Abstract
Using microarray technology, we studied the early differential expression of 3,528 genes in human meningothelial cells in response to meningococcal challenge. Thirty-two genes were up-regulated, and four were down-regulated. Those up-regulated included the tumor necrosis factor alpha, interleukin-6 (IL-6), and IL-8 (but not IL-1β) genes, suggesting that meningeal cells may be a local and early source of these cytokines. Also, a trend in up-regulation of anti-apoptotic genes and down-regulation of pro-apoptotic genes was observed. This is the first evidence that meningothelial cells may mount cytoprotective responses to pathogenic bacteria.
Neisseria meningitidis (meningococci) and Neisseria gonorrhoeae (gonococci) are the only two obligate human pathogens of the genus Neisseria, family Neisseriaceae. N. meningitidis is a major cause of septicemia and meningitis, while N. gonorrhoeae is the agent of gonorrhoea. Meningococcal infection starts with colonization of the upper respiratory tract, i.e., nasopharyngeal and tonsillar mucosa. Following mucosal adherence, and a period of adaptation and proliferation, meningococci can initiate a parasite-directed endocytosis by nonciliated epithelial cells (41–43) and subsequently gain access to the circulation.
After a limited phase of bacteremia, meningococci are able to bind and subsequently cross the blood-brain barrier (BBB) to enter the subarachnoid space. The leptomeninges surrounding the subarachnoid space consist of the arachnoid mater and the pia mater, separated by trabeculae and lined by a type of epithelium termed meningothelial cells (1). The basic cell type and fine structure of these layers have many similarities. Invasion of the BBB can occur at either the meningeal capillaries or the choroid plexus. Meningeal capillaries possess an endothelial layer that elaborates tight junctions with extremely high electrical resistance (7). The choroid plexus, however, comprises a central core of blood vessels, the endothelial layer of which is similar in structure to peripheral capillaries, covered by epithelial cells that possess tight junctions. Although preferential binding of N. meningitidis to the epithelium of choroid plexus has been observed, invasion through the meningeal capillaries constitutes another potential route to the subarachnoid space (35). Further, meningococci have been shown to cross a monolayer of tight-junction-forming epithelial cells using a transcellular pathway which does not affect the barrier function of tight junctions (37).
Following invasion of the BBB, meningococcal meningitis is characterized by the presence of high levels of the pro-inflammatory cytokines tumor necrosis factor alpha (TNF-α), interleukin-1β (IL-1β), and IL-6 and the chemokine IL-8 (CXCL8) in cerebral spinal fluid (CSF) and the recruitment of large numbers of leukocytes (47, 48), but there is conflicting evidence regarding the cellular source of these cytokines. Bacterial meningitis, as opposed to other forms of the condition, is associated with increased levels of the chemokines IL-8, growth-related oncogene alpha (CXCL1), monocyte chemotactic protein 1 (MCP-1) (CCL2), macrophage inflammatory protein 1α (MIP-1α) (CCL3), and MIP-1β (CCL4). It has been proposed that these chemokines contribute to the rapid initial influx of neutrophils that is later followed by monocytes and T cells (47).
High concentrations of cytokines within the CSF of patients with meningitis, but with undetectable levels of the same cytokines in plasma, suggests that the cytokines are locally produced (25, 30, 32). Possible tissue sources for local cytokines in the CSF include microglia, activated astrocytes, neurons, microvascular endothelial cells, choriod plexus epithelial cells, and meningothelial cells (9, 29, 47). For example, the choroid plexus ependymal cells of pig and guinea pig have been shown to produce TNF-α following in vitro and in vivo endotoxin challenge (46). Choroid plexus and arachnoid membrane was also shown to express high levels of intercellular adhesion molecule 1 (ICAM-1) along the microvilli in lipopolysaccharide-stimulated rats (12).
The receptor-mediated infiltration of leukocytes and resulting CSF pleocytosis provides another rich source of chemokine production which further complicates the question of the origin of pro-inflammatory cytokines and chemokines. Studies in rabbits have detected TNF-α mRNA within leukocytes during inflammation of the meninges in a pneumococcal meningitis model (6, 52), while in rats, pro-inflammatory and anti-inflammatory cytokines were shown to be expressed by the brain parenchyma (10). Another source of cytokines may involve blood-borne cytokines crossing the BBB using a saturable transport system. Evidence shows that passage of cytokines across the BBB occurs, which may potentially affect brain function (4, 5).
Meningiomas are benign epithelial meningeal tumors that arise from arachnoidal meningothelial cells and have been demonstrated as a suitable model for N. meningitidis interactions (19). Pilus-mediated adherence to a meningioma monolayer has been shown, but there was no evidence of invasion (19). In this study we used cDNA expression arrays to identify early differential gene expression induced by meningococcal challenge, focusing on whether meninges-derived human cells may be a source of the cytokines detected in CSF during meningitis.
Human meningothelial cells, obtained from surgically removed tumors of several patients, were isolated and cultured using a method based on that described by Hardy et al. (19). The epithelial origin of the cultured cells was confirmed with the detection of the epithelial membrane antigen and desmoplakins I and II (13, 19) by fluorescence microscopy (data not shown). Meningiomas of passage 5 were grown to confluence in two separate 175-cm2 tissue culture flasks (Nunc) using Dulbecco's modified Eagle medium (DMEM; GIBCO, Paisley, United Kingdom) supplemented with 10% fetal calf serum and 1% antibiotic-antimycotic (GIBCO). N. meningitidis strain MC58 (B:15:P1.7.16b) was cultured in Mueller-Hinton broth (Oxoid, Basingstoke, United Kingdom) to mid-logarithmic phase and diluted to approximately 106 CFU/ml. The cell monolayers were washed three times with DMEM to remove fetal calf serum and antibiotics. DMEM containing 107 meningococci (confirmed by viable count) was added to the test monolayer, while the control received fresh DMEM only.
Both the test and control flasks were incubated in 5% CO2 at 37°C for 4 h; meningococci were then removed, and both monolayers were washed three times with fresh DMEM. Total RNA was extracted from each monolayer using an RNeasy Mini kit (Qiagen Ltd, Crawley, United Kingdom) according to the manufacturer's recommendations. Radiolabeled probes were synthesized and used to probe three human broad-range cDNA expression arrays (Atlas arrays; Clontech Laboratories Inc., Palo Alto, Calif.), 1.2I, 1.2II, and 1.2III. Membranes were subjected to autoradiography using Biomax MR film (Kodak) to detect radiolabeled signals. These experiments were repeated twice on two different patients' meningothelial cells, and reproducible results were obtained.
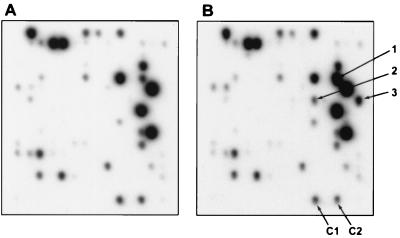
Dots were analyzed using transmission densitometry and NIH Image 1.62 software. Figure 1 shows an example of differential gene expression representing F-block, Atlas array 1.2I.
FIG. 1.
Microarray results from human Atlas array 1.2I (F block) of equivalently exposed hybridizations from meningioma cells (A) and meningioma cells incubated with N. meningitidis for 4 h (B). Examples of differentially expressed genes and controls are indicated on array B. Controls are cytoplasmic β-actin (C1) and 60S ribosomal protein L13A (C2), respectively. Up-regulated genes indicated: 1, MCP-1; 2, MIP-2α; 3, IL-8.
The ratios for potential differentially regulated genes were calculated after correction for probe variation using constitutively expressed genes on equivalent arrays. Independently, 20 constitutively expressed control genes, including those involved in the cell cycle, were compared on respective arrays and calculated to change by only 1.00 ± 0.17-fold. Any genes calculated to have a differential expression of less than 1.5-fold were disregarded. This very stringent cutoff value was set to eliminate false positives, but it should be noted that doing so may have excluded some genes that were differentially expressed by low, but biologically significant amounts.
From the three arrays, incorporating cDNA from 3,528 human genes, only 32 genes were up-regulated and 4 were down-regulated after 4 h of incubation with meningococci. Many of these meningeal-derived genes were associated with inflammatory cytokine responses or apoptosis and could be grouped accordingly. The genes which did not fall into either of these categories were involved in, for example, cell signaling and transcriptional regulation. The differentially expressed genes are listed in Table 1, together with their fold-difference expression levels.
TABLE 1.
Meningeal genes differentially regulated following meningococcal challenge for 4 h
| Genes and products | Expression levels
|
|
|---|---|---|
| Fold increase | Fold decrease | |
| Cytokine, chemokine, and adhesion molecule genes | ||
| IL-6a | 4.0 | |
| IL-8a | +b | |
| ICAM-1a | 10.0 | |
| LIFa | 12.0 | |
| MIP-2αa | 113 | |
| MCP-1a | 11.0 | |
| Opnc | 5.0 | |
| TNF-αa | 350 | |
| VCAM-1a | 2.9 | |
| VEGFa | 4.9 | |
| Apoptosis-related genes | ||
| BB2-bombesin receptorc | + | |
| BDNFa | 6.0 | |
| Caspase 10a | 6.0 | |
| IEX-1L anti-death proteina | + | |
| IRF-1a | 3.5 | |
| Opnc | 5.0 | |
| Other regulated genes | ||
| Bcl-3a | 6.4 | |
| B94 proteina | 2.5 | |
| Basic helix-loop-helix protein DEC1c | 1.9 | |
| E16 amino acid transportera | 3.2 | |
| Erythroblastosis virus oncoprotein homolog ETS-1; p54ac | 2.8 | |
| Fos-related antigen (Fra-1)a | 4.8 | |
| 40S rRNAa | 5.0 | |
| gadd45a | 5.3 | |
| Glucose transporter 1a | 2.3 | |
| Guanine nucleotide binding proteina | + | |
| Human immunodeficiency virus enhancer binding protein 2a | 3.8 | |
| Insulin-like growth factor binding protein 1a | 1.5 | |
| NOR-1c | + | |
| Placenta growth factors 1 and 2a | 1.6 | |
| Proto-oncoprotein c-Jun; transcription factor AP-1a | 2.0 | |
| RNA polymerase II subunitd | 1.8 | |
| Stanniocalcinc | 3.4 | |
| Sterol-C5 desaturasec | 10.0 | |
| Transforming growth factor-β inducible early genec | 4.2 | |
| TG-interacting factorc | 1.6 | |
| Transcription factor AP-2a | 8.4 | |
| Vav-2 proteinc | 7.5 | |
Atlas array 1.2 I.
+, not detected on control arrays, represented by array A (Fig. 1).
Atlas array 1.2 II.
Atlas array 1.2 III.
This investigation demonstrated an up-regulation of gene expression for several pro-inflammatory cytokines and chemokines by meningioma cells (after only 4 h), suggesting that TNF-α, IL-6, and IL-8 are capable of being produced by epithelial cells of the meninges in response to meningococci. Expression of IL-1β, however, was not up-regulated, despite a report that it may be produced by ventricular ependymal cells of the BBB during bacterial meningitis (47). A recent study of meningeal inflammation demonstrated that this cytokine was produced by macrophages present in the meninges (16), and a study of inflammatory responses to experimental human gonococcal infections (38) similarly found local IL-6, IL-8, and TNF-α production, but IL-1β proved to be derived from infiltrating leukocytes. The present data are therefore consistent with these findings.
Up-regulated gene expression of several additional pro-inflammatory factors, i.e., MIP-2α (CXCL2), MCP-1, leukemia-inhibitory factor (LIF), vascular endothelial growth factor (VEGF), and osteopontin (Opn), was detected; however, there was no differential expression of genes encoding anti-inflammatory factors such as transforming growth factor-β (8) and IL-11 (23). It has recently been shown that TNF-α expression may be induced by brief incubation of monocytes and endothelial cells with meningococci (45). This cytokine has many functions, including increased local vascular permeability (providing enhanced access for immune cells, antibodies, and complement) and induction of MIP-2 production by microvascular endothelial cells after traumatic brain injury (34); it also performs an important role in containing local infection by blood vessel occlusion. TNF-α is required for efficient clearance of meningococci in the early phase of infection in animal models (50), but extreme high levels in CSF have been shown to correlate with damage to the BBB (39). IL-6 is another factor with pleiotropic effects, including lymphocyte activation and enhancement of antibody production, but it performs a number of crucial functions in the CNS, coordinating neuroimmune function and protecting neurons from damage (17). IL-8 and MIP-2α have similar functions as chemotactic factors for neutrophils (3, 26), while MCP-1 is a chemoattractant for monocytes, inducing their migration from the bloodstream to become tissue macrophages (36). High levels of VEGF, known to induce expression of the chemokine MCP-1 (28), have been found in the CSF of patients with carcinomatous or bacterial meningitis (44), and LIF (a member of the IL-6 family of cytokines) also induces MCP-1 expression (20). Opn, which is induced by TNF-α, is expressed at high levels during early stages of cell-mediated immunity in vivo (2). It is involved in the recruitment and activation of leukocytes, polarizing early T-helper 1 subset responses through induction of monocytes to produce IL-12 and inhibition of IL-10.
Up-regulated gene expression of the vascular cell adhesion molecule 1 (VCAM-1) and ICAM-1, which mediate the adhesion and migration of leukocytes, was also detected in meningioma cells after incubation with meningococci. This was consistent with the findings of Dixon and coworkers (11), who showed that N. meningitidis and its lipooligosaccharide are potent inducers of these adhesion molecules in human umbilical vein endothelial cells. Early effects of meningococci upon meningeal cells therefore include the production of pro-inflammatory cytokines and chemokines and up-regulation of adhesion molecules, for recruitment of macrophages, polymorphonucleocytes, and lymphocytes to the area of infection, thus promoting the removal of invading pathogens.
In addition to proinflammatory cytokine and adhesion molecule genes, differential expression levels of a number of apoptosis-related genes were also detected following incubation of meningioma cells with meningococci. Apoptosis is the ordered process of elimination of cells in a manner which, in contrast with necrosis, does not evoke an inflammatory response. There are several main pathways leading to apoptosis, including positive induction mediated by the binding of TNF-like ligands to membrane receptors, negative induction by the loss of activity of a suppressor, the ceramide pathway secondary to membrane change, and the mitochondrial pathway. These pathways lead to the activation of a cascade of cysteine aspartate-specific proteases (caspases), which are responsible for disassembly of the cell and formation of apoptotic bodies. There is accumulating evidence that apoptosis plays an important role in the pathogenesis of a variety of infectious diseases, where pathogens induce or block the process (15). Interestingly, conflicting evidence exists relating to the neisserial porin PorB and its ability to induce (31) or protect (28a) epithelial cell lines from apoptosis. It is known that translocation of the neisserial porin Por B into host cell membranes triggers apoptosis in epithelial cell lines in vitro, increasing cytosolic concentrations of calcium ions and thus activating caspase 3 (31).
An early effect of meningococcal interaction with meningioma cells appeared to be changes in gene expression which would, collectively, lead to inhibition of apoptosis. There was no differential gene expression of the pro-apoptotic initiator and effector genes including caspases 1 to 9 (40). Gene expression of caspase 10, however, an initiator of the caspase cascade (49), was down-regulated along with brain-derived neurotrophic factor (BDNF), which has both positive and negative effects upon apoptosis. BDNF is known to be synthesized by hippocampal and cortical neurons and accelerates nitric oxide-induced apoptosis of cultured cortical neuronal cells (22). Conversely, it is able to block caspase 3 activation in neonatal brain (18). IEX-1L anti-death protein gene expression, however, was up-regulated, and this molecule has anti-apoptotic activity, playing an important role in the protection of cells from Fas- or TNF-α-induced apoptosis (51). The BB2-bombesin receptor was also up-regulated; bombesin is known to inhibit apoptosis during fetal lung development via interaction with this receptor (24) and to make human umbilical vein endothelial cells less susceptible to cell death induced by serum deprivation (14). As described previously, Opn gene expression was up-regulated; in addition to its pro-inflammatory role, it functions to inhibit apoptosis in several cell types and has been associated with the repair of damaged tissue following inflammation (33). Although the general trend appears to be toward the increased expression of protective anti-apoptotic genes and down-regulation of pro-apoptotic genes, interferon regulatory factor 1 (IRF-1) stands out as the exception. Up-regulation of IRF-1, which is known to be a positive mediator of apoptosis (21), was detected. Collectively, however, differential expression of apoptosis-related genes by cells of the meninges is an important novel finding.
It would be inappropriate to comment on the actual values of increased or decreased gene expression, since differences at the transcriptional level may not result in a similar up- or down-regulation in protein expression. Indeed, the magnitude of the differential in gene expression may not reflect biological significance (27). In future experiments, assays will be carried out to measure the kinetics and amounts of cytokines and chemokines produced, so that the issue of biological activity can be addressed. The mechanisms by which these pro-inflammatory and apoptosis-related responses are induced by meningococci will be investigated and compared in meningioma cells and other cell lines including endothelial cells.
In summary, there were two major categories defining the early gene responses of meningeal-derived cells to meningococcal challenge. First, the cells were stimulated to up-regulate transcription of pro-inflammatory cytokine, chemokine, and adhesion molecule genes, which in vivo could lead to the recruitment of leukocytes, thus promoting removal of these pathogens. These data indicate that cells of the meninges may be an early source of the cytokines and chemokines found in CSF during meningitis. Second, the differential expression of several genes involved in apoptosis is a novel and important finding. It represents the first evidence that cells of the BBB actually take measures to resist the damaging effects of pathogenic bacteria. Such responses may ultimately have a role in maintaining the integrity of the BBB and preventing infectious organisms from entering brain tissues during meningitis.
Acknowledgments
We thank J. Firth and J. Punt (Department of Neurosciences) for providing meningeal tumors, Janet Palmer and Kathi Fowkes for help with handling meningiomas, and J. Lowe and K. Robson, who helped with diagnosis of tumors. For critically reviewing the manuscript, we thank J. Lowe, Ian Todd, and Adrian Robins. We also thank Sue Stevens for technical support.
This study was supported by the Dr. Hadwen Trust for Humane Research.
REFERENCES
- 1.Alcolado R, Weller R O, Parrish E P, Garrod D. The cranial arachnoid and pia mater in man: anatomical and ultrastructural observations. Neuropathol Appl Neurobiol. 1988;14:1–17. doi: 10.1111/j.1365-2990.1988.tb00862.x. [DOI] [PubMed] [Google Scholar]
- 2.Ashkar S, Weber G F, Panoutsakopoulou V, Sanchirico M E, Jansson M, Zawaideh S, Rittling S R, Denhardt D T, Glimcher M J, Cantor H. Eta-1 (osteopontin): an early component of type-1 (cell-mediated) immunity. Science. 2000;287:860–864. doi: 10.1126/science.287.5454.860. [DOI] [PubMed] [Google Scholar]
- 3.Baggiolini M, Loetscher P. Chemokines in inflammation and immunity. Immunol Today. 2000;21:418–420. doi: 10.1016/s0167-5699(00)01672-8. [DOI] [PubMed] [Google Scholar]
- 4.Banks W A, Kastin A J, Broadwell R D. Passage of cytokines across the blood-brain barrier. Neuroimmunomodulation. 1995;2:241–248. doi: 10.1159/000097202. [DOI] [PubMed] [Google Scholar]
- 5.Banks W A, Plotkin S R, Kastin A J. Permeability of the blood-brain barrier to soluble cytokine receptors. Neuroimmunomodulation. 1995;2:161–165. doi: 10.1159/000096887. [DOI] [PubMed] [Google Scholar]
- 6.Bitsch A, Trostdorf F, Bruck W, Schmidt H, Fischer F R, Nau R. Central nervous system TNFalpha-mRNA expression during rabbit experimental pneumococcal meningitis. Neurosci Lett. 1997;237:105–108. doi: 10.1016/s0304-3940(97)00830-6. [DOI] [PubMed] [Google Scholar]
- 7.Butt A M, Jones H C, Abbott N J. Electrical resistance across the blood-brain barrier in anaesthetized rats: a developmental study. J Physiol (London) 1990;429:47–62. doi: 10.1113/jphysiol.1990.sp018243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cerwenka A, Swain S L. TGF-betal: immunosuppressant and viability factor for T lymphocytes. Microbes Infect. 1999;1:1291–1296. doi: 10.1016/s1286-4579(99)00255-5. [DOI] [PubMed] [Google Scholar]
- 9.Chao C C, Hu S, Close K, Choi C S, Molitor T W, Novick W J, Peterson P K. Cytokine release from microglia: differential inhibition by pentoxifylline and dexamethasone. J Infect Dis. 1992;166:847–853. doi: 10.1093/infdis/166.4.847. [DOI] [PubMed] [Google Scholar]
- 10.Diab A, Zhu J, Lindquist L, Wretlind B, Bakhiet M, Link H. Haemophilus influenzae and Streptococcus pneumoniae induce different intracerebral mRNA cytokine patterns during the course of experimental bacterial meningitis. Clin Exp Immunol. 1997;109:233–241. doi: 10.1046/j.1365-2249.1997.4441343.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dixon G L, Heyderman R S, Kotovicz K, Jack D L, Andersen S R, Vogel U, Frosch M, Klein N. Endothelial adhesion molecule expression and its inhibition by recombinant bactericidal/permeability-increasing protein are influenced by the capsulation and lipooligosaccharide structure of Neisseria meningitidis. Infect Immun. 1999;67:5626–5633. doi: 10.1128/iai.67.11.5626-5633.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Endo H, Sasaki K, Tonosaki A, Kayama T. Three-dimensional and ultrastructural ICAM-1 distribution in the choroid plexus, arachnoid membrane and dural sinus of inflammatory rats induced by LPS injection in the lateral ventricles. Brain Res. 1998;793:297–301. doi: 10.1016/s0006-8993(98)00042-0. [DOI] [PubMed] [Google Scholar]
- 13.Feurer D J, Weller R O. Barrier functions of the leptomeninges: a study of normal meninges and meningiomas in tissue culture. Neuropathol Appl Neurobiol. 1991;17:391–405. doi: 10.1111/j.1365-2990.1991.tb00739.x. [DOI] [PubMed] [Google Scholar]
- 14.Fukai F, Mashimo M, Akiyama K, Goto T, Tanuma S, Katayama T. Modulation of apoptotic cell death by extracellular matrix proteins and a fibronectin-derived antiadhesive peptide. Exp Cell Res. 1998;242:92–99. doi: 10.1006/excr.1998.4076. [DOI] [PubMed] [Google Scholar]
- 15.Gao L Y, Kwaik Y A. The modulation of host cell apoptosis by intracellular bacterial pathogens. Trends Microbiol. 2000;8:306–313. doi: 10.1016/s0966-842x(00)01784-4. [DOI] [PubMed] [Google Scholar]
- 16.Garabedian B V, Lemaigre-Dubreuil Y, Mariani J. Central origin of IL-1beta produced during peripheral inflammation: role of meninges. Brain Res Mol Brain Res. 2000;75:259–263. doi: 10.1016/s0169-328x(99)00320-4. [DOI] [PubMed] [Google Scholar]
- 17.Gruol D L, Nelson T E. Physiological and pathological roles of interleukin-6 in the central nervous system. Mol Neurobiol. 1997;15:307–339. doi: 10.1007/BF02740665. [DOI] [PubMed] [Google Scholar]
- 18.Han B H, Holtzman D M. BDNF protects the neonatal brain from hypoxic-ischemic injury in vivo via the ERK pathway. J Neurosci. 2000;20:5775–5781. doi: 10.1523/JNEUROSCI.20-15-05775.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hardy S J, Christodoulides M, Weller R O, Heckels J E. Interactions of Neisseria meningitidis with cells of the human meninges. Mol Microbiol. 2000;36:817–829. doi: 10.1046/j.1365-2958.2000.01923.x. [DOI] [PubMed] [Google Scholar]
- 20.Hartner A, Goppelt-Struebe M, Hocke G M, Sterzel R B. Differential regulation of chemokines by leukemia inhibitory factor, interleukin-6 and oncostatin M. Kidney Int. 1997;51:1754–1760. doi: 10.1038/ki.1997.241. [DOI] [PubMed] [Google Scholar]
- 21.Iadecola C, Salkowski C A, Zhang F, Aber T, Nagayama M, Vogel S N, Ross M E. The transcription factor interferon regulatory factor 1 is expressed after cerebral ischemia and contributes to ischemic brain injury. J Exp Med. 1999;189:719–727. doi: 10.1084/jem.189.4.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ishikawa Y, Ikeuchi T, Hatanaka H. Brain-derived neurotrophic factor accelerates nitric oxide donor-induced apoptosis of cultured cortical neurons. J Neurochem. 2000;75:494–502. doi: 10.1046/j.1471-4159.2000.0750494.x. [DOI] [PubMed] [Google Scholar]
- 23.Ito Y, Yamamoto M, Li M, Mitsuma N, Tanaka F, Doyu M, Suzumura A, Mitsuma T, Sobue G. Temporal expression of mRNAs for neuropoietic cytokines, interleukin-11 (IL-11), oncostatin M (OSM), cardiotrophin-1 (CT-1) and their receptors (IL-11Ralpha and OSMRbeta) in peripheral nerve injury. Neurochem Res. 2000;25:1113–1118. doi: 10.1023/a:1007674113440. [DOI] [PubMed] [Google Scholar]
- 24.Kresch M, Christian C, Zhu L, Obe M, Sanders M M, Hussain N. Bombesin inhibits apoptosis in developing fetal rat lung. Lung. 1999;177:241–251. doi: 10.1007/pl00007644. [DOI] [PubMed] [Google Scholar]
- 25.Leist T P, Frei K, Kam-Hansen S, Zinkernagel R M, Fontana A. Tumor necrosis factor alpha in cerebrospinal fluid during bacterial, but not viral, meningitis. Evaluation in murine model infections and in patients. J Exp Med. 1988;167:1743–1748. doi: 10.1084/jem.167.5.1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Magazin M, Vita N, Cavrois E, Lefort S, Guillemot J C, Ferrara P. The biological activities of gro beta and IL-8 on human neutrophils are overlapping but not identical. Eur Cytokine Netw. 1992;3:461–467. [PubMed] [Google Scholar]
- 27.Manger I D, Relman D A. How the host ‘sees’ pathogens: global gene expression responses to infection. Curr Opin Immunol. 2000;12:215–218. doi: 10.1016/s0952-7915(99)00077-1. [DOI] [PubMed] [Google Scholar]
- 28.Marumo T, Schini-Kerth V B, Busse R. Vascular endothelial growth factor activates nuclear factor-kappaB and induces monocyte chemoattractant protein-1 in bovine retinal endothelial cells. Diabetes. 1999;48:1131–1137. doi: 10.2337/diabetes.48.5.1131. [DOI] [PubMed] [Google Scholar]
- 28a.Massori P, Ho Y, Wetzler L M. Neisseria meningitidis porin PorB interacts with mitochondria and protects cells from apoptosis. Proc Natl Acad Sci USA. 2000;97:9070–9075. doi: 10.1073/pnas.97.16.9070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Medana I M, Hunt N H, Chaudhri G. Tumor necrosis factor-alpha expression in the brain during fatal murine cerebral malaria: evidence for production by microglia and astrocytes. Am J Pathol. 1997;150:1473–1486. [PMC free article] [PubMed] [Google Scholar]
- 30.Moller B, Mogensen S C, Wendelboe P, Bendtzen K, Petersen C M. Bioactive and inactive forms of tumor necrosis factor-alpha in spinal fluid from patients with meningitis. J Infect Dis. 1991;163:886–889. doi: 10.1093/infdis/163.4.886. [DOI] [PubMed] [Google Scholar]
- 31.Muller A, Gunther D, Dux F, Naumann M, Meyer T F, Rudel T. Neisserial porin (PorB) causes rapid calcium influx in target cells and induces apoptosis by the activation of cysteine proteases. EMBO J. 1999;18:339–352. doi: 10.1093/emboj/18.2.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mustafa M M, Ramilo O, Olsen K D, Franklin P S, Hansen E J, Beutler B, McCracken G H., Jr Tumor necrosis factor in mediating experimental Haemophilus influenzae type B meningitis. J Clin Investig. 1989;84:1253–1259. doi: 10.1172/JCI114292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.O'Regan A W, Nau G J, Chupp G L, Berman J S. Osteopontin (Eta-1) in cell-mediated immunity: teaching an old dog new tricks. Immunol Today. 2000;21:475–478. doi: 10.1016/s0167-5699(00)01715-1. [DOI] [PubMed] [Google Scholar]
- 34.Otto V I, Heinzel-Pleines U E, Gloor S M, Trentz O, Kossmann T, Morganti-Kossmann M C. sICAM-1 and TNF-alpha induce MIP-2 with distinct kinetics in astrocytes and brain microvascular endothelial cells. J Neurosci Res. 2000;60:733–742. doi: 10.1002/1097-4547(20000615)60:6<733::AID-JNR5>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 35.Pron B, Taha M K, Rambaud C, Fournet J C, Pattey N, Monnet J P, Musilek M, Beretti J L, Nassif X. Interaction of Neisseria meningitidis with the components of the blood-brain barrier correlates with an increased expression of PilC. J Infect Dis. 1997;176:1285–1292. doi: 10.1086/514124. [DOI] [PubMed] [Google Scholar]
- 36.Proost P, Wuyts A, Van Damme J. Human monocyte chemotactic proteins-2 and -3: structural and functional comparison with MCP-1. J Leukoc Biol. 1996;59:67–74. doi: 10.1002/jlb.59.1.67. [DOI] [PubMed] [Google Scholar]
- 37.Pujol C, Eugene E, de Saint Martin L, Nassif X. Interaction of Neisseria meningitidis with a polarized monolayer of epithelial cells. Infect Immun. 1997;65:4836–4842. doi: 10.1128/iai.65.11.4836-4842.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ramsey K H, Schneider H, Cross A S, Boslego J W, Hoover D L, Staley T L, Kuschner R A, Deal C D. Inflammatory cytokines produced in response to experimental human gonorrhea. J Infect Dis. 1995;172:186–191. doi: 10.1093/infdis/172.1.186. [DOI] [PubMed] [Google Scholar]
- 39.Sharief M K, Ciardi M, Thompson E J. Blood-brain barrier damage in patients with bacterial meningitis: association with tumor necrosis factor-alpha but not interleukin-1 beta. J Infect Dis. 1992;166:350–358. doi: 10.1093/infdis/166.2.350. [DOI] [PubMed] [Google Scholar]
- 40.Stennicke H R, Salvesen G S. Catalytic properties of the caspases. Cell Death Differ. 1999;6:1054–1059. doi: 10.1038/sj.cdd.4400599. [DOI] [PubMed] [Google Scholar]
- 41.Stephens D S. Gonococcal and meningococcal pathogenesis as defined by human cell, cell culture, and organ culture assays. Clin Microbiol Rev. 1989;2(Suppl):S104–S111. doi: 10.1128/cmr.2.suppl.s104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stephens D S, Farley M M. Pathogenic events during infection of the human nasopharynx with Neisseria meningitidis and Haemophilus influenzae. Rev Infect Dis. 1991;13:22–33. doi: 10.1093/clinids/13.1.22. [DOI] [PubMed] [Google Scholar]
- 43.Stephens D S, McGee Z A. Attachment of Neisseria meningitidis to human mucosal surfaces: influence of pili and type of receptor. J Infect Dis. 1981;143:525–532. doi: 10.1093/infdis/143.4.525. [DOI] [PubMed] [Google Scholar]
- 44.Stockhammer G, Poewe W, Burgstaller S, Deisenhammer F, Muigg A, Kiechl S, Schmutzhard E, Maier H, Felber S, Schumacher P, Gunsilius E, Gastl G. Vascular endothelial growth factor in CSF: a biological marker for carcinomatous meningitis. Neurology. 2000;54:1670–1676. doi: 10.1212/wnl.54.8.1670. [DOI] [PubMed] [Google Scholar]
- 45.Taha M K. Neisseria meningitidis induces the expression of the TNF-alpha gene in endothelial cells. Cytokine. 2000;12:21–25. doi: 10.1006/cyto.1999.0506. [DOI] [PubMed] [Google Scholar]
- 46.Tarlow M J, Jenkins R, Comis S D, Osborne M P, Stephens S, Stanley P, Crocker J. Ependymal cells of the choroid plexus express tumour necrosis factor-alpha. Neuropathol Appl Neurobiol. 1993;19:324–328. doi: 10.1111/j.1365-2990.1993.tb00447.x. [DOI] [PubMed] [Google Scholar]
- 47.Tauber M G, Moser B. Cytokines and chemokines in meningeal inflammation: biology and clinical implications. Clin Infect Dis. 1999;28:1–11. doi: 10.1086/515079. [DOI] [PubMed] [Google Scholar]
- 48.Waage A, Halstensen A, Shalaby R, Brandtzaeg P, Kierulf P, Espevik T. Local production of tumor necrosis factor alpha, interleukin 1, and interleukin 6 in meningococcal meningitis. Relation to the inflammatory response. J Exp Med. 1989;170:1859–1867. doi: 10.1084/jem.170.6.1859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang J, Zheng L, Lobito A, Chan F K, Dale J, Sneller M, Yao X, Puck J M, Straus S E, Lenardo M J. Inherited human caspase 10 mutations underlie defective lymphocyte and dendritic cell apoptosis in autoimmune lymphoproliferative syndrome type II. Cell. 1999;98:47–58. doi: 10.1016/S0092-8674(00)80605-4. [DOI] [PubMed] [Google Scholar]
- 50.Westendorp, R. G., J. A. Langermans, T. W. Huizinga, C. L. Verweij, and A. Sturk. 1997. Genetic influence on cytokine production in meningococcal disease. 349:1912–1913. [DOI] [PubMed]
- 51.Wu M X, Ao Z, Prasad K V, Wu R, Schlossman S F. IEX-IL, an apoptosis inhibitor involved in NF-kappaB-mediated cell survival. Science. 1998;281:998–1001. doi: 10.1126/science.281.5379.998. [DOI] [PubMed] [Google Scholar]
- 52.Zysk G, Bruck W, Huitinga I, Fischer F R, Flachsbarth F, van Rooijen N, Nau R. Elimination of blood-derived macrophages inhibits the release of interleukin-1 and the entry of leukocytes into the cerebrospinal fluid in experimental pneumococcal meningitis. J Neuroimmunol. 1997;73:77–80. doi: 10.1016/s0165-5728(96)00173-7. [DOI] [PubMed] [Google Scholar]