Corresponding Author

Key Words: acute myocardial infarction, cardiopulmonary arrest, in-hospital mortality, risk factor, young patients
It is widely known that acute myocardial infarction (AMI) is associated with various potential undesirable complications ranging from arrhythmias, pericardial inflammation, and cardiopulmonary arrest (CPA) to death. Although advancements in treatment, including primary percutaneous intervention (PCI), have reduced post-AMI mortality rates in the elderly, the reductions have been less marked in younger adults, especially women.1,2 Unfortunately, disability and mortality in young adults are associated with grave social and economic consequences.
In this issue of JACC: Asia, Ando et al3 report a large retrospective cohort study focused on evaluating in-hospital adverse outcomes and associated factors in young patients with AMI in Japan who underwent PCI.
The study entailed extracting patient-level data from the large J-PCI (Japanese Percutaneous Coronary Intervention) registry over 5 years, from January 2014 to December 2018. The study evaluated 213,197 cases, of whom 23,985 (11.2%) were young, aged between 20 and 49 years, whereas the vast majority (n = 189,312) were older (50-80 years). The inclusion criteria for the study were individuals who had both experienced an AMI based on a protocol-based definition (n = 277,015) and were aged ≥19 years and ≤80 years.
The primary endpoints of interest were: 1) CPA at presentation to the hospital (asystole, ventricular fibrillation, and pulseless ventricular tachycardia that required cardiopulmonary resuscitation within 24 hours before PCI); 2) in-hospital (30-day) mortality; and 3) bleeding complications.
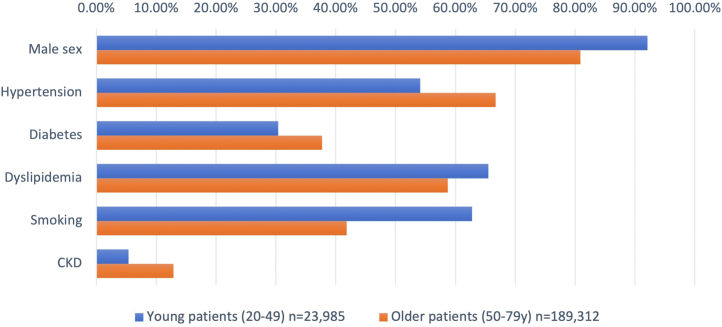
As compared with the older patients, younger patients were predominantly male, had lower levels of traditional coronary risk factors (eg, diabetes and hypertension), lower levels of comorbidities (history of myocardial infarction, history of heart failure, chronic kidney disease [CKD]) but higher prevalence of smoking and dyslipidemia (Figure 1). Although the in-hospital mortality was higher in older compared with younger patients, the relative risk of CPA at presentation was about 1.5 times higher in younger patients than in older patients. Moreover, in a subgroup analysis restricted to young patients, those with CPA at presentation had 10-fold higher risk of in-hospital mortality than counterparts without CPA. CKD was independently associated was each adverse endpoint: CPA at presentation, in-hospital mortality, and bleeding complications.
Figure 1.
Characteristics of Young and Old Patients With Myocardial Infarction in Japan
Comparison of risk factors between young (20-49 years) and older (50-79 years) patients with acute myocardial infarction registered in the J-PCI (Japan-Percutaneous Coronary Intervention) registry during 2004 to 2008. CKD = chronic kidney disease.
Thus, Ando et al3 show that only a small proportion of patients with AMI requiring PCI are young, and their in-hospital mortality is much lower than in older patients. However, their findings are alarming: CPA at presentation is more likely to occur in younger patients. Furthermore, presentation with CPA substantially elevates the risk of death in younger patients. These findings are consistent with other studies done worldwide, albeit of smaller size.
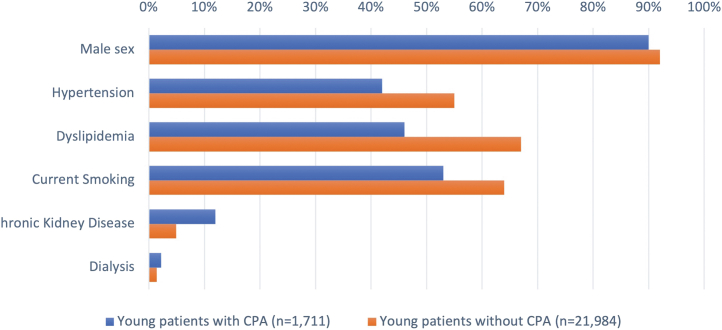
The exact mechanisms behind younger patients being more susceptible to CPA and possibly related mortality are poorly understood. Several potential explanations exist but need further evaluation. First, “ischemic preconditioning" may play a role here. This term refers to the notion that the myocardium adapts to transiently reduced coronary perfusion over time in several or complex atherosclerotic lesions.4 Older patients with previous heart and/or coronary disease have myocardium conditioned to handle transient reductions in perfusion, perhaps contributing to lower rates of post-treatment reperfusion injuries than in younger patients.5 Younger patients may have "immature ischemic preconditioning" and therefore are more likely to present with CPA after AMI. Second, differential pathogeneses of AMI in the young vs older adults could be 1 of the reasons. In older patients, rupture of atherosclerotic plaques is a common cause of AMI, whereas coronary vasospasms and plaque erosion, often a consequence of physical or emotional stress, are more common in younger patients.6 Epidemiologic studies suggest a link between anxiety and psychosocial stress and cardiac arrests.7 Third, the differential risk factors and comorbidities may also have a unique role in adverse post-AMI presentation and outcomes between young and older patients. For example, smoking and dyslipidemia were much more common risks in younger patients. By contrast, diabetes, previous MI, congestive heart failure, and hypertension were far more common in older patients, which enhances the likelihood of ischemic preconditioning, which tends to protect from CPA. Furthermore, young patients who experienced CPA were more likely to die in the presence of CKD (Figure 2). This is unsurprising because CKD is an independent risk factor for CVD mortality, and the presentation of AMI is often atypical in patients with CKD.8,9
Figure 2.
Characteristics of Young Patients With and Without CPA in Japan
Comparison of risk factors between young presenting with versus without cardiopulmonary arrest (CPA) and registered in the J-PCI (Japan-Percutaneous Coronary Intervention) registry during 2004 to 2008.
The main strengths of the work by Ando et al3 include a large database with a sizeable number of patients <50 years of age, and a comprehensive PCI registry inclusive of patients from all public and private hospitals in Japan with a strong quality assurance program.
However, the findings of Ando et al3 must be viewed in consideration of several limitations. First are the potential selection biases inherent to all registry data. Only patients with AMI who received PCI qualified for the study. This excludes patients with AMI who were unable to arrive to a 24-hour PCI-enabled hospital and those too critically ill (especially elderly patients) to receive the needed therapy to meet eligibility criteria.
Second, J-PCI registry data included too few women. This is surprising because younger women with diabetes and AMI have been shown to have higher mortality than younger men.10 Thus, potential under-representation of women in the J-PCI registry could affect the validity and generalizability of the findings.
Third, it is interesting that in the multivariable models, smoking appeared to lower the risk of adverse outcomes in patients with AMI. Notwithstanding the flawed notion of a “smoker’s paradox,” this seemingly protective association could reflect a bias on when and how J-PCI collected information on “current” smoking.11 Patients who experience AMI, especially those critically ill (and more likely to have an adverse prognosis), tend to quit smoking immediately, potentially underestimating the relationship between smoking and adverse events in a retrospective study. It is well-established that smoking is 1 of the most powerful risk factors for AMI and is associated with adverse outcomes even after PCI.11,12
Fourth, information on some key socioeconomic factors (eg, income, employment), co-morbid conditions (eg, Kawasaki disease) and use of oral contraceptives that are associated with AMI were unavailable.13 Those patients with AMI that receive welfare assistance in Japan are more likely to be younger and have poorer prognoses.14 It is possible that the young patients with an excess of these unfavorable factors thereby leading to higher risk of CPA at presentation of AMI.
Fifth, the analysis implying higher mortality after CPA in younger patients was restricted to a subgroup of younger patients only, which could increase the possibility of a chance finding.15 Finally, the retrospective observational nature of the study precludes causality in all the relationships. Nevertheless, the analysis by Ando et al3 provides valuable insights for future research and has public health implications.
Overall, the findings of Ando et al3 underscore the necessity of implementing preventative public health legislation for tobacco control, other healthy lifestyle measures, and preventive pharmacologic interventions in patients at high risk of coronary heart disease.16 Future research is needed to corroborate these findings and must try to address the potential under-representation of women in PCI registries. Etiological research on AMI and adverse outcomes, and more effective strategies for prevention and treatment are also needed. Clinicians must also be aware of the elevated risks of AMI in young patients and address the potential gender bias by appropriately evaluating and treating women at high risk or with AMI.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Wilmot K.A., O'Flaherty M., Capewell S., Ford E.S., Vaccarino V. Coronary heart disease mortality declines in the United States from 1979 through 2011: evidence for stagnation in young adults, especially women. Circulation. 2015;132(11):997–1002. doi: 10.1161/CIRCULATIONAHA.115.015293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zaman S., Kovoor P. Sudden cardiac death early after myocardial infarction: pathogenesis, risk stratification, and primary prevention. Circulation. 2014;129(23):2426–2435. doi: 10.1161/CIRCULATIONAHA.113.007497. [DOI] [PubMed] [Google Scholar]
- 3.Ando H., Yamaji K., Kohsaka S., et al. Clinical presentation and in-hospital outcomes of acute myocardial infarction in young patients: Japanese nationwide registry. JACC: Asia. 2022;2(5):574–585. doi: 10.1016/j.jacasi.2022.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kloner R.A. Clinical application of remote ischemic preconditioning. Circulation. 2009;119(6):776–778. doi: 10.1161/CIRCULATIONAHA.108.832832. [DOI] [PubMed] [Google Scholar]
- 5.Heinen A., Behmenburg F., Aytulun A., et al. The release of cardioprotective humoral factors after remote ischemic preconditioning in humans is age- and sex-dependent. J Transl Med. 2018;16(1):112. doi: 10.1186/s12967-018-1480-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klein L.W., Nathan S. Coronary artery disease in young adults. J Am Coll Cardiol. 2003;41(4):529–531. doi: 10.1016/s0735-1097(02)02861-9. [DOI] [PubMed] [Google Scholar]
- 7.Batelaan N.M., Seldenrijk A., van den Heuvel O.A., et al. Anxiety, mental stress, and sudden cardiac arrest: epidemiology, possible mechanisms and future research. Front Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.813518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gansevoort R.T., Correa-Rotter R., Hemmelgarn B.R., et al. Chronic kidney disease and cardiovascular risk: epidemiology, mechanisms, and prevention. Lancet. 2013;382(9889):339–352. doi: 10.1016/S0140-6736(13)60595-4. [DOI] [PubMed] [Google Scholar]
- 9.Sarnak M.J., Amann K., Bangalore S., et al. Chronic kidney disease and coronary artery disease: JACC state-of-the-art review. J Am Coll Cardiol. 2019;74(14):1823–1838. doi: 10.1016/j.jacc.2019.08.1017. [DOI] [PubMed] [Google Scholar]
- 10.Wang Y., O'Neil A., Jiao Y., et al. Sex differences in the association between diabetes and risk of cardiovascular disease, cancer, and all-cause and cause-specific mortality: a systematic review and meta-analysis of 5,162,654 participants. BMC Med. 2019;17(1):136. doi: 10.1186/s12916-019-1355-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Redfors B., Furer A., Selker H.P., et al. Effect of smoking on outcomes of primary PCI in patients with STEMI. J Am Coll Cardiol. 2020;75(15):1743–1754. doi: 10.1016/j.jacc.2020.02.045. [DOI] [PubMed] [Google Scholar]
- 12.Wilson K., Gibson N., Willan A., Cook D. Effect of smoking cessation on mortality after myocardial infarction: meta-analysis of cohort studies. Arch Intern Med. 2000;160(7):939–944. doi: 10.1001/archinte.160.7.939. [DOI] [PubMed] [Google Scholar]
- 13.Nakamura Y., Yanagawa H., Kawasaki T. Mortality among children with Kawasaki disease in Japan. N Engl J Med. 1992;326(19):1246–1249. doi: 10.1056/NEJM199205073261903. [DOI] [PubMed] [Google Scholar]
- 14.Watanabe S., Usui M. Clinical features of ST-segment elevation myocardial infarction in patients receiving welfare public assistance in urban area of Japan. J Cardiol. 2021;77(4):404–407. doi: 10.1016/j.jjcc.2020.10.013. [DOI] [PubMed] [Google Scholar]
- 15.Ioannidis J.P.A. Why most published research findings are false. PLoS Med. 2005;2(8):e124. doi: 10.1371/journal.pmed.0020124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Herman P.M., Walsh M.E. Hospital admissions for acute myocardial infarction, angina, stroke, and asthma after implementation of Arizona's comprehensive statewide smoking ban. Am J Public Health. 2011;101(3):491–496. doi: 10.2105/AJPH.2009.179572. [DOI] [PMC free article] [PubMed] [Google Scholar]