | 31(44) | 16(36) | 34(49) | 75(60) | 28(46) | |||
| Pack years (m ± SD) | 16 ± 14.1 | 12.5 ± 9.3 | 0.73 | 12.5 ± 12.3 | 17 ± 17.3 | 10.2 ± 9.4 | 0.10 | |
| Recurrent MDE (n(%)) | 48(68) | 30(67) | 1 | 53(76) | 94(75) | 50(82) | 0.54 | |
| Onset age MDE (in years) (m ± SD) | 36.6 ± 15.1 | 36.4 ± 15.7 | 0.91 | 35.9 ± 13.3 | 34.2 ± 14.4 | 34 ± 14.1 | 0.60 | |
| Baseline HDRS (m ± SD) | 24.2 ± 4.6 | 25.5 ± 5.6 | 0.23 | 24.3 ± 4.9 | 25.1 ± 4.7 | 24.4 ± 5.1 | 0.31 | |
| Therapy (n(%)) | SSRI | 31(44) | 17(38) | 0.24 | 27(39) | 54(43) | 25(41) | 0.37 |
| SNRI | 26(37) | 22(49) | 30(43) | 52(41) | 20(33) | |||
| TCA | 6(8) | 0(0) | 5(7) | 10(8) | 3(5) | |||
| Other | 5(7) | 3(7) | 7(10) | 7(6) | 11(18) | |||
| ECT | 3(4) | 3(7) | 1(1) | 3(2) | 2(3) | |||
| Missing at follow-up (n(%)) | M1 | 2(3) | 2(4) | 0.64 | 3(4) | 9(7) | 3(5) | 0.78 |
| M3 | 16(23) | 16(36) | 0.14 | 28(40) | 36(29) | 21(34) | 0.25 | |
| M6 | 23(51) | 23(51) | 0.44 | 35(50) | 56(44) | 29(48) | 0.75 | |
| Metabolomic Cohort | ||||||||
| n = 33 | n = 19 | n = 27 | n = 44 | n = 24 | ||||
| Age (in years) (m ± SD) | 43.5 ± 12 | 49.2 ± 11 | 0.91 | 44.3 ± 13 | 48.3 ± 12.6 | 46.5 ± 10.7 | 0.50 | |
| Education (n(%)) | Primary | 3(9) | 2(11) | 0.26 | 3(11) | 5(11) | 2(8) | 0.050 |
| High school | 10(30) | 5(26) | 11(41) | 15(34) | 17(71) | |||
| University | 19(58) | 12(63) | 13(48) | 24(55) | 5(21) | |||
| Ethnicity (n(%)) | Caucasian | 31(94) | 18(95) | 0.70 | 27(100) | 41(93) | 21(88) | 0.16 |
| African | 0(0) | 1(5) | 0(0) | 3(7) | 3(12) | |||
| Mixed | 2(6) | 0(0) | 0(0) | 0(0) | 0(0) | |||
| Smoking status (n(%)) | Current | 14(42) | 8(42) | 0.93 | 8(30) | 11(25) | 11(46) | 0.018 * |
| Former | 5(15) | 4(21) | 3(11) | 0(0) | 3(12) | |||
| Non | 14(42) | 7(37) | 16(59) | 33(75) | 10(42) | |||
| Pack years (m ± SD) | 14.5 ± 13.4 | 14.8 ± 10.1 | 0.70 | 10.5 ± 10.6 | 17.7 ± 12.2 | 11.8 ± 9.8 | 0.054 | |
| Recurrent MDE (n(%)) | 20(61) | 10(53) | 0.38 | 19(70) | 30(68) | 20(83) | 0.39 | |
| Onset age MDE (in years) (m ± SD) | 36 ± 15.7 | 40.2 ± 15.8 | 0.60 | 36.9 ± 12.7 | 37 ± 14.1 | 34.8 ± 14.5 | 0.77 | |
| Baseline HDRS (m ± SD) | 23.5 ± 4.3 | 23.8 ± 4.9 | 0.30 | 22 ± 3.2 | 23.7 ± 3.8 | 23.9 ± 4.5 | 0.15 | |
| ATD-naïve (n(%)) | 12(36) | 10(53) | 0.46 | 11(41) | 18(41) | 8(33) | 0.70 | |
| Therapy (n(%)) | SSRI | 13(39) | 7(37) | 0.79 | 9(33) | 20(45) | 12(50) | 0.14 |
| SNRI | 14(42) | 11(58) | 13(48) | 15(34) | 7(29) | |||
| TCA | 3(9) | 0(0) | 2(7) | 7(16) | 0(0) | |||
| Other | 3(9) | 1(5) | 2(7) | 2(5) | 4(17) | |||
| ECT | 0(0) | 0(0) | 1(4) | 0(0) | 1(4) | |||
Sociodemographic characteristics of males and females of the clinical and metabolomic cohorts according to MAOB rs1799836 genotypes. Males are hemizygous for either allele T or C. Females are either TT homozygotes, TC heterozygotes, or CC homozygotes. Wilcoxon rank-sum tests were used to compare age, pack years, onset age of MDE, and baseline HDRS (presented as mean ± standard deviation) between males, while Kruskal–Wallis tests were used to compare these variables between females. Fisher’s exact tests were used to compare education status, ethnicity, smoking status at baseline, MDE recurrence, prescribed therapy, missing at follow-up rates over time, and ATD-naïve status (presented as the group number and percentage). * p < 0.05. ATD, antidepressant drug; ECT, electroconvulsive therapy; HDRS, 17-item Hamilton Depression Rating Scale; m, mean; M1, after 1 month of treatment; M3, after 3 months of treatment; M6, after 6 months of treatment; MDE, major depressive episode; n, number of individuals; p, p-value; SD, standard deviation; SNRI, serotonin norepinephrine reuptake inhibitor; SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressant.
2.3. Clinical Improvement According to Variant Genotypes
We first examined associations of the MAOA rs979605 and MAOB rs1799836 genetic polymorphisms with clinical measures using the proposed full model for analyzing X-chromosomal variants, including the dominance term and polymorphism × sex interaction. In the model of the 17-item Hamilton Depression Rating Scale (HDRS) score, the MAOA rs979605 genetic polymorphism × sex interaction was significant after controlling for other factors (F1,367 = 6.32, p = 0.012), corresponding to a difference in the association of rs979605 with the HDRS score depending on sex (see Table 5). The MAOB rs1799836 genetic polymorphism was not a significant factor in models of clinical outcomes at a Bonferroni-corrected level of p < 0.025, and neither were its interactions with time or sex (see Table 5).
Table 5.
Clinical associations with MAOA rs979605 and MAOB rs1799836 genotypes using the proposed full model for X-chromosomal variants.
| HDRS | Response | Remission | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SS | MS | df (num) | df (den) | F | p | χ2 | df | p | χ2 | df | p | |
| MAOA rs979605 | ||||||||||||
| Age | 0.44 | 0.44 | 1 | 369.04 | 0.015 | 0.90 | 2.68 | 1 | 0.10 | 0.78 | 1 | 0.38 |
| Sex | 149.07 | 149.07 | 1 | 385.70 | 4.97 | 0.026 | 1.44 | 1 | 0.23 | 2.84 | 1 | 0.092 |
| ATD class | 122.64 | 30.66 | 4 | 374.77 | 1.02 | 0.40 | 2.92 | 4 | 0.57 | 6.22 | 4 | 0.18 |
| Loss to follow-up (M1) | 86.28 | 86.28 | 1 | 442.40 | 2.88 | 0.091 | 1.56 | 1 | 0.21 | 0.32 | 1 | 0.57 |
| Smoking status | 19.39 | 9.70 | 2 | 369.28 | 0.32 | 0.72 | 3.70 | 2 | 0.16 | 0.40 | 2 | 0.82 |
| Time | 28,305.80 | 9435.27 | 3 | 857.69 | 314.42 | <0.001 * | 35.66 | 2 | <0.001 * | 36.81 | 2 | <0.001 * |
| rs979605 dominance term | 7.16 | 7.16 | 1 | 894.03 | 0.24 | 0.63 | 0.011 | 1 | 0.91 | 1.02 | 1 | 0.31 |
| rs979605 | 0.14 | 0.14 | 1 | 392.04 | 0.0048 | 0.94 | 0.12 | 1 | 0.73 | 0.025 | 1 | 0.88 |
| Time:rs979605 | 181.21 | 30.20 | 6 | 867.34 | 1.01 | 0.42 | 1.77 | 4 | 0.78 | 8.04 | 4 | 0.090 |
| Sex:rs979605 | 189.65 | 189.65 | 1 | 367.50 | 6.32 | 0.012 * | 2.81 | 1 | 0.094 | 3.27 | 1 | 0.071 |
| Sex:Time | 251.64 | 83.88 | 3 | 868.36 | 2.80 | 0.039 | 3.00 | 2 | 0.22 | 0.22 | 2 | 0.90 |
| MAOB rs1799836 | ||||||||||||
| Age | 5.93 | 5.93 | 1 | 359.18 | 0.20 | 0.66 | 2.77 | 1 | 0.10 | 0.97 | 1 | 0.32 |
| Sex | 4.12 | 4.12 | 1 | 352.08 | 0.14 | 0.71 | 0.99 | 1 | 0.32 | 2.11 | 1 | 0.15 |
| ATD class | 156.33 | 39.08 | 4 | 368.79 | 1.29 | 0.27 | 3.69 | 4 | 0.45 | 6.46 | 4 | 0.17 |
| Ethnicity | 81.42 | 40.71 | 2 | 366.62 | 1.35 | 0.26 | 4.35 | 2 | 0.11 | 0.29 | 2 | 0.86 |
| Smoking status | 16.58 | 8.29 | 2 | 364.20 | 0.27 | 0.76 | 3.10 | 2 | 0.21 | 0.10 | 2 | 0.95 |
| Time | 35,802.44 | 11,934.15 | 3 | 853.23 | 395.00 | <0.001 * | 32.94 | 2 | <0.001 * | 39.08 | 2 | <0.001 * |
| rs1799836 dominance term | 31.48 | 31.48 | 1 | 845.36 | 1.04 | 0.31 | 0.95 | 1 | 0.33 | 1.47 | 1 | 0.22 |
| rs1799836 | 119.36 | 119.36 | 1 | 356.46 | 3.95 | 0.048 | 1.52 | 1 | 0.22 | 2.17 | 1 | 0.14 |
| Time:rs1799836 | 121.70 | 20.28 | 6 | 856.73 | 0.67 | 0.67 | 4.45 | 4 | 0.35 | 1.85 | 4 | 0.76 |
| Sex:rs1799836 | 3.34 | 3.34 | 1 | 354.56 | 0.11 | 0.74 | 0.74 | 1 | 0.39 | 0.26 | 1 | 0.61 |
| Sex:Time | 138.63 | 46.21 | 3 | 855.42 | 1.53 | 0.21 | 4.23 | 2 | 0.12 | 1.11 | 2 | 0.57 |
Results of mixed-effects models of the HDRS score, response, and remission using the proposed full model. HDRS was assessed using the Satterthwaite method while response and remission were assessed using the Wald chi-square method. * p < 0.025. ATD, antidepressant drug; den, denominator; df, degrees of freedom; F, F statistic; HDRS, 17-item Hamilton Depression Rating Scale; MS, mean squares; num, numerator; p, p-value; SS, sum of squares; χ2, chi-square.
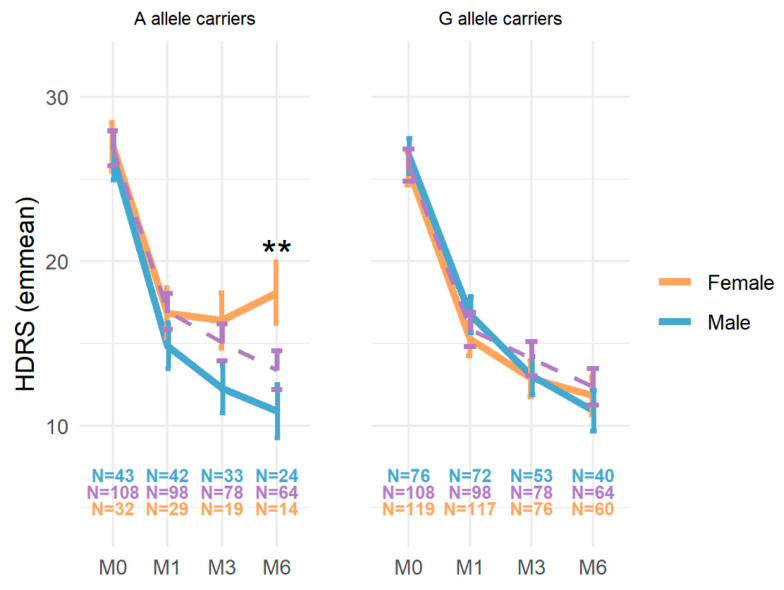
We further investigated the association between rs979605 and the HDRS score in A and G allele subgroups under different XCI status assumptions. When modeling the HDRS score in A allele carriers (n = 183) assuming random XCI (i.e., males coded the same as homozygous females), sex was a significant factor at a Bonferroni-corrected level of p < 0.0125 to account for the four models examined after controlling for other factors (F1,187 = 7.66, p = 0.0062), corresponding to a difference in the association of the MAOA rs979605 A allele with the HDRS score depending on sex (see Table S1). At M6, a significantly higher HDRS score was observed in female rs979605 AA homozygotes (n = 14, 18.1 ± 1.87) compared to male A carriers (n = 24, 10.9 ± 1.61) following Bonferroni correction (coef. = 7.21, 95%CI [3.03–11.38], p = 0.0067) (see Figure 1). No other allele-specific associations with the HDRS score were observed.
Figure 1.
HDRS scores according to sex and MAOA rs979605 genotypes. Model estimates of the HDRS score (y-axis) at different study time points (x-axis) for MAOA rs979605 A allele female homozygotes (orange), female heterozygotes (purple dashed), and male carriers (blue). G allele carriers (right) are shown for comparison only. ** p < 0.01 following Bonferroni correction for the nine comparisons in A allele carriers. HDRS, 17-item Hamilton Depression Rating Scale.
We also examined the association of the MAOA rs979605 genetic polymorphism in male and female subgroups. However, neither it nor its interaction with time was a significant factor in either male or female populations after controlling for other factors.
2.4. MAO Activity Estimation According to Variant Genotypes
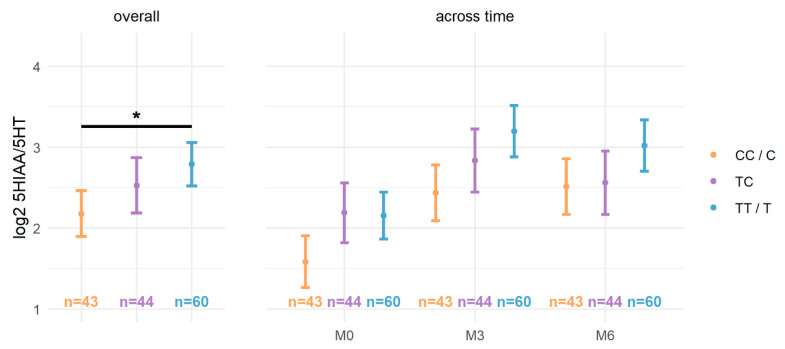
We also examined the associations of rs979605 and rs1799836 with the plasma 5HIAA/5HT ratio using the proposed full model. The plasma 5HIAA/5HT ratio was log2 transformed due to non-normality (see Figure S2). Baseline plasma 5HIAA/5HT ratios (mean = 8.84, SD = 11.15) were lower compared to ratios at M3 (mean = 15.02, SD = 12.75) and M6 (mean = 15.34, SD = 16.75). After controlling for other factors, including significant ones (i.e., age, ATD class, ATD-naïve status, and time), the plasma 5HIAA/5HT ratio was significantly associated with the MAOB rs1799836 genetic polymorphism (F1,133 = 5.92, p = 0.016) (see Table 6). In a model without the non-significant sex interactions, rs1799836 remained significant after controlling for the same factors (F1,135 = 6.00, p = 0.016) (see Table S2). Globally, TT/T females/males had a significantly higher 5HIAA/5HT ratio (2.79 ± 0.27) compared to CC/C females/males (2.18 ± 0.28) following Bonferroni correction for the three comparisons (coef. = 0.61, 95%CI [0.12–1.11], p = 0.047) (see Figure 2).
Table 6.
Plasma 5HIAA/5HT ratio associations with MAOA rs979605 and MAOB rs1799836 genotypes.
| SS | MS | df (num) | df (den) | F | p | |
|---|---|---|---|---|---|---|
| MAOA rs979605 | ||||||
| Age | 11.61 | 11.61 | 1 | 135.08 | 5.99 | 0.016 * |
| Sex | 0.33 | 0.33 | 1 | 136.39 | 0.17 | 0.68 |
| ATD class | 46.99 | 11.75 | 4 | 136.21 | 6.07 | <0.001 * |
| Smoking status | 2.66 | 1.33 | 2 | 136.27 | 0.69 | 0.50 |
| ATD-naïve status | 22.77 | 22.77 | 1 | 376.32 | 11.76 | <0.001 * |
| Time | 41.03 | 20.52 | 2 | 300.99 | 10.60 | <0.001 * |
| rs979605 dominance term | 0.02 | 0.02 | 1 | 330.21 | 0.0083 | 0.93 |
| rs979605 | 2.55 | 2.55 | 1 | 135.88 | 1.32 | 0.25 |
| Time:rs979605 | 0.26 | 0.07 | 4 | 285.41 | 0.034 | 1.00 |
| Sex:rs979605 | 3.45 | 3.45 | 1 | 135.91 | 1.78 | 0.18 |
| Sex:Time | 3.81 | 1.91 | 2 | 285.33 | 0.98 | 0.38 |
| MAOB rs1799836 | ||||||
| Age | 15.53 | 15.53 | 1 | 133.66 | 8.02 | <0.001 * |
| Sex | 0.71 | 0.71 | 1 | 134.63 | 0.37 | 0.55 |
| ATD class | 42.30 | 10.58 | 4 | 134.71 | 5.47 | <0.001 * |
| Smoking status | 2.47 | 1.23 | 2 | 134.54 | 0.64 | 0.53 |
| ATD-naïve status | 23.74 | 23.74 | 1 | 372.91 | 12.27 | <0.001 * |
| Time | 40.46 | 20.23 | 2 | 298.70 | 10.45 | <0.001 * |
| rs1799836 dominance term | 0.00 | 0.00 | 1 | 313.20 | 0.0023 | 0.96 |
| rs1799836 | 11.46 | 11.46 | 1 | 133.94 | 5.92 | 0.016 * |
| Time:rs1799836 | 2.91 | 0.73 | 4 | 282.18 | 0.38 | 0.83 |
| Sex:rs1799836 | 0.25 | 0.25 | 1 | 134.42 | 0.13 | 0.72 |
| Sex:Time | 2.42 | 1.21 | 2 | 282.57 | 0.63 | 0.54 |
Results for mixed-effects models of the 5HIAA/5HT ratio assessed using the Satterthwaite method. * p < 0.025. ATD, antidepressant drug; den, denominator; df, degrees of freedom; F, F statistic; MS, mean squares; num, numerator; p, p-value; SS, sum of squares.
Figure 2.
Log2 5HIAA/5HT ratios according to MAOB rs1799836 genotypes. The log2 5HIAA/5HT ratio (y-axis) according to rs1799836 genotypes (see legend) both overall (left) and across time (right). * p < 0.05 following Bonferroni correction for the three comparisons.
We also examined whether baseline or serial log2-transformed plasma 5HIAA/5HT ratios were associated with clinical outcomes. However, neither 5HIAA/5HT ratios nor their interactions with rs979605 and rs1799836 genotypes or time were significant factors in models of clinical outcomes after controlling for other factors.
2.5. Power Analysis
We had sufficient power to detect an R2 = 3% for the HDRS score (SD = 7.48) between genotypes for both rs979605 and rs1799836 among the 259 individuals at M3 and an R2 = 5.2% for baseline plasma 5HIAA/5HT ratio (SD = 1.97) variation between genotypes for both polymorphisms among the 148 individuals of the metabolomic cohort.
3. Discussion
In this ancillary investigation of METADAP, we analyzed the association between the rs979605 and rs1799836 genetic polymorphisms of MAOA and MAOB—encoding for the monoamine oxidases—respectively, and clinical improvement following ATD treatment in depressed patients. The allele frequency of rs1799836(C) in METADAP (45.1%) was comparable to that of non-Finnish Europeans of gnomAD (45.6%) [36], but rs979605(A) was more frequent in METADAP (34.8%), notably in males (38.2%) compared to males of this same gnomAD population (29.7%). The MAOB rs1799836 genetic polymorphism was not significantly associated, and neither were its interactions with time or sex, with clinical outcomes. The rs979605 × sex interaction was significantly associated with the HDRS score, and after 6 months of treatment, a significantly higher HDRS score was observed in female rs979605 AA homozygotes compared to male A carriers.
The MAOA rs6323 polymorphism—in LD with rs979605—was previously examined in association with response to ATD treatment in several contexts, including rapid versus delayed response and response in placebo- versus ATD-treated individuals [16,22]. Its analysis in two cohorts of depressed patients (baseline HDRS score ≥18) following several weeks of ATD treatment corresponds best with our own [23,24]. However, where Bi et al. observed that rs6323(T) was associated with poorer clinical outcomes in 6-week venlafaxine-treated Han Chinese females [24], Tadić et al. observed that, among females of their European population, TT homozygotes had significantly improved HDRS scores compared to G allele carriers after 4 weeks of mirtazapine treatment [23]. The former finding may be due to ethnic differences. Indeed, in our analysis of predominantly Caucasian (~90%) and 6-month SSRI- or SNRI-treated (81%) depressed patients (baseline HDRS score ≥18), we observed that females homozygous for rs979605(G)—in LD with rs6323(T)—had decreased HDRS scores compared to AA homozygotes although these differences were not significant.
Although we examined male and female populations separately like Tadić et al., associations with rs979605 only approached significance in these subpopulations. However, by analyzing males and females together, we observed a significant rs979605 × sex interaction. This finding suggests that genetic variants of MAOA may have an influence on the response to ATD therapy in depressed patients in a sex-dependent manner. Importantly, this observation could extend to other X-chromosomal genetic polymorphisms involved in ATD pharmacodynamics.
We also examined the plasma 5HIAA/5HT ratio as an estimate of MAO activity. Decreased platelet MAO activity was previously reported in female MAOA rs979605(G) carriers [5] and male MAOB rs1799836(T) carriers [27]. We observed a significant association of the plasma 5HIAA/5HT ratio with rs1799836 but not rs979605. Overall, TT/T females/males had a significantly higher ratio compared to CC/C females/males, which could be indicative of increased MAO activity, a result that contradicts previous findings [27]. However, compared to this study, we analyzed a population of depressed individuals. Importantly, MAO activity was shown to differ in depressed individuals compared to healthy controls [8,9]. MAO expression and activity is influenced by demographic—including age, sex, and smoking [5]—and biological factors, including epigenetics [37], which, at least for MAOB, is influenced by smoking [6]. We were able to control for the former but not the latter (at least not directly and not completely). Additionally, we estimated MAO activity from peripheral plasma 5HT and 5HIAA levels measured using ultraperformance liquid chromatography coupled with mass spectrometry (UPLC-MS), while the previous studies measured MAO activity using radiometric assays. Of note, most peripheral 5HT is stored in platelets that only contain MAOB, which only weakly metabolizes 5HT [7], while the rest is metabolized in peripheral organs [38]. Peripheral 5HT metabolism may differ from that of the brain. However, platelet MAO activity and MAOB density in the prefrontal cortex were both increased in depressed individuals [4,9], suggesting that MAO expression/activity in peripheral platelets may mirror that of the brain [4].
MAO expression is influenced by many factors. The sex hormones estrogen and progesterone can inhibit and promote 5HT degradation, respectively [39]. Glucocorticoids can also regulate brain MAOA activity [4,40]. MAOA and MAOB promoter regions contain binding elements for Sp1 [7], a transcription factor (TF) that regulates the expression of many genes. Altered Sp1 binding activity was observed in 3-week fluoxetine-treated rats [41], suggesting a role for Sp1 in the response to ATDs. At least for MAOA, members of the Sp family can bind to these Sp1-binding sites and either activate (Sp1, Sp4) or inhibit (Sp3) transcription [42]. Sp1 can also interact with transcription machinery and other TFs [42,43], including the glucocorticoid-regulated CDCA7L/R1 protein, and possibly the estrogen receptor [44]. The five MAOA genetic polymorphisms we identified were in LD. It is intriguing to speculate that some of these genetic polymorphisms are functional and may disrupt downstream processes linked to ATD therapy response, for example, through their interaction(s) with TFs. The potential and varied interactions between TFs and sex hormones in the context of MDD may contribute to the differential response to ATD treatment we observed between female rs979605(A) homozygotes and male A carriers.
Recent evidence suggests that pharmacogenomics-guided care improves treatment outcomes in depressed patients compared to treatment-as-usual, with 40% and 49% increases in response and remission, respectively [45]. It remains possible that an expanded genomic panel may further improve guided care. Polygenic risk scores also show promise as predictive tools although, to date, only nominal associations with antidepressant response in the context of MDD have been reported [46]. Given the differences between males and females in the context of depression [2], sex-specific factors may help improve the utility of each method. Although our results suggest a sex-dependent association of the MAOA rs979605 polymorphism with response following ATD treatment, this should be further replicated in an independent cohort of depressed individuals.
The present study has several limitations. First, the proportion of missing data was high. However, the proportion at M6 was comparable to that of the STAR*D cohort at 12 weeks [47]. Second, the genetic and metabolomic cohorts greatly differ in size. Studies with greater sample sizes and a balance of males and females would help corroborate our findings. Third, we only had access to peripheral metabolite levels, which may differ from those in the brain. This study benefits from its naturalistic and prospective design, which allows for the analysis of treatment response across a 6-month period in a “real-world” clinical setting. The modeling strategy by Chen et al. [48] also allowed us to more robustly analyze these X-chromosomal variants. To date, and to the best of our knowledge, this is the largest analysis of MAOA/MAOB variants in clinical response following ATD treatment in a predominantly Caucasian population of depressed patients.
4. Materials and Methods
4.1. Study Design
Do Antidepressants Induce Metabolic Syndromes (METADAP) is a 6-month prospective, multicentric, and observational cohort study carried out in a psychiatric setting [49]. Individuals with a current MDE were treated in naturalistic conditions and assessed before and during ATD treatment. This study was registered by the French National Agency for Medicine and Health Products Safety (ANSM) and the Commission Nationale de l’Informatique et des Libertés (CNIL). It was approved by the Ethics Committee of Paris-Boulogne (France) and conformed to international ethical standards (ClinicalTrials.gov identifier: NCT00526383).
4.2. Patient Population
Males and females 18–65 years of age without a serious medical or inflammatory condition were recruited. Inclusion criteria were presentation with a MDE in the context of MDD (DSM-IVTR)—assessed by the Mini International Neuropsychiatric Interview (MINI)—a score ≥ 18 on the HDRS [50], and need for a new ATD treatment. Individuals with psychotic disorder, bipolar disorder, alcohol or drug dependence, or an eating disorder were excluded, as previously described [49]. Measures and samples were obtained prior to beginning ATD treatment (M0) and at M1, M3, and M6.
Among the 643 individuals included in METADAP, 19 had major protocol deviations and were excluded. Of the 624 available for analysis, 519 individuals provided samples for genetic studies. From these, 400 underwent high-throughput sequencing. Nine samples were removed due to technical difficulties (n = 2), having a heterozygous call as a male (n = 1), or for having a missing genotype rate > 50% (n = 6). Ten samples without follow-up measures (i.e., M0 only) were removed given our objective to examine clinical response following ATD treatment. Three samples treated by MAO inhibitors were removed given our objective to examine the influence of MAOA/MAOB gene variants on clinical response, including their potential impact on MAO function. Thus, 378 individuals were analyzed (clinical cohort). Dropouts occurred mainly because of ATD changes, unauthorized drug use, or loss to follow-up. Ancestry was self-reported. Caucasian individuals were defined as having Caucasian parents; African individuals as having Sub-Saharan African and/or Afro-Caribbean parents; and Asian individuals as having East Asian, Central Asian, and/or South Asian parents [51]. In the original metabolite analysis of METADAP [38], 173 individuals were analyzed. Among them, 148 were present within the clinical cohort and analyzed (metabolomic cohort). All individuals provided written informed consent for study participation and genetic analyses [49].
4.3. Antidepressant Treatment
Monotherapies were prescribed by a psychiatrist in a “real world” psychiatric treatment setting as previously described [49] and belonged to one of five classes: SSRI; serotonin norepinephrine reuptake inhibitors (SNRI); tricyclic antidepressants (TCA); other ATDs; and electroconvulsive therapy (ECT). In this ancillary study of 378 individuals, 41% were prescribed an SSRI, 40% an SNRI, 7% a TCA, 9% another ATD treatment, and 3% received ECT. If a change in treatment was required during follow-up, the individual was dropped from the study.
4.4. Clinical Improvement after Antidepressant Treatment
The HDRS [50] was used to assess depression severity at M0 and clinical improvement after ATD treatment at M1, M3, and M6. Responders and remitters were defined by a decreased HDRS score ≥ 50% relative to baseline and a HDRS score ≤ 7 after ≥4 weeks of treatment, respectively. Clinical assessments were performed blind to genotyping results. Each interview and diagnostic assignment was reviewed by a senior psychiatrist. For each individual, all visits were reviewed by the same psychiatrist.
4.5. High-Throughput Sequencing, Sequence Alignment, and Variant Calling
For sequencing, 5 mL of whole blood was collected at baseline. Leukocytic DNA was extracted from 1 mL of blood using a Puregene Kit (Gentra systems, Minneapolis, MN, USA) and stored at −20 °C. DNA was sequenced using a targeted-exome panel of genes involved in mood disorders and ATD metabolism. The protocols for high-throughput sequencing [52] and information about the gene panel and variant calling [53] are described elsewhere.
4.6. Genetic Variant Selection
Variant call format data were loaded into R (v4.1.0) [54] using the vcfR package (v1.9.0) [55], as previously described [56]. Variant calls with a sequencing depth < 20, SNPs with a quality score (QUAL) < 275, insertion/deletions with a QUAL < 770, heterozygous calls with an allele balance (AB) < 0.34 or >0.79, and homozygous calls with an AB < 0.96 were annotated as poor-quality calls. Variants with a call rate (# poor-quality calls/# calls) < 95% were removed [57]. Variants with a MAF ≥ 5% were selected for further analysis.
4.7. Haplotype Analysis, Genotype Imputation, and Functional Annotation
HWE and LD were assessed using Haploview (v4.2) [58]. Variants were considered to be in LD by a r2 ≥ 0.8, as assessed in the subgroup of Caucasians comprising 91% of the study population. The variant with the highest MAF was selected as a haplotype proxy for further analysis.
4.8. 5HT and 5HIAA Measurement
Methods for metabolite level determination were previously described [38]. Metabolite extracts were prepared from 50 μL of fasting plasma stored at −80 °C via protein precipitation with 250 μL of acetonitrile, evaporation under nitrogen, and reconstitution in 50 μL of water. Three reference human plasma samples were prepared in each analytical batch as a control within and between analyses. UPLC-MS was performed using a Waters Acquity UPLC system coupled to a Thermo Scientific Q Exactive mass spectrometer. A proportion of values were below the lower limits of quantification (LLOQ) for 5HT (21.4%; LLOQ: 0.00113 μM) and 5HIAA (3.6%; 0.0131 μM) and were imputed as LLOQ/√2 (5HT:0.000799 μM; 5HIAA:0.00926 μM), as previously described [38].
4.9. Data Analysis
Statistical analyses were performed using R (v4.1.0) [54]. Quantitative variables were analyzed using nonparametric Wilcoxon rank sum or Kruskal–Wallis tests. Qualitative variables were analyzed using Fisher’s exact tests. Linear mixed-effects models and generalized linear mixed-effects models were constructed using the lme4 package (v1.1-27.1) [59]. The main variable to be explained was the HDRS total score. Other variables to explain were the response and remission rates and the plasma 5HIAA/5HT ratio. Chen et al. recently proposed a method (referred to as the proposed full model) that is robust to XCI, XCI skewness, and escape from XCI [48]. Briefly, unknown XCI status and XCI skewness were accounted for by analytical equivalencies to the variant × sex interaction and dominance term (i.e., female heterozygotes coded as 1 and all others as 0), respectively. Variant genotype and its interactions with time and sex were the main explanatory variables examined. Age, sex, the dominance term, time, and the sex × time interaction were included a priori as fixed-effects covariables in all full models. ATD class was also included a priori in all models to control for potential differences in treatment efficacy (in clinical models) or the plasma 5HIAA/5HT ratio (in metabolomic models) between treatment classes (e.g., SSRIs and ECT). As smoking and smoking history impact MAO activity [5,6], smoking status (i.e., non-smoker, current smoker, or former smoker) was also included a priori in all models. Since ATDs alter 5HT levels, ATD-naïve status was also included as a fixed-effect covariable in models of the plasma 5HIAA/5HT ratio. Sociodemographic and baseline clinical variables that significantly differed (i.e., p < 0.05) between genotypes were also included as fixed-effects covariables. Individual was included as a random-effect to account for repeated measures. Significance of fixed effects was assessed using the Satterthwaite method in linear mixed-effects models and the Wald chi-square test in generalized linear mixed-effects models. As one MAOA SNP and one MAOB SNP were analyzed, a Bonferroni-corrected threshold of p < 0.025 (0.05/2) was considered significant. If variant × sex interactions were significant in the full model, mixed-effects models were constructed in allelic subgroups under different XCI status assumptions (i.e., using different coding strategies). Post hoc comparisons were carried out using the emmeans package [60].
Power analyses were performed using the genpwr package assuming an additive genetic model [61]. MAFs of 29.8% (rs979605) and 45.6% (rs1799836) as observed in non-Finnish Europeans of gnomAD [36], an alpha level of 5%, and a power of 80% were used.
5. Conclusions
In conclusion, we observed that the MAOA rs979605(A>G) polymorphism was significantly associated with clinical improvement following ATD treatment in a sex-dependent manner. Female rs979605(A) homozygotes had higher HDRS scores compared to male A carriers after 6 months of treatment. Since rs979605 is linked to other MAOA genetic variants, this association may be due to the effect(s) of other linked variants. Given the role of MAOA in 5HT metabolism and previous associations of MAOA genetic variants with clinical improvement after ATD treatment, their potential as biomarkers for clinical improvement following ATD therapy should continue to be investigated.
Acknowledgments
We would like to thank the participants of the METADAP study, the staff of the Centre de Recherche en Epidemiologie et Santé des Populations, and the members of the Psychiatry Department at Bicêtre Hospital. We also thank the Centre de Ressources Biologiques Paris-Saclay (CRB Paris-Saclay) for the storage of METADAP’s biological samples (BRIF Number: BB-0033-00089). We would also like to thank Céline Bellenguez and Julie Le Borgne for their insight and discussion regarding X-linked genetic variant analysis.
Supplementary Materials
The supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijms24010497/s1.
Author Contributions
Conceptualization, K.C. and C.V.; methodology, K.C. and R.C.; software, K.C.; validation, C.V. and E.C.; formal analysis, K.C.; investigation, K.C.; resources, J.B., C.V., E.C., and B.F.; data curation, J.B., E.C., R.C., S.T., L.B. and B.F.; writing—original draft preparation, K.C. and C.V.; writing—review and editing, K.C., C.V., J.B., L.B., R.C., E.C. and B.F.; visualization, K.C.; supervision, C.V. and J.B.; project administration, E.C. and B.F.; funding acquisition, E.C. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study was registered by the French National Agency for Medicine and Health Products Safety (ANSM) and the Commission Nationale de l’Informatique et des Libert’es (CNIL). It was approved by the Ethics Committee of Paris-Boulogne (France) and conformed to international ethical standards (ClinicalTrials.gov identifier: NCT00526383). All patients provided written informed consent for study participation and for genetic analyses.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study data are under the protection of health data regulation set by the French National Commission on Informatics and Liberty (Commission Nationale de l’Informatique et des Libertés, CNIL) in line with European regulations, the Data Protection Act, and the Comité de protection des personnes (CPP, equivalent to the Research Ethics Committee). Data are not publicly available, as French law forbids free access to METADAP data. Data are available upon reasonable request to the principal investigator of the study (emmanuelle.corruble@aphp.fr).
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
The METADAP study was funded by a national grant (PHRC, AOM06022) and sponsored by the Assistance Publique-Hôpitaux de Paris (APHP) (ClinicalTrials.gov Identifier: NCT00526383).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.World Health Organization . Depression and Other Common Mental Disorders: Global Health Estimates. World Health Organization; Geneva, Switzerland: 2017. [Google Scholar]
- 2.LeGates T.A., Kvarta M.D., Thompson S.M. Sex differences in antidepressant efficacy. Neuropsychopharmacology. 2019;44:140–154. doi: 10.1038/s41386-018-0156-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Trivedi M.H., Hollander E., Nutt D., Blier P. Clinical evidence and potential neurobiological underpinnings of unresolved symptoms of depression. J. Clin. Psychiatry. 2008;69:246–258. doi: 10.4088/JCP.v69n0211. [DOI] [PubMed] [Google Scholar]
- 4.Uzbekov M.G. Monoamine Oxidase as a Potential Biomarker of the Efficacy of Treatment of Mental Disorders. Biochem. Mosc. 2021;86:773–783. doi: 10.1134/S0006297921060146. [DOI] [PubMed] [Google Scholar]
- 5.Jansson M., McCarthy S., Sullivan P.F., Dickman P., Andersson B., Oreland L., Schalling M., Pedersen N.L. MAOA haplotypes associated with thrombocyte-MAO activity. BMC Genet. 2005;6:46. doi: 10.1186/1471-2156-6-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Launay J.-M., Pino M.D., Chironi G., Callebert J., Peoc’h K., Mégnien J.-L., Mallet J., Simon A., Rendu F. Smoking Induces Long-Lasting Effects through a Monoamine-Oxidase Epigenetic Regulation. PLoS ONE. 2009;4:e7959. doi: 10.1371/journal.pone.0007959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tipton K., O’Sullivan J., Youdim M. Encyclopedia of Neuroscience. Elsevier; Amsterdam, The Netherlands: 2004. Monoamine oxidase (MAO): Functions in the central nervous system. [Google Scholar]
- 8.Meyer J.H., Ginovart N., Boovariwala A., Sagrati S., Hussey D., Garcia A., Young T., Praschak-Rieder N., Wilson A.A., Houle S. Elevated Monoamine Oxidase A Levels in the Brain: An Explanation for the Monoamine Imbalance of Major Depression. Arch. Gen. Psychiatry. 2006;63:1209. doi: 10.1001/archpsyc.63.11.1209. [DOI] [PubMed] [Google Scholar]
- 9.Moriguchi S., Wilson A.A., Miler L., Rusjan P.M., Vasdev N., Kish S.J., Rajkowska G., Wang J., Bagby M., Mizrahi R., et al. Monoamine Oxidase B Total Distribution Volume in the Prefrontal Cortex of Major Depressive Disorder. JAMA Psychiatry. 2019;76:634–641. doi: 10.1001/jamapsychiatry.2019.0044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meyer J.H., Wilson A.A., Sagrati S., Miler L., Rusjan P., Bloomfield P.M., Clark M., Sacher J., Voineskos A.N., Houle S. Brain Monoamine Oxidase A Binding in Major Depressive Disorder: Relationship to Selective Serotonin Reuptake Inhibitor Treatment, Recovery, and Recurrence. Arch. Gen. Psychiatry. 2009;66:1304–1312. doi: 10.1001/archgenpsychiatry.2009.156. [DOI] [PubMed] [Google Scholar]
- 11.Barton D.A., Esler M.D., Dawood T., Lambert E.A., Haikerwal D., Brenchley C., Socratous F., Hastings J., Guo L., Wiesner G., et al. Elevated Brain Serotonin Turnover in Patients With Depression: Effect of Genotype and Therapy. Arch. Gen. Psychiatry. 2008;65:38–46. doi: 10.1001/archgenpsychiatry.2007.11. [DOI] [PubMed] [Google Scholar]
- 12.Visser A.K.D., van Waarde A., Willemsen A.T.M., Bosker F.J., Luiten P.G.M., den Boer J.A., Kema I.P., Dierckx R.A.J.O. Measuring serotonin synthesis: From conventional methods to PET tracers and their (pre)clinical implications. Eur. J. Nucl. Med. Mol. Imaging. 2011;38:576–591. doi: 10.1007/s00259-010-1663-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Behl T., Kaur D., Sehgal A., Singh S., Sharma N., Zengin G., Andronie-Cioara F.L., Toma M.M., Bungau S., Bumbu A.G. Role of Monoamine Oxidase Activity in Alzheimer’s Disease: An Insight into the Therapeutic Potential of Inhibitors. Molecules. 2021;26:3724. doi: 10.3390/molecules26123724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Müller D.J., Serretti A., Sicard T., Tharmalingam S., King N., Artioli P., Mandelli L., Lorenzi C., Kennedy J.L. Further evidence of MAO-A gene variants associated with bipolar disorder. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2007;144B:37–40. doi: 10.1002/ajmg.b.30380. [DOI] [PubMed] [Google Scholar]
- 15.Yoshida K., Naito S., Takahashi H., Sato K., Ito K., Kamata M., Higuchi H., Shimizu T., Itoh K., Inoue K., et al. Monoamine oxidase: A gene polymorphism, tryptophan hydroxylase gene polymorphism and antidepressant response to fluvoxamine in Japanese patients with major depressive disorder. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2002;26:1279–1283. doi: 10.1016/S0278-5846(02)00267-1. [DOI] [PubMed] [Google Scholar]
- 16.Peters E.J., Slager S.L., McGrath P.J., Knowles J.A., Hamilton S.P. Investigation of serotonin-related genes in antidepressant response. Mol. Psychiatry. 2004;9:879–889. doi: 10.1038/sj.mp.4001502. [DOI] [PubMed] [Google Scholar]
- 17.Cusin C., Serretti A., Zanardi R., Lattuada E., Rossini D., Lilli R., Lorenzi C., Smeraldi E. Influence of monoamine oxidase A and serotonin receptor 2A polymorphisms in SSRI antidepressant activity. Int. J. Neuropsychopharmacol. 2002;5:27–35. doi: 10.1017/S1461145701002711. [DOI] [PubMed] [Google Scholar]
- 18.Müller D.J., Schulze T.G., Macciardi F., Ohlraun S., Gross M.M., Scherk H., Neidt H., Syagailo Y.V., Grässle M., Nöthen M.M., et al. Moclobemide Response in Depressed Patients: Association Study with a Functional Polymorphism in the Monoamine Oxidase A Promoter. Pharmacopsychiatry. 2002;35:157–158. doi: 10.1055/s-2002-33199. [DOI] [PubMed] [Google Scholar]
- 19.Tzeng D.-S., Chien C.-C., Lung F.-W., Yang C.-Y. MAOA gene polymorphisms and response to mirtazapine in major depression. Hum. Psychopharmacol. 2009;24:293–300. doi: 10.1002/hup.1024. [DOI] [PubMed] [Google Scholar]
- 20.Domschke K., Hohoff C., Mortensen L.S., Roehrs T., Deckert J., Arolt V., Baune B.T. Monoamine oxidase A variant influences antidepressant treatment response in female patients with Major Depression. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2008;32:224–228. doi: 10.1016/j.pnpbp.2007.08.011. [DOI] [PubMed] [Google Scholar]
- 21.Yu Y.W.-Y., Tsai S.-J., Hong C.-J., Chen T.-J., Chen M.-C., Yang C.-W. Association study of a monoamine oxidase a gene promoter polymorphism with major depressive disorder and antidepressant response. Neuropsychopharmacol. Off. Publ. Am. Coll. Neuropsychopharmacol. 2005;30:1719–1723. doi: 10.1038/sj.npp.1300785. [DOI] [PubMed] [Google Scholar]
- 22.Leuchter A.F., McCracken J.T., Hunter A.M., Cook I.A., Alpert J.E. Monoamine Oxidase A and Catechol-O-Methyltransferase Functional Polymorphisms and the Placebo Response in Major Depressive Disorder. J. Clin. Psychopharmacol. 2009;29:372–377. doi: 10.1097/JCP.0b013e3181ac4aaf. [DOI] [PubMed] [Google Scholar]
- 23.Tadić A., Müller M.J., Rujescu D., Kohnen R., Stassen H.H., Dahmen N., Szegedi A. The MAOA T941G polymorphism and short-term treatment response to mirtazapine and paroxetine in major depression. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2007;144B:325–331. doi: 10.1002/ajmg.b.30462. [DOI] [PubMed] [Google Scholar]
- 24.Bi Y., Ren D., Guo Z., Ma G., Xu F., Chen Z., An L., Zhang N., Ji L., Yuan F., et al. Influence and interaction of genetic, cognitive, neuroendocrine and personalistic markers to antidepressant response in Chinese patients with major depression. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2021;104:110036. doi: 10.1016/j.pnpbp.2020.110036. [DOI] [PubMed] [Google Scholar]
- 25.Hotamisligil G.S., Breakefield X.O. Human monoamine oxidase A gene determines levels of enzyme activity. Am. J. Hum. Genet. 1991;49:383–392. [PMC free article] [PubMed] [Google Scholar]
- 26.Tadić A., Rujescu D., Müller M.J., Kohnen R., Stassen H.H., Dahmen N., Szegedi A. A monoamine oxidase B gene variant and short-term antidepressant treatment response. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2007;31:1370–1377. doi: 10.1016/j.pnpbp.2007.05.015. [DOI] [PubMed] [Google Scholar]
- 27.Garpenstrand H., Ekblom J., Forslund K., Rylander G., Oreland L. Platelet monoamine oxidase activity is related to MAOB intron 13 genotype. J. Neural Transm. 2000;107:523–530. doi: 10.1007/s007020070075. [DOI] [PubMed] [Google Scholar]
- 28.Cotton A.M., Ge B., Light N., Adoue V., Pastinen T., Brown C.J. Analysis of expressed SNPs identifies variable extents of expression from the human inactive X chromosome. Genome Biol. 2013;14:R122. doi: 10.1186/gb-2013-14-11-r122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carrel L., Willard H.F. X-inactivation profile reveals extensive variability in X-linked gene expression in females. Nature. 2005;434:400–404. doi: 10.1038/nature03479. [DOI] [PubMed] [Google Scholar]
- 30.Stabellini R., de Mello J.C.M., Hernandes L.M., Pereira L.V. MAOA and GYG2 are submitted to X chromosome inactivation in human fibroblasts. Epigenetics. 2009;4:388–393. doi: 10.4161/epi.4.6.9492. [DOI] [PubMed] [Google Scholar]
- 31.Tukiainen T., Villani A.-C., Yen A., Rivas M.A., Marshall J.L., Satija R., Aguirre M., Gauthier L., Fleharty M., Kirby A., et al. Landscape of X chromosome inactivation across human tissues. Nature. 2017;550:244–248. doi: 10.1038/nature24265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pain O., Hodgson K., Trubetskoy V., Ripke S., Marshe V.S., Adams M.J., Byrne E.M., Campos A.I., Carrillo-Roa T., Cattaneo A., et al. Identifying the Common Genetic Basis of Antidepressant Response. Biol. Psychiatry Glob. Open Sci. 2022;2:115–126. doi: 10.1016/j.bpsgos.2021.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fabbri C., Kasper S., Kautzky A., Bartova L., Dold M., Zohar J., Souery D., Montgomery S., Albani D., Raimondi I., et al. Genome-wide association study of treatment-resistance in depression and meta-analysis of three independent samples. Br. J. Psychiatry. 2019;214:36–41. doi: 10.1192/bjp.2018.256. [DOI] [PubMed] [Google Scholar]
- 34.Uher R., Tansey K.E., Henigsberg N., Wolfgang M., Mors O., Hauser J., Placentino A., Souery D., Farmer A., Aitchison K.J., et al. Common Genetic Variation and Antidepressant Efficacy in Major Depressive Disorder: A Meta-Analysis of Three Genome-Wide Pharmacogenetic Studies. Am. J. Psychiatry. 2013;170:207–217. doi: 10.1176/appi.ajp.2012.12020237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Biernacka J.M., Sangkuhl K., Jenkins G., Whaley R.M., Barman P., Batzler A., Altman R.B., Arolt V., Brockmöller J., Chen C.H., et al. The International SSRI Pharmacogenomics Consortium (ISPC): A genome-wide association study of antidepressant treatment response. Transl. Psychiatry. 2015;5:e553. doi: 10.1038/tp.2015.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Karczewski K.J., Francioli L.C., Tiao G., Cummings B.B., Alföldi J., Wang Q., Collins R.L., Laricchia K.M., Ganna A., Birnbaum D.P., et al. The mutational constraint spectrum quantified from variation in 141,456 humans. Nature. 2020;581:434–443. doi: 10.1038/s41586-020-2308-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pinsonneault J.K., Papp A.C., Sadée W. Allelic mRNA expression of X-linked monoamine oxidase a (MAOA) in human brain: Dissection of epigenetic and genetic factors. Hum. Mol. Genet. 2006;15:2636–2649. doi: 10.1093/hmg/ddl192. [DOI] [PubMed] [Google Scholar]
- 38.Colle R., Masson P., Verstuyft C., Fève B., Werner E., Boursier-Neyret C., Walther B., David D.J., Boniface B., Falissard B., et al. Peripheral tryptophan, serotonin, kynurenine, and their metabolites in major depression: A case–control study. Psychiatry Clin. Neurosci. 2020;74:112–117. doi: 10.1111/pcn.12944. [DOI] [PubMed] [Google Scholar]
- 39.Del Río J.P., Alliende M.I., Molina N., Serrano F.G., Molina S., Vigil P. Steroid Hormones and Their Action in Women’s Brains: The Importance of Hormonal Balance. Front. Public Health. 2018;6:141. doi: 10.3389/fpubh.2018.00141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sun X., Ming Q., Zhong X., Dong D., Li C., Xiong G., Cheng C., Cao W., He J., Wang X., et al. The MAOA Gene Influences the Neural Response to Psychosocial Stress in the Human Brain. Front. Behav. Neurosci. 2020;14:65. doi: 10.3389/fnbeh.2020.00065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Frechilla D., Otano A., Del Rio J. Effect of chronic antidepressant treatment on transcription factor binding activity in rat hippocampus and frontal cortex. Prog. Neuropsychopharmacol. Biol. Psychiatry. 1998;22:787–802. doi: 10.1016/S0278-5846(98)00040-2. [DOI] [PubMed] [Google Scholar]
- 42.Wu J.B., Chen K., Li Y., Lau Y.-F.C., Shih J.C. Regulation of monoamine oxidase A by the SRY gene on the Y chromosome. FASEB J. 2009;23:4029–4038. doi: 10.1096/fj.09-139097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.O’Connor L., Gilmour J., Bonifer C. The Role of the Ubiquitously Expressed Transcription Factor Sp1 in Tissue-specific Transcriptional Regulation and in Disease. Yale J. Biol. Med. 2016;89:513–525. [PMC free article] [PubMed] [Google Scholar]
- 44.Jones D.N., Raghanti M.A. The role of monoamine oxidase enzymes in the pathophysiology of neurological disorders. J. Chem. Neuroanat. 2021;114:101957. doi: 10.1016/j.jchemneu.2021.101957. [DOI] [PubMed] [Google Scholar]
- 45.Brown L., Vranjkovic O., Li J., Yu K., Al Habbab T., Johnson H., Brown K., Jablonski M.R., Dechairo B. The clinical utility of combinatorial pharmacogenomic testing for patients with depression: A meta-analysis. Pharmacogenomics. 2020;21:559–569. doi: 10.2217/pgs-2019-0157. [DOI] [PubMed] [Google Scholar]
- 46.Meerman J.J., Janzing J.G.E., ter Hark S.E., Coenen M.J.H. The Potential of Polygenic Risk Scores to Predict Antidepressant Treatment Response in Major Depression: A systematic review. J. Affect. Disord. 2022;304:1–11. doi: 10.1016/j.jad.2022.02.015. [DOI] [PubMed] [Google Scholar]
- 47.Muthén B., Asparouhov T., Hunter A., Leuchter A. Growth Modeling with Non-Ignorable Dropout: Alternative Analyses of the STAR*D Antidepressant Trial. Psychol. Methods. 2011;16:17–33. doi: 10.1037/a0022634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen B., Craiu R.V., Strug L.J., Sun L. The X factor: A robust and powerful approach to X-chromosome-inclusive whole-genome association studies. Genet. Epidemiol. 2021;45:694–709. doi: 10.1002/gepi.22422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Corruble E., El Asmar K., Trabado S., Verstuyft C., Falissard B., Colle R., Petit A.-C., Gressier F., Brailly-Tabard S., Ferreri F., et al. Treating major depressive episodes with antidepressants can induce or worsen metabolic syndrome: Results of the METADAP cohort. World Psychiatry. 2015;14:366–367. doi: 10.1002/wps.20260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hamilton M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Morales J., Welter D., Bowler E.H., Cerezo M., Harris L.W., McMahon A.C., Hall P., Junkins H.A., Milano A., Hastings E., et al. A standardized framework for representation of ancestry data in genomics studies, with application to the NHGRI-EBI GWAS Catalog. Genome Biol. 2018;19:21. doi: 10.1186/s13059-018-1396-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bouali N., Francou B., Bouligand J., Imanci D., Dimassi S., Tosca L., Zaouali M., Mougou S., Young J., Saad A., et al. New MCM8 mutation associated with premature ovarian insufficiency and chromosomal instability in a highly consanguineous Tunisian family. Fertil. Steril. 2017;108:694–702. doi: 10.1016/j.fertnstert.2017.07.015. [DOI] [PubMed] [Google Scholar]
- 53.Chappell K., Francou B., Habib C., Huby T., Leoni M., Cottin A., Nadal F., Adnet E., Paoli E., Oliveira C., et al. Galaxy Is a Suitable Bioinformatics Platform for the Molecular Diagnosis of Human Genetic Disorders Using High-Throughput Sequencing Data Analysis. Five Years of Experience in a Clinical Laboratory. Clin. Chem. 2022;68:313–321. doi: 10.1093/clinchem/hvab220. [DOI] [PubMed] [Google Scholar]
- 54.R Core Team . R: A Language and Environment for Statistical Computing. R Core Team; Vienna, Austria: 2020. [Google Scholar]
- 55.Knaus B.J., Grünwald N.J. vcfr: A package to manipulate and visualize variant call format data in R. Mol. Ecol. Resour. 2017;17:44–53. doi: 10.1111/1755-0998.12549. [DOI] [PubMed] [Google Scholar]
- 56.Chappell K., Ait Tayeb A.E.K., Colle R., Bouligand J., El-Asmar K., Gressier F., Trabado S., David D.J., Feve B., Becquemont L., et al. The association of ARRB1 polymorphisms with response to antidepressant treatment in depressed patients. Front. Pharmacol. 2022;13:974570. doi: 10.3389/fphar.2022.974570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Anderson C.A., Pettersson F.H., Clarke G.M., Cardon L.R., Morris A.P., Zondervan K.T. Data quality control in genetic case-control association studies. Nat. Protoc. 2010;5:1564–1573. doi: 10.1038/nprot.2010.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Barrett J.C., Fry B., Maller J., Daly M.J. Haploview: Analysis and visualization of LD and haplotype maps. Bioinformatics. 2005;21:263–265. doi: 10.1093/bioinformatics/bth457. [DOI] [PubMed] [Google Scholar]
- 59.Bates D., Mächler M., Bolker B., Walker S. Fitting Linear Mixed-Effects Models Using lme4. J. Stat. Softw. 2015;67:1–48. doi: 10.18637/jss.v067.i01. [DOI] [Google Scholar]
- 60.Lenth R. emmeans: Estimated Marginal Means, aka Least-Squares Means 2022. [(accessed on 16 November 2022)]. Available online: https://cran.r-project.org/package=emmeans.
- 61.Moore C.M., Jacobson S.A., Fingerlin T.E. Power and Sample Size Calculations for Genetic Association Studies in the Presence of Genetic Model Misspecification. Hum. Hered. 2019;84:256–271. doi: 10.1159/000508558. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study data are under the protection of health data regulation set by the French National Commission on Informatics and Liberty (Commission Nationale de l’Informatique et des Libertés, CNIL) in line with European regulations, the Data Protection Act, and the Comité de protection des personnes (CPP, equivalent to the Research Ethics Committee). Data are not publicly available, as French law forbids free access to METADAP data. Data are available upon reasonable request to the principal investigator of the study (emmanuelle.corruble@aphp.fr).