Abstract
Background & Aims:
EGJ outflow obstruction (EGJOO) per Chicago Classification v4.0 (CCv4.0) represents a high-resolution manometry (HRM) diagnosis with uncertain clinical significance. This study aimed to evaluate FLIP Panometry among patients with EGJOO on HRM/CCv4.0 to assess clinical/manometric associations and treatment outcomes.
Methods:
An observational cohort study was performed on patients that completed FLIP during endoscopy and had an HRM/CCv4.0 diagnosis of EGJOO, i.e. HRM-EGJOO (inconclusive). Abnormal FLIP Panometry motility classifications were applied to identify FLIP-confirmed ‘conclusive EGJOO’. Rapid drink challenge on HRM and timed barium esophagram were also assessed. Clinical management plan was determined by treating physicians and assessed via chart review. Clinical outcome was defined using the Eckardt score (ES) during follow-up evaluation: ES<3 was considered a good outcome.
Results:
Of 139 adult patients with manometric EGJOO (inconclusive per CCv4.0), a treatment outcome ES was obtained in 55 after ‘achalasia-type’ treatment (i.e. pneumatic dilation, peroral endoscopic myotomy, laparoscopic Heller’s myotomy (LHM), or botulinum toxin injection) and 36 patients after other ‘non-achalasia-type’ treatment. Among patients with ‘conclusive EGJOO’ by HRM-FLIP complementary impression, 77% (33/43) had a good outcome after achalasia-type treatment, while 0% (0/12) of patients had a good outcome after non-achalasia-type treatment. Of patients with normal EGJ opening on FLIP, 1/3 patients treated with achalasia-type treatment had a good outcome while 9/10 treated conservatively had a good outcome.
Conclusions:
FLIP Panometry provides a useful complement to clarify the clinical significance of an HRM/CCv4.0 EGJOO diagnosis and help direct management decisions.
Keywords: dysphagia, achalasia, spasm, impedance
Introduction
Esophagogastric junction (EGJ) outflow obstruction (EGJOO) is a manometric classification defined by abnormal EGJ outflow pressures (i.e. elevated integrated relaxation pressure (IRP)) with presence of esophageal peristalsis.1, 2 This high-resolution manometry (HRM) classification creates clinical challenges as it is associated with a variety of different clinical diagnoses including achalasia (variant or early form), mechanical obstruction, hiatal hernia, or even a false positive HRM related to pressure artifact.3, 4 Recognizing the heterogeneous nature of HRM-EGJOO, the recent update to the Chicago Classification (CCv4.0) incorporated additional parameters to improve the clinical relevance of this HRM pattern.1, 3 However, while it was noted that additional findings from provocative HRM maneuvers such as a rapid drink challenge (RDC) may be utilized to complement the baseline HRM classification, CCv4.0 recommended that the HRM-EGJOO classification always be considered clinically ‘inconclusive’. Further, it was advised that additional testing with barium esophagram or functional lumen imaging probe (FLIP) be utilized to confirm the clinical relevance of the diagnosis (i.e. identify ‘clinically-relevant EGJOO’), especially prior to pursuing achalasia-type treatments.1, 3
We recently described an esophageal motility classification using FLIP Panometry.5 FLIP Panometry is the FLIP technique that displays esophageal diameter changes along a space-time continuum with associated pressure during a controlled volumetric distension protocol.5–7 Incorporating the evaluation of esophagogastric junction (EGJ) opening mechanics and the contractile response to distension, i.e. secondary peristalsis, yielded an evaluation of esophageal motility that often parallels conclusive diagnoses provided by HRM/CCv4.0. 5, 8, 9 Thus, we hypothesized that among patients with an HRM/CCv4.0 diagnosis of EGJOO, an abnormal FLIP Panometry motility assessment (i.e. one often observed among patients with a conclusive HRM diagnosis of achalasia) would represent a ‘conclusive’ clinically-relevant EGJOO with potential to be effectively treated akin to achalasia. Conversely, FLIP Panometry motility classifications involving normal EGJ opening likely reflect patients without true EGJ obstruction in which a conservative treatment approach would be preferred.
The aim of this study was to evaluate patients with manometrically-defined EGJOO (inconclusive per CCv4.0) and assess whether the complementary application of FLIP Panometry could identify clinically relevant phenotypes, such as normal EGJ opening versus conclusive EGJOO.
Methods
Subjects
Patients included this study are a subgroup of a previously described cohort 5, 8, 9 including adult patients (age 18–89) that presented to the Esophageal Center of Northwestern for evaluation of esophageal symptoms between November 2012 and December 2019 who were prospectively evaluated with data maintained in an esophageal motility registry. The larger cohort included consecutive patients evaluated for primary esophageal motility disorders (i.e. exclusion of patients with potential causes of secondary esophageal motor abnormalities such as previous foregut surgery or mechanical obstruction/esophagitis) that completed FLIP during sedated endoscopy and also a corresponding HRM. Patients with EGJOO on HRM per CCv4.0 were included as the focus of this study (Figure S1). Additional baseline clinical evaluation with timed barium esophagram (TBE) was obtained at the discretion of the primary treating gastroenterologist, as was the clinical treatment plan (described below). The study protocol was approved by the Northwestern University Institutional Review Board.
FLIP Study Protocol and Analysis
The FLIP study using 16-cm FLIP (EndoFLIP® EF-322N; Medtronic, Inc, Shoreview, MN) was performed during sedated endoscopy as previously described; expanded details are included in supplemental material.10–12 The FLIP study included stepwise 10-ml FLIP distensions (each stepwise distension volume being maintained for 30–60 seconds) with the FLIP catheter positioned across the EGJ (1–3 intragastric channels). The FLIP Panometry analysis was performed using a customized program (available open source at http://www.wklytics.com/nmgi) and focused on the 50ml, 60ml, and 70ml fill volumes. The FLIP Panometry analysis was performed blinded to clinical data including HRM, treatment plan, and outcome. As previously described and summarized in the Table 1, the contractile response (CR) pattern and classification of EGJ opening were applied to assign a FLIP Panometry motility classification.5, 8, 9 The CR pattern was assigned based on the presence of specific features and patterns of contractility that occurred over the course of the 50, 60, and 70ml fill volumes.8 The analysis of EGJ opening applied the EGJ distensibility index (DI) at the 60ml FLIP fill volume and the maximum EGJ diameter that was achieved during the 60ml or 70ml fill volume.9
Table 1.
Classification of esophageal motility with FLIP Panometry.
| Definition | |
|---|---|
| FLIP Panometry Contractile Response (CR) Patterns | |
| Normal Contractile Response | Repetitive Antegrade Contraction (RACs), defined by the RAC Rule of 6s: • ≥6 consecutive antegrade contractions of • ≥6 cm in axial length occurring at • 6+/−3 antegrade contractions per minute regular rate |
| Borderline Contractile Response | • Not meeting RAC Rule-of-6s • Distinct antegrade contractions of at least 6-cm axial length present • Not SRCR |
| Impaired/Disordered Contractile Response | • No distinct antegrade contractions • May have sporadic or chaotic contractions not meeting antegrade contractions • Not SRCR |
| Absent Contractile Response | • No contractile activity in the esophageal body |
| Spastic-Reactive Contractile Response (SRCR) | • Presence of any of the following features: • Sustained occluding contractions (SOC) or • Sustained lower esophageal sphincter (LES) contractions or • Repetitive retrograde contractions (RRCs), defined by at least 6 consecutive retrograde contractions occurring at a rate of > 9 contractions per minute |
| /// /// /// /// /// /// /// /// /// /// /// /// /// /// /// /// /// | |
| FLIP Panometry EGJ opening classification | |
| Reduced EGJ opening (REO) | • EGJ-DI <2.0 mm2/mmHg AND • Maximum EGJ diameter <12mm |
| Borderline EGJ opening (BEO) | • EGJ-DI <2.0 mm2/mmHg OR•Maximum EGJ diameter <16 mm, • but not REO ○ Further BEO classification: ○ Borderline-reduced if maximum EGJ diameter <14mm or ○ Borderline-normal if maximum EGJ diameter ≥14mm |
| Normal EGJ opening (NEO) | • EGJ-DI ≥2.0 mm2/mmHg AND • Maximum EGJ diameter ≥16mm |
| FLIP Panometry Motility Classifications | |
| Normal | • Normal EGJ opening and Normal CR or • Normal EGJ opening and Borderline CR ❖ Complementary application to HRM/CCv4.0 EGJOO = normal EGJ opening |
| Weak | • Normal EGJ opening and Impaired/disordered CR or • Normal EGJ opening and Absent CR ❖ Complementary application to HRM/CCv4.0 EGJOO = normal EGJ opening |
| Obstruction with weak CR | • Reduced EGJ opening and Impaired/disordered CR or • Reduced EGJ opening and Absent CR ❖ Complementary application to HRM/CCv4.0 EGJOO = conclusive EGJOO |
| Spastic-reactive | • Spastic-reactive CR • (any EGJ opening classification) ❖ Complementary application to HRM/CCv4.0 EGJOO = conclusive EGJOO |
| Inconclusive | • Reduced EGJ opening and borderline CR or • Borderline EGJ opening and normal CR, borderline CR, impaired/disordered CR, or absent CR (i.e. BEO and any CR except spastic-reactive) ❖ Complementary application to HRM/CCv4.0 EGJOO = inconclusive EGJOO |
The contractile response (CR) to distension was based on evaluation of the FLIP study protocol from the 50ml to 70ml fill volume. Esophagogastric junction (EGJ) opening applied the EGJ-distensibility index (DI) from the 60ml FLIP fill volume and the maximum EGJ diameter from the 60ml or 70ml FLIP fill volume. HRM – high-resolution manometry. CCv4.0 – Chicago Classification version 4.0. EGJOO – EGJ outflow obstruction.
The FLIP Panometry motility classification was then applied to create a CCv4.0 impression among this cohort of patients with EGJOO on HRM. Patients with EGJOO on HRM/CCv4.0 that had abnormal FLIP Panometry motility classifications of ‘obstruction with weak CR’ or ‘spastic-reactive’ were thus considered as ‘conclusive EGJOO’. Conversely, patients with a FLIP Panometry motility classification of normal or weak were considered ‘normal EGJ opening’. Inconclusive FLIP Panometry were described as inconclusive.
HRM protocol and analysis
After a minimum 6-hour fast, HRM studies were completed using a 4.2-mm outer diameter solid-state assembly with 36 circumferential pressure sensors at 1-cm intervals (Medtronic Inc, Shoreview, MN). The HRM assembly was placed transnasally and positioned to record from the hypopharynx to the stomach with approximately three intragastric pressure sensors. After a 2-minute baseline recording (during which the basal EGJ pressure was measured during end expiration), the HRM protocol was performed with ten, 5-ml liquid swallows in a supine position and with five 5-ml liquid swallows in an upright, seated position.1 Manometry studies were analyzed according to the CCv4.0 and independent of FLIP results.1, 3 The IRP, was measured for the 10 supine swallows and 5 upright swallows; median values for each position were applied. A median IRP of >15 mmHg was considered abnormal for supine swallows; a median IRP of >12 mmHg was considered abnormal for upright swallows.1 The patient cohort was defined by an HRM/CCv4.0 classification of EGJOO in patient meeting each of the following: a) elevated IRP in both the supine and upright positions, b) presence of intrabolus pressure >20mmHg in ≥20% of supine swallows, c) esophageal contractility present such that a criteria for a diagnosis of achalasia (subtypes I, II, or III) was not met, and d) a patient report of dysphagia or chest pain.1, 3 The primary peristalsis or contractility pattern was assigned based on the percentages of swallow types among the supine swallows.1
Most patient also completed an RDC during HRM. The RDC was completed in the seated, upright position and involved drinking 200cc liquid as rapidly as the patient was able. The RDC was analyzed by measurement of the IRP (using a 30-second measurement window from RDC onset), with an RDC-IRP >12mmHg considered abnormal, and for presence of panesophageal pressurization (PEP) at a 30mmHg isobaric contour.1, 13–15 The RDC-HRM was then categorized as ‘abnormal’ when both RDC-IRP was >12mmHg and PEP were present; ‘intermediate’ when RDC-IRP was >12mmHg or PEP were present (but not both); or ‘normal’ when RDC-IRP was ≤12mmHg and PEP was absent.
Additional baseline clinical evaluation
Timed barium esophagram (TBE) with barium tablet was obtained in patients at the discretion of the patients’ treating physicians. The barium column height above the EGJ was measured from images obtained at 1, 2 and 5 minutes after ingestion of 200 mL barium. If liquid barium cleared, a 12.5 mm barium tablet was also administered, and images obtained at timed intervals until passed into the stomach. TBE results were categorized for analysis based on the findings of greatest severity by: a) 5-minute column height >5cm, b) 1-minute column height >5cm or inability of the barium tablet to pass, or c) ‘normal’ (i.e. not meeting preceding severity criteria).
Most subjects completed validated self-reported symptom scores at the time of baseline testing with FLIP and HRM including, Brief Esophageal Dysphagia Questionnaire (BEDQ) and GerdQ.16, 17 The Eckardt score (ES) was also obtained with baseline testing (expanded below).18 Some patients chose not to complete the symptom questionnaires, and thus scores were not available for all subjects. For all three symptom scores, greater scores indicate greater symptom severity.
Treatment plans and clinical outcomes
Treatment plans and clinical outcomes were assessed via retrospective chart review. Treatment plans were completed under the direction of the patients’ primary treating gastroenterologist based on the cumulative baseline clinical evaluation. When completed treatment included pneumatic dilation (PD), per-oral endoscopic myotomy (POEM), laparoscopic Heller’s myotomy (LHM), or botulinum toxin injection it was considered as “achalasia-type” treatment. Other forms of treatment were considered as “non-achalasia treatment”. Non-achalasia treatments included reassurance/observation, acid suppressive therapy, off-label use of esophageal smooth muscle relaxants, GI-focused cognitive behavioral therapy, endoscopic dilation (≤20mm); and one patient in this cohort completed a hiatal hernia repair with Toupet fundoplication. However, given that multiple treatment modalities (often applied in parallel) were utilized, isolated treatment modalities and associated outcomes could not be assessed.
The ES obtained at follow-up after treatment was applied as the measure of clinical treatment outcome.19, 20 The ES includes four 4-point Likert scale questions (scored 0–3) that assess the frequency of dysphagia, chest pain, and regurgitation and the degree of weight loss, with items summed to yield a score of 0–12. Although an ES threshold of <4 has been applied in previous clinical trials, we defined a “good clinical outcome” by an ES <3 because an ES=3 often involves daily symptoms. Additionally, analysis was conducted focused on the only the dysphagia item score. The ES-dysphagia outcome was defined as “good” if scored 0 (no dysphagia) or 1 (occasional dysphagia) vs “poor” if scored 2 (daily dysphagia) or 3 (dysphagia with every meal). The standard treatment follow-up protocol at out center is to assess outcomes at 6–12 months post-treatment, particularly after pneumatic dilation, POEM, or laparoscopic Heller myotomy; if a follow-up ES was only available obtained outside of this timeframe, it was applied. An exception to this was after treatment with botulinum toxin injection in which a symptomatic outcome obtained at greater than 12 months was considered void (and thus as no outcome assessed) based on the waning effects of the botulinum toxin.
Statistical Analysis
Results were reported as mean (standard deviation; SD), or median (interquartile range; IQR) depending on data distribution. Groups were compared using Chi-square test for categorical variables and ANOVA/t-tests or Kruskal-Wallis/Mann-Whitney U for continuous variables, depending on data distribution. Test were two-sided as appropriate and all tests controlled the type I error rate at α = 5%; the Bonferroni correction was utilized to adjust for multiple comparisons.
Results
Subjects
139 patients, mean (SD) age 59 (15) years, 57% female with HRM-EGJOO (inconclusive) were included (Figure S1). Endoscopy findings among the cohort included small hiatal hernia in 13 patients (9%), low-grade erosive esophagitis in 3 (2 Los Angeles grade A, 1 grade B), and esophageal (e.g. epiphrenic) diverticulum in 7 patients (5%). The primary peristalsis / contractility pattern on HRM was premature in 25 patients (18%), hypercontractile in 28 (20%), ineffective in 14 (10%), and otherwise normal in 71 (52%). EGJ morphology on HRM was type I in 79% while 21% had a type II or type III EGJ morphology (i.e. possible or small hiatal hernia). Additionally, of the 125 patients that completed RDC with HRM (90% of cohort), an elevated RDC-IRP (>12mmHg) was observed in 61 (49%) and PEP during RDC in 45 (36%). TBE was completed in 64 patients (46% of cohort): 16 (25%) had a 5-minute column height >5cm, 25 (39%) had a 1-minute column height >5cm (n=18) or impaction of a barium tablet (n=7), and 23 (36%) had a normal TBE.
FLIP Panometry findings and complementary CCV4.0 impression among patients with HRM-EGJOO (inconclusive)
Among the HRM-EGJOO (inconclusive) cohort, the FLIP Panometry EGJ opening classifications were reduced EGJ opening (REO) in 67 patients (48%), borderline EGJ opening (BEO) in 42 (30%: 24 (17%) borderline-reduced; 18 (13%) borderline-normal), and normal EGJ opening (NEO) in 30 (22%). The FLIP CR patterns were normal CR in 8 (6%), borderline CR in 29 (21%), impaired/disordered CR in 60 (43%), absent CR in 23 (17%), and spastic-reactive CR in 19 (14%).
Applying both the EGJ and contractile response classifications, the FLIP Panometry motility classifications were ‘normal’ in 20 patients (14%) and ‘weak’ in 10 (7%) patients which yielded an impression of normal EGJ opening (i.e. refuted the HRM classification of EGJOO) in 21% of the cohort (Figure 1; Table 2). Abnormal FLIP motility classifications of ‘obstruction with weak CR’ was observed in 49 patients (35%) and ‘spastic-reactive’ was observed in 19 patients (14%), which supported a conclusive, clinically relevant EGJOO in 49% of the cohort. Finally, FLIP Panometry was inconclusive in 41 patients (29%).
Figure 1. Identification of conclusive, clinically relevant manometric EGJ outflow obstruction (EGJOO) using FLIP Panometry per Chicago Classification v4.0 (CCv4.0).
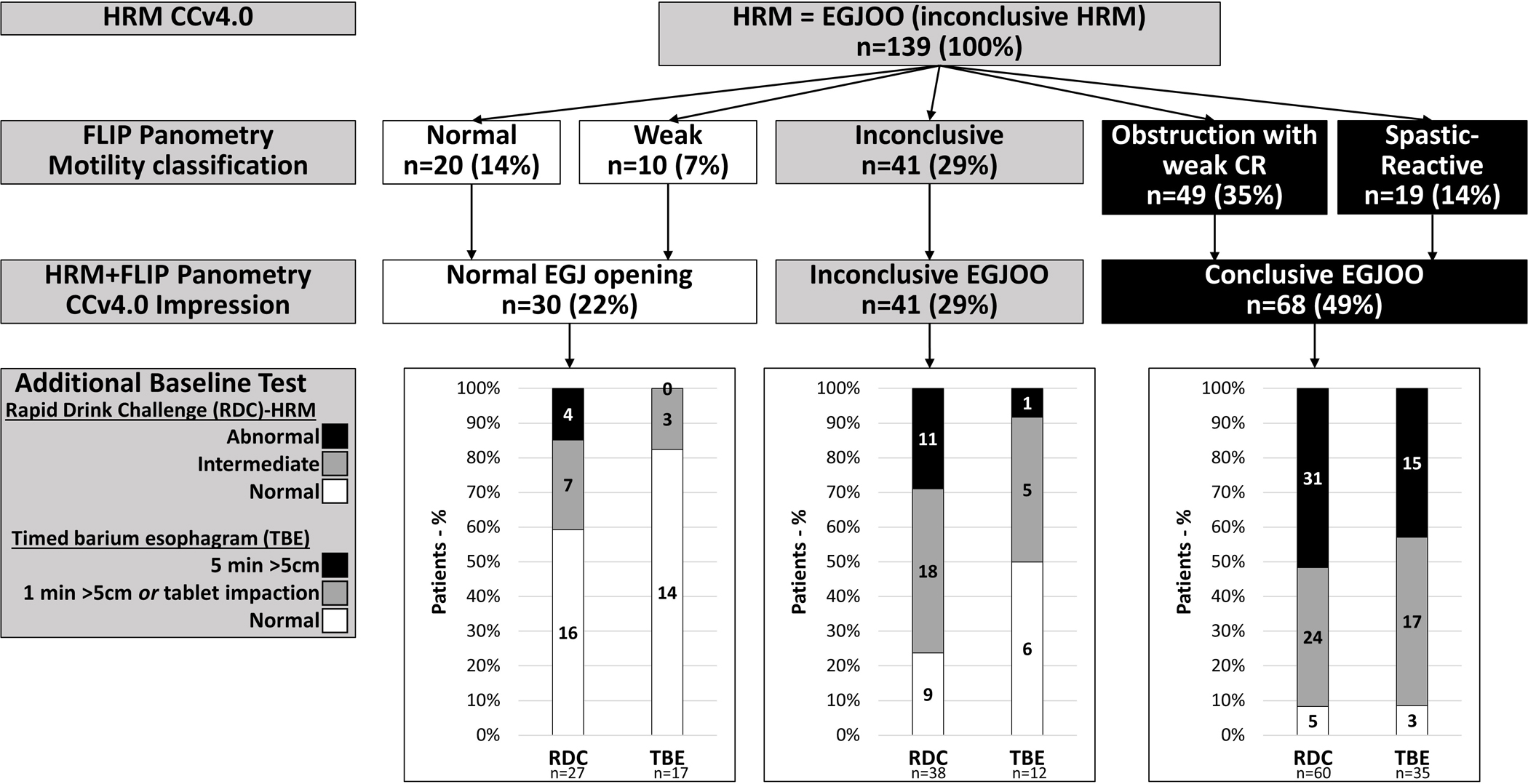
Criteria for FLIP Panometry classification are included in Table 1. The associated finding from other baseline tests (Rapid Drink Challenge (RDC) on HRM and Timed Barium Esophagram (TBE) relative to the complementary CCv4.0 HRM+FLIP Panometry impression are also displayed. Figure used with permission from the Esophageal Center of Northwestern.
Table 2.
Clinical characteristics by Chicago Classification v4.0 (CCv4.0) Impression of EGJ outflow obstruction (EGJOO) based on complementary application of high resolution manometry (HRM) and FLIP Panometry.
| HRM+FLIP Panometry CCv4.0 Impression | Normal EGJ opening | ‘Conclusive EGJOO’ | Inconclusive |
|---|---|---|---|
|
| |||
| Patient characteristics | |||
|
| |||
| n (%) | 30 (22) | 68 (49) | 41 (29) |
|
| |||
| Age, mean (SD) years | 56 (16) | 60 (14) | 60 (14) |
|
| |||
| Sex; n (%) female | 20 (67) | 34 (50) | 25 (61) |
|
| |||
| Baseline HRM | |||
|
| |||
| HRM, median supine IRP, mmHg, median (IQR)* | 22 (18–27) | 26 (22–34) | 22 (18–26) |
|
| |||
| HRM, median upright IRP, mmHg, median (IQR)** | 18 (14–24) | 29 (20–35) | 20 (17–27) |
|
| |||
| HRM, Basal EGJ pressure (end-expiration), mmHg, median (IQR) | 31 (18–39) | 32 (21–46) | 30 (19–36) |
|
| |||
| HRM EGJ morphology, n (%) | |||
| Type I | 20 (67) | 56 (82) | 34 (83) |
| Type II or III | 10 (33) | 12 (18) | 7 (17) |
|
| |||
| Intrabolus pressurization (IBP); Percent of supine swallows with IBP > 20mmHg, median (IQR)* | 80 (50–100) | 100 (70–100) | 100 (50–100) |
|
| |||
| HRM-primary peristalsis/contractility pattern, n (%)* | |||
| Normal | 26 (87) | 31 (46) | 22 (53) |
| Ineffective | 2 (7) | 6 (9) | 0 |
| Hypercontractile | 2 (7) | 11 (16) | 8 (20) |
| Premature | 1 (3) | 20 (29) | 11 (27) |
|
| |||
| HRM-rapid drink challenge (RDC) | |||
| [Completed RDC] | [n=27] | [n=60] | [n=38] |
| RDC-IRP, mmHg, median (IQR)** | 10 (5–13) | 15 (10–24) | 12 (9–16) |
| RDC-IRP > 12mmHg, n (%)* | 8 (29) | 37 (62) | 16 (42) |
| PEP>30mmHg, n (%)** | 7 (26) | 49 (82) | 24 (63) |
|
| |||
| Baseline Timed Barium Esophagram (TBE) | |||
|
| |||
| [Completed TBE] | [n=17] | [n=35] | [n=12] |
| I minute column height, cm, median (IQR) | 0 (0–4) | 13 (7–21) | 0 (0–4) |
| 5 minute column height, cm, median (IQR) | 0 (0–0) | 3 (0–13) | 0 (0–0) |
|
| |||
| Baseline symptom scores | |||
|
| |||
| [completed Eckardt score] | [n=23] | [n=47] | [n=34] |
| Eckardt score, median (IQR) | 4 (2–8) | 5 (3–8) | 5 (2–7) |
| Eckardt score ≥3, n (%) | 16 (70) | 41 (87) | 25 (74) |
| Eckardt dysphagia score, median (IQR) | 0 (0–1) | 1 (0–2) | 1 (0–2) |
| Eckardt dysphagia score ≥2, n (%) | 10 (40) | 32 (68) | 19 (56) |
|
| |||
| [completed BEDQ] | [n=25] | [n=51] | [n=36] |
| BEDQ score, median (IQR)* | 6 (4–17) | 16 (10–23) | 18 (9–23) |
| BEDQ score ≥10 n (%)* | 10 (40) | 40 (78) | 27 (75) |
|
| |||
| [completed GerdQ] | [n=24] | [n=46] | [n=31] |
| GerdQ score, median (IQR) | 9 (6–11) | 9 (8–10) | 7 (6–10) |
| GerdQ score ≥9, n (%) | 14 (58) | 29 (63) | 13 (42) |
P<0.05
P<0.001 on comparison between EGJOO impressions.
CR – contractile response; BEDQ - Brief Esophageal Dysphagia Questionnaire; IRP – integrated relaxation pressure; PEP – panesophageal pressurization.
Associations of baseline characteristics associated with complementary HRM+FLIP Panometry CCv4.0 EGJOO impression
Overall, other baseline findings (i.e. those not from FLIP) were less frequently abnormal among patients with a CCv4.0 HRM+FLIP Panometry impression of normal EGJ opening than in patients with conclusive EGJOO; Table 2. Characteristics associated with each FLIP Panometry motility classification among this EGJOO cohort are included in Table S1.
On baseline HRM, IRP values (on supine swallows, upright swallows, and with RDC) were lower in normal EGJ opening than conclusive EGJOO (P-values ≤0.004); Table 2. RDC-IRP was less frequently abnormal (29% vs 62%) and PEP less frequently present (26% vs 82%) in normal EGJ opening than conclusive EGJOO (Figure 1). The primary peristalsis/contractility pattern differed between CCv4.0 impressions of EGJOO such that normal primary peristalsis was observed in 87% of patients with normal EGJ opening vs 46% with conclusive EGJOO (Table 2). Further, hypercontractile or premature contractility patterns were observed in 10% of patients with normal EGJ opening vs 45% of patients with conclusive EGJOO. Of the 3 patients with normal EGJ opening and HRM with hypercontractile or premature contractility, two completed TBE and both were normal.
Among patients that completed TBE, the frequency of TBE findings differed by CCv4.0 HRM+FLIP Panometry impression (Figure 1). Of the patients with normal EGJ opening, zero had a 5-minute column >5cm, while 82% (14/17 patients) had a normal TBE. Among patients with conclusive EGJOO, a 5-minute column >5cm was observed in 43% (15/35 patients), while 9% (3/25) had a normal TBE.
Baseline symptom scores (BEDQ, GerdQ, ES) were completed in 112, 102, and 112 patients, respectively. Patients with normal EGJ opening reported less severe dysphagia (i.e. lower BEDQ scores) than those with conclusive EGJOO (P=0.008) with 40% (10/25 patients) of normal EGJ opening reporting severe dysphagia (BEDQ ≥10) vs 78% (40/51) with conclusive EGJOO; Table 2. Baseline GerdQ and ES were not statistically different.
Association of clinical treatment outcomes based on complementary HRM+FLIP Panometry CCv4.0 EGJOO impression
Among this HRM-EGJOO (inconclusive) cohort, 68 (49%) completed achalasia-type treatments: 14 pneumatic dilation, 24 POEM, 9 LHM, and 21 botulinum toxin injection (3 additional patients were treated initial with botulinum toxin, but with lack of response and subsequently treated with (and categorized as) pneumatic dilation (1) or POEM (2), Figure S1. A treatment outcome ES was obtained in 40 patients at mean (SD) 21 (14) months after PD (n=11), POEM (n=22), or LHM (n=7); in 15 patients at mean (SD) 6 (5) months after botulinum toxin injection, and 36 patients after mean (SD) 23 (14) months of non-achalasia treatment.
Among patients with normal EGJ opening, 1/3 (33%) with achalasia-type treatment (treated with botulinum toxin injection) had a good outcome, while 90% (9/10 patients) with non-achalasia type treatment had a good outcome (Figures 2 and 3). Among patients with a HRM+FLIP Panometry impression of ‘conclusive EGJOO’, 77% (33/43) had a good outcome after achalasia-type treatment, while 0% (0/12) patients had a good outcome after non-achalasia type treatment. Similar outcome results were observed if defining outcome with the Eckardt score dysphagia item (Figure S2).
Figure 2. Clinical outcomes by treatment approach and FLIP Panometry motility classification among patients with manometric EGJ outflow obstruction (EGJOO) per Chicago Classification v4.0.
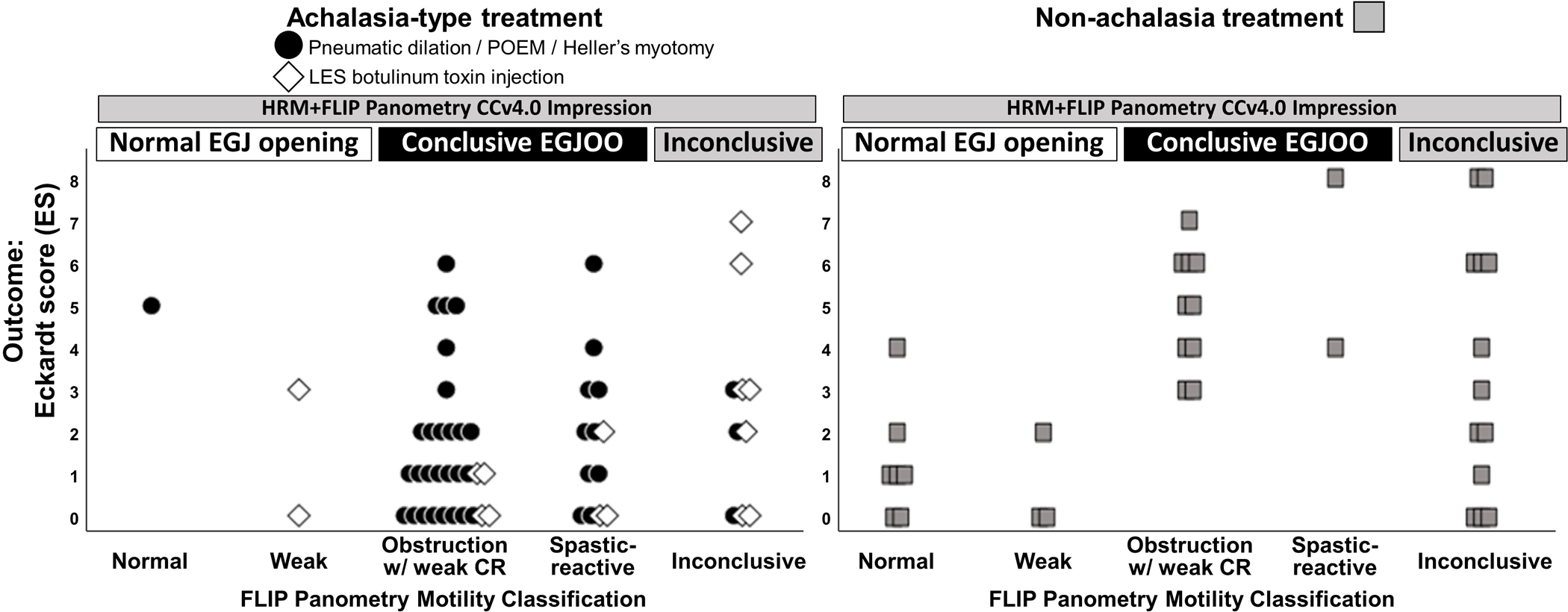
LES – lower esophageal sphincter; POEM – peroral endoscopic myotomy; CR – contractile response. Figure used with permission from the Esophageal Center of Northwestern.
Figure 3. Treatment outcomes by complementary evaluation of high-resolution manometry (HRM) – EGJ outflow obstruction (EGJOO) per the Chicago Classification v4.0 (CCv4.0).
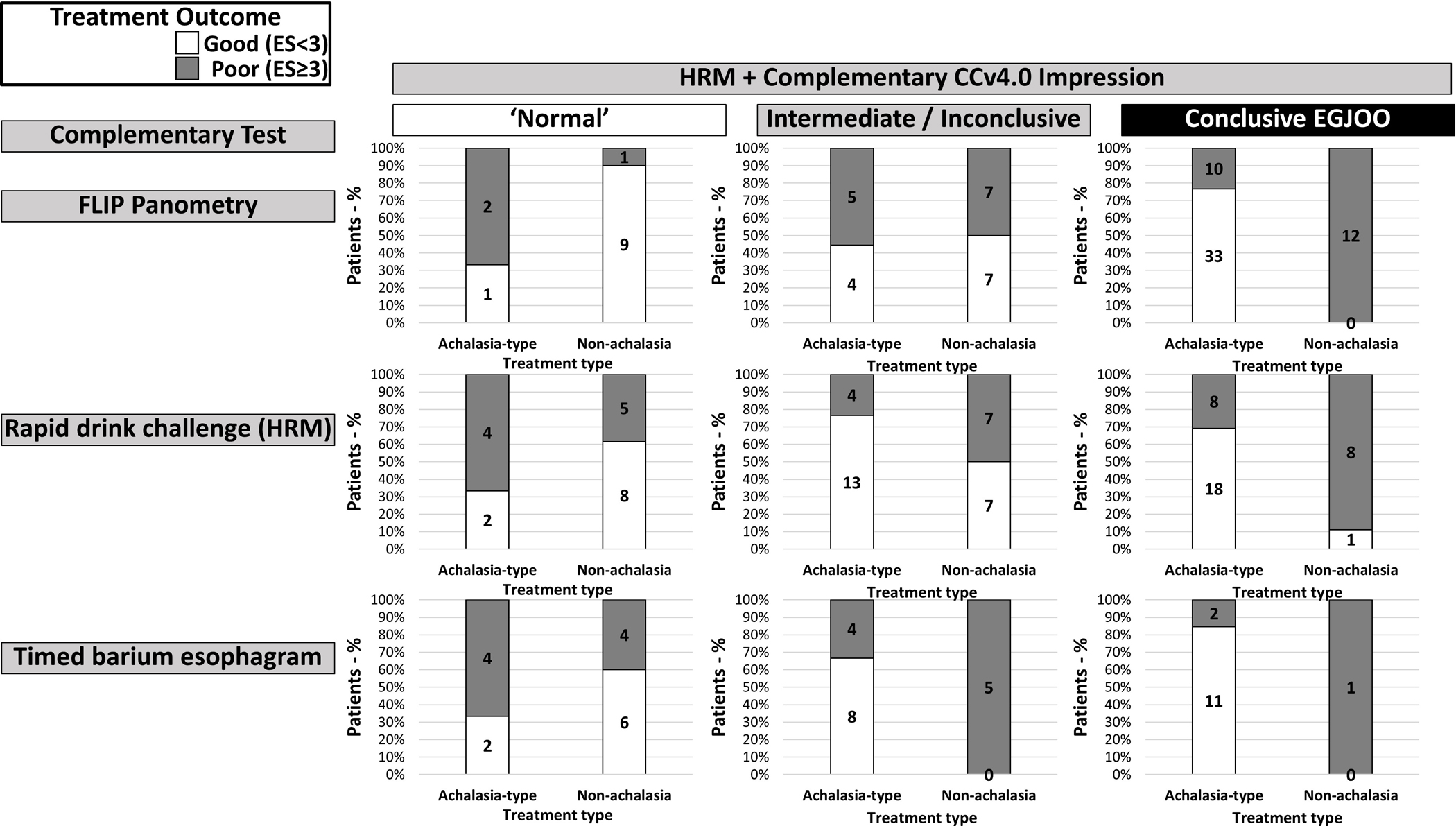
The HRM + complementary CCv4.0 impression (i.e. “normal”‘, “intermediate/inconclusive”, or “conclusive EGJOO”) was derived from the application of each individual complementary test: FLIP Panometry, rapid drink challenge (RDC) on HRM, or timed barium esophagram (TBE). Numbers within the bars indicate the number of patients relative to treatment and outcome for each test. ES – Eckardt score.
Additionally, among the patients initially managed with non-achalasia type treatments, 18 patients completed a repeat HRM at a mean (SD) 30 (11) months after the baseline HRM/FLIP (Table 3). Of these, progression to an HRM/CCv4.0 diagnosis of achalasia was observed in 6 patients (1 type I, 2 type II, and 3 type III achalasia), 4 of whom had a baseline HRM+FLIP Panometry impression of conclusive EGJOO; the other two had an inconclusive FLIP Panometry (Table 3). Both patients with normal FLIP Panometry at baseline did not have a disorder of EGJ outflow on follow-up,
Table 3.
Follow-up high resolution manometry (HRM) among patients without achalasia-type treatment.
| FLIP motility classification | Normal | Weak | Obstruction with weak CR | Spastic-reactive | Inconclusive |
|---|---|---|---|---|---|
| Repeat/follow-up HRM | |||||
| Progression (CCv4.0=Achalasia I, II, or III) | 0 | 0 | 3 (50) | 1 (17) | 2 (33) |
| Consistent (CCv4.0=EGJOO) | 0 | 0 | 2 (33) | 0 | 4 (67) |
| Resolution (CCv4.0=not disorder of EGJOO) | 2 (33) | 0 | 1 (17) | 0 | 3 (50) |
Values reflect n (%). CCv4.0 – Chicago Classification version 4.0. CR – contractile response. EGJOO – esophagogastric junction outflow obstruction.
Association of HRM-RDC and TBE findings with clinical outcome
The association of treatment outcomes was also assessed relative to baseline HRM-RDC and TBE findings (as available based on test completion); Figure 3 (jitter plots displaying individual patient outcomes relative to HRM-RDC and TBE are displayed in Figure S3).
If applying only the RDC-IRP, 61% (11/18) of patients with a normal RDC-IRP (<12mmHg) had a good outcome after achalasia-type treatment while 50% (11/22) had a good outcome after non-achalasia treatment. Of patients with an RDC-IRP ≥12mmHg, 39% (7/18) had a good outcome after achalasia-type treatment, while 36% (5/14) had a good outcome after non-achalasia treatment.
When categorizing RDC using IRP and presence of PEP, among patients with a normal HRM-RDC, 67% (4/6) had a poor outcome after achalasia-type treatment while 62% (8/13) had a good outcome after non-achalasia treatment (Figure 3; Figure S3). Among patients with an abnormal HRM-RDC, 69% (18/26) had a good outcome after achalasia-type treatment, while 89% (8/9) patients had a poor outcome after non-achalasia type treatment.
Among patients with a 5-minute column height >5cm on TBE, 85% (11/13) had a good outcome after achalasia-type treatment, while only one such patient was treated with non-achalasia type treatment and had a poor outcome (Figure 3; Figure S3). Of patients with a normal TBE, 67% (4/6) had a poor outcome after achalasia-type treatment while 60% (6/10) had a good outcome after non-achalasia treatment.
Discussion
The findings of this observational study of a 139 patient cohort with HRM-EGJOO (inconclusive per CCv4.0) suggest that motility assessment with FLIP Panometry provides a means to identify clinically relevant EGJOO and guide management in these challenging patients. Defining ‘conclusive EGJOO’ by the complementary finding of EGJ obstruction on FLIP Panometry, 77% of such patients reported significant clinical improvement following achalasia-type treatments. This compared to a high likelihood of no significant improvement in such patients with a conservative (‘non-achalasia’) treatment approach (12 of 12 patients). On the other hand, a FLIP Panometry finding of normal EGJ opening (contradicting the HRM-EGJOO classification), was associated with a good outcome with non-achalasia type treatment. Ultimately, however, EGJOO on HRM (even with the updated criteria in CCv4.0) remains associated with clinical heterogeneity and diagnostic uncertainty emphasizing the value of a comprehensive motility evaluation incorporating FLIP Panometry appears to guide management.
Refinement of the criteria for the HRM diagnosis for EGJOO was a major focus of CCv4.0 as it sought to identify clinically relevant cases among this heterogeneous group.1, 3 This study demonstrates success of CCv4.0 in this regard evident by the higher proportion of ‘achalasia-like’ HRM-EGJOO in this study compared to previous reports describing HRM EGJOO using diagnostic criteria from earlier versions of the CC.21, 22 Nonetheless, the ongoing heterogeneity of the HRM-EGJOO classification remains apparent, also supporting the CCv4.0 recommendation to always consider a HRM-EGJOO diagnosis clinically inconclusive pending complementary testing.1, 3 The present study represents advances in both the HRM classification of EGJOO attributable to CCv4.0 and the evolution of FLIP Panometry in esophageal motility diagnostics.1, 2, 5 These findings strengthen our earlier report suggesting utility of FLIP Panometry in identifying the subset of HRM EGJOO patients akin to achalasia-variants, likely to benefit from achalasia-type treatments.23
This study also demonstrated the complimentary nature of FLIP Panometry, TBE, and RDC on HRM in identifying clinically relevant EGJOO. Another recent observational study that evaluated treatment outcomes among patients with HRM-defined EGJOO also demonstrated the utility of provocative maneuvers on HRM (RDC and solid-test meals) to predict treatment outcome.15 In the present study, using CCv4.0 diagnostic criteria, the RDC appeared useful to predict treatment outcomes, though more so using both RDC-IRP and PEP (compared to only RDC-IRP). Another technical consideration with defining EGJOO entirely on the basis of an elevated IRP is that this metric can be influence by recording artefacts.24, 25 Thus as outlined in CCv4.0, utilizing HRM study protocols with supine and upright swallows, as well as incorporation of HRM pressurization patterns, appears essential.1, 3, 26 The previous study also suggested that barium esophagram had limited utility in predicting outcome among HRM-EGJOO, which differed from the findings of the present study.15 The performance of esophagram in the present study was likely enhanced by the utilization of the TBE protocol and barium tablet, protocol components that likely increase diagnostic yield of esophagram.27
Overall, while the benefit of comprehensive evaluation utilizing complementary tests are demonstrated in this study, none of the tests (including the baseline HRM) are perfect in isolation. Given the correlation demonstrated between FLIP Panometry, TBE, and HRM-RDC, the decisions regarding diagnostic evaluation plan for additional evaluation of an inconclusive EGJOO diagnosis on HRM involves balancing costs, local availability and experience, and patient preferences. This data supports including RDC among a standard HRM protocol, as needing to repeat HRM (if the initial HRM study did not include RDC) is likely undesirable to many patients. However, while RDC findings during an initial HRM can help set the degree of suspicion for a relevant EGJOO, neither a normal nor abnormal RDC would likely be sufficient to conclude a diagnostic evaluation. TBE, while requiring access and radiation exposure, provides substantial benefit when significantly abnormal (25% of this cohort), though diagnostic uncertainty may still persist if TBE is normal or indeterminate. And if a second look endoscopy, or endoscopy with potential for therapeutic intervention, is warranted, FLIP Panometry offers the potential to help direct treatment decision making at the time of that endoscopy. Further, FLIP performed with an initial (i.e. pre-HRM) endoscopy may subject an HRM unnecessary (particularly if FLIP Panometry is normal), and thus avoid the potential for an inconclusive EGJOO diagnosis all together.28
It is also worth acknowledging the challenge of having an inconclusive FLIP Panometry in a patient with an inconclusive HRM (i.e. EGJOO), a combination that occurred in 29% of this cohort (or intermediate RDC or TBE findings, which occurred in 39% and 39% of the cohort, respectively). Supportive findings of obstruction based on were also heterogeneous in this group, as were treatment outcomes. Among these patients, reliance on a full array of complementary testing with TBE and provocative maneuvers on HRM is likely necessary. Clearly, there is room for future work to further refine management approaches for these patients. Ultimately, when uncertainty of the clinical relevance of the EGJOO persists despite the application of a comprehensive evaluation, the prudent management decision involves a conservative management approach, reserving irreversible treatment options for those who demonstrate disease progression.
While this study carries strengths related to its application of novel diagnostic approaches to a challenging clinical cohort, it has limitations as well. Although this is the largest cohort study of HRM-EGJOO patients to date (uniformly defined by CCv4.0 criteria) and they were comprehensively evaluated, the observational study design carries inherent limitations. This includes the lack of random or blinded assignment of treatment plans, i.e. potential bias of treatment assignment based on test results and thus with outcomes subject to a potential self-fulfilling prophecy, and missing data points, particularly with patients lost to follow-up. The partial completion of TBE and RDC within the cohort also limited direct comparisons between these tests. Also, a variety of treatment approaches was also utilized, which reflects the heterogeneity of approaches to the HRM-EGJOO patient cohort, and also limits for evaluation of responses among treatments. The use of the ES as the primary outcome measure is also a limitation, even though it is frequently used as the primary outcome in clinical trials.19, 20 Nonetheless, this study provides valuable clinical data within the inherent limitations of an observational study.
In conclusion, there is value in incorporating complementary findings provided by a comprehensive esophageal motility evaluation including FLIP Panometry in the management of EGJOO patients. The isolated abnormal finding of an elevated IRP on an HRM study is inconclusive and its clinical relevance uncertain. However, findings supporting esophageal outflow obstruction from complementary FLIP Panometry, TBE, and/or RDC on HRM can help establish a clinical diagnosis of ‘conclusive EGJOO’ and help identify patients with potential to benefit from achalasia-like treatments. Though future study will likely refine the approach to these complex patients, this study further establishes the value of FLIP Panometry in the management of esophageal motility disorders.
Supplementary Material
STUDY HIGHLIGHTS.
WHAT IS KNOWN:
A diagnosis of esophagogastric junction outflow obstruction (EGJOO) on high-resolution manometry (HRM) is clinically inconclusive and requires additional testing to clarify its clinical relevance.
The Chicago Classification version 4.0 (CCv4.0) recommends additional testing with functional lumen imaging probe (FLIP) or barium esophagram to confirm the clinical relevance of the EGJOO on HRM.
WHAT IS NEW HERE:
FLIP Panometry facilitated identification of patients with conclusive, clinically relevant EGJOO with an association with treatment outcomes.
Timed barium esophagram and rapid drink challenge on HRM often had parallel findings with FLIP Panometry and treatment outcomes and thus also appeared to offer useful complementary evaluation for EGJOO.
Grant support:
This work was supported by P01 DK117824 (JEP) from the Public Health service and American College of Gastroenterology Junior Faculty Development Award (DAC).
Footnotes
Disclosures:
JEP, PJK, and Northwestern University hold shared intellectual property rights and ownership surrounding FLIP Panometry systems, methods, and apparatus with Medtronic Inc.
DAC: Medtronic (Speaking, Consulting); Phathom Pharmaceuticals (Consulting)
PJK: Ironwood (Consulting); Reckitt Benckiser (Consulting), Johnson & Johnson (consulting)
JEP: Sandhill Scientific/Diversatek (Consulting, Speaking, Grant), Takeda (Speaking), Astra Zeneca (Speaking), Medtronic (Speaking,Consulting, Patent, License), Torax (Speaking, Consulting), Ironwood (Consulting)
JMS, WK: none
References
- 1.Yadlapati R, Kahrilas PJ, Fox MR, et al. Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0((c)). Neurogastroenterol Motil. 2021;33(1):e14058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27(2):160–74.4308501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bredenoord AJ, Babaei A, Carlson D, et al. Esophagogastric junction outflow obstruction. Neurogastroenterol Motil. 2021:e14193. [DOI] [PubMed] [Google Scholar]
- 4.Babaei A, Szabo A, Yorio SD, Massey BT. Pressure exposure and catheter impingement affect the recorded pressure in the Manoscan 360 system. Neurogastroenterol Motil. 2018.PMC6129441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carlson DA, Gyawali CP, Khan A, et al. Classifying Esophageal Motility by FLIP Panometry: A Study of 722 Subjects With Manometry. Am J Gastroenterol. 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carlson DA, Lin Z, Rogers MC, Lin CY, Kahrilas PJ, Pandolfino JE. Utilizing functional lumen imaging probe topography to evaluate esophageal contractility during volumetric distention: a pilot study. Neurogastroenterol Motil. 2015;27(7):981–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carlson DA, Gyawali CP, Kahrilas PJ, et al. Esophageal motility classification can be established at the time of endoscopy: a study evaluating real-time functional luminal imaging probe panometry. Gastrointest Endosc. 2019;90(6):915–23 e1.PMC6875629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carlson DA, Baumann AJ, Prescott JE, et al. Validation of secondary peristalsis classification using FLIP panometry in 741 subjects undergoing manometry. Neurogastroenterol Motil. 2021:e14192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carlson DA, Prescott JE, Baumann AJ, et al. Validation of Clinically Relevant Thresholds of Esophagogastric Junction Obstruction Using FLIP Panometry. Clin Gastroenterol Hepatol. 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carlson DA, Kahrilas PJ, Lin Z, et al. Evaluation of Esophageal Motility Utilizing the Functional Lumen Imaging Probe. Am J Gastroenterol. 2016;111(12):1726–35.PMC5224528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carlson DA, Kou W, Lin Z, et al. Normal Values of Esophageal Distensibility and Distension-Induced Contractility Measured by Functional Luminal Imaging Probe Panometry. Clin Gastroenterol Hepatol. 2019;17(4):674–81 e1.6360138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carlson DA, Baumann AJ, Donnan EN, Krause A, Kou W, Pandolfino JE. Evaluating esophageal motility beyond primary peristalsis: Assessing esophagogastric junction opening mechanics and secondary peristalsis in patients with normal manometry. Neurogastroenterol Motil. 2021:e14116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ang D, Hollenstein M, Misselwitz B, et al. Rapid Drink Challenge in high-resolution manometry: an adjunctive test for detection of esophageal motility disorders. Neurogastroenterol Motil. 2017;29(1) [DOI] [PubMed] [Google Scholar]
- 14.Krause AJ, Su H, Triggs JR, et al. Multiple rapid swallows and rapid drink challenge in patients with esophagogastric junction outflow obstruction on high-resolution manometry. Neurogastroenterol Motil. 2020:e14000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sanagapalli S, McGuire J, Leong RW, et al. The Clinical Relevance of Manometric Esophagogastric Junction Outflow Obstruction Can Be Determined Using Rapid Drink Challenge and Solid Swallows. Am J Gastroenterol. 2021;116(2):280–8 [DOI] [PubMed] [Google Scholar]
- 16.Jonasson C, Wernersson B, Hoff DA, Hatlebakk JG. Validation of the GerdQ questionnaire for the diagnosis of gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2013;37(5):564–72 [DOI] [PubMed] [Google Scholar]
- 17.Taft TH, Riehl M, Sodikoff JB, et al. Development and validation of the brief esophageal dysphagia questionnaire. Neurogastroenterol Motil. 2016;28(12):1854–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eckardt VF, Aignherr C, Bernhard G. Predictors of outcome in patients with achalasia treated by pneumatic dilation. Gastroenterology. 1992;103(6):1732–8 [DOI] [PubMed] [Google Scholar]
- 19.Taft TH, Carlson DA, Triggs J, et al. Evaluating the reliability and construct validity of the Eckardt symptom score as a measure of achalasia severity. Neurogastroenterol Motil. 2018;30(6):e13287.5992017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boeckxstaens GE, Annese V, des Varannes SB, et al. Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med. 2011;364(19):1807–16 [DOI] [PubMed] [Google Scholar]
- 21.van Hoeij FB, Smout AJ, Bredenoord AJ. Characterization of idiopathic esophagogastric junction outflow obstruction. Neurogastroenterol Motil. 2015;27(9):1310–6 [DOI] [PubMed] [Google Scholar]
- 22.Schupack D, Katzka DA, Geno DM, Ravi K. The clinical significance of esophagogastric junction outflow obstruction and hypercontractile esophagus in high resolution esophageal manometry. Neurogastroenterol Motil. 2017;29(10):1–9 [DOI] [PubMed] [Google Scholar]
- 23.Triggs JR, Carlson DA, Beveridge C, Kou W, Kahrilas PJ, Pandolfino JE. Functional Luminal Imaging Probe Panometry Identifies Achalasia-Type Esophagogastric Junction Outflow Obstruction. Clin Gastroenterol Hepatol. 2020;18(10):2209–17.PMC7246143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Babaei A, Lin EC, Szabo A, Massey BT. Determinants of pressure drift in Manoscan() esophageal high-resolution manometry system. Neurogastroenterol Motil. 2015;27(2):277–84.PMC4437530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Su H, Krause AJ, Masihi M, et al. Normal Values of High-resolution Manometry Parameters With Provocative Maneuvers. J Neurogastroenterol Motil. 2021;27(3):354–62.PMC8266507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Triggs JR, Carlson DA, Beveridge C, et al. Upright Integrated Relaxation Pressure Facilitates Characterization of Esophagogastric Junction Outflow Obstruction. Clin Gastroenterol Hepatol. 2019;17(11):2218–26 e2.PMC6663640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blonski W, Kumar A, Feldman J, Richter JE. Timed Barium Swallow: Diagnostic Role and Predictive Value in Untreated Achalasia, Esophagogastric Junction Outflow Obstruction, and Non-Achalasia Dysphagia. Am J Gastroenterol. 2018;113(2):196–203 [DOI] [PubMed] [Google Scholar]
- 28.Baumann AJ, Donnan EN, Triggs JR, et al. Normal Functional Luminal Imaging Probe Panometry Findings Associate With Lack of Major Esophageal Motility Disorder on High-Resolution Manometry. Clin Gastroenterol Hepatol. 2021;19(2):259–68 e1.PMC7502471 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


