Abstract
Over the past decade, healthcare providers nationwide have contended with a growing boarding crisis as pediatric patients await psychiatric treatment in emergency departments (EDs). COVID-19 has exacerbated this urgent youth mental health crisis, driving EDs to act as crisis units. Journey mapping is a robust methodology with which to examine strengths and challenges in patient care workflows such as boarding and emergency psychiatric care. Psychiatric, emergency medicine, and hospitalist providers serving patients boarding at a northeastern children’s hospital participated in semi-structured qualitative interviews. Investigators conducted directed content analysis with an inductive approach to identify facilitators, barriers, and persistent needs of boarding patients, which were summarized in a patient journey map. Findings were presented to participants for feedback and further refinement. Quantitative data showed a three-fold increase in the number of patients who boarded over the past three years and a 60% increase in the average time spent boarding in the ED. Emergent qualitative data indicated three stages in the boarding process: Initial Evaluation, Admitted to Board, and Discharge. Data highlighted positive and negative factors affecting patient safety, availability of beds in pediatric hospital and psychiatric inpatient settings, high patient-provider ratios that limited staffing support, and roadblocks in care coordination and disposition planning. Patient journey mapping provided insight into providers’ experiences serving patients boarding for psychiatric reasons. Findings described bright points and pain points at each stage of the boarding process with implications for psychiatric care and systemic changes to reduce boarding volume and length of stay.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10488-022-01249-4.
Keywords: Psychiatry, Emergency medicine, Suicide, Mental health
The nation’s emergency departments (ED) are rapidly becoming the first point of contact for youth experiencing psychiatric crises. Boarding patients, defined as patients held in EDs and medical units for an extended period of time while awaiting psychiatric placements, often receive limited psychiatric intervention due to limited hospital resources (Alakeson et al., 2010; Campbell & Pierce, 2018; Leyenaar et al., 2021). The increased need for specialized psychiatric services and an inability to provide appropriate psychiatric intervention has led to a nationwide crisis as patients who are boarding wait days to weeks for a psychiatric placement. The COVID-19 pandemic has further exacerbated the youth mental health crisis, intensifying urgency as hospitals respond to higher volumes of psychiatric emergencies. Qualitative methods used in implementation science may prove useful in examining factors contributing to the flow of boarding patients through emergency and medical services and provide insight towards systemic improvement.
Rising Numbers of Psychiatric ED Presentations
The past two decades prior to the COVID-19 pandemic have seen a sharp rise in child and adolescent psychiatric emergencies, leading to an increase in patient volume in EDs. National trends in mental health show that between 2009 and 2015, mental health-related ED visits increased 56.4% for pediatric patients, and a recent study demonstrated an increase of 329% in ED visits from 2007 to 2016 for deliberate self-harm (Lo et al., 2020; Santillanes et al., 2020). Primarily designed to address urgent physical health problems, EDs lack the resources and staffing to adequately address this rising need (Campbell & Pierce, 2018). At the same time, availability of community-based services and psychiatric inpatient beds has decreased, leaving fewer options for disposition and transfer to necessary care (Nicks & Manthey, 2012).
Impact of COVID-19 on Emergency Mental Health Services
Since the onset of the COVID-19 pandemic, the boarding crisis has continued to grow due to a confluence of strained healthcare systems and increasing mental health concerns. Rates of child and adolescent anxiety, depression, and suicidal thoughts and behaviors have risen substantially over the course of the COVID-19 pandemic (Kudinova et al., 2021; Power et al., 2020; Thompson et al., 2021). Increased suicidal ideation and attempts among adolescents correspond with elevated distress due to COVID-related stressors and heightened community responses (Hill et al., 2021; Yard et al., 2021). In addition to exacerbating the mental health crisis, the COVID-19 pandemic interrupted the regular foundation of healthcare, increasing strain on staff and directing resources away from usual community-based care to accommodate urgent need for acute medical care (Fegert et al., 2020). Due in part to these disruptions, EDs have assumed a greater role in responding to psychiatric emergencies (Cloutier & Marshaall, 2021) and the number of mental health presentations to the ED now exceeds pre-pandemic patient volumes (Goldenberg & Parwani, 2021; Yard et al., 2021). For youth ages 12–17 specifically, there was a 31% increase in mental health-related ED visits in 2020 compared to 2019 (Yard et al., 2021), further contributing to longer wait times for access to appropriate psychiatric care (Zeller et al., 2014). The growing need for emergency psychiatric services coupled with strained healthcare systems have further extended boarding times such that many hospitals now report an average wait for admission or transfer to a psychiatric bed of 48 h (Leyenaar et al., 2021).
Mapping as a Tool for Identifying Contributing Factors
In light of critical challenges at the intersection of the youth mental health and boarding crises, as well as the COVID pandemic, further work examining the process by which psychiatric patients travel through the healthcare system may provide insights to reduce wait times, enhance quality of care, and improve provider experiences. Journey mapping – a research methodology often used in implementation science to assess organizational workflows in clinical settings – provides a structured qualitative process by which to evaluate care of boarded patients. A journey map is a visual representation of patients’ movements through a complex healthcare system in a simple and succinct progression (Kushniruk et al., 2020). Investigators create journey maps through a multi-step process involving semi-structured interviews of patients or individuals who work within the system, visualizing the steps a patient takes through the system, and reviewing the steps with interviewees to create a complete map using an iterative process. Following inductive content analysis, data presented in journey maps highlight common themes and systematic barriers to include in an initial map, which is then used to obtain additional cross validation and feedback for revision (Bearnot & Mitton, 2020; Vears & Gillam, 2022). In visualizing the coordination of multiple disciplines of care, treatment teams can identify barriers and inefficiencies in the system and thus determine points of intervention within the treatment team’s control (Andersen et al., 2014; Trebble et al., 2010). Further, stakeholders can utilize mapping insights to improve quality of care and facilitate a cohesive flow between the multiple healthcare disciplines involved in pediatric psychiatric patient care (Crowe et al., 2020; Trebble et al., 2010).
The Current Study
The current study aimed to better understand the boarding process within one pediatric hospital by collecting quantitative and qualitative data about patients admitted to board. In particular, the study sought to identify strengths and contributors to success in keeping patients safe while awaiting inpatient psychiatric care, obstacles to quality care, bottlenecks in patient flow, and potential points of intervention by which to alleviate burden and strain on patients, families, hospital staff, and resources. To address these aims, the study evaluated quantitative data related to the number of patients presenting to the ED for psychiatric reasons, the length of stay in the ED, and the length of stay patients are boarding. Based on qualitative data, a patient journey map was developed from the perspective of emergency and hospital staff. A final study aim was to provide insights into this process which may guide future efforts towards quality improvement.
Methods
Design & Setting
The study followed an emergent design which included quantitative and qualitative data collection conducted in a children’s hospital in the northeastern United States (Husebø & Olsen, 2016). On average, over 4,000 youth presented at the target hospital each year for psychiatric concerns, accounting for approximately 8% of the total patient population. The local Institutional Review Board gave a determination of exemption for this study.
Qualitative interviews were conducted in a semi-structured format with medical and emergency staff involved in the psychiatric admission and boarding process. To best capture and visualize the patient journey from the staff perspective, we designed a question list for the semi-structured interviews based on the literature and expertise of the project team (consisting of psychologists, post-doctoral fellows, clinical interns, and research assistants). The questions focused on the steps of the patient journey, prior problems and barriers to care, suggested and attempted improvements as well as outcomes and persistent needs, and staff experience of their role in the patient journey. A full outline of interview questions can be found in Appendix A. Interviews were conducted between September and December 2021.
Participants included 15 healthcare providers from teams with a prominent role in the daily care coordination and disposition planning of patients boarding for psychiatric reasons, including the Psychiatric Consult-Liaison (CL) team, Pediatric Psychiatric Emergency Services (Pedi PES) team, nursing staff, social work, and pediatric and adolescent medicine hospitalists. The sample of providers included: psychiatrists (n = 3), psychologists (n = 2), pediatricians (n = 2), a licensed social work counselor (n = 1), registered nurses/nurse practitioners (n = 4), a physician’s assistant (n = 1), and psychiatry residents (n = 2). The range of experiences in this setting ranged from three months to 22 years (M = 8.8 years). Potential participants were identified by stakeholders on the CL and Pedi PES teams, and were contacted via email or through the electronic medical record software (EPIC) private chat with stakeholder support regarding interest and availability for participation in the current study. The semi-structured interviews lasted for approximately 20–45 min and were conducted by study staff. Interviews were conducted with two study staff present: one functioned as a primary interviewer (TC, EH, JW) and one functioned as a note-taker (SS, SC, MM). Direct quotes were obtained from the participants whenever possible.
Data Analysis
An emergent design was used to create the patient journey map, following Galloway’s guidelines (Galloway, 1994; Kim et al., 2016). The first part of the data analysis utilized this design to view the emergent themes in the patient journey without assigned codes. Such an approach allowed for the connections between concepts and factors in the journey map to be viewed within different care contexts (Elo & Kyngäs, 2008). We evaluated the process of a pediatric psychiatric patient moving through the emergency department to their final disposition. The study team defined the start point (initial evaluation), middle points (admission to board), and end points (discharge) of the patient journey. Multiple members of the research team open coded interviews, developed and revised versions of the journey map based on interviews, and arrived at an internal consensus via group discussion. This process was repeated iteratively to yield a visual representation of the journey map that the research team presented to PES and CL team stakeholders for validation and discussion for further refinement.
In the second step of data analysis, following the development of the primary stages of the patient journey map, interview notes were closely reviewed by study staff using an inductive content analysis approach (Kyngäs, 2020; Schouten et al., 2021; Vears & Gillam, 2022). An inductive content analysis approach was utilized in the current study given the approach’s suitability for understudied processes or phenomena (Elo & Kyngäs, 2008). Study staff reviewed each of the interview documents and developed a coded list of a priori bright points (“what is working?”) and pain points (“what is a barrier?”). Study personnel then collaboratively reviewed individually coded themes and extracted the steps of the patient journey from the analyses, with the inclusion of quotes when applicable (Schouten et al., 2021). A summary of the coding themes is presented in Table 1. This procedure of coding, research team discussion and consensus, stakeholder review, and revision occurred twice and concluded when sufficient agreement was met. Stakeholders contributed to the subsequent preparation and review of this manuscript to ensure accuracy of results and provide perspective to conclusions and discussion.
Table 1.
Summary of inductive codes for the stages of the patient journey
| 1. Initial evaluation | 2. Awaiting disposition | 3. Discharge |
|---|---|---|
| 1.1 Bright points | 2.1 Bright points | 3.1 Bright points |
| 1.2 Pain points | 2.2 Pain points | 3.2 Pain points |
Results
Quantitative Review of Medical Record Data
Chart review data demonstrated a rapid increase in the number of patients admitted as boarders for psychiatric reasons from 260 in 2019 to 837 in 2021. Nearly half (49%) of patients presenting for psychiatric reasons in 2021 required a higher level of care (i.e., psychiatric inpatient care, intensive outpatient hospitalization, etc.). For psychiatric patients ages 4–11, the most frequent presenting problem was adjustment problems (45%); and for patients ages 12–18, the most common presenting problem was depression (54%). Over the past three years, patients awaiting psychiatric treatment have spent an average of three to four days in the hospital ED awaiting a disposition. From 2019 to 2021, there was a 61% increase in the average length of time patients spent in the ED. Although there was an increase in presentations to the ED and time spent waiting in the ED, patients spent about 14 hours less on average on a medical floor and six hours less in total time boarding in 2021 compared to 2019. See Table 2 for boarder rates and length of stay data from 2019 to 2021.
Table 2.
Number of pediatric patients boarding for psychiatric reasons and time patients spent in the stages of the patient journey
| Number of psychiatric patients boarding | Average time spent boarding in ED (Hours) | Average time boarding on medical floor (Hours) | Average total time boarding (Days) | ||
|---|---|---|---|---|---|
| 2019 | 260 | 11.76 | 86.16 | 4.08 | |
| 2020 | 572 | 8.40 | 62.40 | 2.94 | |
| 2021 | 837 | 18.96 | 72.72 | 3.81 | |
Note: Dates represent fiscal years. 2019 = 10/1/18 − 9/30/19; 2020 = 10/1/19 − 9/30/20; 2021 = 10/1/20 − 9/30/21
Stages of the Patient Journey
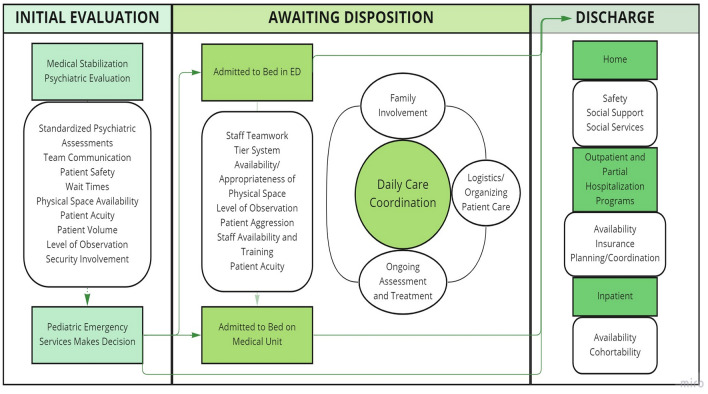
Emergent data from the qualitative interviews suggested that there were three phases that reflected the timeline of the patient journey: Initial Evaluation, Admission to Board, and Discharge (See Figure. 1). Additional themes were inductively derived from the interviews which related to the decision points and staff experiences within each phase that described bright points and pain points.
Figure. 1.
Patient Journey Map
Initial Evaluation
The patient’s journey began with initial presentation to the ED. Upon arrival, ED nursing staff triaged individuals for type and level of care. If the patient required specialized psychiatric evaluation and did not need medical stabilization, they were further evaluated by a consulting psychiatric specialty service within the hospital (e.g., Pedi PES). If requiring medical stabilization, patients were medically admitted, either for routine medical care or to the Pediatric Intensive Care Unit prior to evaluation and psychiatric consultation.
Within the initial psychiatric evaluation stage, several key themes affected a patient’s journey. The bright points included the use of standardized questionnaires to guide psychiatric assessment, active and effective coordination between medical, Pedi PES, and CL teams, and consistent maintenance of patient safety. During ED triage, patients completed the Columbia-Suicide Severity Rating Scale, a standardized assessment that was used to guide clinical decisions around safety. This information was helpful in identifying the patient’s primary concern and providing the assessing clinician with a baseline for Pedi PES involvement. An emergency social worker stated, “if the CSSRS score was high, the attending ER doctor ordered the consult for Pedi PES.” This was further helpful for guiding clinical decisions and assessing initial safety information. As patients were seen, frequent communication between Pedi PES and CL provided important collaboration to ensure services “get kids where they need to be.” As assessment and disposition planning occurred, this collaboration and communication contributed to maintaining safety and providing clinical care.
In terms of pain points, the overarching theme at this stage was extended wait times. As one Pedi PES provider described, “patients are sometimes in the ED for hours even before the PES consult service is called.” Subthemes included availability and appropriateness of physical space, acuity of patients, ED patient volume, and staff availability. Multiple interviewees noted the lack of appropriate physical space to place patients while they awaited clinician decisions and placements. One Pedi PES provider described the ED waiting space as only “a little waiting room” that cannot meet the needs of patient and family volume. This also created a barrier for assessment and disposition planning as one provider stated, “we don’t have physical spaces to pull families out of double rooms and have necessary conversations.” Further, one PES provider described, the noise of the ED and lack of privacy for conversations was a common family frustration. Observing varying psychiatric needs (e.g., aggression, psychosis), may also have created emotional distress for patients and families waiting in proximity. Another pain point at this stage was the overall volume of patients presenting to the ED which subsequently limited staff availability for addressing basic needs. Security staff availability, which was crucial for ensuring a safe environment with patients of varying acuity, was cited as “a big problem right now; we’ve lost a lot of staff in the past few months.” Contributing to long wait times, the ED and supporting CL and Pedi PES teams were not designed to support the volume and acuity of patients presenting with mental health concerns. Administrative staff expressed that “with no cap for the volume of patients in these settings, compared to the finite number of beds on an inpatient psychiatric unit, there were simply not enough clinicians [to meet the emergency psychiatric needs of patients].”
Boarding in the ED
If a patient required inpatient psychiatric care but could not transfer directly to an appropriate program, the Pedi PES team alerted the ED team who entered the admission order. This alerted the hospital to a bed request for boarding status. Two hours following the admission order, the patient was considered to be inpatient status, and care then transferred to the pediatric hospitalist team even if the patient was still physically in the ED. There may have been an extended period spent boarding in the ED prior to moving to the medical floor.
Consistent with the initial evaluation stage, this stage of the patient journey highlighted bright points associated with strong communication and collaboration between different services. Many interviewees expressed “as a team we work well together to make sure every child is seen; we do the best we can.” Others spoke to the strong support they feel from team leadership. One PES provider expressed, “we support one another and have awesome leadership.” These sentiments suggested that teams were very effective in supporting each other as they met incredibly complex needs within systems not specifically designed to meet those needs. Teams also worked together to identify and problem solve system adjustments internally. In one example, a tier system was developed in response to the growing number of boarded patients and the need to communicate level of patient risk more effectively as they boarded in a non-psychiatric physical space.
Positive supports and camaraderie from leaders and between teams helped to offset the various factors that contributed to the difficulty of assigning available beds to move patients out of the ED. These pain points included the level of observation needed (e.g., 1:1, security) and patients’ cohortability, or the degree to which different patient characteristics (e.g., age, psychiatric presentations, trauma, aggression, sexualized behavior) affects their ability to safely cohabitate in double rooms while awaiting psychiatric treatment. In addition, it was noted that psychiatric patients may have been more difficult to place in the hospital system compared to traditional medical patients because of their acuity and the stigma surrounding mental health, despite the inappropriateness of boarding these individuals in the ED setting. One clinician highlighted that “people don’t see mental health as important as physical issues; even the kids feel this way.” Given the difficulty of placing psychiatric patients, psychiatric providers at times have individually advocated for patients to transition to the medical unit which was stated to be “predominately done to prevent a patient from falling through the cracks.” For patients who remained in the ED for extended periods, the most prominent pain point was the inability to address basic needs in this setting (e.g. meal options, hygiene, limited focused therapeutic support). This was noted by several interviewees and was described as distressing to both patients and staff. For example, one ED provider described, “I’m concerned that kids aren’t getting to shower regularly. Some kids in the ED choose the same food every day. I’ve had parents complain that they aren’t changing undergarments or [receiving] new scrubs.”
Boarding on a Medical Unit
As medical beds became available, patients were moved out of the ED and onto a medical floor to await disposition. Once on the medical floors, the CL team became the central coordinators of care and disposition planning. Communication between teams, providers, and leaders was again a noted bright spot within this part of the process. Although services were not designed to meet this high level of need, providers within the services were strongly committed to these patients and worked together to engage patients in brief clinician interventions focused on safety in the hospital while they awaited more specialized care. An additional bright point for patients once boarding included a newly created pediatric behavioral intervention (PBI) team, who treated patients both in the ED and on medical floors. This team was described as a “group of people who are not counselors/social workers/psychologists but are trained in some way in our system to provide therapeutic support with the kids all day to provide coping skills, distractions, etc.” Others described this service as a first line to help engage and de-escalate kids who are dysregulated before security is involved. Having these therapeutic supports appeared helpful in managing some of the daily challenges with engaging patients as they waited for specialized placement.
While the PBI team provided necessary therapeutic support for patients and staff, the team was unfortunately not large enough to support the immense influx of patients in need of psychiatric care. Medical rooms were also not designed for psychiatric safety; there were multiple ligature and other risks that may have posed a threat for both patient and staff safety. Uniformly, interviewees commented on pain points related to limited opportunities, staffing, and space for therapeutic interventions with patients on the medical floors. As one PES provider reported, “It’s really hard because there is really not a lot of clinical intervention being offered while they are here.” Providers often referred to the lack of time available to provide these services given the patient volume. Several people also noted the negative effect this has had on the morale of providers. One CL provider shared, “It’s hard to maintain good morale when I know that there’s a 10-year-old whose birthday is today but he’s stuck here. It’s that kind of stuff. If I knew he was getting more intervention, it wouldn’t feel quite as bad.” Relatedly, the inadequacy of the physical space had been a persistent pain point. In typical inpatient psychiatric care, patients participate in a therapeutic milieu intended to provide positive behavioral activation and socialization. However, boarding patients were often confined to their rooms with few activities and limited socialization. As one CL provider described, “For the majority of the day, kids are left to their own devices and can stay in bed with the lights out and isolate themselves without much intervention.” Another CL provider described, “These patients are just sitting in their rooms throughout their stay. Even if they are 1:1, they rarely interact in a therapeutic way throughout the boarding process.”
In addition to challenges with therapeutic intervention, organizing who assumed responsibility for boarded patients was another noted pain point. Because boarding patients were identified as medical patients, the primary team responsible was a hospitalist team. However, this team often deferred to CL for treatment decisions given their expertise in psychiatric care. As one hospitalist provider described, there was a potential for “diffusion of responsibility in which people slowly become a little less detail-oriented due to the overlap of hospitalists and psych CL service” in caring for the patient. Other concerns with hospitalists acting as the primary team included hospitalists feeling less equipped to manage psychiatric medications, prioritizing traditional medical cases when caseloads were high, and lacking a daily hand-off system to quickly understand the most pertinent updates. Added to this, CL providers recognized being “chronically overrun” as they supported both patients who are boarding and traditional medical inpatients in need of psychiatric consultations. The hospitalist and CL teams also had multiple providers and trainees rotating in and out of services daily which increased both numbers of supporting staff and challenges with continuity of care. For example, one CL provider described, “You are just coming in and seeing the patient and don’t really know their journey.” Disruptions in provider continuity contributed to difficulties in disposition planning given the lack of time to understand significant background information, as well as build rapport with patients and families, which was crucial to providing feedback on next steps. These barriers, as well as the acuity of patients and lack of availability of lower-level or community-based services, often contributed to the difficulty of appropriately diverting patients away from psychiatric inpatient services that may not have been necessary for all boarding patients as their time in the hospital continued. It was also challenging to have difficult conversations with families (e.g., about psychiatric needs, medications, and safety risks) without having adequate time for rapport building or in-depth, serial parent psychoeducation.
A final pain point cited by multiple interviewees included the lack of psychiatric training for general providers and hospital staff. Many hospital staff were not trained in de-escalation and behavioral management skills, which often led to discomfort from minimal experience in caring for psychiatric patients. Hiring additional staff was a suggested intervention in almost all interviews, and one psychiatry resident highlighted that in addition to increased staffing, “We need to spend more time training and educating the staff that we have so they are more comfortable interacting with these patients”.
Discharge
In addition to ensuring safety, the primary focus for boarding patients was moving them off the medical floor to appropriate psychiatric care. Although the system was not specifically designed to address this need for the number of patients it was supporting, the system was moving patients towards appropriate care placements while maintaining safety. As one CL provider described, the system was still “far from what [the patients] deserve and need”, but it had been successful “in keeping kids safe, which is the most important thing at its core.” This success was often attributed to previously noted bright spots of comradery, communication, professionalism, and all-around teamwork.
To link patients with psychiatric services, the process was labor intensive and time consuming, and sometimes patients left the hospital without being linked to appropriate care. A frequently discussed pain point associated with discharge planning and coordination was the current organizational structure for determining availability of services. As one PES provider described, the “administrative system of getting patients beds appears to be more challenging and labor intensive than needed.” Another CL provider described the process as “profoundly inefficient.” Discharge planning required psychiatric consult providers to individually maintain communication with multiple service coordinators (e.g., through email chains or secure chat) to determine bed/placement availability. They also determined which patients were most appropriate for a particular service. Because no dedicated staff were available for coordinating this process, consult providers filled this role in addition to the clinical services they provided. It was also noted that not all providers could bill for care coordination efforts, further limiting who could perform this task and how much time a given provider was able to dedicate to it. While considerable care coordination did take place during this phase, providers also voiced frustrations that they could not always communicate this coordination information or the extent of their efforts to families given that the status frequently changed, further adding to families’ and providers’ frustrations.
One of the most mentioned pain points at this phase was a lack of available service options. Many interviewees noted increased length of stay on psychiatric inpatient units, a lack of outpatient providers, long waiting lists with in-home providers, and unavailable spots at lower levels of care (e.g., partial hospitalization programs). As one CL provider described, “The lack of outpatient supports creates a ripple effect where patients in inpatient programs have nowhere to be discharged to, thus creating more [boarding of patients]. If they are determined to be safe to go home, they also have nowhere to go in outpatient and continue boarding.” The increase in patients who are boarding also affected who was routed to the highest levels of care. Some youth stabilized while they were boarding; however, given time limitations for ongoing assessment and care coordination, it became less likely that a patient was diverted and instead was admitted for inpatient care. One CL provider noted this irony, “[Hospital administration] recognizes that the busier we get, the softer the admissions have become.” In other words, during periods of high patient volume, Pedi PES and CL teams had less ability to work on alternate levels of care, impacting the ability to divert patients later in the boarding process and leading some patients to be admitted to inpatient level of care.
Other challenges related to discharge planning and care coordination included individual patient and family factors such as patients refusing to safety plan or caregivers not feeling comfortable taking a child home. One PES provider described, “The number one barrier (to changing a disposition plan once a patient is boarding) is parents feeling terrified about safety. Once the highest level of care is suggested, it is often really hard for parents to understand how they can safely take the patient home.” An extension of the inability to provide therapeutic intervention was the absence of resources to provide family level interventions. One CL provider added, “There is no re-routing kids without family work. We don’t have physical space to attend to that; we don’t have physical space or resources to have family meetings and safety plan.” Other challenges affecting discharge include complex patient needs such as those involved with other systems (e.g., DCYF or group-homes). Children were often first brought to the ED when their current services could no longer meet their needs. This placed the burden on the boarding process to maintain the child’s safety while coordinating adequate services. Disposition limitations for gender minority patients was also identified as a pain point. Many inpatient, residential, and group home placements have restrictions based on sex and gender. This created an extra barrier for gender minority youth. Within the inpatient setting, one CL provider described the “discriminatory effects of rooming policies for gender diverse and gender fluid kids” which affected available options when coordinating placements. The multiple barriers to determining appropriate levels of care and disposition placements perpetuated the already lengthy wait time of boarding patients.
Discussion
The current study provided valuable insights into the boarding of pediatric psychiatric patients from the perspective of staff facilitating the process. Chart review data demonstrated a more than three-fold increase in the number of patients admitted to board over the past three years, highlighting the rapid increase in this crisis. Moreover, nearly half of the most recent (2021) patients presenting to the ED for psychiatric reasons were admitted to board while awaiting a higher level of psychiatric care. The average time spent awaiting disposition was more than three days on average. Time spent boarding in the ED increased 60% in 2021, compared to two years prior, while time spent boarding on a medical floor decreased somewhat during that same time period. Overall, our data was consistent with other studies that have identified an excessive wait time of 20–40 hours on average for patients who are boarding, which grossly exceeds the Joint Commission’s standard recommendation for disposition within four hours (Leyenaar et al., 2021; Zeller et al., 2014).
The development of a patient journey map provided a snapshot of how care was delivered for acute pediatric psychiatric patients in an ED and primary medical setting. This tool can be used to develop more effective interventions and promote more efficient processes in emergency settings. The study identified the main phases of the patient journey through the local ED (Initial Evaluation, Admission to Board, Discharge) and further explored the positive and negative components of each phase based on providers’ reports. Results demonstrated that although the system was not specifically designed to support the acute needs of pediatric patients experiencing psychiatric crises, providers and staff were reaching the critical goal of maintaining safety for these high-risk youth while they awaited specialized psychiatric placement. Bright spots included supportive team functioning, collaboration, and communication. The current journey mapping approach provided a snapshot of the delivery of care and helped illustrate contributing factors to these excessive wait times that may be targets for future quality improvement initiatives in emergency settings.
In developing this patient journey map, we recognize there are other contributing factors that impede a patient’s journey throughout the emergency psychiatric healthcare system both before the patient presents to the emergency room and after discharge. Though change is needed in contributing systems that support youth mental health such as schools, social service agencies, and insurance coverage, understanding the factors within hospital and ED systems that perpetuate this boarding crisis can help healthcare systems set both universal and facility-specific quality improvement goals that may enhance patient experiences and improve the quality of care.
Throughout the interviews, several suggestions were made by staff which may improve the patient journey through the boarding process. Several providers identified inadequate staffing and training as a pain point in providing care for patients who are boarding. Some of these challenges may be addressed through training non-psychiatric medical staff in de-escalation and emotion regulation strategies as well as behavior management techniques to prevent reinforcing negative patient behaviors. Medical staff, including nurses, may also benefit from universal training in safety planning procedures that may equip patients and families to better cope with distress and to prevent psychiatric crises. Other studies have demonstrated the effectiveness of training nurses and other medical staff in similar brief interventions (Wolff et al., 2018). Along these lines, a bright point identified was the recent hiring of support staff (e.g., PBIs) to help deliver basic psychiatric interventions, such as coping strategies. Additional support staff may also be able to assist with care coordination activities such as communicating with families and identifying openings in outside agencies. In addition, telehealth or online interventions that have empirical support could be helpful adjunctive services that can be utilized while patients are boarding to provide psychoeducation and treatment strategies for both youth and caregivers.
The assessment process for patients who are boarding may also warrant change to streamline disposition planning and minimize wait times. The standardized assessment of suicide in the ED was seen as a bright spot; however, there was no standardized assessment for aggression or homicidality in place. This could have led to idiosyncrasies in mental status assessment and disposition planning. Evaluating these important risk factors may bolster self-efficacy in provider decision-making and inform methods to target stabilization as indicated. Standardizing daily care assessments may be particularly important given the many players involved in managing the care of patients who are boarding, especially trainees who may feel more empowered to advocate for discharge with reference to standardized measures of risk factors over the course of care.
Additionally, innovations to increase ED efficiency may include the development of a centralized database of mental health care options within a given catchment area that includes hospital-based and community clinics with real-time updates on openings, wait times, accepted insurance and payment options, and information about services and eligibility. The current approach to disposition planning can lead to confusion, frustration, disparities in access to care, and anomalous decision-making procedures influenced by any given provider’s knowledge of services (or lack thereof), bias, or time constraints. A centralized referral system, paired with initiatives to provide education to families regarding the pros and cons of various levels of care, may help to streamline disposition planning and manage expectations and considerations of importance for families.
Limitations
Several study limitations should be noted. The current study conducted interviews with medical providers and did not gather information from the perspective of youth or their families. While the current study described components of the journey for these youth, their first-hand accounts are glaringly absent from the literature and worthy of future research. In addition, the current study was conducted at a single academic medical facility that is a standalone children’s hospital. Similar facilities may find variations in the boarding process and results may not apply to general or community hospitals where most youth receive care for acute mental health services (Santillanes et al., 2020). Finally, it should be noted that the journey map did not extend to factors before patients present to the ED (e.g., appropriateness of school referrals, availability of mental health treatment) or systems outside the ED setting that contribute to the bottleneck (e.g., extended lengths of stay on inpatient units, lack of social service agency support).
Conclusion
This study aimed to provide insight into the pediatric psychiatric boarding crisis from the perspective of staff involved in the patient journey. The study identified three phases of this journey through the boarding process and provided insight into the positive and negative components of each phase. The insight gained from this study can be used to develop interventions and system-wide changes which address the challenges to the boarding crisis in the future.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jennifer C. Wolff, Email: Jennifer_Wolff@brown.edu
Micaela Maron, Email: micaela_maron@brown.edu.
Tommy Chou, Email: po-hun_chou@brown.edu.
Erik Hood, Email: erik_hood@brown.edu.
Sophia Sodano, Email: sophia_sodano@brown.edu.
Shayna Cheek, Email: shayna1cheek@gmail.com.
Elizabeth Thompson, Email: elizabeth_thompson@brown.edu.
Kathleen Donise, Email: kdonise@lifespan.org.
Emily Katz, Email: EKatz1@lifespan.org.
Margaret Mannix, Email: margaret_mannix@brown.edu.
References
- Alakeson V, Pande N, Ludwig M. A plan to reduce emergency room ‘Boarding’ of psychiatric patients. Health Affairs. 2010 doi: 10.1377/hlthaff.2009.0336. [DOI] [PubMed] [Google Scholar]
- Andersen H, Røvik KA, Ingebrigtsen T. Lean thinking in hospitals: is there a cure for the absence of evidence? A systematic review of reviews. British Medical Journal Open. 2014;4(1):e003873. doi: 10.1136/bmjopen-2013-003873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bearnot B, Mitton JA. “You’re always jumping through Hoops”: Journey mapping the care experiences of individuals with opioid use disorder-associated Endocarditis. Journal of Addiction Medicine. 2020 doi: 10.1097/ADM.0000000000000648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell M, Pierce J. A retrospective analysis of boarding times for adolescents in psychiatric crisis. Social Work in Health Care. 2018 doi: 10.1080/00981389.2018.1434586. [DOI] [PubMed] [Google Scholar]
- Cancilliere MK, Donise K. A Comparison of Acute Mental Health Presentations to Emergency Services Before and During the COVID-19 Pandemic. Rhode Island Medical Journal. 2022;105(4):9–15. [PubMed] [Google Scholar]
- Cloutier RL, Marshaall R. A dangerous pandemic pair: Covid19 and adolescent mental health emergencies. The American Journal of Emergency Medicine. 2021 doi: 10.1016/j.ajem.2020.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowe C, Collie C, Johnson C, Stirman W, S, An intervention mapping process to increase evidence-based psychotherapy within a complex healthcare system. American Psychologist. 2020 doi: 10.1037/amp0000631. [DOI] [PubMed] [Google Scholar]
- Elo S, Kyngäs H. The qualitative content analysis process. Journal of Advanced Nursing. 2008;62(1):107–115. doi: 10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- Fegert JM, Vitiello B, Plener PL, Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child and Adolescent Psychiatry and Mental Health. 2020 doi: 10.1186/s13034-020-00329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galloway D. Mapping work processes. ASQC Quality Press; 1994. [Google Scholar]
- Goldenberg MN, Parwani V. Psychiatric emergency department volume during Covid-19 pandemic. The American Journal of Emergency Medicine. 2021 doi: 10.1016/j.ajem.2020.05.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill RM, Rufino K, Kurian S, Saxena J, Saxena K, Williams L. Suicide ideation and attempts in a pediatric emergency department before and during COVID-19. Pediatrics. 2021 doi: 10.1542/peds.2020-029280. [DOI] [PubMed] [Google Scholar]
- Husebø SE, Olsen ØE. Impact of clinical leadership in teams’ course on quality, efficiency, responsiveness and trust in the emergency department: study protocol of a trailing research study. British Medical Journal Open. 2016;6(8):e011899. doi: 10.1136/bmjopen-2016-011899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim B, Rodrigues S, Dell NS, Elwy R. Process mapping appointments to identify improvements in care delivered to patients who screen positive for depression. European Journal for Person Centered Healthcare. 2016;4(3):433. doi: 10.5750/ejpch.v4i3.1097. [DOI] [Google Scholar]
- Kudinova AY, Bettis AH, Thompson EC, Thomas SA, Nesi J, Erguder L, MacPherson HA, Burke TA, Wolff JC. COVID-19 related daily stressors, coping, and suicidal ideation in psychiatrically hospitalized youth. Child and Youth Care Forum. 2021 doi: 10.1007/s10566-021-09641-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushniruk A, Borycki EM, Parush A. A case study of patient journey mapping to identify gaps in healthcare: Learning from experience with cancer diagnosis and treatment. Knowledge Management & E-Learning: An International Journal. 2020 doi: 10.34105/j.kmel.2020.12.022. [DOI] [Google Scholar]
- Kyngäs H. Inductive Content Analysis. In: Kyngäs H, Mikkonen K, Kääriäinen M, editors. The Application of Content Analysis in Nursing Science Research. Springer International Publishing; 2020. pp. 13–21. [Google Scholar]
- Leyenaar JK, Freyleue SD, Bordogna A, Wong C, Penwill N, Bode R. Frequency and duration of boarding for pediatric mental health conditions at acute care hospitals in the US. Journal Of The American Medical Association. 2021;326(22):2326. doi: 10.1001/jama.2021.18377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo CB, Bridge JA, Shi J, Ludwig L, Stanley RM. Children’s mental health emergency department visits: 2007–2016. Pediatrics. 2020;145(6):e20191536. doi: 10.1542/peds.2019-1536. [DOI] [PubMed] [Google Scholar]
- Nicks BA, Manthey DM. The impact of psychiatric patient boarding in emergency departments. Emergency Medicine International. 2012 doi: 10.1155/2012/360308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power E, Hughes S, Cotter D, Cannon M. Youth mental health in the time of COVID-19. Irish Journal of Psychological Medicine. 2020;37(4):301–305. doi: 10.1017/ipm.2020.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santillanes G, Axeen S, Lam CN, Menchine M. National trends in mental health-related emergency department visits by children and adults, 2009–2015. The American Journal of Emergency Medicine. 2020 doi: 10.1016/j.ajem.2019.12.035. [DOI] [PubMed] [Google Scholar]
- Schouten B, Driesen BEJM, Merten H, Burger BHCM, Hartjes MG, Nanayakkara PWB, Wagner C. Experiences and perspectives of older patients with a return visit to the emergency department within 30 days: Patient journey mapping. European Geriatric Medicine. 2021 doi: 10.1007/s41999-021-00581-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson EC, Thomas SA, Burke TA, Nesi J, MacPherson HA, Bettis AH, Kudinova AY, Affleck K, Hunt J, Wolff JC. Suicidal thoughts and behaviors in psychiatrically hospitalized adolescents pre- and post- COVID-19: A historical chart review and examination of contextual correlates. Journal of Affective Disorders Reports. 2021 doi: 10.1016/j.jadr.2021.100100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trebble TM, Hansi N, Hydes T, Smith MA, Baker M. Process mapping the patient journey: An introduction. Bmj. 2010;341(aug13 1):c4078–c4078. doi: 10.1136/bmj.c4078. [DOI] [PubMed] [Google Scholar]
- Vears DF, Gillam L. Inductive content analysis: A guide for beginning qualitative researchers. Focus on Health Professional Education: A Multi-Professional Journal. 2022;23(1):111–127. doi: 10.11157/fohpe.v23i1.544. [DOI] [Google Scholar]
- Yard E, Radhakrishnan L, Ballesteros MF, Sheppard M, Gates A, Stein Z, Hartnett K, Kite-Powell A, Rodgers L, Adjemian J, Ehlman DC, Holland K, Idaikkadar N, Ivey-Stephenson A, Martinez P, Law R, Stone DM. Emergency Department visits for suspected suicide attempts among persons aged 12–25 years before and during the COVID-19 Pandemic—United States, January 2019–May 2021. MMWR Morbidity and Mortality Weekly Report. 2021;70(24):888–894. doi: 10.15585/mmwr.mm7024e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff Jennifer C., Frazier Elisabeth A., Weatherall Sarah L., Thompson Alysha D., Liu Richard T., Hunt Jeffrey I. Piloting of COPES: An Empirically Informed Psychosocial Intervention on an Adolescent Psychiatric Inpatient Unit. Journal of Child and Adolescent Psychopharmacology. 2018;28(6):409–414. doi: 10.1089/cap.2017.0135. [DOI] [PubMed] [Google Scholar]
- Zeller S, Calma N, Stone A. Effect of a regional dedicated psychiatric emergency service on boarding and hospitalization of psychiatric patients in area emergency departments. Western Journal of Emergency Medicine. 2014;15(1):1–6. doi: 10.5811/westjem.2013.6.17848. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.