Abstract
We conducted a narrative review to assess the use and effectiveness of breathing techniques for pain control as the only non-pharmacological resource during labor and childbirth. A search was conducted using PubMed, PEDro, SciELO, and Scopus with publications between January 2005 and September 2021 in English, Portuguese, or Spanish. Seven publications were selected. Most of the articles reported on the use of slow and deep breathing during contractions in the first stage of labor and breathing associated with pushing-down efforts in the second stage. The information regarding the moment when guidance on the use of the techniques was provided varied across studies. According to the reviewed papers, breathing techniques offer benefits for women in labor without adverse effects on newborns.
Keywords: breathing exercises, labor, pain, childbirth, antenatal education
INTRODUCTION
The progress in obstetric care has rendered safer childbirth for both the mother and the baby. In many settings, the focus of care is not only a favorable outcome but also a positive childbirth experience for women, their partners, and the newborn. Labor and childbirth, important events in a woman’s life, still, in many settings, continue to be one of the major concerns regarding fear of pain and how to cope with it. Fear of pain during labor was one of the main reasons reported by pregnant women for requesting an elective cesarean (Faisal et al., 2014) and has been associated with some obstetric outcomes such as increased instrumental births and an increase in the number of cesarean surgeries (Handelzalts et al., 2015).
Pharmacological and non-pharmacological approaches have been developed to help women cope with pain during labor and delivery. The non-pharmacological approaches are based on the transmission of knowledge on existing techniques to reduce pain, stress, and fear of childbirth and improve wellbeing. These techniques do not require sophisticated technology and can be performed by the woman herself during labor and delivery without the need for assistance from health care professionals (Chaillet et al., 2014).
It has been recommended that pregnant women receive information on how to manage pain and be in control during birthing and on how their physical conditioning and the use of non-pharmacological techniques will benefit them during pregnancy, labor, and delivery. The World Health Organization (WHO) recommends that pregnant women receive information and guidance on relaxation techniques and non-pharmacologic techniques, including breathing techniques (World Health Organization, 2018), provided by trained health care professionals at various moments during antenatal care and labor (Gayeski & Brüggemann, 2010).
There are still controversies regarding the effectiveness of non-pharmacological approaches for pain management during labor and the improvement in women’s well-being and satisfaction during childbirth. Data on the use of non-pharmacological methods during labor and the associated obstetric outcomes remains scarce, and only a small number of publications on the subject involve clear methodology regarding the evaluation of the efficacy of these techniques (Chaillet et al., 2014). Within non-pharmacological techniques, breathing techniques constitute a simple resource that pregnant women can use during labor to control pain and improve well-being during childbirth, with no adverse effects on the newborn (Michaels, 2010). Furthermore, it has been reported that no differences were found between those women who used breathing techniques and those who did not regarding the vitality of the newborn infant valuated according to the Apgar score (Gadade & Podder, 2015; Gayeski & Brüggemann, 2010), with a relative risk (RR) of 1.04; 95% confidence interval (95%CI) 0.96–1.12 and in a sensitivity analysis, aRR of 1.05; 95%CI 0.95–1.16 (Boaviagem et al., 2017). Controlled breathing helps women in labor to be more aware, more attentive, and more focused on managing labor and childbirth (Lothian, 2011). In addition, the use of breathing in combination with other non-pharmacological techniques may improve women’s satisfaction (Bonapace et al., 2013; Heim et al., 2019; Yildirim & Sahin, 2004), reduce pain (Bonapace et al., 2013; Miquelutti et al., 2013, 2015) and decrease the duration of labor (Bonapace et al., 2013).
Breathing techniques represent a low-cost, non-pharmacological resource that can be used by women to control pain and anxiety and improve wellbeing during labor and childbirth. A review of the data available on these techniques is important for healthcare providers providing obstetric care. Therefore, the objective of our study was to conduct a narrative review of studies involving the effectiveness of breathing techniques for the management of pain during labor, as well as the benefits and limitations of these techniques, and the ideal moment at which to provide pregnant women with information on this non-pharmacologic resource.
Breathing techniques represent a low-cost, non-pharmacological resource that can be used by women to control pain and anxiety and improve wellbeing during labor and childbirth.
MATERIAL AND METHODS
We conducted a narrative review of the available literature on the use of breathing techniques during labor. Due to the scarce number of publications, together with the diversity of interventions and the different scenarios during labor that posed a barrier to the possibility of a systematic review, we opted to conduct a narrative review based on systematic methodologies and bibliographic research strategy (Collins & Fauser, 2005).
Search
Publications for inclusion were selected from five databases: PubMed, Scopus, PEDro, and SciELO, among those published between January 2005 and September 2021 in English, Portuguese, or Spanish. Different terms were used to expand, and narrow searches; the keywords used were: “breathing exercises” OR “breathing techniques” AND “labor.” In SciELO, as permitted, the keywords used in Portuguese were “respiração” AND “trabalho de parto,” and in Spanish “trabajo de parto” AND “respiración.”
The inclusion criteria were: Articles based on studies conducted with pregnant women who used breathing techniques as the main non-pharmacological technique during labor, which reported information on the evaluation of the intervention with breathing techniques through randomized clinical trials (RCT), non-RCT, and observational studies involving a control group. Since the use of relaxation techniques is frequently associated with the use of breathing techniques, studies that reported relaxation associated with breathing techniques were also considered for this review. Studies in which the intervention group used only breathing techniques and the control group used any other non-pharmacological technique were also included. Studies that reported on the use of breathing techniques in conjunction with other non-pharmacological techniques in the intervention group were excluded.
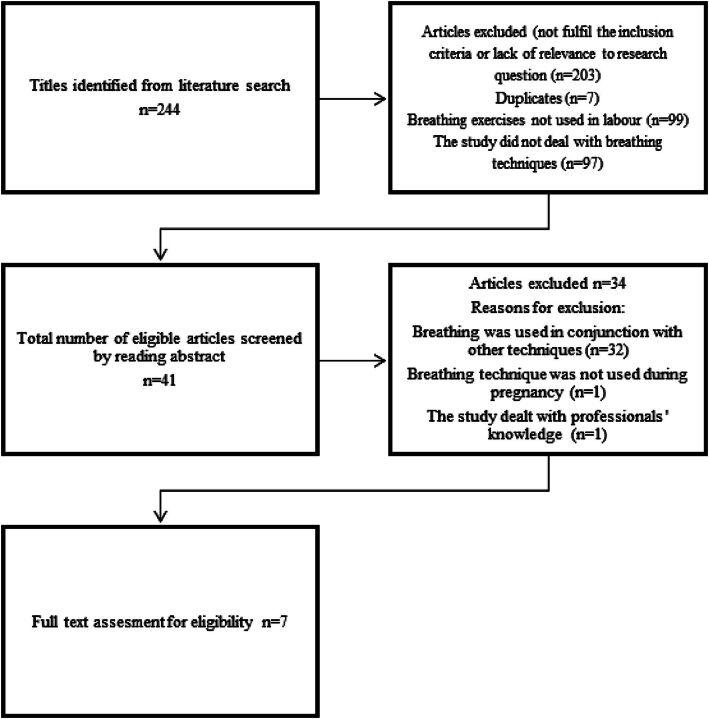
Initially, articles identified in the databases consulted were selected based on the titles that referred to non-pharmacological techniques, labor pain, childbirth, and antenatal education. Secondly, the abstracts of the selected articles were analyzed to identify if the main intervention had been breathing techniques, if the use of the birthing technique had been evaluated, and the other selection criteria. Seven articles were selected for the narrative review (Figure 1).
Figure 1. Literature selection process for review.
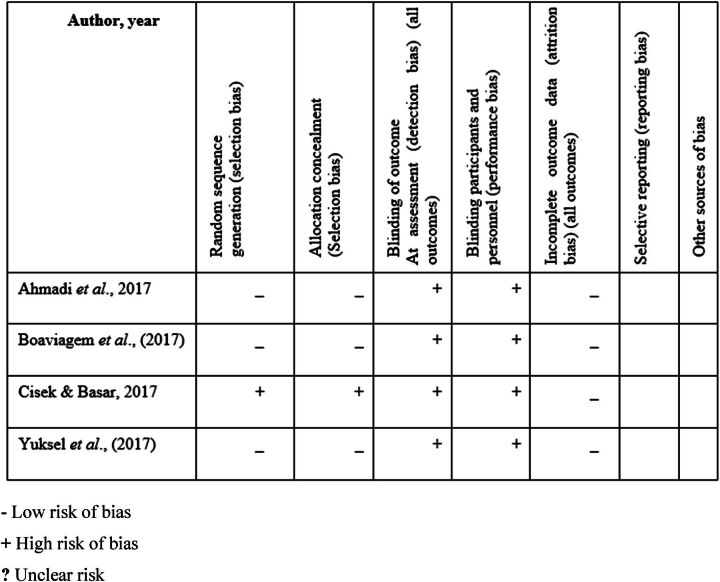
The analysis of the articles was performed by each author separately; extracts of the data were compared, and based on common agreement, articles were included in the narrative review. The main data considered were: Author, year of publication, inclusion criteria, when the guidance on breathing techniques was provided, description of breathing techniques used, how the evaluation was conducted, and the main results presented. An assessment of the risk of bias of the RCTs was performed (Figure 2).
Figure 2. Assessment of risk of bias of RCTs.
RESULTS
Of the seven articles selected, three were from Brazil (Almeida et al., 2005; Boaviagem et al., 2017; Lemos et al., 2011;), two were from Turkey (Cicek & Basar, 2017; Yuksel et al., 2017) and two from Iran (Ahmadi et al., 2017; Kamalifard et al., 2012). Except for one of the articles that was published in Portuguese (Almeida et al., 2005), all the others were published in English. Four articles presented findings from randomized controlled trials to evaluate the interventions (Ahmadi et al., 2017; Boaviagem et al., 2017; Cicek & Basar, 2017; Yuksel et al., 2017) and all the studies were performed in hospital settings. Three out of the seven studies included in the review reported data on the health care professional who provided information and guidance on breathing techniques: A physical therapist (Boaviagem et al., 2017), a nurse (Almeida et al., 2005), and the third study reported that a healthcare professional with experience in breathing techniques had provided guidance on breathing techniques without specifying who the health care professional was (Cicek & Basar, 2017). Two studies included women in labor regardless of parity (Boaviagem et al., 2017; Lemos et al., 2011), while the other five studies included only nulliparous women (Ahmadi et al., 2017; Almeida et al., 2005; Cicek & Basar, 2017; Kamalifard et al., 2012; Yuksel et al., 2017). All the studies included only low-risk pregnant women.
In all the selected studies, breathing techniques were the main resource used to control pain; however, in two of the studies, women were also instructed to perform global muscle relaxation associated with taking a deep breath in the intervals between contractions (Almeida et al., 2005; Yuksel et al., 2017). Six of the studies reported that the information on breathing techniques was given in the maternity ward during labor (Ahmadi et al., 2017; Almeida et al., 2005; Boaviagem et al., 2017; Cicek & Basar, 2017; Lemos et al., 2011; Yuksel et al., 2017). Regarding information provision and guidance, the analyzed articles reported diverse scenarios: Women received the information once during the active stage of labor when dilatation was between 4 cm and 8 cm (Boaviagem et al., 2017), at all stages of labor: Active, transition, and second stage of labor (Cicek & Basar, 2017), and during the latent stage (up to 4 cm of dilation) and women were encouraged to perform breathing techniques throughout labor (Almeida et al., 2005). Only one of the studies included in our review reported that information on breathing techniques was provided during pregnancy (36th week) and that women received reinforcement at the time of admission to the maternity ward in labor (Kamalifard et al., 2012).
The main common themes identified in the articles included in our review were organized into three categories: (a) use in the first stage of labor, (b) use in the second stage of labor, and (c) evaluation of the effectiveness of breathing techniques.
Use of Breathing Techniques During the First Stage of Labor
The main benefits of using breathing techniques during labor reported were: Pain control (Kamalifard et al., 2012), reduction in anxiety (Almeida et al., 2005; Cicek & Basar, 2017), and decrease in the duration of labor (Cicek & Basar, 2017). Regarding breathing techniques used, most of the reviewed articles referred to slow and deep breathing during contractions (Almeida et al., 2005; Boaviagem et al., 2017; Cicek & Basar, 2017). The Lamaze breathing technique described in two of the studies (Almeida et al., 2005; Cicek & Basar, 2017) was defined as a deep breath followed by slow, deep breathing—in through the nose and out through pursed lips. In the latent stage, the breathing was diaphragmatic, with the woman breathing in slowly; then breathing out slowly during the contraction. In the active and transition stages, differences were observed in breathing techniques between the studies.
Almeida et al. (2005) reported that during the active stage, the breathing technique recommended was slow and thoracic, with a slow, deep intake of breath, while in the transition stage, breathing was slow, with a deep sustained intake of breath followed by a long exhalation. Cicek et al. (2017) reported that during the active stage of labor, the guidance given to pregnant women was to perform shallow breathing, inhaling and exhaling through the mouth (making a “hee-hee-hoo” sound), and accelerate the rhythm of breathing as the contraction increased in intensity. In the transition stage, inhalation was similar to that performed in the active stage, and for exhalation, women were instructed to imagine that they were blowing out a candle.
According to Kamalifard et al. (2012), the use of breathing techniques was effective in controlling pain at 4, 6, and 10 cm of dilatation. Also, our review showed that the use of breathing techniques during labor helped to control anxiety, both during the latent (Almeida et al., 2005) and active stages of labor (Almeida et al., 2005; Cicek & Basar, 2017). In both of the aforementioned studies, women received information and guidance on how to perform breathing techniques according to the stage of labor and were monitored by a health care professional who encouraged them to use breathing techniques during labor.
In addition, Boaviagem et al. (2017) reported that information and guidance on breathing techniques were provided at the beginning of labor. At that time, women in the intervention group were oriented to inhale slowly on a count of 1–5, then to exhale slowly while counting down from 5 to 1, and when they were with 7–10 cm of dilatation women were instructed to pause for a count of 1–2 before starting a new breathing cycle and to perform pursed-lip breathing. No differences in anxiety scores or pain control were observed when compared to the intervention and control groups. Furthermore, in another study in our review, the use of the Lamaze breathing technique during the first stage of labor reduced the duration of the latent and active stages of labor (Cicek & Basar, 2017).
Use of Breathing Techniques During the Second Stage of Labor
The main benefits described in the reviewed articles on the use of breathing techniques during the second stage of labor were pain control (Yuksel et al., 2017), decreased duration of labor (Yuksel et al., 2017), and reduction in perineal trauma (Ahmadi et al., 2017). Two of the articles reported that breathing techniques used during the expulsion period were associated with the Valsalva maneuver (Almeida et al., 2005; Cicek & Basar, 2017). In one of the articles, the technique described was an intake of breath followed by an exhalation of 4 or 5 seconds while pushing down (Ahmadi et al., 2017). In the other article, women could choose between the Valsalva maneuver and breathing out while pushing down (Yuksel et al., 2017).
According to Lemos et al. (2011), the Valsalva maneuver could affect the well-being of the infant since the apnea associated with the effort can alter the acid-base balance, increasing fetal distress. No reduction in the duration of the expulsion period was found with this technique, and the author’s recommended that this breathing technique should be avoided. In another study, the Valsalva maneuver was compared with the technique of breathing out while pushing, and the effect of these two techniques on the pelvic floor was analyzed, and the authors concluded that the Valsalva maneuver should be avoided to protect the perineum from trauma (Ahmadi et al., 2017).
Yuksel et al. (2017) reported that information and guidance provided during the first stage of labor was for women to take a deep breath associated with apnea or prolonged exhalation through the mouth instead of the Valsalva maneuver during pushing. Also, women were informed that it was inadvisable to fill the abdomen with air and that they should push it down. The results showed that this breathing technique reduced pressure on the perineum at the time of expiratory force, helped women control pain, and reduced the expulsion stage by up to 50 minutes compared to women who did not use the technique.
Evaluation of the Effectiveness of Breathing Techniques
In the reviewed articles, the main variables analyzed to evaluate the effectiveness of breathing techniques were pain during childbirth (Almeida et al., 2005; Boaviagem et al., 2017; Cicek & Basar, 2017; Yuksel et al., 2017), anxiety (Almeida et al., 2005; Boaviagem et al., 2017; Cicek & Basar, 2017), the duration of labor (Almeida et al., 2005; Boaviagem et al., 2017; Cicek & Basar, 2017; Yuksel et al., 2017), and perineal integrity (Ahmadi et al., 2017). The instrument most commonly used for the evaluation of labor pain was the visual analog scale (VAS) from 0 to 10 (Almeida et al., 2005; Boaviagem et al., 2017; Kamalifard et al., 2012; Yuksel et al., 2017). Almeida et al. (2005) used the VAS score at the beginning of the latent, active, and transition stages during a uterine contraction. In two other articles, the VAS scale was used for evaluation after the intervention had been completed (Boaviagem et al., 2017; Kamalifard et al., 2012).
The State-Trait Anxiety Inventory (STAI) was the instrument most commonly used to evaluate anxiety (Almeida et al., 2005; Boaviagem et al., 2017; Cicek & Basar, 2017). Boaviagem et al. (2017) reported that women in their study completed the inventory after randomization and again two hours after the intervention. Almeida et al. (2005) used the Trait Anxiety Inventory (TAI-T) in the latent stage of labor and the State Anxiety Scale (STAI-S) in the active, transition, and immediate postpartum stages. Cicek et al. (2017) also used the STAI-Sat at three different moments: In the early latent stage (0–1 cm of dilation), in the late latent stage (4 cm), and in the late active stage (8 cm).
The duration of labor was assessed using a partogram (Boaviagem et al., 2017) or based on the investigator’s observation (Cicek & Basar, 2017; Lemos et al., 2011), and some studies did not specify how this evaluation was performed (Almeida et al., 2005; Yuksel et al., 2017). Other instruments used were: The Modified Borg Scale to evaluate fatigue (Boaviagem et al., 2017), an inspection of the perineum (classified as intact, anterior, or posterior tearing, and episiotomy (Ahmadi et al., 2017), an analysis of umbilical cord blood samples (Lemos et al., 2011), and neonatal outcome, as obtained from the medical records (Boaviagem et al., 2017; Lemos et al., 2011). Table 1 shows aspects of the studies selected for inclusion in this review.
TABLE 1. Summary of the Articles Selected for Inclusion in the Review.
| Authors—year of publication | Inclusion criteria | Stage of labor—information given | Breathing technique described | Stage of labor—use of breathing technique | When and how results were evaluated | Results |
|---|---|---|---|---|---|---|
| Almeida et al. (2005) | Primigravidae women with low-risk pregnancy and no associated pathology, in the latent stage of labor (≤ 4 cm), progression to normal delivery, no participation in antenatal preparation. | Information was provided during the latent stage and reinforcement given throughout labor. | Based on breathing techniques described by Read and Lamaze. Latent stage: Slow breathing with deep inhalation and exhalation. Active stage: Slow breathing with deep and prolonged inhalation and exhalation. Transition stage: Slow breathing, breathing deeply and holding the breath while pushing during contractions. Expulsion stage: Pressure breathing while bearing down. | Breathing techniques were used from the latent stage until expulsion stage. | The VAS scale was applied at the beginning of the latent, active and transition stages when the woman experienced pain. The STAI-T was applied during the latent stage of labor and the STAI-S during the active and transition stages, and immediately following delivery. | Women, who used breathing techniques, maintained a low level of anxiety through the latent, active and transition stages. No significant results in terms of pain during labor were reported. The duration of the latent stage was longer in the study group. |
| Lemos et al. (2011) | Primigravidae and multigravidae women 18–35 years old; with a low-risk pregnancy of 37–42 weeks and already admitted to the hospital. | Throughout the expulsion stage (between 10 cm of cervical dilatation and foetal expulsion). | Deep inhalation and apnea, Valsalva maneuver while bearing down. | Second stage of labor. | A chronometer was used to evaluate the duration of the expulsion stage. Pulse oximetry to measure oxygen saturation and a heart monitor to measure maternal heart rate were also used. In postpartum, the perineum was examined to evaluate the need of episiotomy and the degree of perineal trauma. Samples of umbilical cord blood, Apgar and newborn weight were evaluated. | Maternal outcomes were not associated with the duration of the Valsalva maneuver. A prolonged Valsalva maneuver was associated with reduced umbilical venous pH and venous base excess in the newborn infant. |
| Kamalifard et al. (2012) | Primigravidae women 20–35 years old and 36 weeks of gestational age. | Women received information at 36 weeks of pregnancy and at admission to the hospital. | Not specified. | Group I: Breathing techniques at 4 and 8 cm of dilatation. Group II: Breathing technique at 6 and 10 cm of dilatation. Group III: Massage at 4 and 8 cm of dilatation. Group IV: Massage at 6 and 10 cm of dilatation. | Thirty minutes after initiating the use of a technique, the VAS scale was used to evaluate pain. Blood pressure, pulse rate and body temperature were also evaluated. Partogram was used to evaluate the progression of labor and Apgar score to evaluate the vitality of the newborn. | There was a reduction in pain with breathing techniques at 4, 6, and 10 cm. of dilatation. However at 10 cm comparing the massage technique with breathing techniques, there was a significant reduction in pain. |
| Cicek et al. (2017) | Nulliparous women; 18–35 years old; 38–42 weeks of gestation without pregnancy complications, with a single healthy fetus in cephalic position; expected to have a spontaneous vaginal delivery, and in the early latent stage of labor (0–1 cm). | Information was provided at: The latent, active, transition and second stage of labor. Guidance and training were given for approximately 30 minutes. | First stage: Inhale slowly through the nose and exhale through the mouth. Second stage: Inhale through the nose to a count of 5 and exhale through the mouth in the same slow manner to a count of 5. Third stage: Breathe in and out rapidly through the mouth. The pattern includes the cleansing breath and the rhythmic hee-hee-hoo. Fourth stage: Breathe in and out through the mouth, with rapid and shallow blowing. | Throughout labor. | The STAI-S was used to asses’ anxiety. The duration of labor was evaluated by the researchers performed when the parturient women were at 0–1 cm, at 4 cm and at 8 cm of dilatation, respectively. | There was a reduction in anxiety at 8 cm of dilatation, and a reduction in the duration of the first stage of labor in the intervention group compared to the control group. |
| Boaviagem et al. (2017) | Pregnant women 12–40 years old, in active labor, with gestational age of 37–41 weeks. | Women received information during labor at 4 and 8 cm of dilatation. | At 4–6 cm of dilatation, women were instructed to breath slowly and deeply counting from 1 to 5 and to breathe out gradually counting from 5 to 1. At 7–10 cm of dilatation, women were instructed to slowly inhale through the nose and to breathe out through pursed lips. | Breathing techniques were performed for two consecutive hours after woman received the initial information | The STAI and VAS scales were applied 2 hours after the beginning of the intervention. The Modified Borg Scale was used to evaluate levels of maternal fatigue. | There was no significant difference between the intervention and control groups in relation to anxiety, pain, fatigue, or satisfaction. |
| Yuksel et al. (2017) | Nulliparous pregnant women at gestational age 37–42 weeks. | Women received information during the first stage of labor and received printed material for reinforcement of the information provided orally. | The women were instructed to breathe deeply and hold their breath for as long as possible while bearing down exhaling slowly. | Second stage of labor. | The VAS scale was used at the second stage of labor. | Pain was controlled and the duration of the second stage of labor was reduced (by ∼50 minutes). |
| Ahmadi et al. (2017) | Primiparous women, 18–35 years old with singleton pregnancy low-risk pregnancy at term, with cephalic presentation, candidate for vaginal delivery, who were at 3–5 cm of dilatation, normal and BMI (19.8–20.0). | Before the expulsion stage. | Women were instructed to take two deep breaths, then inhale and exhale through the mouth over 4–5 seconds while bearing down. In the control group, the Valsalva maneuver was used while bearing down. | Second stage of labor. | Pelvic floor was evaluated during labor and following delivery. Perineal trauma was assessed according to: Intact, posterior tear, anterior tear, episiotomy. | There was more probability of an intact perineum in women of the intervention group. The different forms of perineal tearing (1st-degree, 2nd-degree, 3rd-degree) was more frequent in the control group. |
Note. BMI = body mass index; STAI = state-trait anxiety inventory; STAI-S = state anxiety scale; STAI-T = trait anxiety inventory; VAS = visual analogue scale.
We assessed the four RCTs included in our review for selection, performance, detection, attrition, and reporting bias by the two authors. Results are presented in Figure 2. They did not present problems with random sequence generation, and one of them presented selection bias of allocation concealment. The four studies provided valuable information for health care professionals regarding the use of breathing techniques during different stages of labor.
The main findings of our narrative review on the use of breathing techniques without association with other non-pharmacological techniques showed that it could be beneficial for low-risk pregnant women during labor.
DISCUSSION
The main findings of our narrative review on the use of breathing techniques without association with other non-pharmacological techniques showed that it could be beneficial for low-risk pregnant women during labor. The main benefits observed for the laboring women were: Reduction in pain, anxiety, duration of labor, and perineal trauma; improvement in the well-being of the parturient women without risk for the newborn infant. Despite the differences in breathing techniques described in the reviewed articles, the results appeared to be largely similar, particularly with respect to pain control and well-being reported by the women.
When asked about the benefits of breathing techniques, women have reported that it helps to control pain during labor contractions (Akca et al., 2017; Miquelutti et al., 2013) and is more effective in controlling pain during labor when compared to other non-pharmacological techniques such as relaxation, acupressure, or massage (Brown et al., 2001). Furthermore, women who performed slow and deep breathing during uterine contractions and were prepared to initiate breathing techniques as soon as the contraction began reported that they were able to focus better on labor and birth and maximize their strength and control during each contraction (Nattah & Abbas, 2015). Articles published during the last decade have mainly focused on the use of breathing techniques associated with other non-pharmacological techniques (Akca et al., 2017; Bonapace et al., 2013).
The approach to using non-pharmacological methods to help women to control pain during labor and birth is not new. As previously described by Dick-Read, the concept is that eliminating fear would alleviate tension and reduce pain, thus breaking the vicious cycle of anxiety, pain, and fear (Anarado et al., 2015; Michaels, 2010). Dick-Read also recommended that each woman should focus on her natural rhythm and that the depth and rate of breathing would increase with the increase of the intensity of the contractions (Blankfield, 1969). This approach continues to be of the utmost relevance and interest in obstetric care, although it is not always used in the care of women in labor.
In the studies included in our review, the description of breathing techniques used varied between slow and deep breathing and more rapid breathing in the first stage of labor and between the Valsalva maneuver and slow and deep breathing in the second stage of labor. A previous study showed that deep breathing was the technique most commonly recommended by health care professionals and most commonly used in the first stage of labor (de Araújo et al., 2018). A recent study recommended that breathing techniques should be performed at a comfortable and individual rhythm to avoid dizziness and help the woman relax (Ciobanu, 2010).
Insofar as data from the second stage of labor are concerned, the lack of studies was more evident. There was no consensus in relation to the best breathing technique to be used during the expulsion stage since different variables were evaluated in each one of the articles reviewed (pain, duration, intact perineum, umbilical cord analysis) (Ahmadi et al., 2017; Lemos et al., 2011; Yuksel et al., 2017). However, in general, the deep and slow breathing technique was the one most commonly used, both in the first and the second stages of labor, and the one that produced the best results, both for the woman and for the newborn infant, compared to the Valsalva maneuver.
Breathing is one of the non-pharmacological techniques for women in labor, proposed by the WHO for the control of pain and to improve women’s wellbeing during childbirth. Recently, the WHO (World Health Organization, 2018) recommended that breathing techniques alone or in conjunction with other non-pharmacological techniques such as music, mindfulness, massage, and application of warm packs, among others, are recommended for healthy pregnant women when they claim for pain relief during labor and depending on a woman’s preferences.
Health care providers involved in antenatal care (ANC) represent one of the principal sources of information on childbirth for pregnant women (Neerland et al., 2019). Nevertheless, a recent study conducted in Brazil showed that no time is set aside at ANC consultations for the provision of information, with only routine exams being conducted. Therefore, the women had to resort to a variety of other sources of information, such as the internet or the experience of others (Heim et al., 2019). Information on the use of breathing techniques during labor could easily be transmitted by trained health care providers with no need for any specific resources or physical space, and these techniques can be used by pregnant women after receiving proper information.
Further studies on breathing techniques are required to define when pregnant women should be given information on this technique and what type of guidance is more effective.
Our review revealed a lack of studies on the benefits of using breathing techniques without association with other non-pharmacological techniques during childbirth. As for those studies that are available, there are discrepancies in the findings, differences in the methodology used to evaluate the results, and a lack of clarity regarding the methods used to assess the benefits of breathing techniques in some studies. Further studies on breathing techniques are required to define when pregnant women should be given information on this technique and what type of guidance is more effective. A relevant point that is worthwhile to be highlighted as a result of our review refers to the fact that none of the articles selected for inclusion in our review reported on an intervention given throughout ANC to make women aware of the benefits of the use of breathing techniques and how to use it correctly as a means to control contractions, reduce pain, and improve wellbeing.
The reviewed studies reported that women received information on breathing techniques at the hospital when labor had already begun or during birthing (Ahmadi et al., 2017; Almeida et al., 2005; Boaviagem et al., 2017; Cicek & Basar, 2017; Lemos et al., 2011; Yuksel et al., 2017). It is also important to emphasize that all the studies reviewed reported benefits resulting from the use of these techniques, with none of the studies reporting any adverse events, either for the mother or for the child. In conclusion, breathing techniques reported in our review, irrespective of the moment at which information on the technique is given and the manner in which guidance was provided, is a non-pharmacological technique that provides pain relief during contractions and can improve women’s well-being without adverse effects on the newborn infant.
Our study may present a limitation due to possible variations from country to country in the understanding and the definitions of concepts such as low-risk pregnancy, labor, labor progress, breathing, and coping with pain, among others. Also, the reviewed papers did not present information on the broader context regarding the procedures implemented in obstetrical care in the different countries, and this obviously can have an influence on how women deal with birthing. The different instruments used and the different times of evaluation in the reviewed studies did not permit a granular discussion on reliability and validity across the different settings. However, the strength of our review is that it presents information on the evaluation of the use of breathing techniques that is helpful for health care providers; because of the differences presented in the reviewed articles, the results seem quite consistent regarding pain control and well-being of women.
Biographies
MARIA A. HEIM, psychotherapist, Master in Science and PhD candidate at the Post Graduate Program, Department of Obstetrics and Gynecology, School of Medicine, State University of Campinas, Brazil.
MARIA Y. MAKUCH, Clinical Psychologist, Master and PhD in Mental Health, Participating Professor at the Post Graduate Program, Department of Obstetrics and Gynecology, School of Medicine, State University of Campinas, Brazil.
DISCLOSURE
The authors have no relevant financial interest or affiliations with any commercial interests related to the subjects discussed within this article.
FUNDING
The author(s) received no specific grant or financial support for the research, authorship, and/or publication of this article.
CONTRIBUTIONS
Both authors were involved in the conception and design of the study, data collection, analysis, and interpretation of data; writing of the article and the final approval of the version to be published.
REFERENCES
- Ahmadi, Z., Shanaz, T., Roosta, F., Shaker, N., & Mhmoodi, N. (2017). Effect of breathing technique of blowing on the extent of damage to the perineum at the moment of delivery: A randomized clinical trial. Iranian Journal of Nursing and Midwifery Research, 22(1), 62–66. 10.4103/1735-9066.202071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akca, A., Esmer, A. C., & Osyurek, E. S., Aydin, A., Korkmaz, N., Gorgen, H., & Akbayir, O. (2017). The influence of the systematic birth preparation program on childbirth satisfaction. Archives of Gynecology and Obstetrics, 295(5), 1127–1133. 10.1007/s00404-017-4345-5 [DOI] [PubMed] [Google Scholar]
- Almeida, N. A. M., de Souza, J. T., Bachion, M. M., & Silveira, N. A. (2005). Utilização de técnicas de respiração e relaxamento para alívio de dor e ansiedade no processo de parturização. Revista Latino-Americana de Enfermagem, 13(1), 52–58. 10.1590/s0104-11692005000100009 [DOI] [PubMed] [Google Scholar]
- Anarado, A., Ali, E., Nwonu, E., Chinweuba, A., & Ogbolu, Y. (2015). Knowledge and willingness of prenatal women in Enugu Southeastern Nigeria to use in labor non-pharmacological pain reliefs. African Health Sciences, 15(2), 568–575. 10.4314/ahs.v15i2.32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blankfield, A. (1969). Spontaneous respiratory rate in first stage labor-comparison with the breathing exercises of natural-childbirth methods. Australian and New Zealand Journal of Obstetrics and Gynaecology, 9(118), 118–121. 10.1111/j.1479-828x.1969.tb02543.x [DOI] [PubMed] [Google Scholar]
- Boaviagem, A., Melo Junior, E., Lubambo, L., Souza, P., Aragão, C., Albuquerque, S., & Lemos, A. (2017). The effectiveness of breathing patterns to control maternal anxiety during the first period of labor: A randomized controlled clinical trial. Complementary Therapies in Clinical Practice, 26, 30–35. 10.1016/j.ctcp.2016.11.004 [DOI] [PubMed] [Google Scholar]
- Bonapace, J., Chaillet, N., Gaumond, I., Paul-Savoie, E., & Marchand, S. (2013). Evaluation of the Bonapace Method: A specific educational intervention to reduce pain during childbirth. Journal of Pain Research, 6, 653–661. 10.2147/JPR.S46693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, S. T., Douglas, C., & Flood, L. P. (2001). Women’s evaluation of intrapartum nonpharmacological pain relief methods used during labor. Journal of Perinatal Education, 10(3), 1–8. 10.1624/105812401X88273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaillet, N., Belaid, L., Crochetière, C., Roy, L., Gagné, G. P., Moutquin, J. M., Rossignol, M., Dugas, M., Wassef, M., & Bonapace, J. (2014). Nonpharmacologic approaches for pain management during labor compared with usual care: A meta-analysis. Birth, 41(2), 122–137. 10.1111/birt.12103 [DOI] [PubMed] [Google Scholar]
- Cicek, S., & Basar, F. (2017). The effects of breathing techniques training on the duration of labor and anxiety levels of pregnant women. Complementary Therapies in Clinical Practice, 29, 213–219. 10.1016/j.ctcp.2017.10.006 [DOI] [PubMed] [Google Scholar]
- Ciobanu, D. I. (2010). Relaxation and breathing techniques—positive factors in the deployment of pregnant woman’s labor and delivery. European Journal of Physical and Health Education, 3(2), 39–48. [Google Scholar]
- Collins, J. A., & Fauser, B. C. (2005). Balancing the strengths of systematic and narrative reviews. Human Reproduction Update, 11, 103–104. 10.1093/humupd/dmh058 [DOI] [PubMed] [Google Scholar]
- de Araújo, A. E., Delgado, A., Boaviagem, A., & Lemos, A. (2018). Prescription of breathing orientations given by the healthcare team during labor: A cross-sectional study. O Mundo da Saúde, 42(3), 628–641. [Google Scholar]
- Faisal, I., Matinnia, N., Hejar, A. R., & Khodakarami, Z. (2014). Why do primigravidae request caesarean section in a normal pregnancy? A qualitative study in Iran. Midwifery, 30(2), 227–233. 10.1016/j.midw.2013.08.011 [DOI] [PubMed] [Google Scholar]
- Gadade, M., & Podder, L. (2015). Effectiveness of selected paced breathing on anxiety level and pain perception during first stage of labor among parturient in Pune. International Journal of Nursing Research and Practice, 2(1), 28–32. [Google Scholar]
- Gayeski, M. E., & Brüggemann, O. M. (2010). Non-pharmacological approach to pain relief during labor as hard-light care technology: A systematic review. Texto e Contexto Enfermagem, 19(4), 628–634. 10.1590/S0104-07072010000400022 [DOI] [Google Scholar]
- Handelzalts, J. E., Becker, G., Ahren, M.-P., Lurie, S., Raz, N., Tamir, Z., & Sadan, O. (2015). Personality, fear of childbirth and birth outcomes in nulliparous women. Archive of Gynecology and Obstetrics, 291(5), 1055–1062. 10.1007/s00404-014-3532-x [DOI] [PubMed] [Google Scholar]
- Heim, M. A., Miquelutti, M. A., & Makuch, M. Y. (2019). Perspective of pregnant women regarding antenatal preparation: A qualitative study. Women and Birth, 32(6), 558–563. 10.1016/j.wombi.2018.11.016 [DOI] [PubMed] [Google Scholar]
- Kamalifard, M., Shahnazi, M., Melli, M. S., Allahverdizabeh, S., Toraby, S., & Ghahvechi, A. (2012). The efficacy of massage therapy and breathing techniques on pain intensity and physiological responses to labor pain. Journal of Caring Sciences, 1(2), 73–78. 10.5681/jcs.2012.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemos, A., Dean, E., & de Andrade, A. D. (2011). The Valsalva maneuver duration during labor expulsive stage: Repercussions on the maternal and neonatal birth condition. Revista Brasileira de Fisioterapia, 15(1), 66–72. 10.1590/s1413-35552011000100012 [DOI] [PubMed] [Google Scholar]
- Lothian, J. A. (2011). Lamaze breathing: What every pregnant woman needs to know. The Journal of Perinatal Education, 20(202), 118–120. 10.1891/1058-1243.20.2.118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michaels, P. A. (2010). Comrades in the labor room: The Lamaze method of childbirth preparation and France’s cold war home front, 1951–1957. The American Historical Review, 115(4), 1031–1060. 10.1086/ahr.115.4.1031 [DOI] [Google Scholar]
- Miquelutti, M. A., Cecatti, J. G., & Makuch, M. Y. (2013). Antenatal education and the birthing experience of Brazilian women: A qualitative study. BMC Pregnancy and Childbirth, 13(171) 10.1186/1471-2393-13-171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miquelutti, M. A., Cecatti, J. G., & Makuch, M. Y. (2015). Developing strategies to be added to the protocol for antenatal care: An exercise and birth preparation program. Clinics, 70(4), 231–236. 10.6061/clinics/2015(04)02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nattah, F. M., & Abbas, W. A. K. (2015). Assessment of level of pain and its relation with breathing exercise in the first stage of labor among primi mothers at Hilla teaching hospital. European Journal of Scientific Research, 135, 121–128. [Google Scholar]
- Neerland, C. E., Avery, M. D., Saftner, M. A., & Gurvich, O. V. (2019). Maternal confidence for physiologic birth: Associated prenatal characteristics and outcomes. Midwifery, 77, 110–116. 10.1016/j.midw.2019.07.004 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2018). WHO recommendations: Intrapartum care for a positive childbirth experience, Geneva. Available from: /www.ncbi.nlm.nih.gov/books/NBK513809. [Accessed 30 sep 2019]. [PubMed]
- Yildirim, G., & Sahin, N. H. (2004). The effect of breathing and skin stimulation techniques on labor pain perception of Turkish women. Pain Research and Management, 9(4), 183–187. 10.1155/2004/686913 [DOI] [PubMed] [Google Scholar]
- Yuksel, H., Cayir, Y., Kosan, Z., & Tastan, K. (2017). Effectiveness of breathing exercises during the second stage of labor on labor pain and duration: A randomized controlled trial. Journal of Integrative Medicine, 15(6), 456–461. 10.1016/S2095-4964(17)60368-6 [DOI] [PubMed] [Google Scholar]