Dear Editor,
Suicide is a major problem in modern society. About 800,000 people kill themselves annually worldwide (Kim, 2021). In particular, with the recent COVID-19 pandemic, there is growing concern about the increased risk of suicide due to the aftereffects of COVID-19 infection (Tandon, 2021). Suicide and non-fatal self-harm cost nearly $490 billion in medical expenses, work-loss costs, and quality-of-life costs in 2019 (Peterson et al., 2021). As latitude increases, cumulative sunlight exposure decreases. Reduced sunlight exposure could increase mood disorders, such as depression, which may be considered a cause of suicide (Kim et al., 2021). Therefore, we aimed to analyze the global prevalence of suicide by latitude.
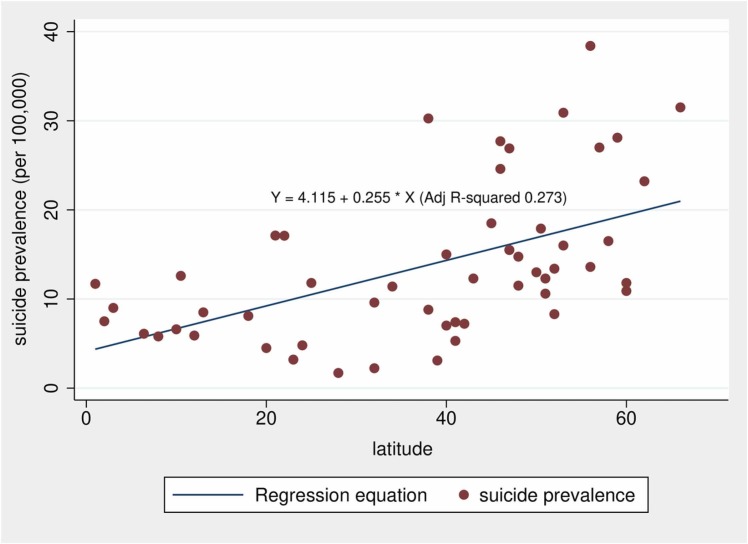
The detailed methodology of this study is presented in the Supplementary text. Twenty cross-sectional studies covering 40,694–74,652,466 participants published from 1982 to 2020 were used for analysis. A PRISMA flow diagram is shown in Supplementary Fig. 1. The characteristics and risk of bias assessment are summarized in Supplementary Tables 1 and 2, respectively. The overall weighted average suicide prevalence of this study was 13.34 (11.41–15.26) (Supplementary Fig. 2). The weighted average suicide prevalence was 8.12 (6.77–9.47) in the 0–14°, 8.54 (2.92–14.15) in the 15–29°, 9.97 (6.29–13.65) in the 30–44°, 19.23 (16.67–21.80) in the 45–59°, and 15.28 (9.12–21.44) in the 60–75°. As a result of the regression analysis, the beta coefficient was 0.255, which means that for every 1° increase, the suicide prevalence increased by 0.255 per 100,000 people ( Fig. 1). The regression model with latitude change explained approximately 27.3% of the suicide prevalence (adjusted R-squared, 0.273).
Fig. 1.
Regression analysis of global prevalence of suicide by latitude.
The global suicide prevalence in men was 11.93 (10.38–13.48) in the 0–14°, 15.04 (4.34–25.73) in the 15–29°, 13.38 (9.21–17.55) in the 30–44°, 33.43 (28.51–17.65) in the 45–59°, and 16.64 (15.72–17.56) in the 60–75° (Supplementary Fig. 3). The global suicide prevalence in women was 4.20 (3.02–5.38) in the 0–14°, 3.94 (2.02–5.86) in the 15–29°, 3.95 (3.11–4.80) in the 30–44°, 7.17 (6.01–8.33) in the 45–59°, and 6.29 (5.34–7.25) in the 60–75° (Supplementary Fig. 4).
According to subgroup analyses performed in median latitude (30–59°), the weighted average global suicide prevalence in men was 25.91 (21.90–29.92), and the weighted average global suicide prevalence in women was 5.66 (5.00–6.33) (Supplementary Fig. 5). The global suicide prevalence was 15.40 (12.7–18.10) in the gun-permissive countries and 16.46 (95 % CI 9.52–23.40) in the gun-control countries (Supplementary Fig. 6). The global suicide prevalence was 1.43 (1.04–3.90) in the 0–14 age, 3.25 (0.79–5.71) in the 15–24 age, 4.95 (0.54–9.37) in the 25–34 age, 5.84 (1.65–10.04) in the 35–44 age, 7.37 (4.31–10.44) per in the 45–54 age, 9.39 (7.06–11.72) in the 55–64 age, and 15.97 (10.18–21.76 in the 65–74 age (Supplementary Fig. 7). The global suicide prevalence was 13.68 (8.71–18.64) in the lower-middle income countries, 22.68 (17.60–27.76) in the upper-middle income countries, 12.72 (9.59–15.86) in the high-income countries (Supplementary Fig. 8).
According to weighted average analysis, the global suicide prevalence tended to increase according to latitude, such as 8.12, 8.54, 9.97, 19.23, and 15.28, except for the 60–75°. Regression analysis showed a positive linear association between latitude and suicide prevalence. A serotonin neurotransmitter has been proposed as a candidate pathway explaining the biological plausibility of sun exposure and suicide (Vyssoki et al., 2014). Low sunlight exposure reduces serotonin neurotransmitter binding in blood platelets and the brain, and this condition could increase impulsive aggressive traits and mood disorders like depression (Vyssoki et al., 2014).
Suicide ideation and behavior were more frequent in women, while mortality from suicide was much higher in men, which is called the gender paradox in suicide (Canetto and Sakinofsky, 1998). The causes were explained by the fatality of suicide methods, recall bias, rates of depression and alcohol abuse, and cultural acceptability of suicide (Canetto and Sakinofsky, 1998). According to Sloan et al. (1990), there was no difference in overall suicidal prevalence according to the degree of firearm regulation in both regions, but the prevalence of suicide by firearm was significantly higher in the gun-permissible region (Sloan et al., 1990). However, there is a large body of evidence that gun control lowers the total suicide prevalence (Lewiecki and Miller, 2013), so the generalization of our results should be cautious. In the subgroup analysis by age, it may be inferred that the suicide prevalence increased as the probability of exposure to risk factors, such as social isolation, economic poverty, and health abnormalities, increased with age (Conejero et al., 2018). The suicide prevalence may be affected not only by income level but also by various confounding variables such as race, religion, and vital registration system (WHO, 2014).
We found that the suicide global prevalence tended to increase as latitude increased. It may partially be explained by the difference in sun exposure according to latitude.
CRediT authorship contribution statement
Seongjun An: Methodology, Investigation, Formal analysis, Data curation, Writing – original draft. Sungju Lim: Methodology, Investigation, Formal analysis, Data curation, Writing – original draft. Hyun-Woo Kim: Conceptualization, Methodology, Supervision. Hyung-Sik Kim: Software, Validation, Visualization. Dongjun Lee: Software, Validation, Visualization. Eunjeong Son: Methodology, Formal analysis. Tae Woo Kim: Methodology, Formal analysis. Tae Sik Goh: Methodology, Formal analysis, Supervision. Kihun Kim: Conceptualization, Visualization, Project administration, Writing – review & editing, Supervision. Yun Hak Kim: Conceptualization, Visualization, Project administration, Funding acquisition, Writing – review & editing, Supervision. The manuscript has been read and approved by all named authors.
Financial Disclosure
This work was supported by the Medical Research Center (MRC) program through the National Research Foundation of Korea (2018R1A5A2023879) and the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI) (HI22C1377), funded by the Ministry of Health & Welfare, Republic of Korea.
Conflict of Interest
All authors have none to declare.
Acknowledgement
Not applicable.
Data Availability statement
Data sharing is not applicable to this article, as no datasets were generated or analyzed in this study.
Footnotes
PROSPERO registration number: CRD42021252706.
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.ajp.2023.103454.
Appendix A. Supplementary material
Supplementary material.
References
- Canetto S.S., Sakinofsky I. The gender paradox in suicide. Suicide Life‐Threat. Behav. 1998;28:1–23. [PubMed] [Google Scholar]
- Conejero I., Olié E., Courtet P., Calati R. Suicide in older adults: current perspectives. Clin. Interv. Aging. 2018;13:691. doi: 10.2147/CIA.S130670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim A.M. A relationship between abortion and suicide rates: a cross-sectional analysis of 62 countries. Asian J. Psychiatry. 2021;65 doi: 10.1016/j.ajp.2021.102821. (e102821-e102821) [DOI] [PubMed] [Google Scholar]
- Kim S.Y., Bang M., Wee J.H., Min C., Yoo D.M., Han S.-M., Kim S., Choi H.G. Short-and long-term exposure to air pollution and lack of sunlight are associated with an increased risk of depression: a nested case-control study using meteorological data and national sample cohort data. Sci. Total Environ. 2021;757 doi: 10.1016/j.scitotenv.2020.143960. [DOI] [PubMed] [Google Scholar]
- Lewiecki E.M., Miller S.A. Suicide, guns, and public policy. Am. J. Public Health. 2013;103:27–31. doi: 10.2105/AJPH.2012.300964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson C., Miller G.F., Barnett S.B.L., Florence C. Economic cost of injury—United States, 2019. Morb. Mortal. Wkly. Rep. 2021;70:1655. doi: 10.15585/mmwr.mm7048a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloan J.H., Rivara F.P., Reay D.T., Ferris J.A., Kellermann A.L. Firearm regulations and rates of suicide: a comparison of two metropolitan areas. N. Engl. J. Med. 1990;322:369–373. doi: 10.1056/NEJM199002083220605. [DOI] [PubMed] [Google Scholar]
- Tandon R. COVID-19 and suicide: just the facts. Key learnings and guidance for action. Asian J. Psychiatry. 2021;60 doi: 10.1016/j.ajp.2021.102695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vyssoki B., Kapusta N.D., Praschak-Rieder N., Dorffner G., Willeit M. Direct effect of sunshine on suicide. JAMA Psychiatry. 2014;71:1231–1237. doi: 10.1001/jamapsychiatry.2014.1198. [DOI] [PubMed] [Google Scholar]
- WHO, 2014. Preventing suicide: a global imperative.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material.
Data Availability Statement
Data sharing is not applicable to this article, as no datasets were generated or analyzed in this study.