Abstract
The consistent increase of Coronavirus disease 2019 (COVID-19) cases parallel with the rate of deaths and the controversial response regarding the vaccines caused an increase in the burden of psychological diseases. This study aimed to evaluate the psychological condition of healthcare workers (HCWs) in a pediatric cancer hospital and to identify the knowledge, attitude, and perception (KAP) of HCWs toward COVID-19 vaccination. A cross-sectional observational study was conducted between April to May 2021. A validated, confidential survey was employed to measure the mental health of HCWs and the KAP toward COVID-19 vaccines. The total responses were 395, of which 11.4% physicians, 18.5% pharmacists, and 70.1% were nurses. Sixty-six percent of HCWs had different degrees of anxiety and depression. Nurses significantly accounted for the highest anxiety levels (P = 0.003), while the cumulative anxiety score was significantly higher in HCWs who had a positive history of COVID-19 infection (P = 0.026). Although 67.6% of HCWs believe that “vaccines are essential for us,”, the vaccination rate was 21.3%. The Factors associated with not receiving the vaccine were younger ages (P = 0.014), nurses (P = 3.6987 × 10–7), negative history of COVID-19 infection (P = 0.043) and believing that infections can happen after taking the vaccine (P = 1.5833 × 10–7). Healthcare organizations must take serious intervention to decrease the mental load on HCWs and facilitate the vaccination process.
Subject terms: Psychology, Human behaviour
Introduction
Coronavirus disease 2019 (COVID-19) is a respiratory infectious disease that the World Health Organization (WHO) declared it as a pandemic during 20201. The causative virus; severe acute respiratory syndrome coronavirus 2 (SARS-CoV2) infected over two hundred million worldwide and resulted in more than four million deaths until September 20211,2. In Egypt, the cumulative number of the confirmed cases is 294,482, and 16,908 deaths due to COVID-19 in September 20212. The consistent increase of cases parallel with the rate of deaths causes an increase in the workload and the demand for healthcare workers (HCWs). In addition, the extensive media coverage, rumors and fake news, and controversial response regarding the available vaccines put extra pressure on HCWs. This altogether increases the burden of psychological diseases such as anxiety and depression3–5.
HCWs are the most exposed category to psychological dysfunctions6. Over history, infectious diseases’ outbreaks were associated with emotional distress and anxiety symptoms among HCWs. Moreover, anxiety, depression, and burnout were also reported in HCWs after the outbreaks were over7,8. Despite that, most HCWs do not receive training to provide mental health care9. As a result, the extreme pressure on HCWs during COVID-19 led them to suffer from psychological and mental problems5.
A systematic review was carried out to investigate the psychological impact of COVID-19 in HCWs in different countries. Eleven articles were included in the analysis and identified the prevalence of anxiety ranging from 24.1 to 44.6%. In addition, the prevalence of moderate to severe depression ranged from 12.1% to 50.4%.Severe degrees of symptoms were reported in frontline nurses, younger ages, and female workers5. In Egypt, a study conducted in 20 hospitals (502 HCWs) reported that 76.4% had an abnormality of anxiety scale, 67.7% had positive insomnia symptoms, and 77.2% showed symptoms of depression10.
The effect of the pandemic on HCWs mental health can vary individually or based on particular circumstances11. A cross-sectional study conducted in Egypt in May 2020 (540 HCWs) surveyed HCWs working in quarantine hospitals and found that adverse psychological symptoms were significantly predicted in younger ages HCWs, those who were not ready to work in quarantine hospitals, and HCWs who had insomnia12. Working with suspected or confirmed COVID-19 cases has been challenging for HCWs, resulting in negative psychological impact11. In addition, supporting oncology patients and maintaining their services during the pandemic is another huge challenge13.
Responding to the epidemic, hundreds of vaccines have gone through experimentation registered on ClinicalTrials.gov. Different technologies for the vaccines’ development were used, such as viral vectors vaccines, inactivated vaccines, RNA vaccines, and others. A systematic review that included 13 randomized clinical trials confirmed the efficacy and safety of several COVID-19 vaccines14. Several vaccines are now being administered globally. To date, all the data recommends the efficacy of COVID-19 vaccines in providing significant protection against COVID-19 infection. However, the long-term efficacy and safety are not yet established14.
There is controversy regarding taking the vaccine or not15. In a systematic review that estimated the vaccine acceptance rates in 33 countries reported the lowest acceptance rates in the Middle East, Africa, Russia, and many European countries. In addition, the acceptance of the vaccine among doctors and nurses ranged from 27.7 to 78.1% based on the country. Similarly, in a study conducted in Bangladesh, 60% of the participants said they plan to take the vaccine15. The hesitancy to take COVID-19 vaccines negatively affects the global efforts toward controlling the pandemic16.
A lower vaccination rate in any country can result in new variants that the current vaccines may fail to protect us. A study that analyzed 15 surveys on vaccine acceptance in lower- and middle-income countries found that the most common reason for vaccines refusal is side effects17. However, a national survey conducted among the United States citizens suggested that responders are influenced to take COVID-19 vaccines when they understand the expected benefits rather than the expected side effects18.
The degree of pandemic effect on mental status is now a global concern11. Moreover, HCWs' decision-making and physiological functioning rely on their psychological status to be assessed and addressed19. Few studies have been published that evaluated employees' mental health in working in healthcare facilities in Egypt, and the limited evidence regarding the acceptance of vaccination in the Egyptian population, especially HCWs. Thus, the aim of the present study is to evaluate the psychological condition of HCWs in a pediatric cancer hospital using validated scales and to explore the factors associated with psychological symptoms, such as sociodemographic data and occupation circumstances. Also, it aims to identify the knowledge, attitude, perception (KAP), and acceptance of HCWs toward COVID-19 vaccination.
Methods
Study design
A cross-sectional observational study (hospital-based survey) was conducted in Children’s Cancer Hospital 57,357 (CCHE), Cairo, Egypt.
Population and sample size
The target population was HCWs at CCHE. The inclusion criteria were licensed physicians, pharmacists, and nurses working at CCHE who completed the survey during the time of the data collection, while the exclusion criteria were HCWs who reported a positive history of depression, anxiety, or other previous phycological illness and HCWs who reported receiving medication for a psychological condition. The sample size was calculated using the sample-to-variable ratio method of 15:120,21. For the pilot and the main survey, at least 50 and 375 subjects were recommended, respectively. A minimum number was recommended for each profession as follows: for the pilot study: 8 pharmacists, 5 physicians, and 37 nurses were recommended, while for the main survey: 40 physicians, 59 pharmacists, and 276 nurses.
Data collection
The survey was distributed between April 2021 to May 2021 to all HCWs in two forms: paper-based or electronic. The duration of data collection was parallel to the arrival of COVID-19 vaccines in the country. An informed consent was written at the beginning of the study that stated the aim of the study, and the obtained anonymous data will be only used for the study. The agreement on the informed consent was accomplished by completing the survey.
Survey tools
A validated, confidential survey was conducted to obtain the data required for the study. Experts in the field assessed the face and content validity of the survey. A pilot study was conducted first to examine the feasibility of the study that is intended to be used on a larger scale ultimately. The survey consisted of three sections; the first section included demographic data, questions regarding the history of the infection, the history of working in COVID-19 unites, and the history of the psychiatric illness. The second section consisted of two validated scales; generalized anxiety disorder 7-item GAD-7 scale22 and patient health questionnaire PHQ-923 to assess anxiety and depression levels, respectively. The third section included general questions assessing the KAP toward COVID-19 vaccines. The questions were in (yes OR no) or multiple choices. The primary outcome was the extent of depression and anxiety. Other outcomes of interest were the factors associated with depression and anxiety and the acceptance of COVID-19 vaccination15.
Statistical analysis
The data were analyzed and graphed using Microsoft Excel® and IBM’s SPSS Statistics package (version 26). Descriptive statistics (frequency, percentages, mean, standard deviation) were performed for socio-demographics and the survey questions’ responses. The Chi-square test was used for categorical variables, while Mann–Whitney U test was used for continuous variables. A P value < 0.05 was considered to be statistically significant.
Ethical approval and consent to participate
The study was approved by the institutional review board in Children’s Cancer Hospital 57,357 (CCHE). The informed consent of participants was gained at the beginning of the survey.
Results
Sociodemographic characteristics of the study sample
A total of 415 HCWs participated in the survey. Of which, 20 responses were excluded due to positive history of psychiatric illness and/or receiving medication for a psychiatric condition. Thus, the included number for the analysis was 395 responses, of which 45 (11.4%) were physicians, 73 (18.5%) were pharmacists, and 277 (70.1%) were nurses. The corresponding response rate per profession was 50.36% for nurses, 48.67% for pharmacists, and 45% for physicians. Female participants accounted for 54.94%, and more than half of the participants lay between the age group 25–35 years (55.19%). In addition, approximately one-third had extra credentials after their bachelor’s degree. One hundred eighty-seven (47.3%) of the participants reported a positive history of COVID-19 infection, and 112 (28.4%) worked in a COVID-19 isolation unit. The sociodemographic and basic characteristics of the total included sample are illustrated in Table 1.
Table 1.
Sociodemographic data and basic characteristics of HCWs working at CCHE who responded to the survey.
| Characteristic | N (%) (Total N = 395) |
|---|---|
| Age (years) | |
| < 25 | 97 (24.56%) |
| 25–35 | 218 (55.19%) |
| 36–45 | 64 (16.20%) |
| > 45 | 16 (4.05%) |
| Gender | |
| Male | 178 (45.06%) |
| Female | 217 (54.94%) |
| Profession | |
| Physicians | 45 (11.4%) |
| Assistant consultant | 2 |
| Consultant | 12 |
| Fellowship | 2 |
| Resident | 14 |
| Specialist | 15 |
| Pharmacists | 73 (18.5%) |
| Ambulatory care | 4 |
| Dispensing pharmacist | 16 |
| IV/Admixture pharmacist | 10 |
| Ward pharmacist | 8 |
| Specialty pharmacist | 35 |
| Nurses | 277 (70.1%) |
| Charge nurse | 66 |
| Clinical instructor | 5 |
| Head nurse | 15 |
| Staff nurse | 191 |
| Extra credentials | |
| Yes | 134 (33.9%) |
| No | 261 (66.1%) |
| Years of Practicing the profession | |
| < 5 years | 170 (43.04%) |
| 5–9.9 years | 134 (33.92%) |
| 10–14.9 years | 56 (14.18%) |
| 15–19.9 years | 21 (5.32%) |
| ≥ 20 years | 14 (3.54%) |
| History of COVID-19 infection | |
| Yes | 187 (47.3%) |
| No | 208 (52.7%) |
| Endorsed history of working in a COVID-19 Unit | |
| Yes | 112 (28.4%) |
| No | 283 (71.6%) |
| Median working hours/day ± SD* | 12 ± 4.3 h |
*SD = standard deviation.
Anxiety assessment and associated factors
The anxiety level was estimated using the GAD-7 scale (the total score is 21). A score of (0–4) is considered minimal anxiety, (5–9) mild anxiety, (10–14) moderate anxiety, and (15–21) severe anxiety22. A considerable number of HCWs (261, 66.1%) had abnormal anxiety degrees on the scale mild to severe, 148 (37.5%) had mild anxiety, 76 (19.2%) had moderate anxiety, and 37 (9.4%) had severe anxiety. Non-statistical significance was observed when comparing age groups, gender, years of practice, positive history of COVID-19 infection, endorsed a history of working in a COVID-19 unit with the anxiety level and anxiety score. However, among different professions, nurses had the highest levels of anxiety in comparison to physicians and pharmacists, and it was statistically significant (P = 0.003) (Table 2). Also, the cumulative anxiety score was significantly higher in HCWs who had a positive history of COVID-19 infection (P = 0.026) (Table 3).
Table 2.
The level of anxiety among HCWs (using GAD-7 scale).
| Variable N (% within category) |
Minimal anxiety | Mild anxiety | Moderate anxiety | Severe anxiety | P-value |
|---|---|---|---|---|---|
| Total N = 395 | 134 (33.9%) | 148 (37.5%) | 76 (19.2%) | 37 (9.4%) | |
| Age | |||||
| < 25 | 40 (41.24%) | 27 (27.84%) | 17 (17.52%) | 13 (13.4%) | 0.120 |
| 25–35 | 69 (31.7%) | 88 (40.4%) | 46 (21%) | 15 (6.9%) | |
| 36–45 | 21 (32.8%) | 27 (42.2%) | 11 (17.2%) | 5 (7.8%) | |
| > 45 | 4 (25%) | 6 (37.5%) | 2 (12.5%) | 4 (25%) | |
| Gender | |||||
| Male | 64 (36%) | 69 (38.8%) | 29 (16.3%) | 16 (8.9%) | 0.562 |
| Female | 70 (32.3%) | 79 (36.4%) | 47 (21.7%) | 21 (9.6%) | |
| Profession | |||||
| Physicians | 7 (15.5%) | 25 (55.6%) | 12 (26.7%) | 1 (2.2%) | 0.003 |
| Pharmacists | 21 (28.8%) | 24 (32.9%) | 16 (21.9%) | 12 (16.4%) | |
| Nurses | 106 (38.3%) | 99 (35.7%) | 48 (17.3%) | 24 (8.7%) | |
| Years of practice | |||||
| < 5 years | 60 (35.3%) | 59 (34.7%) | 31 (18.2%) | 20 (11.8%) | 0.293 |
| 5 – 9.9 years | 47 (35.1%) | 51 (38.1%) | 29 (21.6%) | 7 (5.2%) | |
| 10 – 14.9 years | 12 (21.43%) | 27 (48.21%) | 12 (21.43%) | 5 (8.93%) | |
| 15 – 19.9 years | 9 (42.9%) | 8 (38.1%) | 2 (9.5%) | 2 (9.5%) | |
| ≥ 20 years | 6 (42.9%) | 3 (21.4%) | 2 (14.3%) | 3 (21.4%) | |
| History COVID-19 infection | |||||
| Yes | 55 (29.4%) | 75 (40.1%) | 39 (20.9%) | 18 (9.6%) | 0.348 |
| No | 79 (38%) | 73 (35.1%) | 37 (17.8%) | 19 (9.1%) | |
| History of working in a COVID-19 Unit | |||||
| Yes | 41 (36.6%) | 38 (33.9%) | 18 (16.1%) | 15 (13.4%) | 0.224 |
| No | 93 (32.8%) | 110 (38.9%) | 58 (20.5%) | 22 (7.8%) | |
Table 3.
The history of COVID-19 infection and anxiety score.
| History of COVID-19 infection | Anxiety score Mean ± SD* 95% CI* |
P-value |
|---|---|---|
| Positive History |
7.52 ± 4.85 (6.82–8.22) |
P = 0.026 |
| Negative History |
6.75 ± 4.89 (6.08–7.42) |
*SD = standard deviation, CI = confidence interval for the mean.
Significant values are in bold.
Depression assessment and associated factors
The level of depression was assessed using the PHQ-9 questionnaire (the total score is 27). The interpretation of the score is as follows: non-minimal (1–4), mild depression (5–9), moderate depression (10–14), moderately severe (15–19), and severe depression (20–27)23. Two hundred sixty-one HCWs (66%) had abnormal degrees of depression (mild to severe). Higher levels of depression were observed in HCWs who had a previous history of working in COVID-19 units or had COVID-19 infection. The depression level and score were not significant compared to all the factors Table 4.
Table 4.
The level of depression among HCWs (using PH-Q9 scale).
| Variable N (% within category) |
Non-minimal | Mild depression | Moderate depression | Moderately severe depression | Severe depression | P-value |
|---|---|---|---|---|---|---|
| Total N = 395 | 134 (33.9%) | 155 (39.2%) | 62 (15.7%) | 30 (7.6%) | 14 (3.5%) | |
| Age | ||||||
| < 25 | 31 (32%) | 38 (39.2%) | 14 (14.4%) | 11 (11.3%) | 3 (3.1%) | 0.903 |
| 25–35 | 74 (33.94%) | 89 (40.83%) | 32 (14.68%) | 16 (7.34%) | 7 (3.21%) | |
| 36–45 | 23 (35.94%) | 23 (35.94%) | 13 (20.3%) | 2 (3.13%) | 3 (4.69%) | |
| > 45 | 6 (37.5%) | 5 (31.25%) | 3 (18.75%) | 1 (6.25%) | 1 (6.25%) | |
| Gender | ||||||
| Male | 62 (34.8%) | 71 (39.9%) | 29 (16.3%) | 10 (5.6%) | 6 (3.4%) | 0.758 |
| Female | 72 (33.2%) | 84 (38.7%) | 33 (15.2%) | 20 (9.2%) | 8 (3.7%) | |
| Profession | ||||||
| Physicians | 14 (31.1%) | 21 (46.7%) | 6 (13.3%) | 3 (6.7%) | 1 (2.2%) | 0.740 |
| Pharmacists | 22 (30.14%) | 31 (42.46%) | 10 (13.7%) | 5 (6.85%) | 5 (6.85%) | |
| Nurses | 98 (35.4% | 103 (37.2%) | 46 (16.6%) | 22 (7.9%) | 8 (2.9%) | |
| Years of practice | ||||||
| < 5 years | 52 (30.6%) | 68 (40%) | 27 (15.9%) | 18 (10.6%) | 5 (2.9%) | 0.58 |
| 5–9.9 years | 54 (40.3%) | 49 (36.6%) | 18 (13.4%) | 8 (6%) | 5 (3.7%) | |
| 10–14.9 years | 13 (23.2%) | 25 (44.6%) | 13 (23.2%) | 3 (5.4%) | 2 (3.6%) | |
| 15–19.9 years | 9 (42.86%) | 9 (42.86%) | 2 (9.52%) | 0 (0%) | 1 (4.76%) | |
| ≥ 20 years | 6 (42.9%) | 4 (28.6%) | 2 (14.3%) | 1 (7.1%) | 1 (7.1%) | |
| History COVID-19 infection | ||||||
| Yes | 56 (29.9%) | 71 (38%) | 34 (18.2%) | 18 (9.6%) | 8 (4.3%) | 0.225 |
| No | 78 (37.5%) | 84 (40.38%) | 28 (13.46%) | 12 (5.77%) | 6 (2.89%) | |
| History of working in a COVID-19 Unit | ||||||
| Yes | 35 (31.25%) | 42 (37.5%) | 20 (17.85%) | 9 (8.04%) | 6 (5.36%) | 0.662 |
| No | 99 (34.98%) | 113 (39.93%) | 42 (14.84%) | 21 (7.42%) | 8 (2.83%) | |
Knowledge, attitude, and perception about COVID-19 vaccines
The responses to the KAP assessment section are shown in Table 5. The participants were asked if they knew about the vaccine efficacy and safety; 80% and 83.3% answered yes, respectively. For the knowledge item, the comparison of the responses between professions was statistically significant regarding knowing that the infection can happen after taking the vaccine (P = 7.018 × 10–9). In addition, 67.6% believe that the vaccines are essential for us, while only 21.3% received at least one dose of a COVID-19 vaccine (P = 3.6987 × 10–7).
Table 5.
KAP assessment response for each profession.
| Item | Total (n = 395) |
Physicians (n = 45) |
Pharmacists (n = 73) |
Nurses (n = 277) |
P value |
|---|---|---|---|---|---|
| Item.1: Knowledge | |||||
| Do you know about the effectiveness of COVID-19 vaccines? | |||||
| Yes | 316 (80%) | 41 (91.1%) | 61 (83.6%) | 214 (77.3%) | 0.069 |
| No | 79 (20%) | 4 (8.9%) | 12 (16.4%) | 63 (22.7%) | |
| Do you know about the side effects of COVID-19 vaccines? | |||||
| Yes | 329 (83.3%) | 41 (91.1%) | 61 (83.6%) | 227 (81.9%) | 0.31 |
| No | 66 (16.7%) | 4 (8.9%) | 12 (16.4%) | 50 (18.1%) | |
| Can COVID-19 infection happen after taking the vaccine? | |||||
| Yes | 272 (68.9%) | 38 (84.4%) | 68 (93.2%) | 166 (59.9%) | 7.018 × 10–9 |
| No | 36 (9.1%) | 4 (8.9%) | 0 (0%) | 32 (11.6%) | |
| I don’t know | 87 (22%) | 3 (6.7%) | 5 (6.8%) | 79 (28.5%) | |
| Who should have been vaccinated? | |||||
| Those who have not yet been infected with COVID-19 | 28 (7.1%) | 1 (2.2%) | 2 (2.7%) | 25 (9%) | 0.31 |
| People infected with COVID-19 | 8 (2%) | 1 (2.2%) | 2 (2.7%) | 5 (1.8%) | |
| Elderly and patients with chronic diseases | 70 (17.7%) | 10 (22.2%) | 10 (13.7%) | 50 (18.1%) | |
| Everyone | 289 (73.2%) | 33 (73.3%) | 59 (80.8%) | 197 (71.1%) | |
| Item.2: Attitude | |||||
| The COVID-19 vaccines are essential for us | |||||
| Yes | 267 (67.6%) | 30 (66.7%) | 55 (75.3%) | 182 (65.7%) | 0.07 |
| No | 44 (11.1%) | 1 (2.2%) | 6 (8.2%) | 37 (13.4%) | |
| I don’t know | 84 (21.3%) | 14 (31.1%) | 12 (16.4%) | 58 (20.9%) | |
| I received at least one dose of a COVID-19 vaccine | |||||
| Yes | 84 (21.3%) | 21 (46.7%) | 23 (31.5%) | 40 (14.4%) | 3.6987 × 10–7 |
| No | 311 (78.7%) | 24 (53.3%) | 50 (68.5%) | 237 (85.6%) | |
| I will encourage my family/friends / relatives to get vaccinated | |||||
| Yes | 248 (62.8%) | 32 (71.1%) | 46 (63%) | 170 (61.4%) | 0.014 |
| No | 58 (14.7%) | 0 (0%) | 16 (21.9%) | 42 (15.2%) | |
| I don’t know | 89 (22.5%) | 13 (28.9%) | 11 (15.1%) | 65 (23.5%) | |
| Item.3: Perception | |||||
| Do you think that if everyone in society maintains the preventive measures, the COVID-19 pandemic can be eradicated without vaccination? | |||||
| Yes | 98 (24.8%) | 9 (20%) | 28 (38.4%) | 61 (22%) | 0.025 |
| No | 204 (51.6%) | 26 (57.8%) | 35 (47.9%) | 143 (51.6%) | |
| I don’t know | 93 (23.5%) | 10 (22.2%) | 10 (13.7%) | 73 (26.4%) | |
| What might convince you to take a COVID-19 vaccine OR convinced you if you already took it? (Choose all that apply) | |||||
| The people I know get the vaccine without issues | 119 (30.1%) | 14 (31.1%) | 23 (31.5%) | 82 (29.6%) | 0.94 |
| Getting the vaccine meant I would no longer have to wear a mask or social distance | 60 (15.1%) | 6 (13.3%) | 12 (16.4%) | 42 (15.2%) | 0.901 |
| Getting the vaccine can protect me from getting the infection | 232 (58.7%) | 33 (73.3%) | 31 (42.5%) | 168 (60.6%) | 0.002 |
| It is required for international travel | 127 (32.2%) | 19 (42.2%) | 27 (37%) | 81 (29.2%) | 0.139 |
| Nothing—I don’t believe vaccines are safe | 47 (12%) | 1 (2.2%) | 11 (15.1%) | 35 (12.6%) | 0.088 |
| Other reason | 28 (7.1%) | 5 (11.1%) | 14 (19.2%) | 9 (3.2%) | 0.000008 |
Significant values are in bold.
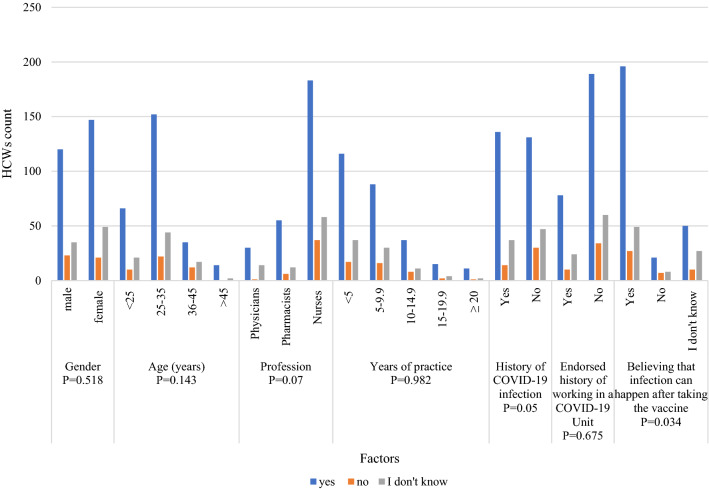
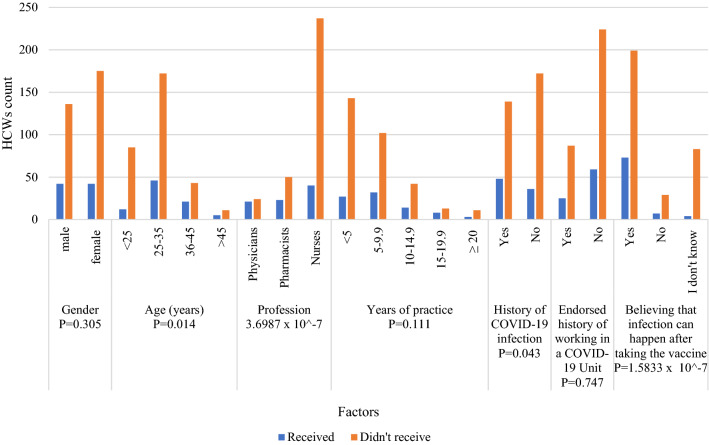
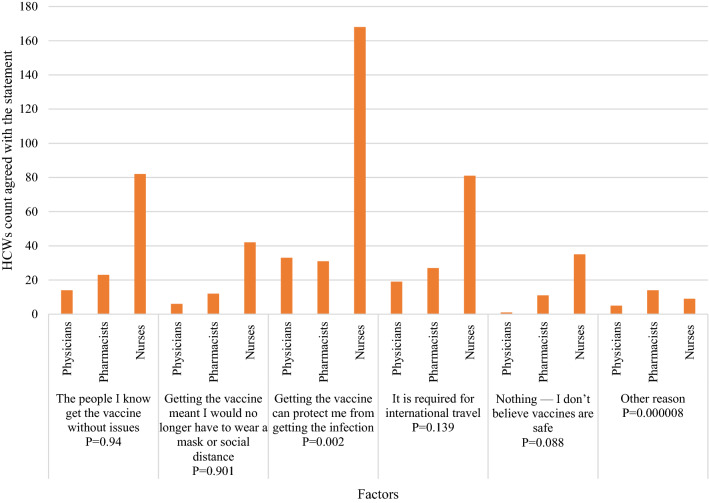
The vaccine acceptance was compared with several factors (Fig. 1). Nurses were significantly the most category through different professions who believe vaccines are essential for us (P = 0.07). Also, HCWs who agreed that vaccines are essential significantly believe that the infection can happen after taking the vaccine (P = 0.034). Furthermore, some factors significantly influenced the decision to receive at least one dose of COVID-19 vaccine, including the age between 25 and 35 years (P = 0.014), being a nurse (P = 3.6987 × 10–7), not having a history of COVID-19 infection (P = 0.043) and believing that the infection can happen after taking the vaccine (P = 7.018 × 10–9) (Fig. 2). In addition, pharmacists were the least HCWs convinced by the statement “Getting the vaccine can protect me from getting the infection” (P = 0.002) (Fig. 3).
Figure 1.
Factors affecting vaccination acceptance among HCWs.
Figure 2.
Factors affecting receiving at least one dose of a COVID-19 vaccine among HCWs.
Figure 3.
HCWs responses to “What might convince you to take a COVID-19 vaccine OR convinced you if you already took it? (Choose all that apply).
Discussion
Remarkable results from the current study have shown that more than half of HCWs (66%) who worked during the COVID-19 pandemic suffer from abnormal anxiety and depression symptoms. Those findings are consistent with published data during the pandemic inside and outside Egypt4,5,12. An online survey conducted during the first wave of the COVID-19 pandemic revealed that 40% of the participated HCWs had clinically significant emotional disorders. The results are also supported by a systematic review and meta-analysis that reported high prevalence rates for anxiety, depression, post-traumatic stress disorder, and distress 40%, 37%, 49%, and 37%, respectively11. High rates of fear, anxiety and abnormal psychological symptoms were expected and are known consequences of global pandemics24. During COVID-19, HCWs are predisposed to numerous factors that highly impact their mental health. Such factors include excessive workload, facing deaths daily, fear of getting the infection or transmitting it to their families, shortage of protective equipment, and lack of effective social support6,25. On top of that, the estimated mortality rate among oncology patients infected with COVID-19 was 20% due to weak immunity and postponing their cancer treatment regimens26. Hence, high anxiety and depression levels in our study could also be attributed to the fact that facing oncology patients is associated with additional distress27.
A highlighted finding embedded in the data is the significantly higher level of anxiety among nurses in comparison to physicians and pharmacists; (mild: nurses 99, physicians 25, pharmacists 24), (moderate: nurses 48, physicians 12, pharmacists 16), (severe: nurses 24, physicians 1, pharmacists 12), (P = 0.003). Nurses are the largest occupational staff in our facility, and they account for approximately 69% of the total healthcare task force. In addition, as per the World Health Organization (WHO) report, nurses and midwives comprise more than 50% of HCWs in many countries28. Moreover, they are considered the first and the direct line who interact consistently with patients29.
During COVID-19, severe degrees of psychological symptoms were reported in nursers rather than in other professions5. A cross-sectional study in the Philippines reported 37% (n = 325) of abnormal anxiety symptoms among frontline nurses. Interestingly, anxiety levels were lower in those with high levels of personal resilience and who received social and organizational support30. Another study found that nurses experienced higher levels of distress during previous SARS outbreaks. Suggested causes were fear for their health state, social isolation, and job workload29. Nurses account for the majority of the healthcare workforce worldwide. More importantly, HCWs who work long shifts, particularly nurses, are prone to sickness and absence31,32 In turn, it is essential to address the causes of their mental disorders and to provide efficient mental health support to them32.
Although our results indicated the lack of association between sociodemographics and the level of anxiety or depression, Alnazly et al. identified several factors positively correlated to psychological distress among HCWs. The determining factors were being male, older ages (above 40 years old), direct interaction with positive COVID-19 patients, and extended professional experience33. In contrast, Youssef et al. indicated that female HCWs and younger ages are more predisposed to adverse psychological symptoms12. We also reported another crucial finding: HCWs with a previous history of a positive COVID-19 infection expressed higher anxiety scores. Psychiatric comorbidities were previously reported consequence in COVID-19 survivors, as anxiety and depression likely happen in 42% and 31% of survivors, respectively34. In context, regardless of the differential factors that prone HCWs to significant psychological symptoms, they suffer from anxiety and depressive symptoms that need direct support and management.
Our findings point to the importance of psychological care and support that is urgent and required for all HCWs to decrease the levels of psychological distress. Several actions can be considered, such as emotional support programs provided by government and healthcare facilities35,36, encouragement of relaxation techniques such as yoga and meditation37, offering therapist’s visits when needed38. Additionally, shortening the working hours of39, consistently checking the staff who have burnout and need support (41), and conducting educational and training programs about mental health can also improve HCWs’ mental health status40. It is worth mentioning the successful prophylactic model “CREAT” implemented in Princess Margaret Cancer Centre, one of the world's largest cancer tertiary teaching hospitals. The program was implemented during the first wave of the COVID-19 pandemic (March 2020s) and targeted to provide support for oncology HCWs. It consisted of psychosocial coaches' support given to frontline HCWs to prevent burnout and emotional distress during the pandemic. The model included several interventions such as identifying HCWs' emotional needs, providing calming techniques, and providing online mental health support. The implementation of the such program led to a reduction in distress levels and an increase in team resilience27.
Adequate levels of knowledge, attitude, and perception toward COVID-19 vaccines were reported among HCWs. Our findings showed that the efficacy and safety of COVID-19 vaccines are well-recognized among HCWs (80%, 83.3%), respectively. Also, they have sufficient knowledge about COVID-19 vaccines, as reflected by the 68.9% who agreed that COVID-19 infection could happen after taking the vaccine and 73.2% who agreed that everyone should be vaccinated. Similar results were observed in a study conducted in three hospitals in Uganda in which 83.9% of the participants had good knowledge about COVID-19 vaccines41. Furthermore, HCWs in our facility reported that they do not believe that if everyone in society maintains the preventive measures, the COVID-19 pandemic can be eradicated without vaccination (P = 0.025). The knowledge level was expected to be high among HCWs giving reasons for their occupation and experience.
In different nations, vaccines still face doubt and rejection. The Centre of Disease Control and Prevention (CDC) reported that in the 2018–2019 flu season, only 45% of adults received a flu vaccination. In addition, about 35.8% of adults refuse to take the flu vaccine18. The vaccination acceptance rate in our study against COVID-19 was 67.6%. Closer rates were reported earlier in other studies on the general population (a global survey), HCWs, or both (71.5%, 64.9%, 60.6%), respectively42–44. Despite that, the percentage of HCWs who received at least one dose of a COVID-19 vaccine was only 21.3%. The difference between the acceptance percentage and the actual percentage of HCWs received the vaccine may be due to the limited vaccine availability at the survey time in Egypt.
Unexpectedly, nurses were the most profession who believed in COVID-19 vaccines, however, they were the least vaccinated group (P = 3.6987 × 10–7). An earlier study reported that medical doctors were more likely to accept the vaccine, but that was not statistically different among other professions44. Also, the educational level was insignificantly correlated with vaccine acceptance among Arabs45. Nurses in our institution lay within a wide age range, educational, and experience levels. Such diversity could contribute to the controversial result. Another factor significantly associated with a lower vaccination rate is believing that the infection can happen even after taking the vaccine and the lack of COVID-19 infection history (P = 1.5833 × 10–7), (P = 0.043), respectively. Such beliefs are actual even among HCWs, although all the available vaccines significantly protect from getting the infection and prevent hospitalization due to the infection14. Lastly, younger ages (< 25 and 25–35 years old) were the least vaccinated group (65%), which contradicts earlier findings reported by Elharake JA et al. in Saudi Arabia. In the later study, younger ages were more likely to accept the vaccines (49.2%), giving the reason for the extreme restrictions employed by Saudi authorities among their population aiming to control the pandemic43. However, fewer restrictions were employed in Egypt, which may lead younger HCWs to be less encouraged to take the vaccines.
Interestingly, 58.7% of our study sample agreed on taking the vaccine because it can protect them from getting the infection, 62.8% agreed on encouraging their relatives and friends to take the vaccine, while 12% refused to take it because they believe vaccines are not safe. In different countries, one of the major factors that potentially affect the decision to take the vaccines are side effects. A study conducted in the United States by Kreps et al. found that the vaccine acceptance rate is positively affected when the efficacy is higher, and the rate is reduced when the side effects are severe. Furthermore, a lower incidence of major side effects was associated with significantly higher acceptance rates46. Similarly, the most common reason for COVID-19 vaccine refusal among HCWs in Saudi Arabia was fear of side effects (59%)43. Those numbers indicate that HCWs can be encouraged to take the vaccines for their protection and control the pandemic for society. Also, raising the knowledge of the benefits of vaccines will likely increase the acceptance among HCWs. Concisely, better vaccination rates will be influenced by a better understating of the vaccine's benefits with facilitating the vaccination process.
We are aware that our research may have some limitations, given that the suggestive bias due to self-reporting of the assessment tools can result in some sources of error. Also, the nature of the cross-sectional study design as causality cannot be established as well as the single-centered model. Nevertheless, our study provided an overview of HCWs’ mental health in the middle of the pandemic. It also stratified the findings based on the profession that in turn, reported crucial results and summarized the factors that significantly impact the COVID-19 vaccination rate. Lastly, it offers an example of assessing and surveying HCWs in an organization and utilizing the results as a baseline for mental health educational programs.
Conclusion
Our study was conducted during the COVID-19 pandemic, parallel with the emergence of COVID-19 vaccines. Approximately 66% of the study sample suffered from different anxiety and depressive symptoms. Increased anxiety levels were reported in nurses and those with a history of COVID-19 infection. In addition, despite the poor vaccination rate, sufficient knowledge, positive attitude, and perception toward COVID-19 vaccines were reported. Government and healthcare organizations must take serious interventions to decrease the mental load on HCWs. Also, to prioritize and facilitate the vaccination process for HCWs.
Acknowledgements
None.
Author contributions
All the authors participated equally in the conception and design of the work, drafting the work and revising it critically, data analysis, final approval of the version to be published, and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mishra SK, Tripathi T. One year update on the COVID-19 pandemic: Where are we now? Acta Trop. 2021;214:105778. doi: 10.1016/j.actatropica.2020.105778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. WHO Coronavirus (COVID-19) Dashboard. https://covid19.who.int/ (2021).
- 3.Rajkumar RP. COVID-19 and mental health: A review of the existing literature. Asian J. Psychiatry. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Young KP, et al. Health care workers’ mental health and quality of life during COVID-19: Results from a mid-pandemic, National Survey. Psychiatr. Serv. 2021;72:122–128. doi: 10.1176/appi.ps.202000424. [DOI] [PubMed] [Google Scholar]
- 5.Vizheh M, et al. The mental health of healthcare workers in the COVID-19 pandemic: A systematic review. J. Diabetes Metab. Disord. 2020;19:1967–1978. doi: 10.1007/s40200-020-00643-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Di Tella M, Romeo A, Benfante A, Castelli L. Mental health of healthcare workers during the COVID-19 pandemic in Italy. J. Eval. Clin. Pract. 2020;26:1583–1587. doi: 10.1111/jep.13444. [DOI] [PubMed] [Google Scholar]
- 7.Lee SM, Kang WS, Cho A-R, Kim T, Park JK. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr. Psychiatry. 2018;87:123–127. doi: 10.1016/j.comppsych.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chong M-Y, et al. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br. J. Psychiatry. 2004;185:127–133. doi: 10.1192/bjp.185.2.127. [DOI] [PubMed] [Google Scholar]
- 9.Lima CKT, et al. The emotional impact of Coronavirus 2019-nCoV (new Coronavirus disease) Psychiatry Res. 2020;287:112915. doi: 10.1016/j.psychres.2020.112915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elkholy H, et al. Mental health of frontline healthcare workers exposed to COVID-19 in Egypt: A call for action. Int. J. Soc. Psychiatry. 2020 doi: 10.1177/0020764020960192. [DOI] [PubMed] [Google Scholar]
- 11.Saragih ID, et al. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2021;121:104002. doi: 10.1016/j.ijnurstu.2021.104002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Youssef N, Mostafa A, Ezzat R, Yosef M, ElKassas M. Mental health status of health-care professionals working in quarantine and non-quarantine egyptian hospitals during the covid-19 pandemic. East. Mediterr. Heal. J. 2020;26:1155–1164. doi: 10.26719/emhj.20.116. [DOI] [PubMed] [Google Scholar]
- 13.Datta SS, Mukherjee A, Ghose S, Bhattacharya S, Gyawali B. Addressing the mental health challenges of cancer care workers in LMICS during the time of the COVID-19 pandemic. JCO Glob. Oncol. 2020 doi: 10.1200/GO.20.00470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kai X, et al. Efficacy and safety of COVID-19 vaccines: A systematic review. Chinese J. Contemp. Pediatr. 2021;23:221–228. doi: 10.7499/j.issn.1008-8830.2101133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Islam M, et al. Knowledge, attitudes and perceptions towards COVID-19 vaccinations: a cross-sectional community survey in Bangladesh. medRxiv. 2021;21:1–11. doi: 10.1186/s12889-021-11880-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sallam M. Covid-19 vaccine hesitancy worldwide: A concise systematic review of vaccine acceptance rates. Vaccines. 2021;9:1–15. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Solís Arce JS, et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat. Med. 2021;27:1385–1394. doi: 10.1038/s41591-021-01454-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaplan RM, Milstein A. Influence of a COVID-19 vaccine’s effectiveness and safety profile on vaccination acceptance. Proc. Natl. Acad. Sci. 2021;118(10):e2021726118. doi: 10.1073/pnas.2021726118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heath C, Sommerfield A, von Ungern-Sternberg BS. Resilience strategies to manage psychological distress among healthcare workers during the COVID-19 pandemic: A narrative review. Anaesthesia. 2020;75:1364–1371. doi: 10.1111/anae.15180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Memon MA, et al. Sample size for survey research: Review and recommendations. J. Appl. Struct. Equ. Model. 2020;4:i–xx. [Google Scholar]
- 21.Memon MA, Ting H, Ramayah T, Chuah F, Cheah J-H. A Review of the methodological misconceptions and guidelines related to the application of structural equation modeling: A Malaysian scenario. J. Appl. Struct. Equ. Model. 2017;1:1–3. [Google Scholar]
- 22.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 23.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shah K, et al. Focus on mental health during the coronavirus (COVID-19) pandemic: Applying learnings from the past outbreaks. Cureus. 2020;12:e7405. doi: 10.7759/cureus.7405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ji D, et al. Prevalence of psychological symptoms among Ebola survivors and healthcare workers during the 2014–2015 Ebola outbreak in Sierra Leone: A cross-sectional study [Prevalencia de síntomas psicológicos entre los supervivientes del ébola y los trabajadores sani. Oncotarget. 2017;8:12784–12791. doi: 10.18632/oncotarget.14498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wise J. Covid-19: Cancer mortality could rise at least 20% because of pandemic, study finds. BMJ. 2020;369:m1735. doi: 10.1136/bmj.m1735. [DOI] [PubMed] [Google Scholar]
- 27.Shapiro GK, et al. An institutional model for health care workers’ mental health during Covid-19. NEJM Catal. 2021 doi: 10.1056/CAT.20.0684. [DOI] [Google Scholar]
- 28.World Health Organization. Nursing personnel (number). https://www.who.int/data/gho/data/indicators/indicator-details/GHO/nursing-personnel-(number) (2018).
- 29.Maunder RG, Lancee WJ, Rourke S, Hunter JJ, Goldbloom D, Balderson K, Petryshen P, Steinberg R, Wasylenki D, Koh D, Fones CS. Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in Toronto. Psychosom. Med. 2004;66:938–942. doi: 10.1097/01.psy.0000145673.84698.18. [DOI] [PubMed] [Google Scholar]
- 30.Labrague LJ, De los Santos JAA. COVID-19 anxiety among front-line nurses: Predictive role of organisational support, personal resilience and social support. J. Nurs. Manag. 2020;28:1653–1661. doi: 10.1111/jonm.13121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dall’Ora C, et al. Are long nursing shifts on hospital wards associated with sickness absence? A longitudinal retrospective observational study. J. Nurs. Manag. 2019;27:19–26. doi: 10.1111/jonm.12643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sampaio F, Sequeira C, Teixeira L. Nurses’ mental health during the COVID-19 outbreak: A cross-sectional study. J. Occup. Environ. Med. 2020;62:783–787. doi: 10.1097/JOM.0000000000001987. [DOI] [PubMed] [Google Scholar]
- 33.Alnazly E, Khraisat OM, Al-Bashaireh AM, Bryant CL. Anxiety, depression, stress, fear and social support during COVID-19 pandemic among Jordanian healthcare workers. PLoS ONE. 2021;16:e0247679. doi: 10.1371/journal.pone.0247679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gennaro M, Lorenzo RD, Conte C, Poletti S. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Elsevier Journal, Brain Behav Immun. 2020;89:594–596. doi: 10.1016/j.bbi.2020.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. 2020;323:2133–2134. doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- 36.Zhang J, Wu W, Zhao X, Zhang W. Recommended psychological crisis intervention response to the 2019 novel coronavirus pneumonia outbreak in China: A model of West China Hospital. Precis. Clin. Med. 2020;3:3–8. doi: 10.1093/pcmedi/pbaa006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Patel RS, Bachu R, Adikey A, Malik M, Shah M. Factors related to physician burnout and its consequences: A review. Behav. Sci. 2018;8:98. doi: 10.3390/bs8110098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xiao H, Zhang Y, Kong D, Li S, Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019(COVID-19) in January and February 2020 in China. Med. Sci. Monit. 2020;26:1–8. doi: 10.12659/MSM.923549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu Y, et al. Emergency management of nursing human resources and supplies to respond to coronavirus disease 2019 epidemic. Int. J. Nurs. Sci. 2020;7:135–138. doi: 10.1016/j.ijnss.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jiang X, et al. Psychological crisis intervention during the outbreak period of new coronavirus pneumonia from experience in Shanghai. Psychiatry Res. 2020;286:112903. doi: 10.1016/j.psychres.2020.112903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kamacooko O, et al. Knowledge, attitudes, and practices regarding covid-19 among healthcare workers in Uganda: A cross-sectional survey. Int. J. Environ. Res. Public Health. 2021;18:1–12. doi: 10.3390/ijerph18137004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lazarus JV, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021;27:225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Elharake JA, et al. COVID-19 vaccine acceptance among health care workers in the Kingdom of Saudi Arabia. Int. J. Infect. Dis. 2021;109:286–293. doi: 10.1016/j.ijid.2021.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Elhadi M, et al. Knowledge, attitude, and acceptance of healthcare workers and the public regarding the COVID-19 vaccine: A cross-sectional study. BMC Public Health. 2021;21:1–21. doi: 10.1186/s12889-021-10987-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kaadan MI, Abdulkarim J, Chaar M, Zayegh O, Keblawi MA. Determinants of COVID-19 vaccine acceptance in the Arab world: A cross-sectional study. Glob. Heal. Res. Policy. 2021;6:1–17. doi: 10.1186/s41256-021-00202-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kreps S, et al. Factors associated With US adults’ likelihood of accepting COVID-19 vaccination. JAMA Netw. Open. 2020;3:e2025594–e2025594. doi: 10.1001/jamanetworkopen.2020.25594. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.